Introduction
Gastric cancer has a relatively high prevalence,
especially in East Asia, and it is one of the most common causes of
cancer-related death worldwide. Despite many improvements in its
diagnosis and treatment, the prognosis of gastric cancer remains
poor, especially in its advanced stages. It exhibits several
distinct metastatic patterns depending on the histological subtype,
tumor location, and disease progression. The metastatic spread of
the primary gastric cancer can occur through four pathways:
peritoneal dissemination, hematogenous dissemination, lymphatic
spread, and direct tumor invasion. Based on previous registration
studies evaluating the hematogenous metastasis of gastric cancer,
17, 6, 5, and 1% of patients present with liver, lung, bone, and
brain metastasis at the time of diagnosis, respectively (1). This report describes a very rare case
of gastric cancer with metastasis to the pulmonary veins, which has
not been reported previously. Tumor embolization of the pulmonary
vein is a precarious condition because it can cause serious
embolism if it migrates to the arteries.
Case report
A 71-year-old male with a 20-year smoking history
underwent laparoscopic distal gastrectomy, D1 lymph node
dissection, and Billroth-I reconstruction for gastric cancer at a
previous hospital in March 2021. The histological examinations
revealed moderately differentiated tubular adenocarcinoma with No4d
lymph node metastasis; pT1b(SM)N1M0 pStage1B (UICC TNM 8th
edition). Seven months after the first surgery, partial hepatic
resection was performed for a solitary S7 hepatic recurrence,
followed by a 12-month course of postoperative chemotherapy with
S-1 and docetaxel.
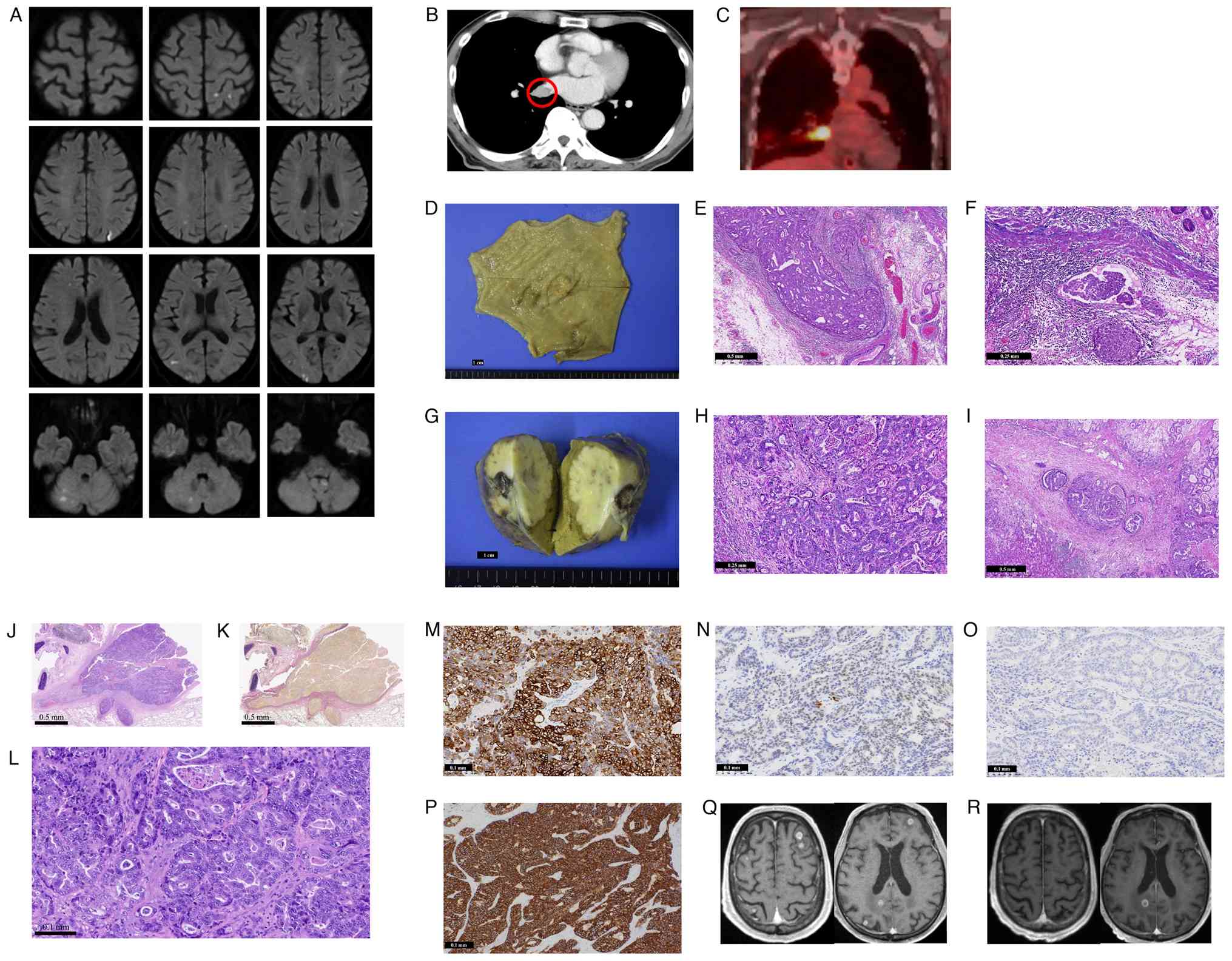
In December 2023, the patient presented with
weakness and numbness of the right lower extremity and was admitted
