Introduction
According to the American Cancer Society, 13,240 new
cases of cervical cancer were registered in the United States in
2018 (1). When regional or distant
metastases are detected, survival rates within four years are 57
and 17%, respectively (1). The
involvement of the lymphatic system is one of the most important
predictors of poor prognosis (2) and
the standard method used to determine the presence of lymph node
(LN) involvement with precision is histological examination
(3). MRI was subsequently developed
for pre-operative evaluation and post-operative follow-up. Through
morphological and functional tools, LN metastasis can be detected,
categorized and staged using MRI (4,5).
An important tool in MRI is diffusion-weighted
imaging (DWI), which randomizes molecular movement and provides
insight into how tumors behave in the tissue environment (6). DWI uses the apparent diffusion
coefficient (ADC) to analyze the magnitude of diffusion by
measuring the diffusion of water molecules inside the tissue
(5). In cancer tissues, ADC is
normally low due to the high cancer cellularity and abundance of
membranes (2,7–9). As the
size, shape, extension of tumor outside the tissue and presence of
necrosis can impact directly on treatment, these aspects must be
evaluated to detect the existence of metastatic LNs (10,11).
Therefore, it is important to discriminate which LN
has a higher chance of being metastatic, based on its morphological
and functional aspects, to avoid complications of lymphadenectomy
as well as to define an optimal radiotherapy plan, without having
to irradiate healthy tissue unnecessarily (12).
The current study evaluated morphological
characteristics and DWI results of pelvic and paraaortic LNs using
MRI in patients with cervical cancer and compared these results to
histological analysis. To the best of the authors knowledge,
previous studies did not successfully compare imaging examinations
of metastatic LNs in detail. The current study was designed to
identify metastatic LNs with a higher precision compared with
histopathological findings, and obtain more specific and sensitive
results. The aim of the present study was to evaluate the accuracy
of DWI and morphological features at 3 Tesla (T) and 1.5T MRI for
diagnosing metastatic LNs in cervical cancer.
Materials and methods
Patient data
The present study was entirely based on the review
of patients medical records, and no human samples were used.
Approval was obtained from the Ethics Committee of Barretos Cancer
Hospital (approval no. 1150/2016; Barretos, Brazil). All patients
consented to the use of their medical records in the current study.
Medical records of patients with cervical cancer who attended the
Gynecologic Oncology Department between January 2013 and December
2016 were retrospectively reviewed to obtain patient demographics,
imaging findings, surgical-pathological data and follow-up
information after treatment. The present study included 45 female
patients (age range, 26–74 years) with stage IA1 to IVB who also
had lymph vascular space invasion, who had an MRI examination for
primary local tumor staging. This group of patients belong to a
group that underwent pelvic and/or paraaortic lymphadenectomy as
part of surgical staging or primary treatment. Patients who did not
undergo MRI examination or pelvic and/or paraaortic lymphadenectomy
were excluded from this study. These patients were followed up
after treatment until December 2019.
Recently, the International Federation of Gynecology
and Obstetrics (FIGO) staging systems for cervical cancer have been
revised and two new sub-categories were included to classify the
stage by LN involvement, including IIIC1 (pelvic LN metastasis) and
IIIC2 (para-aortic LN metastasis) (13). Since the information for the current
study was collected before the update, patients were reclassified
according to the new FIGO recommendations.
Histological analyses
Histological analyses were made on LNs resected in
pelvic and/or paraaortic chains. All the LNs were cut into 3-mm
thickness before they were embedded into paraffin cubes and cut
using microtomes. The final thickness measured 4 µm and the LNs
were visualized using an optical microscope.
Image analyses
At the Barretos Cancer Hospital the inferior abdomen
of patients with cervical cancer is evaluated though MRI scans,
since the analysis of tumor and its relation to adjacent structures
using MRI can yield superior visualization compared with that by
abdominal CT. When evaluating pelvis and its structures, including
those of suspected LNs, MRI scans exhibit superior accuracy
compared with CT. However, renal veins are evaluated using
contrasted CT at the Barretos Cancer Hospital. The public health
system in Brazil does not cover positron emission tomography-CT
(PET-CT) analyses in patients with cervical and endometrial cancer.
In addition, since the Barretos Cancer Hospital is a public
institution, CT technology was not available between January 2013
and December 2016.
The standard protocol performed at The Radiology
Department of Barretos Cancer Hospital to obtain the pelvic MRI
images for cervical cancer included T2-weighted images (WI) in
different planes (axial, sagittal and coronal) and T1-WI (slice
thickness, 3 mm; slice gap, 0.3-mm). Images were acquired from the
superior portion of the antero-superior iliac spine to the inferior
portion of inferior pubic branches. High resolution T2-WI sequences
were taken of the axial plane at 3 mm slice thickness, which were
adjusted by sagittal and coronal planes (acquired in the same
exam), with 3 mm slice thickness and no gap. The diffusion weighted
sequence is acquired by using the same axial plane and slice
thickness in the T2-weighted sequence with high resolution. This
protocol also includes an additional T2-weighted sequence, with
slice thickness of 3 and 0.3 mm gaps, which were acquired from the
left renal vein until the lower pubic branches. Although these MRI
images were captured to visualize pelvic LNs, the final sequence in
the T2-WI aforementioned, which were taken using the same
protocols, was also used to evaluate paraaortic LNs, since this
sequence has higher cutting thickness and possible artifacts
imaging (for instance intestinal gases and movement), which could
reduce the analysis accuracy of the paraaortic LN.
