Introduction
Non-SMC condensin I complex subunit G (NCAPG) was
originally identified from nuclear extracts of HeLa cells (1). NCAPG has been shown to be involved in
chromosomal organization and rearrangement via interaction with
non-SMC condensin I complex subunit H (NCAPH) (2) and non-SMC condensin I complex subunit
D2 (NCAPD2) (3) to form condensin
complex I, which maintains the overall stability of chromosomes
through participating in chromosome organization and rearrangement,
and by promoting the correct segregation and accurate distribution
of chromosomes during mitosis (4,5). Hara
et al (2) found that the
NCAPG-NCAPH subcomplex consists of the N-terminal domain of
polypeptide human chromosome-associated polypeptide-G (hCAP-G)
linked to its C-terminal domain and a fragment of polypeptide human
chromosome-associated polypeptide-H (hCAP-H) containing motif IV.
This subcomplex has the ability to interact with both double- and
single-stranded DNA, contributing to the correct assembly and
segregation of chromosomes. The homologue of the NCAPG subunit in
Drosophila is the dCAP-G protein. The dCAP-G mutation
results in delayed chromosome condensation at prometaphase, and
failure of sister chromatid segregation at anaphase (6). Murphy and Sarge (7) found that the three potential
phosphorylation sites on the hCAP-G subunit were Thr-308, Thr-332
and Thr-931, and mutation of these residues to alanine was
demonstrated to affect the localization of NCAPG during
mitosis.
However, it has been revealed that abnormal
expression of NCAPG often affects the occurrence and development of
a wide variety of tumours, including lung cancer (8,9),
hepatocellular carcinoma (HCC) (10,11),
colorectal cancer (12), pancreatic
cancer (13,14), breast cancer (BC) (15), ovarian cancer (16), endometrial carcinoma (17), glioma (18), rhabdomyosarcoma (19) and melanoma (20). When NCAPG is highly expressed, the
proliferation and invasion of tumours is promoted, and the
expression level of NCAPG is negatively correlated with the
prognosis of patients, suggesting that NCAPG is a factor that
adversely affects the survival of patients with tumour.
Surprisingly, NCAPG is expressed at low levels in basal cell
carcinoma (BCC) (21),
lymphoblastic acute myeloid leukemia (4) and multiple myeloma (22), and this may be associated with
immune infiltration and reduced mitogenic gene expression, leading
to cell proliferation arrest.
In HCC (11),
colorectal cancer (12) and lung
adenocarcinoma (LUAD) (23), NCAPG
expression has been identified to be closely associated with the
degree of lymph node metastasis, tumour clinical stage and tumour
progression, and overexpression of NCAPG was associated with poor
prognosis in these patients. In addition, high expression of NCAPG
was associated with tumour infiltration of several immune cell
types, including B cells and CD4 memory T cells in non-small cell
lung cancer (NSCLC) (9) and
neutrophils in HCC (24),
suggesting accordingly that NCAPG fulfils an important role in
regulating tumour immunity.
NCAPG has been reported to have pro-carcinogenic
biological functions, including promoting tumour cell
proliferation, cell cycle function, cell migration, in vivo
tumour formation in mice and in vivo metastasis, and it has
been proposed that this may be associated with cellular pathways,
cell cycle, mismatch repair and cellular damage (25–28).
Therefore, further study of the function and underlying mechanisms
of NCAPG should enable improved understanding of the processes of
tumourigenesis and development, in order to potentially provide
novel targets and strategies for tumour therapy.
Role of NCAPG in tumourigenesis and
development
Association between NCAPG and cell
proliferation, apoptosis, migration and invasion
A large number of studies have demonstrated that
NCAPG is able to regulate cell proliferation, apoptosis, migration
and invasion. NCAPG has been shown to be overexpressed in HCC, and
its level of expression correlates with clinicopathological
features, such as recurrence, time to recurrence, metastasis,
differentiation and tumour-node-metastasis staging (11). The long non-coding RNA (lncRNA)
taurine-upregulated gene 1 (TUG1) was revealed to be overexpressed
in HCC, where it mediates HCC cell growth, epithelial-mesenchymal
transition (EMT) and metastasis (29). Li et al (30) found that TUG1 could target and
regulate NCAPG, and the expression of NCAPG is negatively
correlated with survival in HCC. It has been demonstrated that,
upon knockdown of NCAPG, the expression levels of the cell cycle
proteins A1 and CDK2, Bcl-2 and N-calmodulin are inhibited, causing
the cell cycle to stall in the S-phase (11), resulting in a weakening of the
ability of cells to migrate and invade (31), thereby inducing apoptosis. It has
also been revealed that knockdown of NCAPG reduces cell viability,
causes abnormal mitosis and mitochondrial fragmentation and
promotes apoptosis (32). Ai et
al (33) detected that the
microRNA (miRNA) miR-181c was significantly downregulated in HCC
and that the expression level of miR-181c was negatively correlated
with the expression level of NCAPG. Knockdown of NCAPG was also
found to result in decreased rates of cell proliferation, invasion
and migration, a reduced level of EMT and the promotion of
apoptosis.
A previously published study by Li et al
(34) revealed that NCAPG is a key
gene in castration-resistant prostate cancer (CRPC). In a previous
study, Goto et al (35)
showed that miR-145-3p was lowly expressed in CRPC tissues, where
it acted as a negative regulator of NCAPG, thereby functioning as a
tumour suppressor. Furthermore, the miRNA miR-99a-3p was found to
significantly downregulate NCAPG expression in CRPC, suggesting
that it may fulfil an important oncogenic function in CRPC
(36).
Yu et al (37) reported that knockdown of NCAPG
resulted in cell cycle blockade in the S and G2 phases of the
cycle, which resulted in a marked decrease in the proliferative and
invasive capabilities of ovarian cancer cells and in the induction
of apoptosis.
Song et al (38) demonstrated that NCAPG is highly
expressed in gastric cancer and is enriched in the cell cycle.
NCAPG serves as a downstream target of miR-193b-3p, and it is
negatively regulated by this miRNA; moreover, its overexpression
was found to promote the proliferation of gastric cancer cells. Sun
et al (39) found that the
expression level of NCAPG in the tumour cells of patients with
advanced gastric cancer was markedly increased compared with that
in the early stage of the disease. Knockdown of NCAPG induced cell
cycle arrest in G0/G1 phase, thereby inhibiting both the rates of
cell proliferation, migration and invasion and EMT. Zhang et
al (27) found that, in gastric
cancer, silencing of NCAPG resulted in cell cycle arrest in G1
phase, downregulation of the expression of the cell cycle proteins
cyclin D1, CDK4 and CDK6, an increase in the expression of cell
cycle inhibitors (p21 and p27) and reduced cellular proliferation
rates, whereas the opposite effects were observed with the
overexpression of NCAPG. Taken together, these findings suggested
that NCAPG affects cell proliferation via regulating the cell
cycle, thereby providing a novel strategy for the treatment of
gastric cancer with CDK4/6 inhibitors.
Clear cell renal cell carcinoma (ccRCC) is a common
type of renal cancer (40). It has
been revealed that the expression level of NCAPG is significantly
upregulated in ccRCC (41). Li
et al (42) showed that
knocking down NCAPG resulted in a decrease in CDK1 expression, with
the subsequent inhibition of cell proliferation, whereas
overexpression of CDK1 partly reversed the reduction in the cell
proliferation rate, suggesting that NCAPG is involved in the
proliferation of ccRCC through its interaction with the CDK1
signalling pathway.
