Introduction
As the leading cause of cancer mortality, lung
cancer accounts for 18.2% of total cancer deaths worldwide
(1). Furthermore, ~80% of patients
with lung cancer patients have non-small-cell lung cancer (NSCLC).
The incidence of NSCLC has increased in women during the last two
decades worldwide (2). It has been
reported that the 5-year survival rate of NSCLC is <15%
(3). Surgical resection,
conventional chemotherapy and radiotherapy are widely used for the
clinical treatment of patients with NSCLC (4).
During the course of treatment, one-half of all
patients with NSCLC patients undergo radiotherapy (5). It has been reported that early-stage
patients can benefit from stereotactic body radiation therapy
(6). Stereotactic body radiation
therapy has been used as a standard care modality in medically
inoperable patients with early-stage NSCLC (7). However, previous studies have
indicated that the outcome of radiotherapy alone is not always
satisfactory (8), which may be due
to the development of radiotherapy resistance (9,10).
Moreover, laboratory and clinical data indicated that radiotherapy
may cause clinical adverse effects for patients with NSCLC. For
example, radiotherapy can increase tumor invasion and metastasis by
upregulating TGFβ-1 expression (11). Cancer cells treated with radiation
acquire mesenchymal-like morphology (12). X-ray irradiation can also increase
the invasion of NSCLC cells (13).
In addition, radiation can stimulate the malignancy of residual,
incompletely treated and viable tumors surrounding the treatment
zone (14,15). Thus, understanding the mechanisms
involved in radiation-induced malignancy in NSCLC cells is needed
in order to improve the therapeutic efficacy of radiotherapy.
Cytokines, such as visfatin, are involved in the
progression of NSCLC (16). It has
been reported that visfatin mediates doxorubicin (Dox) resistance
of human NSCLC cells through Akt-mediated upregulation of
ATP-binding cassette subfamily C member 1 (17). Furthermore, visfatin triggers cell
motility of NSCLC cells by increasing the expression of matrix
metalloproteinases (MMPs) (18).
Targeted inhibition of visfatin has been proposed as a potential
therapeutic approach for NSCLC treatment (19). Visfatin is a cytokine synthesized
and released by adipocytes and inflammatory cells (20). Its expression can also be induced
during radiation therapy in cancer tissues (21,22).
However, whether visfatin is involved in radiation-induced
malignancy of NSCLC remains unknown.
Epithelial-mesenchymal transition (EMT) is the first
step of tumor metastasis (23) and
is critical to the progression and metastasis of NSCLC (24). During EMT, transcription factors,
such as Snail, can bind to the E-box motif of the E-cadherin
(E-Cad) gene promoter and inhibit its expression (25,26).
In a previous study, high protein expression of Snail is detectable
in 21% of NSCLC samples (27). The
levels of Snail are associated with poor prognosis in patients with
NSCLC (28). It has been reported
that the protein expression of Snail is essential for EMT induction
in NSCLC cells (29). In the
present study, the expression levels of cytokines, such as IL-6,
IL-8, IL-10, VEGFA, TGF-β, TNF-α and visfatin were examined in
NSCLC cell lines treated with radiation. Further, the potential
roles and mechanisms of visfatin in radiation-induced migration and
invasion of NSCLC cells were investigated.
Materials and methods
Cell culture and radiation
treatment
The human NSCLC A549 and H1299 cell lines and human
bronchial epithelial cells (HBEpC) were purchased from American
Type Culture Collection and maintained in DMEM (Invitrogen; Thermo
Fisher Scientific, Inc.) supplemented with 10% FBS (Gibco; Thermo
Fisher Scientific, Inc.), penicillin and streptomycin at 37°C in 5%
CO2. Mycoplasma contamination was monitored
weekly during experiments. Radiation treatment was conducted
according to a previous study (30). Briefly, 5×105 cells/well
were seeded in a 6-well plate and were irradiated at room
temperature using a 6 MV X-ray linear accelerator (Varian 23Ex;
Varian Inc.) at a dose rate of 300 cGy/min for the time required to
apply the dose used in each assay. In order to determine the role
of visfatin, anti-visfatin neutralizing antibody (100 ng/ml) or
recombinant-visfatin (rVisfatin;100 ng/ml) were added into culture
medium for 24 h at 37°C in 5% CO2, then irradiated at
room temperature.
Reagents
Scramble negative control (NC) microRNA (miR,
5′-UUCUCCGAACGUGUCACGUTT-3′), miR-34a inhibitor
(5′-AAGCUCCAUUUCGCAACCUUAC-3′), small interfering RNA (siRNA) NC
(si-NC; 5′-GCACAACAAGCCGAAUACA-3′) and siRNA targeting Snail
(5′-CAUCCGAAGCCACACGCUG-3′) were purchased from Sigma-Aldrich;
Merck KGaA. The neutralizing antibody specific for visfatin
(anti-Visfatin; cat. no. A300-778A) and recombinant visfatin (cat.
no. RP-75758) were obtained from Invitrogen; Thermo Fisher
Scientific, Inc.
Wound healing and Transwell Matrigel™
assay
Cells (1.5×106 cells per well) were
plated in 12-well plates and cultured to 80% confluence in complete
medium. The cell layer was scratched with a 200 µl pipette tip,
washed twice with PBS, then cultured with medium containing 0.5%
FBS, with or without the indicated treatments, as described in
Figure legends. The migration distance was recorded in the same
visual fields under a phase-contrast microscope. The relative
migration rate was calculated according to a previous study
(31), using the following formula:
[(scratch area at 0 h-scratch area at 48 h)/scratch area at 0 h] ×
100%.
Cell invasion was assessed using a Transwell
Matrigel invasion chamber (8-µm pore filters; Corning, Inc.)
according to the manufacturer's instructions. A total of
2×105 cells was seeded into the upper chamber of a
24-well chamber with FBS-free medium. The bottom chamber received
0.6 ml complete medium. After the indicated treatment and culture
for 24 h, the invading cells were fixed using methanol for 15 min
at room temperature, dried under a laminar flow safety cabinet,
stained with 0.5% crystal violet (Sigma-Aldrich; Merck KGaA) for 2
h at room temperature, then observed under an inverted optical
microscope. The number of invading cells in five randomly selected
fields of view was quantified using ImageJ software version 1.47
(National Institutes of Health). The relative invasion rate was
calculated by dividing the number of stained cells by the number of
stained cells in the control group.
Reverse transcription-quantitative
(RT-q) PCR analysis
Total RNA was isolated using TRIzol®
reagent (Invitrogen; Thermo Fisher Scientific, Inc.). cDNA was
generated by using the PrimeScript RT reagent kit with gDNA Eraser
(Takara Biotechnology Co., Ltd.) for mRNA at 37°C for 15 min, or
the qScript microRNA cDNA synthesis kit (Quantabio) for miRNA at
37°C for 60 min followed by 5 min at 70°C, respectively. For mRNA
targets, qPCR was conducted using a SYBR-Green PCR Kit (Qiagen
GmbH) on the Step-One Plus Real-Time PCR System (Applied
Biosystems, Inc.). The thermocycling conditions consisted of an
initial denaturation at 95°C for 5 min, followed by 50 cycles at
95°C for 15 sec and 60°C for 30 sec. The primer sequences were as
follows: i) IL-6 forward, 5′-CCTCCAGAACAGATTTGAGAGTAGT-3′ and
reverse, 5′-GGGTCAGGGGTGGTTATTGC-3′; ii) IL-8 forward,
5′-GAGAGTGATTGAGAGTGGACCAC-3′ and reverse,
5′-CACAACCCTCTGCACCCAGTTT-3′; iii) IL-10 forward,
5′-GTGGCATTCAAGGAGTACCTC-3′ and reverse,
5′-TGATGGCCTTCGATTCTGGATT-3′; iv) VEGFA forward,
5′-TACCTCCACCATGCCAAGTGGT-3′ and reverse,
5′-AGGACGGCTTGAAGATGTAC-3′; v) TGF-β forward,
5′-GGCCAGATCCTGTCCAAGC-3′ and reverse, 5′-GTGGGTTTCCACCATTAGCAC-3′;
vi) TNF-α forward, 5′-CCTCTCTCTAATCAGCCCTCTG-3′ and reverse,
5′-GAGGACCTGGGAGTAGATGAG-3′; vii) visfatin forward,
5′-AGGGTTACAAGTTGCTGCCACC-3′ and reverse,
5′-CTCCACCAGAACCGAAGGCAAT-3′; viii) Snail forward,
5′-GACCACTATGCCGCGCTCTT-3′ and reverse,
5′-TCGCTGTAGTTAGGCTTCCGATT-3′; ix) Slug forward,
5′-AGCAGTTGCACTGTGATGCC-3′ and reverse, 5′-ACACAGCAGCCAGATTCCTC-3′;
x) Twist forward, 5′-CGGACAAGCTGAGCAAGATT-3′ and reverse,
5′-CCTTCTCTGGAAACAATGAC-3′; xi) Zeb1 forward,
5′-GCACCTGAAGAGGACCAGAG-3′ and reverse, 5′-TGCATCTGGTGTTCCATTTT-3′;
xii) GAPDH forward, 5′-GTCAACGGATTTGGTCTGTATT-3′ and reverse,
5′-AGTCTTCTGGGTGGCAGTGAT-3′.