Lymph node status was classified by the impression
of the radiologists (R.R.S and M.D.S), according to the chain
removed, including right pelvic (RP), left pelvic (LP) and
paraaortic (PA) and its quality: Diagnostic and non-diagnostic
samples were classified according to the subjective impression of
the radiologists. Non-diagnostic samples were excluded from the
analysis. All images were captured at baseline assessment using
Achieva 3.0T (Philips Healthcare) or a Signa™ 1.5T HDxT (GE
Healthcare). PACS software (version 3.3.36) inside packages with
PixViewer and Viewer MPR (year 2019; version 19.9.0; Pixeon Medical
Systems SA) was used to visualize the images.
The MRI images were analyzed before surgery by two
experienced radiologists (RRR and MDS) in a blinded manner. The
final report was through consensual analyzes and each LN was
classified as normal or suspect. For correct distribution, all
statistical analyses considered the following criteria for
assessing the signal sequences of the MRI: i) Appearance,
homogenous or heterogenous; ii) presence of necrosis, yes or no;
and iii) T2 intensity, low broadcast, areas with low signal or
normal signal. For assessing the morphological aspects using the
conventional sequences of MRI, for following criteria were used: i)
Size, short-axis diameter >10 mm; ii) morphology, usual, rounded
or amorphous, iii) limits, regular, irregular or imprecise; iv)
diffusion, normal or greater restriction than expected for normal
tissue; and v) aspect, suspected or normal. Patients with ≥1 LN
classified as suspect using MRI were considered positive, since the
chain analyzed in MRI was the same chain that was removed in
posterior surgery and then identified as positive by histology.
Statistical analysis
Statistical analyses were performed using the SPSS
software (version 21; IBM Corp.). Quantitative criteria (symmetric
and non-symmetric) were presented as the mean ± standard deviation
and categorical data were presented as n (%) in tables. The κ and
concordance test were used to evaluate if the variable MRI had a
link with histopathology results, where values closer to 1 was
considered to indicate higher degrees of concordance between the
MRI and histopathology data. P<0.05 was considered to indicate a
statistically significant difference. Sensitivity (S), specificity
(E), positive predictive value (PPV) and negative predictive value
(NPV) were used to determine the accuracy of MRI images. Study data
will be collected and managed using Redcap software version 9.5.14
(Research Electronic Data Capture) electronic data capture tools
hosted at MD Anderson (Texas) (14).
Results
General results
A total of 45 patients with cervical cancer who
underwent pelvic and/or paraaortic lymphadenectomy were included in
the current study. The median age was 50 years (age range, 26–74).
Among these 45 patients, 34 (75.6%) had squamous carcinoma, 8
(17.8%) had adenocarcinoma and 3(6.6%) had other histological
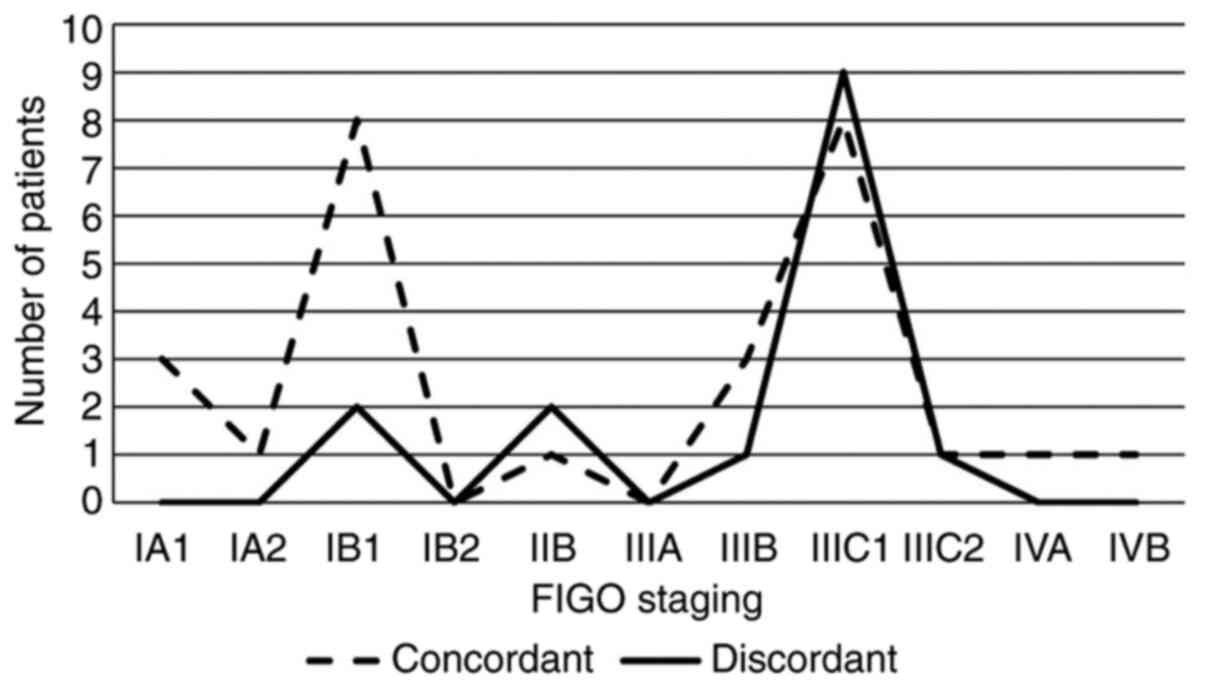
subtypes. According to the revised FIGO staging system 4 patients
(8.9%) were categorized as IA1, 1 (2.2%) as IA2, 10 (22.2%) as IB1,
8 (18.8%) as IIB, 1 (2.2%) as IIIA, 3 (6.7%) as IIIB, 9 (20.0%) as
IIIC1, 5 (11.1%) as IIIC2, 1 (2.2%) as IVA and 3 (6.7%) as IVB. In
addition, FIGO stage diagnoses obtained by physical examination
were compared with the FIGO stage prediction made using MRI before
surgery. A total of 27 patients (60%) were concordant and 18
patients (40%) were discordant comparing histological FIGO stage
and presumed FIGO stage by MRI, respectively. The number of
concordant and discordant patients was determined at each FIGO
stage (IA1-IVB; Fig. 1).
