Introduction
Pancreatic cancer (PaCa) has one of the poorest
prognoses among all gastrointestinal cancers and is the third
leading cause of cancer-related death in the US (1). In recent years, new chemotherapy
regimens, such as FOLFIRINOX and nab-paclitaxel plus gemcitabine,
and new radiotherapy modalities, such as stereotactic body
radiotherapy, intensity modulated radiotherapy, and carbon-ion
radiotherapy, have been introduced (2–6).
However, the 5-year survival rate of patients with PaCa is still
very low, at 8.5-9% (1,7). Because the number of patients with
PaCa is expected to increase (8),
there is an urgent need to develop new treatment methods.
One of the main reasons for the increase in PaCa
malignancy is its high local invasion capacity. The most effective
treatment for PaCa is curative surgery (9,10),
yet many PaCa cases are judged unresectable at diagnosis (11). The combination of chemotherapy and
radiotherapy for treating locally advanced PaCa has been reported
to prolong overall survival (12);
however, these approaches are often not sufficiently effective
because PaCa quickly becomes resistant to these treatments. The
mechanism through which PaCa develops resistance to radiotherapy
remains unclear. Therefore, elucidation of the mechanisms of
radiation resistance may improve PaCa treatment.
Chemokines and their receptors have been discovered
as essential and selective mediators in leukocyte migration to the
inflammatory site and to secondary lymphoid organs (13). They play critical roles in tumor
initiation, promotion, and progression (14). C-X-C chemokine receptor type 4
(CXCR4) is the receptor for C-X-C motif chemokine ligand 12
(CXCL12) and has been shown to act as a coreceptor for human
immunodeficiency virus (HIV) entry (15). Recently, the association between
CXCR4 and cancer has become a focus of research as CXCR4 is
overexpressed in various types of cancer and contributes to tumor
growth, angiogenesis, metastasis, and treatment resistance
(16–18). Similar results have been described
in PaCa (19–22). CXCR4 antagonists were initially
developed as a novel treatment for HIV infection (23,24).
As our understanding of the functions of CXCR4 grows, CXCR4
antagonists are being used for purposes other than anti-HIV
treatment. Several reports have described the effects of CXCR4
antagonists on malignant tumors, including breast cancer (25), small cell lung cancer (26), cholangiocarcinoma (27), gastric cancer (28), and PaCa (29–31).
We previously reported that the CXCL12/CXCR4 axis is involved in
gemcitabine resistance in PaCa and that a CXCR4 antagonist exhibits
antitumor effects on gemcitabine-resistant PaCa cell lines
(32). However, the role of CXCR4
in PaCa radiation resistance is still unknown.
Here, we established two radiation-resistant PaCa
cell lines. Using multiple methods, we confirmed the higher
expression of CXCR4 in radiation-resistant cells compared with that
in normal PaCa cell lines. The purpose of this study was to clarify
the roles of the CXCL12/CXCR4 axis in radiation resistance in PaCa
and evaluate the effects of CXCR4 antagonism on radiation-resistant
PaCa cell lines.
Materials and methods
Reagents
AMD070 trihydrochloride
(C21H30Cl3N5; CID
11256587) was purchased from Med Chem Express (Cosmo Bio Co.,
Ltd.), and dimethyl sulfoxide (DMSO) was obtained from
Sigma-Aldrich (Merck KGaA). AMD070 solution (326.90 mM) was
prepared in DMSO, stored in small aliquots at −20°C, and then
thawed and diluted in cell culture medium as required. CXCL12 was
purchased from R&D Systems.
Cell lines and treatments
The human pancreatic duct epithelial (HPDE) cell
line H6c7 was purchased from Kerafast. Human skin fibroblasts (FBs;
cat. no. T0904) were purchased from Applied Biological Materials.
The human PaCa cell lines AsPC-1, BxPC-3, Capan2, MIA PaCa-2,
PANC-1, and SW1990 were purchased from the American Type Culture
Collection (ATCC). The H6c7 cell line was maintained in
keratinocyte serum-free medium (Gibco/Thermo Fisher Scientific,
Inc.). The AsPC-1, BxPC-3, and Capan2 cell lines were maintained in
RPMI-1640 medium (Sigma Aldrich; Merck KGaA). The MIA PaCa-2,
PANC-1, and SW1990 cell lines and FBs were maintained in Dulbecco's
modified Eagle's medium (DMEM; Sigma Aldrich; Merck KGaA). Both
RPMI-1640 medium and DMEM were supplemented with 10% fetal bovine
serum (FBS; Gibco/Thermo Fisher Scientific, Inc.). All media were
supplemented with 10 mg/ml streptomycin, 10,000 U/ml penicillin,
and 25 µg amphotericin B (Gibco/Thermo Fisher Scientific, Inc.).
All cell lines were cultured at 37°C in a humidified incubator with
5% CO2.
Establishment of radiation-resistant
PaCa cell lines
Radiation-resistant cancer cell lines have been
previously established from nasopharyngeal, esophageal, breast, and
lung cancers (33–37). Here, we established
radiation-resistant PaCa cell lines by referencing these methods.
PaCa cell lines (AsPC-1, BxPC-3, MIA PaCa-2, and SW1990) were
seeded in 100-mm dishes and cultured. Upon reaching 50% confluence,
the cells were irradiated with 2 Gy radiation and incubated until
reaching 90% confluence, after which the cells were passaged. With
each passage, the irradiation process was repeated until the total
radiation dose reached at least 60 Gy. The radiation resistance of
the cell lines was assessed by colony formation assay.
Total mRNA microarray analysis
Total mRNA from normal and radiation-resistant MIA
PaCa-2 cells was isolated using the RNeasy Plus Mini kit (Qiagen,
Inc.) according to the manufacturer's instructions. The mRNA
microarray experiments were performed by Hokkaido System Science
Co., Ltd. Transcripts amplified from total mRNA were hybridized to
a SurePrint G3 Human 8×60K v3 array (Agilent Technologies, Inc.)
according to the manufacturer's protocol. The results were analyzed
using Agilent Genomic Workbench Software (Agilent Technologies,
Inc.).
Colony formation assay
Irradiating a small number of cells with a high
radiation dose will kill all cells. Therefore, the number of
radiation-resistant PaCa cells to be seeded (200, 400, 1,000,
2,000, or 40,000) depended on the dose (0, 2, 4, 6, or 10 Gy). The
cells were seeded in 60-mm dishes, cultured overnight, irradiated
with each radiation dose, and cultured at 37°C for 14 days. To
assess the efficacy of AMD070, a CXCR4 antagonist, PaCa cells were
seeded in 60-mm dishes and treated with 2.5 µM AMD070 for 72 h. The
treated cells were seeded in 60-mm dishes, cultured overnight,
irradiated with 2 Gy radiation, and cultured at 37°C for 14 days.
Cells were fixed and stained using a Diff-Quick cell staining kit
(Dade Behring), and colonies were counted under five different
fields. A colony was defined as a group of at least 50 cells.
Immunohistochemistry
Pancreatic tissues were analyzed from 92 patients
who underwent surgery at Nagoya City University Hospital (Nagoya,
Japan) between January 2006 and December 2016. The mean age of the
patients was 67.6 years (range 32–85 years), and the male-female
ratio was 62 males and 30 females. All pancreatic tissues were
obtained from patients or their relatives who provided informed
consent. This study was conducted upon the approval of the
institutional review board established by Nagoya City University
(approval no. 60–18-0025, date of approval; May 6, 2018).
