Introduction
Mammary tumors are the most common neoplastic
process in female dogs, representing ~52% of neoplasms, of which
41–53% are histologically diagnosed as malignant, with distant
metastasis being the most common cause of death in female dogs
(1–6). Canine mammary tumors (CMTs) are
similar to human breast cancers (5,7), thus
they are a suitable animal model for the study of mammary
carcinogenesis in the two species (2,8).
Prognosis is directly associated with factors such
as tumor size, lymph-node involvement, presence of distant
metastasis, histological type, histologic grade and intravascular
growth (9). Therapy based on
prognostic assessment enables the application of different
therapeutic modalities used in cancer treatment with the intensity
and effectiveness appropriate for each patient, increasing survival
(10,11).
Angiogenesis is a process in which new blood vessels
are formed from pre-existing vasculature (12), which is necessary to supply
nutrients and maintain homeostasis in the tissues of the body
(13). This process has been shown
to be a necessary process for oncogenesis as well, in addition to
subsequent tumor growth and dissemination through metastases
(14).
Angiogenesis is regulated by a number of pro- and
antiangiogenic factors, such as vascular endothelial growth factor
(VEGF) and hypoxia-inducible factor (HIF) (15,16).
These factors, which are released by tumor cells promote
activation, proliferation and migration of endothelial cells to
tumor tissue, allowing for the rapid formation of functional
neovasculature (17).
HIF transcription factors mediate the primary
transcriptional response to hypoxic conditions in normal and
neoplastic cells. HIFs form heterodimeric complexes composed of the
α and a stable β subunit. Together these subunits bind hypoxia
response elements (HREs) to hundreds of genes that facilitate the
adaptation to hypoxia, specifically promoter elements present in
the promoter region of VEGF (18,19).
HIF-1α is an oxygen-liable subunit, that in normal
oxygen conditions is maintained at a low level (20,21) as
it is recognized by the Hippel-Lindau tumor suppressor (pVHL) and
degraded by the proteasome (22–24).
Under hypoxic conditions, pVHL binds to nitric oxide (NO) and the
HIF-1α is not recognized, allowing the migration of HIF-1α from the
cytoplasm to the nucleus, therebey inducing the expression of VEGF
(15,16,25–28).
VEGF and its receptors are confirmed signaling
pathways in angiogenesis (29).
VEGF stimulates endothelial cell proliferation, migration and
capillary tube formation (28,30–31).
Tumor growth through angiogenesis is directly correlated with VEGF
expression in breast cancer (15,16,32–34).
It was reported that VEGF expression in canine and feline mammary
carcinomas is associated with a more aggressive behavior and a poor
diagnosis/prognosis (35–37).
The aims of this study were to determine the serum
levels and gene expression of VEGF and HIF-1α in female dogs with
malignant mammary neoplasia, and to verify their correlation with
clinicopathological parameters and clinical evolution, aiming to
determine its prognostic value.
Materials and methods
Ethical considerations
This study was approved by the Ethics Committee of
Sao Jose do Rio Preto Medical School (protocol no. 5230/2010).
Sample characterization
Peripheral blood samples and tumor fragments from 24
female dogs with malignant mammary neoplasia (study group) and 26
female non-affected dogs (control group) were collected at the
veterinary clinics in São José do Rio Preto, SP, Brazil and the
surrounding region between 2011 and 2012. Exclusion criteria for
the control group were rigorously followed and included females
with no tumor history and no detectable disease
inflammation/infections in the period prior to the sampling.
Female dogs from the study group were evaluated by
the veterinary with respect to physical (age and breed),
pathological (time-course, the interval between tumor diagnosis and
surgical removal, tumor localization, lymph-node involvement, tumor
mass size, clinical staging, ulceration and vascularization) and
clinical (metastasis, local recurrence and death)
characteristics.
Following the tumor excision and blood collection,
the animals of study group were followed for 12 months. During this
period the presence of local tumor recurrence, metastasis
(confirmed by X-ray) and death were described by the veterinary,
allowing the determination of survival time and disease-free
survival time (the time from excision until the detection of
metastasis and/or recurrence).
The tumor fragments collected at excision were
divided into two sections: The first one was fixed in buffered 10%
formaldehyde for 24 h and paraffin-embedded. Histological sections
(3 μm) were obtained and stained with hematoxylin and eosin
(H&E) by standard histological procedures for histopathology.
The second section was immersed in RNA stabilizing solution,
RNAlater (Invitrogen Life Technologies, Eugene, OR, USA) for qPCR
analysis.
The parameters employed for the histological
classification were performed according to the Canine Mammary
Neoplasms Histological Classification, modified from Misdorp et
al (38,39) and the clinical staging system (TNM)
of canine mammary carcinomas established by Owen (40).
Most of the malignant tumors consisted of simple
carcinoma, such as tubulopapillary carcinoma type (16/24) (67%).
The age range of the animals was 7–14 years (mean, 10 years) and
25% of animals were of indeterminate breed. Among the
clinicopathological characteristics, there was a predominance of
time course >6 months (11/24) (46%), tumors with multiple
location (14/24) (58%), lymph-node involvement N0 (17/24) (71%),
tumor mass size <3 cm (12/24) (50%), clinical staging I (10/24)
(42%), tumors without ulceration (20/24) (83%) and moderate
vascularization (16/24) (67%). The local recurrence rate was 17%,
metastasis 25% and death 33%. The patient characteristics are shown
in Table I.
 | Table IMean serum concentration of VEGF and
serum percentage of HIF-1α and its correlation with
clinicopathological parameters. |
Table I
Mean serum concentration of VEGF and
serum percentage of HIF-1α and its correlation with
clinicopathological parameters.
