|
1
|
Hashibe M, Boffetta P, Zaridze D, Shangina
O, Szeszeni-Dabrowska N, Mates D, Fabiánová E, Rudnai P and Brennan
P: Contribution of tobacco and alcohol to the high rates of
squamous cell carcinoma of the supraglottis and glottis in Central
Europe. Am J Epidemiol. 165:814–820. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Curado MP and Hashibe M: Recent changes in
the epidemiology of head and neck cancer. Curr Opin Oncol.
21:194–200. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Talamini R, Bosetti C, La Vecchia C, Dal
Maso L, Levi F, Bidoli E, Negri E, Pasche C, Vaccarella S, Barzan L
and Franceschi S: Combined effect of tobacco and alcohol on
laryngeal cancer risk: A case-control study. Cancer Causes Control.
13:957–964. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Pöschl G and Seitz HK: Alcohol and cancer.
Alcohol Alcohol. 39:155–165. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Galli J, Cammarota G, De Corso E, Agostino
S, Cianci R, Almadori G and Paludetti G: Biliary laryngopharyngeal
reflux: A new pathological entity. Curr Opin Otolaryngol Head Neck
Surg. 14:128–132. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Tutar H, Erdamar H, Köybaşioğlu A, Dinç
AE, Ceylan A and Uslu S: Can bile acids be an etiological factor
for laryngeal carcinoma? ORL J Otorhinolaryngol Relat Spec.
73:156–161. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Geterud A, Bove M and Ruth M:
Hypopharyngeal acid exposure: An independent risk factor for
