Introduction
Hepatocellular carcinoma (HCC) is now the third
leading cause of cancer-related deaths worldwide. Almost half a
million people are diagnosed with this disease every year (1), and it is quite prevalent among
developing countries (2,3). Although the standard protocols and
treatment methods have been well accepted and used for clinical HCC
management, the prognosis for patients who are candidates to
receive curative treatments such as surgical resection and
ablation, is mainly unfavorable (4). Therefore, early diagnosis appears to
be critical. HCC can be diagnosed by non-invasive imaging such as
contrast-enhanced computerized tomography (CT) or magnetic
resonance imaging (MRI), and by several reported biomarkers, such
as α-fetoprotein (AFP), glypican-3 and des-gamma-carboxy
prothrombin (5). Although these
markers are currently reported to have been accepted for HCC
screening, their sensitivity and specificity are somehow
unsatisfactory (6). Furthermore, in
the updated practice guidelines by the American Association for the
Study of Liver Disease (AASLD) for HCC management, obtaining the
AFP serum level was not recommended as a screening test due to its
inadequate sensitivity (7). Hence,
there is still urgent need to find a sensitive biomarker for HCC
prognosis and potential therapeutic targeting.
Peroxiredoxins (PRDXs), which are widely expressed
in human and animal cells, refer to a thiol-specific anti-oxidant
enzyme family (8,9). It has been indicated that prolonged
oxidative stress leading to the activation of multiple signaling
pathways and alterations of transcription factors is a driving
mechanism of currently known carcinogenesis (10,11).
As a family member of PRDXs, PRDX2 is capable of regulating
intracellular redox status byscavenging peroxides and reactive
oxygen species (ROS), which are believed to be the most vital
stimulito trigger several signaling pathways related to oxidative
stress and cancer progression (12,13).
Emerging studies have demonstrated that PRDX2 is frequently
overexpressed in several types of cancers, such as lung, colorectal
and ovarian cancer (14–16). It can be acknowledged from these
studies that a high level of PRDX2 may generate a protective effect
to cancer cells, and PRDX2-induced ROS reduction is beneficial for
cancer cell survival. A recent study led by Zhou et al
reported that PRDX2 silencing promoted
H2O2-induced ROS production and led to
increased cell death in HCC SMMC-7721 cells; while PRDX2
upregulation inhibited cancer cell death (17). According to our recently published
research study led by Zhao et al, using 2-dimensional gel
electrophoresis and matrix-assisted laser desorption ionization
time-of-flight mass spectrometry, 11 different proteins were
identified from 10 poorly differentiated HCC tissues and 10 well
differentiated HCC tissues, among which PRDX2 was found to be
upregulated in poorly differentiated HCC tissues compared to the
well differentiated HCC tissues. Using bioinformatics tools, it was
revealed that PRDX2 may be correlated with tumor invasion,
metastasis, and poor prognosis, thus serving as a potentially
useful diagnostic and therapeutic biomarker (18). However, whether the expression level
of PRDX2 has clinical significance in HCC patients has yet to be
reported. Thus, our study aimed to investigate the prognostic value
of PRDX2 in HCC patients.
Materials and methods
Cell lines and antibodies
The human HCC cell line HCCLM3 and normal liver cell
line L-02 were purchased from the Cell Bank of the Chinese Academy
of Sciences (Shanghai, China). All cell lines were routinely
incubated (37°C, 5% CO2) in high-glucose Dulbecco's
modified Eagle's medium (DMEM; Invitrogen; Thermo Fisher
Scientific, Inc., Waltham, MA, USA), supplemented with 10% fetal
bovine serum (FBS). The rabbit monoclonal anti-PRDX2 antibody
(EPR5154) (cat. no. ab109367) was purchased from Abcam (Cambridge,
MA, USA). The HRP-conjugated anti-rabbit IgG (cat. no. A9169) was
purchased from Sigma-Aldrich; Merck KGaA (Darmstadt, Germany).
Pathological tissues and follow-up of
patients
Paraffin-embedded HCC and corresponding adjacent
normal liver tissue samples were obtained from 180 cases of
patients who underwent radical surgery at The First Affiliated
Hospital of Lanzhou University (Gansu, China) from January 2009 to
April 2010. A total of 176 cases of HCC patients were enrolled in
tissue microarray analysis. The follow-up period was defined as the
time interval from the date of surgery to the date of death or last
follow-up date. The latest follow-up information was updated in
June 2016. All patients were regularly followed-up at an outpatient
clinic every 3 months during the first year, every 6 months until
the 5th year, and then annually. All included patients had complete
follow-up information until death or the latest follow-up date. At
follow-up visits, all medical data regarding preoperative
diagnosis, surgery, recurrence, clinical staging, adjuvant
treatment, clinical follow-up, and cause of death were re-assessed
and recorded to our database by a surgery specialist. The current
vital status of each patient was reviewed by confirming deaths from
the patient registry of the hospital or, if uncertain, from the
Gansu Branch of China Population Register Centre (Lanzhou City,
China). Overall survival (OS) was defined as the interval from the
date of surgery to the time that the patient succumbed to HCC.
Patients alive at the end of follow-up were censored. Disease-free
survival (DFS) was defined as the interval between the day that
surgery was performed and the day that recurrence was first
detected. If recurrence was not diagnosed, the date of death due to
HCC or the last follow-up was used. The tumor-node-metastasis (TNM)
staging was classified according to the criteria proposed by the
Standard American Joint Committee on Cancer (AJCC). The present
study was approved by the Ethics Committee on human research at The
First Affiliated Hospital of Lanzhou University (approval no.
LDYYLL-2010-56). Informed and written consents were obtained from
the patients or their relatives for the use of these clinical
materials for research, which were performed in accordance with the
Declaration of Helsinki of the World Medical Association.
Tissue microarrays and
immunohistochemistry
Hematoxylin and eosin (H&E) staining was applied
on sections obtained from a total of 180 paraffin-embedded HCC
tissue samples and their matched adjacent normal liver tissues
samples; 1-mm core samples for tissue microarray construction
(Beecher Instruments, Inc., Sun Prairie, WI, USA) were obtained
from typical regions from each section of 176 enrolled tumor
samples and their matched normal liver tissue samples (total 352
cores). Regions of benign liver and HCC were determined by an
experienced pathologist for each patient. Tumor staging and
pathological grading were determined by a qualified pathologist
before scoring any immunostaining. Finally, 2 sets of tissue
microarrays entirely carrying 176 paired cores were successfully
constructed to further implement PRDX2 immunostaining.
An immunohistochemical kit (GeneTech, Co., Ltd.,
Shanghai, China) was used to perform immunostaining of PRDX2 on
tissue microarrays, the applied concentration of rabbit monoclonal
antibodies to PRDX2 was: 1.0%. All steps were performed according
to the manufacturer's protocols. The PRDX2 immunostaining score was
defined as follows: Score 0, negative; score 1, <30% positive
cancer cells; score 2, 30–50% positive cancer cells; score 3,
51–70% positive cancer cells; and score 4, >70% positive cancer
cells. The PRDX2 staining intensity score was defined as: 0, no
color or extremely weak; 1, light yellow; 2, light brown; or 3,
brown (19,20). Microarrays were cross-assessed by 2
experienced pathologists.