The MRI evaluated was before surgery (median, 43
days; range, 3–163 days). Among 45 patients, 14 (31.1%) and 31
(68.9%) had metastatic and negative LNs by histology, respectively.
Among these 14 metastatic patients, 9 (64.3%) had positive LNs in
both pelvic (RP and LP) and PA chains, 4 (28.6%) in PA and 1 (7.1%)
in RP and PA. Among the 14 (31.1%) patients with positive LNs, 8
(57.2%) had no recurrence after treatment at the Barretos Cancer
Hospital. However, recurrence was recorded in 6 (42.8%) patients.
These recurrences were diagnosed by MRI. Two patients (33.3%) had
recurrence in pelvic organs, 2 (33.3%) in the abdomen, 1 (16.7%) in
pelvic LNs and 1 (16.7%) pelvic LNs and lungs. Recurrence in the
same lymphatic chain that had prior lymphadenectomy was observed in
3 patients (50%). Among the 31 patients with negative LNs, 26
(83.8%) had no recurrence, whereas 5 (16.2%) had recurrence. A
total of 4 (80%) of these patients were diagnosed only by MRI and
one (20%) by MRI and tomography. Among the 5 patients with
recurrence, 3 (60%) were in the abdomen, 1 (20%) in liver and
lungs, and 1 (20%) in pelvic organs.
Comparison between data obtained using
histology and MRI
Comparing between histology and MRI findings, 12
patients (26.7%) had suspected LN metastasis by MRI and were tested
positive by histological analysis, 26 (57.8%) were tested negative
for LN metastasis by both MRI and histology, five (11.1%) were
tested negative by histology and positive by MRI and two (4.4%)
were tested positive by histology and negative by MRI (Table I). Based on these results, further
analysis revealed the sensitivity, specificity, PPV, NPV and
accuracy to be 85.7, 83.9, 70.6, 92.9 and 84.4%, respectively. The
κ test exposed a general outcome of 0.657 (P<0.05), suggesting
that the data obtained using histology and MRI have substantial
concordance. According to the κ test, the value for data obtained
using histology and MRI was calculated to be 1 for paraaortic LN
and 0.657 for pelvic LN (both P<0.05).
 | Table I.Patients with suspect and non-suspect
lymph nodes by MRI comparing to histopathological results. |
Table I.
Patients with suspect and non-suspect
lymph nodes by MRI comparing to histopathological results.
| MRI | Positive by
histological analysis N (%) | Negative by
histological analysis N (%) | Total N (%) |
|---|
| Positive for
suspected metastasis | 12 (26.7) | 5 (11.1) | 17 (37.8) |
| Negative for
suspected metastasis | 2 (4.4) | 26 (57.8) | 28 (62.2) |
| Total | 14 (31.1) | 31 (68.9) | 45 (100) |
To identify possible errors, the false negative and
false positive cases were analyzed further to verify the
concordance between data obtained by histological and MRI
examinations. A total of two false negative cases were found, of
which one (50%) did not reveal suspected LN metastasis by MRI and
was subsequently admitted for pelvic and paraaortic
lymphadenectomy. This patient had an important difference in the
short axis diameter by pre-operative MRI (6 mm) compared with that
revealed by histological analysis (23 mm), possibly due to the
41-day gap between MRI to surgery. The other false negative case
had suspected LN metastasis in the bilateral pelvic chains as
revealed by MRI and was admitted for paraaortic lymphadenectomy 15
days after MRI. Among the five false positive cases, three (60%)
had suspected bilateral pelvic LN metastasis as revealed by MRI,
one (20%) metastasis was detected in the right pelvic LN and one
(20%) in the left pelvic LN. All five patients were admitted for
pelvic and paraaortic lymphadenectomy. The MRI method used to
analyze paraaortic LN is a one-sequence scan that was performed
without good resolution and therefore could be the reason for
underdiagnosis. The medical records of the five false positive
cases were reviewed to examine the follow up status up until
October 2019. In total, four (80%) patients were alive without
disease and one (20%) died in 2015 as a result of cervical
cancer.
Among the 12 true positive cases, four (33.3%) had
suspected bilateral pelvic LN metastasis by MRI and were admitted
for pelvic and paraaortic surgery, three (25.0%) had suspected
right pelvic LN metastasis and received pelvic and paraaortic
surgery, two (16,7%) had suspected bilateral pelvic and paraaortic
LN metastasis and received paraaortic surgery, one (8.3%) had
suspected right pelvic LN metastasis and was admitted for right
pelvic and paraaortic surgery, one (8.3%) had suspected left pelvic
LN metastasis and received pelvic and paraaortic surgery, one
(8.3%) had suspected paraaortic LN metastasis and had paraaortic
surgery.
As aforementioned, five cases (11.1%) were
considered false positive, two (4.4%) as false negative and 12
(26.7%) as true positive, totaling 19 patients. These 19 patients
had three possible outcomes comparing both MRI and histological
analyses: i) The number of LN metastases encountered by MRI were
equal to that by histology; ii) MRI revealed more LN metastases
compared with histology; and iii) MRI encountered less LN
metastases compared with histology. Therefore, a total of 57
possible analytical combinations were found for these 19 patients.