laryngeal cancer? Laryngoscope. 113:2201–2205. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Sereg-Bahar M, Jerin A and
Hocevar-Boltezar I: Higher levels of total pepsin and bile acids in
the saliva as a possible risk factor for early laryngeal cancer.
Radiol Oncol. 49:59–64. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Altman KW, Prufer N and Vaezi MF: A review
of clinical practice guidelines for reflux disease: toward creating
a clinical protocol for the otolaryngologist. Laryngoscope.
121:717–723. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Assimakopoulos D and Patrikakos G: The
role of gastroesophageal reflux in the pathogenesis of laryngeal
carcinoma. Am J Otolaryngol. 23:351–357. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Sasaki CT, Marotta J, Hundal J, Chow J and
Eisen RN: Bile-induced laryngitis: Is there a basis in evidence?
Ann Otol Rhinol Laryngol. 114:192–197. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
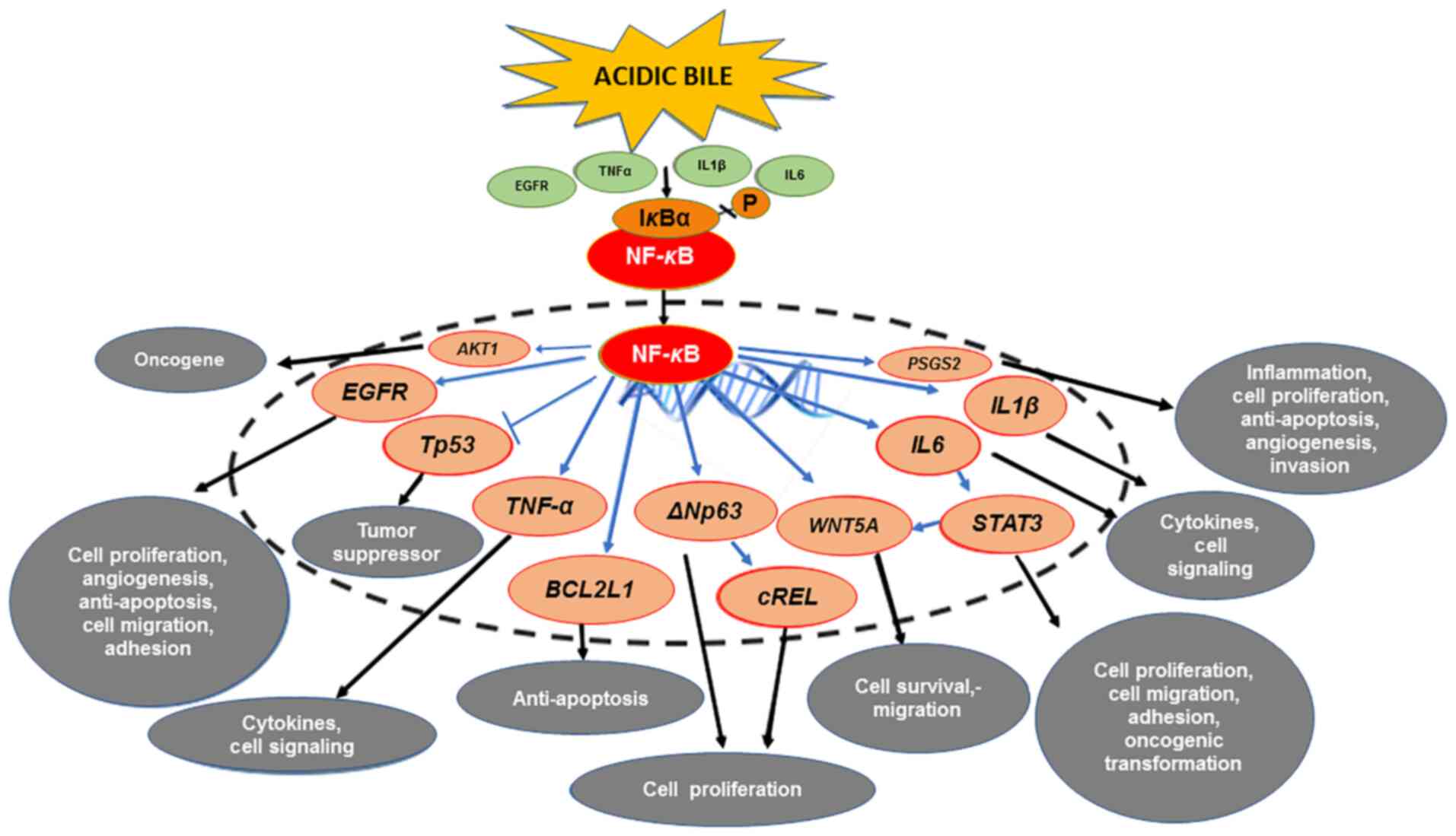
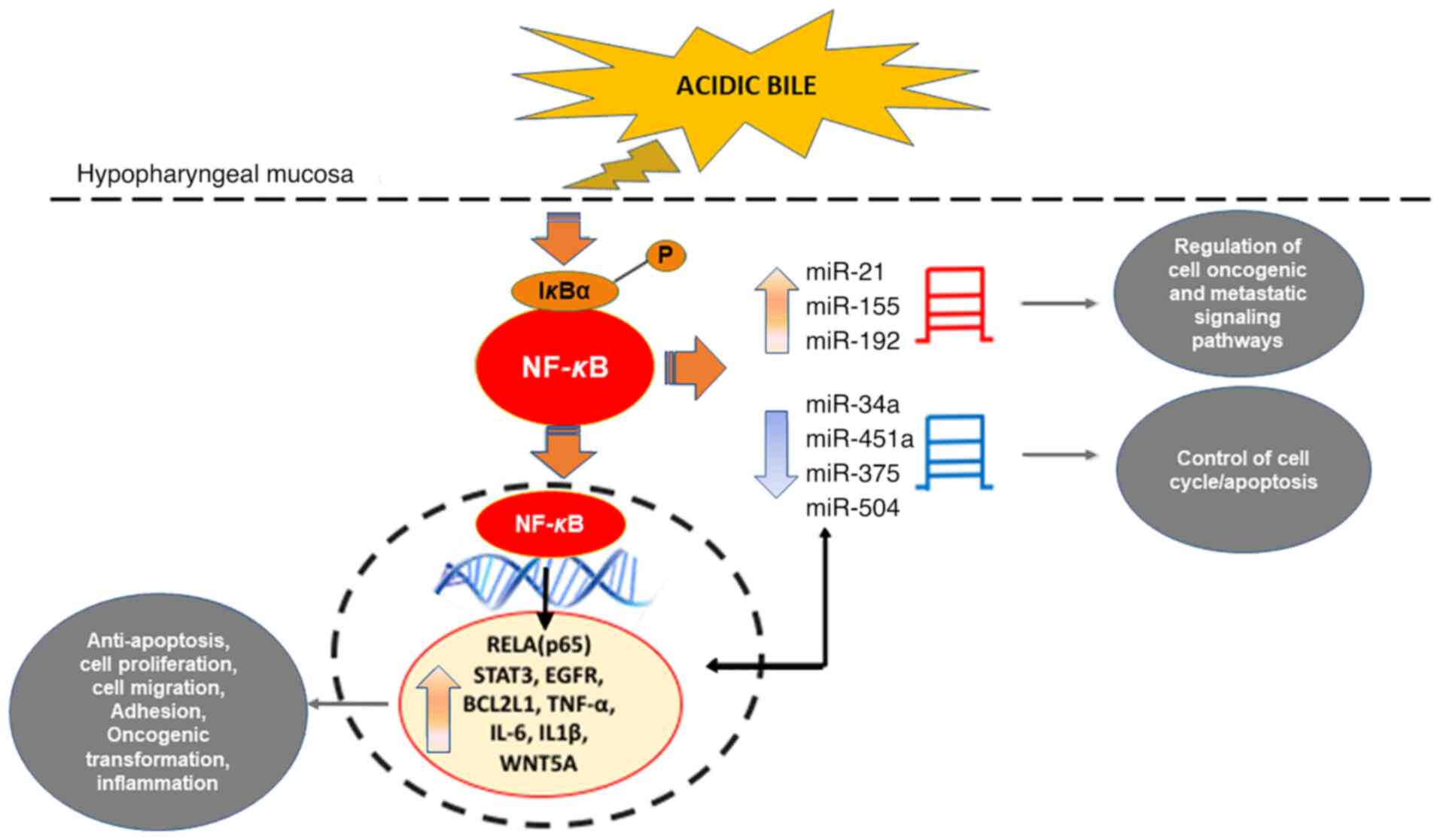
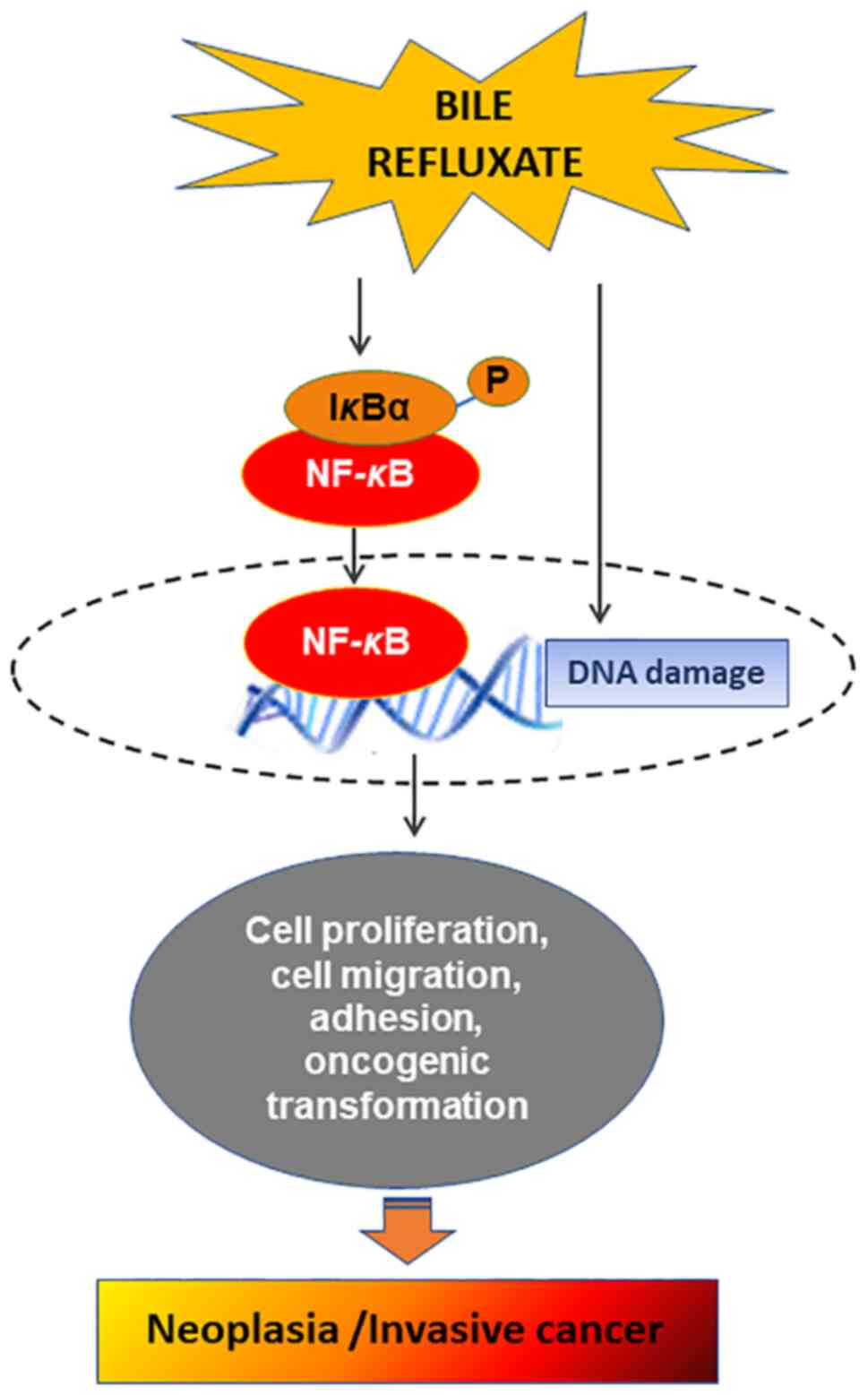
Sasaki CT, Issaeva N and Vageli DP: In
vitro model for gastroduodenal reflux-induced nuclear factor-kappaB
activation and its role in hypopharyngeal carcinogenesis. Head
Neck. 38 (Suppl 1):E1381–E1391. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Vageli DP, Prasad ML and Sasaki CT:
Gastro-duodenal fluid induced nuclear Factor-κappaB activation and
early pre-malignant alterations in murine hypopharyngeal mucosa.