Specimens were fixed in 10% formalin and then
embedded in paraffin. Specimens were sectioned into 3-µm-thick
slices, and the sections were deparaffinized, subjected to
autoclave treatment in 10 mM sodium citrate buffer for 10 min at
120°C, and cooled to room temperature. Next, the sections were
treated with 0.3% H2O2 in methanol for 30
min, blocked with Block Ace (Megmilk Snow Brand; KAC Co., Ltd.) for
10 min, and incubated with anti-CXCR4 antibody (1:250; Proteintech
Group; cat. no. 60042-1-Ig) overnight at 4°C, followed by EnVision+
System- HRP Labelled Polymer anti-mouse (DAKO/Agilent Technologies;
cat. no. K4001) for 45 min at room temperature. The peroxidase
reaction was visualized by incubating the sections with the Liquid
DAB+ Substrate Chromogen System (DAKO/Agilent Technologies; cat.
no. K3467), followed by hematoxylin counterstaining.
Immunohistochemical staining was evaluated as follows. The
intensity of CXCR4 immunostaining was graded semi-quantitatively on
a 4-point scale (−, +, ++, +++) by three independent observers. Of
the 92 patients, 8 had stage 1 disease, 4 had stage 2 disease, 37
had stage 3 disease, 41 had stage 4 disease, and 2 had an unknown
disease stage. However, analyses were performed in a blinded
manner, and the observer was not aware of the patient's stage and
outcome. The concordance rate was greater than 90%. Differences in
opinion were resolved by consensus with a fourth evaluator. The
cases were classified into a high expression group and a weak
expression group according to the intensity of immunostaining in
cancer cells, in which an immunostaining score of ++ or +++ was
defined as high expression.
Immunofluorescence staining
PaCa cells (5×104) were seeded in glass
chamber slides and cultured overnight. The cells were fixed using
4% paraformaldehyde for 20 min at room temperature. Next, the cells
were permeabilized with 0.1% Triton-X for 3 min and incubated with
blocking buffer [3% bovine serum albumin in phosphate-buffered
saline (FUJIFULM Wako Pure Chemical Corp.)] for 1 h at room
temperature. The cells were incubated with anti-CXCR4 antibody
(1:200; Abcam; cat. no. ab124824) overnight at 4°C, followed by
Alexa Fluor 488 goat anti-rabbit IgG secondary antibody (1:1,000;
Abcam; cat. no. ab6939) for 1 h at room temperature. The nuclei
were visualized by DAPI staining at room temperature for 10 min.
Images of the stained slides were captured using a BZ-X710
fluorescence microscope (Keyence Corporation) at ×200
magnification.
Reverse-transcription quantitative
polymerase chain reaction (RT-qPCR)
Total RNA was isolated from HPDE and PaCa cells
using an RNeasy Plus Mini kit (Qiagen GmbH), according to the
manufacturer's protocols, and quantified using a NanoDrop 1000
(Thermo Fisher Scientific, Inc.). Total RNA (1 µg) was reverse
transcribed using Super Script III First-Strand Synthesis Super Mix
for RT-qPCR (Invitrogen/Thermo Fisher Scientific, Inc.) following
the manufacturer's protocols. RT-qPCR was performed using TaqMan
Fast Advanced Master Mix and TaqMan Gene Expression Assays for
CXCR4 (Hs00607978_s1) and glyceraldehyde 3-phosphate
dehydrogenase (GAPDH; Hs99999905_m1) on a 7900HT Fast
Real-Time PCR System (all from Applied Biosystems/Thermo Fisher
Scientific, Inc.). The following thermocycling conditions were
used: initial denaturation at 95°C for 20 sec, followed by 40
cycles at 95°C for 1 sec and 60°C for 20 sec. The expression level
of CXCR4 was reported relative to that of GAPDH in
each sample, using the relative standard curve method (38).
Western blotting
Proteins were extracted from cells using
radioimmunoprecipitation lysis buffer containing Protease Inhibitor
Single Use Cocktail and Phosphatase Inhibitor Cocktail (Thermo
Fisher Scientific, Inc.). The protein concentrations were measured
using a Pierce BCA protein assay kit (Thermo Fisher Scientific,
Inc.). Protein extracts (20 or 30 µg) were denatured at 90°C for 5
min and separated on 10% Mini-PROTEAN TGX Precast gels (Bio-Rad
Laboratories). The protein bands were transferred to nitrocellulose
membranes and blocked in iBind Flex Solution (iBind Flex Buffer,
iBind Flex Additive, and distilled water; Thermo Fisher Scientific,
Inc.) for 20 min at room temperature. The primary and secondary
antibody reactions were performed for 3 h at room temperature using
the iBind Flex Western System (Thermo Fisher Scientific, Inc.)
according to the manufacturer's instructions. The membranes were
incubated with anti-CXCR4 (1:1,000; Proteintech Group; cat. no.
60042-1-Ig) or anti-GAPDH (1:1,000; Santa Cruz Biotechnology; cat.
no. SC-47724) primary antibodies, followed by horseradish
peroxidase-conjugated goat anti-mouse polyclonal secondary
antibodies (1:2,000; DAKO/Agilent Technologies; cat. no. P0447).
The protein-antibody complexes were visualized using SuperSignal
West Femto Chemiluminescent Substrate or Pierce ECL Western
Blotting Substrate (Thermo Fisher Scientific, Inc.). The
immunoreactive protein bands were detected using an Amersham Imager
600 (Cytiva), and the densities of the detected bands were
calculated using ImageJ software 1.52v (National Institutes of
Health).
RNA interference
CXCR4 small interfering RNA (siRNA; s15412:
CCUGUUUCCGUGAAGAAAA) and nontargeting negative control siRNA
(Silencer Select Negative Control No. 1; cat. no. 4390843: sequence
not provided) were predesigned siRNAs purchased from Thermo Fisher
Scientific, Inc. PaCa cells were seeded at 2.5×105
cells/well in 6-well plates, cultured overnight, and then
transfected with siRNA. According to the manufacturer's
instructions, siRNAs and Lipofectamine RNAiMAX (Invitrogen/Thermo
Fisher Scientific, Inc.) were mixed with Opti-MEM
(Invitrogen/Thermo Fisher Scientific, Inc.) and incubated for 5 min
at room temperature. The siRNA-lipid complex was diluted in DMEM to
achieve a final siRNA concentration of 10 nM. Cells were incubated
for 48 h in a 5% CO2 incubator at 37°C.
Invasion assay
In vitro invasion assays were performed using
Corning BioCoat Matrigel Invasion Chambers (Corning, Inc.)
according to the manufacturer's protocol. Normal and
radiation-resistant PaCa cells (1×105) were seeded in
the upper chamber, which contained DMEM without FBS. The
chemoattractant used in the lower chamber was 10% FBS in DMEM. In
addition, AMD070 (1 µM) and CXCL12 (100 ng/ml) were added to the
lower chamber, or the cells were cocultured with FBs. After
incubation for 24 h, the upper surface of the upper chambers was
wiped with a cotton swab, and the invading cells were fixed and
stained using a Diff-Quick cell staining kit (Dade Behring). The
number of cells in nine random microscopic fields (×200
magnification) was counted.
Statistical analysis
Differences between two samples were analyzed using
unpaired t-tests. Multiple group comparisons were performed by
one-way analysis of variance with the post-hoc Bonferroni test for
subsequent comparisons of individual groups. Comparisons of groups
with two independent variables were performed using two-way
analysis of variance. Comparisons of patient stage were performed
using Fisher's exact test. Survival curves based on CXCR4
expression were generated using the Kaplan-Meier method and were
compared using log-rank tests. Results with a P-value <0.05 were
considered statistically significant. The data from experiments
performed in at least triplicate are expressed as means ± standard
deviations.
