|
1
|
Torres CR and Hart GW: Topography and
polypeptide distribution of terminal N-acetylglucosamine residues
on the surfaces of intact lymphocytes. Evidence for O-linked
GlcNAc. J Biol Chem. 259:3308–3317. 1984. View Article : Google Scholar : PubMed/NCBI
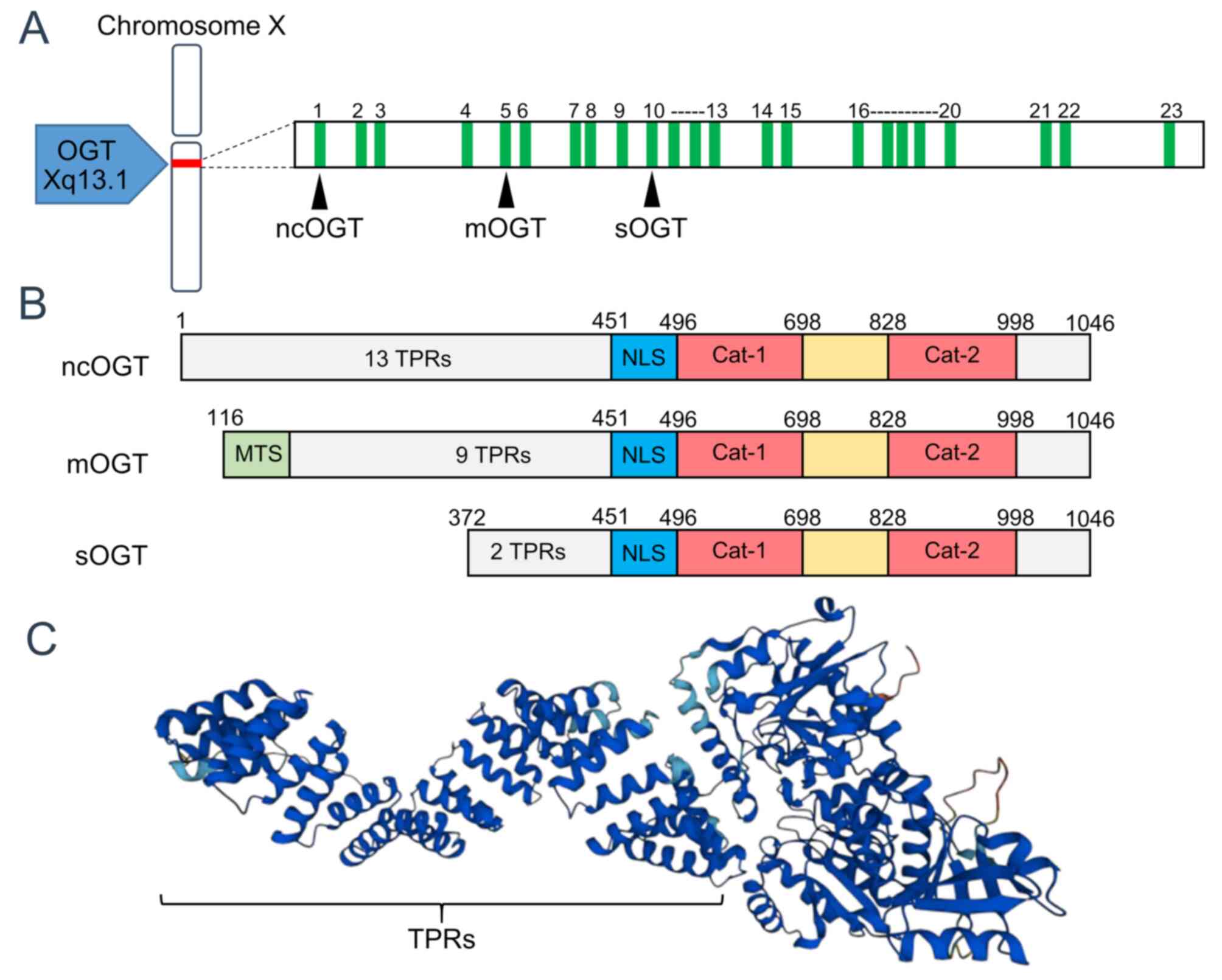
|
|
2
|
Haltiwanger RS, Blomberg MA and Hart GW:
Glycosylation of nuclear and cytoplasmic proteins. Purification and
characterization of a uridine diphospho-N-acetylglucosamine:
Polypeptide beta-N-acetylglucosaminyltransferase. J Biol Chem.