A previous study by Li et al (43) demonstrated that NCAPG is a key gene
in LUAD, and a high expression level of NCAPG was shown to be
strongly correlated with poor patient prognosis. Zhang et al
(27) found that silencing NCAPG
impeded the progression of NSCLC cells through inhibiting their
proliferation, invasion and tumour growth, both in vitro and
in vivo. Further investigation revealed that silencing NCAPG
resulted in decreased expression levels of CDK4, CDK6 and cyclin
D1, and an increased expression of p27 and p21, resulting in
blockade of the cell cycle at G1 phase and the induction of
apoptosis (27,44). Proline-rich protein 11 (PRR11) and
spindle and kinetochore-associated 2 (SKA2) together form a
classical head-to-head gene pair that serves an important role in
tumour development (45). A
previous study (46) demonstrated
that, in NSCLC, NCAPG is able to interact with PRR11 and SKA2 to
activate the Hedgehog (Hh) pathway, and the use of inhibitors of
the Hh-regulated transcription factors GLI1 and GLI2 led to a
marked reduction in the expression levels of PRR11, SKA2 and NCAPG.
Taken together, these findings suggested that these three proteins
are regulated by the Hh-GLI signalling pathway, thereby affecting
the proliferation and migration rates of NSCLC cells.
Moura-Castro et al (47) reported that one of the mechanisms
that may be associated with hyper-diploid acute lymphoblastic
leukemia is an increased heterogeneity of the chromosome copy
number due to the downregulation of NCAPG expression, which leads
to the cohesion defect of sister chromosomes. It has been revealed
that downregulation of NCAPG expression is also present in patients
with multiple myeloma or acute myeloid leukemia, and that this may
help to slow the proliferation rate and aggressiveness of cells
associated with these types of cancer (22).
Association of NCAPG and cell
stemness
Stemness, defined as the ability of a cell or tissue
to self-renew and differentiate into multiple cell types, was
originally identified in human embryonic stem cells, although
subsequently it was found that pluripotent stem cells could be
obtained from undifferentiated somatic cells by induction (48,49).
In addition, certain normally differentiated cells have been shown
to regain stem cell-like abilities in the event of loss of
differentiation characteristics, and these are referred to as
cancer stem cells (CSCs) (50,51).
CSCs are capable of self-renewal and multidirectional
differentiation, and exert an important role in promoting tumour
progression, drug resistance and recurrence (52,53).
Through a biosignature study, Pan et al
(54) demonstrated that NCAPG could
be used as a biomarker for the characterization of bladder cancer
stem cells. Subsequently, Li et al (55) found that, in brain low-grade gliomas
(LGG), NCAPG was able to influence the E2F pathway and promote
tumour recurrence through upregulating the expression level of the
stemness indicator, aurora kinase A (AURKA). It has been found by
Li et al (56) that
expression of the circular RNA circNCAPG is higher in glioma stem
cells compared with that in differentiated glioma cells, and that
this is also associated with a worse prognosis. Ras response
element binding protein 1 (RREB1) binds to circNCAPG and can
regulate circNCAPG through the U2 nucleoprotein cofactor 65 kDa
(U2AF65), thereby constituting a U2AF65/circNCAPG/RREB1 positive
feedback loop. It was further found that RREB1 is able to promote
the expression of proteins such as CD133, SRY-box transcription
factor 2 (SOX2), Nanog and Oct4, whereas it had no direct
regulatory effect on gene expression at the RNA level.
In addition, it has been identified that, in gastric
cancer, high expression levels of NCAPG are associated with a
higher stemness index and longer overall survival time compared
with lower expression levels of NCAPG (57–59).
Zhang et al (60) revealed
that, in LUAD, NCAPG was positively correlated with the glycolysis
marker genes HK2, PKM9 and LDHA. Upon knockdown of NCAPG, both the
glycolytic level and the glycolytic capability of LUAD cells were
found to be markedly reduced. Moreover, the expression levels of
CD133, CD44 and Oct-4 were significantly increased when NCAPG was
overexpressed, whereas the use of glycolysis inhibitors led to a
reversal of the observed changes, suggesting that NCAPG promotes
stemness of LUAD cells via activating the glycolytic pathway.
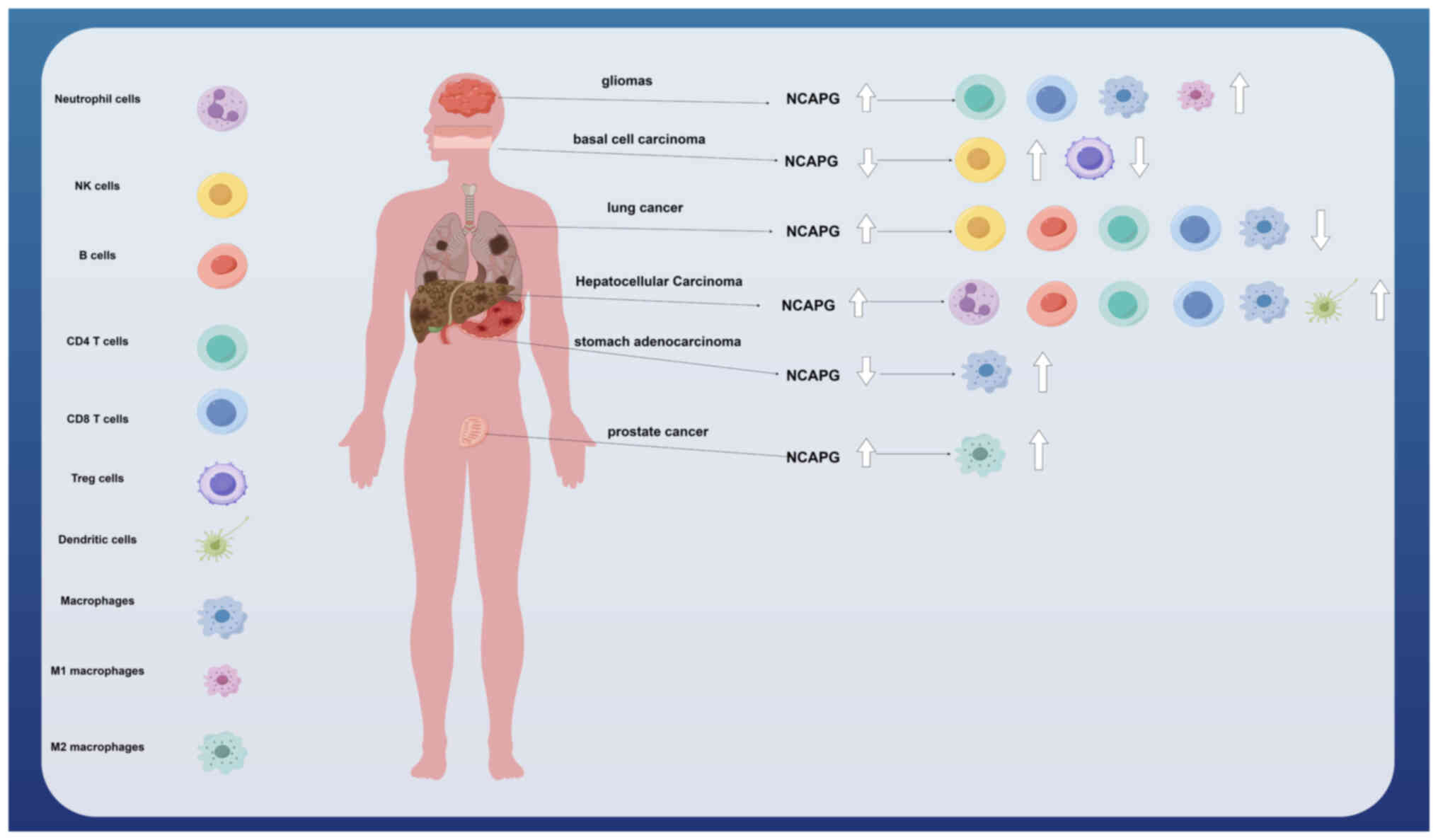
Association of NCAPG and immune
infiltration
In tumour tissues, there are numerous other types of
cells associated with the tumour microenvironment, such as normal
stromal cells, immune cells and vascular endothelial cells
(61,62). Interactions between tumour cells and
the tumour microenvironment influence tumour development, and
gaining an improved understanding of their roles should provide the
key to unlocking a new era of tumour therapy (63,64).
