Introduction
Primary central nervous system lymphoma (PCNSL) is a
type of non-Hodgkin lymphoma that originates in the intracranial
lymphoreticular system. The average annual incidence rate of PCNSL
was 0.44 cases/100,000 individuals/year in the US in 2017–2021, and
the incidence of PCNSL was significantly higher in males than
females (incident rate ratio=1.20, P<0.0001). PCNSL accounts for
4–6% of extra-nodal lymphomas and 1.8% of all brain and other
central nervous system tumors. In addition, the 1-, 5- and 10-year
survival rates for PCNSL were 56.8, 40.2 and 32.5% in 2004–2020.
Therefore, PCNSL had a low incidence, high mortality and poor
outcomes (1–3). Diffuse large B-cell lymphoma (DLBCL)
is the most common subtype, accounting for ~90% of PCNSLs (4,5). Most
PCNSL lesions are supratentorial and periventricular, often
involving the corpus callosum, basal ganglia, central grey matter,
hypothalamus, posterior fossa or thalamus (6,7). The
occurrence of multiple PCNSL extending into the ventricle system,
medulla and interpeduncular cistern is rare. In the present study,
a case of multiple PCNSL arising in the ventricle system, and
involving the medulla and interpeduncular cistern, is reported. The
present study also summarized cases of PCNSL arising in the
ventricular system, aiming to raise awareness of this rare brain
tumor and describe the treatment experience.
Case report
A 67-year-old male with no history of
