|
1
|
Ono T, Losada A, Hirano M, Myers MP,
Neuwald AF and Hirano T: Differential contributions of condensin I
and condensin II to mitotic chromosome architecture in vertebrate
cells. Cell. 115:109–121. 2003. View Article : Google Scholar
|
|
2
|
Hara K, Kinoshita K, Migita T, Murakami K,
Shimizu K, Takeuchi K, Hirano T and Hashimoto H: Structural basis
of HEAT-kleisin interactions in the human condensin I subcomplex.
EMBO Rep. 20:e471832019. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kinoshita K, Kobayashi TJ and Hirano T:
Balancing acts of two HEAT subunits of condensin I support dynamic
assembly of chromosome axes. Dev Cell. 33:94–106. 2015. View Article : Google Scholar
|
|
4
|
Xiao C, Gong J, Jie Y, Cao J, Chen Z, Li
R, Chong Y, Hu B and Zhang Q: NCAPG is a promising therapeutic
target across different tumor types. Front Pharmacol. 11:3872020.
View Article : Google Scholar
|
|
5
|
Eberlein A, Takasuga A, Setoguchi K, Pfuhl
R, Flisikowski K, Fries R, Klopp N, Fürbass R, Weikard R and Kühn
C: Dissection of genetic factors modulating fetal growth in cattle
indicates a substantial role of the non-SMC condensin I complex,
subunit G (NCAPG) gene. Genetics. 183:951–964. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Dej KJ, Ahn C and Orr-Weaver TL: Mutations
in the Drosophila condensin subunit dCAP-G: Defining the
role of condensin for chromosome condensation in mitosis and gene
expression in interphase. Genetics. 168:895–906. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Murphy LA and Sarge KD: Phosphorylation of
CAP-G is required for its chromosomal DNA localization during
mitosis. Biochem Biophys Res Commun. 377:1007–1011. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
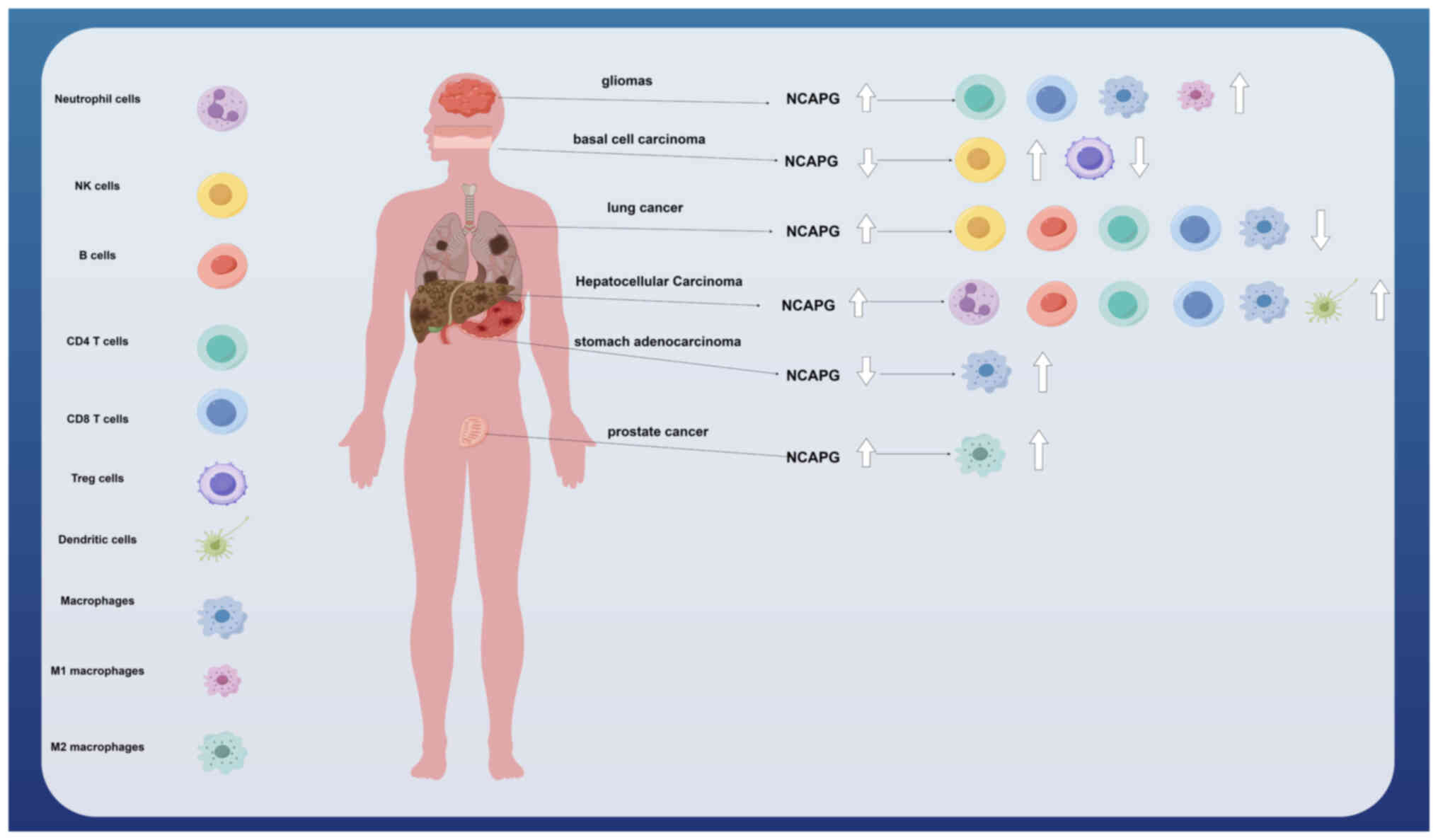
8
|
Sun H, Zhang H, Yan Y, Li Y, Che G, Zhou
C, Nicot C and Ma H: Correction: NCAPG promotes the oncogenesis and
progression of non-small cell lung cancer cells through