Oncotarget. 7:5892–5908. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
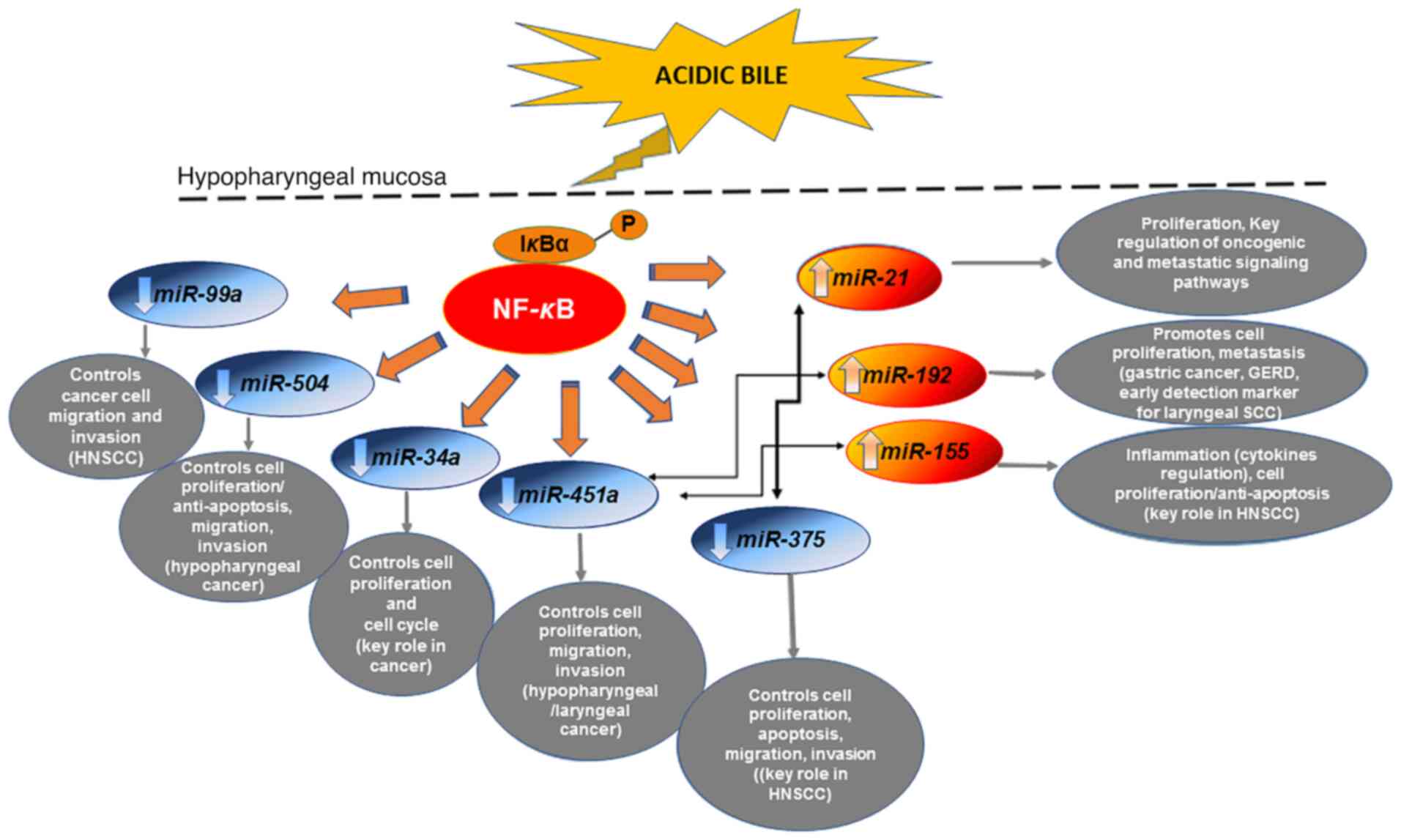
Sasaki CT and Vageli DP: MiR-21, miR-155,
miR-192, and miR-375 deregulations related to NF-kappaB activation
in gastroduodenal Fluid-Induced early Preneoplastic lesions of
laryngeal mucosa in vivo. Neoplasia. 18:329–338. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Sasaki CT, Doukas SG, Costa J and Vageli
DP: The progressive mutagenic effects of acidic bile refluxate in
hypopharyngeal squamous cell carcinogenesis: New insights. Cancers
(Basel). 12:10642020. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Sasaki CT, Doukas SG, Doukas PG and Vageli
DP: Weakly acidic bile is a risk factor for hypopharyngeal
carcinogenesis evidenced by DNA damage, antiapoptotic function, and
premalignant dysplastic lesions in vivo. Cancers (Basel).
13:8522021. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Doukas SG, Cardoso B, Tower JI, Vageli DP
and Sasaki CT: Biliary tumorigenic effect on hypopharyngeal cells
is significantly enhanced by pH reduction. Cancer Med. 8:4417–4427.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Sasaki CT, Doukas SG, Costa J and Vageli
DP: Biliary reflux as a causal factor in hypopharyngeal carcinoma:
New clinical evidence and implications. Cancer. 125:3554–3565.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Sasaki CT, Doukas SG and Vageli DP: In
Vivo Short-Term topical application of BAY 11-7082 prevents the
acidic Bile-Induced mRNA and miRNA oncogenic phenotypes in exposed
Murine Hypopharyngeal Mucosa. Neoplasia. 20:374–386. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Vageli DP, Doukas SG, Spock T and Sasaki
CT: Curcumin prevents the bile reflux-induced NF-κB-related mRNA
oncogenic phenotype, in human hypopharyngeal cells. J Cell Mol Med.
22:4209–4220. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Vageli DP, Doukas SG and Sasaki CT:
Inhibition of NF-kappaB prevents the acidic bile-induced oncogenic
mRNA phenotype, in human hypopharyngeal cells. Oncotarget.
9:5876–5891. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Doukas SG, Vageli DP and Sasaki CT: NF-κB
inhibition reverses acidic bile-induced miR-21, miR-155, miR-192,
miR-34a, miR-375 and miR-451a deregulations in human hypopharyngeal
cells. J Cell Mol Med. 22:2922–2934. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Doukas PG, Vageli DP, Doukas SG and Sasaki
CT: Temporal characteristics of NF-κB inhibition in blocking
bile-induced oncogenic molecular events in hypopharyngeal cells.
Oncotarget. 10:3339–3351. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Doukas SG, Doukas PG, Sasaki CT and Vageli
D: The in vivo preventive and therapeutic properties of curcumin in
bile reflux-related oncogenesis of the hypopharynx. J Cell Mol Med.
24:10311–10321. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Vageli DP, Kasle D, Doukas SG, Doukas PG
and Sasaki CT: The temporal effects of topical NF-κB inhibition, in
the in vivo prevention of bile-related oncogenic mRNA and miRNA
phenotypes in murine hypopharyngeal mucosa: A preclinical model.
Oncotarget. 11:3303–3314. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Hofmann AF: Chemistry and enterohepatic
circulation of bile acids. Hepatology. 4 (Suppl 5):4S–14S. 1984.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Greek Medicine, . http://www.greekmedicine.net/b_p/Four_Humors.html
|
|
28
|
Rather LJ: Disturbance of function
(functio laesa): The legendary fifth cardinal sign of inflammation,
added by Galen to the four cardinal signs of Celsus. Bull NY Acad
Med. 47:303–322. 1971.PubMed/NCBI
|
|
29
|
Virchow R and Rather LJ: Disease, Life,
and Man: Selected Essays. Stanford University Press; Stanford, CA:
1958
|
|
30
|
Cook JW: Carcinogenic chemical agents.
Yale J Biol Med. 11:1–13. 1938.PubMed/NCBI
|
|
31
|
Bernstein H, Bernstein C, Payne CM,
Dvorakova K and Garewal H: Bile acids as carcinogens in human
gastrointestinal cancers. Mutat Res. 589:47–65. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Kuwahara A, Saito T and Kobayashi M: Bile
acids promote carcinogenesis in the remnant stomach of rats. J
Cancer Res Clin Oncol. 115:423–428. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Hill MJ: Bile flow and colon cancer. Mutat
Res. 238:313–320. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Bayerdörffer E, Mannes GA, Ochsenkühn T,
Dirschedl P, Wiebecke B and Paumgartner G: Unconjugated secondary
bile acids in the serum of patients with colorectal adenomas. Gut.
36:268–273. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Nehra D, Howell P, Williams CP, Pye JK and
Beynon J: Toxic bile acids in gastro-oesophageal reflux disease:
Influence of gastric acidity. Gut. 44:598–602. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Vaezi MF and Richter JE: Double reflux:
Double trouble. Gut. 44:590–592. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Vaezi MF, Singh S and Richter JE: Role of
acid and duodenogastric reflux in esophageal mucosal injury: A
review of animal and human studies. Gastroenterology.
108:1897–1907. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Gotley DC, Morgan AP and Cooper MJ: Bile
acid concentrations in the refluxate of patients with reflux
oesophagitis. Br J Surg. 75:587–590. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Kauer WK, Peters JH, DeMeester TR, Ireland
AP, Bremner CG and Hagen JA: Mixed reflux of gastric and duodenal
juices is more harmful to the esophagus than gastric juice alone.