267:9005–9013. 1992. View Article : Google Scholar : PubMed/NCBI
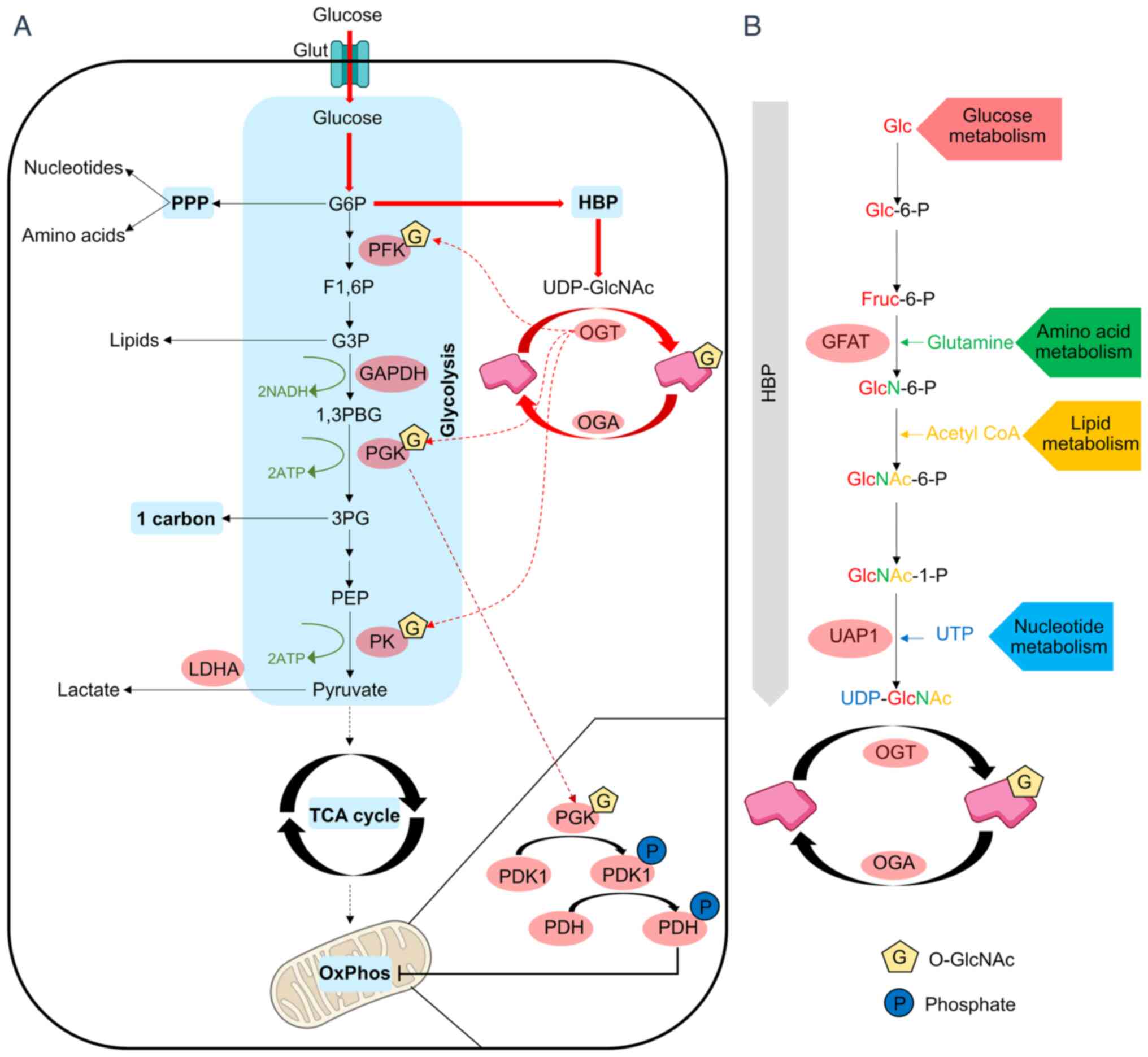
|
|
3
|
Kreppel LK, Blomberg MA and Hart GW:
Dynamic glycosylation of nuclear and cytosolic proteins. Cloning
and characterization of a unique O-GlcNAc transferase with multiple
tetratricopeptide repeats. J Biol Chem. 272:9308–9315. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Starr CM and Hanover JA: Glycosylation of
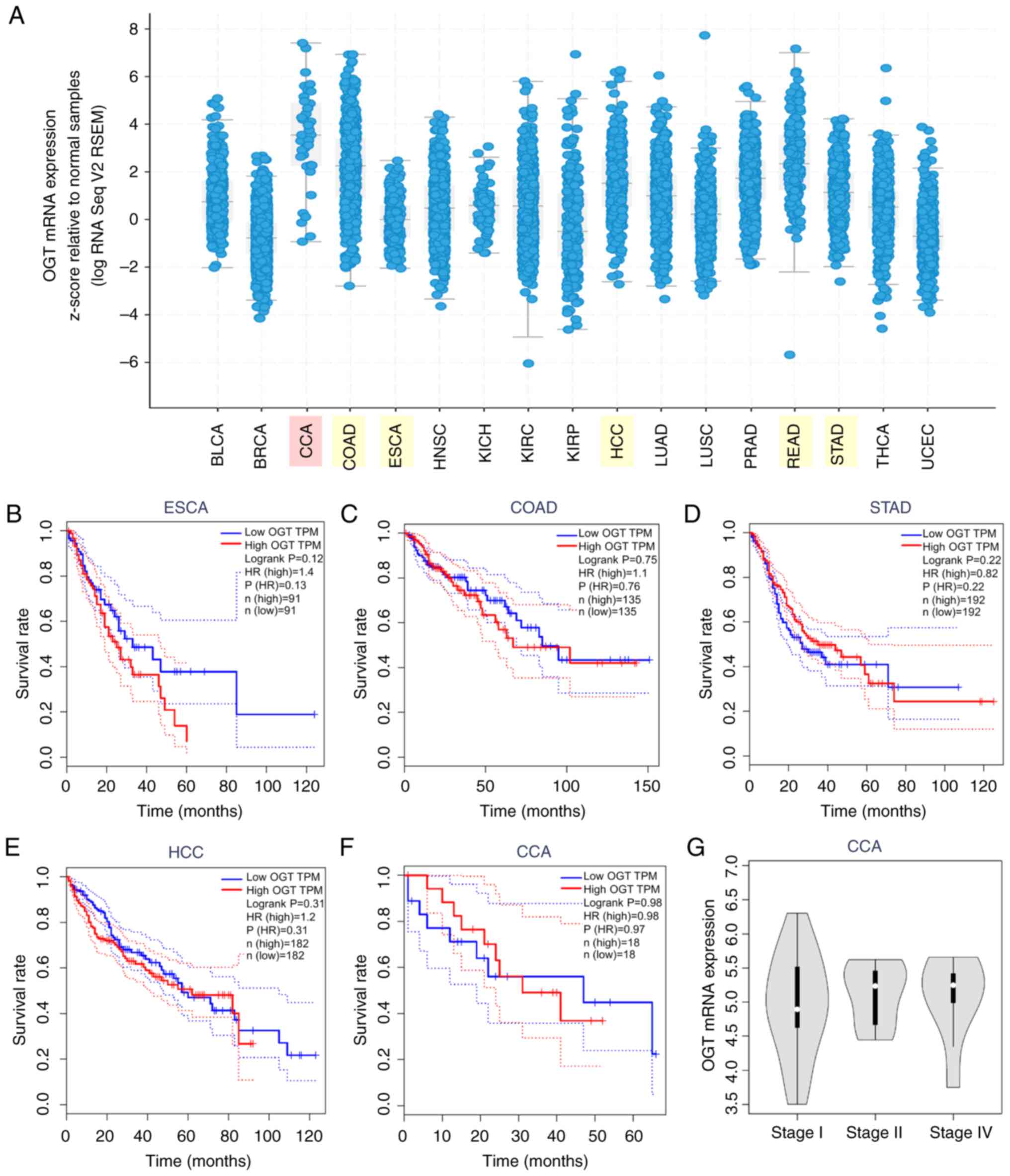
nuclear pore protein p62. Reticulocyte lysate catalyzes O-linked
N-acetylglucosamine addition in vitro. J Biol Chem. 265:6868–6873.
1990. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Gao Y, Wells L, Comer FI, Parker GJ and
Hart GW: Dynamic O-glycosylation of nuclear and cytosolic proteins:
Cloning and characterization of a neutral, cytosolic
beta-N-acetylglucosaminidase from human brain. J Biol Chem.
276:9838–9845. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
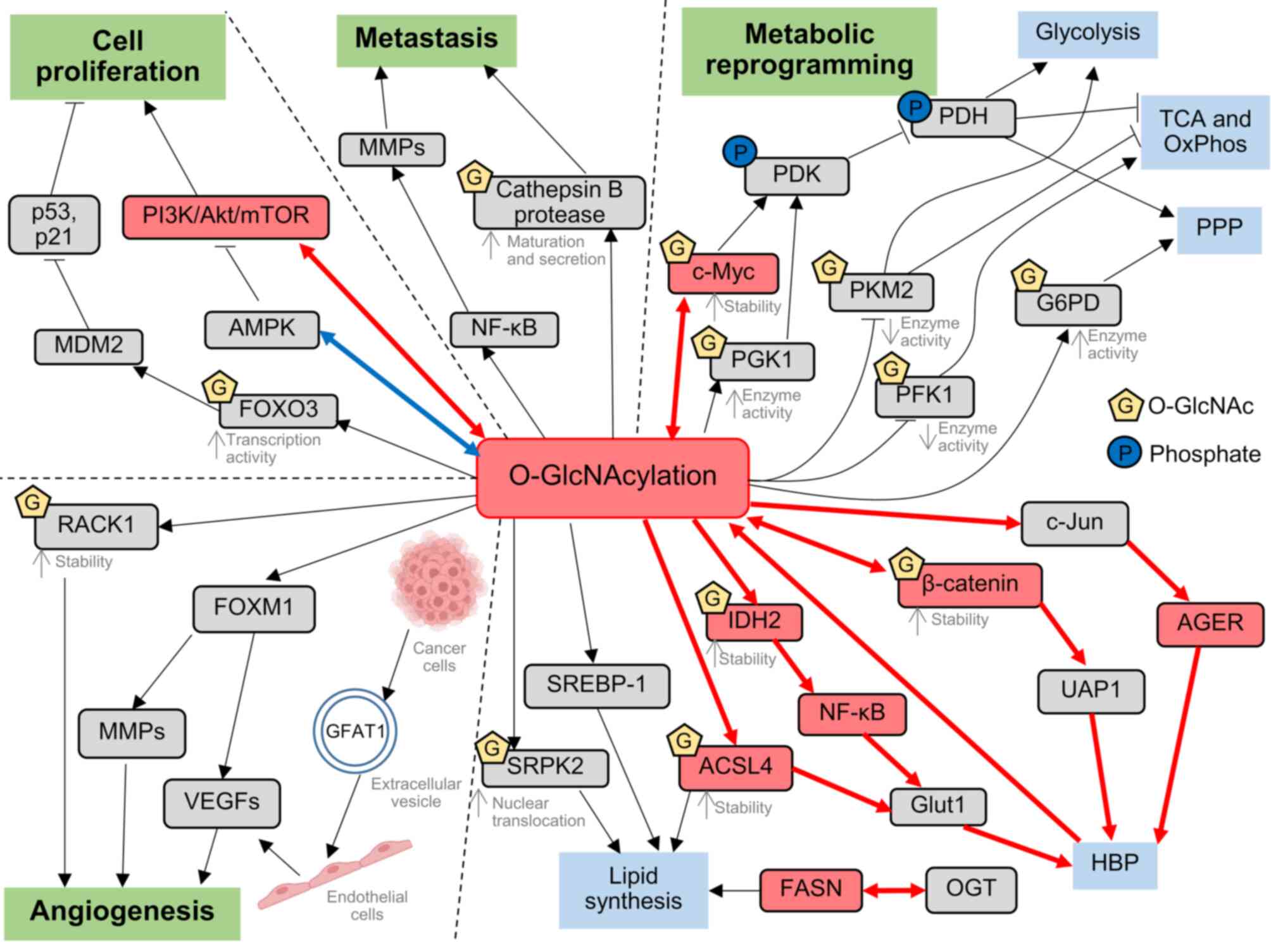
6
|
Dong DL and Hart GW: Purification and
characterization of an O-GlcNAc selective
N-acetyl-beta-D-glucosaminidase from rat spleen cytosol. J Biol
Chem. 269:19321–19330. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Nolte D and Müller U: Human O-GlcNAc