upregulating LGALS1 expression. Mol Cancer. 21:2212022. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Yuan Y, Jiang X, Tang L, Wang J, Zhang D,
Cho WC and Duan L: FOXM1/lncRNA TYMSOS/miR-214-3p-mediated high
expression of NCAPG correlates with poor prognosis and cell
proliferation in non-small cell lung carcinoma. Front Mol Biosci.
8:7857672022. View Article : Google Scholar
|
|
10
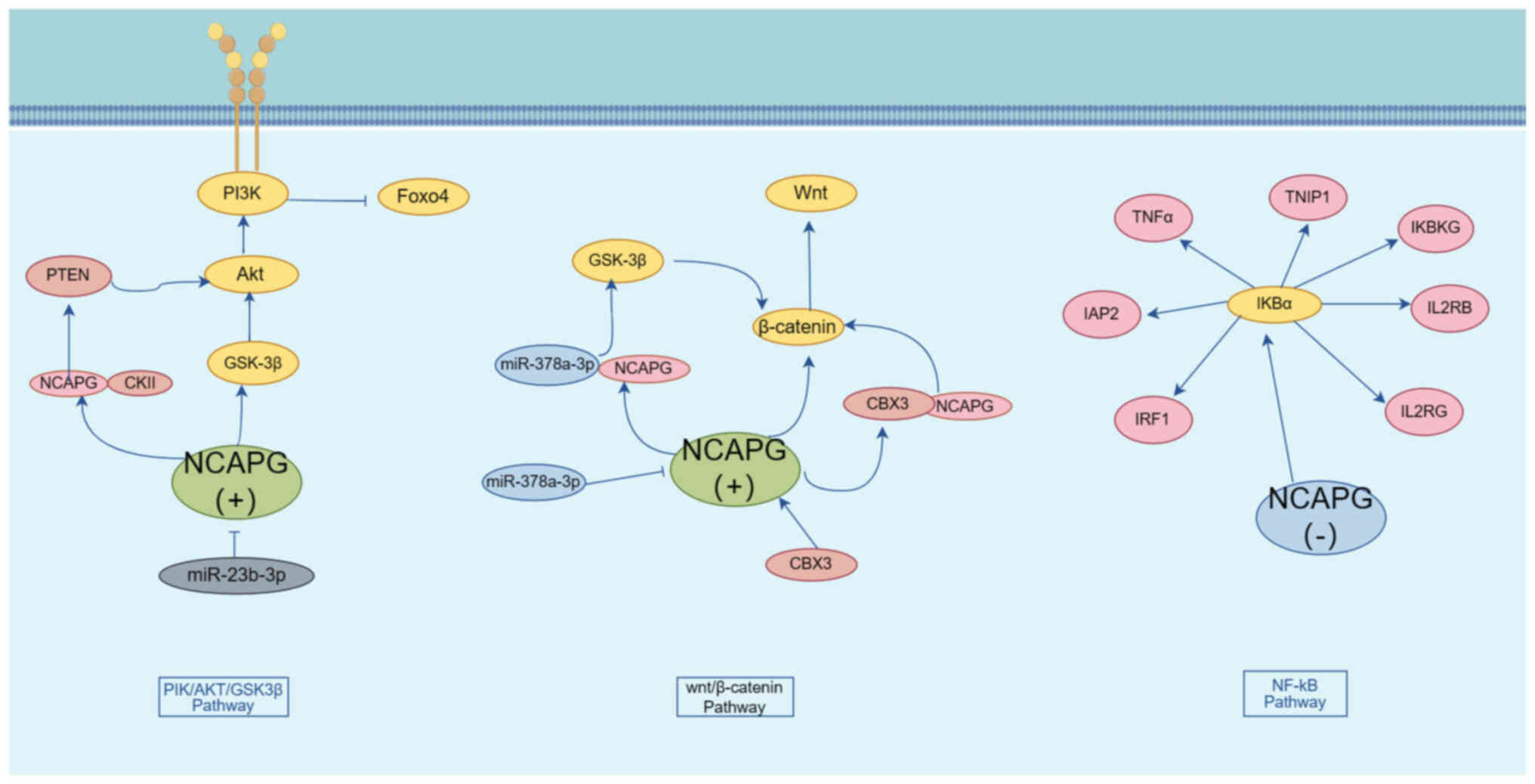
|
Fu Q, Yang F, Zhao J, Yang X, Xiang T,
Huai G, Zhang J, Wei L, Deng S and Yang H: Bioinformatical
identification of key pathways and genes in human hepatocellular
carcinoma after CSN5 depletion. Cell Signal. 49:79–86. 2018.
View Article : Google Scholar
|
|
11
|
Liu W, Liang B, Liu H, Huang Y, Yin X,
Zhou F, Yu X, Feng Q, Li E, Zou Z and Wu L: Overexpression of
non-SMC condensin I complex subunit G serves as a promising
prognostic marker and therapeutic target for hepatocellular
carcinoma. Int J Mol Med. 40:731–738. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Shi Y, Ge C, Fang D, Wei W, Li L, Wei Q
and Yu H: NCAPG facilitates colorectal cancer cell proliferation,
migration, invasion and epithelial-mesenchymal transition by
activating the Wnt/β-catenin signaling pathway. Cancer Cell Int.
22:1192022. View Article : Google Scholar
|
|
13
|
Wu C, Huang ZH, Meng ZQ, Fan XT, Lu S, Tan
YY, You LM, Huang JQ, Stalin A, Ye PZ, et al: A network
pharmacology approach to reveal the pharmacological targets and
biological mechanism of compound kushen injection for treating
pancreatic cancer based on WGCNA and in vitro experiment
validation. Chin Med. 16:1212021. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Zhang D, Cui F, Peng L, Wang M, Yang X,
Xia C, Li K, Yin H, Zhang Y, Yu Q, et al: Establishing and
validating an ADCP-related prognostic signature in pancreatic
ductal adenocarcinoma. Aging (Albany NY). 14:6299–6315. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Hitti E, Bakheet T, Al-Souhibani N,
Moghrabi W, Al-Yahya S, Al-Ghamdi M, Al-Saif M, Shoukri MM, Lánczky