For miR targets (miR-137, miR-34a, miR-153 and
miR-22), qPCRs were performed using the NCode miRNA qRT-PCR
analysis kit (Invitrogen; Thermo Fisher Scientific, Inc.). The
thermocycling conditions included an initial denaturation at 95°C
for 3 min followed by 40 cycles at 95°C for 15 sec and 60°C for 30
sec. The forward primer is the exact sequence of the mature miRNA.
The forward primer for U6 was 5′-TGCGGGTGCTCGCTTCGCAGC-3′. Gene
expression levels were calculated using the 2−ΔΔCq
method (32) and standardized to
GAPDH and U6 for mRNA and miR targets, respectively. All RT-qPCR
reactions were performed three times.
Western blot analysis
Cells were lysed using RIPA buffer (Beyotime
Institute of Biotechnology) and protein extracts were collected.
Protein concentration was measured using a BCA Protein Assay Kit
(Pierce™; Thermo Fisher Scientific, Inc.). After denaturation in
boiling water for 10 min, proteins (20 µg per lane) were separated
by SDS-PAGE on 10% gels, then transferred to PVDF membranes. The
membranes were blocked with 5% skimmed milk at room temperature for
2 h, and then incubated with primary antibodies at 4°C for at least
15 h. The primary antibodies used were specific for GAPDH (cat. no.
ab9485; Abcam; 1:1,000), E-Cad (cat. no. 14472S; Cell Signaling
Technology, Inc.; 1:1,000) and Snail (cat. no. ab82846; Abcam;
1:1,000). Membranes were incubated with HRP-conjugated secondary
antibodies (cat. no. ab7090; Abcam; 1:10,000 dilution) for 90 min
at 25°C. The protein were visualized using RapidStep™ ECL detection
reagent (EMD Millipore) in a GeneGnome XRQ Chemiluminescence
Imaging System (Syngene). The gray values were analyzed using the
ImageJ software (version 1.46; National Institutes of Health).
GAPDH primary antibody was used as a control.
ELISA
The levels of visfatin in culture medium were
measured using the Nampt/Visfatin human ELISA kit (cat. no.
RAG004R; BioVendor R&D) according to the manufacturer's
instructions. The absorbance was measured at 450 nm using a
microplate reader (BioTek Instruments, Inc.)
Protein and mRNA stability assay
Protein and mRNA stability was evaluated as
previously reported (33,34). Briefly, cells were treated with 10
µg/ml cycloheximide (CHX; Sigma-Aldrich; Merck KGaA) or 5 µg/ml
actinomycin-D (Act-D; Sigma-Aldrich; Merck KGaA) for the indicated
time periods. mRNA and protein expression levels were measured by
RT-qPCR and western blot analysis, respectively.
Dual luciferase reporter assay
Dual luciferase reporter assays were carried out as
described previously (35).
Briefly, the wild-type (WT) Snail 3-unstranslated region (3′-UTR)
luciferase vector containing the putative binding site for miR-34a
was purchased from OriGene Technologies, Inc., then mutated using
the QuickChange Mutagenesis kit (Stratagene) to produce the mutant
(MUT) Snail 3′-UTR construct. Both WT and mutant Snail 3′-UTR were
subcloned into the pmiR-GLO plasmid (Promega Corporation). A549
cells in 96-well plate (5×103 cells/well) were
transfected with the pmiR-GLO-WT or pmiR-GLO-Mut, together with
scramble control or miR-34a inhibitor for 24 h. The activity was
measured immediately at the end of the transfection period.
Luciferase activity was analyzed as previously reported (35) using the Dual-Luciferase®
Reporter Assay system (Promega Corporation). The Firefly luciferase
activity was normalized to Renilla luciferase activity.
Cell transfection
All miRNA mimics, inhibitors, siRNAs and the
respective negative control were transfected using
Lipofectamine® 2000 (Invitrogen; Thermo Fisher
scientific, Inc.) according to the manufacturer's protocol at
concentration of 10 nmol/l in transfection medium (αMEM with 10%
fetal calf serum, both from Thermo Fisher Scientific, Inc.).
Briefly, cells were cultured to 50–60% confluence. The culture
medium was then replaced with transfection medium. After incubation
with RNA oligonucleotides for 6 h, the transfection medium was
replaced with full medium, and the cells were incubated for another
24 or 48 h before harvest.
Statistical analysis
Data are presented as the mean ± SD of three
independent experiments and analyzed using SPSS 20 (IBM Corp.).
Differences between two experimental groups were assessed using
unpaired Student's t-test (two-tailed). One-way ANOVA followed by
Tukey's post hoc test was used when making pairwise comparisons
among ≥3 groups. P<0.05 was considered to indicate a
statistically significant difference.
Results
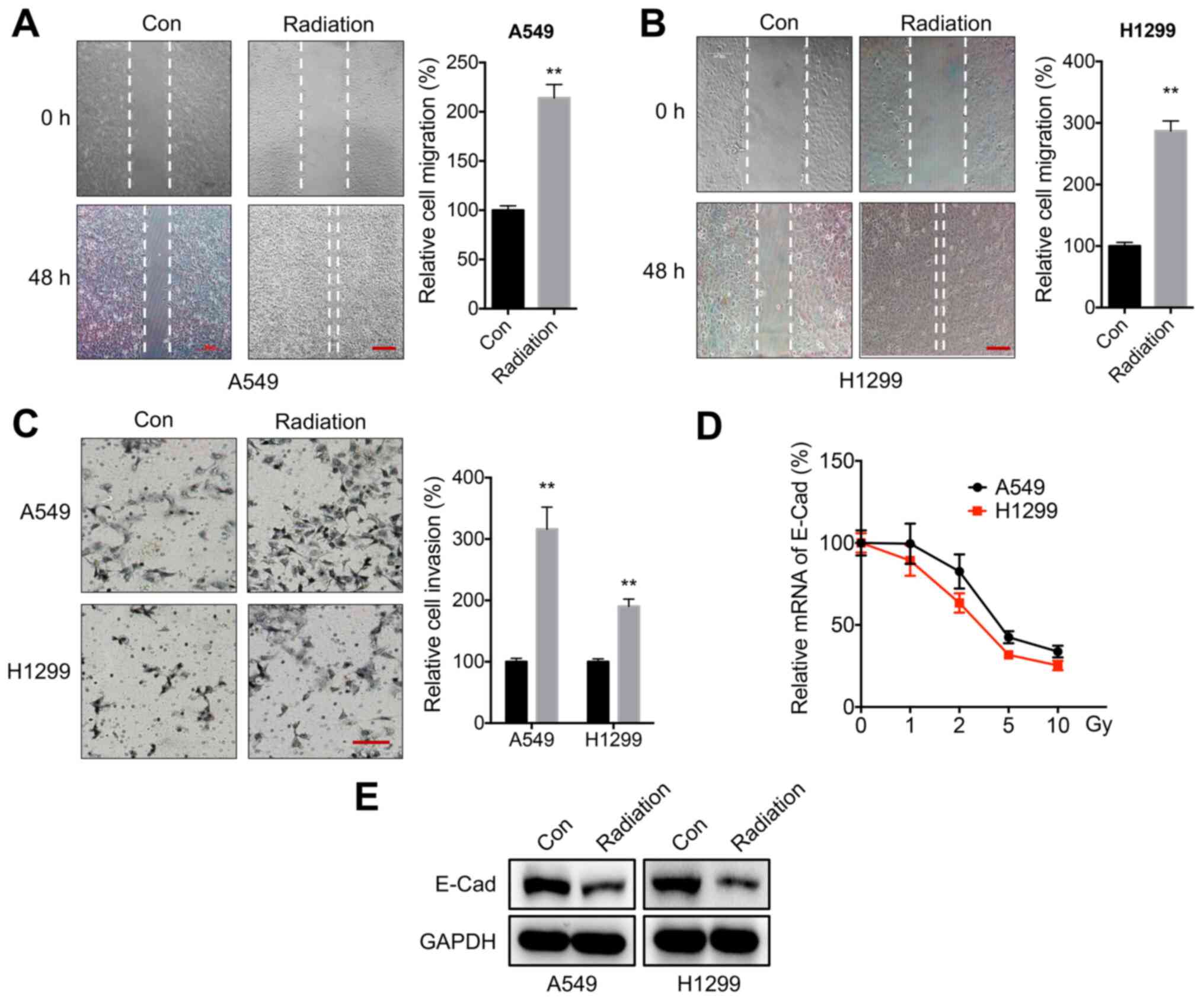
Radiation increases the motility of
NSCLC cells
In order to evaluate the potential effects of
radiation on the characteristics of NSCLC cells, A549 and H1299
were treated cells with 5 Gy of radiation according to previous
studies (30,36–38).
