Introduction
Paclitaxel is a frequently used anticancer drug with
a broad spectrum of activity against malignant solid tumors,
including breast, ovarian and lung cancer (1). However, the considerable variability
in drug efficiency and toxicity of paclitaxel treatment results in
unpredictable patient responses. Neurotoxicity is one common
adverse effect following treatment with paclitaxel (2). This effect is apparently dose-related,
since several studies have shown a trend towards increased
neurotoxicity with increased paclitaxel AUC (area under the
concentration curve) (3–5). The reasons for this inter-individual
variability have not been determined. Many studies are therefore
focusing on genetic variation in genes encoding metabolising and
drug-transporting proteins. Paclitaxel is mainly metabolised by the
CYP2C8 enzyme to its primary metabolite, 6α-hydroxypaclitaxel
(6) and to a lesser extent by the
CYP3A4 enzyme (7). Furthermore,
paclitaxel is a substrate for ABCB1 (MDR1; P-glycoprotein), an
important membrane efflux protein (3,8). ABCB1
is expressed in the blood-brain barrier and is thought to protect
peripheral nervous tissue, as it transports toxic substances back
to the systemic circulation (9,10).
Recently, genetic polymorphisms in these enzymes have been
described. However, the clinical relevance of these variations has
not as yet been fully explored in clinical studies.
In a cohort of 97 Caucasian cancer patients, no
significant association was observed between different alleles in
the ABCB1, CYP2C8 and CYP3A4 genes and the pharmaco-kinetics of
paclitaxel (11). Moreover, a
recent study showed no association between polymorphisms in ABCB1
and the pharmacokinetics of paclitaxel (12). These authors conclude that the
inter-individual variability in the pharmacokinetics of paclitaxel
cannot be attributed to genetic variations in this gene. However,
adverse effects such as neurotoxicity might be associated with
inherited alleles in these genes through mechanisms unrelated to
plasma pharmacokinetics. Genetic variation in ABCB1 has been
associated with response to paclitaxel treatment, but the
literature has not been conclusive (24).
The purpose of this study was to investigate the
association between the occurrence and degree of neurotoxicity
following paclitaxel treatment in breast and ovarian cancer and to
correlate these clinical findings with the allele frequency of
variants in the ABCB1, CYP2C8 and CYP3A4 genes reportedly leading
to impaired enzyme activity.
Materials and methods
Patient selection
This study comprised 36 female patients with breast
cancer (24 patients) or ovarian cancer (12 patients), all of which
developed clinical neurotoxicity grade 1–2 according to the
NCI-CTCAE (v. 3.0) during paclitaxel-containing chemotherapy.
Information concerning debut of toxicity was obtained from
chart-review. Among the breast cancer patients, 4 were treated with
paclitaxel as a single drug (2 on a weekly basis), 18 with
paclitaxel, epirubicin and capecitabine, while 2 received
paclitaxel and herceptin. Among the ovarian cancer patients, 1
received weekly paclitaxel and 11 were administered combination
chemotherapy with paclitaxel and carboplatin. Prior chemotherapy
had been administered to 15 of the total 36 patients. The patients
median age was 58 years (range, 40–80). The patients were diagnosed
and treated at the Department of Oncology at Sahlgrenska University
Hospital. Informed consent was obtained, and the study was approved
by the regional ethics committee. Our control sample consisted of
50 healthy blood donors at Sahlgrenska University Hospital.
Genetic analysis/genotyping
Genomic DNA was isolated from peripheral leucocytes
from the 36 blood samples using the Puregene® DNA
Isolation Kit (Gentra Systems, Minneapolis, MN, USA). PCR primers
were purchased from Invitrogen®.
Genotyping of the CYP2C8*3 allele was
performed by a polymerase chain reaction-based restriction fragment
length polymorphism (PCR-RFLP) as previously described (6). The analysis was conclusive for 35
samples. Genotyping of the CYP3A4*1b allele was also
performed by PCR-RFLP (13). The
analysis was conclusive for 31 samples.
Genotyping of the SNP 2677G/T/A of the ABCB1 gene
was performed by PCR (14),
followed by DNA sequence analysis using the ABI 3100 PRISM Genetic
Analyzer and the Big Dye Terminator Cycle Sequencing Ready Reaction
Kit (both from Applied Biosystems, Foster City, CA, USA).