This combination was subsequently divided according to the three
groups as listed above and to the associated lymphadenectomy chains
(LP, RP and PA). Of the 57 possible combinations, there were 30
(52.6%) cases in which had MRI and histology revealed an equal
number of metastatic LNs, 17 (29.8%) cases where MRI diagnosed a
greater number of LN metastases and 10 (17.5%) cases in which MRI
diagnosed a lower number of LN metastases compared with histology
(Table II).
 | Table II.Distribution of number of analysis
regarding number of lymph nodes encountered, according to
lymphadenectomy performed and pre-operative MRI evaluation. |
Table II.
Distribution of number of analysis
regarding number of lymph nodes encountered, according to
lymphadenectomy performed and pre-operative MRI evaluation.
| Chain | MRI=histology N
(%) | MRI > histology N
(%) | MRI < histology N
(%) | Total N (%) |
|---|
| False positive |
|
|
|
|
| LP | 1 (6.7) | 4 (26.7) | 0 (0.0) | 5 (33.3) |
| RP | 1 (6.7) | 4 (26.7) | 0 (0.0) | 5 (33.3) |
| PA | 4 (26.7) | 0 (0.0) | 1 (6.7) | 5 (33.3) |
| Sub.
Total | 6 (40.0) | 8 (53.3) | 1 (6.7) | 15 (100.0) |
| False negative |
|
|
|
|
| LP | 0 (0.0) | 1 (16.7) | 1 (16.7) | 2 (33.3) |
| RP | 1 (16.7) | 1 (16.7) | 0 (0.0) | 2 (33.3) |
| PA | 1 (16.7) | 0 (0.0) | 1 (16.7) | 2 (33.3) |
| Sub.
Total | 2 (33.3) | 2 (33.3) | 2 (33.3) | 6 (100.0) |
| True positive |
|
|
|
|
| LP | 9 (25.0) | 3 (8.3) | 0 (0.0) | 12 (33.3) |
| RP | 5 (13.9) | 4 (11.1) | 3 (8.3) | 12 (33.3) |
|
PAs | 8 (22.2) | 0 (0.0) | 4 (11.1) | 12 (33.3) |
| Sub.
Total | 22 (61.1) | 7 (19.4) | 7 (19.4) | 36 (100.0) |
| Total | 30 (52.6) | 17 (29.8) | 10 (17.5) | 57 (100) |
Among all lymphadenectomies (pelvic and/or
para-aortic) performed, a total of 976 LNs were resected. Of these,
41 (4.2%) were confirmed to be positive by histological analysis
for metastasis whilst 935 (95.8%) were considered negative by
histology. Further analysis revealed that from the 41 positive LNs,
three (7.3%) were encountered in the LP, 10 (24.4%) in the RP, 18
(43.9%) in the PA, four (9.8%) in both LP and RP and six (14.6%) in
pelvic (LP and/or RP) and PA.
MRI analyses
In terms of exam quality, examination of all 45
patients (100%) resulted in a successful diagnosis. A total of 44
LNs were analyzed using MRI, of which 42 (95.5%) were suspected to
be metastatic by MRI and two (4.5%) were considered to be negative
for metastasis. Among the 44 cases, two (4.5%) were found in the
LP, eight (18.2%) in the RP, two (4.5%) in the PA, 19 (43.2%) in
both LP and RP, and 13 (29.5%) in pelvic (left and/or right) and
PA.
The morphological characteristics of the 42 (95.5%)
suspected LN metastases as determined by DWI in MRIs were then
compared against their corresponding histology data, which is
considered to be the golden-standard. It was found that those with
short axes >10 mm had an major impact in determining the
probability of an LN being metastatic in subsequent histological
analyses, as 90.5% of the metastatic LNs found using MRI that were
>10 mm were subsequently found to be metastatic in histological
analysis. LN metastases with T2 hypointensities had an association
of 81.0%, rounded morphology had an association of 78.6%, greater
restriction than one would expect for this tissue had an
association of 76.2%, heterogenous appearance had an association of
69%, presence of necrosis had an association of 47.6% whilst LN
metastases with irregular limits had an association of 40.5%
(Table III). When investigating the
smallest diameter of the short axis in suspected metastases in LNs
using MRI, it was concluded that the median size of all suspected
metastases in LNs was 16.8 mm (5–50 mm), with a standard deviation
of 0.96.
 | Table III.Association between suspect lymph
nodes in morphological and functional features revealed using MRI
that were subsequently found to be positive for metastasis by
histological analysis. |
Table III.
Association between suspect lymph
nodes in morphological and functional features revealed using MRI
that were subsequently found to be positive for metastasis by
histological analysis.