Quantitative real-time
reverse-transcription PCR analysis
To assess PRDX2 expression at transcript
levels, RT-PCR was performed to amplify PRDX2 cDNA fragments
from total RNAs purified from isolated cells and frozen
specimens using TRIzol reagent (Invitrogen; Thermo Fisher
Scientific, Inc.). Total RNA (1 µg) was reverse-transcribed
with the PrimeScript™ RT reagent Kit and gDNA Eraser (Takara Bio,
Inc., Kusatsu, Japan). All the reactions were performed in
triplicate, and the GAPDH gene was used as the internal
control. Primer sequences used for the amplification of human genes
were as follows: PRDX2 forward, 5′-GGACTCTCAGTTCACCCACCT-3′
and reverse, 5′-GCCCTCATCTGTTTTCAGCA-3′; and GAPDH forward,
5′-TGACTTCAACAGCGACACCCA-3′ and reverse,
5′-CACCCTGTTGCTGTAGCCAAA-3′. Primers were designed to span
different exons of PRDX2 genes to ensure the amplification
of cDNAs instead of contaminated genomic DNA, and
RNAs without reverse transcription were used as negative
controls. The relative expression levels of mRNAs were
calculated using the 2 - (ΔΔCq sample - ΔΔCq control) method
(21).
Western blot analysis
To assess PRDX2 expression at protein levels, the
tumor tissues and cells were rinsed with PBS, and lysates were
prepared using RIPA buffer (Sigma-Aldrich; Merck KGaA). Total
protein concentrations were determined using a BCA protein
concentration assay kit (Beyotime Institute of Biotechnology,
Haimen, China). Before blotting, 10% separating gel (Beyotime
Institute of Biotechnology) and 5% stacking gel (Beyotime Institute
of Biotechnology) were prepared. In both cell line and tissue
western blot experiments, a quantity of 50 µg protein sample was
loaded to each lane before electrophoresis began. Then the
polyvinylidene fluoride (Millipore; Merck KGaA) was used to perform
protein transfer. Blotted membranes were firstly moved to blocking
buffer containing 5% bovine serum albumin (BSA; cat. no. 180549; MP
Biomedicals, LLC., Solon, OH, USA), shaking at room temperature for
1 h, then incubated with 0.879 mg/ml rabbit monoclonal anti-PRDX2
(diluted 1:1,000; cat. no. ab109367; Abcam, Cambridge, MA, USA) and
polyclonal anti-actin (diluted 1:1,000; cat. no. ab8227; Abcam)
primary antibodies at 4°C overnight, and then incubated with 2
mg/ml HRP-conjugated anti-rabbit IgG (diluted 1:5,000; cat. no.
A9169; Sigma-Aldrich; Merck KGaA) for 1 h at room temperature.
After washing, ECL Western Blotting reagent (Millipore; Merck KGaA)
was applied for the detection. The Glyco Bandscan software (version
5.0; Glyco, Inc., Madison, WI, USA) was used for densitometry.
PRDX2 knockdown by
lentivirus-expressed short hairpin RNAs
Lentivirus-expressing short hairpin RNAs (shRNAs)
designed to target different sites of the PRDX2 transcript
were obtained from Shanghai GeneChem Co., Ltd. (Shanghai, China).
To knock down PRDX2 gene expression in HCC cell line HCCLM3, a
total of 4 shRNA-expressing lentiviruses
(PRDX2-shRNA1-PRDX2-shRNA4) and corresponding control empty viruses
were used to transfect the HCC cell line HCCLM3 following
previously described protocols (22). Finally, 2 lentivirus-transfected
HCCLM3 clones, HCCLM3-sh-PRDX2-1 and HCCLM3-sh-PRDX2-3 were used in
further experiments. In brief, HCC cells were co-cultured with 8
mg/ml hexadimethrine bromide (Sigma-Aldrich; Merck KGaA) in the
presence of 1 ml lentiviral particles containing medium with a
multiplicity of infection of 0.5–1. Cells were incubated at 37°C in
a humidified incubator in an atmosphere of 5% CO2 for 20
h, and then washed and cultured in fresh media. The cells were
cultured for another 4 days, and then the levels of PRDX2 protein
were assessed by western blotting. Stably transfected clones were
selected and validated for PRDX2 expression by q-RT-PCR and
western blotting.
Cell proliferation assay
Cells (2,000/well) were dispensed with culture media
(100 µl) into 96-well plates. At specified time-points (0, 24, 48,
72 and 96 h), 10 µl CCK-8 solution (Dojindo Molecular Technologies,
Inc., Kumamoto, Japan) was added to each well. The absorbance at
450 nm was assessedat the end of the incubation (4 h). All
experiments were performed in triplicate.
Cell migration assay
Cell migration assays were performed using a
24-cluster Transwell plate (8-µm pore size; EMD Millipore,
Billerica, MA, USA). A total of 1×105 cells were
dispensed to upper chambers, suspended in DMEM (upper, 100 µl with
1% FBS; lower, 600 µl with 20% FBS). Folowing incubation (48 h),
the cells remaining in the upper chamber were retrieved via cotton
swabs. Cells on the lower membrane surface were fixed in 4%
paraformaldehyde and stained (Giemsa), and 5 microscopic fields
(magnification, ×200) were counted. All experiments were performed
in triplicate.
Statistical analysis
Categorical variables were assessed using the
Chi-square test, and ordinal variables were assessed using the
Mann-Whitney U test. The difference of continuous variables between
groups were compared with t-tests. The comparisons of paired
ordinal data were performed using the Wilcoxon signed-rank test.
The Kaplan-Meier method was used to calculate the disease-free and
overall survival of patients, and the log-rank test was used to
analyze the differences between groups. The Cox proportional
hazards regression model was applied for univariate and
multivariate analysis, and P<0.05 was considered to indicate a
statistically significant difference. All the statistical analyses
were conducted using IBM SPSS Statistics 20 (IBM Corp., Armonk, NY,
USA).