| Clinicopathological
parameters | Number of dogs | VEGF (pg/ml) | HIF-1α (% of
control) |
|---|
| Clinical
feature |
| Control | 24 | 51.77±4.875 | 100.0±5.442 |
| Samples | 26 | 136.4±48.79 | 78.51±3.146 |
| P-value | | 0.03a | 0.001a |
| Age |
| <10 anos | 11 (46%) | 79.95±35.46 | 84.83±5.193 |
| ≥10 anos | 13 (54%) | 161.3±78.59 | 73.16±3.290 |
| p-value | | 0.37 | 0.06 |
| Tumor location |
| Multiple | 14 (58%) | 146.2±71.87 | 77.89±4.850 |
| Single | 10 (42%) | 96.63±52.86 | 79.38±3.606 |
| P-value | | 0.59 | 0.82 |
| Time course |
| 1 month | 4 (17%) | 22.27±12.51 | 75.93±4.763 |
| Up to 6
months | 9 (37%) | 144.5±64.98 | 78.53±3.796 |
| More than 6
months | 11 (46%) | 138.7±84.96 | 79.43±6.119 |
| P-valueb | | p>0.05 | p>0.05 |
| Tumor mass
size |
| T1 | 12 (50%) | 155.3±79.83 | 78.63±3.607 |
| T2 | 4 (17%) | 132.8±108.6 | 89.10±14.11 |
| T3 | 8 (33%) | 63.40±6.664 | 71.63±2.902 |
| P-valueb | | p>0.05 | p>0.05 |
| Lymph node
involvement |
| N0 | 17 (71%) | 33.13±6.188 | 77.30±2.646 |
| N1/N2 | 7 (29%) | 176.7±68.16 | 80.93±8.144 |
| P-value | | 0.01a | 0.59 |
| Metastasis |
| M0 | 18 (75%) | 45.64±9.238 | 75.79±2.545 |
| M1/M2 | 6 (25%) | 201.6±96.53 | 94.47±12.73 |
| P-value | | 0.01a | 0.02a |
| Clinical
staging |
| I/II | 12 (50%) | 85.51±59.44 | 78.79±3.487 |
| III/IV | 12 (50%) | 104.7±45.72 | 77.30±5.352 |
| P-value | | 0.80 | 0.81 |
| Ulceration |
| Yes | 4 (17%) | 225.6±168.9 | 73.35±4.272 |
| No | 20 (83%) | 95.32±36.62 | 79.54±3.670 |
| P-value | | 0.24 | 0.47 |
|
Vascularization |
| Abundant | 8 (33%) | 247.7±121.4 | 77.38±7.972 |
| Moderate | 16 (67%) | 41.35±9.111 | 79.07±2.807 |
| P-value | | 0.02a | 0.80 |
| Recurrence |
| Yes | 4 (17%) | 41.70±8.763 | 98.88±16.26 |
| No | 20 (83%) | 137.9±52.20 | 75.90±2.524 |
| P-value | | 0.44 | 0.01a |
| Censorship |
| Death | 8 (33%) | 238.1±92.95 | 79.72±8.220 |
| Alive | 16 (67%) | 38.81±9.467 | 77.90±2.633 |
| P-value | | 0.02a | 0.79 |
Enzyme-linked immunosorbent assay
(ELISA)
For the enzyme-linked immunosorbent assay, the blood
(3 ml) was collected in a CORVAC serum separator tube (Labor
import, São Paulo, SP, Brazil) containing clot activation additive
and barrier gel, stored at 4°C, processed by centrifugation (1,000
× g, 25 min) and passed through a 13-mm serum filter to remove
potentially contaminating cells. The serum was immediately
cryopreserved at −80°C (7).
Quantification of serum VEGF
VEGF content was determined by using a Quantikine
Canine VEGF Immunoassay kit (R&D Systems, Minneapolis, MN,
USA). A specific monoclonal antibody anti-canine VEGF was
pre-coated onto a 96-well polystyrene microplate, and 100 μl
of buffered protein solution, standards and samples were pipetted
into the wells. After incubation for 2 h, the microplate was washed
three times with 300 μl/well. The reaction also included
incubations at room temperature with 200 μl/well of
enzyme-linked polyclonal antibody against VEGF conjugated to
horseradish peroxidase for 2 h followed by another wash and 200
μl/well of substrate solution (H2O2
and tetramethylbenzidine) for 25 min. Then, 50 μl of stop
solution (2 N sulfuric acid) was added to each well and the optical
density (OD) was measured at 450 nm in a microplate reader (Thermo
Fisher Scientific, Waltham, MA, USA). The reaction intensity was
proportional to the concentration of VEGF. The calculation of OD
was determined through the adjustment curve four parameter logistic
(4-PL), using the software SkanIt for Multiskan FC 2.5.1 (Thermo
Fisher Scientific).
Quantification of serum HIF-1α
HIF-1α content was determined by using a HIF-1α
Transcription Factor Assay kit (Abnova, Taipei, Taiwan). First, 90
μl/well of complete transcription factor binding assay
buffer (CTFB) (composited by UltraPure Water, 4X transcription
factor binding assay buffer concentrate, transcription factor
reagent A and 300 mM dithiothreitol, DTT), and 10 μl of
transcription factor HIF-1α-positive control were mixed with
samples in the appropriate wells. After overnight incubation at
4°C, the microplate was washed five times with 200 μl/well.
The antibodies employed were transcription factor HIF-1α primary
antibody 1:100 in 1X antibody binding buffer (ABB) and
transcription factor goat anti-rabbit HRP-conjugated secondary
antibody 1:100 in 1X ABB. The reaction also included subsequent
incubations at room temperature with 100 μl/well of
transcription factor developing solution (chromogenic substratum)
for 15–45 min. OD was measured at 450 nm in a microplate reader
(Thermo Fisher Scientific). The reaction intensity was proportional
to the concentration of HIF-1α. The mean HIF-1α serum absorbance of
the control group was established as 100%, the serum percentage of
HIF-1α in the study group being calculated in relation to the
control group.
Quantitative PCR (qPCR)
Sample processing
Tumor samples were collected in a falcon tube of 15
ml containing RNA-stabilizing solution, RNAlater (Invitrogen Life
Technologies), stored at room temperature for 24 h, manually
processed using a razor into 100 mg/section, immersed in TRIzol
reagent (Invitrogen Life Technologies) and macerated for total RNA
extraction, according to the manufacturer’s instructions. The RNA
concentration of each sample was determined with a NanoDrop 2000
(Thermo Fisher Scientific), and RNA integrity was confirmed on a 1%
agarose gel. The RNA from each sample was reverse-transcribed to
complementary DNA (cDNA) using a High Capacity cDNA kit (Applied
Biosystems, Foster City, CA, USA).
Gene expression of VEGF and
HIF-1α
The standard curve was calculated, and analyses for
the differential expression of HIF1A or VEGFA and endogenous
control genes RPS19 and RPL8 were performed in
triplicate using StepOnePlus System (Applied Biosystems) and TaqMan
Universal Master mix (Applied Biosystems), as recommended by the
manufacturer. Each transcript level was normalized by division with
the expression values of RPS19 and RPL8 used as an
endogenous control. The assays used were HIF-1α (Cf02741632_m1),
VEGFA (Cf02623449_m1) and RPL8 (Cf02663820_m1) and the RPS19 primer
sequences used for amplification were: sense (5′-GCC TTC CTC AAA
AAG TCT GGG -3′), antisense (5′-GCT TGC TCC CTA CGA TGA GAA C-3′)
and probe (5′-CCC TGA ATG GGT GGA C-3′) (Applied Biosystems).