| MRI finding | Metastasis-positive
lymph nodes by histology N (%) |
|---|
| Short-axis >10
mm | 38 (90.5) |
| T2
hipointensity | 34 (81.0) |
| Rounded
morphology | 33 (78.6) |
| Greater restriction
than one would expect | 32 (76.2) |
| Heterogeneous
appearance | 29 (69.0) |
| Presence of
necrosis | 20 (47.6) |
| Irregular
limits | 17 (40.5) |
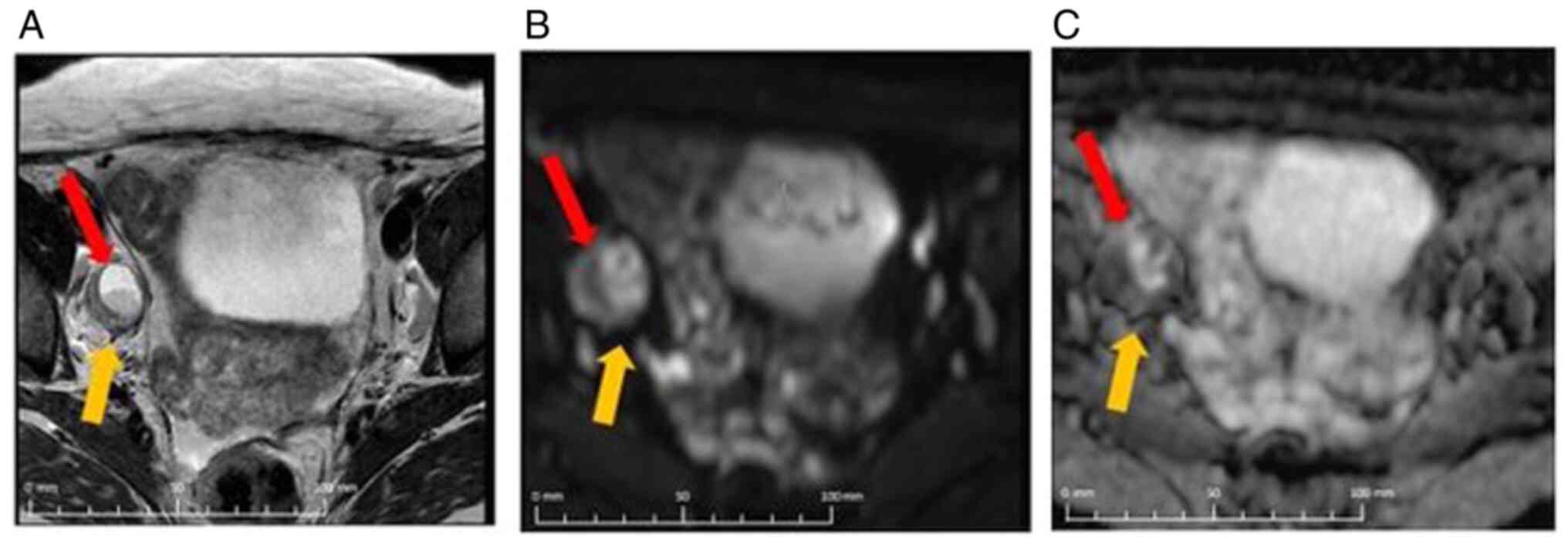
A representative case of a true positive patient
with a metastatic LN as diagnosed by MRI and histological analysis,
both in the RP chain is shown in Fig.
2. Morphological and functional characteristics that were
associated with metastatic status were short-axis diameter
measuring 21 mm, presence of necrosis associated with liquid level,
areas with greater restriction than would be expected for this
tissue, presence of round morphology and heterogenous appearance
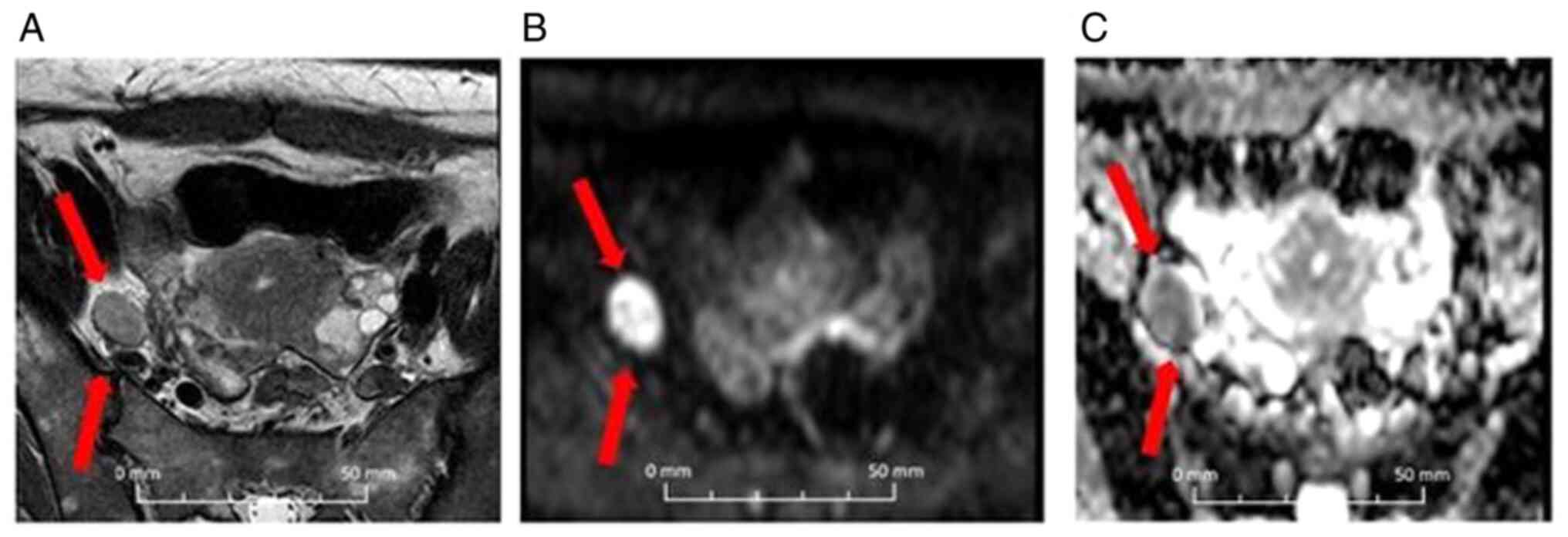
and irregular limits. For comparative purposes, a representative
case of a false positive exam was also shown (Fig. 3). This patient was tested positive for
LN metastasis in the RP by MRI and but negative by histological
analysis. The morphological and functional characteristics that
were associated with this image are short-axis diameter measuring
14 mm, areas with greater restriction than one would expect,
rounded morphology, homogenous appearance and regular limits.