Results
PRDX2 is downregulated in HCC
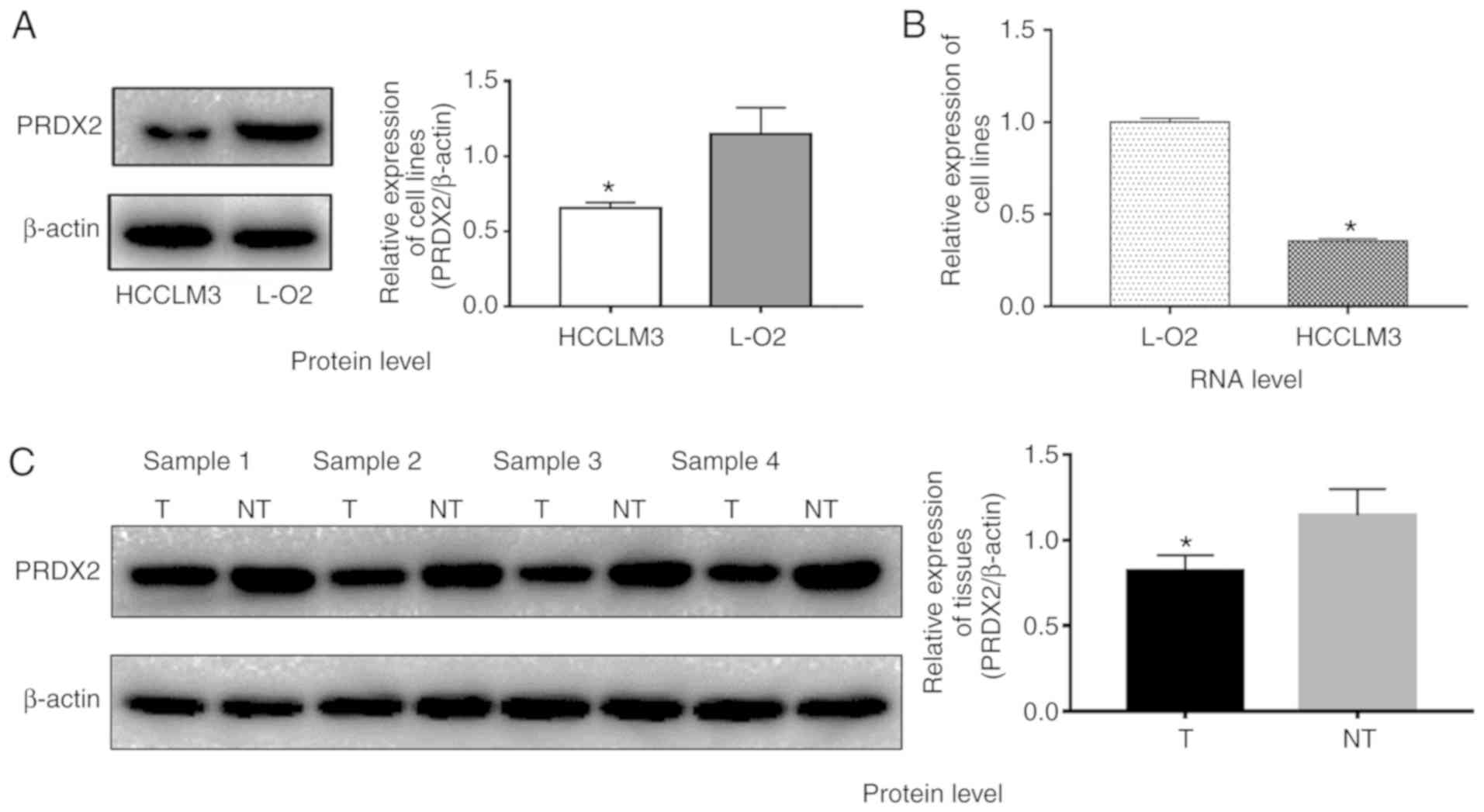
Due to the expression differences of PRDX2 at
mRNA and protein levels between HCC cell lines and normal liver
cell lines are not studied according to recently published studies
(17,23), to clarify this issue, western blot
and q-RT-PCR analyses were employed to investigate the PRDX2
expression levels in HCC cell line HCCLM3 and normal liver cell
line L-02. The results revealed that HCCLM3 cells expressed
relatively less PRDX2 at the protein level when compared to normal
liver cell line L-02 (Fig. 1A;
P<0.05). The PRDX2 mRNA level in HCCLM3 cells was much
lower than that of L-02 as well (Fig.
1B; P<0.05).
PRDX2 protein expression level is
downregulated in HCC tissues
Four paired HCC tissue samples and their matched
adjacent normal liver tissue samples were used to compare PRDX2
expression at the protein level by western blotting. As shown in
Fig. 1C, PRDX2 expression was
downregulated in all 4 HCC tissue samples compared to that of their
matched normal liver tissue samples (Fig. 1C; P<0.05), indicating
downregulation of PRDX2 may be a universal phenomenon in HCCs. To
validate this hypothesis, immunohistochemitry was applied on 2 sets
of tissue microarrays carrying a total of 176 paired samples. In
these paired cancer samples, 80.7% (142/176) of the normal tissues
exhibited strong staining (score 3); 10.8% (19/176) of the normal
tissues exhibited moderate staining (score 2); 8.5% (15/176) of the
normal liver tissues exhibited weak staining (score 1); none of the
normal liver tissues exhibited negative staining (score 0);
conversely, 5.7% (10/176) of the HCC tissues exhibited negative
staining (score 0); 35.2% (62/176) of the HCC tissues exhibited
weak staining (score 1); 47.7% (84/176) of the tumor tissues
exhibited moderate staining (score 2), and 11.4% (20/176) exhibited
strong staining (score 3) (Table
I). The Wilcoxon signed-rank test revealed that the PRDX2
staining index between HCC tissues and normal liver tissues was
significantly different (Table I;
P<0.05). Collectively, these results indicated that PRDX2
protein expression was frequently downregulated in HCC.
 | Table I.Difference of PRDX2 staining
intensity index between HCC tissues and normal liver tissues. |
Table I.
Difference of PRDX2 staining
intensity index between HCC tissues and normal liver tissues.
|
| Normal |
|
|---|
|
|
|
|
|---|
| HCC | Score 0 (N=0) | Score 1 (N=15) | Score 2 (N=19) | Score 3
(N=142) | P-value |
|---|
| Score 0 |
| (N=10) | 0 | 3 | 5 | 2 |
|
| Score 1 |
| (N=62) | 0 | 3 | 6 | 53 |
|
| Score 2 |
|
|
|
| <0.001 |
| (N=84) | 0 | 6 | 4 | 74 |
|
| Score 3 |
| (N=20) | 0 | 3 | 4 | 13 |
|
Association between PRDX2 expression
and the clinicopathological features of HCC patients
To investigate if the expression of PRDX2 was
associated with the clinicopathological features of HCC patients,
HCC patients were divided into 2 subgroups depending on their
relatively low or high PRDX2 expression levels. High PRDX2
expression was defined as a staining index score ≥4, and low PRDX2
expression was defined as a staining index <4 (Staining index =
staining intensity + tumor cell staining grade) (19,20)
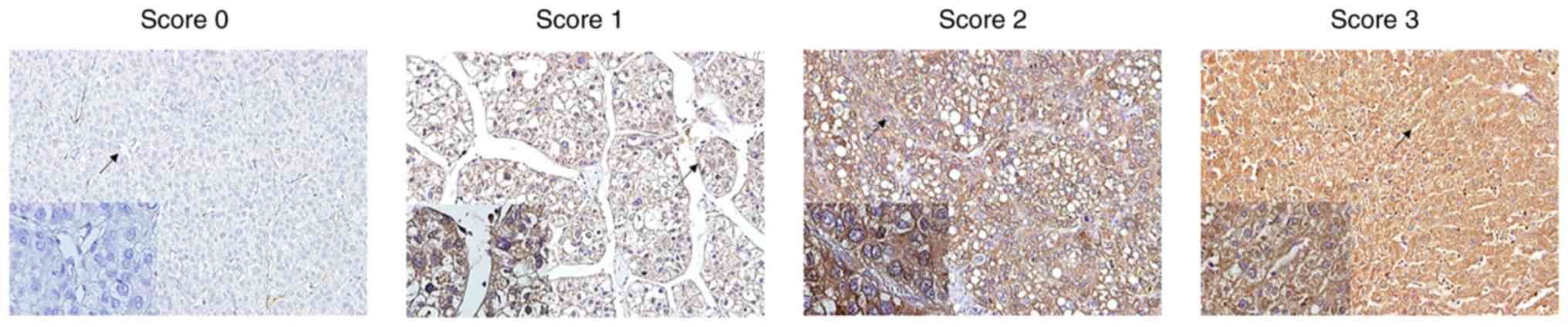
(Fig. 2). In addition, as observed
in Fig. 2, it was also clear that
PRDX2 expression was cytoplasmic. It was revealed that high PRDX2
expression was negatively associated with tumor size (P<0.001),
microvascular invasion (P<0.001), tumor encapsulation (P=0.047),
tumor differentiation (P=0.016), and TNM stage of HCC (P=0.015)
(Table II). However, no
significant association was observed between the expression level
of PRDX2 and the age of patients (P=0.865), sex (P=0.718), HBsAg
level (P=0.556), serum AFP level (P=0.487), liver cirrhosis
(P=0.417) or tumor number (P=0.665) (Table II).