transferase (OGT): Genomic structure, analysis of splice variants,
fine mapping in Xq13.1. Mamm Genome. 13:62–64. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Hanover JA, Yu S, Lubas WB, Shin SH,
Ragano-Caracciola M, Kochran J and Love DC: Mitochondrial and
nucleocytoplasmic isoforms of O-linked GlcNAc transferase encoded
by a single mammalian gene. Arch Biochem Biophys. 409:287–297.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lu Q, Zhang X, Liang T and Bai X:
O-GlcNAcylation: An important post-translational modification and a
potential therapeutic target for cancer therapy. Mol Med.
28:1152022. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Love DC, Kochan J, Cathey RL, Shin SH and
Hanover JA: Mitochondrial and nucleocytoplasmic targeting of
O-linked GlcNAc transferase. J Cell Sci. 116:647–654. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Lubas WA, Frank DW, Krause M and Hanover
JA: O-Linked GlcNAc transferase is a conserved nucleocytoplasmic
protein containing tetratricopeptide repeats. J Biol Chem.
272:9316–9324. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Stephen HM, Adams TM and Wells L:
Regulating the regulators: mechanisms of substrate selection of the
O-GlcNAc cycling enzymes OGT and OGA. Glycobiology. 31:724–733.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Boyd SS, Robarts DR, Nguyen K, Villar M,
Alghusen IM, Kotulkar M, Denson A, Fedosyuk H, Whelan SA, Lee NCY,
et al: Multi-omics after O-GlcNAc alteration identified cellular
processes promoting aneuploidy after loss of O-GlcNAc transferase.
Mol Metab. 90:1020602024. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Levine ZG, Potter SC, Joiner CM, Fei GQ,
Nabet B, Sonnett M, Zachara NE, Gray NS, Paulo JA and Walker S:
Mammalian cell proliferation requires noncatalytic functions of
O-GlcNAc transferase. Proc Natl Acad Sci USA. 118:e20167781182021.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Tang J, Long G, Li X, Zhou L, Zhou Y and
Wu Z: The deubiquitinase EIF3H promotes hepatocellular carcinoma
progression by stabilizing OGT and inhibiting ferroptosis. Cell
Commun Signal. 21:1982023. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Marshall S, Bacote V and Traxinger RR:
Discovery of a metabolic pathway mediating glucose-induced
desensitization of the glucose transport system. Role of hexosamine
biosynthesis in the induction of insulin resistance. J Biol Chem.
266:4706–4712. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Hanover JA, Krause MW and Love DC: The
hexosamine signaling pathway: O-GlcNAc cycling in feast or famine.