Each reaction consisted of 10 μl of Master
Mix, 1 μl of TaqMan, 8 μl of DEPC water and 1
μl of cDNA (100 ng/ml). The amplification scheme appointed
was: 50°C for 2 min, 95°C for 10 min, followed by 40 cycles of 95°C
for 15 sec and 60°C for 1 min. The expression of each gene of
interest was calculated by the quantification method related to the
average of the normalizing genes used as endogenous controls (ΔΔCt)
(41).
Statistical analysis
Statistical analysis was performed using GraphPad
Prism4 (San Diego, CA, USA) and Stats Direct (London, UK) software.
The results were previously submitted to descriptive analyses for
the determination of normality and were considered to have a normal
distribution. The different clinicopathological characteristics
were separated in groups and compared by the Student’s t-test or
ANOVA, followed by the Bonferroni test. The values were presented
as mean ± standard deviation (SD).
The survival curve was constructed following the
Kaplan-Meyer method. The cut-off points for the VEGF and HIF-1α
levels were established by the receiver operating characteristic
(ROC) curve. For the ROC curve, the percentage of VEGF and HIF-1α
of female dogs who died was compared with that of dogs that
survived until the end of the follow-up period. Survival curves
were plotted by the Kaplan-Meier method and the differences between
the curves were assessed using a log-rank test and hazard
function.
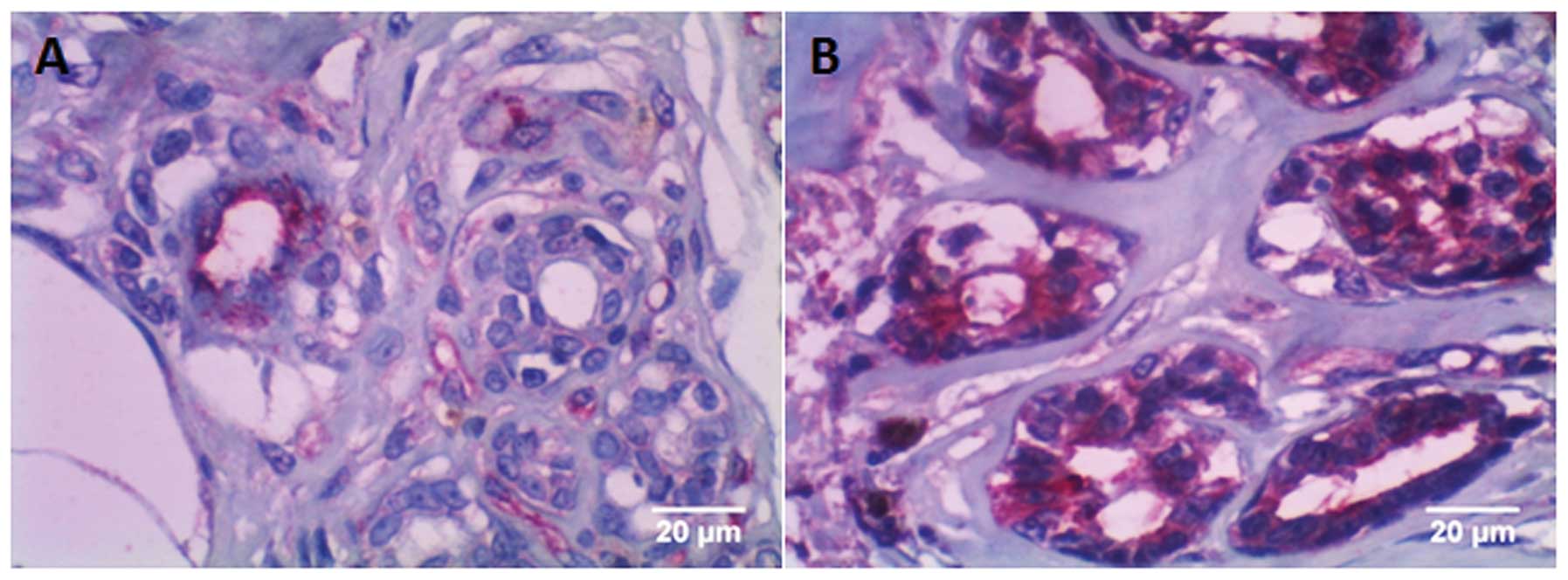
Analysis of tumor vascularization by
double staining immunohistochemistry
Tumor vascularization was analyzed by the
veterinarian at the moment of surgery, based on macroscopic
visualization of the vessels involved in the tumor and it was
subsequently confirmed by the pathologist during the
histopathological examination. According to this observation, the
samples were classified as moderate and abundant vascularization.
To confirm this analysis, we performed a double staining
immunohistochemical technique from the analysis of the presence of
CD34, a transmembrane glycoprotein whose expression is associated
with hematopoietic precursors and capillary endothelial cells, and
intermediate-purity plasma-derived Factor VIII. Images were
captured using Nikon eclipse E200 (Nikon Instrument Group,
Melville, NY, USA).
Tissue microarray technique (TMA)
The double-labeling immunohistochemical technique
was performed according to Maschio et al (42). The tumor fragments were fixed in
formalin and embedded in paraffin and assembled as a tissue
microarray (TMA). TMA consisted of representative areas of the
tumors removed from the donor block and added to the receiver block
in duplicate representing different regions of the tumor, via the
manual tissue arrayer 1 (Beecher Instruments Micro-array
Technology, Silver Spring, MD, USA). Sections (3 μm) from
blocks of TMAs were deposited on electrostatically charged slides
(StarFrost Waldemar Knittel GmbH, Brunswick, Germany). A map
containing the location of each fragment in TMAs was constructed
using Microsoft Excel (Microsoft Co., Redmond, WA, USA).