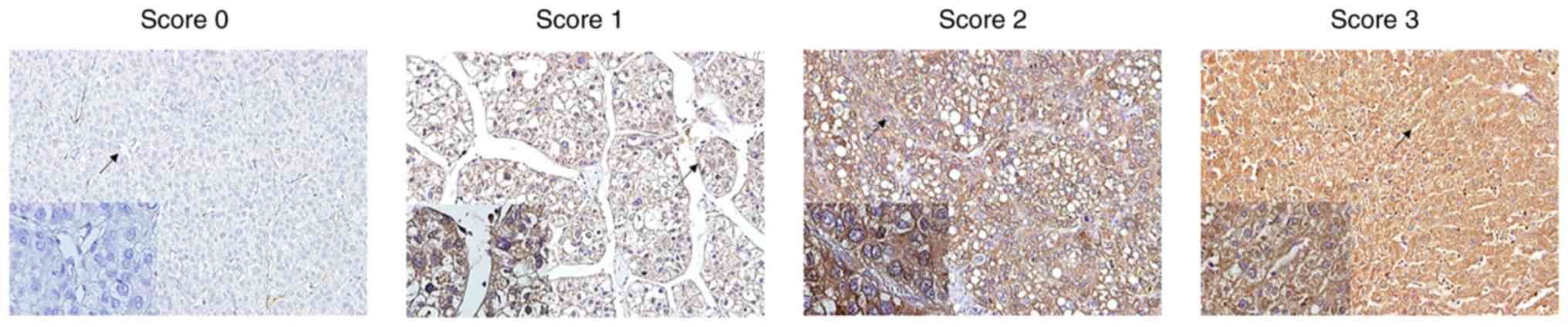 | Figure 2.PRDX2 immunostaining and staining
intensity index in HCC tissue spots illustrated by
immunohistochemistry. PRDX2 immunostaining score was defined as
follows: Score 0, negative; score 1, <30% positive cancer cells;
score 2, 30–50% positive cancer cells; score 3, 51–70% positive
cancer cells; and score 4, >70% positive cancer cells. The
staining intensity index was defined as 0, no color or extremely
weak; 1, light yellow; 2, light brown; or 3, brown. PRDX2,
peroxiredoxin2; HCC, hepatocellular carcinoma. |
 | Table II.Association between PRDX2 expression
and clinicopathologic characteristics of HCC patients. |
Table II.
Association between PRDX2 expression
and clinicopathologic characteristics of HCC patients.
|
|
| PRDX2
expression |
|
|---|
|
|
|
|
|
|---|
| Variables | No. | Low | High | P-value |
|---|
| No. | 176 | 72 | 104 |
|
| Age (years) |
|
|
| 0.865 |
|
≤50 | 72 | 30 | 42 |
|
|
>50 | 104 | 42 | 62 |
|
| Sex |
|
|
| 0.718 |
|
Male | 144 | 58 | 86 |
|
|
Female | 32 | 14 | 18 |
|
| HBsAg |
|
|
| 0.556 |
|
Negative | 26 | 12 | 14 |
|
|
Positive | 150 | 60 | 90 |
|
| AFP (ng/ml) |
|
|
| 0.487 |
|
≤20 | 54 | 20 | 34 |
|
|
>20 | 122 | 52 | 70 |
|
| Liver
cirrhosis |
|
|
| 0.417 |
| No | 24 | 8 | 16 |
|
|
Yes | 152 | 64 | 88 |
|
| Tumor size
(cm) |
|
|
|
<0.001a |
| ≤5 | 111 | 35 | 76 |
|
|
>5 | 65 | 37 | 28 |
|
| Tumor no. |
|
|
| 0.665 |
|
Single | 144 | 60 | 84 |
|
|
Multiple | 32 | 12 | 20 |
|
| Microvascular
invasion |
|
|
|
<0.001a |
| No | 72 | 16 | 56 |
|
|
Yes | 104 | 56 | 48 |
|
| Tumor
encapsulation |
|
|
| 0.047a |
|
None | 82 | 40 | 42 |
|
|
Complete | 94 | 32 | 62 |
|
| Tumor
differentiation |
|
|
| 0.016a |
|
Good | 116 | 40 | 76 |
|
|
Poor | 60 | 32 | 28 |
|
| TNM stage |
|
|
| 0.015a |
| T1 | 54 | 18 | 36 |
|
| T2 | 60 | 20 | 40 |
|
| T3 | 62 | 34 | 28 |
|
PRDX2 expression level is positively
associated with overall survival (OS) and disease-free survival
(DFS) of HCC patients
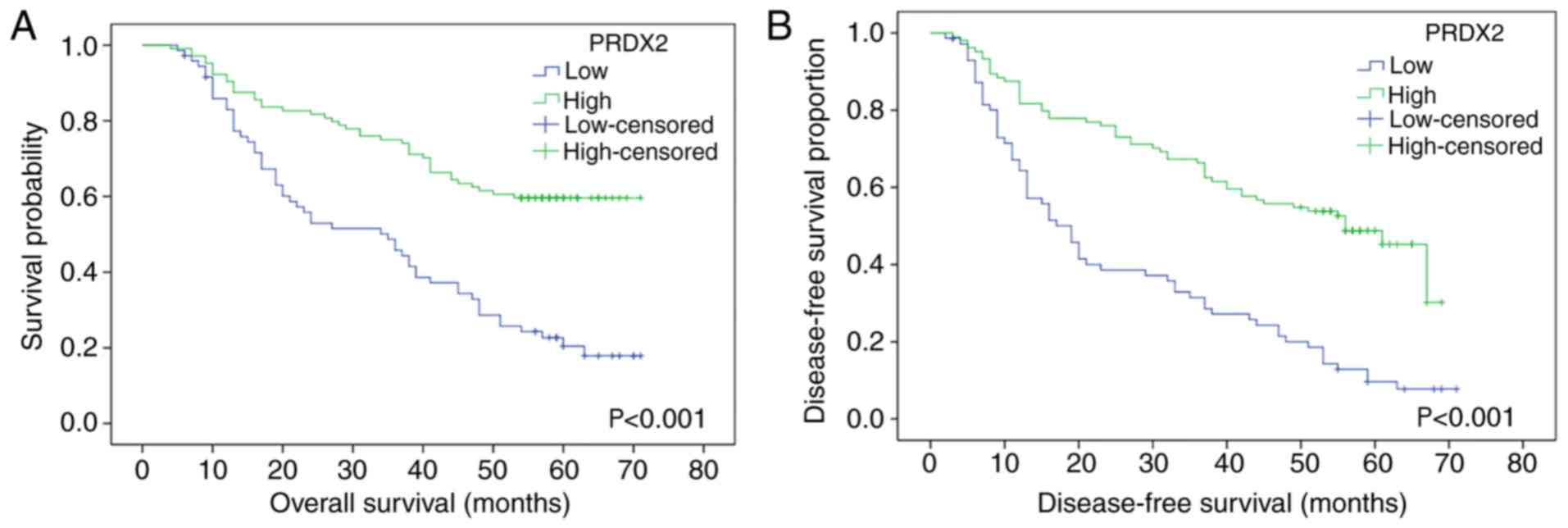
As revealed in Fig.
