Introduction
Neuroblastoma is the most common heterogeneous
extracranial neoplastic disease of childhood, developing from
immature nerve cells found in several areas of the body or where
groups of nerve cells exist (1).
The metastatic phenotype of neuroblastoma is associated to
activation of several genes, some of which are deeply involved in
angiogenesis (2,3). Among these proteins, interleukin-8
(IL-8; or CXCL8) is known to be a major promoter of angiogenesis
and invasiveness of human neuroblastomas (4). Another protein firmly involved in
angiogenesis of neuroblastoma is vascular endothelial growth factor
(VEGF) (5,6). As expected, one of the control levels
is transcription-related to the interaction between IL-8 and VEGF
promoters and different transcription factors, such as NF-κB, AP-1
and C-EBP/NF-IL-6 (7–12). In addition, the expression of IL-8
and VEGF genes may be under the control of epigenetic mechanisms,
such as those regulated by microRNAs in cancer, differentiation and
inflammatory processes (13–23).
MicroRNAs (miRs) are endogenous non-protein coding
RNA molecules, from 19 to 25 nucleotides long, that regulate
specifically mRNAs (24) altering
protein levels, by inhibiting the ability of the ribosome to
'translate' the mRNA. MicroRNAs can increase mRNA degradation or
block the translation to protein with a mechanism depending on the
level of complementarity to mRNAs within the RISC complex (25). Considering that a single miR has
many mRNA targets and that a single mRNA may be targeted by several
microRNAs, it is calculated that a broad segment of the
protein-coding genome is under their regulation in any type of
biological or pathophysiological process, including
differentiation, cell cycle and apoptosis. Accordingly, alteration
of miR regulation can be associated to different diseases,
including cancer (26–28).
Among the microRNAs, miR-93-5p is clearly
demonstrated in a variety of cellular systems to be involved in
post-transcriptional regulation of IL-8 and VEGF gene expression
(15,29–31).
For instance, we found that the effects of bacterial challenge
activating IL-8 gene transcription in epithelial cells are
downregulated by miR-93-5p (29).
On the other hand, miR-93-5p has been found involved also in the
downregulation of VEGF expression (30,31).
The aim of the present investigation was to study
the effects of pre-miR-93-5p and anti-miR-93-5p on the secretome of
a neuroblastoma cell line, in order to compare results studying
IL-8 and VEGF expression with the data obtained on other
chemokines, cytokines and growth factors.
Materials and methods
Neuroblastoma cell line and culture
conditions
The SK-N-AS neuroblastoma cell line, obtained from
bone marrow brain metastasis, was purchased from Sigma
(Sigma-Aldrich, St. Louis, MO, USA) and cultured in humidified
atmosphere of 5% CO2/air in RPMI-1640 medium (Life
Technologies, Monza, Italy) supplemented with 10% fetal bovine
serum (FBS; Celbio, Milan, Italy), 10,000 U/ml penicillin and 10
mg/ml streptomycin (Sigma-Aldrich) (32). To verify possible effects on
proliferation, cell growth was monitored determining the cell
number/ml using a Z2 Coulter Counter (Coulter Electronics, Hialeah,
FL, USA).
Transfection with pre-miR and anti-miR
molecules
SK-N-AS cells were seeded at 2.5×105/500
μl into 12-wells plate and transfected with 200 nM
anti-miR-93-5p (AM:10951), pre-miR-93-5p (PM:10951) and
miR-negative controls (AM:17110, AM:17010) (Ambion, Applied
Biosystems, Foster City, CA, USA) complexed with Lipofectamine
RNAiMAX (Invitrogen, Life Technologies, Carlsbad, CA, USA). After
48 h, cell supernatants were collected and total RNA was isolated
using TRI Reagent™ (Sigma Aldrich) and immediately converted to
cDNA.
Quantification of IL-8 and VEGF mRNA
content
Total RNA (300 ng) was reverse-transcribed to cDNA
using random primers (Applied Biosystems). IL-8 and VEGF mRNAs
analyzed with RT-qPCR were quantified by iQ SYBR-Green Supermix
(Bio-Rad Laboratories, Hercules, CA, US) using the IL-8 reverse
(5′-TTA TGA ATT CTC AGC CCT CTT CAA AAA CTT CTC-3′) and forward
(5′-GTG CAG TTT TGC CAA GGA GT-3′) primers and by VEGF TaqMan Gene
Expression Assays (HS00173626_m1), and normalized to the calibrator
genes RPL13A (code HS03043885_g1) and 18S rRNA (code 4310893E) (all
from Applied Biosystems) according to the manufacturer's
instructions. These assays were carried out with a CFX96 Touch™
Real-Time PCR Detection System (Bio-Rad Laboratories). Relative
quantification of gene expression was performed using the
comparative threshold (CT) method. Changes in mRNA
expression level were expressed as fold-change over Lipofectamine
RNAiMAX treated samples.
Bio-Plex analysis
Cytokines, chemokines and growth factors in tissue
culture supernatants released from the cells under analysis were
measured by Bio-Plex Pro Human Cytokine 27-Plex Assay
(#M50-0KCAF0Y; Bio-Rad Laboratories) as described by the
manufacturer (33,34). The Bio-Plex cytokine assay is
designed for the multiplex quantitative measurement of multiple
cytokines in a single well using as little as 50 μl of
sample. Samples were analyzed on a Bio-Rad 96-well plate reader
using the Bio-Plex Suspension Array System and Bio-Plex Manager
software (Bio-Rad Laboratories) (33,34).
