Introduction
Cervical cancer remains a significant global health
concern, ranking as the fourth most common cancer and the fourth
leading cause of cancer death among women worldwide, with 604,127
new cases and 341,831 associated deaths annually (1). Cervical cancer represents a
substantial portion of the global cancer burden for women,
particularly in low- and middle-income countries, which carry the
majority of this burden (2).
Cervical cancer is one of the most prevalent gynecological
malignancies globally and is closely associated with human
papillomavirus infection, viral persistence, progression and
invasion (3). Accurate preoperative
evaluation is important for effective treatment planning and
prognosis, as it helps to identify potential risks, improve patient
outcomes and reduce the likelihood of complications (4). Preoperative assessment involves
gathering information from multiple sources, including medical
history, interviews, physical examinations and medical tests
(5).
Accurate preoperative assessment of lesion type,
extent and depth of invasion is required to improve the complete
resection rate and reduce the risk of additional surgery (6). The analysis of pathological features,
such as tumor size, stromal invasion and lymph node metastasis
(LNM), plays a notable role in determining the extent of disease
and guiding therapeutic strategies (7). Determining these features is important
for deciding the appropriate management approach, as treatment is
tailored based on the nature of the tumor (7). Pathology results of resected tissues
are often used as diagnostic criteria, and imaging features such as
nodule size and a ground glass sign are significantly correlated
with pathological types (8).
Magnetic resonance imaging (MRI) has emerged as a
valuable tool in the preoperative assessment of cervical cancer,
offering superior soft-tissue contrast and detailed anatomical
visualization compared with other imaging modalities, including
ultrasound, computed tomography (CT) and positron emission
tomography (PET)-CT. MRI has become a notable imaging modality in
radiotherapy, particularly with the development of novel MRI and
image-guidance techniques (9). MRI
provides detailed anatomical images, and functional MRI monitors
physiological activity by recording blood oxygenation (10). As aforementioned, the utility of MRI
lies in evaluating tumor characteristics, including depth of
stromal invasion and parametrial involvement, which are important
for staging and surgical decision-making. The purpose of the
present study was to further explore the correlation between MRI
findings and pathological features in cervical cancer, aiming to
enhance the accuracy of preoperative evaluation and improve patient
outcomes.
Materials and methods
Ethical approval
All experimental procedures were approved by the
Medical Ethics Committee of The Fifth Affiliated Hospital of
Xinjiang Medical University (Ürümqi, China). Written informed
consent was obtained from all individual participants included in
the study. All experimental procedures were approved by the Medical
Ethics Committee of The Fifth Affiliated Hospital of Xinjiang
Medical University (approval no. 2020065).
Patient information
Data were collected from 110 female patients with
cervical cancer who were admitted to The Fifth Affiliated Hospital
of Xinjiang Medical University between December 2019 and December
2024.
Inclusion criteria were as follows: i) Diagnosis of
cervical cancer confirmed by surgery or pathological biopsy; ii) no
contraindications for MRI examination; iii) complete imaging and
clinical pathological data; and iv) patients with clear
consciousness, normal communication ability and cooperative
attitude towards examination. Exclusion criteria included: i)
Presence of other systemic malignant tumors; ii) comorbid
psychiatric disorders; and iii) patients transferred to other
hospitals during the study.
The ages of the patients ranged from 38–75 years,
with a mean age of 53.64±13.84 years. The duration of illness
varied from 0.5–3 years, with a mean of 1.99±0.84 years. Among the
cases, there were 43 instances of cervical small cell carcinoma, 38
cases of cervical adenocarcinoma and 29 cases of cervical squamous
cell carcinoma. The main clinical symptoms of cervical cancer
included increased vaginal discharge (15 cases), cervical erosion
(4 cases), bleeding on contact (27 cases) and irregular vaginal
bleeding (64 cases).
Intervention methods.
Preoperative MRI examination
Prior to scanning, patients were asked to remove all
metallic items, lie in a supine position with legs comfortably
extended and maintain a steady breathing pattern. Patients were
instructed to hold their breath at the end of exhalation and drink
a suitable amount of water to ensure bladder fullness. The
pre-examination intravenous injection of gadoterate meglumine
contrast agent was administered to all patients. The examinations
were conducted using a United Imaging GE Discovery MR750 3.0T MRI
scanner (GE Healthcare). During the examination, with hands
positioned above their heads, patients underwent sequential scans
of pelvic axial T2-weighted imaging (WI), T1WI, diffusion-weighted
imaging (DWI) sequences, a sagittal T2WI sequence and a coronal
T2WI sequence using a body coil. Scan parameters comprised a slice
thickness of 5 mm and an interslice gap of 1 mm. The preoperative
staging for cervical cancer was assessed by at least two MRI
specialists, each with >3 years of experience, relying on the
MRI images of the patients and signs of abnormalities. If opinions
were inconsistent, a comprehensive diagnosis was made in
consultation with another senior physician.