A, Grépin R, et al: Systematic analysis of AU-rich element
expression in cancer reveals common functional clusters regulated
by key RNA-binding proteins. Cancer Res. 76:4068–4080. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Xu T, Dong M, Wang Z, Li H and Li X:
Elevated mRNA expression levels of NCAPG are associated with poor
prognosis in ovarian cancer. Cancer Manag Res. 12:5773–5786. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Zhang W, Gao L, Wang C, Wang S, Sun D, Li
X, Liu M, Qi Y, Liu J and Lin B: Combining bioinformatics and
experiments to identify and verify key genes with prognostic values
in endometrial carcinoma. J Cancer. 11:716–732. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Wang M, Cui Y, Cai Y, Jiang Y and Peng Y:
Comprehensive bioinformatics analysis of mRNA expression profiles
and identification of a miRNA-mRNA network associated with the
pathogenesis of low-grade gliomas. Cancer Manag Res. 13:5135–5147.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Lu S, Sun C, Chen H, Zhang C, Li W, Wu L,
Zhu J, Sun F, Huang J, Wang J, et al: Bioinformatics analysis and
validation identify CDK1 and MAD2L1 as prognostic markers of
rhabdomyosarcoma. Cancer Manag Res. 12:12123–12136. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ryu B, Kim DS, Deluca AM and Alani RM:
Comprehensive expression profiling of tumor cell lines identifies
molecular signatures of melanoma progression. PLoS One. 2:e5942007.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Xie D, Chen X, Wu H, Ning D, Cao X and Wan
C: Prediction of diagnostic gene biomarkers associated with immune
infiltration for basal cell carcinoma. Clin Cosmet Investig
Dermatol. 15:2657–2673. 2022. View Article : Google Scholar
|
|
22
|
Cohen Y, Gutwein O, Garach-Jehoshua O,
Bar-Haim A and Kornberg A: The proliferation arrest of primary
tumor cells out-of-niche is associated with widespread
downregulation of mitotic and transcriptional genes. Hematology.