Discussion
In the present study the accuracy of MRI in
diagnosing LN metastasis in patients with cervical cancer was
compared against that of histological analysis, with emphasis on
common morphological and functional (DWI) characteristics. By
analyzing the combined morphological and functional characteristics
of LN metastases, it was found that a substantial concordance
between the data obtained using pre-operative MRI and histology can
be achieved with high sensitivity and specificity. In addition, it
was found that short axis >10 mm, T2 hypointensity, rounded
morphology and greater restriction than one would expect were the
most common characteristics encountered in metastatic LNs, which
can be used as a diagnostic tool. A technical pelvic exam,
performed in all steps with proper technique by a trained
specialist, can also be used to predict FIGO staging, since the
majority of the patients included in the present study exhibited
concordant results between those obtained by physical and MRI
examinations, especially for the presence of pelvic and para-aortic
LN metastasis. Additionally, MRI was able to correctly identify the
number of suspected LN metastases, specifically in >50% of the
possible candidates for lymphadenectomy. These results potentially
underline the important role of MRI in diagnosing LN metastasis,
especially in the presence of the features aforementioned.
When comparing the number of patients tested
positively for suspected LN using MRI, the present study revealed a
sensitivity of 85.7% and NPV of 92.9%, when other previous studies
(3,15,16)
yielded 92, 86 and 92.1% for sensitivity and 98.2, 84 and 100% for
NPV, respectively. Previous studies (2,17) also
compared the importance of MRI images using DWI for diagnosing
metastatic LN, resulting in values of 83.3 and 95.7% being deduced
for sensitivity and 74.7 and 96.5% for specificity, respectively.
Although the total number of patients in the present study was
considered low, concordance with the current literature exist in
terms of outcomes, as 85.7% was found for sensitivity and 83.9% was
found for specificity in the present study. A previous
meta-analysis performed by Liu et al (18) compared 67 studies which investigated
MRI performance in diagnosing suspected LN metastasis in cervical
cancer. The average of sensitivity and specificity were found to be
54 and 93%, respectively. Chou et al (19) showed that the moderate false-negative
and false-positive rates found for MRI is due to some patients
being staged as IA2-IIA, which can explain some lower sensitivities
observed (19,20). Therefore, it is essential do use the
ADC maps to address this issue (21–24).
It is generally considered that MRI exhibits higher
degrees of diagnostic accuracy in patients with advanced disease,
since the associated LNs are larger in size and has clearer defined
features such as necrosis (25).
Therefore, patients with early stage metastatic disease may be
underdiagnosed using this method (25). This aspect may be considered to be a
limitation in the results from the present study, combined with the
low resolution in the paraaortic sequences.
Lymph node metastasis is one of the most important
features to be categorized in cervical cancer, which serves as an
important prognostic factor for patients with this disease.
Therefore, it is important to differentiate healthy LNs from
suspected metastatic LNs. Generally, healthy LNs tend to be ovoid
in shape, homogenous in appearance, with intermediate signals in
T2-weighted sequences and high signals in DWI sequences (26). In the present study, it was found that
the four most common morphological and functional characteristics
associated with the higher risk of malignancy in pelvic and/or
para-aortic LN metastasis as diagnosed by MRI are, in decreasing
order, short axis >10 mm, T2 hypointensity, rounded morphology
followed by greater restriction than one would expect. It became
clear that the combination of these features using MRI can predict
suspected LN metastasis with high probability. These findings
highlight the benefit of having a protocol to ensure the early and
safe diagnosis of metastasis in lymph nodes.
Exner et al (4)
hypothesized that the most important predictor for the probability
of malignancy is the size of the LN. By contrast, Hawnaur et
al (27) demonstrated a LN to be
malignant when the short-axis was calculated to be >10 mm.
However, other authors claimed that size alone is not a
sufficiently adequate prognostic indicator whilst highlighting the
necessity for including morphological data into the analysis,
including limits, morphology and the presence of necrosis (11,12,28); all
of which were included in the present study in addition to
functional aspects (DWI). Indeed, diagnostic accuracy can be
improved by combining morphological and functional data found using
MRI, especially short axis >10 mm, T2 hypointensity, rounded
morphology and greater restriction than one would expect. However,
when patients are exposed to radiation and/or chemotherapy,
morphology and diffusion can alter the tumor tissue, increasing the
difficulty in obtaining parameters of the tissue itself without any
interference. Liyanage et al (29) previously confirmed that when the
specificity and sensitivity for the standard criteria as
aforementioned is low (29–86%), the difficulty in detecting
micro-metastases in normal sized LNs increases.
The importance of using PET-CT for pre-operative
examinations of potential LN metastases to detect anatomical and
metabolic deviations from healthy LNs should also be recognized
(30). Lin et al (31) evaluated the use of PET-CT in
pre-operative assessments of patients with squamous cervical cancer
associated with positive pelvic LN metastasis, which showed the
sensitivity, specificity, PPV and NPV to be 44, 99, 95 and 78%,
respectively. A meta-analysis performed by Yu et al
(32) investigated sensitivity and
specificity for patients with cervical cancer and positive for
para-aortic LN, which were found to be 71 and 95%, respectively.
The present study yielded the sensitivity, specificity, PPV and NPV
for using MRI obtained for diagnosing pelvic and para-aortic LN
metastasis to be similar to those obtained from PET-CT analysis in
previous studies: 85.7, 83.9, 70.6, 92.9 and 84.4%, respectively.
Therefore, focusing on short axis >10 mm, T2 hypointensity,
rounded morphology and greater restriction than one would expect
using MRI can increase the accuracy of early diagnosis. Some of
these aspects were mentioned in previous studies with PET-CT
(30) and the present study
demonstrated that these same aspects can also be applied in MRI
examinations without compromising accuracy.