Results
Association between CXCR4 expression
in PaCa tissues and patient survival
Resected tissue specimens from patients with PaCa
were subjected to CXCR4 immunostaining (Fig. 1A). The patients were divided into
low and high CXCR4 expression groups according to the intensity of
CXCR4 immunostaining, and survival curves were generated. Of the 29
patients in the high expression group, 2 had stage 1 disease, none
had stage 2 disease, 9 had stage 3 disease, 17 had stage 4 disease,
and 1 had an unknown disease stage. Of the 63 patients in the low
expression group, 6 had stage 1 disease, 4 had stage 2 disease, 28
had stage 3 disease, 24 had stage 4 disease, and 1 had an unknown
disease stage. There were no differences in staging between the
high and low expression groups (P=0.233). Overall survival (OS) was
significantly worse in the high expression group (P=0.0068;
Fig. 1B).
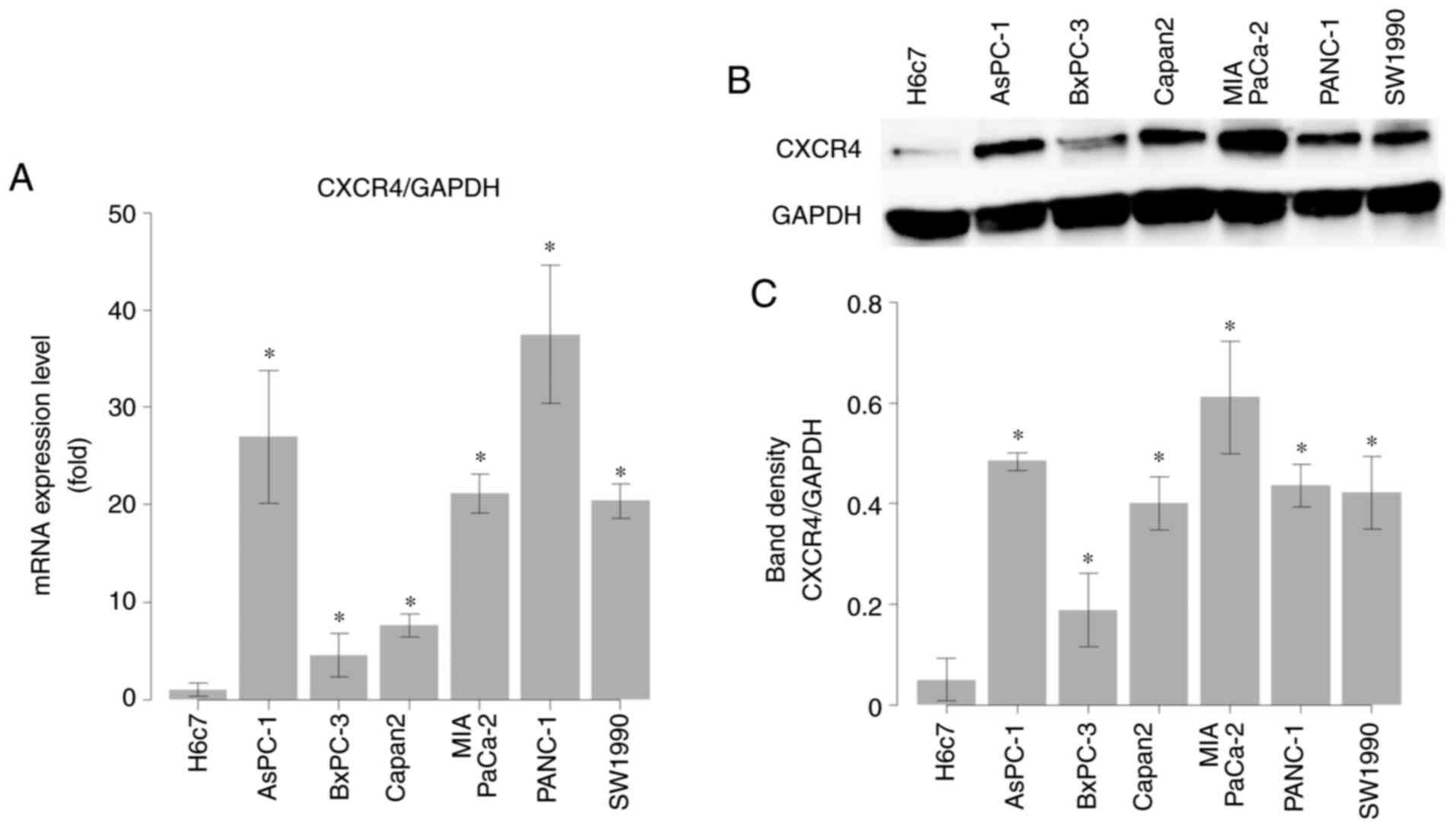
Enhanced expression of CXCR4 in PaCa
cells, but not HPDE cells
Expression of CXCR4 in H6c7 HPDE cells, which are
derived from the near normal pancreatic duct epithelium, and in
PaCa cell lines (AsPC-1, BxPC-3, Capan2, MIA PaCa-2, PANC-1, and
SW1990) was evaluated by RT-qPCR and western blotting. Both CXCR4
mRNA (Fig. 2A) and protein
(Fig. 2B and 2C) levels were
significantly higher in PaCa cell lines than in HPDE cells
(P<0.05).