This radiation dose significantly increased the in vitro
migration rate of both A549 (Fig.
1A) and H1299 (Fig. 1B) cells.
A Transwell invasion assay confirmed that 5 Gy of radiation could
increase the in vitro invasion of both A549 and H1299 cells
(Fig. 1C). Moreover, the expression
of E-Cad in cells was measured following incubation with 1–10 Gy of
radiation. Radiation decreased the mRNA expression levels of E-Cad
in both A549 and H1299 cells in a dose-dependent manner (Fig. 1D). Western blot analysis confirmed
that radiation reduced E-Cad protein expression in A549 and H1299
cells (Fig. 1E). These findings
suggested that radiation increased the motility of NSCLC cells.
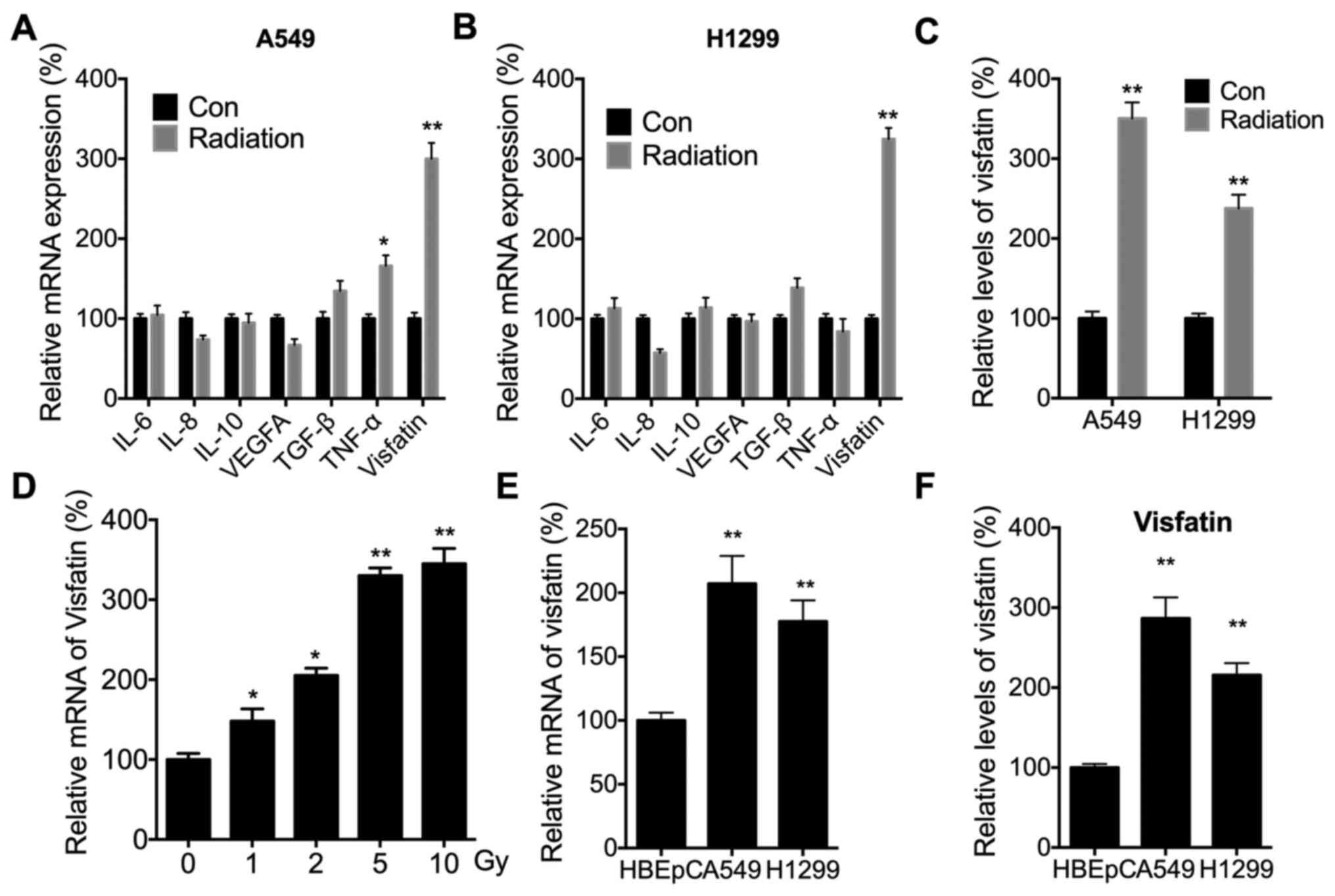
Radiation increases the expression of
visfatin in NSCLC cells
It has been suggested that cytokine levels are
critical for the metastasis of NSCLC cells and might be modulated
by radiation (16,39). The expression levels of IL-6, IL-8,
IL-10, VEGFA, TGF-β, TNF-α and visfatin were therefore measured,
since these cytokines have been shown to be critical for the
motility and metastasis of NSCLC cells (40,41).
Radiation significantly increased the expression of visfatin in
both A549 (Fig. 2A) and H1299
(Fig. 2B) cells. Radiation-induced
expression of visfatin was also confirmed in both cell lines using
ELISA (Fig. 2C). Furthermore,
RT-qPCR demonstrated that radiation increased mRNA expression of
visfatin in A549 cells in a dose-dependent manner (Fig. 2D). RT-qPCR (Fig. 2E) and ELISA (Fig. 2F) also indicated that visfatin
expression was significantly increased in A549 and H1299 cells,
compared with HBEpCs.