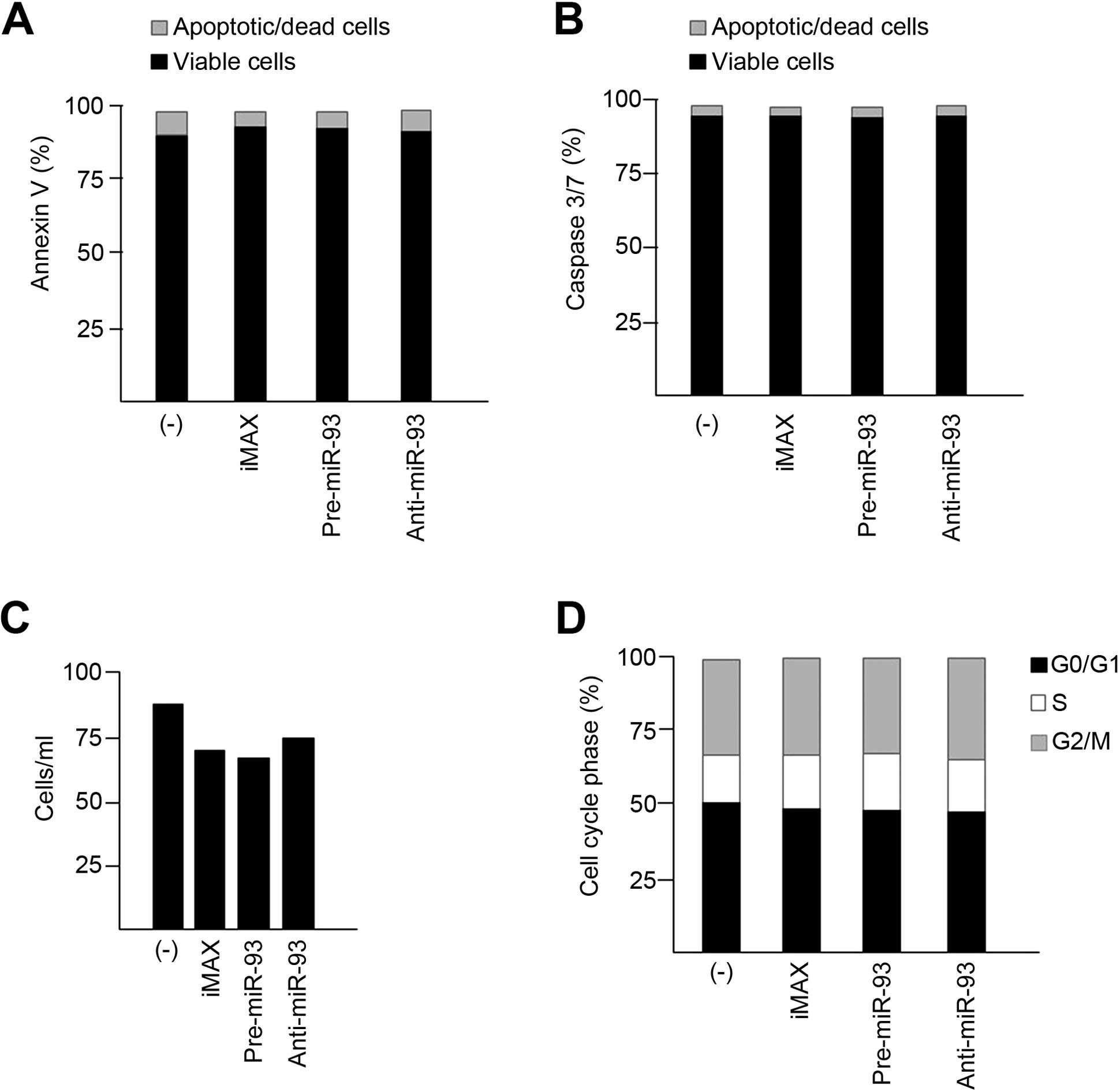
Analysis of apoptosis and cell cycle
SK-N-AS neuroblastoma cells were treated for 48 h
with 200 nM pre-miR-93-5p, anti-miR-93-5p and miR negative
controls, then apoptosis was detected with Annexin V and Dead Cell
and Caspase 3/7 Muse assays. Cell cycle was analyzed with the Muse
Cell Cycle kit (EMD Millipore Corporation, Hayward, CA, USA) using
the Muse Cell Analyzer instrument (Millipore Corporation),
according to the instructions supplied by the manufacturer. Data
from prepared samples were acquired and recorded utilizing
dedicated programs (Millipore) (35).