The need for surgical therapy re-emphasized. Ann Surg. 222:525–531.
1995. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Kauer WK, Peters JH, DeMeester TR,
Feussner H, Ireland AP, Stein HJ and Siewert RJ: Composition and
concentration of bile acid reflux into the esophagus of patients
with gastroesophageal reflux disease. Surgery. 122:874–881. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Domellof L, Reddy BS and Weisburger JH:
Microflora and deconjugation of bile acids in alkaline reflux after
partial gastrectomy. Am J Surg. 140:291–295. 1980. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Fein M, Peters JH, Chandrasoma P, Ireland
AP, Oberg S, Ritter MP, Bremner CG, Hagen JA and DeMeester TR:
Duodenoesophageal reflux induces esophageal adenocarcinoma without
exogenous carcinogen. J Gastrointest Surg. 2:260–268. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
McQuaid KR, Laine L, Fennerty MB, Souza R
and Spechler SJ: Systematic review: The role of bile acids in the
pathogenesis of gastro-oesophageal reflux disease and related
neoplasia. Aliment Pharmacol Ther. 34:146–165. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Oh DS, Hagen JA, Fein M, Bremner CG, Dunst
CM, Demeester SR, Lipham J and Demeester TR: The impact of reflux
composition on mucosal injury and esophageal function. J
Gastrointest Surg. 10:787–796. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Sweet MP, Patti MG, Hoopes C, Hays SR and
Golden JA: Gastro-oesophageal reflux and aspiration in patients
with advanced lung disease. Thorax. 64:167–173. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Covington MF, Krupinski E, Avery RJ and
Kuo PH: Classification schema of symptomatic enterogastric reflux
utilizing sincalide augmentation on hepatobiliary scintigraphy. J
Nucl Med Technol. 42:198–202. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Lewin JS, Gillenwater AM, Garrett JD,
Bishop-Leone JK, Nguyen DD, Callender DL, Ayers GD and Myers JN:
Characterization of laryngopharyngeal reflux in patients with
premalignant or early carcinomas of the larynx. Cancer.
97:1010–1014. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Johnston N, Ondrey F, Rosen R, Hurley BP,
Gould J, Allen J, DelGaudio J and Altman KW: Airway reflux. Ann N Y
Acad Sci. 1381:5–13. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Adams J, Heintz P, Gross N, Andersen P,
Everts E, Wax M and Cohen J: Acid/pepsin promotion of
carcinogenesis in the hamster cheek pouch. Arch Otolaryngol Head
Neck Surg. 126:405–409. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Johnston N, Dettmar PW, Ondrey FG, Nanchal
R, Lee SH and Bock JM: Pepsin: Biomarker, mediator, and therapeutic
target for reflux and aspiration. Ann NY Acad Sci. 1434:282–289.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Johnston N, Wells CW, Samuels TL and
Blumin JH: Pepsin in nonacidic refluxate can damage hypopharyngeal
epithelial cells. Ann Otol Rhinol Laryngol. 118:677–685. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Del Negro A, Araújo MR, Tincani AJ,
Meirelles L, Martins AS and Andreollo NA: Experimental
carcinogenesis on the oropharyngeal mucosa of rats with
hydrochloric acid, sodium nitrate and pepsin. Acta Cir Bras.
23:337–342. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Sasaki CT, Toman J and Vageli D: The in
vitro effect of Acidic-Pepsin on nuclear factor KappaB activation
and its related oncogenic effect on normal human hypopharyngeal
cells. PLoS One. 11:e01682692016. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Doukas PG, Vageli DP, Sasaki CT and Judson
BL: Pepsin promotes activation of epidermal growth factor receptor
and downstream oncogenic pathways, at slightly acidic and neutral
pH, in exposed hypopharyngeal cells. Int J Mol Sci. 22:42752021.
View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Goldstein JL, Schlesinger PK, Mozwecz HL
and Layden TJ: Esophageal mucosal resistance. A factor in
esophagitis. Gastroenterol Clin North Am. 19:565–586. 1990.
View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Stamp D and Jenkins G: An overview of
bile-acid synthesis, chemistry and function. Bile Acids: Toxicology
and Bioactivity. Jenkins GJ and Hardie L: Royal Society of
Chemistry; Cambridge: 2008, Print: Issues in Toxicology; 4.
https://pubs.rsc.org/en/content/ebook/978-0-85404-846-5
View Article : Google Scholar
|
|
57
|
Stamp DH: Three hypotheses linking bile to
carcinogenesis in the gastrointestinal tract: certain bile salts
have properties that may be used to complement chemotherapy. Med
Hypotheses. 59:398–405. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Ireland AP, Peters JH, Smyrk TC, DeMeester
TR, Clark GW, Mirvish SS and Adrian TE: Gastric juice protects
against the development of esophageal adenocarcinoma in the rat.
Ann Surg. 224:358–370. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Dvorak K, Payne CM, Chavarria M, Ramsey L,
Dvorakova B, Bernstein H, Holubec H, Sampliner RE, Guy N, Condon A,
et al: Bile acids in combination with low pH induce oxidative
stress and oxidative DNA damage: Relevance to the pathogenesis of
Barrett's oesophagus. Gut. 56:763–771. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Kauer WK and Stein HJ: Role of acid and
bile in the genesis of Barrett's esophagus. Chest Surg Clin N Am.
12:39–45. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Ulualp SO, Roland PS, Toohill RJ and
Shaker R: Prevalence of gastroesophagopharyngeal acid reflux
events: An evidence-based systematic review. Am J Otolaryngol.
26:239–244. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Lillemoe KD, Gadacz TR and Harmon JW: Bile
absorption occurs during disruption of the esophageal mucosal
barrier. J Surg Res. 35:57–62. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Sasaki CT, Hajek M, Doukas SG and Vageli
DP: The role of bile reflux and its related NF-κB activated pathway
in progression of hypopharyngeal squamous cell cancer. Oral Oncol.
105:1046682020. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Hemmink GJ, Bredenoord AJ, Weusten BL,
Monkelbaan JF, Timmer R and Smout AJ: Esophageal pH-impedance
monitoring in patients with therapy-resistant reflux symptoms: ‘On’
or ‘off’ proton pump inhibitor? Am J Gastroenterol. 103:2446–2453.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Bernstein H, Payne CM, Bernstein C,
Schneider J, Beard SE and Crowley CL: Activation of the promoters
of genes associated with DNA damage, oxidative stress, ER stress
and protein malfolding by the bile salt, deoxycholate. Toxicol
Lett. 108:37–46. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Huo X, Juergens S, Zhang X, Rezaei D, Yu
C, Strauch ED, Wang JY, Cheng E, Meyer F, Wang DH, et al:
Deoxycholic acid causes DNA damage while inducing apoptotic
resistance through NF-κB activation in benign Barrett's epithelial
cells. Am J Physiol Gastrointest Liver Physiol. 301:G278–G286.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Langevin SM, Michaud DS, Marsit CJ, Nelson
HH, Birnbaum AE, Eliot M, Christensen BC, McClean MD and Kelsey KT:
Gastric reflux is an independent risk factor for laryngopharyngeal
carcinoma. Cancer Epidemiol Biomarkers Prev. 22:1061–1068. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Coca-Pelaz A, Rodrigo JP, Takes RP, Silver
CE, Paccagnella D, Rinaldo A, Hinni ML and Ferlito A: Relationship
between reflux and laryngeal cancer. Head Neck. 35:1814–1818. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Attwood SE, Smyrk TC, DeMeester TR,
Mirvish SS, Stein HJ and Hinder RA: Duodenoesophageal reflux and
the development of esophageal adenocarcinoma in rats. Surgery.
111:503–510. 1992.PubMed/NCBI
|
|
70
|
Fein M, Fuchs KH, Stopper H, Diem S and
Herderich M: Duodenogastric reflux and foregut carcinogenesis:
Analysis of duodenal juice in a rodent model of cancer.