Postoperative pathological
examination
All patients received a diagnosis of cervical cancer
based on postoperative pathological examination results. Tissue
samples were removed and preserved in a 10% formaldehyde solution
at room temperature for 12–24 h. After re-washing in tap water,
samples were rinsed in graded alcohol solutions and later cleared
in xylene. Following paraffinization, tissue samples were embedded
in paraffin, then 4-µm serial histological sections were obtained
from a microtome. After deparaffinization and rinsing, sections
were stained with hematoxylin for 10 min, rinsed in tap water for 5
min, differentiated in 0.5–1% acid alcohol for a few seconds,
rinsed again in tap water for 5 min, stained in a weakly alkaline
solution for 1 min and counterstained with eosin. Slides were
dehydrated using absolute ethanol, cleared in xylene and mounted
using neutral balsam. Slides examined pathologically under a light
microscope (Olympus Corporation). The FIGO staging (11) was established by evaluating the
cellular structure of the lesion, the extent of invasion and
whether LNM was present. Specifically, staging was as follows:
Stage IA indicated microscopic invasive carcinoma with a maximum
invasion depth of ≤5 mm; stage IB denoted invasive carcinoma that
exceeded stage IA but remained within the cervix, with an invasion
depth >5 mm; stage IIA involved tumor invasion limited to the
upper two-thirds of the vagina without parametrial involvement;
stage IIB included parametrial invasion without reaching the pelvic
wall; stage IIIA involved the lower one-third of the vagina without
pelvic wall extension; stage IIIB extended to the pelvic wall,
potentially causing hydronephrosis or kidney dysfunction; stage
IIIC involved invasion into the pelvic cavity, including
para-aortic lymph nodes; stage IVA included invasion into the
rectal or bladder mucosa; and stage IVB referred to the spread of
the tumor to distant organs.
Observation indicators
Using the pathological examination results as the
gold standard, the confirmed diagnoses were compared with the
staging results of MRI to evaluate the diagnostic accuracy of MRI
in clinical staging of patients.
The diagnostic performance of MRI (comprising
sensitivity, specificity and accuracy) in detecting pelvic LNM,
parametrial invasion and vaginal involvement was assessed.
Sensitivity was calculated as the proportion of true-positive cases
relative to the sum of true-positive and false-negative cases,
multiplied by 100. Specificity was determined as the proportion of
true-negative cases relative to the sum of true-negative and
false-positive cases, multiplied by 100. Accuracy was defined as
the proportion of true-positive and true-negative cases relative to
the total number of cases, multiplied by 100.
Statistical analysis
Statistical analysis was performed using SPSS 24.0
software (IBM Corp.). Continuous variables, such as age, are
expressed as mean ± standard deviation, while categorical variables
are presented as frequencies (n) and percentages (%), with Fisher's
exact test applied for analysis. P<0.05 was considered to
indicate a statistically significant difference.
Results
Clinical staging
When compared with postoperative pathological
staging, the overall diagnostic accuracy of preoperative MRI for
the clinical staging of cervical cancer was 97.27%, with no
statistically significant difference from the pathological
diagnosis accuracy of 100% (P>0.05; Table I).
 | Table I.Diagnostic accuracy of clinical
staging in cervical cancer. |
Table I.
Diagnostic accuracy of clinical
staging in cervical cancer.
| Stage | Magnetic resonance
imaging (n=110) | Pathological
diagnosis (n=110) | P-value |
|---|
| Stage IA | 7 (6.36) | 8 (7.27) |
|
| Stage IB | 28 (25.45) | 30 (27.27) |
|
| Stage IIA | 12 (10.91) | 12 (10.91) |
|
| Stage IIB | 23 (20.91) | 23 (20.91) |
|
| Stage IIIA | 19 (17.27) | 19 (17.27) |
|
| Stage IIIB | 9 (8.18) | 9 (8.18) |
|
| Stage IIIC | 5 (4.55) | 5 (4.55) |
|
| Stage IVA | 3 (2.73) | 3 (2.73) |
|
| Stage IVB | 1 (0.91) | 1 (0.91) |
|
| Overall accuracy | 107 (97.27) | 110 (100.00) | 0.247 |
Diagnostic results for pelvic LNM,
parametrial invasion and vaginal involvement in cervical
cancer
The detection rates of MRI for pelvic LNM,
parametrial invasion and vaginal involvement in cervical cancer
were not significantly different from those of pathological
diagnosis (all P>0.05) (Table
II).
 | Table II.Diagnostic accuracy rates for pelvic
lymph node metastasis, parametrial invasion and vaginal involvement
in cervical cancer. |
Table II.