Biochim Biophys Acta. 1800:80–95. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Lam C, Low JY, Tran PT and Wang H: The
hexosamine biosynthetic pathway and cancer: Current knowledge and
future therapeutic strategies. Cancer Lett. 503:11–18. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Morales MM and Pratt MR: The
post-translational modification O-GlcNAc is a sensor and regulator
of metabolism. Open Biol. 14:2402092024. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Banales JM, Marin JJG, Lamarca A,
Rodrigues PM, Khan SA, Roberts LR, Cardinale V, Carpino G, Andersen
JB, Braconi C, et al: Cholangiocarcinoma 2020: The next horizon in
mechanisms and management. Nat Rev Gastroenterol Hepatol.
17:557–588. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Bertuccio P, Malvezzi M, Carioli G, Hashim
D, Boffetta P, El-Serag HB, La Vecchia C and Negri E: Global trends
in mortality from intrahepatic and extrahepatic cholangiocarcinoma.
J Hepatol. 71:104–114. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Qurashi M, Vithayathil M and Khan SA:
Epidemiology of cholangiocarcinoma. Eur J Surg Oncol.
51:1070642025. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Razumilava N and Gores GJ:
Cholangiocarcinoma. Lancet. 383:2168–2179. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Benson AB, D'Angelica MI, Abrams T, Abbott
DE, Ahmed A, Anaya DA, Anders R, Are C, Bachini M, Binder D, et al:
NCCN guidelines® insights: Biliary tract cancers,
version 2.2023. J Natl Compr Cancer Netw. 21:694–704. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Vogel A, Bridgewater J, Edeline J, Kelley
RK, Klümpen HJ, Malka D, Primrose JN, Rimassa L, Stenzinger A,
Valle JW, et al: Biliary tract cancer: ESMO clinical practice
guideline for diagnosis, treatment and follow-up. Ann Oncol.
34:127–140. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Valle JW, Lamarca A, Goyal L, Barriuso J
and Zhu AX: New horizons for precision medicine in biliary tract
cancers. Cancer Discov. 7:943–962. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Tsilimigras DI, Endo Y, Guglielmi A,
Aldrighetti L, Weiss M, Bauer TW, Popescu I, Poultsides GA, Maithel
SK, Marques HP, et al: Recurrent intrahepatic cholangiocarcinoma: A
10-point score to predict post-recurrence survival and guide
treatment of recurrence. Ann Surg Oncol. 31:4427–4435. 2024.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Groot Koerkamp B, Wiggers JK, Allen PJ,
Besselink MG, Blumgart LH, Busch OR, Coelen RJ, D'Angelica MI,
DeMatteo RP, Gouma DJ, et al: Recurrence rate and pattern of
perihilar cholangiocarcinoma after curative intent resection. J Am
Coll Surg. 221:1041–1049. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Komaya K, Ebata T, Shirai K, Ohira S,
Morofuji N, Akutagawa A, Yamaguchi R and Nagino M; Nagoya Surgical
Oncology Group, : Recurrence after resection with curative intent
for distal cholangiocarcinoma. Br J Surg. 104:426–433. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Qiao Z, Dang C, Zhou B, Zhang W, Jiang J,
Zhang J, Kong R and Ma Y: O-linked N-acetylglucosamine transferase
(OGT) is overexpressed and promotes O-linked protein glycosylation
in esophageal squamous cell carcinoma. J Biomed Res. 26:268–273.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Jiang M, Qiu Z, Zhang S, Fan X, Cai X, Xu
B, Li X, Zhou J, Zhang X, Chu Y, et al: Elevated O-GlcNAcylation
promotes gastric cancer cells proliferation by modulating cell
cycle related proteins and ERK 1/2 signaling. Oncotarget.
7:61390–61402. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Jang TJ and Kim UJ: O-GlcNAcylation is
associated with the development and progression of gastric
carcinoma. Pathol Res Pract. 212:622–630. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Sharma NS, Gupta VK, Dauer P, Kesh K,
Hadad R, Giri B, Chandra A, Dudeja V, Slawson C, Banerjee S, et al:
O-GlcNAc modification of Sox2 regulates self-renewal in pancreatic
cancer by promoting its stability. Theranostics. 9:3410–3424. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Santos-Laso A, Perugorria MJ and Banales
JM: O-GlcNAcylation: Undesired tripmate but an opportunity for
treatment in NAFLD-HCC. J Hepatol. 67:218–220. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Xu W, Zhang X, Wu JL, Fu L, Liu K, Liu D,
Chen GG, Lai PB, Wong N and Yu J: O-GlcNAc transferase promotes
fatty liver-associated liver cancer through inducing palmitic acid
and activating endoplasmic reticulum stress. J Hepatol. 67:310–320.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Mi W, Gu Y, Han C, Liu H, Fan Q, Zhang X,
Cong Q and Yu W: O-GlcNAcylation is a novel regulator of lung and
colon cancer malignancy. Biochim Biophys Acta. 1812:514–519. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Phueaouan T, Chaiyawat P, Netsirisawan P,
Chokchai-chamnankit D, Punyarit P, Srisomsap C, Svasti J and
Champattanachai V: Aberrant O-GlcNAc-modified proteins expressed in
primary colorectal cancer. Oncol Rep. 30:2929–2936. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Phoomak C, Silsirivanit A, Wongkham C,
Sripa B, Puapairoj A and Wongkham S: Overexpression of
O-GlcNAc-transferase associates with aggressiveness of mass-forming
cholangiocarcinoma. Asian Pac J Cancer Prev. 13 (Suppl):S101–S105.