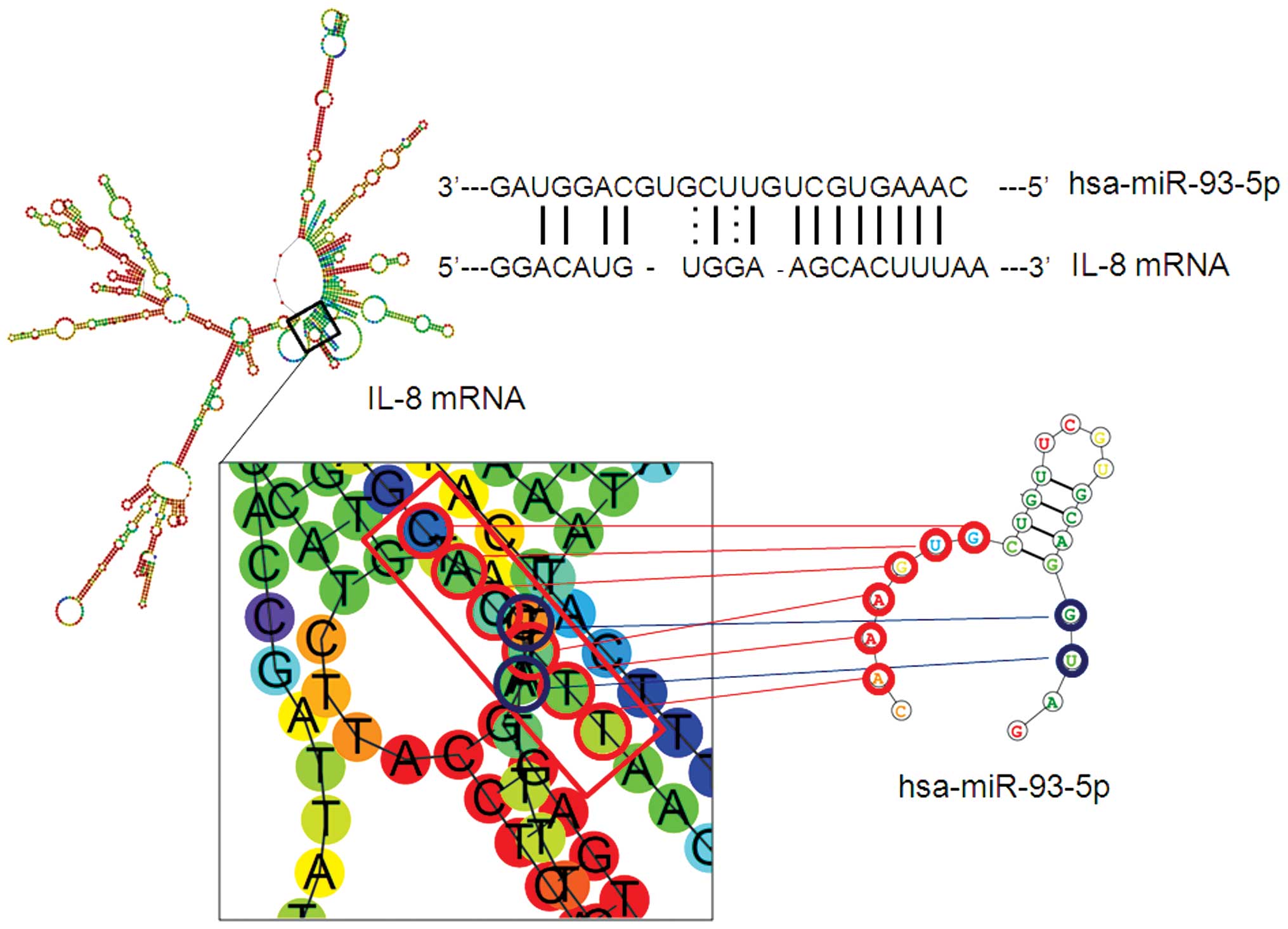
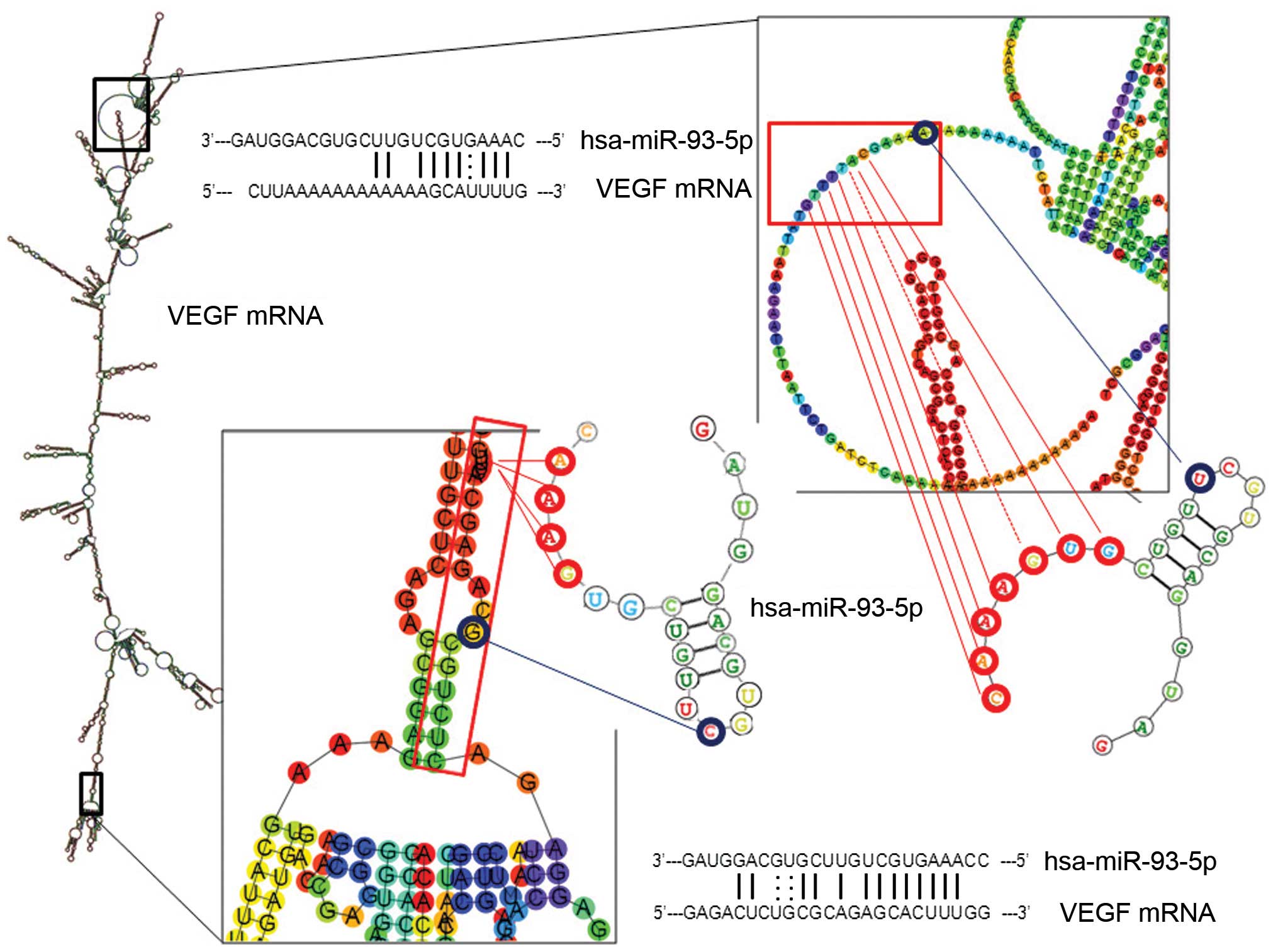
Thermodynamic structure prediction and
interaction
Analysis of RNA secondary structure was performed
using ViennaRNA Web Services, RNA fold server, Institute of
Theoretical Chemistry, University of Vienna (http://rna.tbi.univie.ac.at/cgi-bin/RNAfold.cgi)
(36). RNA sequences were obtained
from UCSC Genome Bioinformatics (http://genome.ucsc.edu/) (37) and microRNA sequence from miRBase,
the microRNA database, University of Manchester (http://www.mirbase.org/) (38,39).