Genotyping for the SNP 3435C/T was performed by a
PCR-RFLP. The PCR primer sequences 5′TGT TTT CAG CTG CTT GAT GG-3′
and 3′CTC CGG TTG TAT GTA CGG AA-5′ were obtained from Epidauros
Biotechnologie AG (Bernried, Germany). The PCR program consisted of
30 cycles at 95°C for 30 sec, 55°C for 30 sec, 72°C for 60 sec and
a final elongation step at 72°C for 7 min. The PCR fragment was
subjected to cleavage with the DpnII enzyme. The analysis
was conclusive for 36 samples.
All products from the PCR-RFLP analysis were
separated on a 3% agarose gel.
Statistical evaluation
Statistical analyses were carried out using the SAS
system. The differences in allele frequencies among literature
control population, blood donor controls and patients were analysed
using the Chi-square test. The analysis of association between mean
debut dose of paclitaxel and grade of neurotoxicity and 3435C/T
SNPs was performed using the Fisher’s exact test.
Results
Patients
Patients were selected for the study when they
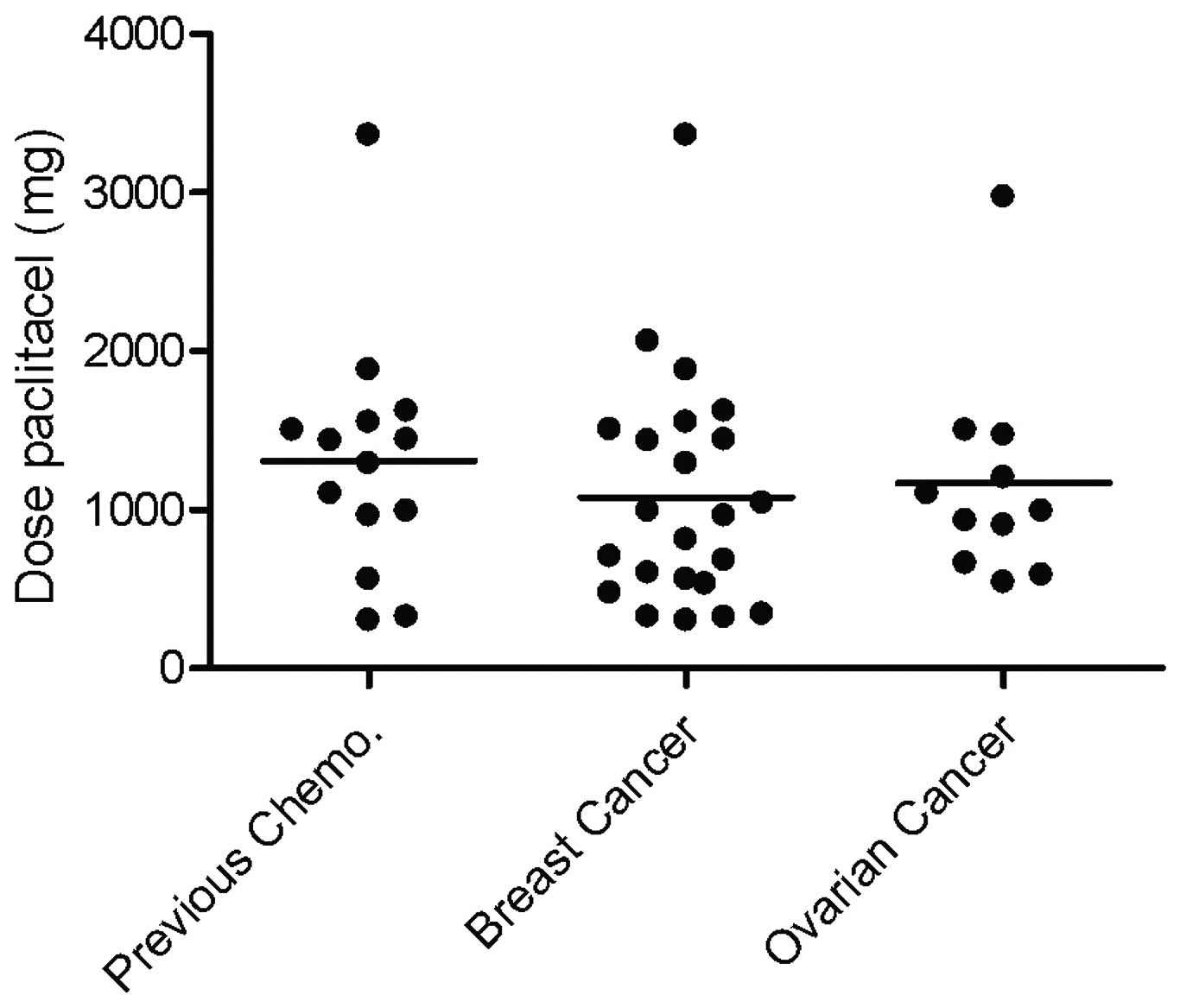
experienced neurotoxicity. There was no significant difference in
the mean debut dose of paclitaxel for neurotoxicity grade 1 based
on diagnosis, or if the patients had received prior chemotherapy.