The double-labeled reactions were performed in
automated immunostaining equipment (Ventana Bench Mark XT, Roche
Diagnostics, Mannheim, Germany), using anti-CD34 and anti-Factor
VIII antibodies (Table II). The
display systems used in the reactions of double-labeled Factor-VIII
and CD34 were Enhanced Alkaline Phosphatase Red Detection and iVIEW
DAB Detection, respectively.
 | Table IIInformation about antibodies used for
double staining immunohistochemistry. |
Table II
Information about antibodies used for
double staining immunohistochemistry.
| Antibody | Specificity | Clone | Dilution | Company | Positive
controls |
|---|
| CD34 | Monoclonal
(mouse) | QBEnd 10 | 0:500 | Dako | Breast normal
tissue |
| Factor VIII | Polyclonal
(rabbbit) | – | 0:200 | Dako | Tonsil tissue |
Deparaffinization was initiated by applying EZPrep
reagent (Roche Diagnostics) and heating at 75°C for 8 min. For
antigen retrieval, cell conditioner (Roche Diagnostics) was applied
for 8 min at 95°C and then 64 min at 100°C. The slides were washed
with reaction buffer (Roche Diagnostics) and incubated for 4 min in
this solution. Then, UV inhibitor (Roche Diagnostics) was applied
for 4 min and the slides were washed with reaction buffer. The
anti-CD34 primary antibody was incubated for 1 h and the slides
were washed with reaction buffer. UV UNIV MULT HRP (Roche
Diagnostics), UV DAB (Roche Diagnostics) and
H2O2 UV DAB reagents (Roche Diagnostics) were
then applied for 8 min each, respectively. Copper UV reagent (Roche
Diagnostics) was applied and the slides were heated to 90°C for 4
min and 37°C for an additional 4 min. Then, 100 ml of the primary
antibody anti-Fator VIII was applied and incubated for 1 h. The UV
Red UNIV MULT (Roche Diagnostics) was incubated for 12 min.
Subsequently, UV Red Enhancer (Roche Diagnostics) was applied for 4
min. Reagents UV Fast Red A (Roche Diagnostics), Naphthol Red UV
(Roche Diagnostics) and UV Fast Red B (Roche Diagnostics) were
applied for 8 min each. After this procedure, the slides were
washed with reaction buffer and incubated with Hematoxylin II
reagent (Roche Diagnostics) for 8 min. The slides were washed with
reaction buffer and incubated with bluing reagent (Roche
Diagnostics) for 4 min and again washed with reaction buffer.
The staining of Factor-VIII antibody was observed in
the cytoplasm as red, and CD34 antibody in the cytoplasmic membrane
as brown (Fig. 1).
Results
Correlation between clinicopathological
parameters and serum levels
The mean serum concentration of VEGF at the surgical
excision moment in female dogs with mammary tumors was
significantly higher than in the control group (136.4 pg/ml vs.
51.77 pg/ml; p=0.03; Table I). By
contrast, the serum percentage of HIF-1α was significantly higher
in the control group (100.0 vs. 78.51%; p=0.001; Table I).
The univariate analysis showed that the VEGF serum
concentration was significantly higher in dogs with highly
vascularized tumors (p=0.02; Table
I), female dogs with lymph node involvement (p=0.01; Table I), metastasis (p=0.01; Table I) and in those that died within the