The interactions between mRNAs and miRNA were predicted with
microrna.org, Memorial Sloan-Kettering Cancer Center
(http://www.microrna.org/microrna/home.do) (40), with TargetScan 6.2, Whitehead
Institute for Biomedical Research (http://www.targetscan.org/) (41) and miRWalk 2.0 Heidelberg University
(http://www.umm.uniheidelberg.de/apps/zmf/mirwalk/)
(42).
Statistical analysis
Results are expressed as mean ± standard deviation
(SD). Comparisons between groups were made using paired Student's
t-test. Statistical significance was defined as p<0.05
(statistically significant) and p<0.01 (highly statistically
significant).
Results
Secretomic profile in SK-N-AS
neuroblastoma cells treated with pre-miR-93-5p and anti-miR-93-5p:
miR-93-5p dependency in genes involved in inflammation
In order to verify whether miR-93-5p regulates
pro-inflammatory genes, a 27-plex cytokine assay was carried out
using supernatants collected from 2-days cultured SK-N-AS
neuroblastoma cells seeded at the initial concentration of
5×105 cells/ml. A preliminary analysis of the secretome
of SK-N-AS cells demonstrates a strong difference with respect to
protein release. Proteins released with highest efficiency (>10
pg/ml) were IL-7, IL-8, IL-15, GM-CSF, G-CSF, IP-10, MCP-1 and VEGF
(data not shown) and were considered in our analysis. To study
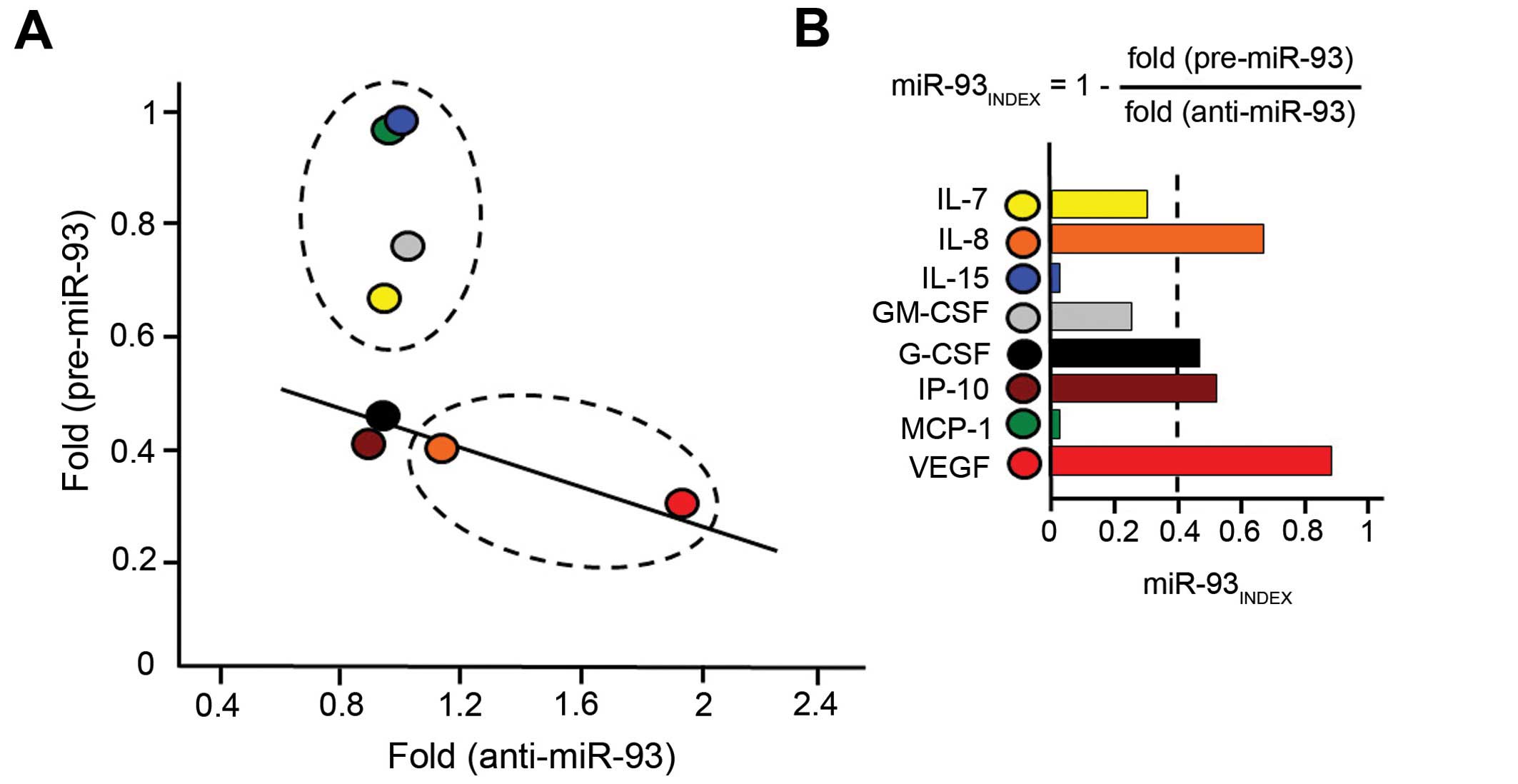
miR-93-5p dependency, SK-N-AS cells were cultured in the absence or
in the presence of pre-miR-93-5p and anti-miR-93-5p. Fig. 1 shows the first set of data firmly
demonstrating that these treatments have no major effects on
SK-N-AS cellular apoptosis (Fig. 1A and
B), cell growth (Fig. 1C) and
cell cycle (Fig. 1D). As far as the
effects of pre-miR-93-5p and anti-miR-93-5p treatments on
secretome, in some cases we found a relevant inverse correlation
between relative content of secreted proteins in cells
pre-transfected with pre-miR-93-5p and the fold increase of
secretion following anti-miR-93-5p treatment (Fig. 2A). We applied an algorithm for
determining the miR-93-5p dependency index (miR-93INDEX)
of SK-N-AS cells, based on the determination of the
treated/untreated fold values as follows: miR-93INDEX =
1 − [fold (pre-miR-93 treatment)/fold (anti-miR-93 treatment)].