3, high expression of PRDX2 was associated with longer OS and
DFS times, while low PRDX2 expression revealed less OS and DFS
times. The log-rank test revealed the difference between the high
PRDX2 group and the low PRDX2 group in terms of the survival rate
of patients, and a statistical difference was revealed between
these 2 groups (for OS, P<0.001; for DFS, P<0.001,
respectively).
Univariate and multivariate analyses were performed
to further investigate whether PRDX2 was an independent prognostic
factor for HCC patients. When univariate analysis was applied, the
results indicated that the expression level of PRDX2 was associated
with both OS and DFS [hazard ratio (HR)=0.714, 95% CI, 0.624–0.817,
P<0.001; HR=0.711, 95% CI, 0.629–0.804, P<0.001,
respectively] (Tables III and
IV). The multivariate analysis was
then conducted to further evaluate all the significant variables.
The results revealed that the expression level of PRDX2 was an
independent prognostic factor for OS (HR=0.785, 95% CI,
0.680–0.905, P=0.001), as well as DFS (HR=0.809, 95% CI,
0.709–0.922, P=0.002), in addition to other variables (Tables III and IV).
 | Table III.Univariate and multivariate analyses
of prognostic factors for overall survival of HCC patients. |
Table III.
Univariate and multivariate analyses
of prognostic factors for overall survival of HCC patients.
|
| Univariate
analysis | Multivariate
analysis |
|---|
|
|
|
|
|---|
| Variable | HR (95% CI) | P-value | HR (95% CI) | P-value |
|---|
| Age (year, >50
vs. ≤50) | 1.000
(0.666–1.502) | 0.998 |
|
|
| Sex (female vs.
male) | 0.629
(0.357–1.108) | 0.109 |
|
|
| HBsAg (positive vs.
negative) | 0.771
(0.451–1.319) | 0.343 |
|
|
| AFP, ng/ml (>20
vs. ≤20) | 1.167
(0.753–1.810) | 0.489 |
|
|
| Liver cirrhosis
(yes vs. no) | 0.847
(0.480–1.493) | 0.565 |
|
|
| Tumor size (cm)
(>5 vs. ≤5) | 4.939
(3.262–7.478) | <0.00 | 2.719
(1.710–4.323) | <0.001 |
| Tumor no. (multiple
vs. single) | 1.459
(0.907–2.347) | 0.120 |
|
|
| Microvascular
invasion (with vs. without) | 7.409
(4.295–12.779) | <0.001 | 4.125
(2.238–7.602) | <0.001 |
| Tumor encapsulation
(complete vs. none) | 0.982
(0.660–1.460) | 0.927 |
|
|
| Tumor
differentiation (poor vs. good) | 0.929
(0.609–1.418) | 0.734 |
|
|
| TNM stage |
| T1 | 1.000 |
| 1.000 |
|
| T2 | 1.257
(0.667–2.368) | 0.479 | 1.452
(0.754–2.795) | 0.264 |
| T3 | 7.570
(4.265–13.439) | <0.001 | 4.266
(2.284–7.970) | <0.001 |
| PRDX2 (high vs.
low) | 0.714
(0.624–0.817) | <0.001 | 0.785
(0.680–0.905) | 0.001 |
 | Table IV.Univariate and multivariate analyses
of prognostic factors for disease-free survival of HCC
patients. |
Table IV.
Univariate and multivariate analyses
of prognostic factors for disease-free survival of HCC
patients.
|
| Univariate
analysis | Multivariate
analysis |
|---|
|
|
|
|
|---|
| Variable | HR (95% CI) | P-value | HR (95% CI) | P-value |
|---|
| Age (year, >50
vs. ≤50) | 0.991
(0.685–1.436) | 0.963 |
|
|
| Sex (female vs.
male) | 0.569
(0.336–0.965) | 0.036 | 0.478
(0.280–0.816) | 0.007 |
| HBsAg (positive vs.
negative) | 1.029
(0.607–1.746) | 0.914 |
|
|
| AFP, ng/ml (>20
vs. ≤20) | 1.354
(0.902–2.033) | 0.143 |
|
|
| Liver cirrhosis
(yes vs. no) | 0.948
(0.559–1.608) | 0.844 |
|
|
| Tumor size (cm)
(>5 vs. ≤5) | 3.463
(2.379–5.042) | <0.001 | 2.337
(1.540–3.547) | <0.001 |
| Tumor no. (multiple
vs. single) | 1.620
(1.059–2.479) | 0.026 | 0.990
(0.635–1.544) | 0.965 |
| Microvascular
invasion (yes vs. no) | 5.384
(3.450–8.404) | <0.001 | 3.146
(1.896–5.221) | <0.001 |
| Tumor encapsulation
(complete vs. none) | 0.831
(0.579–1.193) | 0.316 |
|
|
| Tumor
differentiation (poor vs. good) | 1.281
(0.881–1.863) | 0.194 |
|
|
| TNM stage |
| T1 | 1.000 |
|
|
|
| T2 | 0.799
(0.472–1.352) | 0.403 | 0.945
(0.547–1.634) | 0.840 |
| T3 | 4.969
(3.091–7.990) | <0.001 | 3.226
(1.933–5.384) | <0.001 |
| PRDX2 (high vs.
low) | 0.711
(0.629–0.804) | <0.001 | 0.809
(0.709–0.922) | 0.002 |
Collectively, these data indicated that the
expression level of PRDX2 could be used as an independent factor
for the prognosis of HCC patients.
