Introduction
Despite improvements in surgical techniques, the
recurrence rate after radical resection for esophageal cancer has
been reported to reach 36.8–43.4%, and most cases of recurrence
occur within two years after surgery (1–8).
Establishing a non-invasive and reliable biomarker that enables the
early prediction of clinical outcomes is highly desirable.
Previous reports suggest the relationship between
tumor progression and hemodynamic changes in hepatic blood flow
(9–14). Leveson et al (9) reported that gastrointestinal cancer
patients with simultaneous liver metastasis exhibited a high
hepatic arterial blood flow as measured with scintigraphy when
compared with a control group. In colorectal cancer with
simultaneous liver metastasis, Leen et al (10) demonstrated that the hepatic arterial
blood flow was significantly increased and the portal blood flow
was significantly decreased in comparison with that observed in
healthy volunteers using Doppler ultrasonography. Cuenod et
al (13) reported that
hemodynamic changes, including decreases in the portal blood flow
and increases in the mean transit time, may be detected using CT
perfusion (CTP) in rats with occult liver metastases. Leggett et
al (14) reported that the use
of CTP in colorectal cancer patients with simultaneous liver
metastases revealed that the hepatic arterial blood flow was
significantly increased and the portal blood flow was decreased.
Therefore, hemodynamic changes in the hepatic blood flow can be a
potential biomarker for predicting patient outcomes.
CTP is a non-invasive imaging technique that enables
quantification of tissue blood flow in a target organ, by measuring
the temporal changes in tissue density following administration of
intravenous contrast medium. Since Miles et al (15) first described CTP, it has been
successfully applied in a variety of clinical conditions of the
liver (16–21). In addition, pretreatment CTP has
recently been demonstrated to be a useful marker to evaluate
therapeutic response or to assess cancer progression or outcome in
gastrointestinal cancer patients (22–26).
In this context, our hypothesis is that hepatic
blood flow is a more suitable method for assessing cancer
progression and outcomes than conventional histopathological and
molecular examinations of the primary tumor. Therefore, the aim of
this prospective study was to investigate the relationship between
the clinical outcomes of esophageal cancer patients and hemodynamic
changes in the liver measured by CTP.
Materials and methods
Patient population
The present study was approved by the ethics
committee of our institution, and informed consent was obtained
from all patients. According to the protocol of this study, all
patients had clinically and histopathologically proven esophageal
squamous cell carcinoma (ESCC) without distant metastasis or other
unresectable factors. CTP was performed in all patients prior to
surgery. For the patients receiving preoperative treatment, CTP was
performed after the completion of the preoperative treatment. The
patient eligibility criteria for this study were as follows: (i) 20
to 85 years of age; (ii) no sustained infection with hepatitis
virus; (iii) normal liver function; (iv) adequate renal function (a
serum creatinine level of <1.5 mg/dl) and (v) no past history of
malignant tumors. Sixty-two consecutive patients with ESCC treated
at Chiba University Hospital from June 2010 to December 2012 were
enrolled in this study. Fifteen patients were excluded since
acquired images were not suitable for CTP analysis due to an
insufficient concentration of the contrast agent and excessive
respiratory movements. Therefore, the data analysis was performed
in 47 patients (median age, 67 years; range, 53–82 years). The
median follow-up period was 17 months (range, 1–36 months).
Surgical treatment
Among the study population, 17 patients underwent
subtotal esophagectomy with field lymphadenectomy without
preoperative chemotherapy. Fifteen patients with a preoperative
diagnosis of lymph node metastasis underwent radical resection
after two cycles of neoadjuvant chemotherapy. The FP regimen
consisted of cisplatin at a dose of 80 mg/m2/day via
intravenous administration (day 1) and 5-fluorouracil (5FU) at a
dose of 800 mg/m2/day via continuous intravenous
infusion for five days (days 1–5) (27). Four patients who received
preoperative chemoradiotherapy (total 40 Gy) and underwent
downstaging were included in this study. In addition, 9 patients
were treated with endoscopic submucosal dissection (ESD). The
pathological tumor stage was assessed using the TNM classification
of the Union for International Cancer Control (UICC, 7th edition,
2009).