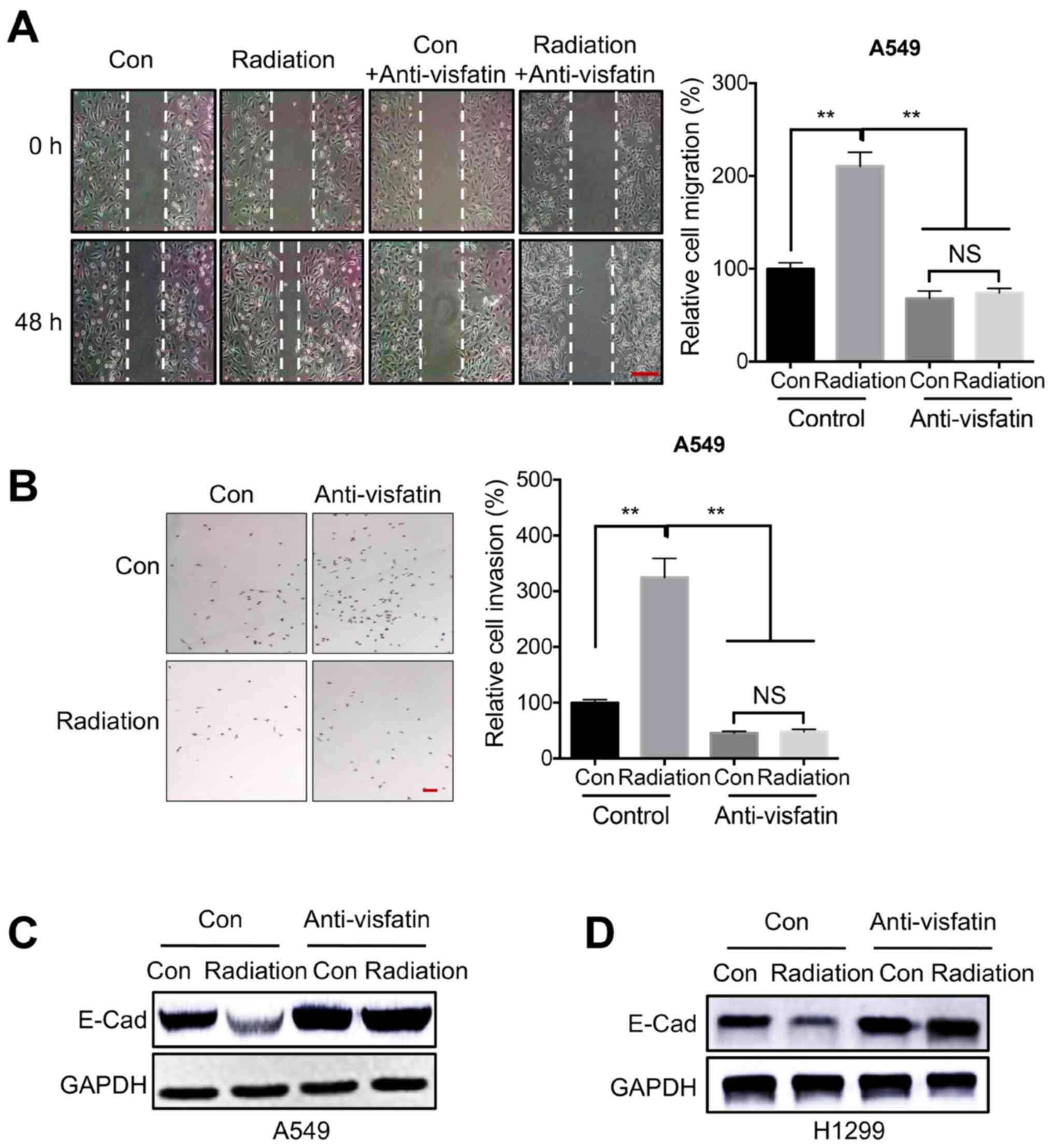
Visfatin is essential for radiation
induced cell motility
Previous studies have indicated that visfatin is
critical for NSCLC development and malignancy (18,42).
Thus, to determine whether visfatin was involved in
radiation-regulated cell motility, cells were treated with a
visfatin neutralizing antibody. Would healing assays indicated that
visfatin blockade inhibited migration in A549 cells, both under
control conditions and following irradiation (Fig. 3A). Similarly, a Transwell invasion
assay also confirmed that the anti-visfatin antibody inhibited
radiation-induced invasion of A549 cells (Fig. 3B). Furthermore, visfatin blockade
reversed the radiation-induced downregulation of E-Cad, both in
A549 (Fig. 3C) and in H1299
(Fig. 3D) cells.
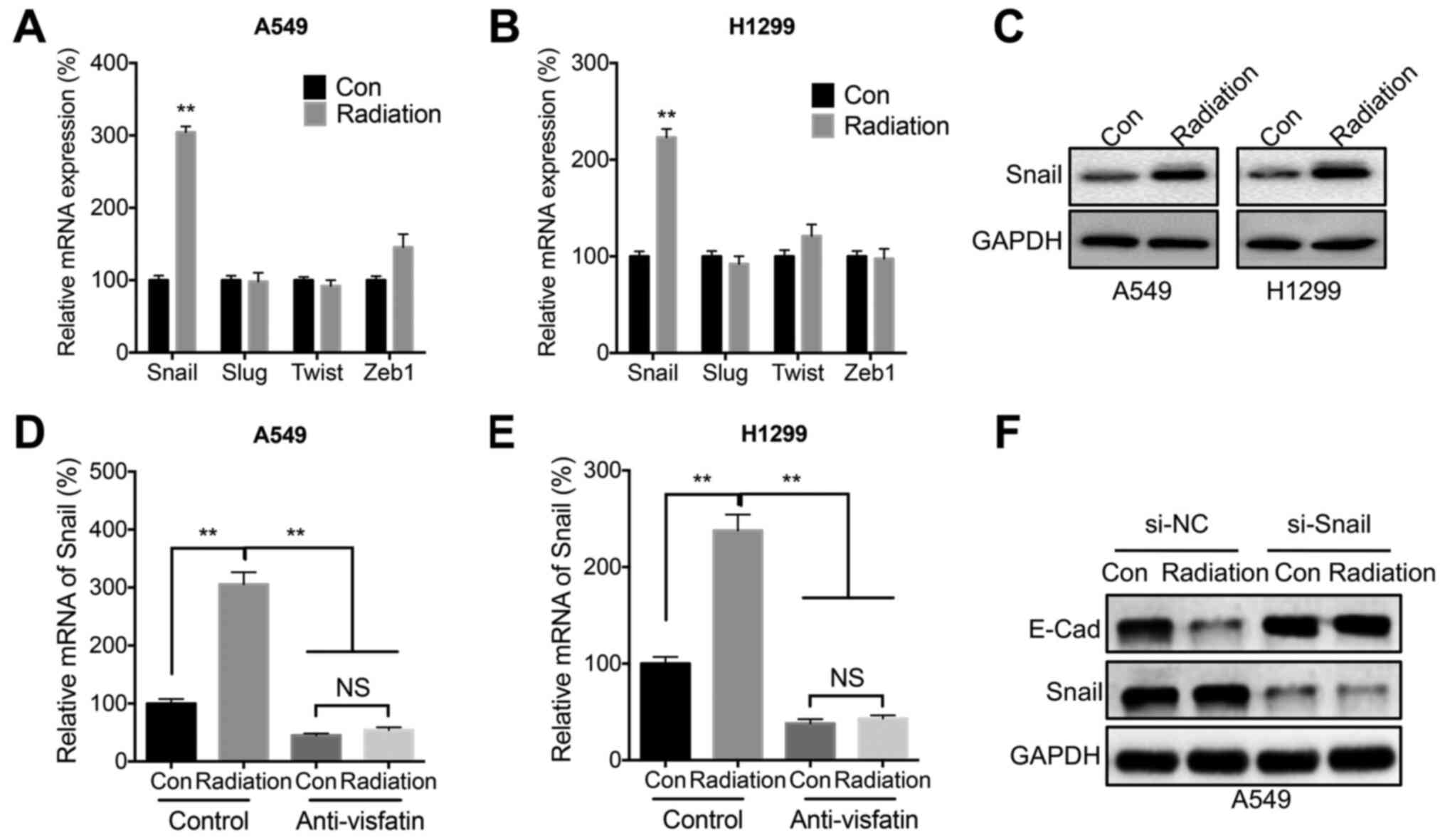
Snail is involved in radiation- and
visfatin-induced cell migration
Since E-Cad was significantly decreased during
radiation-induced cell migration, it was hypothesized that EMT-TF
such as Snail, Slug, Twist, and Zeb1 might be involved in this
process. Radiation significantly increased the mRNA expression
levels of Snail in both A549 (Fig.
4A) and H1299 (Fig. 4B) cells.
Further, western blot analysis confirmed that radiation increased
the protein expression levels of Snail in both cell lines (Fig. 4C). However, radiation-induced
expression of Snail could be blocked following treatment with the
anti-visfatin neutralizing antibody in both A549 (Fig. 4D) and H1299 (Fig. 4E) cells. In addition, Snail siRNA
knockdown reversed the radiation-induced downregulation of E-Cad
(Fig. 4F).