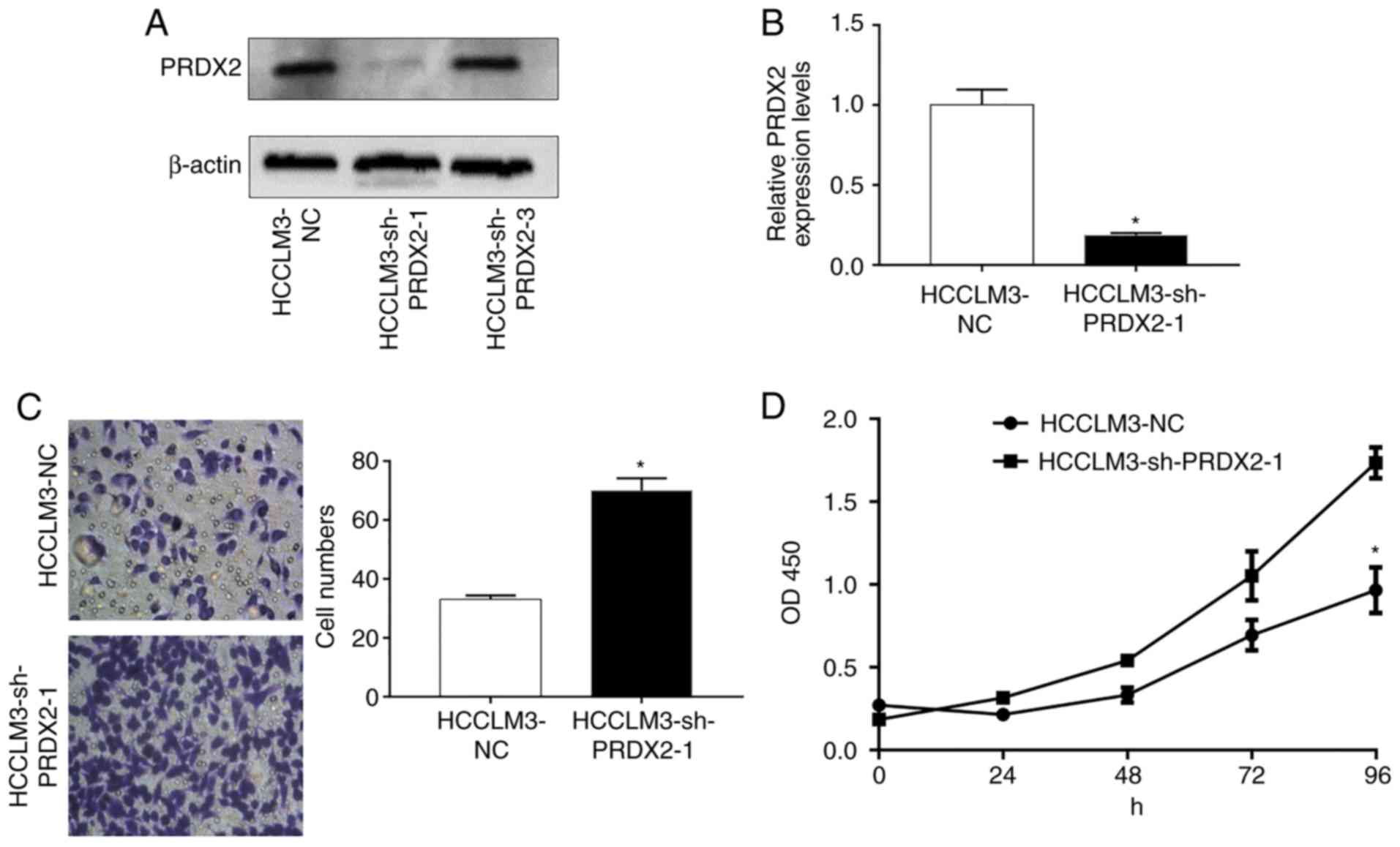
Silencing of PRDX2 in HCCLM3 promotes
cancer cell proliferation and migration
Since PRDX2 expression is usually downregulated in
HCC and is negatively associatedwith HCC progression, it was
hypothesized that PRDX2 inhibited HCC malignancies. To
assessthis hypothesis, stable cell lines whose PRDX2
expression was permanently inhibited in HCCLM3 were established
usinga lentiviral system (HCCLM3-shPRDX2) (Fig. 4A and B; P<0.05).
A Transwell assay was used to assess cell migration
ability after PRDX2 silencing. As revealed in Fig. 4C, silencing of PRDX2 in
HCCLM3 significantly promoted cancer cell migration ability
compared with that of lentiviral green fluorescent protein (GFP)
infected control cell (HCCLM3) (Fig.
4C; P<0.05).
Additionally, cell proliferation was also assessed
by counting the number of cells at the specific time-points
indicated, and as revealed in Fig.
4D (P<0.05) after PRDX2 was inhibited, HCCLM3
presented enhanced cell proliferation abilities.
Discussion
The roles thatPRDX2 has been revealed to play in
carcinogenesis have been described in emerging studies as a
‘dual-effect’ manner and its clinical importance as a prognostic
factor has started drawing increased attention from researchers in
recent years (24). The role of
PRDX2 as a tumor promoter is supported by mounting evidence in
recent years (25), particularly,
it is currently well established in colorectal cancers. According
to Lu et al, it was determinedthat PRDX2 had higher
expression levels in colorectal cancer tissues when compared with
their matched adjacent normal mucosa tissues, and PRDX2 expression
was positively linked to cancer metastasis and TNM stage by
downregulating oxidation-induced cancer cell apoptosis (26). In another related study, it was
indicated that PRDX2 silencing in colorectal cancer cell
lines resulted in elevated cancer cell apoptosis and increased
endogenous ROS production, further leading to Wnt signaling
pathway-associated protein alterations (27). It has also been reported that a high
PRDX2 expression level was associated with tumor progression and
poor survival in colorectal cancer patients (28). Silencing of PRDX2 was
revealed to increase sensitivity of colorectal cancer cells to 5-FU
treatment by suppressing the PI3K/AKT signaling pathway (29). Cruz et al also demonstrated
that PRDX2 was involved in cancer cell resistance to bortezomib,
paclitaxel, and carboplatin in ovarian cancer (30). According to Diao et al, PRDX2
may serve as a downstream target of microRNA-122a, which was found
to be significantly downregulated in HCC and may possess a
tumor-inhibiting effect (23); Zhou
et al determined that PRDX2 downregulation increased
H2O2-induced HCC cell death, thus concluding
that PRDX2 is a tumor promoter in HCC (17). In contrast, evidence to support the
notion that PRDX2 possesses tumor-inhibiting ability is emerging.
In a study published in 2013, Lee et al revealed that in
metastatic melanoma, PRDX2 downregulation resulted in
increased proliferative and migratory activities of tumor cells,
and this tumor-inhibiting effect was mediated by PRDX2 by promoting
ERK-dependent E-cadherin expression and the Src-dependent retention
of β-catenin in the adherens junctions (31). Moreover, another study revealed that
in colon cancer cells, PRDX2 inhibited TGFβ1-induced
epithelial-mesenchymal transition (EMT) and reduced the invasive
phenotype by modulating downstream transcription factors, such as
Twist1, Snail, ZEB1 and ZEB2 (32).
Thus, as revealed by all this evidence, the function of PRDX2 in
cancer progression remains controversial.