The mean debut dose for neurotoxicity for all analyzed patients was
1129 mg (range, 300–3360) (Fig.
1).
CYP2C8 and CYP3A4
The CYP2C8*3 allele frequency in our
study sample (n=35) was determined by PCR-RFLP (data not shown).
The allele frequency was 14.3% as compared to the expected
frequency of 14% (13–15%) noted in populations of similar Caucasian
origin (15).
The allele CYP3A4*1b, with an expected
population frequency of 2.0–9.6% (16), was not found in any of our patients
(n=31), indicating that this risk allele was not abundant in our
patient sample.
ABCB1
The ABCB1 2677G/T/A and 3435C/T SNPs were analysed
by DNA sequencing and RFLP after PCR amplification of exon 21 and
26, respectively.
The distribution of alleles at position 3435C/T and
2677G/T/A was compared with the expected population frequencies
obtained from the analyses of 200 randomly selected individuals
from the southeastern part of Sweden (Table I) (17). The distribution in our patient
sample closely resembled the distribution noted in the literature
control sample, implying that these two cohorts were not
significantly stratified (Chi-square test, p=0.29). This finding
contradicts previously published data suggesting that patients
carrying the 3435T allele have a higher risk for neurotoxicity.
 | Table IFrequencies of ABCB1 3435C/T alleles
in patients, literature controls and blood donor controls. |
Table I
Frequencies of ABCB1 3435C/T alleles
in patients, literature controls and blood donor controls.
| Alleles | |
|---|
|
| |
|---|
| C/C | C/T | T/T | Total |
|---|
| Patients | 12 | 16 | 8 | 36 |
| Literature
controls | 46 | 88 | 66 | 200 |
| Blood donor
controls | 11 | 28 | 11 | 50 |
| Total | 58 | 104 | 74 | 286 |
The literature control population sample we used was
geographically closely linked to our study population, but to
strengthen our data and avoid the possibility of population bias,
we also examined the distribution of the 3435T allele in 50 blood
donor controls from the same university hospital as our patients.
As anticipated, the frequency of each allele did not differ
statistically from that of the literature control population sample
(Chi-square test, p=0.24). The allele frequencies in the control
groups did not differ significantly from published reports
including ethnically similar subjects (22,23).