19:286–292. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Wu Y, Lin Y, Pan J, Tu X, Xu Y, Li H and
Chen Y: NCAPG promotes the progression of lung adenocarcinoma via
the TGF-β signaling pathway. Cancer Cell Int. 21:4432021.
View Article : Google Scholar
|
|
24
|
Guo ZY and Zhu ZT: NCAPG is a prognostic
biomarker associated with vascular invasion in hepatocellular
carcinoma. Eur Rev Med Pharmacol Sci. 25:7238–7251. 2021.
|
|
25
|
Sun DP, Wu CC, Chou CL, Cheng LC, Wang WC,
Lin SS, Hung ST, Tian YF, Fang CL and Lin KY: NCAPG deregulation
indicates poor patient survival and contributes to colorectal
carcinogenesis. Pathol Res Pract. 241:1542382023. View Article : Google Scholar
|
|
26
|
Hou J, Huang P, Xu M, Wang H, Shao Y, Weng
X, Liu Y, Chang H, Zhang L and Cui H: NCAPG promotes the
progression of glioblastoma by facilitating PARP1-mediated E2F1
transactivation. Neuro Oncol. 25:2023. View Article : Google Scholar
|
|
27
|
Zhang X, Wang H, Han Y, Zhu M, Song Z,
Zhan D and Jia J: NCAPG induces cell proliferation in cardia
adenocarcinoma via PI3K/AKT signaling pathway. Onco Targets Ther.
13:11315–11326. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Guo M, Li X, Li J and Li B: Identification
of the prognostic biomarkers and their correlations with immune
infiltration in colorectal cancer through bioinformatics analysis
and in vitro experiments. Heliyon. 9:e171012023. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Farzaneh M, Ghasemian M, Ghaedrahmati F,
Poodineh J, Najafi S, Masoodi T, Kurniawan D, Uddin S and
Azizidoost S: Functional roles of lncRNA-TUG1 in hepatocellular
carcinoma. Life Sci. 308:1209742022. View Article : Google Scholar
|
|
30
|
Li L, Liu S, Peng L, Zhang Y, Zhang Y,
Zeng H, Li G and Zhang C: The identification and preliminary study
of lncRNA TUG1 and its related genes in hepatocellular carcinoma.
Arch Med Sci. 18:1582–1595. 2019.
|
|
31
|
Liu K, Li Y, Yu B, Wang F, Mi T and Zhao
Y: Silencing non-SMC chromosome-associated polypeptide G inhibits
proliferation and induces apoptosis in hepatocellular carcinoma
cells. Can J Physiol Pharmacol. 96:1246–1254. 2018. View Article : Google Scholar
|
|
32
|
Wang Y, Gao B, Tan PY, Handoko YA, Sekar
K, Deivasigamani A, Seshachalam VP, OuYang HY, Shi M, Xie C, et al:
Genome-wide CRISPR knockout screens identify NCAPG as an essential
oncogene for hepatocellular carcinoma tumor growth. FASEB J.
33:8759–8770. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Ai J, Gong C, Wu J, Gao J, Liu W, Liao W
and Wu L: MicroRNA-181c suppresses growth and metastasis of
hepatocellular carcinoma by modulating NCAPG. Cancer Manag Res.
11:3455–3467. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Li Y, Shi H, Zhao Z and Xu M:
Identification of castration-dependent and -independent driver
genes and pathways in castration-resistant prostate cancer (CRPC).