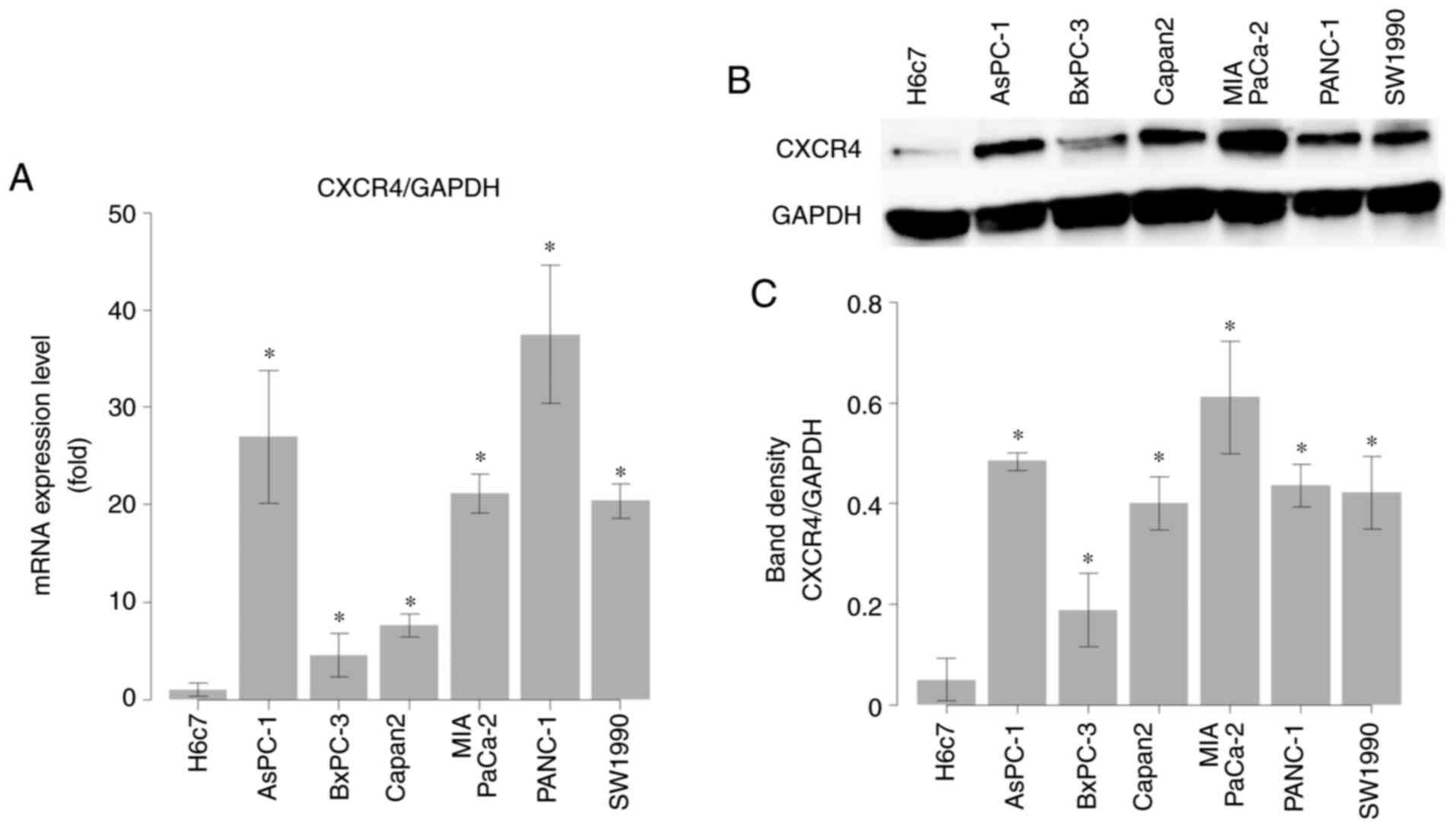 | Figure 2.Comparison of C-X-C chemokine
receptor type 4 (CXCR4) expression between human pancreatic duct
epithelial (HPDE) and pancreatic cancer (PaCa) cell lines. (A)
CXCR4 mRNA levels in HPDE cells (H6c7) and PaCa cells
(AsPC-1, BxPC-3, Capan2, MIA PaCa-2, PANC-1, and SW1990) measured
by RT-qPCR. The mRNA level of CXCR4 was expressed relative
to that of GAPDH in each sample. (B) CXCR4 protein levels in
HPDE cells (H6c7) and PaCa cells (AsPC-1, BxPC-3, Capan2, MIA
PaCa-2, PANC-1, and SW1990) measured by western blotting. (C) The
calculated band density of CXCR4 on western blots relative to that
of GAPDH in each sample. Comparisons between HPDE (H6c7) cells and
PaCa cells were evaluated using t-tests. *P<0.05. |
Establishment of radiation-resistant
PaCa cell lines
We succeeded in establishing radiation resistance in
two PaCa cell lines, MIA PaCa-2 and SW1990. MIA PaCa-2 and SW1990
cells were irradiated with 120 and 60 Gy, respectively. The
decrease in colonization after exposure to high doses of radiation
was significantly attenuated in the radiation-resistant cells
compared with that in their normal counterparts (P<0.05;
Fig. 3A-D).
 | Figure 3.Effects of irradiation on the
colonization of normal and radiation-resistant pancreatic cancer
(PaCa) cell lines (MIA PaCa-2 and SW1990). The number of
radiation-resistant PaCa cells to be seeded (200, 400, 1,000,
2,000, or 40,000) in 60-mm dishes depended on the dose (0, 2, 4, 6,
or 10 Gy). After culturing the cells overnight, irradiation was
performed at doses of 0–10 Gy. (A and B) After culturing for
another 14 days, the cells were fixed and stained, and the number
of colonies formed was counted. The survival rate was calculated as
the number of colonies divided by the number of seeded cells. (C)
MIA PaCa-2 and (D) SW1990 cells. Comparisons between normal PaCa
cells and radiation-resistant PaCa cells were evaluated using
t-tests. *P<0.05. |
cDNA microarray analysis of normal and
radiation-resistant MIA PaCa-2 cells
To investigate comprehensive differences in cDNA
expression between normal and radiation-resistant MIA PaCa-2 cells,
we used a cDNA microarray containing 62,976 probe sets. Of these
probes, 2,397 had higher expression (cut-off value, 2-fold) and
2,154 had lower expression (cut-off value, 0.5-fold) in
radiation-resistant cells compared with that in normal MIA PaCa-2
cells. Among stem cell markers of PaCa and chemokine receptors,
CXCR4 showed the highest expression level (Table I).
 | Table I.cDNA microarray of cancer stem cell
markers and chemokine receptor genes. |
Table I.
cDNA microarray of cancer stem cell
markers and chemokine receptor genes.
| Cancer stem cell
gene name | Fold change | Chemokine receptor
gene name | Fold change |
|---|
| Upregulated |
| Upregulated |
|
|
CXCR4 | 16.37 | CXCR4 | 16.37 |
|
CD44 | 2.97 | CCR10 | 2.28 |
|
CD24 | 1.67 | CXCR3 | 1.64 |
|
Nestin | 1.65 | CXCR1 | 1.29 |
|
BMI-1 | 1.48 | CXCR5 | 1.22 |
|
ESA | 1.29 | CCR1 | 1.15 |
|
EpCAM | 1.18 | CCR2 | 1.15 |
| Downregulated |
| CCR3 | 1.15 |
|
ALDH1A1 | 0.93 | CX3CR1 | 1.15 |
|
PON1 | 0.83 | CCR9 | 1.14 |
|
|
| CXCR2 | 1.13 |
|
|
| CXCR6 | 1.13 |
|
|
| CCR8 | 1.13 |
|
|
| CCR7 | 1.05 |
|
|
| Downregulated |
|
|
|
| CCR5 | 0.92 |
|
|
| CCR4 | 0.86 |
|
|
| XCR1 | 0.82 |
|
|
| CCR6 | 0.80 |
Enhanced expression of CXCR4 in
radiation-resistant PaCa cell lines
Immunofluorescence staining of CXCR4 in normal and
radiation-resistant PaCa cell lines confirmed the higher expression
of CXCR4 in radiation-resistant PaCa cell lines (Fig. 4A). RT-qPCR and western blotting
further confirmed that CXCR4 mRNA (Fig. 4B) and protein (Fig. 4C-F) levels were significantly
increased in radiation-resistant PaCa cell lines compared with
those in normal PaCa cell lines (P<0.05).
Changes in CXCR4 expression level
after knockdown of CXCR4 in PaCa cell lines
RT-qPCR was performed to evaluate changes in the
expression of CXCR4 mRNA in PaCa cell lines transfected with
CXCR4 siRNA. Transfection with CXCR4 siRNA
significantly downregulated CXCR4 in PaCa cell lines
compared with that in control cells and cells transfected with
negative control siRNA (P<0.05; Fig. S1).
The role of the CXCL12/CXCR4 axis in
PaCa cell invasion and the effects of CXCR4 knockdown on cell
invasion
There were no significant differences in cell
invasion ability between the negative control group and the
CXCR4-knockdown group. Addition of CXCL12 enhanced the invasion
ability of PaCa cell lines, and this effect was suppressed by CXCR4
knockdown (Fig. S2).