Following this algorithm we expected high values of
miR-93INDEX for the genes whose expression was regulated
by miR-93. The miR-93INDEX values for the different
cytokines/chemokines/growth factors studied are indicated in
Fig. 2B. Taken together, these
results strongly suggest that the two genes displaying the highest
levels of sensitivity to miR-93-5p are IL-8 and VEGF.
Interestingly, IL-8 and VEGF are demonstrated to play a significant
role in the late stages of neuroblastoma progression, including
interaction with the microenvironment leading to angiogenesis
(2–6,8).
IL-8 and VEGF mRNAs are putative targets
of miR-93-5p
Figs. 3 and 4 show the possible interactions between
miR-93-5p and miR-93-5p binding sites located within the IL-8 mRNA
(Fig. 3) and VEGF mRNA (Fig. 4) sequences. The miR-93-5p target
sequences of IL-8 and VEGF mRNAs are shown, indicating possible
base-pairing with miR-93-5p. These predicted analyses support the
hypothesis that both IL-8 and VEGF mRNAs are targets of
miR-93-5p.
Alteration of IL-8 gene and VEGF gene
expression in SK-N-AS cells transfected with pre-miR-93-5p and
anti-miR-93-5p
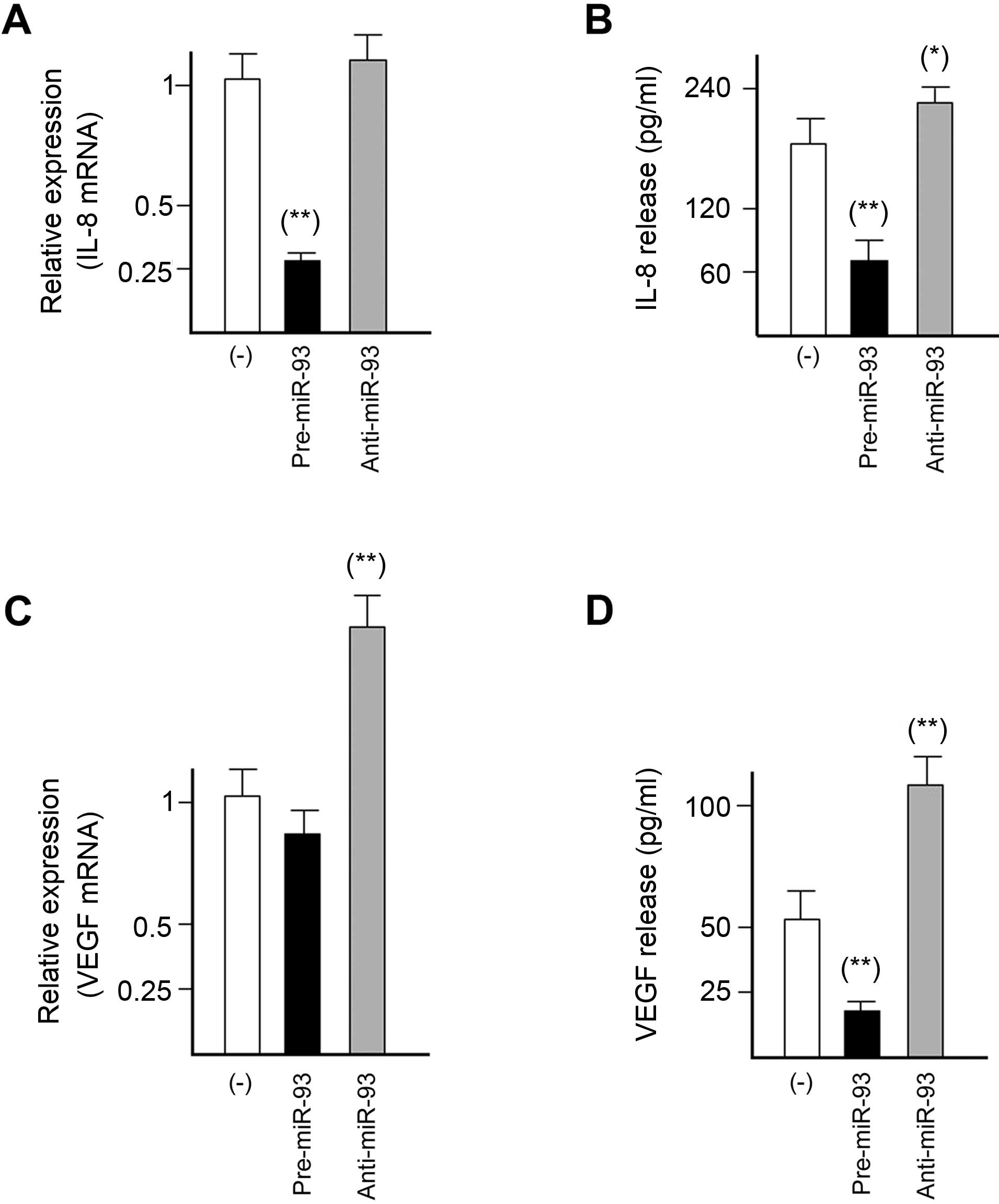
Fig. 5 shows
experiments in which pre-miR-93-5p and anti-miR-93-5p have been
transfected to SK-N-AS cells and gene expression of IL-8 (Fig. 5A and B) and VEGF (Fig. 5C and D) gene expression was
determined by RT-qPCR (Fig. 5A and
C) and Bio-Plex analysis of released proteins (Fig. 5B and D).