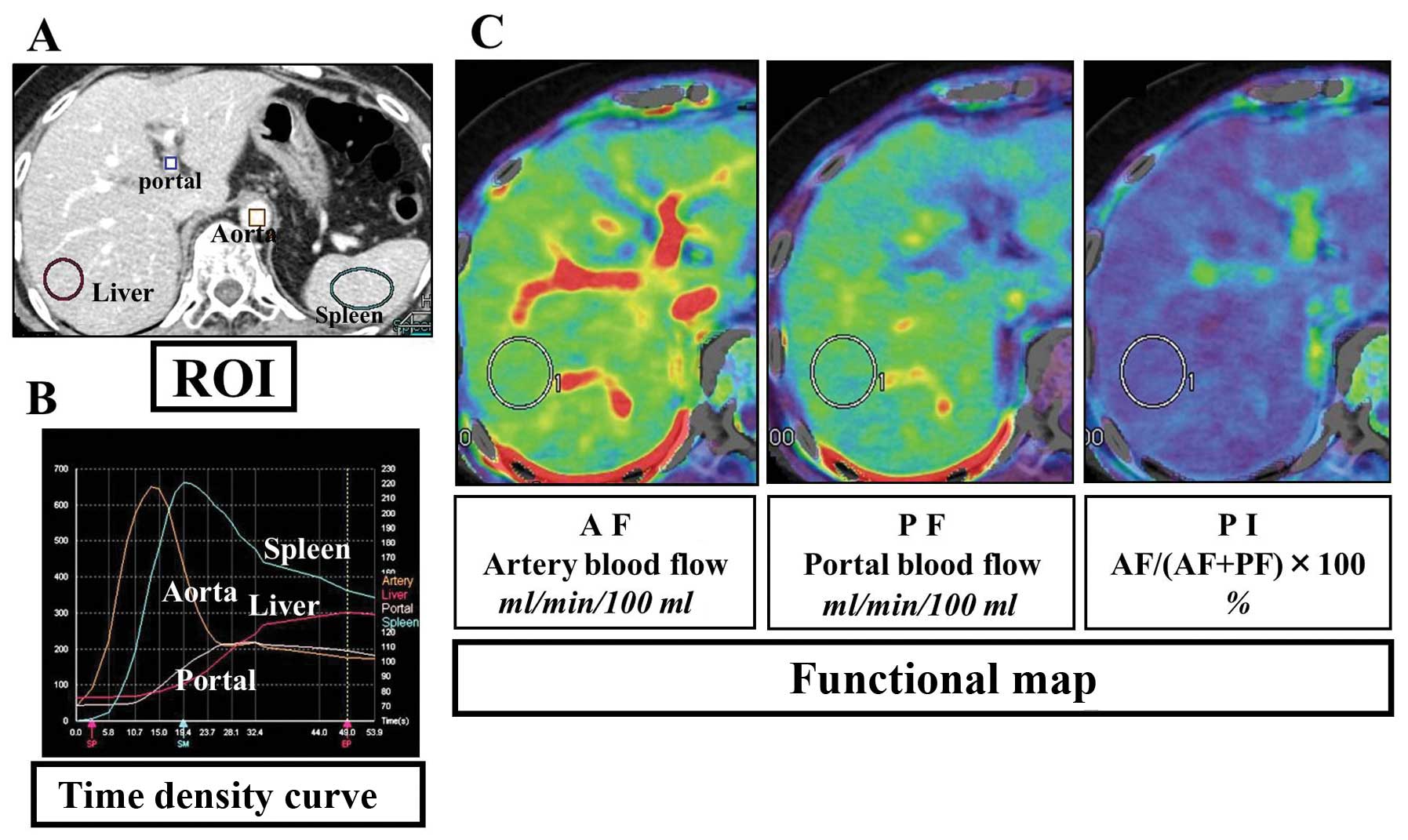
Imaging studies
Hepatic CTP was performed using 320-row area
detector CT (Aquilion One; Toshiba Medical Systems, Ohtawara,
Japan). First, we performed a non-enhanced CT scan of the upper
abdomen to identify the location of the liver. A 16-cm segment of
the whole liver (320 sequential 0.5-mm slices) was selected, and a
dynamic study of the selected area was performed in the static
table position without breath holding. The images were obtained 10
sec after the intravenous injection of 60 ml of iohexol (Omnipaque
300; Daiichi Sankyo, Tokyo, Japan) containing 300 mg of iodine/ml
administered at a rate of 6 ml/sec followed by 20 ml of saline
chaser using a dual power injector. The scanning parameters were as
follows: 0.5-mm reconstructed section thickness, 0.35-sec gantry
rotate time, 120 kV, 100 mA. After completion of the perfusion
scans, intravenous contrast was administered at 3.5 ml/sec, and a
routine thoracoabdominal study was performed. The procedure of the
analysis was as follows. First, the raw volume scan data were
analyzed using a software program (Body Registration; Toshiba
Medical Systems Corporation) in order to remove the influence of
breathing motion artifacts. Second, the registered perfusion data
were analyzed using a software program (Body Perfusion; Toshiba
Medical Systems Corporation), based on the dual input maximum slope
method (15,28). The parameters generated by the
software included the arterial blood flow (AF, ml/min/100 ml
tissue), portal blood flow (PF, ml/min/100 ml tissue) and perfusion
index (%) [PI = AF/(AF + PF) × 100]. In order to obtain these
parameters, it was necessary to set region of interests (ROIs) in
the following four sites; the liver parenchyma, spleen parenchyma,
aorta and portal vein. The time density curve (TDC) of the spleen
was used to separate the blood flow in the arterial phase and
portal phase, and the maximal slope of the liver TDC in each phase
was used to calculate both the arterial and portal perfusion.