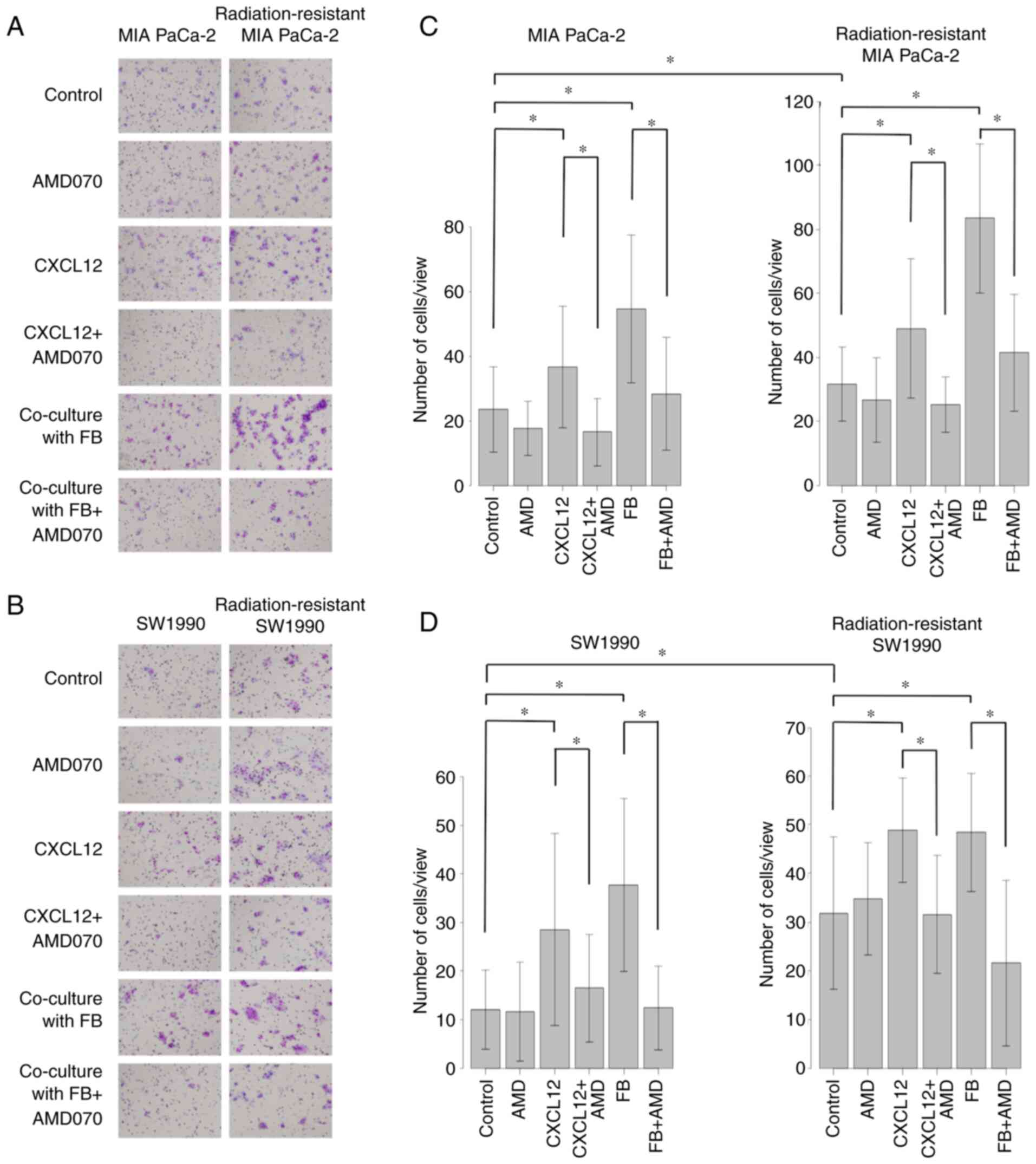
Role of the CXCL12/CXCR4 axis in PaCa
cell invasion and the effects of AMD070 on cell invasion
Cell invasion ability was greater in
radiation-resistant PaCa cell lines (MIA PaCa-2 and SW1990) than in
normal PaCa cell lines. The addition of CXCL12 enhanced the
invasion ability of PaCa cell lines, and this effect was suppressed
by AMD070 (AMD), which has been reported to act as a CXCR4
antagonist. Similarly, coculture with FBs enhanced the invasion
ability of PaCa cell lines, and this increase was suppressed by
AMD070 (Fig. 5A-D).
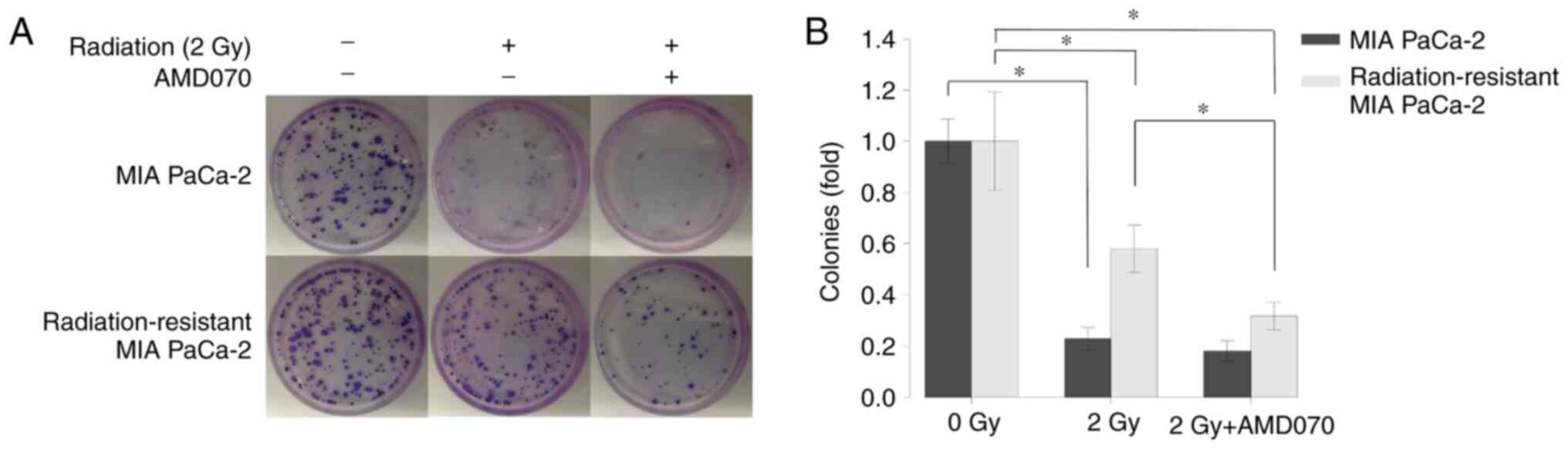
Effects of irradiation and AMD070 on
radiation-resistant PaCa cells
Irradiation (2 Gy) significantly suppressed the
colonization of both normal and radiation-resistant MIA PaCa-2
cells (P<0.05). AMD070 treatment significantly suppressed the
colonization of radiation-resistant MIA PaCa-2 cells after
irradiation (2 Gy) compared with cells treated with irradiation
alone (P<0.05; Fig. 6A and
B).
Discussion
The present study was designed to identify the
factors contributing to radiation resistance in PaCa cells and to
determine whether inhibition of these factors enhanced the
therapeutic effect of radiation. Our findings confirmed that both
C-X-C chemokine receptor type 4 (CXCR4) expression and invasion
ability were enhanced in radiation-resistant PaCa cell lines
compared with that in normal PaCa cell lines. Furthermore, the
CXCR4 antagonist AMD070 suppressed the PaCa cell invasion enhanced
by C-X-C motif chemokine ligand 12 (CXCL12) treatment or fibroblast
(FB) coculture, and when used in combination with irradiation,
AMD070 suppressed the colonization of radiation-resistant PaCa
cells.
Overexpression of CXCR4 has been confirmed in a
variety of tumors (39,40). CXCL12, a ligand for CXCR4, is a
chemokine secreted by stromal cells, FBs, and epithelial cells in a
wide range of tissues (41).