immunosuppression presented with nausea and vomiting after a meal
without any obvious inducement for 6 months, and recent onset of
orthostatic hypotension 2 weeks prior to being admitted to the
General Hospital of the Western Theater Command (Chengdu, China) in
December 2024. Neurological examination showed no focal
deficits.
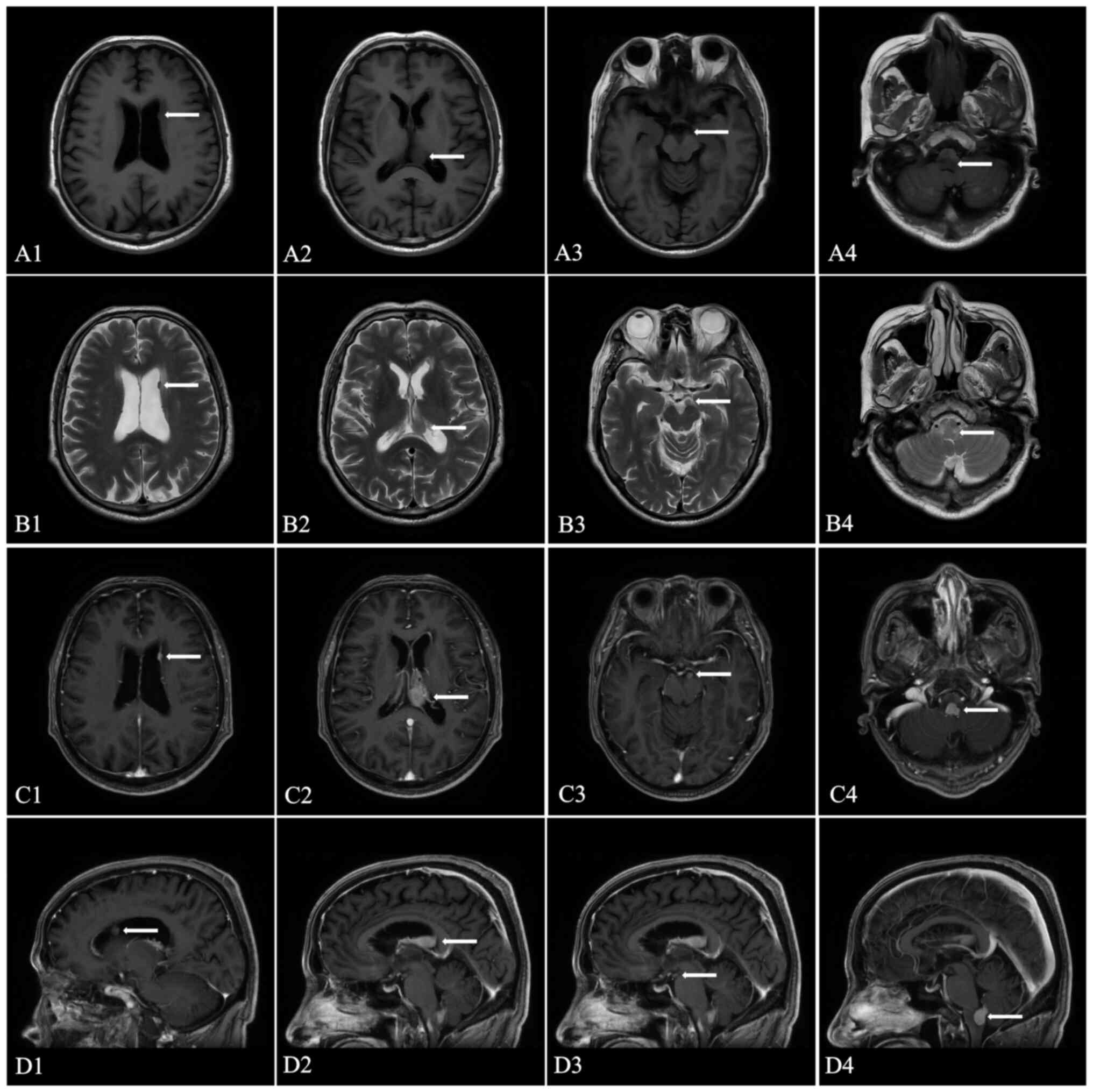
Magnetic resonance imaging (MRI) demonstrated
multiple slightly longer T1 and T2 signal soft-tissue lesions in
the left lateral ventricle, 4th ventricle, medulla and
interpeduncular cistern (Fig. 1A and
B). These lesions showed notable uniform enhancement after
injection of gadolinium-based contrast medium (Fig. 1C and D). The lesion in the 4th
ventricle extended to the medulla with perilesional edema, and
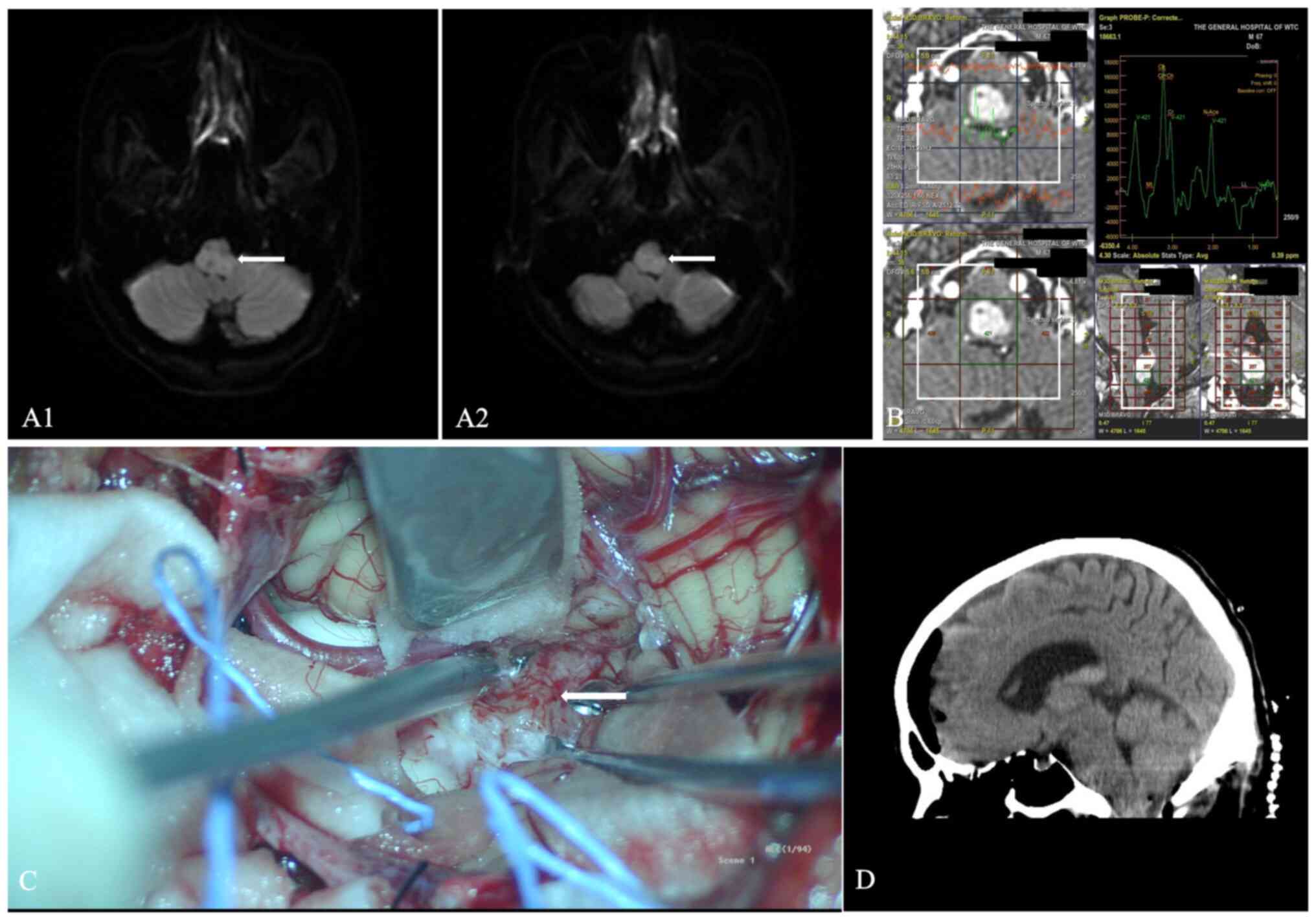
without obstructive hydrocephalus. The lesion in the medulla showed
a slight diffusion restriction on diffusion-weighted imaging and a
low signal using apparent diffusion coefficient imaging (Fig. 2A). Furthermore, magnetic resonance
spectroscopy demonstrated elevation of total choline and a decrease
of N-acetylaspartate levels at the location of the medulla lesion
(Fig. 2B). An MRI of the spine
revealed no obvious malignant neoplasm. Tumor markers such as
CA19-9, α-fetoprotein, CA125 and carcinoembryonic antigen were
negative. A malignant lymphoma was suspected, but ependymoma,
glioma or metastasis could not be excluded.