Xu et al (65) found that NCAPG is one of the pivotal
genes associated with M2-tumour-associated macrophage infiltration
in prostate cancer, and that patients with high NCAPG expression
had a poor prognosis. In addition, Xiang et al (57) found that, in stomach adenocarcinoma
(STAD), increased macrophage expression levels with low expression
of NCAPG led to the promotion of tumour progression and poor
prognosis. NCAPG was positively correlated with the expression of
certain immune checkpoint genes, including CD80, CTLA4, IDO1 and
CD274, suggesting that STAD may be treated with corresponding
immune checkpoint inhibitors. Li et al (55) found that the expression of NCAPG was
upregulated in LGG and correlated with poor prognosis and immune
infiltration (including an increased expression of CD8 T-cells, CD4
memory resting T-cells, macrophages and M1 macrophages). In NSCLC,
a high expression of NCAPG was found to be associated with immune
infiltration in which the levels of B cells, CD4 memory T cells,
CD8 memory T cells, macrophages and natural killer (NK) T cells
were reduced, thereby affecting the prognosis of NSCLC (9). Furthermore, it was shown by Guo and
Zhu (24) that a high expression of
NCAPG in HCC tissues was positively correlated with both immune
cell infiltration (B cells, CD4 memory T cells, CD8 memory T cells,
macrophages, neutrophils and dendritic cells) and the expression of
associated molecular markers (CD19, IRF5, ITGAM and ITGAX), leading
to poor prognosis. Interestingly, Xie et al (21) found that NCAPG was lowly expressed
in BCC, and that this was significantly negatively correlated with
NK cells and positively correlated with T regulatory cells,
suggesting that NCAPG may fulfil an oncogene role in BCC, thereby
providing guidance for new treatment strategies (Fig. 1).
NCAPG is involved in the regulation of
tumour chemotherapy resistance
The tyrosine kinase Src is a proto-oncogene that
exerts a key role in regulating cell proliferation, differentiation
and metastasis (66,67). A previous study (68) revealed that the expression level of
NCAPG is positively correlated with Src-associated genes; moreover,
the expression level of NCAPG is increased in
HER2+/trastuzumab-resistant BC, and this is closely
correlated with shorter patient survival times and recurrence.
Overexpression of NCAPG led to a markedly increased level of Src
phosphorylation, whereas inhibition of Src using either specific
inhibitors or shRNA resulted in reduced rates of cell
proliferation, suggesting the important influence of
NCAPG-dependent trastuzumab resistance. NCAPG overexpression
promotes BC cell proliferation and resistance to apoptosis, and
confers resistance to trastuzumab, whereas knockdown of NCAPG
causes trastuzumab resistance to be restored, suggesting that the
maintenance of low NCAPG expression may be more sensitive to the
application of chemotherapeutic agents.
lncRNAs have been shown to fulfil important roles in
tumour drug resistance (69–71). A
study by Bao et al (72)
found that, in LUAD, the mutation frequency of EGFR was increased
with high expression of NCAPG compared with low NCAPG expression,
and the IC50 value (the half-maximal inhibitory
concentration) was found to be higher with the EGFR-tyrosine kinase
inhibitor (EGFR-TKI) erlotinib, suggesting an association with
resistance to EGFR-TKIs. Higher expression levels of NCAPG were
also found in resistant patients with LUAD who were treated with
either erlotinib or gefitinib. Using Ensembl database (73), it was revealed that NCAPG is able to
potentially regulate the lncRNA AC099850.3; therefore,
understanding the mechanism of the lncRNA AC099850.3-NCAGP
signalling axis, and how this is associated with resistance to
EGFR-TKIs, may provide a novel approach for the treatment of
LUAD.
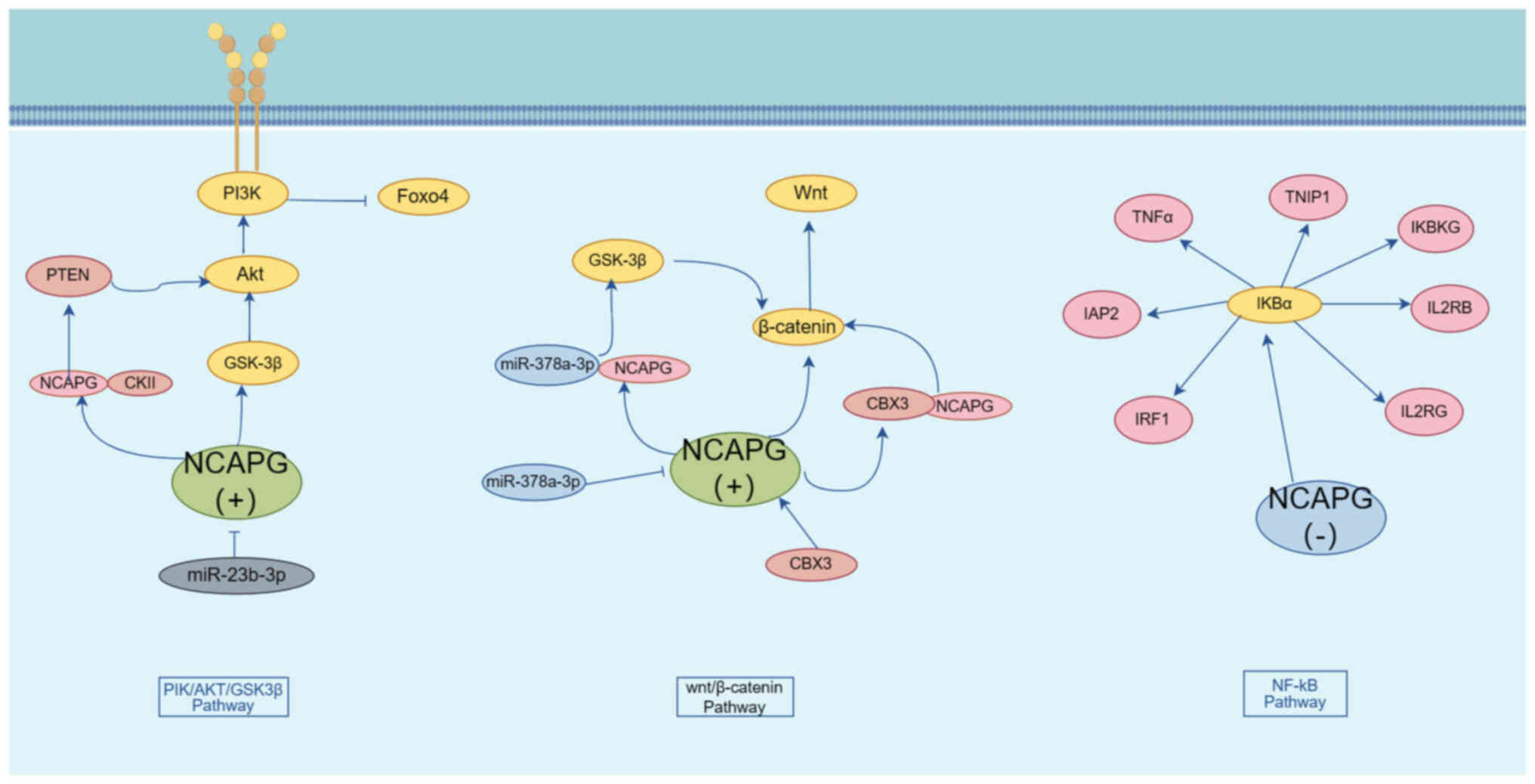
Mechanisms associated with signalling
pathways and NCAPG in regulating tumour cells
NCAPG and the PI3K/AKT pathway
The PI3K/AKT pathway is an important cell signalling
pathway that is involved in a variety of biological processes,
including cell growth, proliferation, migration and invasion
(74). A study by Gong et al
(75) identified that NCAPG
overexpression could both promote the phosphorylation and
activation of PI3K and AKT and lead to the inhibition of FOXO4
phosphorylation, and that NCAPG was able to interact with PI3K, AKT
and FOXO4 to activate PI3K/AKT/FOXO4 signalling, promote HCC cell
proliferation and invasion and inhibit apoptosis; therefore,
targeting and regulating NCAPG expression may provide a possible
new avenue for the treatment of HCC. A study by Zhang et al
(27) revealed that, in pancreatic
adenocarcinoma, overexpression of NCAPG led to an increase in the
phosphorylation levels of PI3K, AKT and GSK3β, whereas the use of
AKT inhibitors caused a marked inhibition of the growth of lung
cancer cells with high NCAPG expression.
