Introduction
True adenocarcinoma of the distal bile duct (i.e.
arising in the retroduodenal or intrapancreatic portion of the
common bile duct) are uncommon neoplasms that comprise a small
portion of all periampullary malignancies necessitating
pancreaticoduodenectomy (PD) (1,2). Since
experience with these neoplasms is limited (2,3), they
are often analyzed in conjunction, either with upper- and mid-third
bile duct carcinoma (4), or with
periampullary malignancies in general (5).
Among several potential recently innovated oral
agents, an oral combined fluoropyrimidine S-1 (tegafur, gimeracil
and oteracil) has been recently used for gastrointestinal (6), pancreatic (7) and bile duct cancer (BDC) (8). Other promising agents include
gemcitabine (9,10) and bevacizumab (11). To date, however, few reports are
available regarding the effects of a combination of these agents on
metastatic BDC.
We report a case of hepatic metastasis from distal
BDC of the ampulla, in which long-term control was obtained by a
multidisciplinary treatment with radiofrequency ablation (RFA),
surgery and chemotherapy using S-1, gemcitabine and
bevacizumab.
Case report
A 65-year-old man presented with intermittent
abdominal pains for several days. His complete blood count showed
leukocytosis and thrombocytosis. Laboratory studies disclosed
elevations in bilirubin (2.5 mg/dl), liver enzymes (AST 577 IU/l,
ALT 452 IU/l) and alkaline phosphatase (149 IU/l). Ultrasonography
(US) showed a slight dilatation of the common bile duct and the
hepatic duct without any sign of a stone or tumor. Endoscopic
retrograde cholangiopancreatogaphy (ERCP) showed a filling defect
in the distal bile duct of the ampullary area, and a biopsy
revealed adenocarcinoma. Computed tomography combined with
angiography revealed a hypervascular tumor in the distal bile duct
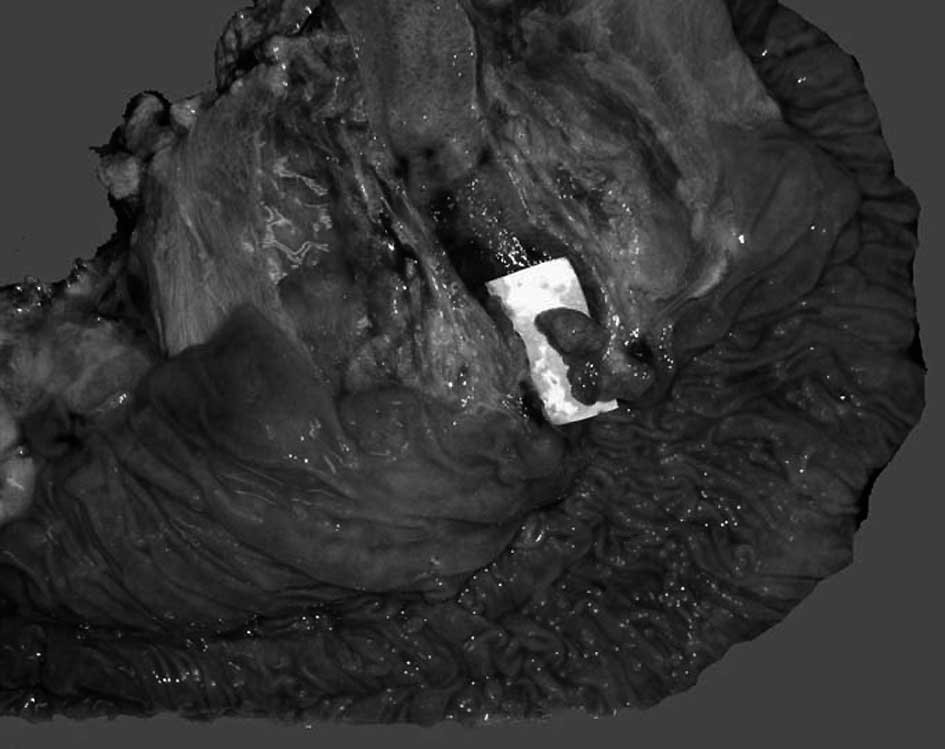
(Fig. 1). The patient underwent a
PD in July, 2006. A surgical specimen showed a small polypoid tumor
(10 × 6 × 6 mm) in the distal bile duct of the ampullary area
(Fig. 2). According to TNM
classification, this case was classified as T1N0M0 (stage I).