A retrospective analysis of 9,000 patients in 3
datasets reported that craniotomy is associated with increased
survival compared with a biopsy for patients with PCNSL (8). The pressure on the medulla from the
lesion may cause orthostatic hypotension; thus, the maximum safe
resection of the lesion in the 4th ventricle was performed by a
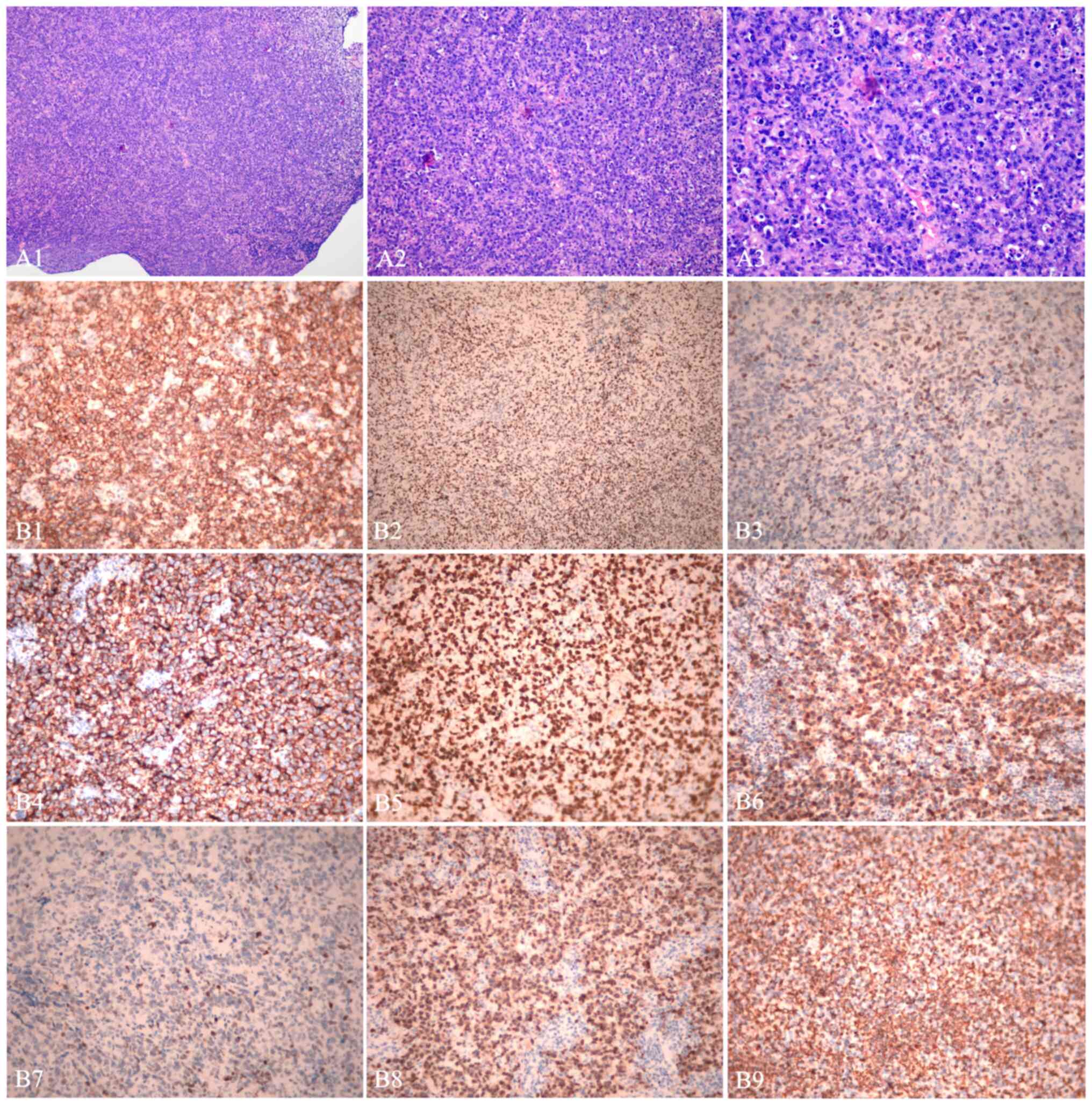
midline posterior fossa craniotomy (Fig. 2C and D). H&E staining [tissues
were fixed in 4% paraformaldehyde for 2 h, dehydrated in 70–90–100%
ethanol (10 min each) sequentially, and cleared twice in xylene (5
min). Paraffin slices (5 µm) were incubated in Mayer's hematoxylin
solution (1 min) and differentiated in 1% HCl ethanol (30 sec).