Consequently, a three-dimensional color map (functional map) was
displayed (Fig. 1). A round or
oval-shaped ROI was placed on the right hepatic lobe on the
functional map (29), so that the
ROI would be as large as possible while avoiding vessels and
artifacts (30). Each parameter was
quantified as the average value of all pixels in the ROI. Data were
analyzed by gastroenterologic surgeons with at least five years of
experience in radiological imaging of gastroenterology. In the
comparison of the perfusion parameters by the three readers, there
were no significant differences between the readers (data not
shown).
Statistical analysis
Statistical significance was evaluated using the
Mann-Whitney U, Kruskal-Wallis and Chi-square tests. In addition,
we determined the optimal cut-off value for a high-risk of
recurrence using a receiver operating characteristic (ROC) curve.
Relapse-free survival curves were drawn according to the
Kaplan-Meier method, and the differences between the curves were
analyzed by applying the log-rank test. In the multivariate
analysis, a logistic regression model was used.
Results
Patient characteristics
The pathological stages were as follows: one patient
had stage 0; 20 patients had stage I (IA, n=18; IB, n=2); 11
patients had stage II disease (IIA, n=6; IIB, n=5); 12 patients had
stage III (IIIA, n=7; IIIB, n=2; IIIC, n=3) and one patient had
stage IV disease due to intramural metastasis in the stomach. Data
were unavailable for two patients for whom the tumor histologically
disappeared under the influence of preoperative treatment.
Therefore, data were available for 45 patients in the present
study.
Relationships between the preoperative
CTP parameters and histological features
The relationships between the histopathological
variables and preoperative perfusion parameters are listed in
Table I. The AF and the PI values
were significantly higher and the PF values were lower in the
patients with poorly differentiated tumors. There were no
significant statistical relationships between the pathological
stage (TNM classification of UICC) and the perfusion parameters
(Table II).
 | Table IPreoperative hepatic perfusion
parameters and clinicopathological features of the patients with
ESCC. |
Table I
Preoperative hepatic perfusion
parameters and clinicopathological features of the patients with