miR-23b-3p is a cancer-associated biomarker that has
been shown to be downregulated in colon cancer, which mediates
tumour cell proliferation, migration and invasion (76,77).
Li et al (78) demonstrated
that miR-23b-3p was negatively correlated with NCAPG. Knockdown of
NCAPG led to an inhibition of AKT phosphorylation and activation;
moreover, NCAPG was found to interact with phosphorylated (p)-PI3K
and p-AKT to negatively regulate apoptosis through influencing the
miR-23b-3p/NCAPG/PI3K/AKT signalling pathway.
PTEN is a phosphatase that negatively regulates the
PI3K/AKT pathway, and cancer may develop as a consequence of loss
or mutation of the PTEN gene (79,80).
Casein kinase 2 α1 (CKII) is a ubiquitous and highly conserved
protein serine/threonine kinase that exerts an important role in
cell cycle regulation and cell proliferation (81). Zhang et al (82) found that, in HCC, NCAPG is able to
interact with CKII, thereby affecting PTEN expression. Upon
overexpression of NCAPG, the levels of CKII, p-AKT and p-PTEN were
found to be higher, resulting in the promotion of cell
proliferation. Subsequently, the promotion of PTEN phosphorylation
upon overexpression of NCAPG was found to be reversed with the use
of CKII inhibitors, impairing cell proliferation. Taken together,
these findings suggested that NCAPG inhibits PTEN expression
through interaction with CKII, which in turn activates the PI3K/AKT
pathway and promotes the proliferation of HCC cells.
NCAPG and the Wnt/β-catenin
pathway
The Wnt pathway is an important signalling pathway
that is involved in the regulation of cell proliferation,
differentiation, apoptosis, stem cell self-renewal, tissue
homeostasis and wound healing (83,84).
Liu et al (85) showed that,
in endometrial cancer, knockdown of NCAPG could inhibit tumour cell
proliferation and promote cell apoptosis through inhibiting the
expression of β-catenin. Zhang et al (86) demonstrated that, in pancreatic
adenocarcinoma, overexpression of NCAPG led to an increase in the
expression of vimentin, N-cadherin, Snail and Slug, and a decrease
in the expression of E-cadherin, suggesting that overexpression of
NCAPG may promote the EMT process in tumour cells. In addition, Shi
et al (12) demonstrated
that knockdown of NCAPG led to the inactivation of Wnt/β-catenin
and EMT, which resulted in a marked inhibition in the migratory and
invasion rates of colon cancer cells, thereby leading to the
elimination of the accelerated cell migration and invasion rates
that were caused by NCAPG overexpression. Moreover, it was revealed
that NCAPG may be a downstream target of the Wnt/β-catenin
signalling pathway, and that it is involved in cell proliferation,
invasion, migration and EMT processes associated with colon cancer.
Yang et al (87) reported
that NCAPG interacts with chromobox protein homolog 3 (CBX3),
which, in turn, regulates the expression of Wnt3a and β-linker
proteins, whereas a deficiency of NCAPG led to an inhibition of
cell invasion and the induction of apoptosis in colorectal cancer
cells through its influence on the CBX3/NCAPG/Wnt pathway.
Li et al (88) revealed that NCAPG was highly
expressed in oral cancer cells, and could directly bind to the
oncogene miR-378a-3p; moreover, it was negatively regulated by
miR-378a-3p. Knockdown of the NCAPG gene caused a marked inhibition
of the GSK-3β/β-catenin pathway, suggesting that miR-378a-3p is
able to regulate the GSK-3β/β-catenin pathway through affecting
NCAPG expression.
NCAPG and the retinoblastoma (RB)
tumour suppressor pathway
The RB pathway is a signalling pathway associated
with cell cycle regulation, which serves an important role in cell
proliferation and apoptosis (89,90).
The core member of the RB pathway is the RB protein (pRb), a
repressive transcription factor that inhibits cell cycle
progression through binding to the transcription factor E2F
(91,92). Xiao et al (4) showed that, in BC, the downregulation
of NCAPG expression resulted in an increase in the level of
poly(ADP-ribose) polymerase (PARP) protein, a decrease in the
expression levels of pRb and cell cycle protein B1 and a marked
inhibition of cell proliferation, suggesting that NCAPG may promote
BC cell proliferation by regulating the RB pathway. In
glioblastoma, Hou et al (26) revealed that NCAPG is able to
interact with PARP1, a co-activator of E2F1, and that NCAPG is a
downstream target gene of E2F1; moreover, a high expression of
NCAPG positively regulates the E2F1 pathway.
NCAPG and the p53 pathway
p53 is an important oncogene that has significant
roles in the regulation of cell cycle, senescence and apoptosis
(93,94). Dong et al (95) identified a number of miRNAs (such as
miR-101-3p, miR-195-5p, miR-214-3p and miR-944) that serve to
reduce NCAPG expression to promote BC development, and these are
enriched in the p53 signalling pathway. In addition, it was
observed that knockdown of NCAPG gene expression resulted in a
significant decrease in the expression level of CDC25C, which acts
as a direct target of p53 transcription factor and cell cycle
arrest in G2/M phase, further emphasizing its function as an
oncogene. Taking all these findings into consideration, it has been
proposed that NCAPG may influence the p53 signalling pathway via
regulating the expression of CDC25C.
NCAPG and the NF-κB pathway
NF-κB represents a class of transcription factors
that fulfill key roles in several biological processes, including
inflammation, immune response and cell growth (96,97). A
previous study by Swindell et al (98) identified NCAPG as a potential NF-κB
target gene. In bladder cancer (99), knockdown of NCAPG was shown to
result in a lower degradation rate of IκBα and inhibition of the
NF-kB pathway in a dose-dependent manner. Knockdown of NCAPG also
resulted in downregulation of the expression of NF-κB downstream
genes, including TNFα, inhibitor of apoptosis 2 (IAP2), inhibitor
of NF-κB kinase regulatory subunit γ (IKBKG), interleukin (IL)-2RB,
IL-2RG, interferon regulatory factor 1 (IRF1) and TNFAIP3
interacting protein 1 (TNIP1), thereby attenuating cell
proliferation. It has been suggested that NCAPG promotes bladder
cancer progression through regulating the NF-κB signalling pathway
(Fig. 2).