BMC Urol. 22:1622022. View Article : Google Scholar
|
|
35
|
Goto Y, Kurozumi A, Arai T, Nohata N,
Kojima S, Okato A, Kato M, Yamazaki K, Ishida Y, Naya Y, et al:
Impact of novel miR-145-3p regulatory networks on survival in
patients with castration-resistant prostate cancer. Br J Cancer.
117:409–420. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Arai T, Okato A, Yamada Y, Sugawara S,
Kurozumi A, Kojima S, Yamazaki K, Naya Y, Ichikawa T and Seki N:
Regulation of NCAPG by miR-99a-3p (passenger strand) inhibits
cancer cell aggressiveness and is involved in CRPC. Cancer Med.
7:1988–2002. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Yu H, Zou D, Ni N, Zhang S, Zhang Q and
Yang L: Overexpression of NCAPG in ovarian cancer is associated
with ovarian cancer proliferation and apoptosis via p38 MAPK
signaling pathway. J Ovarian Res. 15:982022. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Song B, Du J, Song DF, Ren JC and Feng Y:
Dysregulation of NCAPG, KNL1, miR-148a-3p, miR-193b-3p, and
miR-1179 may contribute to the progression of gastric cancer. Biol
Res. 51:442018. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Sun DP, Lin CC, Hung ST, Kuang YY, Hseu
YC, Fang CL and Lin KY: Aberrant expression of NCAPG is associated
with prognosis and progression of gastric cancer. Cancer Manag Res.
12:7837–7846. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Wolf MM, Kimryn Rathmell W and Beckermann
KE: Modeling clear cell renal cell carcinoma and therapeutic
implications. Oncogene. 39:3413–3426. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Liu B, Xiao Y, Li H, Zhang AL, Meng LB,
Feng L, Zhao ZH, Ni XC, Fan B, Zhang XY, et al: Identification and
verification of biomarker in clear cell renal cell carcinoma via
bioinformatics and neural network model. Biomed Res Int.
2020:69547932020.
|
|
42
|
Li H, Zheng P, Li Z, Han Q, Zhou B, Wang X
and Wang K: NCAPG promotes the proliferation of renal clear cell
carcinoma via mediating with CDK1. Dis Markers.
2022:67585952022.PubMed/NCBI
|
|
43
|
Li S, Xuan Y, Gao B, Sun X, Miao S, Lu T,
Wang Y and Jiao W: Identification of an eight-gene prognostic
signature for lung adenocarcinoma. Cancer Manag Res. 10:3383–3392.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Wang X, Tian X, Sui X, Li X, Zhao X, Han
K, Sun L and Dong Y: Increased expression of NCAPG (Non-SMC
condensing I complex subunit G) is associated with progression and
poor prognosis of lung adenocarcinoma. Bioengineered. 13:6113–6125.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Chen J, Yang HM, Zhou HC, Peng RR, Niu ZX
and Kang CY: PRR11 and SKA2 promote the proliferation, migration
and invasion of esophageal carcinoma cells. Oncol Lett. 20:639–646.
2020. View Article : Google Scholar
|
|
46
|
Sun Y, Xu D, Zhang C, Wang Y, Zhang L,
Qiao D, Bu Y and Zhang Y: HEDGEHOG/GLI modulates the PRR11-SKA2
bidirectional transcription unit in lung squamous cell carcinomas.
Genes (Basel). 12:1202021. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Moura-Castro LH, Peña-Martínez P, Castor
A, Galeev R, Larsson J, Järås M, Yang M and Paulsson K: Sister
chromatid cohesion defects are associated with chromosomal copy
number heterogeneity in high hyperdiploid childhood acute
lymphoblastic leukemia. Genes Chromosomes Cancer. 60:410–417. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Yu J, Vodyanik MA, Smuga-Otto K,
Antosiewicz-Bourget J, Frane JL, Tian S, Nie J, Jonsdottir GA,
Ruotti V, Stewart R, et al: Induced pluripotent stem cell lines
derived from human somatic cells. Science. 318:1917–1920. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
49
|
González F, Boué S and Izpisúa Belmonte
JC: Methods for making induced pluripotent stem cells:
Reprogramming à la carte. Nat Rev Genet. 12:231–242. 2011.
View Article : Google Scholar
|
|
50
|
van Es JH, Sato T, van de Wetering M,
Lyubimova A, Yee Nee AN, Gregorieff A, Sasaki N, Zeinstra L, van
den Born M, Korving J, et al: Dll1+ secretory progenitor cells
revert to stem cells upon crypt damage. Nat Cell Biol.