ESCC.
| Variables | AF | PF | PI |
|---|
| Tumor location |
| Upper | 28.5 | 128.4 | 18.5 |
| Lower | 25.7 | 127.1 | 16.9 |
| P (or yp)
stage |
| 0/1 | 25.8 | 128.3 | 17.0 |
| 2/3/4 | 27.7 | 127.1 | 18.0 |
| P (or yp) T |
| 0/1 | 26.0 | 130.8 | 16.8 |
| 2/3 | 27.6 | 127.7 | 18.2 |
| P (or yp) N |
| N0 | 26.4 | 129.1 | 17.1 |
| N1/2/3 | 27.5 | 128.4 | 18.1 |
|
Differentiationa |
| Well/moderate | 24.9 | 128.0 | 16.4 |
| Poor | 34.1 | 119.0 | 22.7 |
 | Table IIRelationships between pathological
stage and the preoperative perfusion parameters of the ESCC
patients. |
Table II
Relationships between pathological
stage and the preoperative perfusion parameters of the ESCC
patients.
| P stage (UICC) | AF | PF | PI |
|---|
| 0 (n=1) | 16.8 | 127.3 | 11.7 |
| IA/B (n=18/2) | 26.2 | 128.3 | 17.2 |
| IIA/B (n=6/5) | 27.9 | 133.1 | 17.6 |
| IIIA/B/C
(n=7/2/3) | 25.8 | 124.9 | 17.3 |
| IV (n=1) | 53.8 | 119 | 31.1 |
| P-valuea | N.S | N.S | N.S |
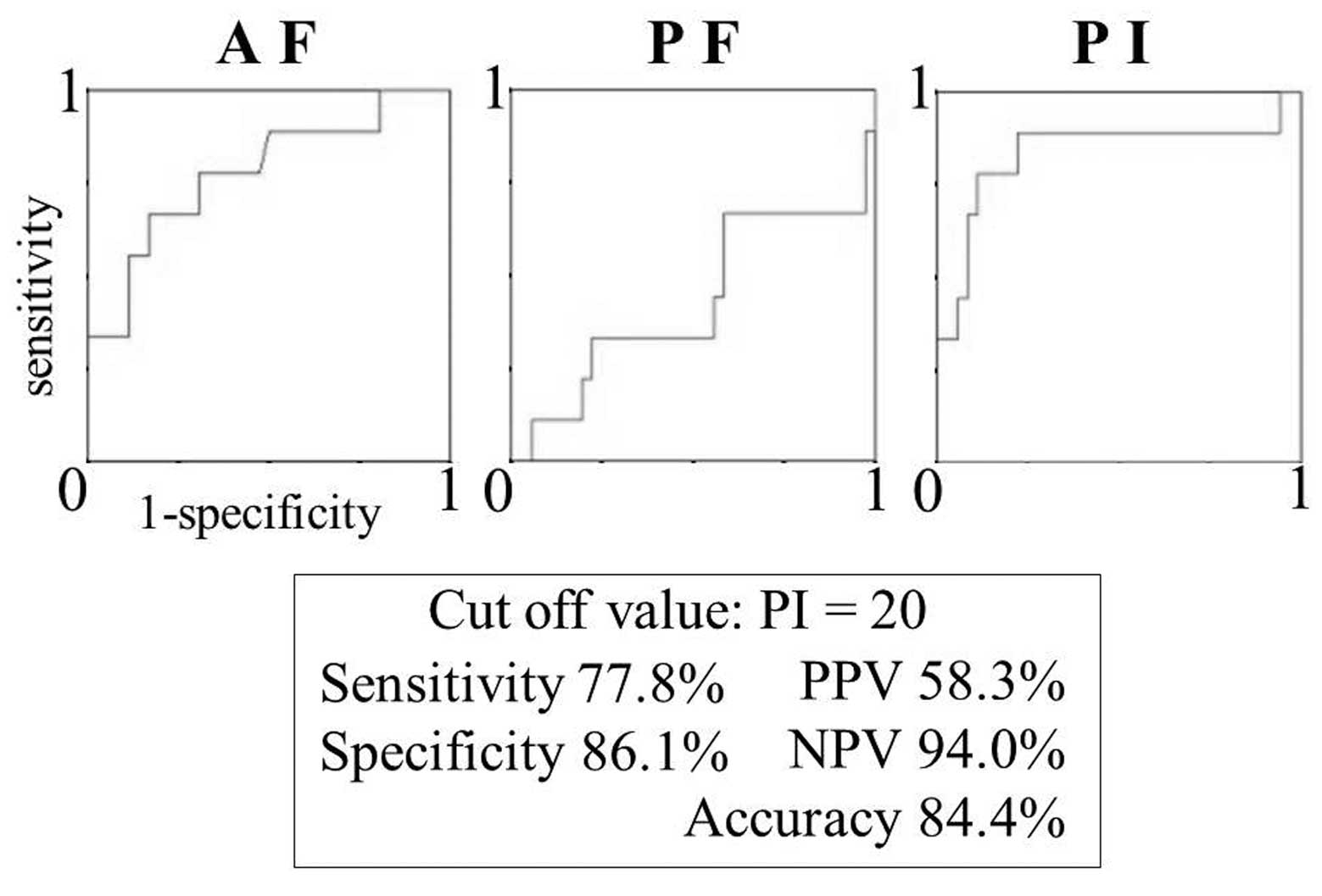
Correlations between the preoperative CTP
parameters and postoperative recurrence
In the present study, postoperative recurrence was
demonstrated in 9 ESCC patients during the short-term observation
period by contrast CT. The sites of recurrence in these 9 patients
were as follows: liver, 5; lymph nodes, 7; peritoneum, 2; bone, 1;
brain, 1; adrenal glands, 1; kidneys, 1 (duplication is included).
In the 9 patients with recurrence, AF and PI values were
significantly higher than those observed in the 36 patients who did
not develop recurrence during the observation period (PI, 23.9 vs.
15.9; P=0.0022, Mann-Whitney U test). The mean PI in the 5 patients
with liver metastasis was 26.5 (range, 10.5–42), while the mean PI
of the 4 patients with recurrence outside of the liver (site of
recurrence: para-aortic lymph node, regional lymph nodes,
multifocal hematogenous distant metastases) was 20.8 (range,
17.3–23.3) (P=0.32, Mann-Whitney U test). To determine the optimal
cut-off value for predicting patients at a high-risk of
postoperative recurrence before surgery, we analyzed the receiver
operating characteristic (ROC) curve of the preoperative CTP
parameters. We identified the ESCC patients with a PI of >20 as
having a high-risk of recurrence and patients with a PI of <20
on preoperative CTP as having a low-risk of recurrence (sensitivity