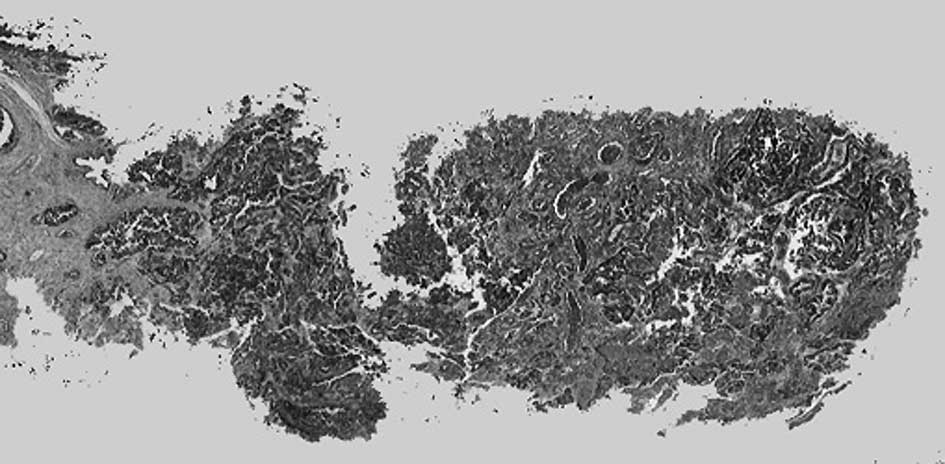
Pathological findings revealed a papillary adenocarcinoma limited
to the biliary mucosa without any infiltration to vessels or the
neural plexus (Fig. 3). No
metastasis was noted in the regional lymph nodes. His
post-operative course was uneventful, and he was discharged from
the hospital without any complications.
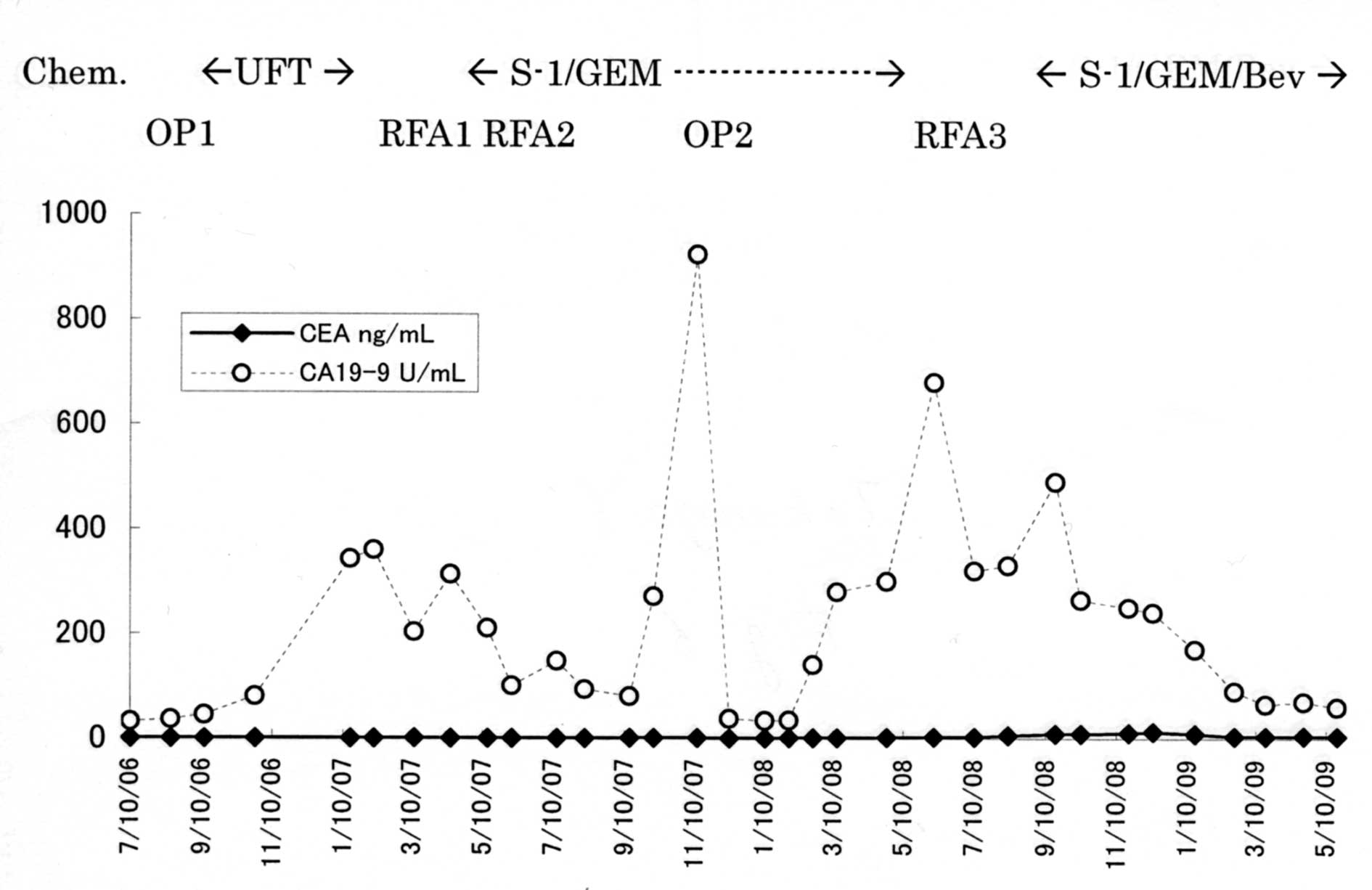
The patient was well without any evidence of
recurrence for 7 months, being managed with adjuvant chemotherapy