Diagnostic accuracy rates for pelvic
lymph node metastasis, parametrial invasion and vaginal involvement
in cervical cancer.
| Cervical cancer
lesion type | Magnetic resonance
imaging (n=110) | Pathological
diagnosis (n=110) | P-value |
|---|
| Pelvic lymph node
metastasis |
|
| 0.247 |
|
Detected | 107 (97.27) | 110 (100.00) |
|
| Not
detected | 3 (2.73) | 0 (0.00) |
|
| Parametrial
invasion |
|
| 0.498 |
|
Detected | 108 (98.18) | 110 (100.00) |
|
| Not
detected | 2 (1.82) | 0 (0.00) |
|
| Vaginal
involvement |
|
| 0.247 |
|
Detected | 107 (97.27) | 110 (100.00) |
|
| Not
detected | 3 (2.73) | 0 (0.00) |
|
Diagnostic value of MRI for pelvic
LNM, parametrial invasion and vaginal involvement
MRI exhibited high sensitivity, specificity and
accuracy in diagnosing pelvic LNM, parametrial invasion and vaginal
involvement. The sensitivity of MRI in detecting vaginal
involvement was higher than that for pelvic LNM and parametrial
invasion (P<0.05). The specificity of MRI in diagnosing pelvic
LNM showed no difference compared with its specificity in
diagnosing parametrial invasion and vaginal involvement
(P>0.05). The accuracy of MRI in diagnosing parametrial invasion
showed no difference compared with its accuracy in diagnosing
pelvic LNM and vaginal involvement (P>0.05; Tables III and IV).
 | Table III.Preoperative magnetic resonance
imaging findings with postoperative pathological diagnoses
regarding pelvic lymph node metastasis, parametrial invasion and
vaginal involvement. |
Table III.
Preoperative magnetic resonance
imaging findings with postoperative pathological diagnoses
regarding pelvic lymph node metastasis, parametrial invasion and
vaginal involvement.
|
| Postoperative
pathology |
|
|---|
|
|
|
|
|---|
| Preoperative magnetic
resonance imaging | Positive | Negative | Total |
|---|
| Lymph node
metastasis |
|
|
|
|
Positive | 18 (16.36) | 2 (1.82) | 20 (18.18) |
|
Negative | 1 (0.91) | 89 (80.91) | 90 (81.82) |
|
Total | 19 (17.27) | 91 (82.73) | 110 (100.00) |
| Parametrial
invasion |
|
|
|
|
Positive | 76 (69.09) | 1 (0.91) | 77 (70.00) |
|
Negative | 1 (0.91) | 32 (29.09) | 33 (30.00) |
|
Total | 77 (70.00) | 33 (30.00) | 110 (100.00) |
| Vaginal
involvement |
|
|
|
|
Positive | 39 (35.45) | 3 (2.73) | 42 (38.18) |
|
Negative | 0 (0.00) | 68 (61.82) | 68 (61.82) |
|
Total | 39 (35.45) | 71 (64.55) | 110 (100.00) |
 | Table IV.Diagnostic efficacy of preoperative
magnetic resonance imaging in detecting pelvic lymph node
metastasis, parametrial invasion and vaginal involvement in
cervical cancer. |
Table IV.
Diagnostic efficacy of preoperative
magnetic resonance imaging in detecting pelvic lymph node
metastasis, parametrial invasion and vaginal involvement in
cervical cancer.