NCAPG and the signal transducer and
activator of transcription 3 (STAT3) signalling pathway
STAT3 is a transcription factor that fulfils
important roles in tumour cell proliferation, metastasis, invasion
and immunosuppression (100,101). A previous study by Li et al
(102) found that, in
triple-negative BC, knockdown of NCAPG resulted in a significant
decrease in the expression of p-EGFR, p-JAK1 and p-STAT3, although
the inhibitory effect of knockdown of NCAPG on p-STAT3 could be
reversed by using agonists of the EGFR and JAK/STAT3 signalling
pathways, accompanied by an increase in cell proliferation,
invasion and migration and a decrease in apoptosis. NCAPG was
demonstrated to affect cell proliferation, invasion, migration and
apoptosis through influencing the EGFR/JAK/STAT3 signalling
pathway. Jiang et al (68)
revealed that overexpression of NCAPG led to an increase in the
transcriptional activity and phosphorylation level of STAT3, as
well as increasing the expression level of the downstream factors
of STAT3 signalling, cytosolic protein D1 and BCL2, whereas
inhibition of NCAPG elicited the opposite results. Taken together,
these results suggested that NCAPG may mediate BC cell
proliferation and exert its anti-apoptotic effects through
activation of the Src/STAT3 signalling pathway.
NCAPG and the transforming growth
factor β (TGF-β) pathway
TGF-β is an important extracellular signalling
molecule that has a key role in physiological processes, including
cell growth, differentiation and migration, apoptosis, immunity and
EMT (103,104). Wu et al (23) found that the expression of p-Smad2
and p-Smad3 in the TGF-β signalling pathway was increased upon
overexpression of NCAPG, leading to the promotion of cell
proliferation, invasion, migration and EMT. Subsequently, upon
overexpression of NCAPG, the use of an inhibitor of the TGF-β
signalling pathway effectively reversed the effects mediated on the
EMT process and the proliferative, migratory and invasive
capabilities of LUAD cells. Li et al (56) demonstrated that circNCAPG is highly
expressed in glioma stem cells, where it interacts with the
RNA-binding protein U2AF65. It was further found that circNCAPG
binds to RREB1, promoting RREB1 entry into the nucleus and
activating the TGF-β1 pathway. It was therefore suggested that
RREB1 promotes glioma stem cell proliferation, invasion and
maintenance of self-renewal through promoting the expression of
U2AF65, enhancing the stability of circNCAPG and forming the
U2AF65/circNCAPG/RREB1 positive feedback pathway.
Conclusions
Intracellularly, increased expression of NCAPG
promotes cell proliferation by facilitating the transition from G1
to S and G2/M phases. NCAPG can also affect the proliferation,
apoptosis and EMT of tumour cells through multiple signalling
pathways, including PI3K/AKT, Wnt, RB, p53, STAT3 and TGF-β,
promoting tumour development and progression. In addition, it is
important to focus on the fact that NCAPG is able to promote the
maintenance of stem cell properties by affecting the Wnt/β-catenin
pathway. Extracellularly, high expression of NCAPG was associated
with enhanced invasiveness and migration of tumour cells.
Furthermore, NCAPG may help tumour cells evade the immune system by
affecting immune cells in the tumour microenvironment. In
conclusion, NCAPG, as a cell cycle regulatory protein, promotes
cell proliferation not only inside the cell by affecting the cell
cycle and cell stemness, but also outside the cell by affecting the
tumour microenvironment to promote tumour invasion and metastasis.
Continuing research and in-depth studies on the function and
underlying molecular mechanisms of NCAPG should lay the foundation
for the discovery of novel antitumour drug targets, and the
realization of precise and personalized tumour therapies.
Acknowledgements
Not applicable.
Funding
The present study was supported by the Affiliated Hospital of
Zunyi Medical University [grant no. Institution (2015) 34], the
Guizhou Provincial Department of Science and Technology [grant no.
Qiankehe LH Zi (2014) 7573], the Affiliated Hospital of Zunyi
Medical University [grant no. Institution (2016) 45] and the
Collaborative Innovation Center of Chinese Ministry of Education
(grant no. 2020-39).
Availability of data and materials
Not applicable.
Authors' contributions
RL and DW drafted the manuscript and contributed
equally to the study. HY and LP participated in the literature
search and analysis of the data to be included in the review. XL
and FY were involved in the design of the study and assisted in the
preparation of the figures. RZ edited and revised the manuscript.
All authors have read and approved the final version of the
manuscript. Data authentication is not applicable.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Ono T, Losada A, Hirano M, Myers MP,
Neuwald AF and Hirano T: Differential contributions of condensin I
and condensin II to mitotic chromosome architecture in vertebrate
cells. Cell. 115:109–121. 2003. View Article : Google Scholar
|
|
2
|
Hara K, Kinoshita K, Migita T, Murakami K,
Shimizu K, Takeuchi K, Hirano T and Hashimoto H: Structural basis
of HEAT-kleisin interactions in the human condensin I subcomplex.
EMBO Rep. 20:e471832019. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kinoshita K, Kobayashi TJ and Hirano T:
Balancing acts of two HEAT subunits of condensin I support dynamic
assembly of chromosome axes. Dev Cell. 33:94–106. 2015. View Article : Google Scholar
|
|
4
|
Xiao C, Gong J, Jie Y, Cao J, Chen Z, Li
R, Chong Y, Hu B and Zhang Q: NCAPG is a promising therapeutic
target across different tumor types. Front Pharmacol. 11:3872020.
View Article : Google Scholar
|
|
5
|
Eberlein A, Takasuga A, Setoguchi K, Pfuhl
R, Flisikowski K, Fries R, Klopp N, Fürbass R, Weikard R and Kühn
C: Dissection of genetic factors modulating fetal growth in cattle
indicates a substantial role of the non-SMC condensin I complex,
subunit G (NCAPG) gene. Genetics. 183:951–964. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Dej KJ, Ahn C and Orr-Weaver TL: Mutations
in the Drosophila condensin subunit dCAP-G: Defining the
role of condensin for chromosome condensation in mitosis and gene
expression in interphase. Genetics. 168:895–906. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Murphy LA and Sarge KD: Phosphorylation of
CAP-G is required for its chromosomal DNA localization during
mitosis. Biochem Biophys Res Commun. 377:1007–1011. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Sun H, Zhang H, Yan Y, Li Y, Che G, Zhou
C, Nicot C and Ma H: Correction: NCAPG promotes the oncogenesis and
progression of non-small cell lung cancer cells through
upregulating LGALS1 expression. Mol Cancer. 21:2212022. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Yuan Y, Jiang X, Tang L, Wang J, Zhang D,
Cho WC and Duan L: FOXM1/lncRNA TYMSOS/miR-214-3p-mediated high
expression of NCAPG correlates with poor prognosis and cell
proliferation in non-small cell lung carcinoma. Front Mol Biosci.
8:7857672022. View Article : Google Scholar
|
|
10
|
Fu Q, Yang F, Zhao J, Yang X, Xiang T,
Huai G, Zhang J, Wei L, Deng S and Yang H: Bioinformatical
identification of key pathways and genes in human hepatocellular
carcinoma after CSN5 depletion. Cell Signal. 49:79–86. 2018.
View Article : Google Scholar
|
|
11
|
Liu W, Liang B, Liu H, Huang Y, Yin X,
Zhou F, Yu X, Feng Q, Li E, Zou Z and Wu L: Overexpression of
non-SMC condensin I complex subunit G serves as a promising
prognostic marker and therapeutic target for hepatocellular
carcinoma. Int J Mol Med. 40:731–738. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Shi Y, Ge C, Fang D, Wei W, Li L, Wei Q
and Yu H: NCAPG facilitates colorectal cancer cell proliferation,
migration, invasion and epithelial-mesenchymal transition by
activating the Wnt/β-catenin signaling pathway. Cancer Cell Int.