using oral UFT (a combination of tegafur and uracil, 375
mg/m2/day). Eight months after surgery, tumor markers
including carcinoembryonic antigen (CEA) and carbohydrate antigen
(CA)19-9 gradually increased. CT scans and magnetic resonance
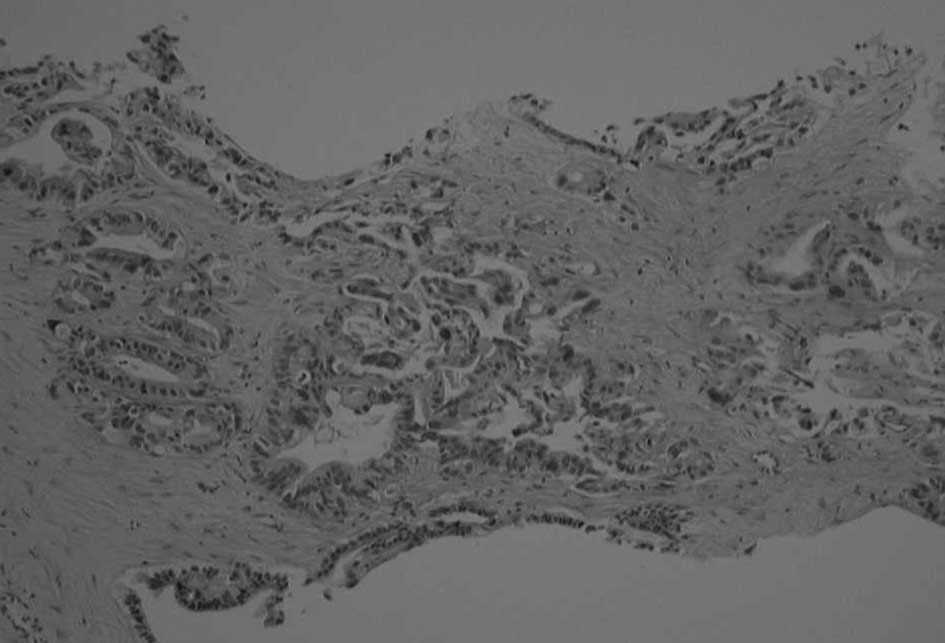
imaging showed a hepatic tumor ~1 cm in diameter (Fig. 4). A biopsy revealed a papillary
adenocarcinoma conjectured to be the result of metastasis from the
primary tumor (Fig. 5), and RFA was
performed upon consent of the patient.