and specificity, 77.8 and 86.1%, respectively) (Fig. 2). We compared the background factors
between the two groups and found no significant differences
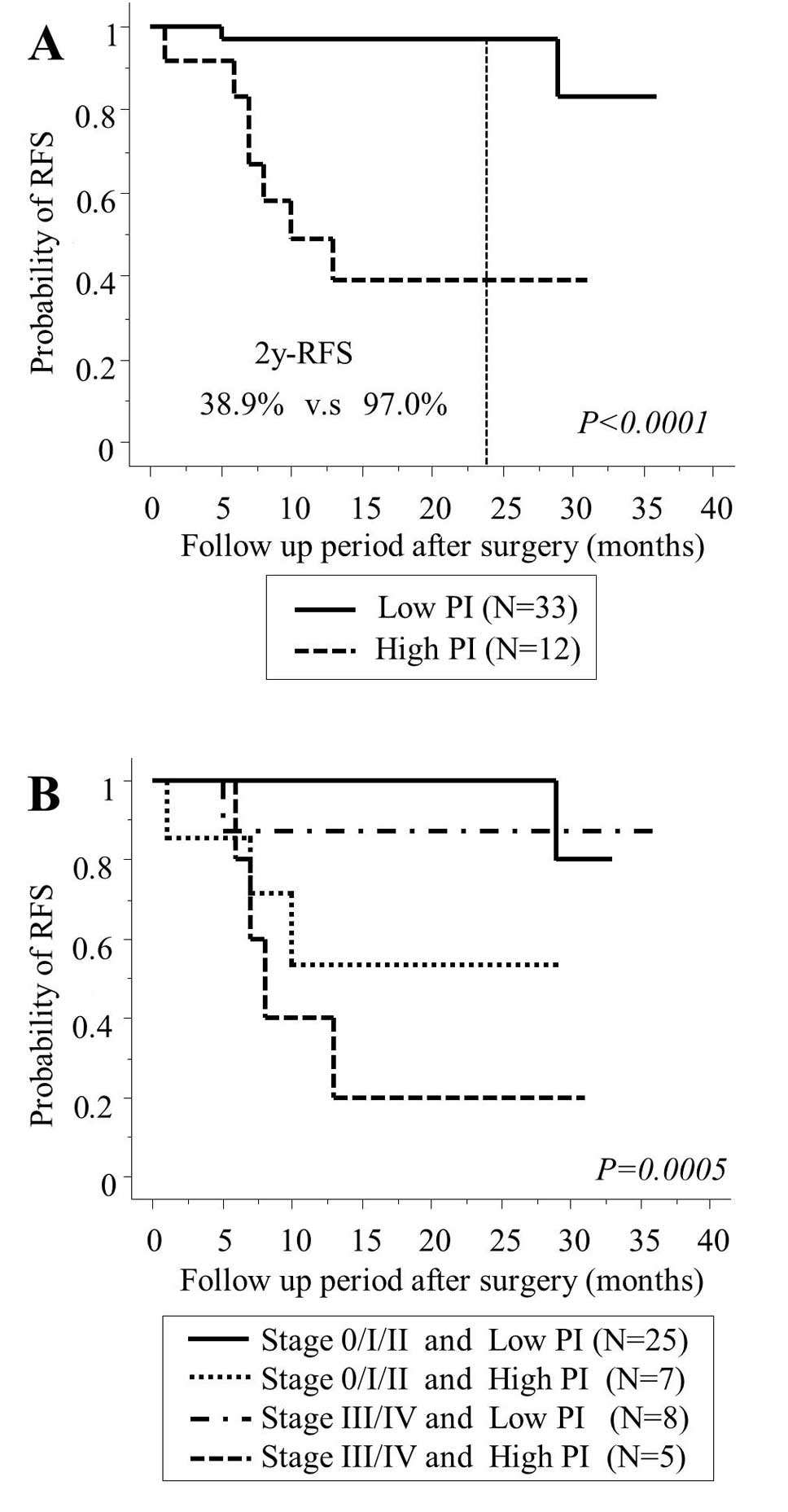
(Table III). An actuarial
analysis of the time to recurrence using the Kaplan-Meier method
showed that the recurrence rate was significantly higher in the
high PI group (>20) than in the low PI group (<20)
(P<0.0001, log-rank test) (Fig.
3A). The 2-year recurrence-free survival rate was 38.9% in the
high PI group and 97.0% in the low PI group. In order to prevent
the influence of a staging bias, a subgroup analysis was performed.
The patients with stage 0/I/II and stage III/IV disease exhibited a
similar tendency (P=0.0005, log-rank test) (Fig. 3B). A multivariate analysis using the
logistic regression model showed that a high PI on preoperative CTP
was an independent risk factor for recurrence (odds ratio, 19.1;
P=0.0369) (Table IV).
 | Table IIIBackground of the high-risk and
low-risk recurrence groups according to the preoperative PI
values. |
Table III
Background of the high-risk and
low-risk recurrence groups according to the preoperative PI
values.
| Variable | Categories | High PI (n=12) | Low PI (n=33) |
|---|
| Mean age
(years) | - | 69.3 | 66.4 |
| P (or yp)
stage | 0/I/II/III/IV | 0/3/4/4/1 | 1/17/7/8/0 |
| P (or yp) T | 0/1/2/3/4 | 0/3/2/7/0 | 1/18/5/9/0 |
| P (or yp) N | 0/1/2/3 | 6/2/1/3 | 21/8/4/0 |
| Preoperative
therapy, n (%) | - | 6 (50%) | 13 (39.4%) |
|
Complicationb
(Clavien-Dindo) | Non, I,
II/III-V | 10/2 | 26/7 |
| Grade | 0/1/2/3 | 0/5/1/0 | 2/7/3/1 |
| Recurrence rate, n
(%) | - | 7 (58.3%)a | 2 (6.1%)a |
 | Table IVUnivariate and multivariate analyses
of the prognostic parameters for time to recurrence after surgery
in the esophageal cancer patients. |
Table IV
Univariate and multivariate analyses
of the prognostic parameters for time to recurrence after surgery
in the esophageal cancer patients.
| | Univariate | Multivariate |
|---|
| |
|
|
|---|
| Variable | Categories | Odds ratio | 95% CI | P-value | Odds ratio | 95% CI | P-value |
|---|
| PI | ≥20 vs. <20 | 21.7 | 3.5–135.8 | 0.0010 | 19.1 | 1.2–303.7 | 0.0369 |
| P (or yp) T | 2/3/4 vs. 0/1 | 11.2 | 1.3–99.3 | 0.0300 | 14.2 | 0.323–621.7 | 0.1693 |
| P (or yp) N | + vs. − | 4 | 0.8–18.8 | 0.0795 | 1.0 | 0.023–48.2 | 0.9806 |
| P (or yp)
stage | III/IV vs.