follow-up period (p=0.02; Table I).
Furthermore, the HIF-1α levels were significantly higher in female
dogs with metastasis (p=0.02; Table
I) and tumor recurrence history (p=0.01; Table I).
As far as the survival curve is concerned, the
samples were divided according to the last VEGF and HIF-1α serum
values measured prior to death, with a cut-off value of 75,483
pg/ml [sensitivity (95% CI) = 75%, specificity (95% CI) = 94%] for
VEGF and a cut-off value of 87,179 percentage of control
[sensitivity (95% CI) = 38%, specificity (95% CI) = 81%] for
HIF-1α. This procedure demonstrated a negative correlation between
VEGF concentration and survival time (OR, 9.169; CI 95% =
5.266–201.8; p=0.0002). No correlation was observed between HIF-1α
serum percentage and survival time (OR, 1.471; CI 95% =
0.3417–7.320; p=0.34) (data not shown).
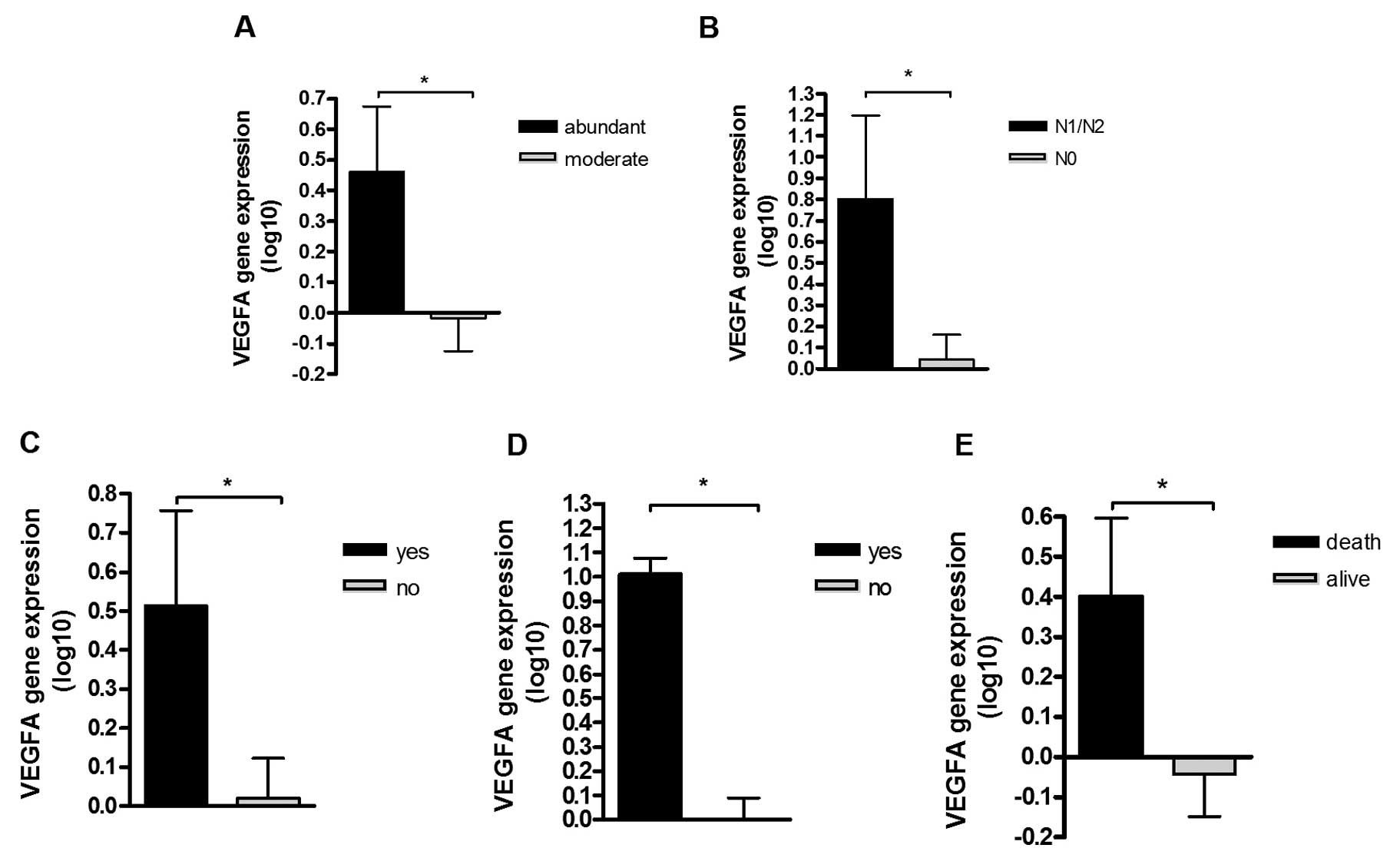
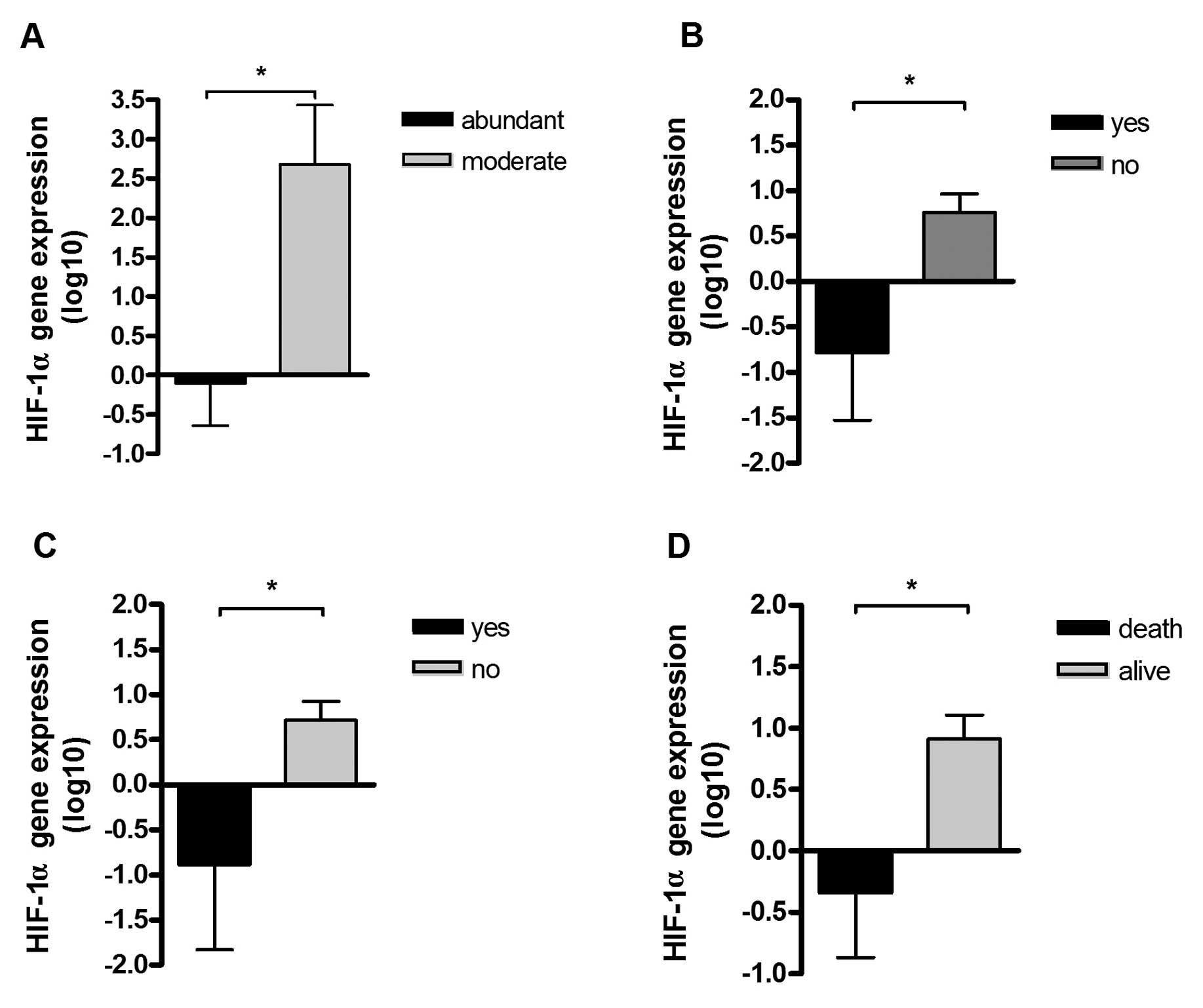
Correlation between clinicopathological
parameters and gene expression
To examine the effect of gene expression of VEGF and
HIF-1α to the spread of the disease we analyzed the correlation
between the gene expression and clinical evolution. The qPCR
analysis revealed that VEGF was significantly overexpressed in
female dogs with highly vascularized tumors (p=0.03; Fig. 2A), lymph-node involvement (p=0.02;
Fig. 2B), metastasis (p=0.04;
Fig. 2C), tumor recurrence
(p=0.0002; Fig. 2D) and death
(p=0.04; Fig. 2E). The HIF-1α was
significantly overexpressed in tumors with moderate vascularization
(p=0.02; Fig. 3A), without
metastasis (p=0.01; Fig. 3B),
without recurrence (p=0.02; Fig.
3C) and female dogs that were still alive when the study was
terminated (p=0.01; Fig. 3D).
Discussion
In this study, we have demonstrated the prognostic
value of VEGF and HIF-1α on female dogs with malignant mammary
tumors and found a correlation between an increase of VEGF serum
levels and clinicopathological parameters of worse prognosis, which
decreased the survival rate in female dogs with malignant mammary
tumors compared to the control group. Additionally, there was a
significant increase of VEGF serum concentration in female dogs
with malignant mammary tumors compared to the control group.
Serum tumor markers play an important role in the
early diagnostic, prognostic determination, specific therapeutic
response prediction, precocious detection of tumor recurrence after
surgery, and follow-up in advanced disease therapy (43,44).
In this context, the VEGF is considered an important indicator of
the development of cancer, and its serum levels can be used to
estimate tumor progression (45).
In accordance with our results, some studies in
humans have shown that serum VEGF levels were higher in patients
with breast cancer when compared to healthy subjects and inversely
correlated with survival (46,47).
On the other hand, Duranyildiz et al (48) and El Tarhouny et al (49) did not observe any significant
difference between serum VEGF levels in patients with breast cancer
and the control group.