2012.PubMed/NCBI
|
|
39
|
Gao J, Aksoy BA, Dogrusoz U, Dresdner G,
Gross B, Sumer SO, Sun Y, Jacobsen A, Sinha R, Larsson E, et al:
Integrative analysis of complex cancer genomics and clinical
profiles using the cBioPortal. Sci Signal. 6:pl12013. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Su Z, Gao A, Li X, Zou S, He C, Wu J, Ding
WQ and Zhou J: DNA polymerase iota promotes esophageal squamous
cell carcinoma proliferation through Erk-OGT-induced G6PD
overactivation. Front Oncol. 11:7063372021. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Xu D, Wang W, Bian T, Yang W, Shao M and
Yang H: Increased expression of O-GlcNAc transferase (OGT) is a
biomarker for poor prognosis and allows tumorigenesis and invasion
in colon cancer. Int J Clin Exp Pathol. 12:1305–1314.
2019.PubMed/NCBI
|
|
42
|
Lei Y, Chen T, Li Y, Shang M, Zhang Y, Jin
Y, Yu Q, Guo F and Wang T: O-GlcNAcylation of PFKFB3 is required
for tumor cell proliferation under hypoxia. Oncogenesis. 9:212020.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Liu Q, Tao T, Liu F, Ni R, Lu C and Shen
A: Hyper-O-GlcNAcylation of YB-1 affects Ser102 phosphorylation and
promotes cell proliferation in hepatocellular carcinoma. Exp Cell
Res. 349:230–238. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Gao S, Miao Y, Liu Y, Liu X, Fan X, Lin Y,
Qian P, Zhou J, Dai Y, Xia L, et al: Reciprocal regulation between
O-GlcNAcylation and β-catenin facilitates cell viability and
inhibits apoptosis in liver cancer. DNA Cell Biol. 38:286–296.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Wang J, Wang Z, Yuan J, Wang J and Shen X:
The positive feedback between ACSL4 expression and O-GlcNAcylation
contributes to the growth and survival of hepatocellular carcinoma.
Aging (Albany NY). 12:7786–7800. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Tang Z, Li C, Kang B, Gao G, Li C and
Zhang Z: GEPIA: A web server for cancer and normal gene expression
profiling and interactive analyses. Nucleic Acids Res. 45((W1)):
W98–W102. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
He X, Li Y, Chen Q, Zheng L, Lou J, Lin C,
Gong J, Zhu Y and Wu Y: O-GlcNAcylation and stablization of SIRT7
promote pancreatic cancer progression by blocking the SIRT7-REGγ
interaction. Cell Death Differ. 29:1970–1981. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Guo H, Zhang B, Nairn AV, Moremen KW,
Buckhaults P and Pierce M: O-linked N-acetylglucosamine (O-GlcNAc)
expression levels epigenetically regulate colon cancer
tumorigenesis by affecting the cancer stem cell compartment via
modulating expression of transcriptional factor MYBL1. J Biol Chem.
292:4123–4137. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Ma Z, Vocadlo DJ and Vosseller K:
Hyper-O-GlcNAcylation is anti-apoptotic and maintains constitutive
NF-κB activity in pancreatic cancer cells. J Biol Chem.
288:15121–15130. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Steenackers A, Olivier-Van Stichelen S,
Baldini SF, Dehennaut V, Toillon RA, Le Bourhis X, El
Yazidi-Belkoura I and Lefebvre T: Silencing the nucleocytoplasmic
O-GlcNAc transferase reduces proliferation, adhesion, and migration
of cancer and fetal human colon cell lines. Front Endocrinol
(Lausanne). 7:462016. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Wang H, Sun J, Sun H, Wang Y, Lin B, Wu L,
Qin W, Zhu Q and Yi W: The OGT-c-Myc-PDK2 axis rewires the TCA
cycle and promotes colorectal tumor growth. Cell Death Differ.
31:1157–1169. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Drury J, Geisen ME, Tessmann JW, Rychahou
PG, Kelson CO, He D, Wang C, Evers BM and Zaytseva YY:
Overexpression of fatty acid synthase upregulates
glutamine-fructose-6-phosphate transaminase 1 and O-linked
N-acetylglucosamine transferase to increase O-GlcNAc protein
glycosylation and promote colorectal cancer growth. Int J Mol Sci.