14:1099–1104. 2012. View Article : Google Scholar
|
|
51
|
Chaffer CL, Brueckmann I, Scheel C,
Kaestli AJ, Wiggins PA, Rodrigues LO, Brooks M, Reinhardt F, Su Y,
Polyak K, et al: Normal and neoplastic nonstem cells can
spontaneously convert to a stem-like state. Proc Natl Acad Sci USA.
108:7950–7955. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Yang L, Shi P, Zhao G, Xu J, Peng W, Zhang
J, Zhang G, Wang X, Dong Z, Chen F and Cui H: Targeting cancer stem
cell pathways for cancer therapy. Signal Transduct Target Ther.
5:82020. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Huang T, Song X, Xu D, Tiek D, Goenka A,
Wu B, Sastry N, Hu B and Cheng SY: Stem cell programs in cancer
initiation, progression, and therapy resistance. Theranostics.
10:8721–8743. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Pan S, Zhan Y, Chen X, Wu B and Liu B:
Identification of biomarkers for controlling cancer stem cell
characteristics in bladder cancer by network analysis of
transcriptome data stemness indices. Front Oncol. 9:6132019.
View Article : Google Scholar
|
|
55
|
Li J, Zhou M, Huang D, Lin R, Cui X, Chen
S, Yao Y, Xian S, Wang S, Fu Q, et al: The recurrent-specific
regulation network of prognostic stemness-related signatures in
low-grade glioma. Dis Markers. 2023:22439282023. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Li H, Jiang Y, Hu J, Xu J, Chen L, Zhang
G, Zhao J, Zong S, Guo Z, Li X, et al: The U2AF65/circNCAPG/RREB1
feedback loop promotes malignant phenotypes of glioma stem cells
through activating the TGF-β pathway. Cell Death Dis. 14:232023.
View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Xiang Z, Cha G, Wang Y, Gao J and Jia J:
Characterizing the crosstalk of NCAPG with tumor microenvironment
and tumor stemness in stomach adenocarcinoma. Stem Cells Int.
2022:18883582022. View Article : Google Scholar
|
|
58
|
Xia X and Li Y: Comprehensive analysis of
transcriptome data stemness indices identifies key genes for
controlling cancer stem cell characteristics in gastric cancer.
Transl Cancer Res. 9:6050–6061. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Guo SH, Ma L and Chen J: Identification of
prognostic markers and potential therapeutic targets in gastric
adenocarcinoma by machine learning based on mRNAsi index. J Oncol.
2022:89261272022. View Article : Google Scholar
|
|
60
|
Zhang Z, Qi D, Liu X and Kang P: NCAPG
stimulates lung adenocarcinoma cell stemness through aerobic
glycolysis. Clin Respir J. 17:884–892. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Xiao Y and Yu D: Tumor microenvironment as
a therapeutic target in cancer. Pharmacol Ther. 221:1077532021.
View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Hinshaw DC and Shevde LA: The tumor
microenvironment innately modulates cancer progression. Cancer Res.
79:4557–4566. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Jin MZ and Jin WL: The updated landscape
of tumor microenvironment and drug repurposing. Signal Transduct
Target Ther. 5:1662020. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Wu T and Dai Y: Tumor microenvironment and
therapeutic response. Cancer Lett. 387:61–68. 2017. View Article : Google Scholar
|
|
65
|
Xu N, Dong RN, Lin TT, Lin T, Lin YZ, Chen
SH, Zhu JM, Ke ZB, Huang F, Chen YH and Xue XY: Development and
validation of novel biomarkers related to M2 macrophages
infiltration by weighted gene co-expression network analysis in
prostate cancer. Front Oncol. 11:6340752021. View Article : Google Scholar
|
|
66
|
Aleshin A and Finn RS: SRC: A century of
science brought to the clinic. Neoplasia. 12:599–607. 2010.
View Article : Google Scholar
|
|
67
|
Roskoski R Jr: Src protein-tyrosine kinase
structure and regulation. Biochem Biophys Res Commun.
324:1155–1164. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Jiang L, Ren L, Chen H, Pan J, Zhang Z,
Kuang X, Chen X, Bao W, Lin C, Zhou Z, et al: NCAPG confers
trastuzumab resistance via activating SRC/STAT3 signaling pathway
in HER2-positive breast cancer. Cell Death Dis. 11:5472020.