Combined chemotherapy with S-1 (80 mg/m2
on days 1–14 with 7 days off) and gemcitabine (1000
mg/m2 on day 8) was initiated after RFA. The
chemotherapy was continued on an outpatient basis. After 3 courses
of chemotherapy, CT scans revealed that the lesion resolved with a
decline in the CA19-9 level (Fig.
6), and the patient appeared to achieved a complete response.
Although the response was maintained for 4 months with the
chemotherapy, there was regrowth of the tumor to 2 cm in diameter.
We performed RFA again and maintained the chemotherapy upon consent
of the patient. Since another metastatic lesion developed in the
marginal zone 4 months after the RFA (Fig. 7), we performed hepatic
segmentectomy. Fourteen months after the hepatectomy, another
hepatic metastasis developed in the remnant liver. Bevacizumab (10
mg/kg on day 8) was added to the combination chemotherapy with S-1
and gemcitabine, since the cancer seemed resistant to the
chemotherapy alone. After 2 courses of chemotherapy with
bevacizumab, abdominal contrast CT scans revealed that the lesion
was resolved with a decline in the tumor markers. The patient was
effectively managed for 3 years after the initial PD by a
multidisciplinary treatment with RFA, surgery and the combination
chemotherapy on an outpatient basis.
Discussion
Experiences regarding the outcome of surgery,
survival and management of patients with distal BDC are limited and
have not been well reported for several reasons. First, it is the
most infrequent type of periampullary malignancy including
pancreatic, ampullary and duodenal cancers. Second, this subset of
cholangiocarcinomas is usually described in combination with hilar
and intrahepatic cholangiocarcinomas which appear to have different
predisposing factors (4,5) and, therefore, may have a very
different natural history.
Todoroki et al reported recurrence patterns
of ampullary cancer including distal BDC after currative resection
(12). The overall frequency of
distant metastasis was 44% and that of local recurrence was 11%.
The most frequent site of distant metastasis was the liver (67%)
and the second most common was the distant lymph nodes (54%)
followed by the peritoneum (21%) and the lung (21%). From the
histopathologic point of view, locoregional spread to lymph nodes
within the resected specimen was less common for distal BDC than
for pancreatic ductal cancer (2,13). In
contrast to lymph nodes metastases, the incidences of direct
lymphatic infiltration (27%) and perineural invasion (60%) suggest
a more aggressive tumor biology and portend a less favorable
prognosis despite the small size of the primary tumors (2,3).
According to published data, the 5-year survival
after resection of distal BDC is approximately 20–30% (1–3).
Although these neoplasms represent a minority of the patient
population undergoing PD and the experience at any institution with
distal DBC is necessarily limited, similar clinical outcome and
survival are consistent and suggest a somewhat better prognosis
than for pancreatic ductal cancer but not quite as good as for
periampullary adenocarcinomas arising from the ampullary or
duodenal mucosa (14,15). This case indicates that distal BDC
even in an early stage has more malignant potential than
anticipated, and that meticulous follow-up with tumor markers and
imaging studies are necessary in these cases.