The results reported regarding the effects on IL-8
gene expression, demonstrate that when SK-N-AS neuroblastoma cells
are transfected with a pre-miR-93-5p RNA a decrease of IL-8 mRNA
occurs (Fig. 5A). This is confirmed
by the Bio-Plex analysis performed on cell growth medium, in which
a sharp decrease of released IL-8 protein was found in
pre-miR-93-5p treated SK-N-AS cell cultures (Fig. 5B). Despite the fact that
pre-miR-93-5p effects on VEGF mRNA were minor (Fig. 5C), the same trend was found for VEGF
release, as shown in Fig. 5D,
demonstrating that VEGF secretion is sharply decreased in
pre-miR-93-5p treated SK-N-AS cells.
In order to further sustain the possible involvement
of miR-93-5p on IL-8 and VEGF expression, we determined whether
treatment of the SK-N-AS neuroblastoma cell line with anti-miR
against miR-93-5p led to increased IL-8 and VEGF. The SK-N-AS
neuroblastoma cells were transfected with anti-miR-93-5p and the
expression of IL-8 and VEGF mRNA content and protein secretion were
analyzed by RT-qPCR and Bio-Plex assays, respectively. The
anti-miR-93-5p was administrated at the concentration of 200 nM
with the Lipofectamine RNAiMAX transfection reagent. We first
demonstrated a 65.2±5.8 reduction of the miR-93-5p accumulation in
SK-N-AS neuroblastoma cells treated with anti-miR-93-5p (data not
shown). Fig. 5 (panels A and B)
demonstrates that the forced downregulation of miR-93-5p is
accompanied by a slight increase of IL-8 mRNA (Fig. 5A) and a significantly higher release
of IL-8 (Fig. 5B). In addition
increased expression of VEGF mRNA (Fig.
5C) and VEGF release (Fig. 5D)
was found in anti-miR-93-5p treated SK-N-AS cells. Altogether, the
data shown in Fig. 5 are fully in
agreement with the hypothesis of an involvement of miR-93-5p in
IL-8 and VEGF gene expression in this tumor cell line.
Discussion
A first conclusion of the present study is that
treatment of SK-N-AS cells with pre-miR-93-5p and anti-miR-93-5p
leads to different effects on expressed cytokines/chemokines/growth
factors. The data obtained are shown in Fig. 2, which demonstrates that miR-93-5p
dependency was found for G-CSF and IP-10, but is particularly
evident for IL-8 (index, 0.65) and VEGF (index, 0.85). As expected
from data in Fig. 2, we found
miR-93-5p binding sites in IL-8 and VEGF mRNAs (see the prediction
analysis of interactions shown in Figs.
3 and 4), in agreement with the
found miR-93INDEX.
The final conclusion of the present study is that
the microRNA miR-93-5p is involved in the control of the expression
of the IL-8 and VEGF genes in the neuroblastoma SK-N-AS cell line
on the basis of the effects of different transfections with
pre-miR-93-5p or anti-miR-93-5p.
The effects of these treatments, showed in Fig. 5, were analyzed by RT-qPCR (looking
at the IL-8 and VEGF mRNA content) and by Bio-Plex analysis
(looking at IL-8 and VEGF protein secretion).
In addition to basic science implications, our data
may be of interest in applied biomedicine (43,44),
since we demonstrated that forced expression of miR-93-5p is able
to reduce IL-8 and VEGF gene expression; therefore, molecules
mimicking pre-miR-93-5p activity may be proposed to reduce IL-8 and
VEGF dependent angiogenesis in neuroblastomas.
Acknowledgments
This study was granted by CIB, by COFIN-2009 and by
AIRC (IG 13575: peptide nucleic acids targeting oncomiR and
tumor-suppressor miRNAs: cancer diagnosis and therapy). E.F. was a
recipient of a CIB-funded fellowship.
Abbreviations:
|
miR
|
microRNA
|
|
IL
|
interleukin
|
|
VEGF
|
vascular endothelial growth factor
|
|
GM-CSF
|
granulocyte-macrophage
colony-stimulating factor
|
|
G-CSF
|
granulocyte-colony stimulating
factor
|
|
IP-10
|
interferon gamma-induced protein
10
|
|
MCP-1
|
monocyte chemotactic protein 1
|
|
PCR
|
polymerase-chain reaction
|
|
RT
|
reverse transcription
|
|
RT-qPCR
|
RT-quantitative PCR
|
References
|
1
|
Park JR, Bagatell R, London WB, Maris JM,
Cohn SL and Mattay KK: Children's Oncology Group's 2013 blueprint
for research: Neuroblastoma. Pediatr Blood Cancer. 60:985–993.