VEGF signaling contribute to the biology and
clinical behavior of canine mammary carcinomas (4). By considering canine mammary tumors,
Kato et al (30) found
higher serum VEGF levels in female dogs with malignant tumors
compared to female dogs with benign tumors, as well as in female
dogs that had lung metastasis after tumor excision. Marked VEGF
mitogenic properties led to an increase in the permeability of
blood vessels, allowing cancer cells to pass through to
extravascular spaces and form distant metastases (50). Significantly higher serum VEGF
concentrations in metastatic and invasive tumor patients with
breast cancer when compared to patients with non-metastatic and
non-invasive tumors have been previously reported (51,52).
The hypoxic environment, which induces gene
expression changes and biological features leading to poor
outcomes, is important in the modulation of tumor angiogenesis
(53,54). In this regard, it has been shown
that HIF-1 is a leading regulator of tumor angiogenesis following
hypoxia, which has been demonstrated to be significantly associated
with the morbidity and mortality of breast cancer (55,56).
However, to the best of our knowledge, there have been no studies
investigating the quantification of HIF-1α in the serum of female
dogs bearing malignant mammary neoplasias in the literature. In
humans, there was a study that compared the serum levels of HIF-1α
in diabetic patients with breast cancer and control groups,
demonstrating the HIF-1α levels were markedly higher in the patient
group than in the controls (55).
Other authors found higher serum HIF-1α levels in patients with
lung cancer (57), as well as
patients with liver cancer (46).
As expected, the VEGFA gene was overexpressed
in female dogs with worse prognosis, however, HIF-1α was
overexpressed in female dogs with better prognosis. Recent advances
in cancer research have indicated that in hypoxia conditions, the
hypoxia-inducible factors, such as HIF-1α, may activate the
transcription of several genes that play key roles in many critical
aspects of cancer biology, particularly VEGF (15,16,25–28).
However, in our study, the gene expression of HIF-1α did not
follow the same pattern as the VEGFA gene expression, and
this can be explained by the fact that HIF-1α acts
synergistically with numerous factors and oncogenes that regulate
the expression of VEGF (56,58)
suggesting other, as yet unidentified factors that promote
VEGF gene transcription by binding to hypoxia response
elements (HREs) (59).
In agreement with our results, findings of previous
studies associated the increase of VEGF expression with
neoplastic cell aggression, disease dissemination and tumor mass
development, reducing survival rate of patients with breast cancer
(9,33,34,60,61).
In dogs, the expression of VEGFA was previously studied by
qPCR and it was associated with tumor aggression (37). Kallergi et al (25) analyzed VEGF expression in metastatic
and non-metastatic mammary cell lines and found an increase of VEGF
expression in the more aggressive cells, especially metastatic
ones.
An increased expression of HIF-1A in various
carcinomas has been associated with aggressive behavior, enhanced
rates of distant metastases, decreased survival rates and increased
resistance to the treatment of breast cancer in patients, as
opposed to our results (62).
Results showing a correlation of the role of HIF-1α in cancer
progression in the literature are controversial, as it is known
that HIF-1α expression is increased with tumor growth because
larger tumors are generally more hypoxic than smaller ones
(63). However, depending on the
severity of hypoxic stimulus, HIF-1α serves as a pro-death gene
capable of promoting apoptosis and cell death (43). Under conditions of severe hypoxia
cells seem to survive, initiating a cascade of events leading to
apoptosis and cell death, thus leading to a reduction in tumor
progression (42).
Despite the fact that our investigations have not
confirmed the correlation between HIF-1α and clinicopathological
characteristics, our results showed that VEGF is correlated with
characteristics of poor prognosis. Therefore, in view of our own
observations and conflicting opinions reported in other studies, it
seems that only VEGF can be employed as a potential prognostic
marker for routine use in the clinic, as it is useful in predicting
disease progression and tumor recurrence in female dogs with
malignant mammary tumors.
Acknowledgments
This study was supported by a grant from
FAPESP/Fundação de Amparo à Pesquisa do Estado de São Paulo
(process no., 2009/14883-6) and a Master’s Studentship (process
no., 2010/13977-4). We would like to thank the Veterinary
Clinicians in São José do Rio Preto, SP, Brazil and the surrounding
region, and the owners of the dogs who contributed to this study.
We extend thanks to Professor Cicero Meneghetti and Professor
Geovanni Dantas Cassali for support in reading and analyzing the
slides, and Ms. Juliano Jampietro and Dr Fernando Augusto Soares
from AC Camago Cancer Center, SP, Brazil for assisting in the
development of the double-labeling immunohistochemical
technique.
References
|
1
|
Zuccari DAPC, Pavam MV, Terzian ACB,
Pereira RS, Ruiz CM and Andrade JC: Immunohistochemical evaluation
of e-cadherin, Ki-67 and PCNA in canine mammary neoplasias:
correlation of prognostic factors and clinical outcome. Pesquisa
Vet Brasil. 28:207–215. 2008.
|
|
2
|
Andrade FH, Figueiroa FC, Bersano PR,
Bissacot DZ and Rocha NS: Malignant mammary tumor in female dogs:
environmental contaminants. Diagn Pathol. 5:452010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Chu PY, Hsu NC, Liao AT, Shih NY, Hou MF
and Liu CH: Overexpression of α-enolase correlates with poor
survival in canine mammary carcinoma. BMC Vet Res. 7:622011.
View Article : Google Scholar
|
|
4
|
Klopfleisch R, von Euler H, Sarli G, Pinho
SS, Gärtner F and Gruber AD: Molecular carcinogenesis of canine
mammary tumors: news from an old disease. Vet Pathol. 48:98–116.
2011. View Article : Google Scholar
|
|
5
|
Michel E, Feldmann SK, Kowalewski MP, Bley
CR, Boos A, Guscetti F and Reichler IM: Expression of prolactin
receptors in normal canine mammary tissue, canine mammary adenomas
and mammary adenocarcinomas. BMC Vet Res. 8:722012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Yoshikawa Y, Morimatsu M, Ochiai K, et al:
Establishment of a PCR analysis method for canine BRCA2. BMC Res
Notes. 5:1732012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Gelaleti GB, Jardim BV, Leonel C,
Moschetta MG and Zuccari DA: Interleukin-8 as a prognostic serum
marker in canine mammary gland neoplasias. Vet Immunol
Immunopathol. 146:106–112. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Phillips JC, Lembcke L and Chamberlin T: A
novel locus for canine osteosarcoma (OSA1) maps to CFA34, the
canine orthologue of human 3q26. Genomics. 96:220–227. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Levalle GE, Bertagnolli AC, Tavares WL and
Cassali GD: Cox-2 expression in canine mammary carcinomas:
correlation with angiogenesis and overall survival. Vet Pathol.
46:1275–1280. 2009. View Article : Google Scholar
|
|
10
|
Abreu E and Koifman S: Fatores
prognósticos no câncer da mama feminina. Rev Bras Cancerol.