| Diagnostic
factor | Lymph node
metastasis | Parametrial
invasion | Vaginal
involvement | P-value |
|---|
| Sensitivity | 94.74 (18/19) | 98.70 (76/77) | 100.00 (39/39) | 0.086 |
| Specificity | 97.80 (89/91) | 96.97 (32/33) | 95.77 (68/71) | 0.859 |
| Accuracy | 97.27
(107/110) | 98.18
(108/110) | 97.27
(107/110) | >0.999 |
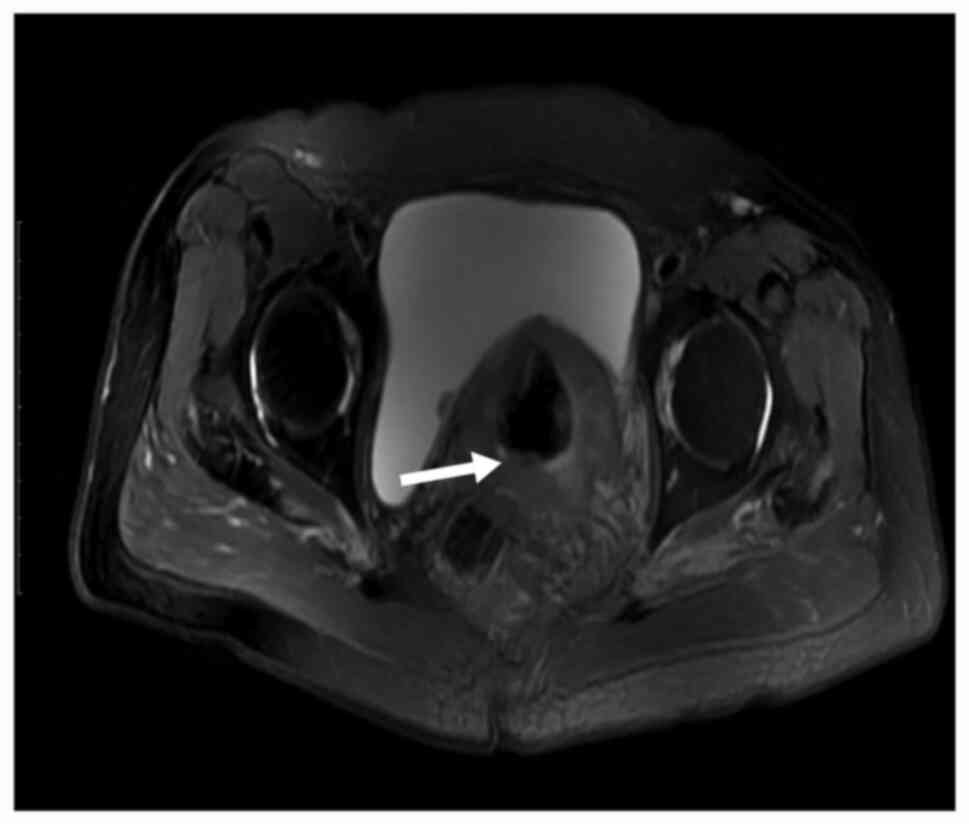
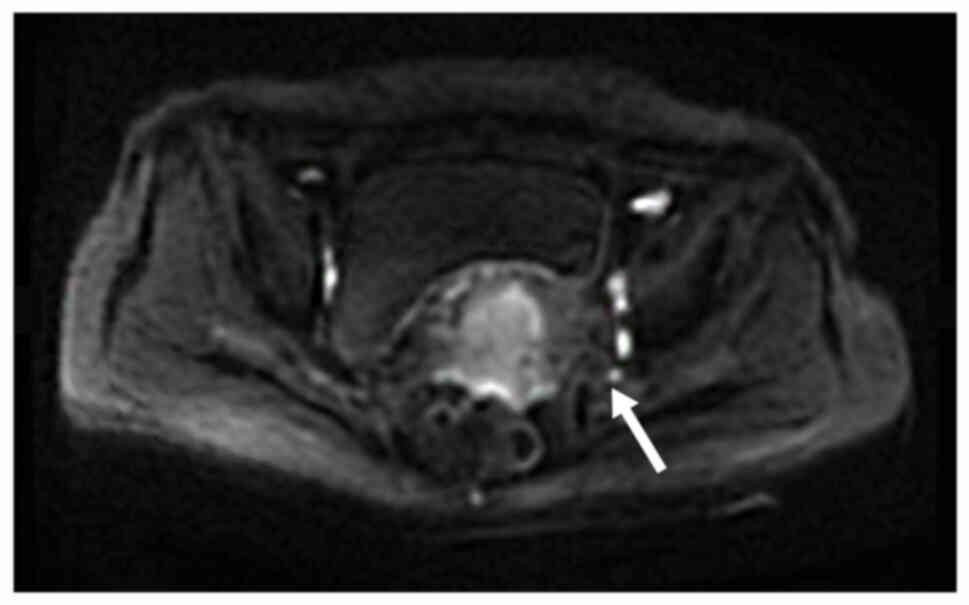
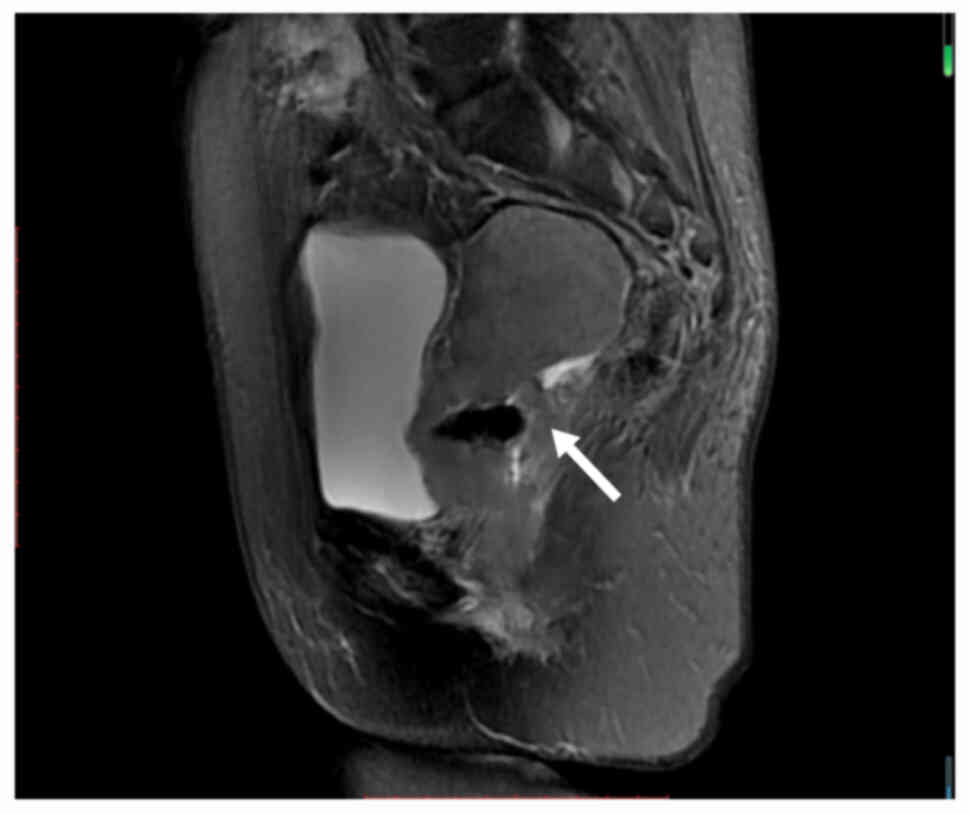