22:1192022. View Article : Google Scholar
|
|
13
|
Wu C, Huang ZH, Meng ZQ, Fan XT, Lu S, Tan
YY, You LM, Huang JQ, Stalin A, Ye PZ, et al: A network
pharmacology approach to reveal the pharmacological targets and
biological mechanism of compound kushen injection for treating
pancreatic cancer based on WGCNA and in vitro experiment
validation. Chin Med. 16:1212021. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Zhang D, Cui F, Peng L, Wang M, Yang X,
Xia C, Li K, Yin H, Zhang Y, Yu Q, et al: Establishing and
validating an ADCP-related prognostic signature in pancreatic
ductal adenocarcinoma. Aging (Albany NY). 14:6299–6315. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Hitti E, Bakheet T, Al-Souhibani N,
Moghrabi W, Al-Yahya S, Al-Ghamdi M, Al-Saif M, Shoukri MM, Lánczky
A, Grépin R, et al: Systematic analysis of AU-rich element
expression in cancer reveals common functional clusters regulated
by key RNA-binding proteins. Cancer Res. 76:4068–4080. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Xu T, Dong M, Wang Z, Li H and Li X:
Elevated mRNA expression levels of NCAPG are associated with poor
prognosis in ovarian cancer. Cancer Manag Res. 12:5773–5786. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Zhang W, Gao L, Wang C, Wang S, Sun D, Li
X, Liu M, Qi Y, Liu J and Lin B: Combining bioinformatics and
experiments to identify and verify key genes with prognostic values
in endometrial carcinoma. J Cancer. 11:716–732. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Wang M, Cui Y, Cai Y, Jiang Y and Peng Y:
Comprehensive bioinformatics analysis of mRNA expression profiles
and identification of a miRNA-mRNA network associated with the
pathogenesis of low-grade gliomas. Cancer Manag Res. 13:5135–5147.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Lu S, Sun C, Chen H, Zhang C, Li W, Wu L,
Zhu J, Sun F, Huang J, Wang J, et al: Bioinformatics analysis and
validation identify CDK1 and MAD2L1 as prognostic markers of
rhabdomyosarcoma. Cancer Manag Res. 12:12123–12136. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ryu B, Kim DS, Deluca AM and Alani RM:
Comprehensive expression profiling of tumor cell lines identifies
molecular signatures of melanoma progression. PLoS One. 2:e5942007.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Xie D, Chen X, Wu H, Ning D, Cao X and Wan
C: Prediction of diagnostic gene biomarkers associated with immune
infiltration for basal cell carcinoma. Clin Cosmet Investig
Dermatol. 15:2657–2673. 2022. View Article : Google Scholar
|
|
22
|
Cohen Y, Gutwein O, Garach-Jehoshua O,
Bar-Haim A and Kornberg A: The proliferation arrest of primary
tumor cells out-of-niche is associated with widespread
downregulation of mitotic and transcriptional genes. Hematology.
19:286–292. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Wu Y, Lin Y, Pan J, Tu X, Xu Y, Li H and
Chen Y: NCAPG promotes the progression of lung adenocarcinoma via
the TGF-β signaling pathway. Cancer Cell Int. 21:4432021.
View Article : Google Scholar
|
|
24
|
Guo ZY and Zhu ZT: NCAPG is a prognostic
biomarker associated with vascular invasion in hepatocellular
carcinoma. Eur Rev Med Pharmacol Sci. 25:7238–7251. 2021.
|
|
25
|
Sun DP, Wu CC, Chou CL, Cheng LC, Wang WC,
Lin SS, Hung ST, Tian YF, Fang CL and Lin KY: NCAPG deregulation
indicates poor patient survival and contributes to colorectal
carcinogenesis. Pathol Res Pract. 241:1542382023. View Article : Google Scholar
|
|
26
|
Hou J, Huang P, Xu M, Wang H, Shao Y, Weng
X, Liu Y, Chang H, Zhang L and Cui H: NCAPG promotes the
progression of glioblastoma by facilitating PARP1-mediated E2F1
transactivation. Neuro Oncol. 25:2023. View Article : Google Scholar
|
|
27
|
Zhang X, Wang H, Han Y, Zhu M, Song Z,
Zhan D and Jia J: NCAPG induces cell proliferation in cardia
adenocarcinoma via PI3K/AKT signaling pathway. Onco Targets Ther.
13:11315–11326. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Guo M, Li X, Li J and Li B: Identification
of the prognostic biomarkers and their correlations with immune
infiltration in colorectal cancer through bioinformatics analysis
and in vitro experiments. Heliyon. 9:e171012023. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Farzaneh M, Ghasemian M, Ghaedrahmati F,
Poodineh J, Najafi S, Masoodi T, Kurniawan D, Uddin S and
Azizidoost S: Functional roles of lncRNA-TUG1 in hepatocellular
carcinoma. Life Sci. 308:1209742022. View Article : Google Scholar
|
|
30
|
Li L, Liu S, Peng L, Zhang Y, Zhang Y,
Zeng H, Li G and Zhang C: The identification and preliminary study
of lncRNA TUG1 and its related genes in hepatocellular carcinoma.
Arch Med Sci. 18:1582–1595. 2019.
|
|
31
|
Liu K, Li Y, Yu B, Wang F, Mi T and Zhao
Y: Silencing non-SMC chromosome-associated polypeptide G inhibits
proliferation and induces apoptosis in hepatocellular carcinoma
cells. Can J Physiol Pharmacol. 96:1246–1254. 2018. View Article : Google Scholar
|
|
32
|
Wang Y, Gao B, Tan PY, Handoko YA, Sekar
K, Deivasigamani A, Seshachalam VP, OuYang HY, Shi M, Xie C, et al:
Genome-wide CRISPR knockout screens identify NCAPG as an essential
oncogene for hepatocellular carcinoma tumor growth. FASEB J.
33:8759–8770. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Ai J, Gong C, Wu J, Gao J, Liu W, Liao W
and Wu L: MicroRNA-181c suppresses growth and metastasis of
hepatocellular carcinoma by modulating NCAPG. Cancer Manag Res.
11:3455–3467. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Li Y, Shi H, Zhao Z and Xu M:
Identification of castration-dependent and -independent driver
genes and pathways in castration-resistant prostate cancer (CRPC).
BMC Urol. 22:1622022. View Article : Google Scholar
|
|
35
|
Goto Y, Kurozumi A, Arai T, Nohata N,
Kojima S, Okato A, Kato M, Yamazaki K, Ishida Y, Naya Y, et al:
Impact of novel miR-145-3p regulatory networks on survival in
patients with castration-resistant prostate cancer. Br J Cancer.
117:409–420. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Arai T, Okato A, Yamada Y, Sugawara S,
Kurozumi A, Kojima S, Yamazaki K, Naya Y, Ichikawa T and Seki N:
Regulation of NCAPG by miR-99a-3p (passenger strand) inhibits
cancer cell aggressiveness and is involved in CRPC. Cancer Med.
7:1988–2002. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Yu H, Zou D, Ni N, Zhang S, Zhang Q and
Yang L: Overexpression of NCAPG in ovarian cancer is associated
with ovarian cancer proliferation and apoptosis via p38 MAPK
signaling pathway. J Ovarian Res. 15:982022. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Song B, Du J, Song DF, Ren JC and Feng Y:
Dysregulation of NCAPG, KNL1, miR-148a-3p, miR-193b-3p, and
miR-1179 may contribute to the progression of gastric cancer. Biol
Res. 51:442018. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Sun DP, Lin CC, Hung ST, Kuang YY, Hseu
YC, Fang CL and Lin KY: Aberrant expression of NCAPG is associated
with prognosis and progression of gastric cancer. Cancer Manag Res.
12:7837–7846. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Wolf MM, Kimryn Rathmell W and Beckermann
KE: Modeling clear cell renal cell carcinoma and therapeutic
implications. Oncogene. 39:3413–3426. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Liu B, Xiao Y, Li H, Zhang AL, Meng LB,
Feng L, Zhao ZH, Ni XC, Fan B, Zhang XY, et al: Identification and
verification of biomarker in clear cell renal cell carcinoma via
bioinformatics and neural network model. Biomed Res Int.