The reason for thismay not only be partially
attributed to different experimental methods and materials adopted
but also, much more importantly, to the underlying mechanism of how
PRDX2 affects redox balancing which is complicated and has not been
fully elucidated by currently known studies (33). Not to mention the multiple roles
that ROS plays during cancer development (11,34),
which have been proposed to both accelerate and delay cancer
initiation and progression (35),
orthe clinical trials clouded by the failure of oral antioxidant
administration in the treatment of several types of cancer, such as
in human skin cancer and mice lung cancer models (36–39),
which was substantiated by the results from a significant vitamin E
randomized clinical trial, namely the Selenium and Vitamin E Cancer
Prevention Trial (SELECT), by revealingthat α-tocopherol
supplementation increased prostate cancer incidence (40). In addition, the decreased
PRDX2 level in HCC cells may weaken ROS scavenging, thus
resulting in intensified oxidative stress, which was believed to
play a pivotal role in non-oncogene addiction (41).
However, the clinical importance and function of
PRDX2 in HCC has not been comprehensively studied. A previous study
conducted in our laboratory illustrated upregulation of PRDX2 in
poorly differentiated HCC tissues by proteomic approaches and
indicated the involvement of PRDX2 in HCC progression (18). Notably, in our present study, our
results revealed the protein expression levels of PRDX2 in HCC
tissues were relatively lower than that of their adjacent normal
liver tissues, not only in all 4 matched tissue specimens, but also
in the protein microarrays which were comprised of 176 paired
tissue spots. These results were consistent with our results
obtained from western blotting and q-RT-PCR experiments applied in
an HCC cell line. Furthermore, there were statistically significant
differences between HCC patients who had high PRDX2 expression
levels and those who had low expression levels in terms of OS and
DFS of patients. Moreover, the hypothesis that PRDX2 possesses
prognostic value was further supported by the result that PRDX2 was
an independent prognostic factor in HCC patients. Data from
experiments in cell lines favor the concept that PRDX2 could serve
not only as a prognostic marker but also as a therapeutic target
for treatment since silencing of PRDX2 promoted cancer cell
proliferation and migration. Further experiments are required to
reveal the underlying signaling mechanism to support the potential
pharmaceutical value of PRDX2.
Collectively, our findings revealed that the
expression level of PRDX2 was positively linked to the OS and DFS
of HCC patients. It was also revealed that PRDX2 was an independent
prognostic indicator. PRDX2 could serve as a useful biomarker for
the prognosis of HCC patients.
Acknowledgements
Not applicable.
Funding
The present study was supported by the National
Natural Science Foundation of China (grant nos. 31570509, 81702326
and 81872036), the Science and Technology Major Project of Gansu
Province (grant no. 1602FKDA001), the Natural Science Foundation of
Gansu Province (grant no. 17JR5RA187), the Gansu Provincial
Administration of Traditional Chinese Medicine (grant no.
GZK-2015-69), the Gansu Province Science Foundation for Youths
(grant no. 17JR5RA259), the Provincial Youth Science and Technology
Foundation of Gansu (grant nos. 1606RJYA276 and17JR5RA259), the
Talent Innovation and Entrepreneurship Program of Lanzhou City
(grant no. 2016-RC-57), the Science and Technology Project of
Chenguan District (grant no. 2017SHFZ0014) and the Foundation of
the First Hospital of Lanzhou University (grant nos. LDYYYN
2017-04, LDYYYN 2017-02 and LDYYYN 2015-01).
Availability of data and materials
The datasets used during the present study are
available from the corresponding author upon reasonable
request.
Authors' contributions
XL was the designer and the principal investigator
(PI) of the present study. BB performed the major clinical and
experimental data collection, the statistical analysis, the
immunohistochemistry experiments and the cell function experiments,
and also writing of the present study (in English). YL also
performed the data collection, the statistical analysis, the
immunohistochemistry experiments and the cell function experiments.
JH performed the Transwell experiments. HW performed the
statistical analysis. LL performed the CCK-8 experiments. SZ
analyzed the correlation between the patients' clinicopathological
variables and PRDX2 expression. JZ performed the western blot
experiments and the image processing. WM performed the lentivirus
transfection experiments. PY the performed cell culture and the
mRNA and protein extraction. ZB performed the PCR experiments. All
authors read and approved the manuscript and agree to be
accountable for all aspects of the research in ensuring that the
accuracy or integrity of any part of the work are appropriately
investigated and resolved.
Ethics approval and consent to
participate
The present study does not contain any studies with
animals performed by any of the authors. The present study was
approved by the Ethics Committee on human research of the First
Affiliated Hospital of Lanzhou University (Approval no.
LDYYLL-2010-56). Informed and written consents were obtained from
the patients or their relatives for the use of these clinical
materials for research, which were performed in accordance with the
Declaration of Helsinki of the World Medical Association.
Patient consent for publication
Not applicable.
Competing interests
The authors state that they have no competing
interests.
References
|
1
|
Dhanasekaran R, Limaye A and Cabrera R:
Hepatocellular carcinoma: Current trends in worldwide epidemiology,
risk factors, diagnosis, and therapeutics. Hepat Med. 4:19–37.
2012.PubMed/NCBI
|
|
2
|
Siegel RL, Miller KD and Jemal A: Cancer
statistics, 2017. CA Cancer J Clin. 67:7–30. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Chen W, Zheng R, Baade PD, Zhang S, Zeng
H, Bray F, Jemal A, Yu XQ and He J: Cancer statistics in China,
2015. CA Cancer J Clin. 66:115–132. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ikeda M, Morizane C, Ueno M, Okusaka T,
Ishii H and Furuse J: Chemotherapy for hepatocellular carcinoma:
Current status and future perspectives. J Clin Oncol. 48:103–114.
2018.
|
|
5
|
Behne T and Copur MS: Biomarkers for
hepatocellular carcinoma. Int J Hepatol 2012. 8590762012.
|
|
6
|
Zhao Y, Gao Q, Pei L, Wang C, Jin L and
Liao F: Current status and future prospects of biomarkers in the
diagnosis of hepatocellular carcinoma. Int J Biol Markers.
32:e361–e369. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Heimbach JK: Overview of the updated AASLD
guidelines for the management of HCC. Gastroenterol Hepatol.
13:751–753. 2017.
|
|
8
|
Bryk R, Griffin P and Nathan C:
Peroxynitrite reductase activity of bacterial peroxiredoxins.
Nature. 407:211–215. 2000. View
Article : Google Scholar : PubMed/NCBI
|
|
9
|
Hillas PJ, del Alba FS, Oyarzabal J, Wilks
A and Ortiz De Montellano PR: The AhpC and AhpD antioxidant defense
system of mycobacterium tuberculosis. J Biol Chem. 275:18801–18809.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Trachootham D, Alexandre J and Huang P:
Targeting cancer cells by ROS-mediated mechanisms: A radical
therapeutic approach? Nat Rev Drug Discov. 8:579–591. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Gorrini C, Harris IS and Mak TW:
Modulation of oxidative stress as an anticancer strategy. Nat Rev
Drug Discov. 12:931–947. 2013. View
Article : Google Scholar : PubMed/NCBI
|
|
12
|
Zhang S, Fu Z, Wei J, Guo J, Liu M and Du
K: Peroxiredoxin 2 is involved in vasculogenic mimicry formation by
targeting VEGFR2 activation in colorectal cancer. Med Oncol.