CXCL12/CXCR4 signaling affects all stages of tumor metastasis,
including migration, proliferation, and angiogenesis (42–45).
Notably, tumor growth is promoted by a small number of tumor stem
cells in cancers (46). CXCR4 is a
stem cell marker in PaCa (47) and
is overexpressed in cancer tissues compared with that noted in
normal pancreatic tissues; activation of the CXCL12/CXCR4 axis
promotes the migration and invasion of PaCa cells (30,42).
Patients with high CXCR4 expression in their resected PaCa tissues
exhibit poor survival (48). These
findings are consistent with the results of the present study.
Moreover, we observed differences in the expression levels of
CXCR4 mRNA and CXCR4 protein in PaCa cell lines. Thus, we
believe that these differences resulted from alterations in the
transcription process.
CXCL12/CXCR4 is involved in drug resistance in PaCa
(49). We previously demonstrated
an association between CXCL12/CXCR4 signaling and gemcitabine
resistance in gemcitabine-resistant PaCa cell lines (32). In addition, CXCR4 may be involved
in radiation resistance in colorectal cancer (50), thyroid cancer (51), and non-small cell lung cancer
(52). We established
radiation-resistant PaCa cell lines to investigate the factors
involved in the radiation resistance of PaCa. After performing DNA
microarray analysis and finding that the expression of CXCR4 was
higher in radiation-resistant than normal PaCa cell lines, we
focused on CXCR4. This is the first report to investigate the
importance of the CXCL12/CXCR4 signaling axis in radiation
resistance and the effects of a CXCR4 antagonist on
radiation-resistant PaCa cell lines.
PaCa manifests as a very stroma-rich, hard, and
scirrhous mass, consisting mainly of FBs, immune cells, blood
vessels, neurons, and various matricellular proteins (53). In PaCa, cancer-associated FBs
(CAFs) and myofibroblasts regulate local immunosuppression and
promote tumor progression, invasion, and distant metastasis
(54). CXCL12 is a chemokine that
controls immunosuppression. Radiation-resistant PaCa cell lines
with high expression of CXCR4 exhibited enhanced invasion ability
compared with normal PaCa cell lines, and the invasion ability was
further enhanced by the addition of CXCL12 or coculture with FBs.
C-X-C chemokine receptor type 7 (CXCR7) is another receptor for
CXCL12 and has also been reported to play important roles in cancer
invasion (55). Therefore, we
evaluated the mRNA levels of CXCR7 in normal and
radiation-resistant PaCa cell lines using RT-qPCR; however, our
results showed that CXCR7 expression was not enhanced in
radiation-resistant PaCa cell lines (data not shown). Furthermore,
irradiation of pancreatic CAFs was found to enhance the secretion
of CXCL12 from CAFs (56);
therefore, the role of the CXCL12/CXCR4 axis in irradiation of PaCa
is also noteworthy in terms of the relationship between PaCa and
FBs.
AMD070 is a small-molecule antagonist of CXCR4 that
is orally bioavailable, selective, and reversible (24). In vitro, AMD070 inhibits the
binding of CXCL12 to CXCR4 and blocks CXCL12-induced signaling
(57). In a phase 2 trial, the
therapeutic effects of AMD070 on warts, hypogammaglobulinemia,
infections, and myelokathexis syndrome, a congenital
immunodeficiency disease (58),
were evaluated, and the results confirmed that AMD070 was generally
safe, although some additional tests are required. We evaluated the
toxicity of AMD070 in PaCa cell lines and found that concentrations
up to 20 µM did not affect cell viability (data not shown). In both
normal and radiation-resistant PaCa cell lines, the invasion
ability enhanced by the addition of CXCL12 or coculture with FBs
was suppressed by AMD070 treatment. However, the addition of AMD070
alone did not suppress parental cell invasion ability, probably due
to the low concentration used or the short incubation time.
Furthermore, the colonization of radiation-resistant PaCa cell
lines was suppressed after treatment with AMD070, followed by
irradiation. Irradiation alone had a sufficient effect on the
colonization of normal PaCa cell lines, and the addition of AMD070
did not enhance the effect of irradiation. This result suggests
that AMD070 treatment may enhance the therapeutic effects of
irradiation in radiation-resistant PaCa and that the CXCL12/CXCR4
axis may be involved in radiation resistance.
The present study had some limitations. First, we
did not perform experiments confirming the protein expression of
the differentially expressed genes identified in the microarray
analysis. Additionally, we did not perform experiments using
CXCR4-overexpressing PaCa cell lines. In addition, we did not
evaluate the mechanisms of CXCR4 in radiation-resistant PaCa cell
lines in the absence of CXCL12 because CXCL12 is always secreted by
stromal cells, and further studies are still needed to elucidate
the mechanisms of radiation resistance in cell derivatives in the
absence of CXCL12.
In conclusion, the results of the present study
showed that CXCL12/CXCR4 signaling enhanced the invasion ability of
PaCa cell lines and that CXCL12/XCXR4 signaling was more active in
radiation-resistant PaCa cell lines. We also showed that the CXCR4
antagonist AMD070 suppressed the invasion ability enhanced by
CXCL12 treatment or FB coculture in radiation-resistant PaCa cell
lines and promoted the effects of irradiation on
radiation-resistant PaCa cell lines. Therefore, AMD070 may
represent a more effective therapeutic agent for PaCa, particularly
when used in combination with irradiation. However, further
investigations are required, including in vivo animal
experiments with nude mice, before AMD070 can be used in the
clinical setting.
Supplementary Material
Supporting Data
Acknowledgements
Not applicable.
Funding
Funding: Not applicable.
Availability of data and materials
The data generated or analyzed in this study are
included in the published article.
Authors' contributions
TK and YM contributed to the conception and design
of the study, analyzed and interpreted the data, and wrote and
reviewed the manuscript. TK, YM, KO, YH, HI, KS, MM, HT, and ST
designed the study. TK, YM, GU, HM, and YA acquired the data. TK,
YA, and YM confirmed the authenticity of all raw data. HM, KO, YH,
MM, and RO wrote the Materials and methods section of the
manuscript. YM, HT, RO, and ST provided technical, administrative,
or material support for performing RT-qPCR, western blotting, and
invasion assays. YM supervised the study. All authors read the
final manuscript and are equally responsible for all aspects of the
study, ensuring its integrity and accuracy.
Ethics approval and consent to
participate
This study was conducted with the approval of the
institutional review board established by Nagoya City University
(Nogoya, Japan) (approval no. 60-18-0025, date of approval; May 6,
2018).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
PaCa
|
pancreatic cancer
|
|
CXCR4
|
C-X-C chemokine receptor type 4
|
|
CXCL12
|
C-X-C motif chemokine ligand 12
|
|
HPDE
|
human pancreatic duct epithelial
|
|
FB
|
fibroblast
|
|
RT-qPCR
|
reverse-transcription quantitative
PCR
|
|
CAFs
|
cancer-associated fibroblasts
|
|
CXCR7
|
C-X-C chemokine receptor type 7
|
References
|
1
|
Siegel RL, Miller KD and Jemal A: Cancer
statistics, 2020. CA Cancer J Clin. 70:7–30. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Conroy T, Desseigne F, Ychou M, Bouché O,
Guimbaud R, Bécouarn Y, Adenis A, Raoul JL, Gourgou-Bourgade S, de
la Fouchardière C, et al: FOLFIRINOX versus gemcitabine for
metastatic pancreatic cancer. N Engl J Med. 364:1817–1825. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Williet N, Petrillo A, Roth G, Ghidni M,
Petrova M, Forestier J, Lopez A, Thoor A, Weislinger L, De Vita F,
et al: Gemcitabine/nab-paclitaxel versus FOLFIRINOX in locally
advanced pancreatic cancer: A European multicenter study. Cancers
(Basel). 13:27972021. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
de Geus SWL, Eskander MF, Kasumova GG, Ng
SC, Kent TS, Mancias JD, Callery MP, Mahadevan A and Tseng JF:
Stereotactic body radiotherapy for unresected pancreatic cancer: A
nationwide review. Cancer. 123:4158–4167. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Krishnan S, Chadha AS, Suh Y, Chen HC, Rao
A, Das P, Minsky BD, Mahmood U, Delclos ME, Sawakuchi GO, et al:
Focal radiation therapy dose escalation improves overall survival
in locally advanced pancreatic cancer patients receiving induction
chemotherapy and consolidative chemoradiation. Int J Radiat Oncol
Biol Phys. 94:755–765. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Shinoto M, Terashima K, Suefuji H,
Matsunobu A, Toyama S, Fukunishi K and Shinoyama Y: A single
institutional experience of combined carbon-ion radiotherapy and
chemotherapy for unresectable locally advanced pancreatic cancer.