0/I/II | 4.4 | 0.9–20.2 | 0.0589 | 2.5 | 0.066–91.5 | 0.6253 |
|
Differentiation | Poor vs.
mod/well | 4.5 | 0.9–22.7 | 0.0701 | 5.5 | 0.316–94.6 | 0.2431 |
| Location | Upper vs.
lower | 1.3 | 0.3–5.5 | 0.7612 | 2.8 | 0.236–33.4 | 0.4145 |
| Age (years) | ≥65 vs. <64 | 1.4 | 0.3–6.6 | 0.6491 | 0.381 | 0.013–11.0 | 0.5740 |
Discussion
In the present study, we demonstrated a correlation
between the preoperative hepatic blood flow and postoperative
recurrence. The postoperative recurrence rate was significantly
higher in the group with increased preoperative PI values. Similar
observations have been reported in previous studies in
gastrointestinal cancer (9,31–33).
Huguier et al (31) reported
that the preoperative hepatic perfusion scintigraphy in patients
with gastrointestinal cancer (including esophageal, gastric,
colorectal and pancreatic cancer) was useful for identifying
patients at low-risk for recurrence of liver metastasis and for
avoiding unnecessary adjuvant chemotherapy. In patients with
colorectal cancer, Warren et al (32) reported similar results in a
prospective assessment of a liver perfusion analysis using
scintigraphy. Furthermore, it has been reported that an increased
ratio of hepatic arterial blood flow to total liver blood flow
detected on color duplex Doppler ultrasonography is significantly
associated with a high incidence of postoperative liver metastasis
and a poorer prognosis regarding colorectal cancer (33). These reports, which demonstrate that
the hepatic blood flow is a useful marker for assessing the
biological malignancy of the tumor and predicting the outcome,
support our present observations. However, most of these reports on
hepatic blood flow focused on colorectal cancer, and there are few
reports on esophageal cancer. Considering the high early recurrence
rate of postoperative esophageal cancer (1,2), liver
perfusion analysis may offer an ideal biomarker that can provide an
optimal follow-up strategy for postoperative esophageal cancer
patients.
The underlying mechanisms of hepatic hemodynamic
changes have been discussed in previous reports (10–12,32,34–39).
Evidence obtained from a liver metastasis model in rats suggests
that a circulating vasoconstrictor is responsible for the increased
splanchnic vascular resistance and subsequent reduction in portal
venous flow (10,11,34).
This reduction in portal venous flow may lead to a relative
increase in the arterial flow in the liver (11,12,40,41).
This hypothesis is known as hepatic arterial buffer response
(HABR), noted under various experimental conditions such as
endotoxinemia (42) or experimental
portal vein ligation (43), in the
clinical setting after liver transplantation (44) and in patients with advanced
cirrhosis (45–48). HABR is an intrinsic regulatory
mechanism of the liver to maintain total hepatic blood flow when
portal perfusion decreases. According to this hypothesis, since
arterial blood is increased when the portal blood is decreased due
to the progression of the tumor, we considered that PI provided by
the ratio of these parameters may be an ideal marker with high
sensitivity. Its potential has been demonstrated by the present
study.
Our study is associated with a few limitations.
First, our findings are based on single center data, and the sample
size was small. Therefore, there may be a selection bias. Our
findings must be confirmed in multicenter investigations, and a
larger patient population should be studied. Second, a consensus
and standardization of data acquisition and analysis of methods
(including the optimal positioning of the ROI on the liver) have
yet to be established for CTP. Third, we did not perform any
pathological validation studies comparing CTP parameters with more
established markers of angiogenesis, such as microvessel density or
the level of vascular endothelial growth factor.
In conclusion, we showed that the preoperative
hepatic blood flow measured by CTP may be a valuable biomarker for
predicting the early recurrence of patients with esophageal
squamous cell carcinoma. To obtain more conclusive results, a
larger patient population should be studied. Nevertheless, our
results provide important insight into selecting the optimal
therapeutic strategy for the treatment of esophageal squamous cell
carcinoma.
References
|
1
|
Miyata H, Yamasaki M, Kurokawa Y, et al:
Survival factors in patients with recurrence after curative
resection of esophageal squamous cell carcinomas. Ann Surg Oncol.
18:3353–3361. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Toh Y, Oki E, Minami K and Okamura T:
Follow-up and recurrence after a curative esophagectomy for
patients with esophageal cancer: the first indicators for
recurrence and their prognostic values. Esophagus. 7:37–43. 2010.
View Article : Google Scholar
|
|
3
|
Kunisaki C, Makino H, Takagawa R, et al:
Surgical outcomes in esophageal cancer patients with tumor
recurrence after curative esophagectomy. J Gastrointest Surg.