32:4142015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Duan T, Fan K, Chen S, Yao Q, Zeng R, Hong
Z, Peng L, Shao Y and Yao B: Role of peroxiredoxin 2 in
H2O2-induced oxidative stress of primary
leydig cells. Mol Med Rep. 13:4807–4813. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Stresing V, Baltziskueta E, Rubio N,
Blanco J, Arriba MC, Valls J, Janier M, Clézardin P, Sanz-Pamplona
R, Nieva C, et al: Peroxiredoxin 2 specifically regulates the
oxidative and metabolic stress response of human metastatic breast
cancer cells in lungs. Oncogene. 32:724–735. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Wang R, Wei J, Zhang S, Wu X, Guo J, Liu
M, Du K, Xu J, Peng L, Lv Z, et al: Peroxiredoxin 2 is essential
for maintaining cancer stem cell-like phenotype through activation
of hedgehog signaling pathway in colon cancer. Oncotarget.
7:86816–86828. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kalinina EV, Berezov TT, Shtil' AA,
Chernov NN, Glazunova VA, Novichkova MD and Nurmuradov NK:
Expression of peroxiredoxin 1, 2, 3, and 6 genes in cancer cells
during drug resistance formation. Bull Exp Biol Med. 153:878–881.
2012.(In English, Russian). View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Zhou S, Han Q, Wang R, Li X, Wang Q, Wang
H, Wang J and Ma Y: PRDX2 protects hepatocellular carcinoma
SMMC-7721 cells from oxidative stress. Oncol Lett. 12:2217–2221.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Zhao S, Su G, Yang W, Yue P, Bai B, Lin Y,
Zhang J, Ba Y, Luo Z, Liu X, et al: Identification and comparison
of differentiation-related proteins in hepatocellular carcinoma
tissues by proteomics. Technol Cancer Res Treat. 16:1092–1101.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Zhou SL, Hu ZQ, Zhou ZJ, Dai Z, Wang Z,
Cao Y, Fan J, Huang XW and Zhou J: miR-28-5p-IL-34-macrophage
feedback loop modulates hepatocellular carcinoma metastasis.
Hepatology. 63:1560–1575. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Wu J, Lu Y, Qin A, Qiao Z and Jiang X:
Overexpression of RAB34 correlates with poor prognosis and tumor
progression in hepatocellular carcinoma. Oncol Rep. 38:2967–2974.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2ΔΔCT method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Dong H, Zhu G, Tamada K, Flies DB, van
Deursen JM and Chen L: B7-H1 determines accumulation and deletion
of intrahepatic CD8+ T lymphocytes. Immunity.
20:327–336. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Diao S, Zhang JF, Wang H, He ML, Lin MC,
Chen Y and Kung HF: Proteomic identification of microRNA-122a
target proteins in hepatocellular carcinoma. Proteomics.
10:3723–3731. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Nicolussi A, D'Inzeo S, Capalbo C,
Giannini G and Coppa A: The role of peroxiredoxins in cancer. Mol
Clin Oncol. 6:139–153. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Park MH, Jo M, Kim YR, Lee CK and Hong JT:
Roles of peroxiredoxins in cancer, neurodegenerative diseases and
inflammatory diseases. Pharmacol Ther. 163:1–23. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Lu W, Fu Z, Wang H, Feng J, Wei J and Guo
J: Peroxiredoxin 2 is upregulated in colorectal cancer and
contributes to colorectal cancer cells' survival by protecting
cells from oxidative stress. Mol Cell Biochem. 387:261–270. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Lu W, Fu Z, Wang H, Feng J, Wei J and Guo
J: Peroxiredoxin 2 knockdown by RNA interference inhibits the
growth of colorectal cancer cells by downregulating Wnt/β-catenin
signaling. Cancer Lett. 343:190–199. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Peng L, Wang R, Shang J, Xiong Y and Fu Z:
Peroxiredoxin 2 is associated with colorectal cancer progression
and poor survival of patients. Oncotarget. 8:15057–15070.
2017.PubMed/NCBI
|
|
29
|
Xu J, Zhang S, Wang R, Wu X, Zeng L and Fu
Z: Knockdown of PRDX2 sensitizes colon cancer cells to 5-FU by
suppressing the PI3K/AKT signaling pathway. Biosci Rep.
37:BSR201604472017. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Cruz G, Fernandois D and Paredes AH:
Ovarian function and reproductive senescence in the rat: Role of
ovarian sympathetic innervation. Reproduction. 153:R59–R68. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Lee DJ, Kang DH, Choi M, Choi YJ, Lee JY,
Park JH, Park YJ, Lee KW and Kang SW: Peroxiredoxin-2 represses
melanoma metastasis by increasing E-Cadherin/β-Catenin complexes in
adherens junctions. Cancer Res. 73:4744–4757. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Feng J, Fu Z, Guo J, Lu W, Wen K, Chen W,
Wang H, Wei J and Zhang S: Overexpression of peroxiredoxin 2
inhibits TGF-β1-induced epithelial-mesenchymal transition and cell
migration in colorectal cancer. Mol Med Rep. 10:867–873. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Neumann CA and Fang Q: Are peroxiredoxins
tumor suppressors? Curr Opin Pharmacol. 7:375–380. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Poprac P, Jomova K, Simunkova M, Kollar V,
Rhodes CJ and Valko M: Targeting free radicals in oxidative
stress-related human diseases. Trends Pharmacol Sci. 38:592–607.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Chandel NS and Tuveson DA: The promise and
perils of antioxidants for cancer patients. N Engl J Med.
371:177–178. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Miller ER III, Pastor-Barriuso R, Dalal D,
Riemersma RA, Appel LJ and Guallar E: Meta-analysis: High-dosage
vitamin E supplementation may increase all-cause mortality. Ann
Intern Med. 142:37–46. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Chen CS and Wells PG: Enhanced
tumorigenesis in p53 knockout mice exposed in utero to high-dose
vitamin E. Carcinogenesis. 27:1358–1368. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Hercberg S, Ezzedine K, Guinot C, Preziosi
P, Galan P, Bertrais S, Estaquio C, Briançon S, Favier A, Latreille
J, et al: Antioxidant supplementation increases the risk of skin
cancers in women but not in men. J Nutr. 137:2098–2105. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Sayin VI, Ibrahim MX, Larsson E, Nilsson
JA, Lindahl P and Bergo MO: Antioxidants accelerate lung cancer
progression in mice. Sci Transl Med. 6:221ra152014. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Klein EA, Thompson IM Jr, Tangen CM,
Crowley JJ, Lucia MS, Goodman PJ, Minasian LM, Ford LG, Parnes HL,
Gaziano JM, et al: Vitamin E and the risk of prostate cancer: The
selenium and vitamin E cancer prevention trial (SELECT). JAMA.
306:1549–1556. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Luo J, Solimini NL and Elledge SJ:
Principles of cancer therapy: Oncogene and non-oncogene addiction.
Cell. 136:823–837. 2009. View Article : Google Scholar : PubMed/NCBI
|