The strength of the present study was that the
morphological features of the LN metastases obtained using MRI were
evaluated in several categories, which were then analyzed in
association with DWI and histopathological results. The limitation
of the present study is the low sample number of patients. However,
the patients included in this study required nodal commitment and
were admitted to receive systematic lymphadenectomy. In addition,
it should be recognized that MRI alone is insufficient for
providing correct evaluations of metastasis in the paraaortic
chain. Novel studies to confirm the results obtained from the
present study is strongly encouraged. However, since the results
performed in the present study were concordant with the current
literature, it can serve as an template that can be replicated in a
subsequent study involving larger cohorts of patients.
In conclusion, to the best of the authors knowledge,
the present study was the first to evaluate LN metastasis by using
a number of morphological and functional categories. It was found
that the most important features found in LN metastases using MRI
are short axis >10 mm, T2 hypointensity, rounded morphology and
greater restriction than one would expect. If these four categories
are combined in MRI, the likelihood of the LN in question harboring
a metastatic tumor by subsequent histological examination is high.
This can potentially guide the decision-making process in the types
of surgery or even types of therapeutic intervention required. If
PET-CT is not available, the use of DWI to obtain morphological
data in defining LN metastasis is recommended for pre-operative
examinations.
Acknowledgements
Not applicable.
Funding
The present study was supported by Fundação de
Amparo à Pesquisa do Estado de São Paulo (FAPESP).
Availability of data and materials
The datasets generated and/or analyzed during the
current study are available in the [Figshare] repository
(https://figshare.com/s/878e54ea121d972aa408).
Authors contributions
TD reviewed and collected patient data from patient
charts, participated in statistical analyses and was the main
writer. RRR and MDS reviewed and analyzed the MRI images, and
participated in paper construction and provided final approval of
the version to be published. CEMDCA, RS and MAV collected data from
patients, participated in paper construction and final approval of
the version to be published. MAL performed statistical analyses and
participated in paper construction. DAPDA contributed to the
discussion of results and participated in paper construction and
final approval of the version to be published. RDR collected data
from patients in consults in our hospital, reviewed and oriented
all steps in the study, including reviewing the paper in all
phases, participated in paper construction and designed the study.
All authors read and approved the final version of this
manuscript.
Ethics approval and consent to
participate
Approval for the present study was obtained from The
Ethical Committee of Barretos Cancer Hospital (approval no.
1150/2016; Barretos, Brazil). All patients consented to the use of
their medical records in the current study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
American Cancer Society, . Cancer Facts
and Figures, 2018. 2018, https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2018/cancer-facts-and-figures-2018.pdf
|
|
2
|
Liu Y, Liu H, Bai X, Ye Z, Sun H, Bai R
and Wang D: Differentiation of metastatic from non-metastatic
lymph-nodes in patients with uterine cervical cancer using
diffusion-weighted imaging. Gynecol Oncol. 122:19–24. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Klerkx W, Veldhuis W, Spijkerboer A, van
den Bosch MA, Mali WP, Heintz AP, Bipat S, Sie-Go DM, van der
Velden J, Schreuder HW, et al: The value of 3.0Tesla
diffusion-weighted MRI for pelvic nodal staging in patients with
early stage cervical cancer. Eur J Cancer. 48:3414–3421. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Exner M, Kühn A, Stumpp P, Höckel M, Horn
LC, Kahn T and Brandmaier P: Value diffusion-wheighted MRI in
diagnosis of uterine cervical cancer: A prosprctive study
evaluating the benefits of DWI compared to convencional MR
sequences in a 3T environment. Acta Radiol. 57:869–877. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Seber T, Caglar E, Uglar T, Karaman N,
Aktas E and Aribas BK: Diagnostic value of diffusion-weighted
magnetic resonance imaging: Differentiation of benign and malignent
lhymh nodes in different regions of the body. Clin Imaging.
39:856–862. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Vandecaveye V, Dresen R and De Keyser F:
Novel imaging techiniques in gynecological cancer. Curr Opin Oncol.
29:335–342. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Nakai G, Matsuki M, Inada Y, Tatsugami F,
Tanikake M, Narabayashi I and Yamada T: Detection and evaluation of
pelvic lymph nodes in patients with gynecologic malignances using
body diffusion-wheighted maginetic resonance imaging. J Compute
Assist Tomogr. 32:764–768. 2008. View Article : Google Scholar
|
|
8
|
He XQ and Wei LN: Diagnostic value of
lymph node metastasis by diffusion-weighted magnetic resonance
imaging in cervical cancer. J Cancer Res Ther. 12:77–83. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lin G, Ho KC, Wang JJ, Ng KK, Wai YY, Chen
YT, Chang CJ, Ng SH, Lai CH and Yen TC: Detection of lymph node
metastasis in cervical and uterine cancers by diffusion-weighted
magnetic resonance imaging at 3T. J Magn Reson Imaging. 28:128–135.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Fenell J, Scholber J, Grosu AL,
Volegova-Neher N, Henne K, Langer M, Meyer PT, Gitsch G and Bartl
N: MRI and FDG-PET/CT imaging in gynecological malignances: The
radiation oncology perspective. Q J Nucl Med Mol Imaging.
60:117–123
|
|
11
|
Yang WT, Lam WW, Yu MY, Cheung TH and
Metreweli C: Comparison of dynamic helical CT and dynamc MR imaging
in the evaluation of pelvic lyhmph nodes in cervical carcinoma. ARJ
Am J Roentgenol. 175:759–766. 2000. View Article : Google Scholar
|
|
12
|
Jung W, Park KR, Lee KJ, Kim K, Lee J,
Jeong S, Kim YJ, Kim J, Yoon HJ, Kang BC, et al: Value of imaging
study in predicting pelvic lymph node metastasis of uterine
cervical cancer. Radiat Oncol J. 35:340–348. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Bathala N, Berek J, Fredes M, Denny LA,
Grenman S, Karunaratne K, Kehoe ST, Konishi I, Olawaiye AB, Prat J,
et al: Cancer of the corpus uteri. Int J Ginecol Obstet:.