Radiother Oncol. 129:333–339. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Matsuda T, Ajiki W, Marugame T, Ioka A,
Tsukuma H and Sobue T; Research Group of Population-Based Cancer
Registries of Japan, : Population-based survival of cancer patients
diagnosed between 1993 and 1999 in Japan: A chronological and
international comparative study. Jpn J Clin Oncol. 41:40–51. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Rahib L, Smith BD, Aizenberg R, Rosenzweig
AB, Fleshman JM and Matrisian LM: Projecting cancer incidence and
deaths to 2030: the unexpected burden of thyroid, liver, and
pancreas cancers in the United States. Cancer Res. 74:2913–2921.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Bilimoria KY, Bentrem DJ, Ko CY, Stewart
AK, Winchester DP and Talamonti MS: National failure to operate on
early stage pancreatic cancer. Ann Surg. 246:173–180. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Doi R, Imamura M, Hosotani R, Imaizumi T,
Hatori T, Takasaki K, Funakoshi A, Wakasugi H, Asano T, Hishinuma
S, et al: Surgery versus radiochemotherapy for resectable locally
invasive pancreatic cancer: final results of a randomized
multi-institutional trial. Surg Today. 38:1021–1028. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Vincent A, Herman J, Schulick R, Hruban RH
and Goggins M: Pancreatic cancer. Lancet. 378:607–620. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Sultana A, Tudur Smith C, Cunningham D,
Starling N, Tait D, Neoptolemos JP and Ghaneh P: Systematic review,
including meta-analyses, on the management of locally advanced
pancreatic cancer using radiation/combined modality therapy. Br J
Cancer. 96:1183–1190. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Vandercappellen J, Van Damme J and Struyf
S: The role of CXC chemokines and their receptors in cancer. Cancer
Lett. 267:226–244. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kulbe H, Levinson NR, Balkwill F and
Wilson JL: The chemokine network in cancer-much more than directing
cell movement. Int J Dev Biol. 48:489–496. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Feng Y, Broder CC, Kennedy PE and Berger
EA: Pillars article: HIV-1 entry cofactor: functional cDNA cloning
of a seven-transmembrane, G protein-coupled receptor. Science.
1996.272:872–877, J Immunol 186. 6076–6081. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Balkwill F: The significance of cancer
cell expression of the chemokine receptor CXCR4. Semin Cancer Biol.
14:171–179. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Chatterjee S, Behnam Azad B and Nimmagadda
S: The intricate role of CXCR4 in cancer. Adv Cancer Res.
124:31–82. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Zlotnik A: New insights on the role of
CXCR4 in cancer metastasis. J Pathol. 215:211–213. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Zhang J, Liu C, Mo X, Shi H and Li S:
Mechanisms by which CXCR4/CXCL12 cause metastatic behavior in
pancreatic cancer. Oncol Lett. 15:1771–1776. 2018.PubMed/NCBI
|
|
20
|
Krieg A, Riemer JC, Telan LA, Gabbert HE
and Knoefel WT: CXCR4-a prognostic and clinicopathological
biomarker for pancreatic ductal adenocarcinoma: A meta-analysis.
PLoS One. 10:e01301922015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Cui K, Zhao W, Wang C, Wang A, Zhang B,
Zhou W, Yu J, Sun Z and Li S: The CXCR4-CXCL12 pathway facilitates
the progression of pancreatic cancer via induction of angiogenesis
and lymphangiogenesis. J Surg Res. 171:143–150. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Sleightholm RL, Neilsen BK, Li J, Steele
MM, Singh RK, Hollingsworth MA and Oupicky D: Emerging roles of the
CXCL12/CXCR4 axis in pancreatic cancer progression and therapy.
Pharmacol Ther. 179:158–170. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
De Clercq E: The bicyclam AMD3100 story.
Nat Rev Drug Discov. 2:581–587. 2003. View
Article : Google Scholar : PubMed/NCBI
|
|
24
|
Skerlj RT, Bridger GJ, Kaller A, McEachern
EJ, Crawford JB, Zhou Y, Atsma B, Langille J, Nan S, Veale D, et
al: Discovery of novel small molecule orally bioavailable C-X-C
chemokine receptor 4 antagonists that are potent inhibitors of
T-tropic (X4) HIV-1 replication. J Med Chem. 53:3376–3388. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Cabioglu N, Summy J, Miller C, Parikh NU,
Sahin AA, Tuzlali S, Pumiglia K, Gallick GE and Price JE:
CXCL-12/stromal cell-derived factor-1alpha transactivates HER2-neu
in breast cancer cells by a novel pathway involving Src kinase
activation. Cancer Res. 65:6493–6497. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Hartmann TN, Burger JA, Glodek A, Fujii N
and Burger M: CXCR4 chemokine receptor and integrin signaling
co-operate in mediating adhesion and chemoresistance in small cell
lung cancer (SCLC) cells. Oncogene. 24:4462–4471. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Ohira S, Sasaki M, Harada K, Sato Y, Zen
Y, Isse K, Kozaka K, Ishikawa A, Oda K, Nimura Y and Nakanuma Y:
Possible regulation of migration of intrahepatic cholangiocarcinoma
cells by interaction of CXCR4 expressed in carcinoma cells with
tumor necrosis factor-alpha and stromal-derived factor-1 released
in stroma. Am J Pathol. 168:1155–1168. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Yasumoto K, Koizumi K, Kawashima A, Saitoh
Y, Arita Y, Shinohara K, Minami T, Nakayama T, Sakurai H, Takahashi
Y, et al: Role of the CXCL12/CXCR4 axis in peritoneal
carcinomatosis of gastric cancer. Cancer Res. 66:2181–2187. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Marchesi F, Monti P, Leone BE, Zerbi A,
Vecchi A, Piemonti L, Mantovani A and Allavena P: Increased
survival, proliferation, and migration in metastatic human
pancreatic tumor cells expressing functional CXCR4. Cancer Res.