Carcinogenesis. 21:2079–2084. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Miwa K, Hattori T and Miyazaki I:
Duodenogastric reflux and foregut carcinogenesis. Cancer. 75 (Suppl
6):S1426–S1432. 1995. View Article : Google Scholar
|
|
72
|
Fang Y, Chen H, Hu Y, Djukic Z, Tevebaugh
W, Shaheen NJ, Orlando RC, Hu J and Chen X: Gastroesophageal reflux
activates the NF-κB pathway and impairs esophageal barrier function
in mice. Am J Physiol Gastrointest Liver Physiol. 305:G58–G65.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
McAdam E, Haboubi HN, Griffiths AP, Baxter
JN, Spencer-Harty S, Davies C and Jenkins GJ: Reflux composition
influences the level of NF-κB activation and upstream kinase
preference in oesophageal adenocarcinoma cells. Int J Cancer.
136:527–535. 2015.PubMed/NCBI
|
|
74
|
Bus P, Siersema PD and van Baal JW: Cell
culture models for studying the development of Barrett's esophagus:
A systematic review. Cell Oncol (Dordr). 35:149–161. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Hormi-Carver K, Zhang X, Zhang HY,
Whitehead RH, Terada LS, Spechler SJ and Souza RF: Unlike
esophageal squamous cells, Barrett's epithelial cells resist
apoptosis by activating the nuclear factor-κB pathway. Cancer Res.
69:672–677. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Karin M: Nuclear factor-kappaB in cancer
development and progression. Nature. 441:431–436. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Wang H and Cho CH: Effect of NF-kappaB
signaling on apoptosis in chronic inflammation-associated
carcinogenesis. Curr Cancer Drug Targets. 10:593–599. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
78
|
DiDonato JA, Mercurio F and Karin M:
NF-kappaB and the link between inflammation and cancer. Immunol
Rev. 246:379–400. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Hoesel B and Schmid JA: The complexity of
NF-kappaB signaling in inflammation and cancer. Mol Cancer.
12:862013. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Nottingham LK, Yan CH, Yang X, Si H,
Coupar J, Bian Y, Cheng TF, Allen C, Arun P, Gius D, et al:
Aberrant IKKα and IKKβ cooperatively activate NF-κB and induce
EGFR/AP1 signaling to promote survival and migration of head and
neck cancer. Oncogene. 33:1135–1147. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Stadler ME, Patel MR, Couch ME and Hayes
DN: Molecular biology of head and neck cancer: Risks and pathways.
Hematol Oncol Clin North Am. 22:1099–1124. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Molinolo AA, Amornphimoltham P, Squarize
CH, Castilho RM, Patel V and Gutkind JS: Dysregulated molecular
networks in head and neck carcinogenesis. Oral Oncol. 45:324–334.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
King KE, Ponnamperuma RM, Allen C, Lu H,
Duggal P, Chen Z, Van Waes C and Weinberg WC: The p53 homologue
DeltaNp63alpha interacts with the nuclear factor-kappaB pathway to
modulate epithelial cell growth. Cancer Res. 68:5122–5131. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Jackson-Bernitsas DG, Ichikawa H, Takada
Y, Myers JN, Lin XL, Darnay BG, Chaturvedi MM and Aggarwal BB:
Evidence that TNF-TNFR1-TRADD-TRAF2-RIP-TAK1-IKK pathway mediates
constitutive NF-kappaB activation and proliferation in human head
and neck squamous cell carcinoma. Oncogene. 26:1385–1397. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Dong J, Jimi E, Zeiss C, Hayden MS and
Ghosh S: Constitutively active NF-kappaB triggers systemic
TNFalpha-dependent inflammation and localized TNFalpha-independent
inflammatory disease. Genes Dev. 24:1709–1717. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Foxwell BM, Bondeson J, Brennan F and
Feldmann M: Adenoviral transgene delivery provides an approach to
identifying important molecular processes in inflammation: Evidence
for heterogenecity in the requirement for NF-kappaB in tumour
necrosis factor production. Ann Rheum Dis. 59 (Suppl 1):i54–i59.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Guyer RA and Macara IG: Loss of the
polarity protein PAR3 activates STAT3 signaling via an atypical
protein kinase C (aPKC)/NF-κB/interleukin-6 (IL-6) axis in mouse
mammary cells. J Biol Chem. 290:8457–8468. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Zhao Y, Zhang C, Huang Y, Yu Y, Li R, Li
M, Liu N, Liu P and Qiao J: Up-regulated expression of WNT5a
increases inflammation and oxidative stress via PI3K/AKT/NF-κB
signaling in the granulosa cells of PCOS patients. J Clin
Endocrinol Metab. 100:201–211. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Bo H, Zhang S, Gao L, Chen Y, Zhang J,
Chang X and Zhu M: Upregulation of Wnt5a promotes
epithelial-to-mesenchymal transition and metastasis of pancreatic
cancer cells. BMC Cancer. 13:4962013. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Klein JD and Grandis JR: The molecular
pathogenesis of head and neck cancer. Cancer Biol Ther. 9:1–7.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Allen CT, Ricker JL, Chen Z and Van Waes
C: Role of activated nuclear factor-kappaB in the pathogenesis and
therapy of squamous cell carcinoma of the head and neck. Head Neck.
29:959–971. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Loercher A, Lee TL, Ricker JL, Howard A,
Geoghegen J, Chen Z, Sunwoo JB, Sitcheran R, Chuang EY, Mitchell
JB, et al: Nuclear factor-kappaB is an important modulator of the
altered gene expression profile and malignant phenotype in squamous
cell carcinoma. Cancer Res. 64:6511–6523. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Chung CH, Parker JS, Ely K, Carter J, Yi
Y, Murphy BA, Ang KK, El-Naggar AK, Zanation AM, Cmelak AJ, et al:
Gene expression profiles identify epithelial-to-mesenchymal
transition and activation of nuclear factor-kappaB signaling as
characteristics of a high-risk head and neck squamous cell
carcinoma. Cancer Res. 66:8210–8218. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Lee TL, Yang XP, Yan B, Friedman J, Duggal
P, Bagain L, Dong G, Yeh NT, Wang J, Zhou J, et al: A novel nuclear
factor-kappaB gene signature is differentially expressed in head
and neck squamous cell carcinomas in association with TP53 status.
Clin Cancer Res. 13:5680–5691. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Coussens LM and Werb Z: Inflammation and
cancer. Nature. 420:860–867. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Souza RF: From reflux esophagitis to
esophageal adenocarcinoma. Dig Dis. 34:483–490. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Wroblewski LE, Peek RM Jr and Wilson KT:
Helicobacter pylori and gastric cancer: Factors that modulate
disease risk. Clin Microbiol Rev. 23:713–739. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Shaheen N and Ransohoff DF:
Gastroesophageal reflux, Barrett esophagus, and esophageal cancer:
Scientific review. JAMA. 287:1972–1981. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Vander Broek R, Snow GE, Chen Z and Van
Waes C: Chemoprevention of head and neck squamous cell carcinoma
through inhibition of NF-kappaB signaling. Oral Oncol. 50:930–941.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Baldwin AS Jr: The NF-kappa B and I kappa
B proteins: New discoveries and insights. Annu Rev Immunol.
14:649–683. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Lee TL, Yeh J, Friedman J, Yan B, Yang X,
Yeh NT, Van Waes C and Chen Z: A signal network involving
coactivated NF-kappaB and STAT3 and altered p53 modulates
BAX/BCL-XL expression and promotes cell survival of head and neck
squamous cell carcinomas. Int J Cancer. 122:1987–1998. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Wheeler SE, Suzuki S, Thomas SM, Sen M,
Leeman-Neill RJ, Chiosea SI, Kuan CT, Bigner DD, Gooding WE, Lai SY
and Grandis JR: Epidermal growth factor receptor variant III
mediates head and neck cancer cell invasion via STAT3 activation.