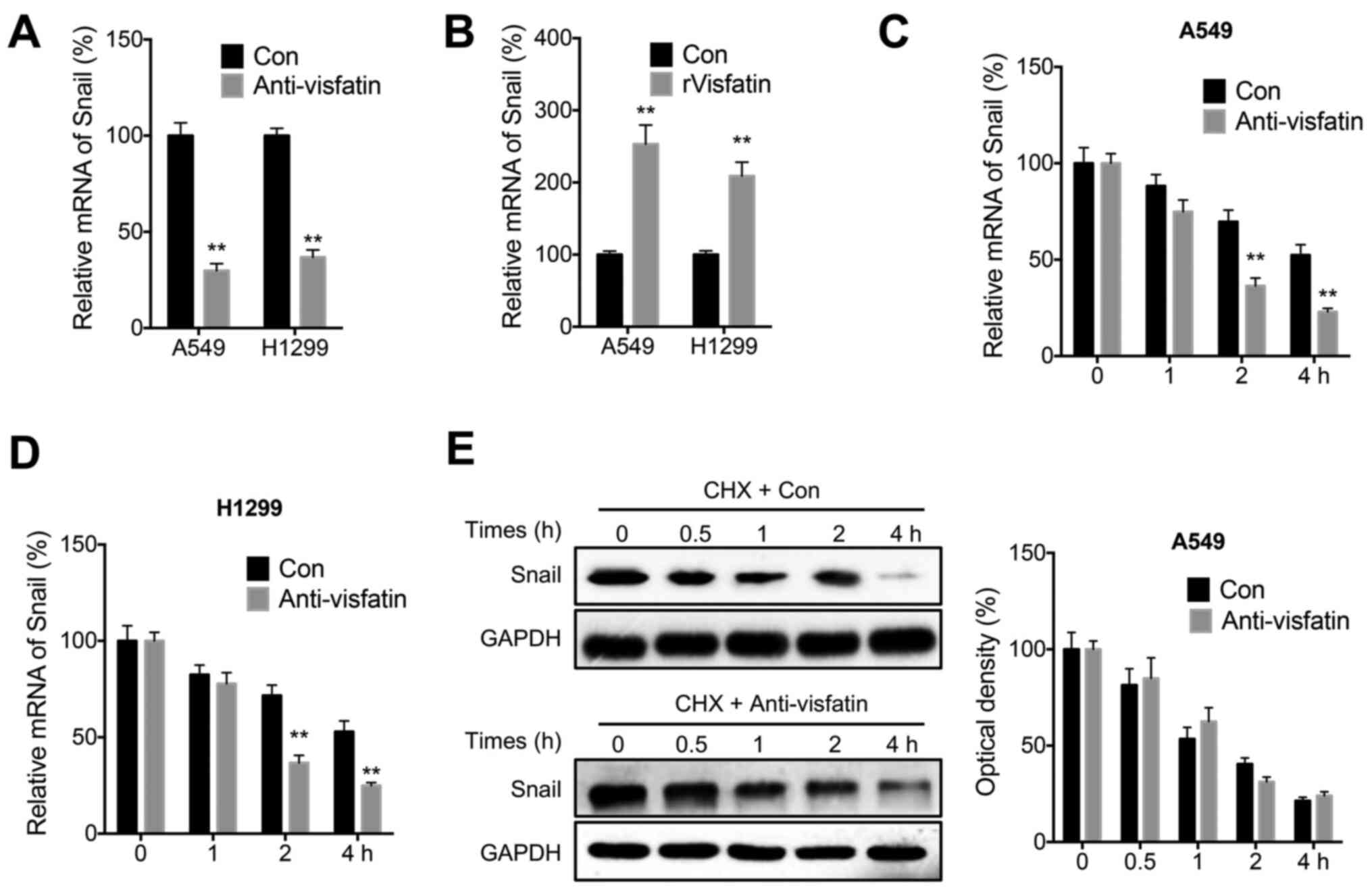
Visfatin regulates the mRNA stability
of Snail
The mechanisms involved in visfatin-mediated
regulation of Snail expression were further examined. The
anti-visfatin neutralizing antibody decreased the mRNA levels of
Snail in both A549 and H1299 cells (Fig. 5A). Conversely, rVisfatin increased
Snail mRNA levels in both cell lines (Fig. 5B). Additionally, the mRNA and
protein stability of Snail was evaluated in NSCLC cells. The
results suggested that anti-visfatin could decrease stability of
Snail at the mRNA level in both A549 (Fig. 5C) and H1299 (Fig. 5D) cells following Act-D treatment.
However, anti-visfatin had no effect on the stability of Snail
protein in A549 cells (Fig. 5E)
following CHX treatment.
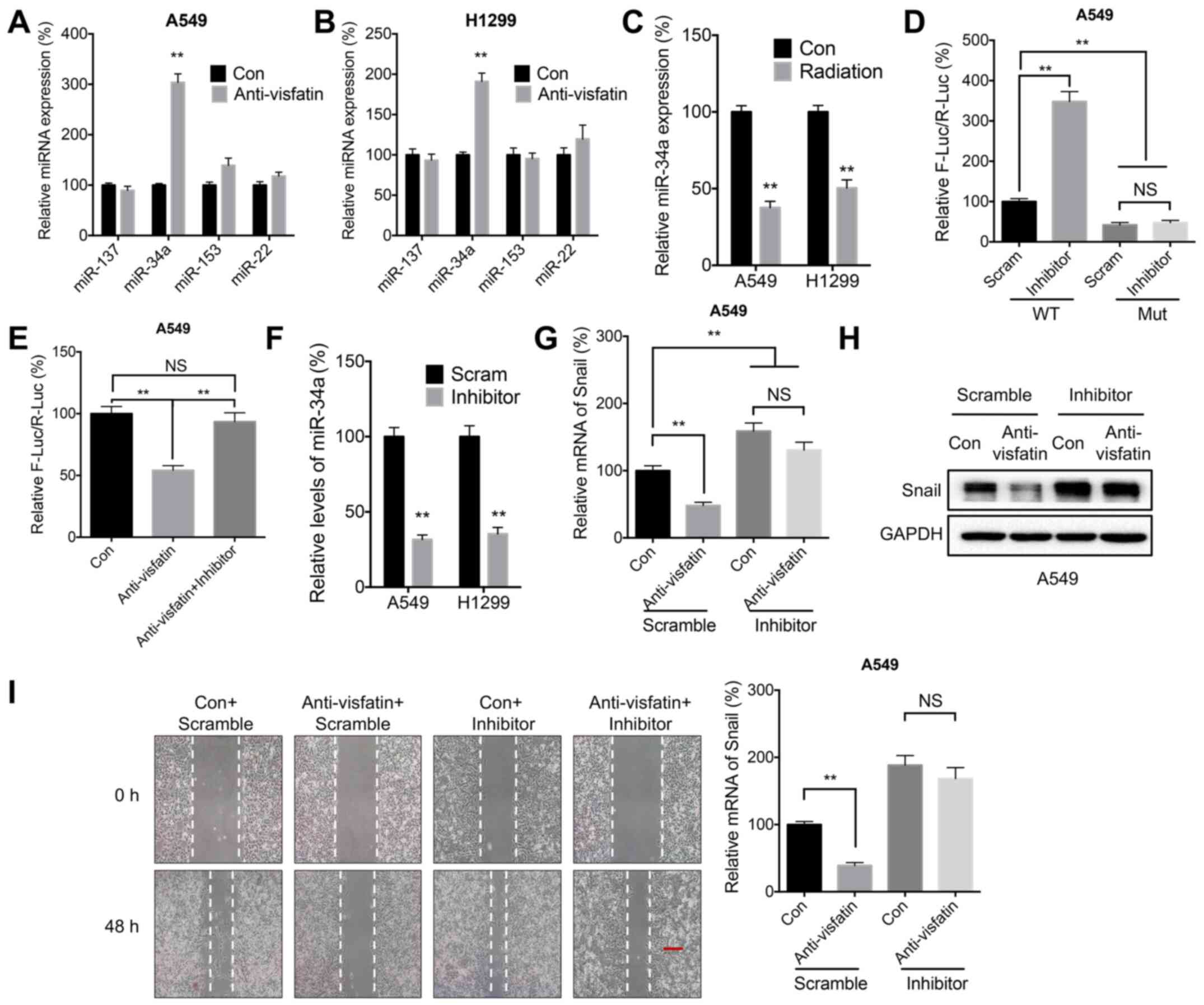
Visfatin may regulate Snail expression
through miR-34a
miRNA molecules can decrease mRNA stability by
binding to its 3′-UTR (43). It has
been suggested that miR-137 (35),
miR-34a (35), miR-153 (44), and miR-22 (45) can directly target Snail mRNA to
inhibit its expression and reduce its stability. In the present
study, anti-visfatin significantly increased the expression of
miR-34a in both A549 (Fig. 6A) and
H1299 (Fig. 6B) cells. Similarly,
radiation also reduced the expression of miR-34a in both cell lines
(Fig. 6C). Moreover, transfection
with the miR-34a inhibitor significantly increased the luciferase
activities of reporter vector containing the WT Snail 3′-UTR.
However, this effect was abrogated following transfection with the
MUT Snail 3′UTR, which contained mutations targeting the predicted
binding site of miR-34a (Fig. 6D).