to our hospital. Non-contrast magnetic resonance imaging (MRI) of
the brain demonstrated multiple small acute infarcts, characterized
by diffusion restriction and low ADC values, located in the left
cerebellar tonsil, right cerebellar hemisphere, and bilateral
frontal watershed regions (Fig.
1A). Contrast-enhanced computed tomography (CT) of the chest
revealed right-sided pleural effusion with no apparent lung
metastatic nodules, but with a filling defect in the right inferior
pulmonary vein (Fig. 1B). The vital
signs upon admission were as follows: oxygen saturation, 99% on
room air; blood pressure, 138/88 mmHg; heart rate, 61/min; and body
temperature, 37.0°C. Physical examination revealed no murmurs or
abnormal sounds during respiration, and echocardiography showed no
evidence of valvular disease or intracardiac thrombus. Positron
emission tomography/CT demonstrated FDG accumulation [maximum
standardized uptake value (SUVmax) 13.0] at the right inferior
pulmonary vein (Fig. 1C). Based on
these findings, the patient was suspected to have multiple cerebral
tumor emboli, likely induced by pulmonary vein metastasis. The
acute cerebral infarctions were managed with rehabilitation and
aspirin therapy, and the patient's right lower extremity weakness
and numbness had improved by two weeks after treatment initiation.
A follow-up contrast-enhanced brain MRI revealed multiple enhancing
lesions in the bilateral cerebellum and cerebrum, which were
consistent with brain metastases. Stereotactic radiotherapy (35
Gy/5 fractions) was delivered to the 9 brain lesions. Subsequently,
video-assisted thoracoscopic right lower lobectomy, pulmonary vein
tumor resection, and left atrial repair were performed in February
2024. Pulmonary vein resection was done for diagnostic purposes, as
well as to prevent any further cerebral infarctions caused by tumor
emboli.