View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Singh D, Assaraf YG and Gacche RN: Long
non-coding RNA mediated drug resistance in breast cancer. Drug
Resist Updat. 63:1008512022. View Article : Google Scholar
|
|
70
|
Wei L, Sun J, Zhang N, Zheng Y, Wang X, Lv
L, Liu J, Xu Y, Shen Y and Yang M: Noncoding RNAs in gastric
cancer: Implications for drug resistance. Mol Cancer. 19:622020.
View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Entezari M, Ghanbarirad M, Taheriazam A,
Sadrkhanloo M, Zabolian A, Goharrizi MASB, Hushmandi K, Aref AR,
Ashrafizadeh M, Zarrabi A, et al: Long non-coding RNAs and exosomal
lncRNAs: Potential functions in lung cancer progression, drug
resistance and tumor microenvironment remodeling. Biomed
Pharmacother. 150:1129632022. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Bao J, Wu Y, Zhang K and Qi H:
AC099850.3/NCAPG axis predicts poor prognosis and is associated
with resistance to EGFR tyrosine-kinase inhibitors in lung
Adenocarcinoma. Int J Gen Med. 15:6917–6930. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Cunningham F, Allen JE, Allen J,
Alvarez-Jarreta J, Amode MR, Armean IM, Austine-Orimoloye O, Azov
AG, Barnes I, Bennett R, et al: Ensembl 2022. Nucleic Acids Res.
50(D1): D988–D995. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
He Y, Sun MM, Zhang GG, Yang J, Chen KS,
Xu WW and Li B: Targeting PI3K/Akt signal transduction for cancer
therapy. Signal Transduct Target Ther. 6:4252021. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Gong C, Ai J, Fan Y, Gao J, Liu W, Feng Q,
Liao W and Wu L: NCAPG promotes the proliferation of hepatocellular
carcinoma through PI3K/AKT signaling. Onco Targets Ther.
12:8537–8552. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Grossi I, Salvi A, Baiocchi G, Portolani N
and De Petro G: Functional role of microRNA-23b-3p in cancer
biology. Microrna. 7:156–166. 2018. View Article : Google Scholar
|
|
77
|
Kou CH, Zhou T, Han XL, Zhuang HJ and Qian
HX: Downregulation of mir-23b in plasma is associated with poor
prognosis in patients with colorectal cancer. Oncol Lett.
12:4838–4844. 2016. View Article : Google Scholar
|
|
78
|
Li P, Wen J, Ren X, Zhou Y, Xue Y, Yan Z,
Li S, Tian H, Tang XG and Zhang GJ: MicroRNA-23b-3p targets non-SMC
condensing I complex subunit G to promote proliferation and inhibit
apoptosis of colorectal cancer cells via regulation of the PI3K/AKT
signaling pathway. Oncol Lett. 22:8122021. View Article : Google Scholar
|
|
79
|
Worby CA and Dixon JE: PTEN. Annu Rev
Biochem. 83:641–669. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Álvarez-Garcia V, Tawil Y, Wise HM and
Leslie NR: Mechanisms of PTEN loss in cancer: It's all about
diversity. Semin Cancer Biol. 59:66–79. 2019. View Article : Google Scholar
|
|
81
|
Oh NS, Yoon SH, Lee WK, Choi JY, Min do S
and Bae YS: Phosphorylation of CKBBP2/CRIF1 by protein kinase CKII
promotes cell proliferation. Gene. 386:147–153. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Zhang R, Ai J, Wang J, Sun C, Lu H, He A,
Li M, Liao Y, Lei J, Zhou F, et al: NCAPG promotes the
proliferation of hepatocellular carcinoma through the
CKII-dependent regulation of PTEN. J Transl Med. 20:3252022.
View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Zhou Y, Xu J, Luo H, Meng X, Chen M and
Zhu D: Wnt signaling pathway in cancer immunotherapy. Cancer Lett.
525:84–96. 2022. View Article : Google Scholar
|
|
84
|
Rim EY, Clevers H and Nusse R: The Wnt
pathway: From signaling mechanisms to synthetic modulators. Annu
Rev Biochem. 91:571–598. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Liu C, Yan Y, Di F, Li W, Yin X and Dong
L: Inhibition of NCAPG expression inactivates the Wnt/β-catenin
signal to suppresses endometrial cancer cell growth in vitro.