Sections were stained with eosin Y solution (1 min), dehydrated
through 70–100% ethanol and cleared with xylene. Slides were
mounted with neutral-buffered formalin-based medium and covered
with glass slides. All of the above steps were performed at room
temperature (21–25°C). Finally, slides were observed under a
microscope (BX45; Olympus Corp.)] indicated that there was atypical
lymphocyte infiltration, medium size rounded cells with irregularly
shaped hyperchromatic nuclei, morphological homogeneity, prominent
nucleoli and a small amount of eosinophilic cytoplasm (Fig. 3A). The immunohistochemical staining
[using the LUMATAS BIOYSTEMS fully automatic immunohistochemical
instrument (Titan). Paraffin slices were deparaffinized and
rehydrated (21–25°C). After antigens were retrieved with Tris-EDTA
buffer (pH 9.0) for 15 min at 100°C, endogenous peroxidase was
blocked with 3% hydrogen peroxide for 10 min (21–25°C). The slices
were incubated with primary antibodies (purchased from Maxim
Biotechnologies) against ATRX chromatin remodeler (1:100 dilution;
cat. no. MAB-0855), terminal deoxynucleotidyl transferase (1:100;
MAB-0676), Bcl-2 (1:100; MAB-0711), Bcl-6 (1:100; MAB-0746), c-Myc
(1:100; RMA-0803), CD10 (1:100; MAB-0668), CD20 (1:100; MAB-0669),
CD21 (1:100; RMA-0811), CD3 (1:100; MAB-0740), CD5 (1:100;
MAB-0827), pan-cytokeratin (1:100; RAB-0050), epithelial membrane
antigen (1:100; MAB-1101), glial fibrillary acidic protein (1:100;
MAB-0769), H3K27M (1:100; RMA-0840), isocitrate dehydrogenase 1
R132H (1:100; MAB-0733), Ki-67 (1:100; RMA-0542), multiple myeloma
oncogene 1 (MUM-1; 1:100; MAB-0885), neuronal nuclear antigen
(1:100; MAB-0578), p53 (1:100; MAB-0674), paired box 5 (PAX-5;
1:100; MAB-0706), S-100 (1:100; RMA-1705) and vimentin (1:100;
MAB-0735) for 30 min (21–25°C). The samples were the incubated with
the secondary antibodies (undiluted highly sensitive enzyme-labeled
anti-mouse/rabbit IgG polymer; cat. no. TT-0805; Maxim
Biotechnologies) for 15 min (21–25°C) and washed with PBS thrice (5
min each), followed by the addition of diaminobenzidine (DAB)
(21–25°C). At last, the slices were counterstained with Mayer's
hematoxylin for 5 min (21–25°C) and observed under a microscope
(BX45; Olympus Corp.)]. The results were as follows: ATRX chromatin
remodeler (−), terminal deoxynucleotidyl transferase (−), Bcl-2 (+;
80%), Bcl-6 (+; 80%), c-Myc (+; 40%), CD10 (−), CD20 (+), CD21 (−),
CD3 (−), CD5 (−), pan-cytokeratin (−), epithelial membrane antigen
(−), glial fibrillary acidic protein (−), H3K27M (−), isocitrate
dehydrogenase 1 R132H (−), Ki-67 (+; 80%), MUM-1 (+), neuronal
nuclear antigen (−), p53 (+), paired box 5 (+), S-100 (−) and
vimentin (+) (Fig. 3B). After the
pathological slices were processed, analysis of Epstein-Barr
virus-encoded small RNAs (EBER) was performed with an EBER test Kit
[in situ hybridization (ISH); cat. no. ISH-7001; ZSGB-BIO]
according to the manufacturer's instructions, and EBER was negative
(data not shown). The immunohistochemical staining indicated
positive expression of B-cell markers CD20, PAX-5 and MUM-1, and
the final pathological diagnosis was DLBCL with a Ki-67
proliferation index of 80% (9). In
addition, the positive expression levels of Bcl-2, Bcl-6 and c-Myc
are prognostic markers in PCNSL (10). The relationship between Epstein-Barr
virus and PCNSL remains elusive, although EBER negativity does not
exclude PCNSL, but helps to exclude EBV-associated differential
diagnoses such as lymphomatoid granulomatosis (11). The patient was subsequently
transferred to the hematology department for chemotherapy, where he
received 8 cycles of high-dose methotrexate (MTX), along with
zanubrutinib and rituximab (rituximab 375 mg/m2 on day
0, MTX 3.5 g/m2 on day 1, zanubrutinib 80 mg for 10
days) (12,13). The patient achieved remission of
symptoms after chemotherapy, the antitumor effect was excellent and
the brain lesions had disappeared on the brain MRI at 6 months
after treatment (data not shown). The follow up (including cranial
MRI) was every 3 months in the first 2 years from the end of
treatment, then every 6 months for another 3 years and subsequently
on an annual basis.
Discussion
The origin of PCNSL is elusive; however, deficiency
of the immune system is a notable risk factor (14,15).
It has been reported that the incidence rate of patients with PCNSL
without immunodeficiency is increasing, with population aging being
an important factor (2,16). PCNSL is rare, accounting for ~4% of
intracranial tumors. Furthermore, PCNSL occurring in the ventricle
system is even rarer.
The present literature review of PCNSL originating
from the ventricular system discusses 20 cases that have been
reported (Table I) (1,5,16–33).
In the present review, these cases revealed that PCNSL had a median
age of onset of 51.4 years and had a male predominance
(male:female, 14:6). Although immunodeficiency is a risk factor for
PCNSL, no patients with immunodeficiency were found in the present
literature review. However, it is possible that PCNSL in the
ventricular system is very rare and the small sample size may be
underpowered to demonstrate that immunodeficiency is a risk factor
for PCNSL. In addition, previous studies demonstrated that there is
an increase in the incidence of PCNSL with advancing age, and which
has been attributed to a possible reduction in immunological
surveillance or an increased number of somatic mutations that
accrue over a lifetime (34,35).
Despite the patients being immunocompetent, the proportion of
patients aged ≥50 years was ~66.67% (14/21). Therefore, it could be
considered that reduction in immunological surveillance or
increased somatic mutations with age may be the potential risk
factors for PCNSL as opposed to immunodeficiency.
 | Table I.Literature review of 20 cases of
PCNSL originating from the ventricular system. |
Table I.