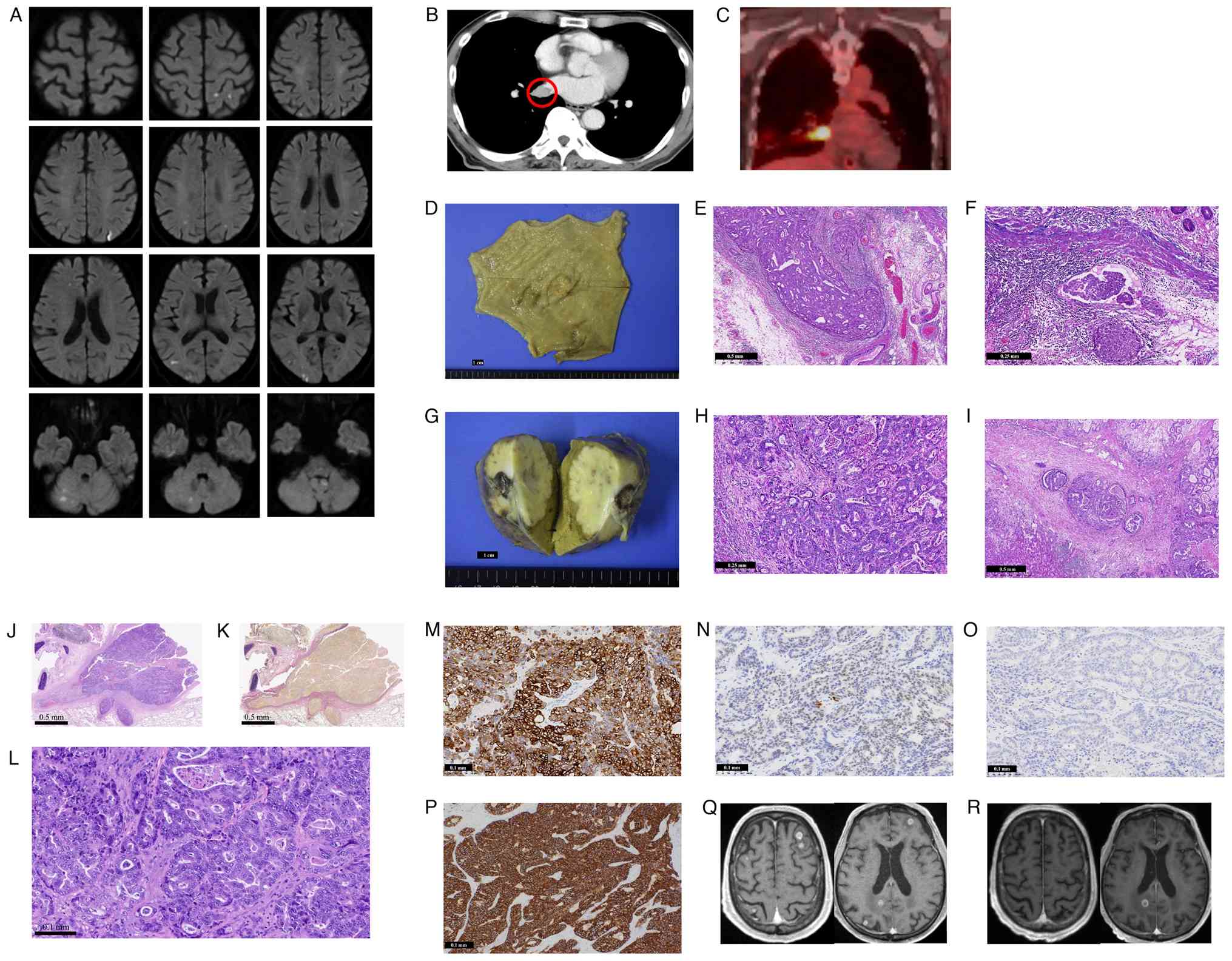 | Figure 1.(A) Diffusion-weighted imaging of
non-contrast brain MRI demonstrating multiple small acute infarcts
characterized by diffusion restriction. Lesions were observed in
the left cerebellar tonsil, right cerebellar hemisphere and
bilateral frontal watershed regions. (B) Contrast-enhanced CT
revealed a filling defect in the right inferior pulmonary vein (red
circle) (C) Positron emission tomography/CT revealed abnormal
uptake in the right inferior pulmonary vein with a maximum
standardized uptake value of 13.0, as well as right-sided pleural
effusion. (D) Gross image of the primary gastric carcinoma specimen
after formalin fixation. Scale bar, 1 cm. (E) H&E-stained
section of the primary gastric carcinoma demonstrating vascular
invasion by adenocarcinoma. Scale bar, 0.5 mm. (F) H&E-stained
section of the primary gastric carcinoma demonstrating lymphatic
invasion by adenocarcinoma. Scale bar, 0.25 mm. (G) Gross image of
the liver metastatic tumor after formalin fixation. Scale bar, 1
cm. (H) H&E-stained section of the liver metastatic tumor
demonstrating adenocarcinoma with morphological features similar to
those of the primary gastric carcinoma. Scale bar, 0.25 mm. (I)
H&E-stained section of the liver metastatic tumor demonstrating
vascular invasion by adenocarcinoma. Scale bar, 0.5 mm. (J)
H&E-stained section of the tumor metastasized to the pulmonary
vein. Scale bar, 0.5 mm. (K) Elastica van Gieson-stained section of
the tumor metastasized to the pulmonary vein, demonstrating tumor
invasion into the pulmonary vein. Scale bar, 0.5 mm. (L)
H&E-stained section of the tumor metastasized to the pulmonary
vein at a magnification of ×100 (objective lens, ×10; ocular lens,
×10). The adenocarcinoma exhibited complex tubulopapillary
structures with a stromal reaction. The tumor morphology was
similar to that of the previously identified primary gastric
carcinoma and liver metastasis. Scale bar, 0.1 mm. (M)
Immunohistochemical staining of the pulmonary vein metastatic tumor