12:802–810. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Nakagawa S, Kanda T, Kosugi S, Ohashi M,
Suzuki T and Hatakeyama K: Recurrence pattern of squamous cell
carcinoma of the thoracic esophagus after extended radical
esophagectomy with three-field lymphadenectomy. J Am Coll Surg.
198:205–211. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Shimada H, Kitabayashi H, Nabeya Y, et al:
Treatment response and prognosis of patients after recurrence of
esophageal cancer. Surgery. 133:24–31. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Worni M, Martin J, Gloor B, et al: Does
surgery improve outcomes for esophageal squamous cell carcinoma? An
analysis using the surveillance epidemiology and end results
registry from 1998 to 2008. J Am Coll Surg. 215:643–651. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Bosset JF, Gignoux M, Triboulet JP, et al:
Chemoradiotherapy followed by surgery compared with surgery alone
in squamous-cell cancer of the esophagus. N Engl J Med.
337:161–167. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Lee JL, Park SI, Kim SB, et al: A single
institutional phase III trial of preoperative chemotherapy with
hyperfractionation radiotherapy plus surgery versus surgery alone
for resectable esophageal squamous cell carcinoma. Ann Oncol.
15:947–954. 2004. View Article : Google Scholar
|
|
9
|
Leveson SH, Wiggins PA, Giles GR, Parkin A
and Robinson PJ: Deranged liver blood flow patterns in the
detection of liver metastases. Br J Surg. 72:128–130. 1985.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Leen E, Goldberg JA, Robertson J,
Sutherland GR and McArdle CS: The use of duplex sonography in the
detection of colorectal hepatic metastases. Br J Cancer.
63:323–325. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Carter R, Anderson JH, Cooke TG, Baxter JN
and Angerson WJ: Splanchnic blood flow changes in the presence of
hepatic tumour: evidence of a humoral mediator. Br J Cancer.
69:1025–1026. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Nott DM, Grime SJ, Yates J, et al: Changes
in the hepatic perfusion index during the development of
experimental hepatic tumours. Br J Surg. 76:259–263. 1989.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Cuenod C, Leconte I, Siauve N, et al:
Early changes in liver perfusion caused by occult metastases in
rats: detection with quantitative CT. Radiology. 218:556–561. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Leggett DA, Kelley BB, Bunce IH and Miles
KA: Colorectal cancer: diagnostic potential of CT measurements of
hepatic perfusion and implications for contrast enhancement
protocols. Radiology. 205:716–720. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Miles KA, Hayball M and Dixon AK: Colour
perfusion imaging: a new application of computed tomography.
Lancet. 337:643–645. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ronot M, Asselah T, Paradis V, et al:
Liver fibrosis in chronic hepatitis C virus infection:
differentiating minimal from intermediate fibrosis with perfusion
CT. Radiology. 256:135–142. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Hashimoto K, Murakami T, Dono K, et al:
Assessment of the severity of liver disease and fibrotic change:
The usefulness of hepatic CT perfusion imaging. Oncol Rep.
16:677–683. 2006.PubMed/NCBI
|
|
18
|
Pandharipande PV, Krinsky GA, Rusinek H
and Lee VS: Perfusion imaging of the liver: current challenges and
future goals. Radiology. 234:661–673. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Van Beers BE, Leconte I, Materne R, Smith
AM, Jamart J and Horsmans Y: Hepatic perfusion parameters in
chronic liver disease: dynamic CT measurement correlated with
disease severity. AJR Am J Roentgenol. 176:667–673. 2001.PubMed/NCBI
|
|
20
|
Tsushima Y, Funabasama S, Aoki J, Sanada S
and Endo K: Quantitative perfusion map of malignant liver tumors,
created from dynamic computed tomography data. Acad Radiol.
11:215–223. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Sahani DV, Holalhere NS, Mueller PR and
Zhu AX: Advanced hepatocellular carcinoma: CT perfusion of liver
and tumor tissue - initial experience. Radiology. 243:736–743.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Satoh A, Shuto K, Okazumi S, et al: Role
of perfusion CT in assessing tumor blood flow and malignancy level
of gastric cancer. Dig Surg. 27:253–260. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Miles KA, Leggett DA, Kelley BB, Hayball
MP, Sinnatamby R and Bunce I: In vivo assessment of
neovascularization of liver metastases using perfusion CT. Br J
Radiol. 71:276–281. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Morsbach F, Pfammatter T, Reiner CS, et
al: Computed tomographic perfusion imaging for the prediction of
response and survival to transarterial radioembolization of liver
metastases. Invest Radiol. 48:787–794. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Hayano K, Okazumi S, Shuto K, et al:
Perfusion CT can predict the response to chemoradiation therapy and
survival in esophageal squamous cell carcinoma: Initial clinical
results. Oncol Rep. 18:901–908. 2007.PubMed/NCBI
|
|
26
|
Hayano K, Shuto K, Koda K, Yanagawa N,
Okazumi S and Matsubara H: Quantitative measurement of blood flow
using perfusion CT for assessing clinicopathologic features and
prognosis in patients with rectal cancer. Dis Colon Rectum.