The optimal chemotherapy regimen for recurrent
hepatic metastasis has not yet been established since previous
chemotherapy with 5-fluorouracil (5-FU) has not proved beneficial
in unresectable BDC and in an adjuvant setting after surgical
resection (16,17). New anticancer agents such as S-1 and
gemcitabine, recently introduced in clinical practice, provide the
potential to improve prognosis in patients with unresectable BDC
and recurrent BDC after surgery (6–10).
S-1, a new oral fluoropyrimidine, consists of tegafur and two
modulators, 5-choloro-2,4-dihydroxypyrimidine (CDHP) and potassium
oxonate (OXO). CDHP is a competitive inhibitor of dihydropyrimidine
dehydrogenase, which is an enzyme for 5-FU degradation. OXO
ameliorates gastrointestinal toxicity of tegafur by a competitive
inhibition of orotate phosphoribosyltransferase in the
gastrointestinal mucosa (6). As a
single agent in a phase II study for advanced pancreatic cancer
(7) and BDC (8), the response rate of S-1 was
approximately 40%, with a low incidence of grade 3 or 4 toxicity
(7,8). Recently, Nakamura et al
reported a response rate of 48% and an overall survival of 12.5
months in a phase II trial of S-1 with gemcitabine for metastatic
pancreatic cancer (18). The study
of the effects of S-1 with gemcitabine on advanced BDC is limited,
though reports on the effects of gemcitabine as a single agent are
available (10).
Bevacizumab was added to the chemotherapy in our
case since the hepatic metastases developed, as the chemotherapy
was continued. This agent was proved to be quite effective for
treatment of advanced colorectal cancer when used in combination
with chemotherapy (11). To date,
however, few reports are available regarding the effects of
bevacizumab on pancreatic cancer or BDC (19).
In the present case, the hepatic metastases were
effectively controlled by a multidisciplinary treatment including
RFA, surgery and combination chemotherapy with S-1, gemcitabine and
bevacizumab. This chemotherapy is feasible on an out-patient basis
and may be one of the treatment options for metastatic BDC.
References
|
1
|
Nakeeb A, Pitt HA, Sohn TA, Coleman J,
Abrams RA, Piantadosi S, Hruban RH, Lillemoe KD, Yeo CJ and Cameron
JL: Cholangiocarcinoma: a spectrum of intrahepatic, perihilar and
distal tumors. Ann Surg. 224:463–475. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Fong Y, Blumgart LH, Lin E, Fortner JG and
Brennan MF: Outcome of treatment for distal bile duct cancer. Br J
Surg. 83:1712–1715. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Bortolasi L, Burgart LJ, Tsiotos GG,
Lugue-De Leon E and Sarr MG: Adenocarcinoma of the distal bile duct
(a clinicopathologic outcome analysis after curative resection).
Dig Surg. 17:36–41. 2000.PubMed/NCBI
|
|
4
|
Nagorney DM, Donohue JH, Farnell MB,
Schleck CD and Ilstrup DM: Outcome after curative resection of
cholangiocarcinoma. Arch Surg. 128:871–879. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kayahara M, Nagakawa T, Ueno K, Ohta T,
Tsukioka Y and Miyazaki I: Surgical strategy for carcinoma of the
pancreas head area based on clinicopathologic analysis of nodal
involvement and plexus invasion. Surgery. 117:616–623. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Shirasaka T, Shimamoto Y, Ohshimo H,
Yamaguchi H, Kato T, Yonekura K and Fukushima M: Development of a
novel form of an oral 5-fluorouracil derivative (S-1) directed to
the potentiation of the tumor selective toxicity of 5-fluorouracil
by two biochemical modulators. Anticancer Drugs. 7:548–557. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Okusaka T, Funakoshi A, Furuse J, Boku N,
Yamao K, Ohkawa S and Saito H: A late phase II study of S-1 for
metastatic pancreatic cancer. Cancer Chemother Pharmacol.