Environ Toxicol. 36:2512–2520. 2021. View Article : Google Scholar
|
|
86
|
Zhang X, Zhu M, Wang H, Song Z, Zhan D,
Cao W, Han Y and Jia J: Overexpression of NCAPG inhibits cardia
adenocarcinoma apoptosis and promotes epithelial-mesenchymal
transition through the Wnt/β-catenin signaling pathway. Gene.
766:1451632021. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Yang H, Pu L, Li R and Zhu R: NCAPG is
transcriptionally regulated by CBX3 and activates the Wnt/β-catenin
signaling pathway to promote proliferation and the cell cycle and
inhibit apoptosis in colorectal cancer. J Gastrointest Oncol.
14:900–912. 2023. View Article : Google Scholar
|
|
88
|
Li J, Sun S, Li J, Zhao X, Li Z, Sha T and
Cui Z: NCAPG, mediated by miR-378a-3p, regulates cell
proliferation, cell cycle progression, and apoptosis of oral
squamous cell carcinoma through the GSK-3β/β-catenin signaling.
Neoplasma. 68:1201–1211. 2021. View Article : Google Scholar
|
|
89
|
Du W and Searle JS: The rb pathway and
cancer therapeutics. Curr Drug Targets. 10:581–589. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Lin SC, Skapek SX and Lee EY: Genes in the
RB pathway and their knockout in mice. Semin Cancer Biol.
7:279–289. 1996. View Article : Google Scholar
|
|
91
|
Nevins JR: The Rb/E2F pathway and cancer.
Hum Mol Genet. 10:699–703. 2001. View Article : Google Scholar
|
|
92
|
Schaal C, Pillai S and Chellappan SP: The
Rb-E2F transcriptional regulatory pathway in tumor angiogenesis and
metastasis. Adv Cancer Res. 121:147–182. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Liu J, Zhang C, Wang J, Hu W and Feng Z:
The regulation of ferroptosis by tumor suppressor p53 and its
pathway. Int J Mol Sci. 21:83872020. View Article : Google Scholar
|
|
94
|
Huang J: Current developments of targeting
the p53 signaling pathway for cancer treatment. Pharmacol Ther.
220:1077202021. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Dong M, Xu T, Cui X, Li H, Li X and Xia W:
NCAPG upregulation mediated by four microRNAs combined with
activation of the p53 signaling pathway is a predictor of poor
prognosis in patients with breast cancer. Oncol Lett. 21:3232021.
View Article : Google Scholar
|
|
96
|
DiDonato JA, Mercurio F and Karin M: NF-κB
and the link between inflammation and cancer. Immunol Rev.
246:379–400. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Oeckinghaus A, Hayden M S and Ghosh S:
Crosstalk in NF-κB signaling pathways. Nat Immunol. 12:695–708.
2011. View Article : Google Scholar
|
|
98
|
Swindell WR, Bojanowski K and Chaudhuri
RK: A novel fumarate, isosorbide di-(methyl fumarate) (IDMF),
replicates astrocyte transcriptome responses to dimethyl fumarate
(DMF) but specifically down-regulates genes linked to a reactive
phenotype. Biochem Biophys Res Commun. 532:475–481. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Tang F, Yu H, Wang X, Shi J, Chen Z, Wang
H, Wan Z, Fu Q, Hu X, Zuhaer Y, et al: NCAPG promotes tumorigenesis
of bladder cancer through NF-κB signaling pathway. Biochem Biophys
Res Commun. 622:101–107. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Yu H, Lee H, Herrmann A, Buettner R and
Jove R: Revisiting STAT3 signalling in cancer: New and unexpected
biological functions. Nat Rev Cancer. 14:736–746. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Zou S, Tong Q, Liu B, Huang W, Tian Y and
Fu X: Targeting STAT3 in cancer immunotherapy. Mol Cancer.
19:1452020. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Li J, Zheng J, Lin B, Sun H, Lu S, Wang D
and Huo H: Knockdown of NCAPG promotes the apoptosis and inhibits
the invasion and migration of triple-negative breast cancer
MDA-MB-231 cells via regulation of EGFR/JAK/STAT3 signaling. Exp
Ther Med. 25:1192023. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Peng D, Fu M, Wang M, Wei Y and Wei X:
Targeting TGF-β signal transduction for fibrosis and cancer
therapy. Mol Cancer. 21:1042022. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Derynck R, Turley SJ and Akhurst RJ: TGFβ
biology in cancer progression and immunotherapy. Nat Rev Clin
Oncol. 18:9–34. 2021. View Article : Google Scholar
|