Literature review of 20 cases of
PCNSL originating from the ventricular system.
| Author, year | Age, years | Sex | Immune status | Symptoms | Location | Solitary or
multiple | Lymphoma
subtype | Treatment | Outcome | (Refs.) |
|---|
| Haegelen et
al, 2001 | 33 | Female |
Immunocompetent | Headaches, vertigo
BCL | 4th ventricle | Solitary | High-grade | Resection,
chemoradiation | No recurrence at 7
months | (33) |
| Pascual et
al, 2002 | 57 | Female |
Immunocompetent | Visual
deterioration, diabetes insipidus and mental confusion | 3rd ventricle | Solitary | Diffuse non-Hodgkin
lymphoma | Resection,
chemoradiation | No recurrence at 6
months | (32) |
| Kelley et
al, 2005 | 53 | Male |
Immunocompetent | Headaches,
seizure | Lateral
ventricle | Solitary | MALT lymphomas | Resection,
chemotherapy | No recurrence at 6
months | (31) |
| Jung et al,
2006 | 63 | Male |
Immunocompetent | Seizure | Lateral
ventricle | Solitary | MALT lymphomas | Resection,
chemotherapy | No information | (30) |
| Jiang et al,
2011 | 14 | Male |
Immunocompetent | Headache | Lateral
ventricle | Solitary | Burkitt
lymphoma | Resection,
chemoradiation | No recurrence at 18
months | (29) |
| Bokhari et
al, 2013 | 50 | Male |
Immunocompetent | Vomiting,
nausea | 4th ventricle | Solitary | High-grade BCL | Resection,
chemoradiation | No recurrence at 18
months | (16) |
| Rao et al,
2013 | 59 | Male |
Immunocompetent | Vomiting, vertigo,
tremors, unsteady gait | 4th ventricle | Solitary | PCNSL | Resection,
chemoradiation | No information | (28) |
| Alabdulsalam et
al, 2014 | 18 | Male |
Immunocompetent | Ataxia, double
vision, facial asymmetry, tinnitus, dysphagia | 4th ventricle | Solitary | Burkitt
lymphoma | Resection,
chemotherapy | No recurrence at 18
months | (27) |
| Liao et al,
2014 | 77 | Male |
Immunocompetent | Vertigo, nausea,
vomiting, unsteady gait | Lateral
ventricle | Solitary | MALT lymphomas | Resection,
chemotherapy | No recurrence at 14
months | (26) |
| Cellina et
al, 2015 | 65 | Male |
Immunocompetent | Weight loss,
headaches, blurred vision, asthenia, unsteady gait | Ventricular
system | Multiple | DLBCL | Biopsy,
chemotherapy | No information | (25) |
| Hsu et al,
2015 | 61 | Male |
Immunocompetent | Headache,
dizziness, unsteady gait | 4th ventricle | Solitary | DLBCL | Resection,
chemotherapy | No recurrence at 3
months | (24) |
| Liu et al,
2016 | 6 | Male |
Immunocompetent | Headache | 4th ventricle | Solitary | Burkitt
lymphoma | Resection,
chemotherapy | No recurrence at 6
months | (23) |
| Brozovich et
al, 2019 | 65 | Male |
Immunocompetent | Seizures, diplopia,
vertigo, nausea, vomiting | 4th ventricle | Solitary | DLBCL | Biopsy,
chemotherapy | No recurrence at 10
months | (4) |
| Nohira et
al, 2021 | 45 | Female |
Immunocompetent | Headache, gait
instability, nausea | 3rd ventricle | Solitary | PLML | Biopsy,
chemotherapy | No recurrence at 24
months | (22) |
| Hajtovic et
al, 2022 | 69 | Female |
Immunocompetent | Headache | Lateral
ventricle | Solitary | MALT lymphomas | Biopsy,
chemotherapy | No recurrence at 6
months | (21) |
| Holanda et
al, 2022 | 45 | Male |
Immunocompetent | Headache, vomiting,
weight loss | 4th ventricle | Solitary | PCNSL | Resection,
chemoradiation | No information | (20) |
| Kojima et
al, 2022 | 54 | Male |
Immunocompetent | Headache,
nausea | 4th ventricle | Solitary | DLBCL | Biopsy,
chemotherapy | No recurrence at 20
months | (19) |
| Muroya et
al, 2023 | 75 | Female |
Immunocompetent | Amnesia, gait
disturbance | 3rd ventricle | Solitary | DLBCL | Biopsy,
chemotherapy | No recurrence at 14
months | (18) |
| Zhao et al,
2023 | 48 | Male |
Immunocompetent | Blurred vision,
dizziness, staggering | 4th ventricle | Solitary | DLBCL | Resection,
chemotherapy | No recurrence at 9
months | (1) |
| Wu et al,
2024 | 71 | Female |
Immunocompetent | Dizziness, ataxia,
gait disorder | Lateral ventricle
and 4th ventricle | Multiple | DLBCL | Resection,
chemotherapy | No recurrence at 12
months | (17) |
The symptoms of PCNSL depend on the site of
involvement, and according the literature review and the present
case report, the most common symptom was intracranial hypertension
(headache, nausea and vomiting), followed by focal neurologic
deficits, seizures and altered mental state (1,4,16–33).
The literature review demonstrated that the majority of PCNSL cases
affect the 4th ventricle (55.6%), followed by the lateral ventricle
(27.8%) and 3rd ventricle (16.7%) (1,4,16–33).
According the literature review, most of the PCNSL cases were
solitary (90%) and the minority were multiple (10%) (1,4,16–33).
Therefore, single or multiple mass lesions in the CNS showed
homogeneous gadolinium enhancement should be considered PCNSL,
particularly multiple mass lesions, as multiple mass lesions are
uncommon. DLBCL constituted the majority of PCNSL (35%), followed
by mucosa-assisted lymphoid tissue lymphoma (20%), Burkitt lymphoma
(15%) and primary leptomeningeal malignant lymphoma (5%); however,
25% of cases were undefined PCNSL, including high-grade BCL and
diffuse non-Hodgkin lymphoma (1,4,16–33).