52:1624–1629. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Ando N, Kato H, Igaki H, et al: A
randomized trial comparing postoperative adjuvant chemotherapy with
cisplatin and 5-fluorouracil versus preoperative chemotherapy for
localized advanced squamous cell carcinoma of the thoracic
esophagus (JCOG9907). Ann Surg Oncol. 19:68–74. 2012. View Article : Google Scholar
|
|
28
|
Miles KA, Hayball M and Dixon AK:
Functional images of hepatic perfusion obtained with dynamic CT.
Radiology. 188:405–411. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Wang X, Xue HD, Jin ZY, et al:
Quantitative hepatic CT perfusion measurement: comparison of
Couinaud’s hepatic segments with dual-source 128-slice CT. Eur J
Radiol. 82:220–226. 2013.
|
|
30
|
Ng CS, Chandler AG, Wei W, et al:
Reproducibility of CT perfusion parameters in liver tumors and
normal liver. Radiology. 260:762–770. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Huguier M, Maheswari S, Toussaint P, Houry
S, Mauban S and Mensch B: Hepatic flow scintigraphy in evaluation
of hepatic metastases in patients with gastrointestinal malignancy.
Arch Surg. 128:1057–1059. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Warren HW, Gallagher H, Hemingway DM, et
al: Prospective assessment of the hepatic perfusion index in
patients with colorectal cancer. Br J Surg. 85:1708–1712. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Leen E, Goldberg JA, Angerson WJ and
McArdle CS: Potential role of doppler perfusion index in selection
of patients with colorectal cancer for adjuvant chemocherapy.
Lancet. 355:34–37. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Hemingway DM, Cooke TG, Grime SJ, Nott DM
and Lenkins SA: Changes in hepatic haemodynamics and hepatic
perfusion index during the growth and development of hypovascular
HSN sarcoma in rats. Br J Surg. 78:326–330. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Hunt TM, Flowerdew AD, Britten AJ, et al:
An association between parameters of liver blood flow and
percentage hepatic replacement with tumour. Br J Cancer.
59:410–414. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Taylor I, Bennett R and Sherriff S: The
blood supply of colorectal liver metastases. Br J Cancer.
38:749–756. 1978. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Leen E, Goldberg JA, Robertson J, et al:
Detection of hepatic metastases using duplex/color Doppler
sonography. Ann Surg. 214:599–604. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Leen E, Goldberg JA, Anderson JR, et al:
Hepatic perfusion changes in patients with liver metastases:
comparison with those patients with cirrhosis. Gut. 34:554–557.
1993. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Leen E, Goldberg JA, Robertson J, et al:
Early detection of occult colorectal hepatic metastases using
duplex colour Doppler sonography. Br J Surg. 80:1249–1251. 1993.
View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Ternberg JL and Butcher HR Jr: Blood-flow
relation between hepatic artery and portal vein. Science.
150:1030–1031. 1965. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Mathie RT, Lam PH, Harper AM and Blumgart
LH: The hepatic arterial blood flow response to portal vein
occlusion in the dog: the effect of hepatic denervation. Pflugers
Arch. 386:77–83. 1980. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Ayuse T, Brienza N, Revelly JP, O’Donnell
CP, Boitnott JK and Robotham JL: Alternations in liver hemodynamics
in an intact porcine model of endotoxin shock. Am J Physiol.
268:H1106–H1114. 1995.PubMed/NCBI
|
|
43
|
Rocheleau B, Ethier C, Houle R, Huet PM
and Bilodeau M: Hepatic artery buffer response following left
portal vein ligation: its role in liver tissue homeostasis. Am J
Physiol. 277:G1000–G1007. 1999.PubMed/NCBI
|
|
44
|
Henderson JM, Gilmore GT, Mackay GJ,
Galloway JR, Dodson TF and Kutner MH: Hemodynamics during liver
transplantation: the interactions between cardiac output and portal
venous and hepatic arterial flows. Hepatology. 16:715–718. 1992.
View Article : Google Scholar
|
|
45
|
Gülberg V, Haag K, Rössle M and Gerbes AL:
Hepatic arterial buffer response in patients with advanced
cirrhosis. Hepatology. 35:630–634. 2002.PubMed/NCBI
|
|
46
|
Gülberg V and Schoenberg SO: Hepatic
arterial buffer response: visualization by multiphasic
high-resolution 3D magnetic resonance angiography. J Hepatol.
40:1812004.PubMed/NCBI
|
|
47
|
Mücke I, Richter S, Menger MD and Vollmar
B: Significance of hepatic arterial responsiveness for adequate
tissue oxygenation upon portal vein occlusion in cirrhotic livers.
Int J Colorectal Dis. 15:335–341. 2000.PubMed/NCBI
|
|
48
|
Richter S, Mücke I, Menger MD and Vollmar
B: Impact of intrinsic blood flow regulation in cirrhosis:
maintenance of hepatic arterial buffer response. Am J Physiol
Gastrointest Liver Physiol. 279:G454–G462. 2000.PubMed/NCBI
|