These results demonstrated the direct binding between miR-34a and
the 3′-UTR of Snail. Furthermore, treatment with the anti-visfatin
neutralizing antibody reduced the luciferase activity of the
reporter vector containing the Snail 3′-UTR, whereas the addition
of miR-34a inhibitor abolished this effect (Fig. 6E). The miR-34a inhibitor was then
used to evaluate whether miR-34a was involved in visfatin-mediated
regulation of Snail expression (Fig.
6F). The results showed that the miR-34a inhibitor could
reverse the downregulation of Snail mRNA (Fig. 6G) and protein (Fig. 6H) induced by visfatin blockade in
A549 cells. In addition, the miR-34a inhibitor promoted migration
and reversed the effect of the anti-visfatin antibody on the
migration of A549 cells (Fig.
6I).
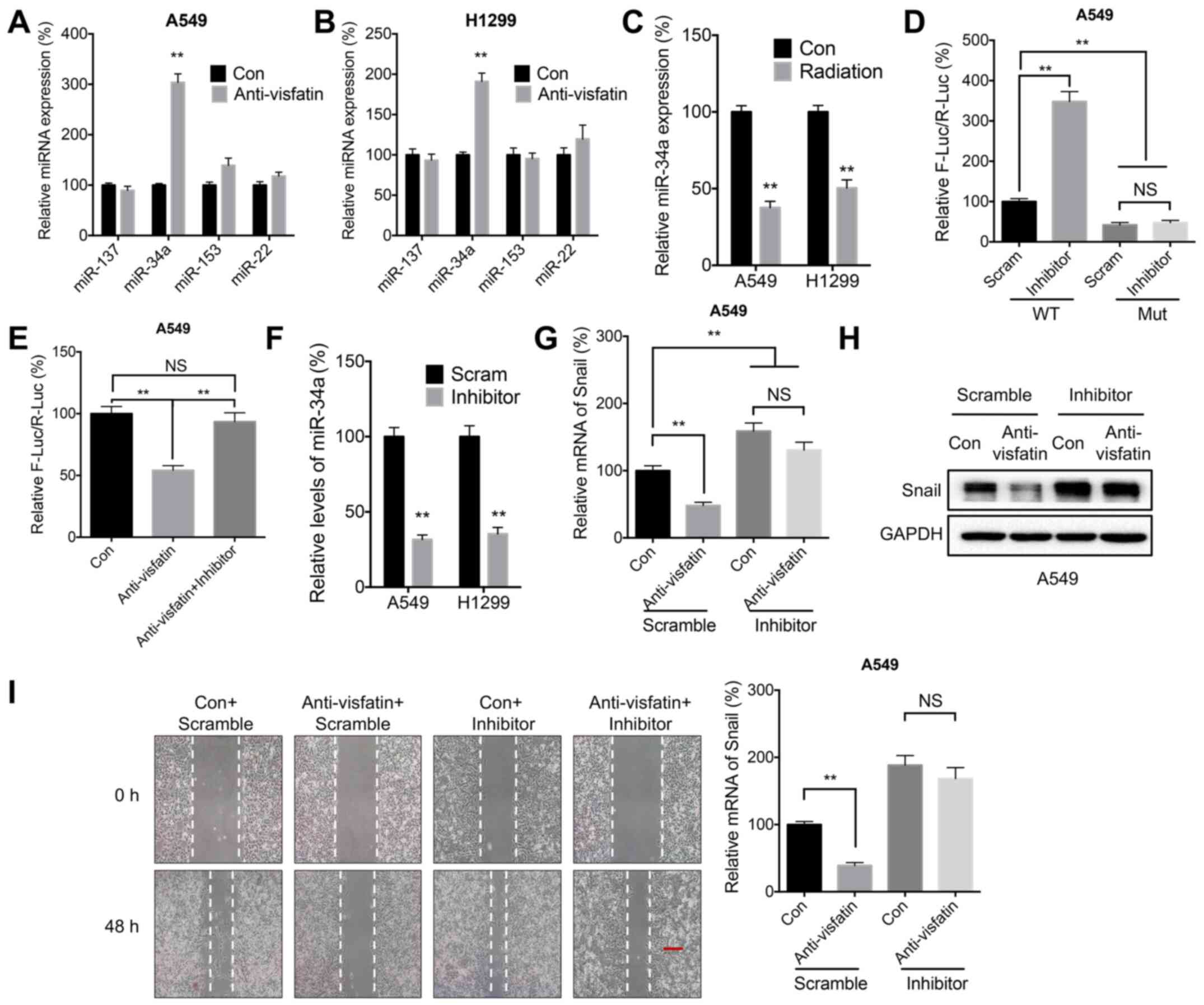 | Figure 6.miR-34a may be involved in
visfatin-regulated expression of Snail. (A and B) miR expression
levels in (A) A549 and (B) H1299 cells treated with (Anti-visfatin)
or without (Con) 100 ng/ml anti-visfatin antibody for 48 h. (C)
miR-34a expression levels in cells treated with (Radiation) or
without (Con) 5 Gy radiation for 24 h. (D) Luciferase activity in
A549 cells co-transfected with WT or MUT Snail-3′-UTR Firefly
luciferase reporter plasmid and Scram or miR-34a inhibitor for 24
h. (E) A549 cells were co-transfected with WT Snail-3′-UTR Firefly
luciferase reporter plasmid with or without miR-34a inhibitor for
12 h. The Anti-visfatin and Anti-visfatin + inhibitor groups were
treated with 100 ng/ml anti-visfatin antibody for 24 h. (F) miR-34a
expression levels in cells transfected with Scram miR or miR-34a
inhibitor for 24 h. (G-I) A549 cells were pre-transfected with
Scram or miR-34a inhibitor for 12 h, then treated with
(Anti-visfatin) or without (Con) 100 ng/ml anti-visfatin antibody
for 48 h. (G) mRNA and (H) protein expression levels of Snail. (I)
Relative cell migration. Scale bar, 100 µm. Data are presented as
the mean ± SD of three independent experiments. **P<0.01. Con,
control; Scram; scramble control; WT, wild-type; MUT, mutant; UTR,
unstranslated region; miR, microRNA; F-Luc, Firefly luciferase;
R-Luc, Renilla luciferase; NS, not significant. |
Discussion
Although radiotherapy is widely used for NSCLC
treatment, the efficacy of this therapeutic approach is not always
satisfactory, even in the absence of radioresistance (8). Previous studies have indicated that
residual cancer cells cancer survive following radiotherapy in many
cancer types and become more malignant (46,47).
For instance, radiation can increase the metastatic ability of
cancer cells through the induction of EMT (48,49).
In the present study, radiation was found to induce the migration
and invasion of NSLC cells, as evidenced by the results of wound
healing assays and invasion assays, as well as E-Cad
downregulation. Similarly, previous studies have demonstrated that
radiation could upregulate MMP-2 and MMP-9 in NSCLC cells,
resulting in increased invasion and migration of lung cancer cells
(13,50). γ-ionizing radiation (IR) also
induces migration/invasion of NSCLC cells (51). Thus, consistent with previous
reports, our present findings highlighted the potential adverse
effects of radiotherapy on NSCLC progression.
In the present study, visfatin was essential for
radiation-induced motility of NSCLC cells. Visfatin has been
reported to regulate angiogenesis, inflammation, and cell viability
(52). A study has indicated that
expression of visfatin is increased in cancer tissues as compared
to that in the normal tissues (53). Furthermore, visfatin promotes the
invasion and migration of several cancer types, such as
hepatocellular carcinoma (54) and
colorectal carcinoma (55). It is
also involved in resistance to Dox treatment in colorectal cancer
(56). Visfatin is upregulated in
lung cancer cells and tissues (42); it also regulates the EMT and
invasion of NSCLC cells (18), as
well as Dox sensitivity (17). In
the present study, visfatin was upregulated after radiation
therapy, and visfatin blockade with a neutralizing attenuated
radiation-induced cell motility. This suggested that visfatin could
promote the malignancy of lung cancer.
The present study revealed that miR-34a/Snail is
involved in visfatin-regulated radiotherapy-induced malignancy of
NSCLC cells. Moreover, it has been reported that visfatin can
upregulate the expression of Snail to induce EMT-like properties in
osteosarcoma cells (57) and
colorectal cancer (55). In NSCLC
cells, visfatin upregulates Snail expression by increasing its mRNA
stability, likely by decreasing the expression of miR-34a. Previous
studies have indicated that Snail was the direct target of miR-34a
in gastric (58), pancreatic
(59), and ovarian (35) cancer cells. In addition, Snail
directly induces ZNF281 transcription and represses miR-34a/b/c,
thereby alleviating ZNF281 mRNA from direct down-regulation by
miR-34 and promoting the EMT of lung cancer cells (60). However, the mechanisms underlying
visfatin-regulated expression of miR-34a remain unclear.