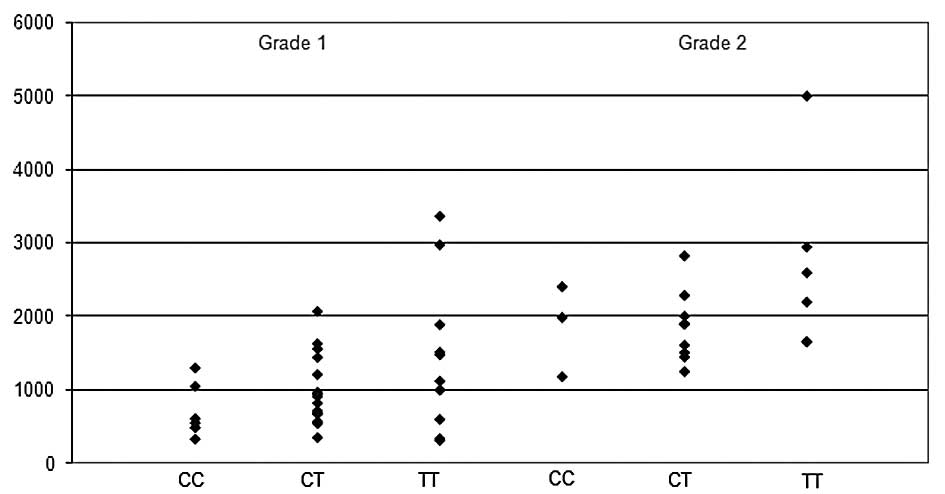
Furthermore, there was no statistically significant difference
between mean debut dose of paclitaxel, grade of neurotoxicity and
3435C/T SNPs (Chi-square test, p=0.61 or Fisher’s exact test,
p=0.69) (Fig. 2).
Discussion
With the aim to study the inter-individual variation
of paclitaxel-induced neurotoxicity in relation to genetic
variation, relevant gene polymorphisms in the three metabolising
enzymes, CYP2C8, CYP3A4 and ABCB1, were analysed. CYP2C8 is the
principle enzyme metabolising paclitaxel. CYP2C8*3,
which is found primarily in Caucasians, has shown only 15% of the
enzymatic turnover number of wild-type CYP2C8 for paclitaxel in
vitro (6). Lower enzyme
activity for CYP2C8*3 compared with the wild-type has
also been shown in human liver microsomes (18). In an attempt to verify in
vivo whether the suggested decrease in enzyme activity for this
allele correlated to neurotoxicity, we analysed the
CYP2C8*3 allele frequency in patients experiencing at
least grade 1–3 neurotoxicity after treatment with paclitaxel. We
reported an allele frequency of 14.3% as compared with the expected
frequency of 14% (13–15%) (15). We
concluded that neurotoxicity as a side effect of paclitaxel
treatment is not associated with an increased incidence of
CYP2C8*3 allele frequency. The suggested decrease in
enzyme activity shown for this allele by the in vitro data
has therefore not been confirmed in this patient group.
CYP3A4 is the most abundant P-450 enzyme in the
human liver and it metabolises more than 50% of prescription drugs.
The CYP3A4*1b allele has been associated with prostate
cancer and estrogen receptor-negative breast cancer (25). Moreover, CYP3A4*1b has
been shown to influence enzyme activity (26).
The allele frequency of the 3A4*1b allele
differs between populations, and the expected frequency in our
Swedish sample was not previously determined. However, as this
allele was not detected in our patient sample, we conclude that it
is probably of minor importance in the pathogenesis of
neurotoxicity.
P-glycoprotein, encoded by ABCB1, is an ATP-driven
drug export pump. It is expressed in many tissues such as the
intestine and the blood-brain barrier. Furthermore, high expression
in ovarian tumour cells has been shown to correlate with a poor
response to treatment with paclitaxel (19). Several SNPs in the ABCB1 gene have
been described and two of them (2677G/T/A and 3435C/T) have been
correlated to p-glycoprotein expression in the Caucasian
population. As a result, individuals homozygous for the 3435T
alleles were shown to express lower levels of p-glycoprotein in the
intestine and subsequently higher plasma levels of the drug
(20). Patients with low
p-glycoprotein expression would be more likely to suffer from
neurotoxicity, since this would indicate a higher systemic
concentration of the drug. Recently, the ABCB1 alleles G2677T/A
were shown to correlate with the response to paclitaxel treatment
in ovarian cancer in a Swedish patient sample (17). In this study by Gréen et al,
the frequency of the T allele was higher in patients experiencing a
favorable response. However, the 3435C/T SNP was not found to
correlate with treatment outcome. Moreover, no significant
difference in SNP frequencies could be found between the reference
population and the patients with ovarian cancer. There are several
previous studies showing an association between the 3435C allele
and poor response. Consequently, Kafka et al showed that the
alleles T/T at position 3435 correlated with a complete clinical
response to chemotherapy in locally advanced breast cancer
(21).