25:48832024. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Cao B, Duan M, Xing Y, Liu C, Yang F, Li
Y, Yang T, Wei Y, Gao Q and Jiang J: O-GlcNAc transferase activates
stem-like cell potential in hepatocarcinoma through O-GlcNAcylation
of eukaryotic initiation factor 4E. J Cell Mol Med. 23:2384–2398.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Qiao Y, Zhang X, Zhang Y, Wang Y, Xu Y,
Liu X, Sun F and Wang J: High glucose stimulates tumorigenesis in
hepatocellular carcinoma cells through AGER-dependent
O-GlcNAcylation of c-Jun. Diabetes. 65:619–632. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Lee SJ and Kwon OS: O-GlcNAc transferase
inhibitor synergistically enhances doxorubicin-induced apoptosis in
HepG2 Cells. Cancers (Basel). 12:31542020. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
de Queiroz RM, Moon SH and Prives C:
O-GlcNAc transferase regulates p21 protein levels and cell
proliferation through the FoxM1-Skp2 axis in a p53-independent
manner. J Biol Chem. 298:1022892022. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Qiu H, Liu F, Tao T, Zhang D, Liu X, Zhu
G, Xu Z, Ni R and Shen A: Modification of p27 with O-linked
N-acetylglucosamine regulates cell proliferation in hepatocellular
carcinoma. Mol Carcinog. 56:258–271. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Shin H, Cha HJ, Na K, Lee MJ, Cho JY, Kim
CY, Kim EK, Kang CM, Kim H and Paik YK: O-GlcNAcylation of the
tumor suppressor FOXO3 triggers aberrant cancer cell growth. Cancer
Res. 78:1214–1224. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Very N, Steenackers A, Dubuquoy C, Vermuse
J, Dubuquoy L, Lefebvre T and El Yazidi-Belkoura I: Cross
regulation between mTOR signaling and O-GlcNAcylation. J Bioenerg
Biomembr. 50:213–222. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Sodi VL, Khaku S, Krutilina R, Schwab LP,
Vocadlo DJ, Seagroves TN and Reginato MJ: mTOR/MYC axis regulates
O-GlcNAc transferase expression and O-GlcNAcylation in breast
cancer. Mol Cancer Res. 13:923–933. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Jin L, Yuan F, Dai G, Yao Q, Xiang H, Wang
L, Xue B, Shan Y and Liu X: Blockage of O-linked GlcNAcylation
induces AMPK-dependent autophagy in bladder cancer cells. Cell Mol
Biol Lett. 25:172020. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Cork GK, Thompson J and Slawson C: Real
talk: The inter-play between the mTOR, AMPK, and hexosamine
biosynthetic pathways in cell signaling. Front Endocrinol
(Lausanne). 9:5222018. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Ravindran Menon D, Hammerlindl H, Gimenez
G, Hammerlindl S, Zuegner E, Torrano J, Bordag N, Emran AA, Giam M,
Denil S, et al: H3K4me3 remodeling induced acquired resistance
through O-GlcNAc transferase. Drug Resist Updat. 71:1009932023.
View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Ishimura E, Nakagawa T, Moriwaki K, Hirano
S, Matsumori Y and Asahi M: Augmented O-GlcNAcylation of
AMP-activated kinase promotes the proliferation of LoVo cells, a
colon cancer cell line. Cancer Sci. 108:2373–2382. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Zibrova D, Vandermoere F, Göransson O,
Peggie M, Mariño KV, Knierim A, Spengler K, Weigert C, Viollet B,
Morrice NA, et al: GFAT1 phosphorylation by AMPK promotes
VEGF-induced angiogenesis. Biochem J. 474:983–1001. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Gélinas R, Mailleux F, Dontaine J, Bultot
L, Demeulder B, Ginion A, Daskalopoulos EP, Esfahani H,
Dubois-Deruy E, Lauzier B, et al: AMPK activation counteracts
cardiac hypertrophy by reducing O-GlcNAcylation. Nat Commun.
9:3742018. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Phoomak C, Vaeteewoottacharn K,
Sawanyawisuth K, Seubwai W, Wongkham C, Silsirivanit A and Wongkham
S: Mechanistic insights of O-GlcNAcylation that promote progression
of cholangiocarcinoma cells via nuclear translocation of NF-κB. Sci
Rep. 6:278532016. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Phoomak C, Vaeteewoottacharn K,
Silsirivanit A, Saengboonmee C, Seubwai W, Sawanyawisuth K,
Wongkham C and Wongkham S: High glucose levels boost the
aggressiveness of highly metastatic cholangiocarcinoma cells via
O-GlcNAcylation. Sci Rep. 7:438422017. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Jiang M, Xu B, Li X, Shang Y, Chu Y, Wang
W, Chen D, Wu N, Hu S, Zhang S, et al: O-GlcNAcylation promotes
colorectal cancer metastasis via the miR-101-O-GlcNAc/EZH2
regulatory feedback circuit. Oncogene. 38:301–316. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Hanahan D and Weinberg RA: Hallmarks of
cancer: The next generation. Cell. 144:646–674. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Itkonen HM, Gorad SS, Duveau DY, Martin
SE, Barkovskaya A, Bathen TF, Moestue SA and Mills IG: Inhibition
of O-GlcNAc transferase activity reprograms prostate cancer cell
metabolism. Oncotarget. 7:12464–12476. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Nie H, Ju H, Fan J, Shi X, Cheng Y, Cang
X, Zheng Z, Duan X and Yi W: O-GlcNAcylation of PGK1 coordinates
glycolysis and TCA cycle to promote tumor growth. Nat Commun.