In summary, the present study demonstrated that
radiation increased the malignancy of NSCLC cells through visfatin
upregulation. miR-34a-regulated mRNA stability of Snail and was
involved in radiation/visfatin regulated motility of NSCLC cells.
Although the detailed mechanisms underlying the role of visfatin
and miR-34a remain to be determined, these findings highlighted the
adverse effects of radiotherapy on NSCLC cell motility.
Acknowledgements
No applicable.
Funding
This work was supported by The National Natural
Science Foundation of China (grant no. 81673099).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
LX, YM, ZT, YZ, HH and FW conceived and designed the
study. LX, YM and FW acquired the data. LX, YM and HH analyzed and
interpreted the data. LX, HH and FW wrote, reviewed and revised the
manuscript. All authors read and approved the final manuscript. LX
and FW confirm the authenticity of the raw data. All authors read
and approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Askoxylakis V, Thieke C, Pleger ST, Most
P, Tanner J, Lindel K, Katus HA, Debus J and Bischof M: Long-term
survival of cancer patients compared to heart failure and stroke: A
systematic review. BMC Cancer. 10:1052010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Schwartz AG, Wenzlaff AS, Prysak GM,
Murphy V, Cote ML, Brooks SC, Skafar DF and Lonardo F: Reproductive
factors, hormone use, estrogen receptor expression and risk of non
small-cell lung cancer in women. J Clin Oncol. 25:5785–5792. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Gondos A, Bray F, Brewster DH, Coebergh
JW, Hakulinen T, Janssen-Heijnen ML, Kurtinaitis J and Brenner H;
EUNICE Survival Working Group, : Recent trends in cancer survival
across Europe between 2000 and 2004: A model-based period analysis
from 12 cancer registries. Eur J Cancer. 44:1463–1475. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Molina JR, Yang P, Cassivi SD, Schild SE
and Adjei AA: Non-small cell lung cancer: Epidemiology, risk
factors, treatment, and survivorship. Mayo Clin Proc. 83:584–594.
2008. View
Article : Google Scholar : PubMed/NCBI
|
|
5
|
Remon J, Ahn MJ, Girard N, Johnson M, Kim
DW, Lopes G, Pillai RN, Solomon B, Villacampa G and Zhou Q:
Advanced-stage non-small cell lung cancer: Advances in thoracic
oncology 2018. J Thorac Oncol. 14:1134–1155. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Antonia SJ, Villegas A, Daniel D, Vicente
D, Murakami S, Hui R, Yokoi T, Chiappori A, Lee KH, de Wit M, et al
PACIFIC investigators, : Durvalumab after chemoradiotherapy in
stage III non-small-cell lung cancer. N Engl J Med. 377:1919–1929.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Shinde A, Li R, Kim J, Salgia R, Hurria A
and Amini A: Stereotactic body radiation therapy (SBRT) for
early-stage lung cancer in the elderly. Semin Oncol. 45:210–219.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Draghiciu O, Walczak M, Hoogeboom BN,
Franken KL, Melief KJ, Nijman HW and Daemen T: Therapeutic
immunization and local low-dose tumor irradiation, a reinforcing
combination. Int J Cancer. 134:859–872. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lee S, Lim MJ, Kim MH, Yu CH, Yun YS, Ahn
J and Song JY: An effective strategy for increasing the
radiosensitivity of human lung cancer cells by blocking
Nrf2-dependent antioxidant responses. Free Radic Biol Med.
53:807–816. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Provencio M, Sánchez A, Garrido P and
Valcárcel F: New molecular targeted therapies integrated with
radiation therapy in lung cancer. Clin Lung Cancer. 11:91–97. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Rube CE, Uthe D, Schmid KW, Richter KD,
Wessel J, Schuck A, Willich N and Rube C: Dose-dependent induction
of transforming growth factor beta (TGF-beta) in the lung tissue of
fibrosis-prone mice after thoracic irradiation. Int J Radiat Oncol
Biol Phys. 47:1033–1042. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Tsukamoto H, Shibata K, Kajiyama H,
Terauchi M, Nawa A and Kikkawa F: Irradiation-induced
epithelial-mesenchymal transition (EMT) related to invasive
potential in endometrial carcinoma cells. Gynecol Oncol.
107:500–504. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Zhao Q, Mao A, Guo R, Zhang L, Yan J, Sun
C, Tang J, Ye Y, Zhang Y and Zhang H: Suppression of
radiation-induced migration of non-small cell lung cancer through
inhibition of Nrf2-Notch Axis. Oncotarget. 8:36603–36613. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kroeze SG, van Melick HH, Nijkamp MW,
Kruse FK, Kruijssen LW, van Diest PJ, Bosch JL and Jans JJ:
Incomplete thermal ablation stimulates proliferation of residual
renal carcinoma cells in a translational murine model. BJU Int.
110:E281–E286. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Shiozawa K, Watanabe M, Takahashi M, Wakui
N, Iida K and Sumino Y: Analysis of patients with rapid aggressive
tumor progression of hepatocellular carcinoma after percutaneous
radiofrequency ablation. Hepatogastroenterology. 56:1689–1695.
2009.PubMed/NCBI
|
|
16
|
Daly ME, Monjazeb AM and Kelly K: Clinical
trials integrating immunotherapy and radiation for non-small-cell
lung cancer. J Thorac Oncol. 10:1685–1693. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Cao Z, Liang N, Yang H and Li S: Visfatin
mediates doxorubicin resistance in human non-small-cell lung cancer
via Akt-mediated up-regulation of ABCC1. Cell Prolif.
50:e123662017. View Article : Google Scholar
|
|
18
|
Wang G, Tian W, Liu Y, Ju Y, Shen Y, Zhao
S, Zhang B and Li Y: Visfatin triggers the cell motility of
non-small cell lung cancer via up-regulation of matrix
metalloproteinases. Basic Clin Pharmacol Toxicol. 119:548–554.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Okumura S, Sasaki T, Minami Y and Ohsaki
Y: Nicotinamide phosphoribosyltransferase: A potent therapeutic
target in non-small cell lung cancer with epidermal growth factor
receptor-gene mutation. J Thorac Oncol. 7:49–56. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Laiguillon MC, Houard X, Bougault C,
Gosset M, Nourissat G, Sautet A, Jacques C, Berenbaum F and Sellam
J: Expression and function of visfatin (Nampt), an adipokine-enzyme
involved in inflammatory pathways of osteoarthritis. Arthritis Res
Ther. 16:R382014. View
Article : Google Scholar : PubMed/NCBI
|
|
21
|
Gujar AD, Le S, Mao DD, Dadey DY, Turski
A, Sasaki Y, Aum D, Luo J, Dahiya S, Yuan L, et al: An
NAD+-dependent transcriptional program governs
self-renewal and radiation resistance in glioblastoma. Proc Natl
Acad Sci USA. 113:E8247–E8256. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Xiang B, Han L, Wang X, Tang L, Li K, Li
X, Zhao X, Xia M, Zhou X, Zhang F, et al: Nicotinamide
phosphoribosyltransferase upregulation by phenylephrine reduces
radiation injury in submandibular gland. Int J Radiat Oncol Biol
Phys. 96:538–546. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Thiery JP: Epithelial-mesenchymal
transitions in tumour progression. Nat Rev Cancer. 2:442–454. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Lu W and Kang Y: Epithelial-mesenchymal
plasticity in cancer progression and metastasis. Dev Cell.
49:361–374. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Batlle E, Sancho E, Francí C, Domínguez D,
Monfar M, Baulida J and García De Herreros A: The transcription
factor snail is a repressor of E-cadherin gene expression in
epithelial tumour cells. Nat Cell Biol. 2:84–89. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Xu J, Lamouille S and Derynck R:
TGF-beta-induced epithelial to mesenchymal transition. Cell Res.