2020:69547932020.
|
|
42
|
Li H, Zheng P, Li Z, Han Q, Zhou B, Wang X
and Wang K: NCAPG promotes the proliferation of renal clear cell
carcinoma via mediating with CDK1. Dis Markers.
2022:67585952022.PubMed/NCBI
|
|
43
|
Li S, Xuan Y, Gao B, Sun X, Miao S, Lu T,
Wang Y and Jiao W: Identification of an eight-gene prognostic
signature for lung adenocarcinoma. Cancer Manag Res. 10:3383–3392.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Wang X, Tian X, Sui X, Li X, Zhao X, Han
K, Sun L and Dong Y: Increased expression of NCAPG (Non-SMC
condensing I complex subunit G) is associated with progression and
poor prognosis of lung adenocarcinoma. Bioengineered. 13:6113–6125.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Chen J, Yang HM, Zhou HC, Peng RR, Niu ZX
and Kang CY: PRR11 and SKA2 promote the proliferation, migration
and invasion of esophageal carcinoma cells. Oncol Lett. 20:639–646.
2020. View Article : Google Scholar
|
|
46
|
Sun Y, Xu D, Zhang C, Wang Y, Zhang L,
Qiao D, Bu Y and Zhang Y: HEDGEHOG/GLI modulates the PRR11-SKA2
bidirectional transcription unit in lung squamous cell carcinomas.
Genes (Basel). 12:1202021. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Moura-Castro LH, Peña-Martínez P, Castor
A, Galeev R, Larsson J, Järås M, Yang M and Paulsson K: Sister
chromatid cohesion defects are associated with chromosomal copy
number heterogeneity in high hyperdiploid childhood acute
lymphoblastic leukemia. Genes Chromosomes Cancer. 60:410–417. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Yu J, Vodyanik MA, Smuga-Otto K,
Antosiewicz-Bourget J, Frane JL, Tian S, Nie J, Jonsdottir GA,
Ruotti V, Stewart R, et al: Induced pluripotent stem cell lines
derived from human somatic cells. Science. 318:1917–1920. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
49
|
González F, Boué S and Izpisúa Belmonte
JC: Methods for making induced pluripotent stem cells:
Reprogramming à la carte. Nat Rev Genet. 12:231–242. 2011.
View Article : Google Scholar
|
|
50
|
van Es JH, Sato T, van de Wetering M,
Lyubimova A, Yee Nee AN, Gregorieff A, Sasaki N, Zeinstra L, van
den Born M, Korving J, et al: Dll1+ secretory progenitor cells
revert to stem cells upon crypt damage. Nat Cell Biol.
14:1099–1104. 2012. View Article : Google Scholar
|
|
51
|
Chaffer CL, Brueckmann I, Scheel C,
Kaestli AJ, Wiggins PA, Rodrigues LO, Brooks M, Reinhardt F, Su Y,
Polyak K, et al: Normal and neoplastic nonstem cells can
spontaneously convert to a stem-like state. Proc Natl Acad Sci USA.
108:7950–7955. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Yang L, Shi P, Zhao G, Xu J, Peng W, Zhang
J, Zhang G, Wang X, Dong Z, Chen F and Cui H: Targeting cancer stem
cell pathways for cancer therapy. Signal Transduct Target Ther.
5:82020. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Huang T, Song X, Xu D, Tiek D, Goenka A,
Wu B, Sastry N, Hu B and Cheng SY: Stem cell programs in cancer
initiation, progression, and therapy resistance. Theranostics.
10:8721–8743. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Pan S, Zhan Y, Chen X, Wu B and Liu B:
Identification of biomarkers for controlling cancer stem cell
characteristics in bladder cancer by network analysis of
transcriptome data stemness indices. Front Oncol. 9:6132019.
View Article : Google Scholar
|
|
55
|
Li J, Zhou M, Huang D, Lin R, Cui X, Chen
S, Yao Y, Xian S, Wang S, Fu Q, et al: The recurrent-specific
regulation network of prognostic stemness-related signatures in
low-grade glioma. Dis Markers. 2023:22439282023. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Li H, Jiang Y, Hu J, Xu J, Chen L, Zhang
G, Zhao J, Zong S, Guo Z, Li X, et al: The U2AF65/circNCAPG/RREB1
feedback loop promotes malignant phenotypes of glioma stem cells
through activating the TGF-β pathway. Cell Death Dis. 14:232023.
View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Xiang Z, Cha G, Wang Y, Gao J and Jia J:
Characterizing the crosstalk of NCAPG with tumor microenvironment
and tumor stemness in stomach adenocarcinoma. Stem Cells Int.
2022:18883582022. View Article : Google Scholar
|
|
58
|
Xia X and Li Y: Comprehensive analysis of
transcriptome data stemness indices identifies key genes for
controlling cancer stem cell characteristics in gastric cancer.
Transl Cancer Res. 9:6050–6061. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Guo SH, Ma L and Chen J: Identification of
prognostic markers and potential therapeutic targets in gastric
adenocarcinoma by machine learning based on mRNAsi index. J Oncol.
2022:89261272022. View Article : Google Scholar
|
|
60
|
Zhang Z, Qi D, Liu X and Kang P: NCAPG
stimulates lung adenocarcinoma cell stemness through aerobic
glycolysis. Clin Respir J. 17:884–892. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Xiao Y and Yu D: Tumor microenvironment as
a therapeutic target in cancer. Pharmacol Ther. 221:1077532021.
View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Hinshaw DC and Shevde LA: The tumor
microenvironment innately modulates cancer progression. Cancer Res.
79:4557–4566. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Jin MZ and Jin WL: The updated landscape
of tumor microenvironment and drug repurposing. Signal Transduct
Target Ther. 5:1662020. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Wu T and Dai Y: Tumor microenvironment and
therapeutic response. Cancer Lett. 387:61–68. 2017. View Article : Google Scholar
|
|
65
|
Xu N, Dong RN, Lin TT, Lin T, Lin YZ, Chen
SH, Zhu JM, Ke ZB, Huang F, Chen YH and Xue XY: Development and
validation of novel biomarkers related to M2 macrophages
infiltration by weighted gene co-expression network analysis in
prostate cancer. Front Oncol. 11:6340752021. View Article : Google Scholar
|
|
66
|
Aleshin A and Finn RS: SRC: A century of
science brought to the clinic. Neoplasia. 12:599–607. 2010.
View Article : Google Scholar
|
|
67
|
Roskoski R Jr: Src protein-tyrosine kinase
structure and regulation. Biochem Biophys Res Commun.
324:1155–1164. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Jiang L, Ren L, Chen H, Pan J, Zhang Z,
Kuang X, Chen X, Bao W, Lin C, Zhou Z, et al: NCAPG confers
trastuzumab resistance via activating SRC/STAT3 signaling pathway
in HER2-positive breast cancer. Cell Death Dis. 11:5472020.
View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Singh D, Assaraf YG and Gacche RN: Long
non-coding RNA mediated drug resistance in breast cancer. Drug
Resist Updat. 63:1008512022. View Article : Google Scholar
|
|
70
|
Wei L, Sun J, Zhang N, Zheng Y, Wang X, Lv
L, Liu J, Xu Y, Shen Y and Yang M: Noncoding RNAs in gastric
cancer: Implications for drug resistance. Mol Cancer. 19:622020.
View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Entezari M, Ghanbarirad M, Taheriazam A,
Sadrkhanloo M, Zabolian A, Goharrizi MASB, Hushmandi K, Aref AR,
Ashrafizadeh M, Zarrabi A, et al: Long non-coding RNAs and exosomal
lncRNAs: Potential functions in lung cancer progression, drug
resistance and tumor microenvironment remodeling. Biomed
Pharmacother. 150:1129632022. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Bao J, Wu Y, Zhang K and Qi H:
AC099850.3/NCAPG axis predicts poor prognosis and is associated
with resistance to EGFR tyrosine-kinase inhibitors in lung
Adenocarcinoma. Int J Gen Med. 15:6917–6930. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Cunningham F, Allen JE, Allen J,
Alvarez-Jarreta J, Amode MR, Armean IM, Austine-Orimoloye O, Azov
AG, Barnes I, Bennett R, et al: Ensembl 2022. Nucleic Acids Res.