64:8420–8427. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Saur D, Seidler B, Schneider G, Algül H,
Beck R, Senekowitsch-Schmidtke R, Schwaiger M and Schmid RM: CXCR4
expression increases liver and lung metastasis in a mouse model of
pancreatic cancer. Gastroenterology. 129:1237–1250. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Bockorny B, Semenisty V, Macarulla T,
Borazanci E, Wolpin BM, Stemmer SM, Golan T, Geva R, Borad MJ,
Pedersen KS, et al: BL-8040, a CXCR4 antagonist, in combination
with pembrolizumab and chemotherapy for pancreatic cancer: the
COMBAT trial. Nat Med. 26:878–885. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Morimoto M, Matsuo Y, Koide S, Tsuboi K,
Shamoto T, Sato T, Saito K, Takahashi H and Takeyama H: Enhancement
of the CXCL12/CXCR4 axis due to acquisition of gemcitabine
resistance in pancreatic cancer: Effect of CXCR4 antagonists. BMC
Cancer. 16:3052016. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Chang JT, Chan SH, Lin CY, Lin TY, Wang
HM, Liao CT, Wang TH, Lee LY and Cheng AJ: Differentially expressed
genes in radioresistant nasopharyngeal cancer cells: gp96 and
GDF15. Mol Cancer Ther. 6:2271–2279. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Matsuyama A, Inoue H, Shibuta K, Tanaka Y,
Barnard GF, Sugimachi K and Mori M: Hepatoma-derived growth factor
is associated with reduced sensitivity to irradiation in esophageal
cancer. Cancer Res. 61:5714–5717. 2001.PubMed/NCBI
|
|
35
|
Fukuda K, Sakakura C, Miyagawa K, Kuriu Y,
Kin S, Nakase Y, Hagiwara A, Mitsufuji S, Okazaki Y, Hayashizaki Y
and Yamagishi H: Differential gene expression profiles of
radioresistant oesophageal cancer cell lines established by
continuous fractionated irradiation. Br J Cancer. 91:1543–1550.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Wang T, Tamae D, LeBon T, Shively JE, Yen
Y and Li JJ: The role of peroxiredoxin II in radiation-resistant
MCF-7 breast cancer cells. Cancer Res. 65:10338–10346. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Xu QY, Gao Y, Liu Y, Yang WZ and Xu XY:
Identification of differential gene expression profiles of
radioresistant lung cancer cell line established by fractionated
ionizing radiation in vitro. Chin Med J (Engl). 121:1830–1837.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Bustin SA: Quantification of mRNA using
real-time reverse transcription PCR (RT-PCR): Trends and problems.
J Mol Endocrinol. 29:23–39. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Sasaki K, Natsugoe S, Ishigami S,
Matsumoto M, Okumura H, Setoyama T, Uchikado Y, Kita Y, Tamotsu K,
Sakurai T, et al: Expression of CXCL12 and its receptor CXCR4
correlates with lymph node metastasis in submucosal esophageal
cancer. J Surg Oncol. 97:433–438. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Taichman RS, Cooper C, Keller ET, Pienta
KJ, Taichman NS and McCauley LK: Use of the stromal cell-derived
factor-1/CXCR4 pathway in prostate cancer metastasis to bone.
Cancer Res. 62:1832–1837. 2002.PubMed/NCBI
|
|
41
|
Luther SA, Bidgol A, Hargreaves DC,
Schmidt A, Xu Y, Paniyadi J, Matloubian M and Cyster JG: Differing
activities of homeostatic chemokines CCL19, CCL21, and CXCL12 in
lymphocyte and dendritic cell recruitment and lymphoid neogenesis.
J Immunol. 169:424–433. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Billadeau DD, Chatterjee S, Bramati P,
Sreekumar R, Shah V, Hedin K and Urrutia R: Characterization of the
CXCR4 signaling in pancreatic cancer cells. Int J Gastrointest
Cancer. 37:110–119. 2006.PubMed/NCBI
|
|
43
|
Zlotnik A: Chemokines in neoplastic
progression. Semin Cancer Biol. 14:181–185. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Kucia M, Jankowski K, Reca R, Wysoczynski
M, Bandura L, Allendorf DJ, Zhang J, Ratajczak J and Ratajczak MZ:
CXCR4-SDF-1 signalling, locomotion, chemotaxis and adhesion. J Mol
Histol. 35:233–245. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Müller A, Homey B, Soto H, Ge N, Catron D,
Buchanan ME, McClanahan T, Murphy E, Yuan W, Wagner SN, et al:
Involvement of chemokine receptors in breast cancer metastasis.
Nature. 410:50–56. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Batlle E and Clevers H: Cancer stem cells
revisited. Nat Med. 23:1124–1134. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Vaz AP, Ponnusamy MP, Seshacharyulu P and
Batra SK: A concise review on the current understanding of
pancreatic cancer stem cells. J Cancer Stem Cell Res. 2:e10042014.
View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Maréchal R, Demetter P, Nagy N, Berton A,
Decaestecker C, Polus M, Closset J, Devière J, Salmon I and Van
Laethem JL: High expression of CXCR4 may predict poor survival in
resected pancreatic adenocarcinoma. Br J Cancer. 100:1444–1451.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Singh S, Srivastava SK, Bhardwaj A, Owen
LB and Singh AP: CXCL12-CXCR4 signalling axis confers gemcitabine
resistance to pancreatic cancer cells: a novel target for therapy.
Br J Cancer. 103:1671–1679. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Wang D, Jiao C, Zhu Y, Liang D, Zao M,
Meng X, Gao J, He Y, Liu W, Zhong Z and Cheng Z: Activation of
CXCL12/CXCR4 renders colorectal cancer cells less sensitive to
radiotherapy via up-regulating the expression of survivin. Exp Biol
Med (Maywood). 242:429–435. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Oweida A, Phan A, Vancourt B, Robin T,
Hararah MK, Bhatia S, Milner D, Lennon S, Pike L, Raben D, et al:
Hypofractionated radiotherapy is superior to conventional
fractionation in an orthotopic model of anaplastic thyroid cancer.
Thyroid. 28:739–747. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Kim JY, Kim HJ, Jung CW, Lee TS, Kim EH
and Park MJ: CXCR4 uses STAT3-mediated slug expression to maintain
radioresistance of non-small cell lung cancer cells: Emerges as a
potential prognostic biomarker for lung cancer. Cell Death Dis.
12:482021. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Mahadevan D and Von Hoff DD: Tumor-stroma
interactions in pancreatic ductal adenocarcinoma. Mol Cancer Ther.
6:1186–1197. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Neesse A, Algül H, Tuveson DA and Gress
TM: Stromal biology and therapy in pancreatic cancer: A changing
paradigm. Gut. 64:1476–1484. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Santagata S, Ieranò C, Trotta AM,
Capiluongo A, Auletta F, Guardascione G and Scala S: CXCR4 and
CXCR7 signaling pathways: A focus on the cross-talk between cancer
cells and tumor microenvironment. Front Oncol. 11:5913862021.
View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Li D, Qu C, Ning Z, Wang H, Zang K, Zhuang
L, Chen L, Wang P and Meng Z: Radiation promotes
epithelial-to-mesenchymal transition and invasion of pancreatic
cancer cell by activating carcinoma-associated fibroblasts. Am J
Cancer Res. 6:2192–2206. 2016.PubMed/NCBI
|
|
57
|
Mosi RM, Anastassova V, Cox J, Darkes MC,
Idzan SR, Labrecque J, Lau G, Nelson KL, Patel K, Santucci Z, et
al: The molecular pharmacology of AMD11070: An orally bioavailable
CXCR4 HIV entry inhibitor. Biochem Pharmacol. 83:472–479. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Dale DC, Firkin F, Bolyard AA, Kelley M,
Makaryan V, Gorelick K, Ebrahim T, Garg V, Tang W, Jiang H, et al:
Results of a phase 2 trial of an oral CXCR4 antagonist,
mavorixafor, for treatment of WHIM syndrome. Blood. 136:2994–3003.
2020. View Article : Google Scholar : PubMed/NCBI
|