Oncogene. 29:5135–5145. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Yan B, Yang X, Lee TL, Friedman J, Tang J,
Van Waes C and Chen Z: Genome-wide identification of novel
expression signatures reveal distinct patterns and prevalence of
binding motifs for p53, nuclear factor-kappaB and other signal
transcription factors in head and neck squamous cell carcinoma.
Genome Biol. 8:R782007. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Yan B, Li H, Yang X, Shao J, Jang M, Guan
D, Zou S, Van Waes C, Chen Z and Zhan M: Unraveling regulatory
programs for NF-kappaB, p53 and microRNAs in head and neck squamous
cell carcinoma. PLoS One. 8:e736562013. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Sriuranpong V, Park JI, Amornphimoltham P,
Patel V, Nelkin BD and Gutkind JS: Epidermal growth factor
receptor-independent constitutive activation of STAT3 in head and
neck squamous cell carcinoma is mediated by the autocrine/paracrine
stimulation of the interleukin 6/gp130 cytokine system. Cancer Res.
63:2948–2956. 2003.PubMed/NCBI
|
|
106
|
Yang X, Lu H, Yan B, Romano RA, Bian Y,
Friedman J, Duggal P, Allen C, Chuang R, Ehsanian R, et al: ΔNp63
versatility regulates a Broad NF-κB gene program and promotes
squamous epithelial proliferation, migration, and inflammation.
Cancer Res. 71:3688–3700. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Du J, Romano RA, Si H, Mattox A, Bian Y,
Yang X, Sinha S, Van Waes C and Chen Z: Epidermal overexpression of
transgenic ΔNp63 promotes type 2 immune and myeloid inflammatory
responses and hyperplasia via NF-κB activation. J Pathol.
232:356–368. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Squarize CH, Castilho RM, Sriuranpong V,
Pinto DS Jr and Gutkind JS: Molecular cross-talk between the
NFkappaB and STAT3 signaling pathways in head and neck squamous
cell carcinoma. Neoplasia. 8:733–746. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Yap LF, Ahmad M, Zabidi MM, Chu TL, Chai
SJ, Lee HM, Lim PV, Wei W, Dawson C, Teo SH, et al: Oncogenic
effects of WNT5A in Epstein-Barr virus associated nasopharyngeal
carcinoma. Int J Oncol. 44:1774–1780. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Sherwood V, Chaurasiya SK, Ekström EJ,
Guilmain W, Liu Q, Koeck T, Brown K, Hansson K, Agnarsdóttir M,
Bergqvist M, et al: WNT5A-mediated β-catenin-independent signalling
is a novel regulator of cancer cell metabolism. Carcinogenesis.
35:784–794. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Asem MS, Buechler S, Wates RB, Miller DL
and Stack MS: Wnt5a Signaling in Cancer. Cancers (Basel). 8:792016.
View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Nakanishi C and Toi M: Nuclear
factor-kappaB inhibitors as sensitizers to anticancer drugs. Nat
Rev Cancer. 5:297–309. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Meng Z, Lou S, Tan J, Xu K, Jia Q and
Zheng W: Nuclear factor-kappa B inhibition can enhance apoptosis of
differentiated thyroid cancer cells induced by 131I. PLoS One.
7:e335972012. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Lin Y, Bai L, Chen W and Xu S: The NF-κB
activation pathways, emerging molecular targets for cancer
prevention and therapy. Expert Opin Ther Targets. 14:45–55. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Van Waes C: Nuclear factor-kappaB in
development, prevention, and therapy of cancer. Clin Cancer Res.
13:1076–1082. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Wilken R, Veena MS, Wang MB and Srivatsan
ES: Curcumin: A review of anti-cancer properties and therapeutic
activity in head and neck squamous cell carcinoma. Mol Cancer.
10:122011. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
LoTempio MM, Veena MS, Steele HL,
Ramamurthy B, Ramalingam TS, Cohen AN, Chakrabarti R, Srivatsan ES
and Wang MB: Curcumin suppresses growth of head and neck squamous
cell carcinoma. Clin Cancer Res. 11:6994–7002. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Naksuriya O, Okonogi S, Schiffelers RM and
Hennink WE: Curcumin nanoformulations: A review of pharmaceutical
properties and preclinical studies and clinical data related to
cancer treatment. Biomaterials. 35:3365–3383. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Fan Y, Mao R and Yang J: NF-κB and STAT3
signaling pathways collaboratively link inflammation to cancer.
Protein Cell. 4:176–185. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Gaykalova DA, Manola JB, Ozawa H, Zizkova
V, Morton K, Bishop JA, Sharma R, Zhang C, Michailidi C, Considine
M, et al: NF-κB and stat3 transcription factor signatures
differentiate HPV-positive and HPV-negative head and neck squamous
cell carcinoma. Int J Cancer. 137:1879–1889. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Khaznadar SS, Khan M, Schmid E, Gebhart S,
Becker ET, Krahn T and von Ahsen O: EGFR overexpression is not
common in patients with head and neck cancer. Cell lines are not
representative for the clinical situation in this indication.
Oncotarget. 9:28965–28975. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Johnson DE, Burtness B, Leemans CR, Lui
VW, Bauman JE and Grandis JR: Head and neck squamous cell
carcinoma. Nat Rev Dis Primers. 6:922020. View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Vander Broek R, Mohan S, Eytan DF, Chen Z
and Van Waes C: The PI3K/Akt/mTOR axis in head and neck cancer:
Functions, aberrations, cross-talk, and therapies. Oral Dis.
21:815–825. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
124
|
Li Z, Yang Z, Passaniti A, Lapidus RG, Liu
X, Cullen KJ and Dan HC: A positive feedback loop involving
EGFR/Akt/mTORC1 and IKK/NF-kB regulates head and neck squamous cell
carcinoma proliferation. Oncotarget. 7:31892–31906. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
125
|
Harris RE: Cyclooxygenase-2 (cox-2) and
the inflammogenesis of cancer. Subcell Biochem. 42:93–126. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
126
|
Lim JW, Kim H and Kim KH: Nuclear
factor-kappaB regulates cyclooxygenase-2 expression and cell
proliferation in human gastric cancer cells. Lab Invest.
81:349–360. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
127
|
Meng F, Liu L, Chin PC and D'Mello SR: Akt
is a downstream target of NF-kappa B. J Biol Chem. 277:29674–29680.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Ahmad A, Biersack B, Li Y, Kong D, Bao B,
Schobert R, Padhye SB and Sarkar FH: Targeted regulation of
PI3K/Akt/mTOR/NF-κB signaling by indole compounds and their
derivatives: Mechanistic details and biological implications for
cancer therapy. Anticancer Agents Med Chem. 13:1002–1013. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
129
|
Baud V and Karin M: Is NF-κB a good target
for cancer therapy? Hopes and pitfalls. Nat Rev Drug Discov.
8:33–40. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
130
|
Tili E, Michaille JJ and Croce CM:
MicroRNAs play a central role in molecular dysfunctions linking
inflammation with cancer. Immunol Rev. 253:167–184. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
131
|
Filipowicz W, Bhattacharyya SN and
Sonenberg N: Mechanisms of post-transcriptional regulation by
microRNAs: Are the answers in sight? Nat Rev Genet. 9:102–114.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
132
|
Svoronos AA, Engelman DM and Slack FJ:
OncomiR or tumor suppressor? The duplicity of microRNAs in cancer.
Cancer Res. 76:3666–3670. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
133
|
Hu A, Huang JJ, Xu WH, Jin XJ, Li JP, Tang
YJ, Huang XF, Cui HJ and Sun GB: MiR-21 and miR-375 microRNAs as
candidate diagnostic biomarkers in squamous cell carcinoma of the
larynx: Association with patient survival. Am J Transl Res.