showing positivity for cytokeratin 7. Scale bar, 0.1 mm. (N)
Immunohistochemical staining of the pulmonary vein metastatic tumor
showing partial positivity for caudal type homeobox 2. Scale bar,
0.1 mm. (O) Immunohistochemical staining of the pulmonary vein
metastatic tumor showing negativity for cytokeratin 20. Scale bar,
0.1 mm. (P) Immunohistochemical staining of the pulmonary vein
metastatic tumor showing strong positivity for HER2. Scale bar, 0.1
mm. Contrast-enhanced brain MRI performed in (Q) October 2024 and
(R) March 2025. After initiating trastuzumab deruxtecan, a partial
radiological response was observed, with some metastatic brain
lesions disappearing on the follow-up MRI. CT, computed tomography;
H&E, hematoxylin and eosin; MRI, magnetic resonance
imaging. |
The resected specimen measured 16×12×7 cm. The
pulmonary vein was dilated to 2.0 cm and filled with a
grayish-white mass, which had similar histologic features as the
previously resected gastric and hepatic tumors (Fig. 1D-L). Immunohistochemical staining
was positive for CK7, partially positive for CDX2, and negative for
CK20, confirming the diagnosis of pulmonary vein metastasis from
gastric adenocarcinoma. Additionally, HER2 immunohistochemistry was
strongly positive (IHC 3+) (Fig.
1M-P). Because the surgical margins of the pulmonary vein were
positive, chemotherapy with S-1, oxaliplatin, and trastuzumab was
subsequently initiated in March 2024. In August 2024, the patient
developed new brain metastases, which were treated with additional
stereotactic radiotherapy (SRT/SRS). In October 2024, the brain
metastases further progressed, prompting a switch in the
chemotherapy regimen to trastuzumab deruxtecan for its potential
efficacy against brain metastases, resulting in partial regression
of the brain lesions (Fig. 1Q and
R). In June 2025, however, chemotherapy was discontinued due to
a decline in the patient's performance status. As of July 2025, the
patient remains alive under best supportive care.