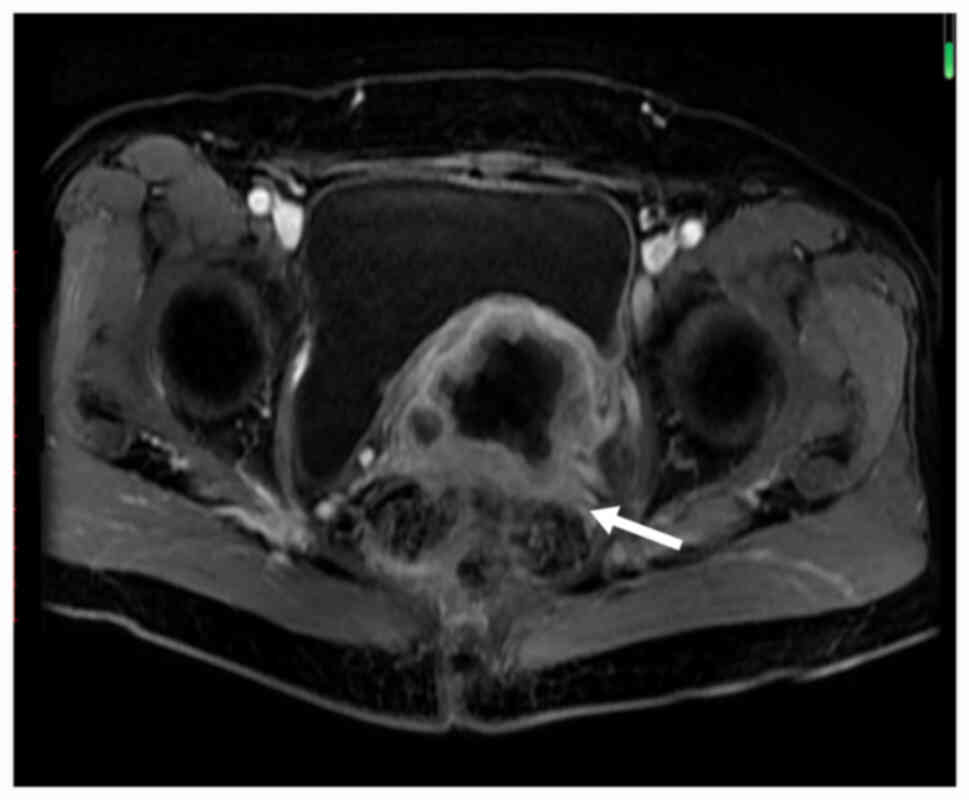
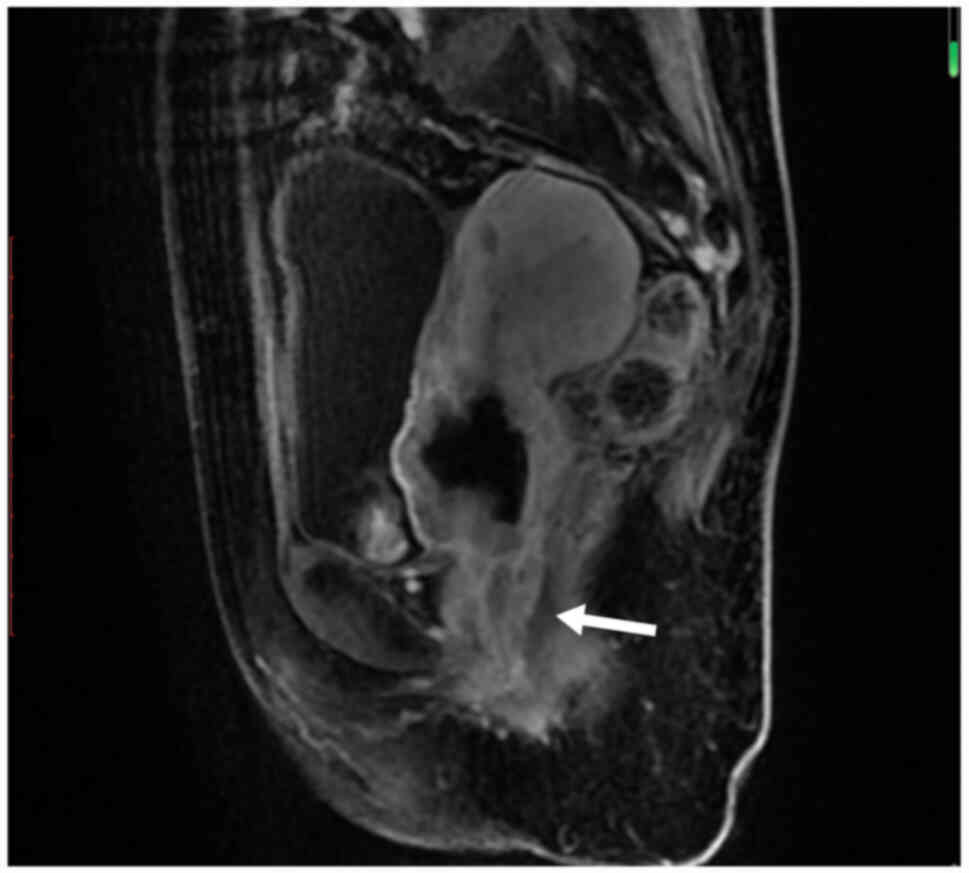
MRI diagnostic image examples
Examples of MRI diagnostic images from multiple
patients are shown in Fig. 1,
Fig. 2, Fig. 3, Fig.
4, Fig. 5. Fig. 1 shows an irregular soft-tissue mass
in the cervical region, clearly visible on the axial sequence of
T2-weighted fat-saturated imaging. The mass may suggest cervical
lesions or tumors. Fig. 2 displays
multiple lymph node metastases in the pelvic region on the axial
sequence of DWI. The high-signal areas indicate that the lymph
nodes might be affected by tumor metastasis. Fig. 3 reveals an irregular soft-tissue
mass in the cervical region on the sagittal sequence of T2-weighted
fat-saturated imaging. The mass is shown to have extended into the
vaginal area, with the sagittal view aiding in the assessment of
the lesion's longitudinal extent. Fig.