145:129–135. 2019.
|
|
14
|
Harris PA, Taylor R, Thielke R, Payne J,
Gonzalez N and Conde JG: Research electronic data capture
(REDCap)-a metadata-driven methodology and workflow process for
providing translational research informatics support. J Biomed
Inform. 42:377–381. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Shen G, Zhou H, Jia Z and Deng H:
Diagnostic performance of difussion-wietihged MRI for detection of
pelvic metastatic lymph nodes in patients with cervical cancer: A
systematic review and meta-analysis. Br J Radiol. 88:201500632015.
View Article : Google Scholar
|
|
16
|
Lucas R, Dias J and Cunha TM: Added value
of diffusion-wheighted MRI in detection of cervical cancer
recurrance: Comparison with morfological and dynamic
contrast-enanced MRI sequences. Diagn Interv Radiol. 21:368–375.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Chen YB, Liao J, Xie R, Chen GL and Chen
G: Discrimination of metastatic from hyperplastic pelvic lymph
nodes in patients with cervical cancer by diffusion-weighted
magnetic resonance imaging. Abdom Imaging. 36:102–109. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Liu B, Gao S and Li S: A Comprehensive
Comparison of CT, MRI, Positron Emission tomography or positron
emission Tomography/CT, and diffusion weighted Imaging-MRI for
detecting the lymph nodes metastases in patients with cervical
cancer: A meta-analysis based on 67 studies. Gynecol Obstet Invest.
82:209–222. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Chou HH, Chang TC, Yen TC, Ng KK, Hsueh S,
Ma SY, Chang CJ, Huang HJ, Chao A, Wu TI, et al: Low value of
[18F]-fluoro-2-deoxy-D-glucose positron emission tomography in
primary staging of early-stage cervical cancer before radical
hysterectomy. J Clin Oncol. 24:123–128. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Driscoll DO, Halpenny D, Jhonston C,
Sheehy N and Keogan M: 18-F-FDG-PET-CT is of limited value in
primary staging of early stage cervical cancer. Abdom Imaging.
40:127–133. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Schieda N, Malone SC, Al Dandan O,
Ramchandani P and Siegelman ES: Multi-modality organ-based approach
to expected imaging findings, complications and recurrent tumour in
the genitourinary tract after radiotherapy. Insights Imaging.
5:25–40. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Vincens E, Balleyguier C, Rey A, Uzan C,
Zareski E, Gouy S, Pautier P, Duvillard P, Haie-Meder C and Morice
P: Accuracy of magnetic resonance imaging in predicting residual
disease in patients treated for stage IB2/II cervical carcinoma
with chemoradiation therapy: Correlation of radiologic findings
with surgicopathologic results. Cancer. 113:2158–2165. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Levy A, Caramella C, Chargari C, Medjhoul
A, Rey A, Zareski E, Boulet B, Bidault F, Dromain C and Balleyguier
C: Accuracy of diffusion-weighted echo-planar MR imaging and ADC
mapping in the evaluation of residual cervical carcinoma after
radiation therapy. Gynecol Oncol. 123:110–115. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Harry VN, Semple SI, Gilbert FJ and Parkin
DE: Diffusion-weighted magnetic resonance imaging in the early
detection of response to chemoradiation in cervical cancer. Gynecol
Oncol. 111:213–220. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Song J, Hu Q, Huang J, Ma Z and Chen T:
Combining tumor size and diffusion-weighted imaging to diagnose
normal-sized metastatic pelvic lymph nodes in cervical cancers.
Acta Radiol. 60:388–395. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Bourgiot C, Chatoupis K and Moulopoulos L:
Current imaging strategies for the evaluation of uterine cervical
cancer. World J Radiol. 8:342–354. 2016. View Article : Google Scholar
|
|
27
|
Hawnaur JM, Carrington BM, Hunter RD and
Isherwood I: Treatment response in carcinoma of the uterine cervix:
Evaluation by magnetic resonance imaging. Tumor Response Monitoring
and Treatment Planning. Breit A, Heuck A, Lukas P, Kneschaurek P
and Mayr M: Springer; Heidelberg: 1992, View Article : Google Scholar
|
|
28
|
Choi HJ, Kim SH, Seo SS, Kang S, Lee S,
Kim JY, Kim YH, Lee JS, Chung HH, Lee JH and Park SY: MRI for
pretreatment lymph node staging in uterine cervical cancer. Am J
Roentgenol. 187:W538–W543. 2006. View Article : Google Scholar
|
|
29
|
Liyanage SH, Roberts CA and Rockall AG:
MRI and PET scans for primary staging and detection of cervical
cancer recurrance. Womens Health (Lond). 6:251–269. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Li K, Sun H and Guo Q: Combinative
evaluation of primary tumor and lymph nodes in predicting pelvic
lymphatic metastasis in early-stage cervical cancer: A
multiparametric PET-CT study. Eur J Radiol. 113:153–157. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Lin AJ, Wright JD, Dehdashti F, Siegel BA,
Markovina S, Schwarz J, Thaker PH, Mutch DG, Powell MA and Grigsby
PW: Impact of tumor histology on detection of pelvic and
para-aortic nodal metastasis with
18F-fluorodeoxyglucose-positron emission tomography in
stage IB cervical cancer. Int J Gynecol Cancer. 29:1351–1354. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Yu W, Kou C, Bai W, Yu X, Duan R, Zhu B,
Li Y, Hua W, Ren X and Yang Y: The diagnostic performance of PET/CT
scans for the detection of para-aortic metastatic lymph nodes in
patients with cervical cancer: A meta-analysis. PLoS One.
14:e02200802019. View Article : Google Scholar : PubMed/NCBI
|