Discussion
The most common metastatic sites of gastric cancer
are the liver, peritoneum, lungs, and bones (1). Although several reports have described
metastases to the pericardium and heart (2–4),
pulmonary vein metastasis is extremely rare. The current literature
describes pulmonary vein metastases from other malignancies such as
hepatocellular carcinoma, chordoma, breast cancer, and melanoma
(5–8), but no reports have described pulmonary
vein metastasis from a gastric adenocarcinoma primary. Thus, this
appears to be the first documented case of its kind.
In this case, the patient presented with acute right
lower extremity weakness and numbness, and brain MRI revealed
multiple infarcts involving the left cerebellar tonsil, right
cerebellar hemisphere, and bilateral frontal watershed regions.
Because the lesions were multiple and small, it was not possible to
identify a definitive responsible focus that could clearly account
for the patient's right lower extremity weakness and numbness. No
notable cerebellar symptoms, such as ataxia or balance disturbance,
were observed.
The distribution of infarcts across both
supratentorial and infratentorial regions suggests that embolic
material reached the brain via more than one arterial route. The
coexistence of watershed infarcts in the frontal lobes and infarcts
in the cerebellum indicates potential involvement of both the
internal carotid and vertebrobasilar arterial systems. In this
patient, it was not possible to definitively determine whether
these multiple cerebral infarctions were caused by tumor emboli
originating from the pulmonary vein, as thrombus retrieval was not
performed. However, previous reports in other malignancies have
described pulmonary vein tumor emboli as a cause of cerebral
infarction (8). Therefore, in
clinical situations where pulmonary vein metastasis is suspected,
careful monitoring for cerebral embolic events is warranted.
For gastrointestinal cancers to metastasize to the
pulmonary vein, the tumor cells must traverse the portal vein, pass
through the right heart, and enter the pulmonary artery before
finally reaching the pulmonary vein. Since gastric cancer cells are
approximately 10 µm in diameter, it is unlikely that they can pass
directly through the pulmonary capillaries, which typically have a
smaller diameter. Additionally, there was no apparent pulmonary
metastasis that could have trapped the tumor in the lungs in this
patient, nor was there definitive evidence of the tumor invading
the myocardium and pericardium. One hypothesis is that microscopic
pulmonary artery-vein shunts could promote the migration of tumor
cells into the pulmonary veins. However, Elastica van Gieson
staining revealed tumor proliferation in the pulmonary veins and
the stroma around the ruptured pulmonary veins, but there was no
obvious pulmonary artery infiltration. Furthermore, a bubble test
echocardiogram performed postoperatively revealed no macroscopic
arteriovenous shunt.
Pulmonary vein metastasis can predispose patients to
hematogenous brain metastases. In this case, nine metastatic
lesions were identified bilaterally in the cerebrum and cerebellum.
After multidisciplinary discussion, the patient underwent
stereotactic radiotherapy and pulmonary vein tumor resection with
left atrial repair, considering the possibility of further brain
metastasis from the pulmonary vein, which could cause a decline in
performance. By preventing appearance of new brain metastases in a
short period of time, HER2-based chemotherapy could have been
introduced, which could improve the chances of long-term survival
(9,10).
This case highlights the importance of recognizing
pulmonary vein metastasis as a potential source of tumor embolism
and brain metastasis in gastric adenocarcinoma. Multimodal
treatment with a combination of surgery, radiotherapy, and systemic
therapy can help achieve long-term disease control even in such
rare and challenging clinical situations.