61:615–621. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ueno H, Okusaka T, Ikeda M, Takezako Y and
Morizane C: Phase II study of S-1 in patients with advanced biliary
tract cancer. Br J Cancer. 15:1769–1774. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lin MH, Chen JS, Chen HH and Su WC: A
phase II trial of gemcitabine in the treatment of advanced bile
duct and periampullary carcinoma. Chemotherapy. 49:154–158. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Okusaka T, Ishii H, Funakoshi A, Yamao K,
Ohkawa S, Saiot S, Saito H and Tsuyuguchi T: Phase II trial of
single-agent gemcitabine in patients with advanced biliary tract
cancer. Cancer Chemother Pharmacol. 57:647–653. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Hurwitz H, Fehrenbacher L, Novotny W,
Cartwright T, Hainsworth J, Heim W, Berlin J, Baron A, Griffing S,
Holmgren E, Ferrara N, Fyfe G, Rogers B, Ross R and Kabbinavar F:
Bevacizumab plus irinotecan, fluorouracil and leucovorin for
metastatic colorectal cancer. N Eng J Med. 350:2335–2342. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Todoroki T, Koike N, Morishita Y, Kawamoto
T, Ohkochi N, Shoda J, Fukuda Y and Takahashi H: Patterns and
failure after curative resections of carcinoma of the ampulla of
Vater. Ann Surg Oncol. 10:1176–1183. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Bhuiya MR, Nimura Y, Kamiya K, Kondo S,
Fukata S, Hayakawa N and Shionoya S: Clinicopathologic studies in
perineural invasion of bile duct carcinoma. Ann Surg. 215:344–349.
1992. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Chan C, Herrera MF, De la Garza L,
Quantanilla-Martinez L, Vargas-Vorackova F, Richaud-Patin Y,
Llorente L, Uscanga L, Robles-Diaz G and Leon E: Clinical behavior
and prognostic factors of periampullary adenocarcinoma. Ann Surg.
222:632–637. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Woo SM, Ryu JK, Lee SH, Yoo JW, Park JK,
Kim YT, Jang JY, Kim SW, Kang GH and Yoon YB: Recurrence and
prognostic factors of ampullary carcinoma after radical resection:
comparison with distal extrahepatic cholangiocarcinoma. Ann Surg
Oncol. 14:3195–3201. 2007. View Article : Google Scholar
|
|
16
|
Takada T, Nimura Y, Katoh H, Nagakawa T,
Nakayama T, Matsushiro T, Amano H and Wada K: Prospective
randomized trial of 5-fluorouracil, doxorubicin and mitomycin C for
non-resectable pancreatic and biliary carcinoma: multicenter
randomized trial. Hepatogastroenterology. 45:2020–2026. 1998.
|
|
17
|
Takada T, Amano H, Yasuda H, Nimura Y,
Matsushiro T, Kato H, Nagakawa T and Nakayama T: Is postoperative
adjuvant chemotherapy useful for gallbladder carcinoma? A phase III
multicenter prospective randomized controlled trial in patients
with resected pancreaticobiliary carcinoma. Cancer. 95:1685–1695.
2002. View Article : Google Scholar
|
|
18
|
Nakamura K, Yamaguchi T, Ishihara T, Sudo
K, Kato H and Saisho H: Phase II trail of oral S-1 combined with
gemcitabine in metastatic pancreatic cancer. Br J Cancer.
94:1575–1579. 2006.PubMed/NCBI
|
|
19
|
Kindler HL, Niedzwiecki D, Hollis D,
Martin EW, Schilsky RL and Goldberg RM: A double-blind,
placebo-controlled, randomized phase III trial of gemcitabine (G)
plus bevacizumab (B) versus gemcitabine plus placebo (P) in
patients (pts) with advanced panreatic cancer (PC): a preliminary
analysis of Cancer and Leukemia Group B (CALGB) 80303. In: ASCO
Gastrointestinal Cancer Symposium. abs. 108. 2007
|