2013. View Article : Google Scholar
|
|
2
|
Ribatti D, Marimpietri D, Pastorino F,
Brignole C, Nico B, Vacca A and Ponzoni M: Angiogenesis in
neuroblastoma. Ann NY Acad Sci. 1028:133–142. 2004. View Article : Google Scholar
|
|
3
|
Ribatti D: Anti-angiogenesis in
neuroblastoma. Crit Rev Oncol Hematol. 86:212–221. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Eggert A, Ikegaki N, Kwiatkowski J, Zhao
H, Brodeur GM and Himelstein BP: High-level expression of
angiogenic factors is associated with advanced tumor stage in human
neuroblastomas. Clin Cancer Res. 6:1900–1908. 2000.PubMed/NCBI
|
|
5
|
Choudhury SR, Karmakar S, Banik NL and Ray
SK: Targeting angiogenesis for controlling neuroblastoma. J Oncol.
2012:7820202012.
|
|
6
|
Shusterman S and Maris JM: Prospects for
therapeutic inhibition of neuroblastoma angiogenesis. Cancer Lett.
228:171–179. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Megison ML, Gillory LA and Beierle EA:
Cell survival signaling in neuroblastoma. Anticancer Agents Med
Chem. 13:563–575. 2013. View Article : Google Scholar :
|
|
8
|
Pistoia V, Bianchi G, Borgonovo G and
Raffaghello L: Cytokines in neuroblastoma: From pathogenesis to
treatment. Immunotherapy. 3:895–907. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Neuschäfer-Rube F, Pathe-Neuschäfer-Rube
A, Hippenstiel S, Kracht M and Püschel GP: NF-κB-dependent IL-8
induction by prostaglandin E2 receptors EP1
and EP4. Br J Pharmacol. 168:704–717. 2013. View Article : Google Scholar
|
|
10
|
Finotti A, Borgatti M, Bezzerri V, Nicolis
E, Lampronti I, Dechecchi M, Mancini I, Cabrini G, Saviano M,
Avitabile C, et al: Effects of decoy molecules targeting NF-kappaB
transcription factors in cystic fibrosis IB3-1 cells: Recruitment
of NF-kappaB to the IL-8 gene promoter and transcription of the
IL-8 gene. Artif DNA PNA XNA. 3:97–296. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Khanjani S, Terzidou V, Johnson MR and
Bennett PR: NFκ B and AP-1 drive human myometrial IL8 expression.
Mediators Inflamm. 2012:5049522012. View Article : Google Scholar
|
|
12
|
Bezzerri V, Borgatti M, Finotti A,
Tamanini A, Gambari R and Cabrini G: Mapping the transcriptional
machinery of the IL-8 gene in human bronchial epithelial cells. J
Immunol. 187:6069–6081. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wei T, Xu N, Meisgen F, Ståhle M, Sonkoly
E and Pivarcsi A: Interleukin-8 is regulated by miR-203 at the
posttranscriptional level in primary human keratinocytes. Eur J
Dermatol. Apr 19–2013.Epub ahead of print.
|
|
14
|
Perng DW, Yang DM, Hsiao YH, Lo T, Lee OK,
Wu MT, Wu YC and Lee YC: miRNA-146a expression positively regulates
tumor necrosis factor-α-induced interleukin-8 production in
mesenchymal stem cells and differentiated lung epithelial-like
cells. Tissue Eng Part A. 18:2259–2267. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Chuang TD, Luo X, Panda H and Chegini N:
miR-93/106b and their host gene, MCM7, are differentially expressed
in leiomy-omas and functionally target F3 and IL-8. Mol Endocrinol.
26:1028–1042. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Zhou R, Li X, Hu G, Gong AY, Drescher KM
and Chen XM: miR-16 targets transcriptional corepressor SMRT and
modulates NF-kappaB-regulated transactivation of interleukin-8
gene. PLoS One. 7:e307722012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Bhattacharyya S, Balakathiresan NS,
Dalgard C, Gutti U, Armistead D, Jozwik C, Srivastava M, Pollard HB
and Biswas R: Elevated miR-155 promotes inflammation in cystic
fibrosis by driving hyperexpression of interleukin-8. J Biol Chem.
286:11604–11615. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Bhaumik D, Scott GK, Schokrpur S, Patil
CK, Orjalo AV, Rodier F, Lithgow GJ and Campisi J: MicroRNAs
miR-146a/b negatively modulate the senescence-associated
inflammatory mediators IL-6 and IL-8. Aging. 1:402–411. 2009.
View Article : Google Scholar
|
|
19
|
Khan FH, Pandian V, Ramraj S, Aravindan S,
Herman TS and Aravindan N: Reorganization of metastamiRs in the
evolution of metastatic aggressive neuroblastoma cells. BMC
Genomics. 16:5012015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Chen L, Li ZY, Xu SY, Zhang XJ, Zhang Y,
Luo K and Li WP: Upregulation of miR-107 inhibits glioma
angiogenesis and VEGF expression. Cell Mol Neurobiol. Jun
18–2015.Epub ahead of print.
|
|
21
|
Tsuchiya M, Kumar P, Bhattacharyya S,
Chattoraj S, Srivastava M, Pollard HB and Biswas R: Differential
regulation of inflammation by inflammatory mediators in cystic
fibrosis lung epithelial cells. J Interferon Cytokine Res.