The association of the 2677G/T/A and 3435C/T SNPs
with paclitaxel-induced neurotoxicity and neutropenia was recently
evaluated in a German study by Sissung et al (12). In this study, comprising 22 patients
experiencing peripheral neuropathy, none of the patients carrying
the 3435C/C alleles developed peripheral neuropathy after
paclitaxel treatment. In addition, there was a trend towards an
increased risk of neurotoxicity for individuals carrying 3435C/T or
3435T/T. This result was not reproduced in our Swedish patient
sample. Given the close proximity of the study populations in these
two studies, we conclude that the 3435T allele does not increase
the risk for paclitaxel-induced neurotoxicity.
The German study also showed that 3435 T/T in
combination with 2667T/T conferred a risk of neutropenia. Linkage
disequilibrium between these two SNPs has been proposed (22) and it was also evident in our
data.
In conclusion, by analysing the CYP2C8, CYP3A4 and
ABCB1 genes implicated in paclitaxel pharmacogenetics, we showed no
association between these alleles and paclitaxel-induced
neurotoxicity. Our data contradict the previously reported
association between the 3435T allele (12) and neurotoxicity. This implies that
other genetic and/or environmental mechanisms regulate the
individual difference in susceptibility to paclitaxel-induced
neurotoxicity.
The data presented here will be re-analysed in a
large, randomised, phase III study comprising more than 300 cases
of breast cancer. In this study, polymorphisms in genes related to
paclitaxel pharmacogenomics will be analysed with the aim of
obtaining an insight into predictive or prognostic factors relating
to paclitaxel efficiency and toxicity.
In addition to SNPs, inter-individual genetic
variation is also composed of small insertions/deletions in the
genome, VNTRs, CNVs as well as epigenetic effects such as DNA
methylation, which also opens possibilities for further studies on
genetic variation and paclitaxel-induced adverse events.
Acknowledgements
This work was supported by grants from the Assar
Gabrielsson Foundation.
References
|
1
|
Socinski MA: Cytotoxic chemotherapy in
advanced non-small cell lung cancer: a review of standard treatment
paradigms. Clin Cancer Res. 10:4210–4214. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Fellner S, Bauer B, Miller DS, et al:
Transport of paclitaxel (Taxol) across the blood-brain barrier in
vitro and in vivo. J Clin Invest. 110:1309–1318. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Walle UK and Walle T: Taxol transport by
human intestinal epithelial Caco-2 cells. Drug Metab Dispos.
26:343–346. 1998.PubMed/NCBI
|
|
4
|
Huizing MT, Giaccone G, van Warmerdam LJ,
et al: Pharmacokinetics of paclitaxel and carboplatin in a
dose-escalating and dose-sequencing study in patients with
non-small cell lung cancer. The European Cancer Centre. J Clin
Oncol. 15:317–329. 1997.PubMed/NCBI
|
|
5
|
Sonnichsen DS, Hurwitz CA, Pratt CB,
Shuster JJ and Relling MV: Saturable pharmacokinetics and
paclitaxel pharmacodynamics in children with solid tumors. J Clin
Oncol. 12:532–538. 1994.PubMed/NCBI
|
|
6
|
Dai D, Zeldin DC, Blaisdell JA, Chanas B,
Coulter SJ, Ghanayem BI and Goldstein JA: Polymorphisms in human
CYP2C8 decrease metabolism of the anticancer drug paclitaxel and
arachidonic acid. Pharmacogenetics. 11:597–607. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Harris JW, Rahman A, Kim BR, Guengerich FP
and Collins JM: Metabolism of taxol by human hepatic microsomes and
liver slices: participation of cytochrome P450 3A4 and an unknown
P450 enzyme. Cancer Res. 54:4026–4035. 1994.PubMed/NCBI
|
|
8
|
Malingré MM, Beijnen JH and Rosing H:
Co-administration of GF120918 significantly increases the systemic
exposure to oral paclitaxel in cancer patients. Br J Cancer.