4 displays an irregular soft-tissue mass in the cervical region
on T1-weighted enhanced imaging. The mass shows significant
heterogeneous enhancement, suggesting that the lesion may be
malignant. Fig. 5 illustrates a
lesion in the cervical and vaginal regions on the sagittal sequence
of T1-weighted enhanced imaging. The lesion area demonstrates
heterogeneous enhancement, further indicating the possibility of a
malignant tumor.
Discussion
Cervical cancer ranks as the fourth most common
cancer among women globally (12).
MRI has emerged as an important imaging modality in clinical
practice, particularly with the advancement of various novel
imaging techniques, including multi-contrast sequences such as
diffusion-weighted imaging, T1- and T2-weighted imaging, 4D-MRI and
virtual contrast-enhanced MRI (9).
Determining the pathological features of lesions is required for
deciding appropriate management approaches and treatment strategies
(7). Accurate preoperative
assessment is important for identifying potential risks and
improving patient outcomes (5). The
present study demonstrated that MRI exhibits high diagnostic
accuracy in the preoperative evaluation of cervical cancer staging
and pathological features, including pelvic LNM, parametrial
invasion and vaginal involvement, with no significant differences
compared with pathological diagnosis. High diagnostic accuracy
supports the use of MRI as a reliable tool for preoperative
assessment, enabling physicians to design more appropriate
treatment strategies and thereby improve patient outcomes.
Previous studies have consistently emphasized the
notable importance of accurate staging and comprehensive diagnosis
in the management of cervical cancer, as these factors
significantly influence treatment planning and patient outcomes
(13–15). The present research findings are
consistent with previous evidence underscoring the diagnostic
accuracy of MRI in cervical cancer evaluation, while recognizing
that certain lesion subtypes may still pose diagnostic challenges
(16). The multi-parametric
capabilities of MRI, including T2WI, DWI and dynamic
contrast-enhanced sequences, provide exemplary soft-tissue contrast
that is particularly valuable in gynecological malignancies. One of
the most significant advancements in cervical cancer imaging has
been the demonstration of the effectiveness of MRI in detecting
LNM, an important factor in determining disease staging and
treatment strategy (17). While the
present study confirmed the overall diagnostic capabilities of MRI,
a particularly strong performance in detecting pelvic LNM was
demonstrated. This observation indicated that although MRI remains
the cornerstone of cervical cancer imaging, PET/CT may provide
complementary value in selected clinical scenarios, especially for
detecting distant metastases and assessing treatment response. The
close concordance between MRI and histopathological findings across
multiple pathological features further underscores its diagnostic
accuracy, and the consistency of the present results with previous
research reinforces the role of MRI as a reliable preoperative
evaluation tool (18).
Specifically, the ability of MRI to accurately
determine the extent of disease spread, including the depth of
stromal invasion and its relationship to adjacent structures, makes
it highly valuable for surgical planning. Its demonstrated
diagnostic strength underscores the role of MRI as a key component
in the diagnostic workup of cervical cancer. This capability
enables the development of tailored treatment strategies, ranging
from fertility-sparing surgeries in early-stage disease to more
extensive procedures or chemoradiation in advanced cases.
Furthermore, integrating advanced MRI techniques with other imaging
modalities, particularly in complex situations, offers a promising
approach to further enhance diagnostic accuracy and improve patient
outcomes in cervical cancer management.
In conclusion, the importance of accurate MRI
diagnosis in cervical cancer cannot be overstated, as it directly
impacts treatment planning and patient outcomes. Looking ahead,
there are several promising directions for advancing MRI-based
cervical cancer diagnosis. Integration of artificial intelligence
and machine learning algorithms could potentially enhance the
diagnostic accuracy of MRI interpretations. Future research should
focus on developing standardized protocols for MRI assessment and
exploring the combination of different imaging modalities to
improve diagnostic precision. Additionally, investigating the role
of advanced MRI techniques, such as DWI and dynamic
contrast-enhanced sequences, could provide more detailed
information about tumor characteristics and treatment response. The
development of quantitative imaging biomarkers through MRI could
also help in predicting treatment outcomes and personalizing
therapeutic approaches.
Acknowledgements
Not applicable.
Funding
The present work was funded by the Tianshan Elite High-level
Medical and Health Talent Training Program (grant no.
TSYC202301B083).