33:121–129. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Cabrini G, Fabbri E, Lo Nigro C, Dechecchi
MC and Gambari R: Regulation of expression of
O6-methylguanine-DNA methyltransferase and the treatment
of glioblastoma (Review). Int J Oncol. 47:417–428. 2015.PubMed/NCBI
|
|
23
|
Bianchi N, Finotti A, Ferracin M,
Lampronti I, Zuccato C, Breveglieri G, Brognara E, Fabbri E,
Borgatti M, Negrini M, et al: Increase of microRNA-210, decrease of
raptor gene expression and alteration of mammalian target of
rapamycin regulated proteins following mithramycin treatment of
human erythroid cells. PLoS One. 10:e01215672015. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Sun K and Lai EC: Adult-specific functions
of animal micro-RNAs. Nat Rev Genet. 14:535–548. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Berindan-Neagoe I, Monroig PC, Pasculli B
and Calin GA: MicroRNAome genome: A treasure for cancer diagnosis
and therapy. CA Cancer J Clin. 64:311–336. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Adams BD, Kasinski AL and Slack FJ:
Aberrant regulation and function of microRNAs in cancer. Curr Biol.
24:R762–R776. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Hayes J, Peruzzi PP and Lawler S:
MicroRNAs in cancer: Biomarkers, functions and therapy. Trends Mol
Med. 20:460–469. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Piva R, Spandidos DA and Gambari R: From
microRNA functions to microRNA therapeutics: Novel targets and
novel drugs in breast cancer research and treatment (Review). Int J
Oncol. 43:985–994. 2013.PubMed/NCBI
|
|
29
|
Fabbri E, Borgatti M, Montagner G, Bianchi
N, Finotti A, Lampronti I, Bezzerri V, Dechecchi MC, Cabrini G and
Gambari R: Expression of microRNA-93 and interleukin-8 during
Pseudomonas aeruginosa-mediated induction of proinflammatory
responses. Am J Respir Cell Mol Biol. 50:1144–1155. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Long J, Wang Y, Wang W, Chang BH and
Danesh FR: Identification of microRNA-93 as a novel regulator of
vascular endothelial growth factor in hyperglycemic conditions. J
Biol Chem. 285:23457–23465. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Fang L, Deng Z, Shatseva T, Yang J, Peng
C, Du WW, Yee AJ, Ang LC, He C, Shan SW, et al: MicroRNA miR-93
promotes tumor growth and angiogenesis by targeting integrin-β8.
Oncogene. 30:806–821. 2011. View Article : Google Scholar
|
|
32
|
Sugimoto T, Tatsumi E, Kemshead JT, Helson
L, Green AA and Minowada J: Determination of cell surface membrane
antigens common to both human neuroblastoma and leukemia-lymphoma
cell lines by a panel of 38 monoclonal antibodies. J Natl Cancer
Inst. 73:51–57. 1984.PubMed/NCBI
|
|
33
|
Borgatti M, Mancini I, Bianchi N, Guerrini
A, Lampronti I, Rossi D, Sacchetti G and Gambari R: Bergamot
(Citrus bergamia Risso) fruit extracts and identified components
alter expression of interleukin 8 gene in cystic fibrosis bronchial
epithelial cell lines. BMC Biochem. 12:152011. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Penolazzi L, Lambertini E, Tavanti E,
Torreggiani E, Vesce F, Gambari R and Piva R: Evaluation of
chemokine and cytokine profiles in osteoblast progenitors from
umbilical cord blood stem cells by BIO-PLEX technology. Cell Biol
Int. 32:320–325. 2008. View Article : Google Scholar
|
|
35
|
Brognara E, Fabbri E, Bazzoli E, Montagner
G, Ghimenton C, Eccher A, Cantù C, Manicardi A, Bianchi N, Finotti
A, et al: Uptake by human glioma cell lines and biological effects
of a peptide-nucleic acids targeting miR-221. J Neurooncol.
118:19–28. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Hofacker IL: Vienna RNA secondary
structure server. Nucleic Acids Res. 31:3429–3431. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Kent WJ, Hsu F, Karolchik D, Kuhn RM,
Clawson H, Trumbower H and Haussler D: Exploring relationships and
mining data with the UCSC Gene Sorter. Genome Res. 15:737–741.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Griffiths-Jones S, Grocock RJ, van Dongen
S, Bateman A and Enright AJ: miRBase: MicroRNA sequences, targets
and gene nomenclature. Nucleic Acids Res. 34:D140–D144. 2006.
View Article : Google Scholar :
|
|
39
|
Kozomara A and Griffiths-Jones S: miRBase:
Annotating high confidence microRNAs using deep sequencing data.
Nucleic Acids Res. 42:D68–D73. 2014. View Article : Google Scholar :
|
|
40
|
Betel D, Wilson M, Gabow A, Marks DS and
Sander C: The http://microRNA.orgurisimplemicroRNA.org resource:
Targets and expression. Nucleic Acids Res. 36(Database): D149–D153.
2008. View Article : Google Scholar
|
|
41
|
Lewis BP, Shih IH, Jones-Rhoades MW,
Bartel DP and Burge CB: Prediction of mammalian microRNA targets.
Cell. 115:787–798. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Mol Biol Dweep H, Gretz N and Sticht C:
miRWalk database for miRNA-target interactions. Methods.
1182:289–305. 2014.
|
|
43
|
Fabbri E, Manicardi A, Tedeschi T, Sforza
S, Bianchi N, Brognara E, Finotti A, Breveglieri G, Borgatti M,
Corradini R, et al: Modulation of the biological activity of
microRNA-210 with peptide nucleic acids (PNAs). ChemMedChem.
6:2192–2202. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Gambari R, Fabbri E, Borgatti M, Lampronti
I, Finotti A, Brognara E, Bianchi N, Manicardi A, Marchelli R and
Corradini R: Targeting microRNAs involved in human diseases: A
novel approach for modification of gene expression and drug
development. Biochem Pharmacol. 82:1416–1429. 2011. View Article : Google Scholar : PubMed/NCBI
|