50(D1): D988–D995. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
He Y, Sun MM, Zhang GG, Yang J, Chen KS,
Xu WW and Li B: Targeting PI3K/Akt signal transduction for cancer
therapy. Signal Transduct Target Ther. 6:4252021. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Gong C, Ai J, Fan Y, Gao J, Liu W, Feng Q,
Liao W and Wu L: NCAPG promotes the proliferation of hepatocellular
carcinoma through PI3K/AKT signaling. Onco Targets Ther.
12:8537–8552. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Grossi I, Salvi A, Baiocchi G, Portolani N
and De Petro G: Functional role of microRNA-23b-3p in cancer
biology. Microrna. 7:156–166. 2018. View Article : Google Scholar
|
|
77
|
Kou CH, Zhou T, Han XL, Zhuang HJ and Qian
HX: Downregulation of mir-23b in plasma is associated with poor
prognosis in patients with colorectal cancer. Oncol Lett.
12:4838–4844. 2016. View Article : Google Scholar
|
|
78
|
Li P, Wen J, Ren X, Zhou Y, Xue Y, Yan Z,
Li S, Tian H, Tang XG and Zhang GJ: MicroRNA-23b-3p targets non-SMC
condensing I complex subunit G to promote proliferation and inhibit
apoptosis of colorectal cancer cells via regulation of the PI3K/AKT
signaling pathway. Oncol Lett. 22:8122021. View Article : Google Scholar
|
|
79
|
Worby CA and Dixon JE: PTEN. Annu Rev
Biochem. 83:641–669. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Álvarez-Garcia V, Tawil Y, Wise HM and
Leslie NR: Mechanisms of PTEN loss in cancer: It's all about
diversity. Semin Cancer Biol. 59:66–79. 2019. View Article : Google Scholar
|
|
81
|
Oh NS, Yoon SH, Lee WK, Choi JY, Min do S
and Bae YS: Phosphorylation of CKBBP2/CRIF1 by protein kinase CKII
promotes cell proliferation. Gene. 386:147–153. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Zhang R, Ai J, Wang J, Sun C, Lu H, He A,
Li M, Liao Y, Lei J, Zhou F, et al: NCAPG promotes the
proliferation of hepatocellular carcinoma through the
CKII-dependent regulation of PTEN. J Transl Med. 20:3252022.
View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Zhou Y, Xu J, Luo H, Meng X, Chen M and
Zhu D: Wnt signaling pathway in cancer immunotherapy. Cancer Lett.
525:84–96. 2022. View Article : Google Scholar
|
|
84
|
Rim EY, Clevers H and Nusse R: The Wnt
pathway: From signaling mechanisms to synthetic modulators. Annu
Rev Biochem. 91:571–598. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Liu C, Yan Y, Di F, Li W, Yin X and Dong
L: Inhibition of NCAPG expression inactivates the Wnt/β-catenin
signal to suppresses endometrial cancer cell growth in vitro.
Environ Toxicol. 36:2512–2520. 2021. View Article : Google Scholar
|
|
86
|
Zhang X, Zhu M, Wang H, Song Z, Zhan D,
Cao W, Han Y and Jia J: Overexpression of NCAPG inhibits cardia
adenocarcinoma apoptosis and promotes epithelial-mesenchymal
transition through the Wnt/β-catenin signaling pathway. Gene.
766:1451632021. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Yang H, Pu L, Li R and Zhu R: NCAPG is
transcriptionally regulated by CBX3 and activates the Wnt/β-catenin
signaling pathway to promote proliferation and the cell cycle and
inhibit apoptosis in colorectal cancer. J Gastrointest Oncol.
14:900–912. 2023. View Article : Google Scholar
|
|
88
|
Li J, Sun S, Li J, Zhao X, Li Z, Sha T and
Cui Z: NCAPG, mediated by miR-378a-3p, regulates cell
proliferation, cell cycle progression, and apoptosis of oral
squamous cell carcinoma through the GSK-3β/β-catenin signaling.
Neoplasma. 68:1201–1211. 2021. View Article : Google Scholar
|
|
89
|
Du W and Searle JS: The rb pathway and
cancer therapeutics. Curr Drug Targets. 10:581–589. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Lin SC, Skapek SX and Lee EY: Genes in the
RB pathway and their knockout in mice. Semin Cancer Biol.
7:279–289. 1996. View Article : Google Scholar
|
|
91
|
Nevins JR: The Rb/E2F pathway and cancer.
Hum Mol Genet. 10:699–703. 2001. View Article : Google Scholar
|
|
92
|
Schaal C, Pillai S and Chellappan SP: The
Rb-E2F transcriptional regulatory pathway in tumor angiogenesis and
metastasis. Adv Cancer Res. 121:147–182. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Liu J, Zhang C, Wang J, Hu W and Feng Z:
The regulation of ferroptosis by tumor suppressor p53 and its
pathway. Int J Mol Sci. 21:83872020. View Article : Google Scholar
|
|
94
|
Huang J: Current developments of targeting
the p53 signaling pathway for cancer treatment. Pharmacol Ther.
220:1077202021. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Dong M, Xu T, Cui X, Li H, Li X and Xia W:
NCAPG upregulation mediated by four microRNAs combined with
activation of the p53 signaling pathway is a predictor of poor
prognosis in patients with breast cancer. Oncol Lett. 21:3232021.
View Article : Google Scholar
|
|
96
|
DiDonato JA, Mercurio F and Karin M: NF-κB
and the link between inflammation and cancer. Immunol Rev.
246:379–400. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Oeckinghaus A, Hayden M S and Ghosh S:
Crosstalk in NF-κB signaling pathways. Nat Immunol. 12:695–708.
2011. View Article : Google Scholar
|
|
98
|
Swindell WR, Bojanowski K and Chaudhuri
RK: A novel fumarate, isosorbide di-(methyl fumarate) (IDMF),
replicates astrocyte transcriptome responses to dimethyl fumarate
(DMF) but specifically down-regulates genes linked to a reactive
phenotype. Biochem Biophys Res Commun. 532:475–481. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Tang F, Yu H, Wang X, Shi J, Chen Z, Wang
H, Wan Z, Fu Q, Hu X, Zuhaer Y, et al: NCAPG promotes tumorigenesis
of bladder cancer through NF-κB signaling pathway. Biochem Biophys
Res Commun. 622:101–107. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Yu H, Lee H, Herrmann A, Buettner R and
Jove R: Revisiting STAT3 signalling in cancer: New and unexpected
biological functions. Nat Rev Cancer. 14:736–746. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Zou S, Tong Q, Liu B, Huang W, Tian Y and
Fu X: Targeting STAT3 in cancer immunotherapy. Mol Cancer.
19:1452020. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Li J, Zheng J, Lin B, Sun H, Lu S, Wang D
and Huo H: Knockdown of NCAPG promotes the apoptosis and inhibits
the invasion and migration of triple-negative breast cancer
MDA-MB-231 cells via regulation of EGFR/JAK/STAT3 signaling. Exp
Ther Med. 25:1192023. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Peng D, Fu M, Wang M, Wei Y and Wei X:
Targeting TGF-β signal transduction for fibrosis and cancer
therapy. Mol Cancer. 21:1042022. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Derynck R, Turley SJ and Akhurst RJ: TGFβ
biology in cancer progression and immunotherapy. Nat Rev Clin
Oncol. 18:9–34. 2021. View Article : Google Scholar
|