This case was previously reported in part by the
Department of Thoracic and Cardiovascular Surgery, focusing on the
surgical technique (JTCVS Tech. 2025;29:103-105) (11). The present report offers a distinct
perspective on the oncological and neurological aspects of the same
case, including the clinical course, cerebral complications and
systemic therapy, and does not overlap with the previous
publication.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
NH and MT confirm the authenticity of all the raw
data. NH conceived and designed the study. Acquisition and
interpretation of data was performed by NH, YY, YK, RS, MO, SO, HN,
JT, RM, MHa, MHo, FO, AY and MT. Writing of the original draft was
undertaken by NH, and writing, review and editing of the manuscript
were carried out by NH and MT. All authors agree to be accountable
for all aspects of the research in ensuring that the accuracy or
integrity of any part of the work are appropriately investigated
and resolved. All authors have read and approved the final version
of the manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent was obtained from the
patient for publication of this case report and the accompanying
images. The patient was informed that all identifying information
would be removed to ensure anonymity.
Competing interests
MT received honoraria from Chugai Pharmaceutical,
AstraZeneca K.K., Bristol-Myers Squibb Company, Novartis Pharma
K.K., and Ono Pharmaceutical. The other authors declare that they
have no competing interests.
References
|
1
|
Qiu M, Shi S, Chen ZH, Yu HE, Sheng H, Jin
Y, Wang DS, Wang FH, Li YH, Xie D, et al: Frequency and
clinicopathological features of metastasis to liver, lung, bone,
and brain from gastric cancer: A SEER-based study. Cancer Med.
7:3662–3672. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Moriyama A, Murata I, Kuroda T, Yoshikawa
I, Tabaru A, Ogami Y and Otsuki M: Pericardiac metastasis from
advanced gastric cancer. J Gastroenterol. 30:512–516. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Bernhardt P, Jones A, Kaufmann J, Hombach
V and Spiess J: Cardiac metastasis of a gastric adenocarcinoma. Eur
Heart J. 30:16552009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Oza T, Shafique K, Gilani A, Lanjewar S
and Shao C: Cardiac metastases of primary gastric adenocarcinoma
presenting as cardiac failure. Am J Clin Pathol. 144 (Suppl
2):A0102015. View Article : Google Scholar
|
|
5
|
Diallo O, Yaméogo VN, Dao SBA, Ouattara B
and Cissé R: Right upper pulmonary vein metastasis from
hepatocarcinoma. Radiol Case Rep. 13:11–13. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Prompona M, Linn J, Burdorf L, Assmann G,
Reichart B, Reiser M and Nikolaou K: Pulmonary vein metastasis of a
sacral chordoma extending into the left atrial cavity. J Cardiovasc
Med (Hagerstown). 10:557–559. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Makhija Z, Luckraz H and Butchart EG:
Pseudo-myxoma: Massive pulmonary vein metastasis from a primary
breast carcinoma. Eur J Cardiothorac Surg. 33:3142008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Nukata R, Ikeda H, Akaike N, Fujiwara T,
Yamashita H, Uezato M, Kinosada M, Kurosaki Y, Shindo K and Chin M:
White embolus-induced basilar artery occlusion due to pulmonary
vein invasion of a metastasis of a malignant melanoma. Intern Med.
62:2889–2893. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Bang YJ, Van Cutsem E, Feyereislova A,
Chung HC, Shen L, Sawaki A, Lordick F, Ohtsu A, Omuro Y, Satoh T,
et al: Trastuzumab in combination with chemotherapy versus
chemotherapy alone for treatment of HER2-positive advanced gastric
or gastro-oesophageal junction cancer (ToGA): A phase 3,
open-label, randomised controlled trial. Lancet. 376:687–697. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Harbeck N, Ciruelos E, Jerusalem G, Müller
V, Niikura N, Viale G, Bartsch R, Kurzeder C, Higgins MJ, Connolly
RM, et al: Trastuzumab deruxtecan in HER2-positive advanced breast
cancer with or without brain metastases: A phase 3b/4 trial. Nat
Med. 30:3717–3727. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Takemura J, Miyata R, Miura S, Hamaji M
and Hosono M: Salvage lobectomy for an intravascular mass occluding
the right lower lobe vein. JTCVS Tech. 29:103–105. 2024. View Article : Google Scholar : PubMed/NCBI
|