6:604–613. 2014.PubMed/NCBI
|
|
134
|
Hu A, Huang JJ, Xu WH, Jin XJ, Li JP, Tang
YJ, Huang XF, Cui HJ, Sun GB, Li RL and Duan JL: MiR-21/miR-375
ratio is an independent prognostic factor in patients with
laryngeal squamous cell carcinoma. Am J Cancer Res. 5:1775–1785.
2015.PubMed/NCBI
|
|
135
|
Arantes LM, Laus AC, Melendez ME, de
Carvalho AC, Sorroche BP, De Marchi PR, Evangelista AF,
Scapulatempo-Neto C, de Souza Viana L and Carvalho AL: MiR-21 as
prognostic biomarker in head and neck squamous cell carcinoma
patients undergoing an organ preservation protocol. Oncotarget.
8:9911–9921. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
136
|
Wu Y, Yu J, Ma Y, Wang F and Liu H:
MiR-148a and miR-375 may serve as predictive biomarkers for early
diagnosis of laryngeal carcinoma. Oncol Lett. 12:871–878. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
137
|
Li J, Wang K, Chen X, Meng H, Song M, Wang
Y, Xu X and Bai Y: Transcriptional activation of microRNA-34a by
NF-kappa B in human esophageal cancer cells. BMC Mol Biol.
13:42012. View Article : Google Scholar : PubMed/NCBI
|
|
138
|
Li HP, Zeng XC, Zhang B, Long JT, Zhou B,
Tan GS, Zeng WX, Chen W and Yang JY: MiR-451 inhibits cell
proliferation in human hepatocellular carcinoma through direct
suppression of IKK-β. Carcinogenesis. 34:2443–2451. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
139
|
Zhou P, Zeng F, Liu J, Lv D and Liu S:
Correlation betweenmir-21 expression and laryngeal carcinoma risks:
A meta-analysis. J Evid Based Med. 9:32–37. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
140
|
Shen Z, Zhan G, Ye D, Ren Y, Cheng L, Wu Z
and Guo J: MicroRNA-34a affects the occurrence of laryngeal
squamous cell carcinoma by targeting the antiapoptotic gene
survivin. Med Oncol. 29:2473–2480. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
141
|
Chen Y, Xian PF, Yang L and Wang SX:
MicroRNA-21 promotes proliferation of fibroblast-like synoviocytes
through mediation of NF-κB nuclear translocation in a rat model of
collagen-induced rheumatoid arthritis. Biomed Res Int.
2016:92790782016.PubMed/NCBI
|
|
142
|
Kikkawa N, Kinoshita T, Nohata N, Hanazawa
T, Yamamoto N, Fukumoto I, Chiyomaru T, Enokida H, Nakagawa M,
Okamoto Y and Seki N: MicroRNA-504 inhibits cancer cell
proliferation via targeting CDK6 in hypopharyngeal squamous cell
carcinoma. Int J Oncol. 44:2085–2092. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
143
|
Kikkawa N, Hanazawa T, Fujimura L, Nohata
N, Suzuki H, Chazono H, Sakurai D, Horiguchi S, Okamoto Y and Seki
N: MiR-489 is a tumour-suppressive miRNA target PTPN11 in
hypopharyngeal squamous cell carcinoma (HSCC). Br J Cancer.
103:877–884. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
144
|
Fukumoto I, Kinoshita T, Hanazawa T,
Kikkawa N, Chiyomaru T, Enokida H, Yamamoto N, Goto Y, Nishikawa R,
Nakagawa M, et al: Identification of tumour suppressive
microRNA-451a in hypopharyngeal squamous cell carcinoma based on
microRNA expression signature. Br J Cancer. 111:386–394. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
145
|
Hui AB, Lenarduzzi M, Krushel T, Waldron
L, Pintilie M, Shi W, Perez-Ordonez B, Jurisica I, O'Sullivan B,
Waldron J, et al: Comprehensive microRNA profiling for head and
neck squamous cell carcinomas. Clin Cancer Res. 16:1129–1139. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
146
|
Tai J, Xiao X, Huang ZG, Yu ZK, Chen XH,
Zhou WG, Chen XJ, Rao YS, Fang JG and Ni X: MicroRNAs regulate
epithelial-mesenchymal transition of supraglottic laryngeal cancer.
Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 48:499–503. 2013.(In
Chinese). PubMed/NCBI
|
|
147
|
Zhao XD, Zhang W, Liang HJ and Ji WY:
Overexpression of miR-155 promotes proliferation and invasion of
human laryngeal squamous cell carcinoma via targeting SOCS1 and
STAT3. PLoS One. 8:e563952013. View Article : Google Scholar : PubMed/NCBI
|
|
148
|
Luzna P, Gregar J, Uberall I, Radova L,
Prochazka V and Ehrmann J Jr: Changes of microRNAs-192, 196a and
203 correlate with Barrett's esophagus diagnosis and its
progression compared to normal healthy individuals. Diagn Pathol.
6:1142011. View Article : Google Scholar : PubMed/NCBI
|
|
149
|
Bus P, Siersema PD, Verbeek RE and van
Baal JW: Upregulation of miRNA-143, −145, −192, and −194 in
esophageal epithelial cells upon acidic bile salt stimulation. Dis
Esophagus. 27:591–600. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
150
|
Chen D, Cabay RJ, Jin Y, Wang A, Lu Y,
Shah-Khan M and Zhou X: MicroRNA deregulations in head and neck
squamous cell carcinomas. J Oral Maxillofac Res. 4:e22013.
View Article : Google Scholar : PubMed/NCBI
|
|
151
|
Yang Z, Fang S, Di Y, Ying W, Tan Y and Gu
W: Modulation of NF-κB/miR-21/PTEN pathway sensitizes non-small
cell lung cancer to cisplatin. PLoS One. 10:e01215472015.
View Article : Google Scholar : PubMed/NCBI
|
|
152
|
Xiao T, Ling M, Xu H, Luo F, Xue J, Chen
C, Bai J, Zhang Q, Wang Y, Bian Q and Liu Q: NF-κB-regulation of
miR-155, via SOCS1/STAT3, is involved in the
PM2.5-accelerated cell cycle and proliferation of human
bronchial epithelial cells. Toxicol Appl Pharmacol. 377:1146162019.
View Article : Google Scholar : PubMed/NCBI
|
|
153
|
Rokavec M, Öner MG, Li H, Jackstadt R,
Jiang L, Lodygin D, Kaller M, Horst D, Ziegler PK, Schwitalla S, et
al: IL-6R/STAT3/miR-34a feedback loop promotes EMT-mediated
colorectal cancer invasion and metastasis. J Clin Invest.
124:1853–1867. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
154
|
Tili E, Croce CM and Michaille JJ:
MiR-155: On the crosstalk between inflammation and cancer. Int Rev
Immunol. 28:264–284. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
155
|
Bharti AC, Donato N, Singh S and Aggarwal
BB: Curcumin (diferuloylmethane) down-regulates the constitutive
activation of nuclear factor-kappa B and IkappaBalpha kinase in
human multiple myeloma cells, leading to suppression of
proliferation and induction of apoptosis. Blood. 101:1053–1062.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
156
|
Dai Y, Pei XY, Rahmani M, Conrad DH, Dent
P and Grant S: Interruption of the NF-kappaB pathway by Bay 11-7082
promotes UCN-01-mediated mitochondrial dysfunction and apoptosis in
human multiple myeloma cells. Blood. 103:2761–2770. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
157
|
Monisha J, Roy NK, Bordoloi D, Kumar A,
Golla R, Kotoky J, Padmavathi G and Kunnumakkara AB: Nuclear factor
kappa B: A potential target to persecute head and neck cancer. Curr
Drug Targets. 18:232–253. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
158
|
Karin M, Yamamoto Y and Wang QM: The IKK
NF-kappa B system: A treasure trove for drug development. Nat Rev
Drug Discov. 3:17–26. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
159
|
Ramadass V, Vaiyapuri T and Tergaonkar V:
Small molecule NF-κB pathway inhibitors in clinic. Int J Mol Sci.