48:113–131. 2002.
|
|
11
|
Rakha EA, Reis-Filho JS and Ellis IO:
Combinatorial biomarker expression in breast cancer. Breast Cancer
Res Treat. 120:293–308. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Jardim-Perassi BV, Arbab AS, Ferreira LC,
et al: Effect of melatonin in tumor growth and angiogenesis in
xenograft modelo f breast cancer. PLoS One. 9:e853112014.
View Article : Google Scholar
|
|
13
|
Roberts E, Cossigny DA and Quan GM: The
role of vascular endothelial growth factor in metastatic prostate
cancer to the skeleton. Prostate Cancer. 2013:4183402013.
View Article : Google Scholar
|
|
14
|
Gavalas NG, Liontos M, Trachana SP, et al:
Angiogenesis-related pathways in the pathogenesis of ovarian
cancer. Int J Mol Sci. 14:15885–15909. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Romon R, Adriaenssens E, Lagadec C,
Germain E, Hondermarck H and Le Bourhis X: Nerve growth factor
promotes breast cancer angiogenesis by activating multiple
pathways. Mol Cancer. 9:1572010. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Greenberg S and Rugo HS: Triple-negative
breast cancer: role of antiangiogenic agents. Cancer J. 16:33–38.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Arbab AS: Activation of alternative
pathways of angiogenesis and involvement of stem cells following
anti-angiogenesis treatment in glioma. Histol Histopathol.
27:549–557. 2012.PubMed/NCBI
|
|
18
|
Sadri N and Zhang PJ: Hypoxia-inducible
factors: mediators of cancer progression; prognostic and
therapeutic targets in soft tissue sarcomas. Cancers. 5:320–333.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Tung KH, Lin CW, Kuo CC, et al: CHC
promotes tumor growth and angiogenesis through regulation of HIF-1α
and VEGF signaling. Cancer Lett. 331:58–67. 2013. View Article : Google Scholar
|
|
20
|
Semenza GL: HIF-1 and tumor progression:
pathophysiology and therapeutics. Trends Mol Med. 8(Suppl 4):
62–66. 2002. View Article : Google Scholar
|
|
21
|
Yang L, Zhao W, Zuo WS, et al: Silencing
of osteopontin promotes the radiosensitivity of breast cancer cells
by reducing the expression of hypoxia inducible factor 1 and
vascular endothelial growth factor. Chin Med J. 125:293–299.
2012.PubMed/NCBI
|
|
22
|
Aranha AMF: Potencial angiogênico de
células pulpares humanas em hipóxia. Araraquara: Universidade
Estadual Paulista - Faculdade de Odontologia de Araraquara.
Dissertação (Doutorado). Programa de Pós-Graduação em Ciências
Odontológicas; Araraquara, São Paulo: 2008
|
|
23
|
Harris AL: Hypoxia - a key regulatory
factor in tumour growth. Nat Rev Cancer. 2:38–47. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Li XR, Liu M, Zhang YJ, et al: ER, PgR,
HER-2, Ki-67, topoisomerase IIα, and nm23-H1 proteins expression as
predictors of pathological complete response to neoadjuvant
chemotherapy for locally advanced breast cancer. Med Oncol.
28(Suppl 1): 48–54. 2011. View Article : Google Scholar
|
|
25
|
Kallergi G, Markomanolaki H, Giannoukaraki
V, et al: Hypoxia-inducible factor-1alpha and vascular endothelial
growth factor expression in circulating tumor cells of breast
cancer patients. Breast Cancer Res. 11:R842009. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Brito LG, Schiavon VF, Andrade JM, Tiezzi
DG, Peria FM and Marana HR: Expression of hypoxia-inducible factor
1-α and vascular endothelial growth factor-C in locally advanced
breast cancer patients. Clinics. 66:1313–1320. 2011.
|
|
27
|
Higashimura Y, Nakajima Y, Yamaji R, et
al: Up-regulation of glyceraldehyde-3-phosphate dehydrogenase gene
expression by HIF-1 activity depending on Sp1 in hypoxic breast
cancer cells. Arch Biochem Biophys. 509:1–8. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Ji B, Liu Y, Zhang P, Wang Y and Wang G:
COX-2 expression and tumor angiogenesis in thyroid carcinoma
patients among northeast Chinese population-result of a
single-center study. Int J Med Sci. 9:237–242. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Ferrara N: Vascular endothelial growth
factor and age-related macular degeneration: from basic science to
therapy. Nat Med. 16:1107–1111. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Kato Y, Asano K, Mogi T, et al: Clinical
significance of circulating vascular endothelial growth factor in
dogs with mammary gland tumors. J Vet Med Sci. 69:77–80. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Pande D, Negi R, Khanna S, Khanna R and
Khanna HD: Vascular endothelial growth factor levels in relation to
oxidative damage and antioxidant status in patients with breast
cancer. J Breast Cancer. 14:181–184. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Taneja P, Maglic D, Kai F, et al:
Classical and novel prognostic markers for breast cancer and their
clinical significance. Clin Med Insights Oncol. 4:15–34.
2010.PubMed/NCBI
|
|
33
|
Zhang J, Lu A, Li L, Yue J and Lu Y: p16
modulates VEGF expression via its interaction with HIF-1alpha in
breast cancer cells. Cancer Invest. 28:588–597. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Koukourakis MI, Limberis V, Tentes I, et
al: Serum VEGF levels and tissue activation of VEGFR2/KDR receptors
in patients with breast and gynecologic cancer. Cytokine.
53:370–375. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Qui CW, Lin DG, Wang JQ, Li CY and Deng
GZ: Expression and significance of PTEN and VEGF in canine mammary
gland tumours. Vet Res Commun. 32:463–472. 2008. View Article : Google Scholar
|
|
36
|
Al-Dissi AN, Haines DM, Singh B and Kidney
BA: Immunohistochemical expression of vascular endothelial growth
factor and vascular endothelial growth factor receptor-2 in canine
simple mammary gland adenocarcinomas. Can Vet J. 51:1109–1114.
2010.
|
|
37
|
Millanta F, Caneschi FV, Ressel L, Citi S
and Poli A: Expression of vascular endothelial growth factor in
canine inflammatory and non-inflammatory mammary carcinoma. J Comp
Pathol. 142:36–42. 2010. View Article : Google Scholar
|
|
38
|
Misdorp W, Else RW, Hellmén E and Lipscomb
E: Definitions and explanatory notes. Who Histological
Classification of Mammary Tumors of the Dog and Cat Washington:
Armed Forces Institute of Pathology; pp. 18–27. 1999
|
|
39
|
Cassali GD, Lavalle GE, De Nardi AB, et
al: Consensus for the diagnosis, prognosis and treatment of canine
mammary tumors. Braz J Vet Pathol. 2:153–180. 2011.
|
|
40
|
Owen LN: The TNM Classification of tumors
in domestic animals. 1st. Geneva: World Health Organization;
1980
|
|
41
|
Schmittgen TD and Livak KJ: Analyzing
real-time PCR data by the comparative CT method. Nat Protoc.