While the treatment of PCNSL has evolved in the past decade, biopsy
followed by chemoradiation therapy is the gold standard treatment
in general (5). In the present
literature review, all patients were found to have undergone biopsy
or resection, adjuvant postoperative chemotherapy, radiotherapy and
other measures to improve the survival rate (1,4,16–33).
In general, due to the potential of multiple PCNSL,
the highly invasive features and the risk of neurologic damage and
implantation metastasis post-operation, total resection of PCNSL is
difficult and discouraged. In addition, previous retrospective
studies have demonstrated that the extent of resection has no
prognostic impact on this disease (35,36).
However, the largest PCNSL trial in Germany has shown that the
progression-free survival and overall survival rates of patients
with subtotal or total resections are markedly improved compared
with biopsied patients (37).
Despite the association between the extent of PCNSL resection and
prognosis not being defined, subtotal or total resection of PCNSL
is encouraged in patients with single lesions if resection is safe.
PCNSL is commonly treated with systemic chemotherapy including MTX
(38%), steroids (13%), radiation (29%) and intrathecal chemotherapy
(9%) (38).
The chemotherapy plan needs to be selected and
adjusted according to the condition of the patient. Advances in
molecular pathology provide more information about unique
characteristics of PCNSL, such as the mechanisms underlying the
pathogenesis and drug resistance in PCNSL, which may help to
identify drug targets and the choice of the therapeutic plan;
however, the patient refused the molecular pathological diagnosis
for personal reasons. High-dose (HD)-MTX, which is a standard
first-line therapy for PCNSL, can markedly improve the overall
survival rate. The CD20 antibody rituximab is a standard component
of the treatment for non-Hodgkin B-cell lymphomas, including DLBCL.
Thus, the current standard adjuvant therapy is HD-MTX and rituximab
is applied as the first-line induction therapy, supplemented by
whole-brain and whole-spinal cord radiotherapy (6). The available evidence suggests PCNSL
with c-Myc and Bcl-2 positive co-expression is rarer and associated
with shorter median overall survival when compared with c-Myc or
Bcl-2 negative (39). The
co-expression of Bcl-2 and c-Myc in the patient of the present case
report indicates a poor prognosis. In addition, the NF-κB/B cell
receptor (BCR) signaling pathway is highly activated in PCNSL and
Bruton's tyrosine kinase (BTK) is a key bridge molecule between
NF-κB and BCR. The treatment scheme containing a BTK inhibitor and
HD-MTX has potential for PCNSL, including relapsed and refractory
PCNSL. Therefore, HD-MTX combined with rituximab and zanubrutinib
(a BTK inhibitor) may be a good prospect for a patient with c-Myc
and Bcl-2 positive expression. Additionally, immunotherapy for
PCNSL, such as chimeric antigen receptor T-cell therapy, has
progressed in previous years (40).
The lesion in the 4th ventricle of the present patient was
relatively independent, caused compression of the medulla and
potential hydrocephalus. The patient underwent a combination of
surgical resection of the lesion in the 4th ventricle and
chemotherapy with MTX, zanubrutinib and rituximab. Due to the
lesions being multiple and dispersed, whole-brain radiotherapy may
have caused severe neurotoxicity; therefore, radiotherapy was not a
priority. Furthermore, a previous study showed that whole-brain
radiotherapy was not associated with improved outcomes in patients
with PCNSL (3). The mechanism of
the formation of multiple PCNSL in the ventricular system in the
present case was elusive; however, it has been reported that PCNSL
likely originates from the choroid plexus (17,41).
As seen on MRI, the patient's lymphoma may have arisen in the
lateral ventricle and appeared to follow the choroid plexus into
the 4th ventricle. In addition, the meningeal dissemination may
also be a reason for multiple lesions in the lateral ventricle,
medulla and interpeduncular cistern. Cerebrospinal fluid (CSF)
cytological assessment is the gold standard for diagnosing
meningeal dissemination of PCNSL. The patient in the present case
study did not consent to lumbar puncture for CSF cytology. For the
diagnosis of PCNSL arising from the ventricular system,
histological confirmation is essential and tumor cell findings in
CSF are also reliable; however, it is not uncommon for CSF samples
from patients with PCNSL to be negative. Monoclonal population or
gene rearrangement analyses by flow cytometry are proposed to
further improve sensitivity (42–44).
In conclusion, the present case study reported a
rare case of PCNSL involving the lateral ventricle, 4th ventricle,
medulla and interpeduncular cistern. The present case adds to the
available evidence that PCNSL is a malignancy that may
predominantly arise in an immunocompetent male. Maximum resection
may be performed to reduce medulla compression symptoms and the
incidence of hydrocephalus to provide a benefit for patient
prognosis.
Acknowledgements
Not applicable.
Funding
The present research was supported by the Spark Talent program
of General Hospital of The Western Theater Command and Research
Project of General Hospital of The Western Theater Command (grant
nos. 2021-XZYG-C37 and 2021-XZYG-A13).
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
QO contributed to writing the manuscript and
acquiring data. BS and JL analyzed data. HS and ZX interpretated
data. YM was involved in the conception and design of the study. QO
and YM confirm the authenticity of all the raw data. All authors
read and approved the final version of the manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Oral and written informed consent was obtained from
the patient for the publication of the case details and any
associated images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Zhao J, Zou C, Guo Z, Cheng P and Lu W:
Primary central nervous system diffuse large B-cell lymphoma in
fourth ventricle: Case report and literature review. Medicine
(Baltimore). 102:e332862023. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Price M, Ballard C, Benedetti J, Neff C,
Cioffi G, Waite KA, Kruchko C, Barnholtz-Sloan JS and Ostrom QT:
CBTRUS statistical report: Primary brain and other central nervous
system tumors diagnosed in the United States in 2017–2021. Neuro
Oncol. 26 (Suppl 6):vi1–vi85. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Janopaul-Naylor JR, Patel JS, Rupji M,
Hoang KB, McCall NS, Qian DC, Shoaf ML, Kothari S, Olson JJ, Shu
HG, et al: Impact of systemic and radiation therapy on survival of
primary central nervous system lymphoma. Cancers (Basel).