21:51642020. View Article : Google Scholar : PubMed/NCBI
|
|
160
|
Greten FR, Arkan MC, Bollrath J, Hsu LC,
Goode J, Miething C, Göktuna SI, Neuenhahn M, Fierer J, Paxian S,
et al: NF-kappaB is a negative regulator of IL-1beta secretion as
revealed by genetic and pharmacological inhibition of IKKbeta.
Cell. 130:918–931. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
161
|
Bromberg JF, Wrzeszczynska MH, Devgan G,
Zhao Y, Pestell RG, Albanese C and Darnell JE Jr: Stat3 as an
oncogene. Cell. 98:295–303. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
162
|
Geiger JL, Grandis JR and Bauman JE: The
STAT3 pathway as a therapeutic target in head and neck cancer:
Barriers and innovations. Oral Oncol. 56:84–92. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
163
|
Nelson EA, Walker SR, Kepich A, Gashin LB,
Hideshima T, Ikeda H, Chauhan D, Anderson KC and Frank DA:
Nifuroxazide inhibits survival of multiple myeloma cells by
directly inhibiting STAT3. Blood. 112:5095–5102. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
164
|
Siddiquee KA, Gunning PT, Glenn M, Katt
WP, Zhang S, Schrock C, Sebti SM, Jove R, Hamilton AD and Turkson
J: An oxazole-based small-molecule Stat3 inhibitor modulates Stat3
stability and processing and induces antitumor cell effects. ACS
Chem Biol. 2:787–798. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
165
|
Johnson DE, O'Keefe RA and Grandis JR:
Targeting the IL-6/JAK/STAT3 signalling axis in cancer. Nat Rev
Clin Oncol. 15:234–248. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
166
|
Goldman A, Shahidullah M, Goldman D,
Khailova L, Watts G, Delamere N and Dvorak K: A novel mechanism of
acid and bile acid-induced DNA damage involving Na+/H+ exchanger:
Implication for Barrett's oesophagus. Gut. 59:1606–1616. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
167
|
Bernstein H, Bernstein C, Payne CM and
Dvorak K: Bile acids as endogenous etiologic agents in
gastrointestinal cancer. World J Gastroenterol. 15:3329–3340. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
168
|
Lechner S, Müller-Ladner U, Schlottmann K,
Jung B, McClelland M, Rüschoff J, Welsh J, Schölmerich J and
Kullmann F: Bile acids mimic oxidative stress induced upregulation
of thioredoxin reductase in colon cancer cell lines.
Carcinogenesis. 23:1281–1288. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
169
|
Kinner A, Wu W, Staudt C and Iliakis G:
Gamma-H2AX in recognition and signaling of DNA double-strand breaks
in the context of chromatin. Nucleic Acids Res. 36:5678–5694. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
170
|
Rothkamm K and Löbrich M: Evidence for a
lack of DNA double-strand break repair in human cells exposed to
very low x-ray doses. Proc Natl Acad Sci USA. 100:5057–5062. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
171
|
Nikitaki Z, Hellweg CE, Georgakilas AG and
Ravanat JL: Stress-induced DNA damage biomarkers: Applications and
limitations. Front Chem. 3:352015. View Article : Google Scholar : PubMed/NCBI
|
|
172
|
Tsantoulis PK, Kotsinas A, Sfikakis PP,
Evangelou K, Sideridou M, Levy B, Mo L, Kittas C, Wu XR,
Papavassiliou AG and Gorgoulis VG: Oncogene-induced replication
stress preferentially targets common fragile sites in preneoplastic
lesions. A genome-wide study. Oncogene. 27:3256–3264. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
173
|
Choudhari SK, Chaudhary M, Gadbail AR,
Sharma A and Tekade S: Oxidative and antioxidative mechanisms in
oral cancer and precancer: A review. Oral Oncol. 50:10–18. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
174
|
Janssens S and Tschopp J: Signals from
within: The DNA-damage-induced NF-kappaB response. Cell Death
Differ. 13:773–784. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
175
|
Kawanishi S, Ohnishi S, Ma N, Hiraku Y and
Murata M: Crosstalk between DNA damage and inflammation in the
multiple steps of carcinogenesis. Int J Mol Sci. 18:18082017.
View Article : Google Scholar : PubMed/NCBI
|
|
176
|
Tafani M, Sansone L, Limana F, Arcangeli
T, De Santis E, Polese M, Fini M and Russo MA: The interplay of
reactive oxygen species, hypoxia, inflammation, and sirtuins in
cancer initiation and progression. Oxid Med Cell Longev.
2016:39071472016. View Article : Google Scholar : PubMed/NCBI
|
|
177
|
Li D and Cao W: Bile acid receptor TGR5,
NADPH Oxidase NOX5-S and CREB mediate bile acid-induced DNA damage
in Barrett's esophageal adenocarcinoma cells. Sci Rep. 6:315382016.
View Article : Google Scholar : PubMed/NCBI
|
|
178
|
Nema R, Vishwakarma S, Agarwal R, Panday
RK and Kumar A: Emerging role of sphingosine-1-phosphate signaling
in head and neck squamous cell carcinoma. Onco Targets Ther.
9:3269–3280. 2016.PubMed/NCBI
|
|
179
|
Tamashiro PM, Furuya H, Shimizu Y, Iino K
and Kawamori T: The impact of sphingosine kinase-1 in head and neck
cancer. Biomolecules. 3:481–513. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
180
|
Liu R, Li X, Hylemon PB and Zhou H:
Conjugated bile acids promote invasive growth of esophageal
adenocarcinoma cells and cancer stem cell expansion via sphingosine
1-phosphate receptor 2-mediated yes-associated protein activation.
Am J Pathol. 188:2042–2058. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
181
|
Pang C, LaLonde A, Godfrey TE, Que J, Sun
J, Wu TT and Zhou Z: Bile salt receptor TGR5 is highly expressed in
esophageal adenocarcinoma and precancerous lesions with
significantly worse overall survival and gender differences. Clin
Exp Gastroenterol. 10:29–37. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
182
|
Guan B, Li H, Yang Z, Hoque A and Xu X:
Inhibition of farnesoid X receptor controls esophageal cancer cell
growth in vitro and in nude mouse xenografts. Cancer.
119:1321–1329. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
183
|
Yu JH, Zheng JB, Qi J, Yang K, Wu YH, Wang
K, Wang CB and Sun XJ: Bile acids promote gastric intestinal
metaplasia by upregulating CDX2 and MUC2 expression via the
FXR/NF-κB signaling pathway. Int J Oncol. 54:879–892.
2019.PubMed/NCBI
|
|
184
|
Schweitzer A, Knauer SK and Stauber RH:
Nuclear receptors in head and neck cancer: Current knowledge and
perspectives. Int J Cancer. 126:801–809. 2010.PubMed/NCBI
|
|
185
|
Gadaleta RM, Oldenburg B, Willemsen EC,
Spit M, Murzilli S, Salvatore L, Klomp LW, Siersema PD, van Erpecum
KJ and van Mil SW: Activation of bile salt nuclear receptor FXR is
repressed by pro-inflammatory cytokines activating NF-κB signaling
in the intestine. Biochim Biophys Acta. 1812:851–858. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
186
|
Wang YD, Chen WD, Wang M, Yu D, Forman BM
and Huang W: Farnesoid X receptor antagonizes nuclear factor kappaB
in hepatic inflammatory response. Hepatology. 48:1632–1643. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
187
|
Wang Z, Li Y and Sarkar FH: Signaling
mechanism(s) of reactive oxygen species in epithelial-mesenchymal
transition reminiscent of cancer stem cells in tumor progression.
Curr Stem Cell Res Ther. 5:74–80. 2010. View Article : Google Scholar : PubMed/NCBI
|