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
XC and XL made substantial contributions to the
conception and design of the study, participated in data analysis
and interpretation, and were involved in drafting and revising the
manuscript. JY and XW contributed to data acquisition and
interpretation, participated in drafting parts of the manuscript
and approved the final version. WY was involved in data validation,
manuscript drafting and critical revision for important
intellectual content and approved the final version. YB contributed
to the conception and design of the study, participated in data
interpretation, critically revised the manuscript for important
intellectual content, approved the final version to be published,
and agreed to be accountable for all aspects of the work. XC and XL
confirm the authenticity of all the raw data. All authors read and
approved the final version of the manuscript.
Ethics approval and consent to
participate
All experimental procedures were approved by the
Medical Ethics Committee of The Fifth Affiliated Hospital of
Xinjiang Medical University (approval no. 2020065). Written
informed consent was obtained from all individual participants
included in the study.
Patient consent for publication
The MRI figures presented in the manuscript were
derived from multiple patients, each of whom provided written
informed consent for the use of their images and for the submission
of the manuscript.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Rajaram S and Gupta B: Screening for
cervical cancer: Choices & dilemmas. Indian J Med Res.
154:210–220. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Mayadev JS, Ke G, Mahantshetty U, Pereira
MD, Tarnawski R and Toita T: Global challenges of radiotherapy for
the treatment of locally advanced cervical cancer. Int J Gynecol
Cancer. 32:436–445. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Gutierrez-Hoya A and Soto-Cruz I: NK cell
regulation in cervical cancer and strategies for immunotherapy.
Cells. 10:31042021. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Zoller DP: The physiology of aging. Am Fam
Physician. 36:112–116. 1987.PubMed/NCBI
|
|
5
|
Komurcu O, Genc C, Kurt BC, Demir O, Akbas
A, Akyurt D, Kuşderci HS, Tulgar S and Süren M: Preoperative
evaluation: Impact on early perioperative hemodynamic and
respiratory complications. BMC Anesthesiol. 24:4352024. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Moleti CA: Caring for socially high-risk
pregnant women. MCN Am J Matern Child Nurs. 13:24–27. 1988.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zhang Z, Zheng X, Zhang M, Li J, Zhao J,
Zheng J and Wang S: Pathological features of persistent adnexal
masses in pregnancy. Ann Transl Med. 9:9732021. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Zhang L, Wan R, Chen J, Xin F and Han H:
Analysis of the correlation between clinical and imaging features
of malignant lung nodules and pathological types. Front Surg.
10:13211182023. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Li T, Wang J, Yang Y, Glide-Hurst CK, Wen
N and Cai J: Multi-parametric MRI for radiotherapy simulation. Med
Phys. 50:5273–5293. 2023. View
Article : Google Scholar : PubMed/NCBI
|
|
10
|
Roth BJ: Can MRI be used as a sensor to
record neural activity? Sensors (Basel). 23:13372023. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Mohamud A, Hogdall C and Schnack T:
Prognostic value of the 2018 FIGO staging system for cervical
cancer. Gynecol Oncol. 165:506–513. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Gopu P, Antony F, Cyriac S, Karakasis K
and Oza AM: Updates on systemic therapy for cervical cancer. Indian
J Med Res. 154:293–302. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Zhang W, Chen C, Liu P, Li W, Hao M, Zhao
W, Lu A and Ni Y: Impact of pelvic MRI in routine clinical practice
on staging of IB1-IIA2 cervical cancer. Cancer Manag Res.
11:3603–3609. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Salib MY, Russell JHB, Stewart VR,
Sudderuddin SA, Barwick TD, Rockall AG and Bharwani N: 2018 FIGO
staging classification for cervical cancer: Added benefits of
imaging. Radiographics. 40:1807–1822. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Narayan K and Lin MY: Staging for cervix
cancer: Role of radiology, surgery and clinical assessment. Best
Pract Res Clin Obstet Gynaecol. 29:833–844. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ohya A, Miyamoto T, Ichinohe F, Kobara H,
Fujinaga Y and Shiozawa T: Problems of magnetic resonance diagnosis
for gastric-type mucin-positive cervical lesions of the uterus and
its solutions using artificial intelligence. PLoS One.
19:e03158622024. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Musunuru HB, Pifer PM, Mohindra P,
Albuquerque K and Beriwal S: Advances in management of locally
advanced cervical cancer. Indian J Med Res. 154:248–261. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Demir G, Arici M and Alkin Z: Preoperative
evaluation of tractional retinal detachment with B-mode
ultrasonography in diabetic vitreous hemorrhage. Beyoglu Eye J.
6:49–53. 2021.PubMed/NCBI
|