17:6182025. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Brozovich A, Ewing D, Burns E, Hatcher C,
Acosta G, Khan U, Chung B, Samuel L, Randhawa J and Pingali SR:
Primary CNS lymphoma arising from the 4(th) ventricle: A case
report and review of the literature. Case Rep Oncol Med.
2019:26717942019.PubMed/NCBI
|
|
5
|
Grommes C, Rubenstein JL, DeAngelis LM,
Ferreri AJM and Batchelor TT: Comprehensive approach to diagnosis
and treatment of newly diagnosed primary CNS lymphoma. Neuro Oncol.
21:296–305. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
DeAngelis L and Batchelor T: Primary CNS
lymphoma: Is there a role for prophylaxis against lymphomatous
meningitis? Expert Rev Neurother. 4 (4 Suppl):S19–2S4. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Cheng L, Zhu H, Wang J, Wang G, Ma X, Zhao
K, Wang J and Shu K: Clinical features, diagnosis, and treatment of
primary intraventricular lymphoma: Insights from a monocentric case
series. Front Neurol. 13:9205052022. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Rae AI, Mehta A, Cloney M, Kinslow CJ,
Wang TJC, Bhagat G, Canoll PD, Zanazzi GJ, Sisti MB, Sheth SA, et
al: Craniotomy and survival for primary central nervous system
lymphoma. Neurosurgery. 84:935–944. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Hadzisejdic I, Klarica L, Babarovic E,
Marijic B, Valkovic T and Jonjic N: Primary nodal unclassifiable
CD20 negative diffuse large B-cell lymphoma with dual IgK and TCR
gene rearrangement: A diagnostic challenge. Clin Pathol.
16:2632010X2211499782023. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Niparuck P, Boonsakan P, Sutthippingkiat
T, Pukiat S, Chantrathammachart P, Phusanti S, Boonyawat K,
Puavilai T, Angchaisuksiri P, Ungkanont A, et al: Treatment outcome
and prognostic factors in PCNSL. Diagn Pathol. 14:562019.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Sadeghipour A, Mohagheghian H, Movahedinia
S, Kosari F and Monabati A: O-6-methylguanine-DNA
methyltransferase, C-MYC, and EBER status in diffuse large B-cell
lymphoma of central nervous system. Int J Mol Cell Med. 13:361–373.
2024.PubMed/NCBI
|
|
12
|
Wang Y, Han J, Yin S, Yang S, Kang X,
Zheng X, Duan L, Li S, Jiang B, Li W and Chen F: Bruton's tyrosine
kinase inhibitor zanubrutinib-based regimens in relapsed/refractory
primary diffuse large B-cell lymphoma of the central nervous
system. Leuk Lymphoma. 66:869–878. 2025. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wang N, Chen FL, Pan L, Teng Y, Wei XJ,
Guo HG, Jiang XM, Huang L, Liu SC, Liang ZL and Li WY: Clinical
outcomes of newly diagnosed primary central nervous system lymphoma
treated with zanubrutinib-based combination therapy. World J Clin
Oncol. 14:606–619. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Haddad R, Alkubaisi A, Al Bozom I, Haider
A and Belkhair S: Solitary primary central nervous system lymphoma
mimicking third ventricular colloid cyst-case report and review of
literature. World Neurosurg. 123:286–294. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Okano R, Suzuki K, Nakano Y and Yamamoto
J: Primary central nervous system lymphoma presenting with
Parkinsonism as an initial manifestation: A case report and
literature review. Mol Clin Oncol. 14:952021. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Bokhari R, Ghanem A, Alahwal M and Baeesa
S: Primary isolated lymphoma of the fourth ventricle in an
immunocompetent patient. Case Rep Oncol Med.
2013:6146582013.PubMed/NCBI
|
|
17
|
Wu YX, Guo L and Guo H: Primary
central-nervous-system lymphoma in the right lateral ventricle and
the fourth ventricle: A case report. Asian J Surg. 47:1696–1698.
2024. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Muroya Y, Suzuki K, Nagasaka S, Nakano Y
and Yamamoto J: Primary central nervous system lymphoma of the
third ventricle with intra-tumoral hemorrhage: A case report and
literature review. Oncol Lett. 25:472023. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kojima Y, Nakajo K, Ichinose T, Morikawa
Y, Osawa M and Goto T: Case report and review of the literature of
primary central nervous system lymphoma of the fourth ventricle.
Surg Neurol Int. 13:5292022. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Holanda TSF, Pimentel IMF, Gosch GO,
Tavora DGF, Bandeira LAB and Filho FL: Immunocompetent patient with
isolated primary fourth ventricle lymphoma. Unusual diagnosis,
their pitfalls, and challenges. Surg Neurol Int. 13:4632022.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Hajtovic S, Yu E, Bershadskiy A, Sacho R
and Gilad R: Primary intracranial marginal zone B-cell lymphoma of
mucosa-associated lymphoid tissue arising in the lateral ventricle:
Case report and review of pathogenesis. Surg Neurol Int.