84:42–47. 2001.PubMed/NCBI
|
|
9
|
Cordon-Cardo C, O’Brien JP, Boccia J, et
al: Multidrug-resistance gene (P-glycoprotein) is expressed by
endothelial cells at blood-brain barrier sites. Proc Natl Acad Sci
USA. 86:695–698. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Schinkel AH, Smit JJ and van Tellingen O:
Disruption of the mouse mdr1a P-glycoprotein gene leads to a
deficiency in the blood-brain barrier and to increased sensitivity
to drugs. Cell. 77:491–502. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Henningsson A, Marsh S and Loos WJ:
Association of CYP2C8, CYP3A4, CYP3A5 and ABCB1 polymorphisms with
the pharmacokinetics of paclitaxel. Clin Cancer Res. 11:8097–8104.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Sissung TM, Mross K, Steinberg SM,
Behringer D, Figg WD, Sparreboom A and Mielke S: Association of
ABCB1 alleles with paclitaxel-mediated peripheral neuropathy and
neutropenia. Eur J Cancer. 42:2893–2896. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Cavalli SA, Hirata MH and Hirata RD:
Detection of MboII polymorphism at the 5′ promoter region of
CYP3A4. Clin Chem. 47:348–351. 2001.
|
|
14
|
Kim DH, Park JY, Sohn SK, et al: Multidrug
resistance-1 gene polymorphisms associated with treatment outcomes
in de novo acute myeloid leukemia. Int J Cancer. 118:2195–2201.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Spratlin J and Sawyer MB: Pharmacogenetics
of paclitaxel metabolism. Crit Rev Oncol Hematol. 61:222–229. 2007.
View Article : Google Scholar
|
|
16
|
Lamba JK, Lin YS, Schuetz EG and Thummel
KE: Genetic contribution to variable human CYP3A-mediated
metabolism. Adv Drug Deliv Rev. 54:1271–1294. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Gréen H, Söderkvist P, Rosenberg P,
Horvath G and Peterson C: Mdr-1 single nucleotide polymorphisms in
ovarian cancer tissue: G2677T/A correlates with response to
paclitaxel chemotherapy. Clin Cancer Res. 12:854–859.
2006.PubMed/NCBI
|
|
18
|
Bahadur N, Leathart JB, Mutch E, et al:
CYP2C8 polymorphisms in Caucasians and their relationship with
paclitaxel 6alpha-hydroxylase activity in human liver microsomes.
Biochem Pharmacol. 64:1579–1589. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Szakács G, Paterson JK, Ludwig JA,
Booth-Genthe C and Gottesman MM: Targeting multidrug resistance in
cancer. Nat Rev Drug Discov. 5:219–234. 2006.
|
|
20
|
Hoffmeyer S, Burk O, von Richter O, et al:
Functional polymorphisms of the human multidrug-resistance gene:
multiple sequence variations and correlation of one allele with
P-glycoprotein expression and activity in vivo. Proc Natl Acad Sci
USA. 97:3473–3478. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kafka A, Sauer G, Jaeger C, Grundmann R,
Kreienberg R, Zeillinger R and Deissler H: Polymorphism C3435T of
the MDR-1 gene predicts response to preoperative chemotherapy in
locally advanced breast cancer. Int J Oncol. 22:1117–1121.
2003.PubMed/NCBI
|
|
22
|
Siddiqui A, Kerb R, Weale ME, et al:
Association of multidrug resistance in epilepsy with a polymorphism
in the drug-transporter gene ABCB1. N Engl J Med. 348:1442–1448.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Cascorbi I, Gerloff T, Johne A, et al:
Frequency of single nucleotide polymorphisms in the P-glycoprotein
drug transporter MDR1 gene in white subjects. Clin Pharmacol Ther.
69:169–174. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Green H: Pharmacogenomics of importance
for paclitaxel chemotherapy. Pharmacogenomics. 9:671–674. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Keshava C, McCanlies EC and Weston A:
CYP3A4 poly-morphisms – potential risk factors for breast and
prostate cancer: a HuGE review. Am J Epidemiol. 160:825–841.
2004.
|
|
26
|
Rodríguez-Antona C, Sayi JG, Gustafsson
LL, Bertilsson L and Ingelman-Sundberg M: Phenotype-genotype
variability in the human CYP3A locus as assessed by the probe drug
quinine and analyses of variant CYP3A4 alleles. Biochem Biophys Res
Commun. 338:299–305. 2005.PubMed/NCBI
|