19:156–172. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Wang G, Ma W, Li Y, Jiang Y, Ma G, Zhang
X, Meng L and Du J: Prognostic value of Twist, Snail and E-cadherin
expression in pathological N0 non-small-cell lung cancer: A
retrospective cohort study. Eur J Cardiothorac Surg. 54:237–245.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Yanagawa J, Walser TC, Zhu LX, Hong L,
Fishbein MC, Mah V, Chia D, Goodglick L, Elashoff DA, Luo J, et al:
Snail promotes CXCR2 ligand-dependent tumor progression in
non-small cell lung carcinoma. Clin Cancer Res. 15:6820–6829. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Zhang Y, Zhang X, Ye M, Jing P, Xiong J,
Han Z, Kong J, Li M, Lai X, Chang N, et al: FBW7 loss promotes
epithelial-to-mesenchymal transition in non-small cell lung cancer
through the stabilization of Snail protein. Cancer Lett. 419:75–83.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Lin Y, Bai X, Zhou W, He Y, Wu Y and Wang
X: Radiation exposure triggers the progression of triple negative
breast cancer via stabilizing ZEB1. Biomed Pharmacother.
107:1624–1630. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Wang Q, Yang G, Jiang Y, Luo M, Li C, Zhao
Y, Xie Y, Song K and Zhou J: XB130, regulated by miR-203, miR-219,
and miR-4782-3p, mediates the proliferation and metastasis of
non-small-cell lung cancer cells. Mol Carcinog. 59:557–568. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Pecoraro A, Carotenuto P, Russo G and
Russo A: Ribosomal protein uL3 targets E2F1 and Cyclin D1 in cancer
cell response to nucleolar stress. Sci Rep. 9:154312019. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Lu L, Chen Z, Lin X, Tian L, Su Q, An P,
Li W, Wu Y, Du J, Shan H, et al: Inhibition of BRD4 suppresses the
malignancy of breast cancer cells via regulation of Snail. Cell
Death Differ. 27:255–268. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Dong P, Xiong Y, Watari H, Hanley SJ,
Konno Y, Ihira K, Yamada T, Kudo M, Yue J and Sakuragi N: MiR-137
and miR-34a directly target Snail and inhibit EMT, invasion and
sphere-forming ability of ovarian cancer cells. J Exp Clin Cancer
Res. 35:1322016. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Kim R-K, Kaushik N, Suh Y, Yoo KC, Cui YH,
Kim MJ, Lee HJ, Kim IG and Lee SJ: Radiation driven
epithelial-mesenchymal transition is mediated by Notch signaling in
breast cancer. Oncotarget. 7:53430–53442. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Feys L, Descamps B, Vanhove C, Vral A,
Veldeman L, Vermeulen S, De Wagter C, Bracke M and De Wever O:
Radiation-induced lung damage promotes breast cancer
lung-metastasis through CXCR4 signaling. Oncotarget. 6:26615–26632.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Lagadec C, Vlashi E, Della Donna L,
Dekmezian C and Pajonk F: Radiation-induced reprogramming of breast
cancer cells. Stem Cells. 30:833–844. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Rodriguez-Ruiz ME, Vitale I, Harrington
KJ, Melero I and Galluzzi L: Immunological impact of cell death
signaling driven by radiation on the tumor microenvironment. Nat
Immunol. 21:120–134. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Strieter RM, Belperio JA, Burdick MD,
Sharma S, Dubinett SM and Keane MP: CXC chemokines: Angiogenesis,
immunoangiostasis, and metastases in lung cancer. Ann NY Acad Sci.
1028:351–360. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Santaniello A, Napolitano F, Servetto A,
De Placido P, Silvestris N, Bianco C, Formisano L and Bianco R:
Tumour microenvironment and immune evasion in EGFR addicted NSCLC:
Hurdles and possibilities. Cancers (Basel). 11:14192019. View Article : Google Scholar
|
|
42
|
Liu T, Miao Z, Jiang J, Yuan S, Fang W, Li
B and Chen Y: Visfatin mediates SCLC cells migration across brain
endothelial cells through upregulation of CCL2. Int J Mol Sci.
16:11439–11451. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Uddin A and Chakraborty S: Role of miRNAs
in lung cancer. J Cell Physiol. Apr 20–2018.(Epub ahead of print).
doi: 10.1002/jcp.26607. View Article : Google Scholar
|
|
44
|
Wang Z and Liu C: MiR-153 regulates
metastases of gastric cancer through Snail. Tumour Biol.
37:15509–15515. 2015. View Article : Google Scholar
|
|
45
|
Zhang K, Li XY, Wang ZM, Han ZF and Zhao
YH: MiR-22 inhibits lung cancer cell EMT and invasion through
targeting Snail. Eur Rev Med Pharmacol Sci. 21:3598–3604.
2017.PubMed/NCBI
|
|
46
|
Cui YH, Suh Y, Lee HJ, Yoo KC, Uddin N,
Jeong YJ, Lee JS, Hwang SG, Nam SY, Kim MJ, et al: Radiation
promotes invasiveness of non-small-cell lung cancer cells through
granulocyte-colony-stimulating factor. Oncogene. 34:5372–5382.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Qian L-W, Mizumoto K, Urashima T, Nagai E,
Maehara N, Sato N, Nakajima M and Tanaka M: Radiation-induced
increase in invasive potential of human pancreatic cancer cells and
its blockade by a matrix metalloproteinase inhibitor, CGS27023.
Clin Cancer Res. 8:1223–1227. 2002.PubMed/NCBI
|
|
48
|
Nambiar DK, Rajamani P and Singh RP:
Silibinin attenuates ionizing radiation-induced pro-angiogenic
response and EMT in prostate cancer cells. Biochem Biophys Res
Commun. 456:262–268. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Zhou YC, Liu JY, Li J, Zhang J, Xu YQ,
Zhang HW, Qiu LB, Ding GR, Su XM, Mei-Shi, et al: Ionizing
radiation promotes migration and invasion of cancer cells through
transforming growth factor-beta-mediated epithelial-mesenchymal
transition. Int J Radiat Oncol Biol Phys. 81:1530–1537. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Wang L, Zhao Y, Xiong Y, Wang W, Fei Y,
Tan C and Liang Z: K-ras mutation promotes ionizing
radiation-induced invasion and migration of lung cancer in part via
the Cathepsin L/CUX1 pathway. Exp Cell Res. 362:424–435. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Cho JH, Hong WG, Jung YJ, Lee J, Lee E,
Hwang SG, Um HD and Park JK: γ-Ionizing radiation-induced
activation of the EGFR-p38/ERK-STAT3/CREB-1-EMT pathway promotes
the migration/invasion of non-small cell lung cancer cells and is
inhibited by podophyllotoxin acetate. Tumour Biol. 37:7315–7325.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Romacho T, Sánchez-Ferrer CF and Peiró C:
Visfatin/Nampt: An adipokine with cardiovascular impact. Mediators
Inflamm. 2013:9464272013. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Carbone F, Liberale L, Bonaventura A,
Vecchiè A, Casula M, Cea M, Monacelli F, Caffa I, Bruzzone S,
Montecucco F, et al: Regulation and function of extracellular
nicotinamide phosphoribosyltransferase/visfatin. Compr Physiol.
7:603–621. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Liang N, Chen Y, Yang L, He S and Liu T:
Visfatin increases miR-21 to promote migration in HCC. Cell Mol
Biol. 64:48–52. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Yang J, Zhang K, Song H, Wu M, Li J, Yong
Z, Jiang S, Kuang X and Zhang T: Visfatin is involved in promotion
of colorectal carcinoma malignancy through an inducing EMT
mechanism. Oncotarget. 7:32306–32317. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Yan X, Zhao J and Zhang R: Visfatin
mediates doxorubicin resis-tance in human colorectal cancer cells
via up regulation of multidrug resistance 1 (MDR1). Cancer
Chemother Pharmacol. 80:395–403. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Wang D, Qian G, Wang J, Wang T, Zhang L,
Yang P and Lin F: Visfatin is involved in the cisplatin resistance
of osteosarcoma cells via upregulation of Snail and Zeb1. Cancer
Biol Ther. 20:999–1006. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Zhang Y, Yuan Y, Zhang Y, Cheng L, Zhou X
and Chen K: SNHG7 accelerates cell migration and invasion through
regulating miR-34a-Snail-EMT axis in gastric cancer. Cell Cycle.
19:142–152. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Tang Y, Tang Y and Cheng YS: miR-34a
inhibits pancreatic cancer progression through Snail1-mediated
epithelial-mesenchymal transition and the Notch signaling pathway.
Sci Rep. 7:382322017. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Hahn S, Jackstadt R, Siemens H, Hünten S
and Hermeking H: SNAIL and miR-34a feed-forward regulation of
ZNF281/ZBP99 promotes epithelial-mesenchymal transition. EMBO J.
32:3079–3095. 2013. View Article : Google Scholar : PubMed/NCBI
|