13:1812022. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Nohira S, Shimato S, Yamanouchi T,
Takeuchi K, Yamamoto T, Ito M, Kato K and Nishizawa T: A case of
primary leptomeningeal lymphoma presenting with hydrocephalus
characterized by disproportionately large fourth ventricle. NMC
Case Rep J. 8:399–404. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Liu H, Hou H and Cheng J: Primary Burkitt
lymphoma of the fourth ventricle mimicking a medulloblastoma in a
child. J Neurooncol. 127:205–207. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Hsu HI, Lai PH, Tseng HH and Hsu SS:
Primary solitary lymphoma of the fourth ventricle. Int J Surg Case
Rep. 14:23–25. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Cellina M, Fetoni V, Baron P, Orsi M and
Oliva G: Unusual primary central nervous system lymphoma location
involving the fourth ventricle and hypothalamus. Neuroradiol J.
28:120–125. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Liao CH, Lin SC, Hung SC, Hsu SP, Ho DM
and Shih YH: Primary large B-cell lymphoma of the fourth ventricle.
J Clin Neurosci. 21:180–183. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Alabdulsalam A, Zaidi SZ, Tailor I, Orz Y
and Al-Dandan S: Primary burkitt lymphoma of the fourth ventricle
in an immunocompetent young patient. Case Rep Pathol.
2014:6309542014.PubMed/NCBI
|
|
28
|
Rao RN, Mishra D, Agrawal P and Kumar R:
Primary B-cell central nervous system lymphoma involving fourth
ventricle: A rare case report with review of literature. Neurol
India. 61:450–453. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Jiang M, Zhu J, Guan YS and Zou LQ:
Primary central nervous system burkitt lymphoma with
non-immunoglobulin heavy chain translocation in right ventricle:
Case report. Pediatr Hematol Oncol. 28:454–458. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Jung TY, Jung S, Lee MC and Lee KH:
Extranodal marginal zone B-cell lymphoma mimicking meningioma in
lateral ventricle: A case report and possible pathogenesis. J
Neurooncol. 80:63–67. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Kelley TW, Prayson RA, Barnett GH, Stevens
GH, Cook JR and His ED: Extranodal marginal zone B-cell lymphoma of
mucosa-associated lymphoid tissue arising in the lateral ventricle.
Leuk Lymphoma. 46:1423–1427. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Pascual JM, Gonzalez-Llanos F and Roda JM:
Primary hypothalamic-third ventricle lymphoma. Case report and
review of the literature. Neurocirugia (Astur). 13:305–310. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Haegelen C, Riffaud L, Bernard M and
Morandi X: Primary isolated lymphoma of the fourth ventricle: Case
report. J Neurooncol. 51:129–131. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Villano JL, Koshy M, Shaikh H, Dolecek TA
and McCarthy BJ: Age, gender, and racial differences in incidence
and survival in primary CNS lymphoma. Br J Cancer. 105:1414–1418.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Bataille B, Delwail V, Menet E,
Vandermarcq P, Ingrand P, Wager M, Guy G and Lapierre F: Primary
intracerebral malignant lymphoma: Report of 248 cases. J Neurosurg.
92:261–266. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Bellinzona M, Roser F, Ostertag H, Gaab RM
and Saini M: Surgical removal of primary central nervous system
lymphomas (PCNSL) presenting as space occupying lesions: A series
of 33 cases. Eur J Surg Oncol. 31:100–105. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Weller M, Martus P, Roth P, Thiel E and
Korfel A; German PCNSL Study Group, : Surgery for primary CNS
lymphoma? Challenging a paradigm. Neuro Oncol. 14:1481–1484. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Ball MK, Morris JM, Wood AJ, Meyer FB,
Kaszuba MC and Raghunathan A: Ventricle-predominant primary CNS
lymphomas: Clinical, radiological and pathological evaluation of
five cases and review of the literature. Brain Tumor Pathol.
37:22–30. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Ge L, Lu S, Xu L and Yan H: MYC, BCL2, and
BCL6 expression as prognostic indicators in primary central nervous
system lymphoma: A systematic review and meta-analysis. Clin Neurol
Neurosurg. 208:1068382021. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Aydin I, Hanalioglu S, Peker HO, Turan Y,
Kina H, Cikla U and Baskaya MK: The tonsillouvular fissure
approach: Access to dorsal and lateral aspects of the fourth
ventricle. World Neurosurg. 114:e1107–e1119. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Baraniskin A and Schroers R: Modern
cerebrospinal fluid analyses for the diagnosis of diffuse large
B-cell lymphoma of the CNS. CNS Oncol. 3:77–85. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Zhao H, Ma M, Zhang L, Zheng G, Lv H, Liu
J, Li X, Song B and Zhang G: Diagnosis of central nervous system
lymphoma via cerebrospinal fluid cytology: A case report. BMC
Neurol. 19:902019. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Bromberg JE, Breems DA, Kraan J, Bikker G,
van der Holt B, Smitt PS, van den Bent MJ, van't Veer M and Gratama
JW: CSF flow cytometry greatly improves diagnostic accuracy in CNS
hematologic malignancies. Neurology. 68:1674–1679. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Fischer L, Martus P, Weller M, Klasen HA,
Rohden B, Röth A, Storek B, Hummel M, Nägele T, Thiel E and Korfel
A: Meningeal dissemination in primary CNS lymphoma: prospective
evaluation of 282 patients. Neurology. 71:1102–1108. 2008.
View Article : Google Scholar : PubMed/NCBI
|