3:1101–1108. 2008. View Article : Google Scholar
|
|
42
|
Maschio LB, Madallozo BB, Capellasso BA,
et al: Immunohistochemical investigation of the angiogenic proteins
VEGF, HIF-1α and CD34 in invasive ductal carcinoma of the breast.
Acta Histochem. 116:148–157. 2014. View Article : Google Scholar
|
|
43
|
Kim HS, Park YH, Park MJ, et al: Clinical
significance of a serum CA15-3 surge and the usefulness of CA15-3
kinetics in monitoring chemotherapy response in patients with
metastatic breast cancer. Breast Cancer Res Treat. 118:89–97. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Hodorowicz-Zaniewska D, Kibil W, Małek A,
Szpor J, Kulig J and Sztefko K: Evaluation of serum concentrations
of vascular endothelial growth factor (VEGF) in breast cancer
patients. Pol J Pathol. 63:255–260. 2012. View Article : Google Scholar
|
|
45
|
Spencer L, Mann C, Metcalfe M, et al: The
effect of omega-3 FAs on tumour angiogenesis and their therapeutic
potential. Eur J Cancer. 45:2077–2086. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Jia D, Hasso SM, Chan J, et al:
Transcriptional repression of VEGF by ZNF24: mechanistic studies
and vascular consequences in vivo. Blood. 121:707–715. 2013.
View Article : Google Scholar :
|
|
47
|
Kapahi R, Manjari M, Uppal MS, Singh NR,
Sambyal V and Guleria K: Association of -2549 insertion/deletion
polymorphism of vascular endothelial growth factor with breast
cancer in North Indian patients. Genet Test Mol Biomarkers.
17:242–248. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Duranyildiz D, Camlica H, Soydinc HO,
Derin D and Yasasever V: Serum levels of angiogenic factors in
early breast cancer remain close to normal. Breast. 18:26–29. 2009.
View Article : Google Scholar
|
|
49
|
El Tarhouny S, Seefeld M, Fan AX, Hahn S,
Holzgreve W and Zhong XY: Comparison of serum VEGF and its soluble
receptor sVEGFR1 with serum cell-free DNA in patients with
breasttumor. Cytokine. 44:65–69. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Thielemann A, Baszczuk A, Kopczyński Z,
Kopczyński P and Grodecka-Gazdecka S: Clinical usefulness of
assessing VEGF and soluble receptors sVEGFR-1 and sVEGFR-2 in women
with breast cancer. Ann Agric Environ Med. 20:293–297.
2013.PubMed/NCBI
|
|
51
|
Coskun U, Günel N, Toruner FB, et al:
Serum leptin, prolactin and vascular endothelial growth factor
(VEGF) levels in patients with breast cancer. Neoplasma. 50:41–46.
2003.PubMed/NCBI
|
|
52
|
Perez-Rivas LG, Jerez JM, Fernandez-De
Sousa CE, et al: Serum protein levels following surgery in breast
cancer patients: A protein microarray approach. Int J Oncol.
41:2200–2206. 2012.PubMed/NCBI
|
|
53
|
Milani M and Harris AL: Targeting tumour
hypoxia in breast cancer. Eur J Cancer. 44:2766–2773. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Flamant L, Notte A, Ninane N, Raes M and
Michiels C: Anti-apoptotic role of HIF-1 and AP-1 in paclitaxel
exposed breast cancer cells under hypoxia. Mol Cancer. 9:1912010.
View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Ece H, Cigdem E, Yuksel K, Ahmet D, Hakan
E and Oktay TM: Use of oral antidiabetic drugs (metformin and
pioglitazone) in diabetic patients with breast cancer: how does it
affect serum Hif-1 alpha and 8Ohdg levels? Asian Pac J Cancer Prev.
13:5143–5148. 2012. View Article : Google Scholar
|
|
56
|
De Francesco EM, Lappano R, Santolla MF,
Marsico S, Caruso A and Maggiolini M: HIF-1α/GPER signaling
mediates the expression of VEGF induced by hypoxia in breast cancer
associated fibroblasts (CAFS). Breast Cancer Res. 15:R642013.
View Article : Google Scholar
|
|
57
|
Liang J, Qian Y, Xu D, Yin Q and Pan HJ:
Serum tumor markers, hypoxia-inducible factor-1α HIF-1α and
vascular endothelial growth factor, in patients with non-small cell
lung cancer before and after intervention. Asian Pac J Cancer Prev.
14:3851–3854. 2013. View Article : Google Scholar
|
|
58
|
Restucci B, Borzacchiello G, Maiolino P,
Martano M, Paciello O and Papparella S: Expression of vascular
endothelial growth factor receptor Flk-1 in canine mammary tumours.
J Comp Pathol. 130:99–104. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Ramanathan M, Pinhal-Enfield G, Hao I and
Leibovich SJ: Synergistic up-regulation of vascular endothelial
growth factor (VEGF) expression in macrophages by adenosine A2A
receptor agonists and endotoxin involves transcriptional regulation
via the hypoxia response element in the VEGF promoter. Mol Biol
Cell. 18:14–23. 2007. View Article : Google Scholar :
|
|
60
|
Mohammed RA, Green A, El-Shikh S, Paish
EC, Ellis IO and Martin SG: Prognostic significance of vascular
endothelial cell growth factors -A, -C and -D in breast cancer and
their relationship with angio- and lymphangiogenesis. Br J Cancer.
96:1092–1100. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Santos AA, Oliveira JT, Lopes CC, Amorim
IF, Vicente CM, Gärtner FR and Matos AJ: Immunohistochemical
expression of vascular endothelial growth factor in canine mammary
tumours. J Comp Pathol. 143:268–275. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Mimeault M and Batra SK: Hypoxia-inducing
factors as master regulators of stemness properties and altered
metabolism of cancer and metastasis initiating cells. J Cell Mol
Med. 17:30–54. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Yamamoto Y, Ibusuki M, Okumura Y, Kawasoe
T, Kai K, Iyama K and Iwase H: Hypoxia-inducible factor 1alpha is
closely linked to an aggressive phenotype in breast cancer. Breast
Cancer Res Treat. 110:465–475. 2008. View Article : Google Scholar
|