11:362020. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Singh JP, Qian K, Lee JS, Zhou J, Han X,
Zhang B, Ong Q, Ni W, Jiang M, Ruan HB, et al: O-GlcNAcase targets
pyruvate kinase M2 to regulate tumor growth. Oncogene. 39:560–573.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Wu MJ, Shi L, Merritt J, Zhu AX and
Bardeesy N: Biology of IDH mutant cholangiocarcinoma. Hepatology.
75:1322–1337. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
He X, Wu N, Li R, Zhang H, Zhao Y, Nie Y
and Wu J: IDH2, a novel target of OGT, facilitates glucose uptake
and cellular bioenergy production via NF-κB signaling to promote
colorectal cancer progression. Cell Oncol (Dordr). 46:145–164.
2023. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Rao X, Duan X, Mao W, Li X, Li Z, Li Q,
Zheng Z, Xu H, Chen M, Wang PG, et al: O-GlcNAcylation of G6PD
promotes the pentose phosphate pathway and tumor growth. Nat
Commun. 6:84682015. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Yi W, Clark PM, Mason DE, Keenan MC, Hill
C, Goddard WA III, Peters EC, Driggers EM and Hsieh-Wilson LC:
Phosphofructokinase 1 glycosylation regulates cell growth and
metabolism. Science. 337:975–980. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Cheng C, Geng F, Cheng X and Guo D: Lipid
metabolism reprogramming and its potential targets in cancer.
Cancer Commun (Lond). 38:272018.PubMed/NCBI
|
|
79
|
Koundouros N and Poulogiannis G:
Reprogramming of fatty acid metabolism in cancer. Br J Cancer.
122:4–22. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Sodi VL, Bacigalupa ZA, Ferrer CM, Lee JV,
Gocal WA, Mukhopadhyay D, Wellen KE, Ivan M and Reginato MJ:
Nutrient sensor O-GlcNAc transferase controls cancer lipid
metabolism via SREBP-1 regulation. Oncogene. 37:924–934. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Tan W, Jiang P, Zhang W, Hu Z, Lin S, Chen
L, Li Y, Peng C, Li Z, Sun A, et al: Posttranscriptional regulation
of de novo lipogenesis by glucose-induced O-GlcNAcylation. Mol
Cell. 81:1890–1904.e7. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Miller DM, Thomas SD, Islam A, Muench D
and Sedoris K: c-Myc and cancer metabolism. Clin Cancer Res.
18:5546–5553. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Llombart V and Mansour MR: Therapeutic
targeting of ‘undruggable’ MYC. EBioMedicine. 75:1037562022.
View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Morrish F, Isern N, Sadilek M, Jeffrey M
and Hockenbery DM: c-Myc activates multiple metabolic networks to
generate substrates for cell-cycle entry. Oncogene. 28:2485–2491.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Itkonen HM, Minner S, Guldvik IJ, Sandmann
MJ, Tsourlakis MC, Berge V, Svindland A, Schlomm T and Mills IG:
O-GlcNAc transferase integrates metabolic pathways to regulate the
stability of c-MYC in human prostate cancer cells. Cancer Res.
73:5277–5287. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Luanpitpong S, Angsutararux P, Samart P,
Chanthra N, Chanvorachote P and Issaragrisil S:
Hyper-O-GlcNAcylation induces cisplatin resistance via regulation
of p53 and c-Myc in human lung carcinoma. Sci Rep. 7:106072017.
View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Aishima S, Fujita N, Mano Y, Kubo Y,
Tanaka Y, Taketomi A, Shirabe K, Maehara Y and Oda Y: Different
roles of S100P overexpression in intrahepatic cholangiocarcinoma:
Carcinogenesis of perihilar type and aggressive behavior of
peripheral type. Am J Surg Pathol. 35:590–598. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Chen T, Ruan Y, Ji L, Cai J, Tong M, Xue
Y, Zhao H, Cai X and Xu J: S100A6 drives lymphatic metastasis of
liver cancer via activation of the RAGE/NF-kB/VEGF-D pathway.
Cancer Lett. 587:2167092024. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Su Y, Luo Y, Zhang P, Lin H, Pu W, Zhang
H, Wang H, Hao Y, Xiao Y, Zhang X, et al: Glucose-induced
CRL4COP1-p53 axis amplifies glycometabolism to drive
tumorigenesis. Mol Cell. 83:2316–2331.e7. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Song P, Gao Z, Bao Y, Chen L, Huang Y, Liu
Y, Dong Q and Wei X: Wnt/β-catenin signaling pathway in
carcinogenesis and cancer therapy. J Hematol Oncol. 17:462024.
View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Raab S, Gadault A, Very N, Decourcelle A,
Baldini S, Schulz C, Mortuaire M, Lemaire Q, Hardivillé S,
Dehennaut V, et al: Dual regulation of fatty acid synthase (FASN)
expression by O-GlcNAc transferase (OGT) and mTOR pathway in
proliferating liver cancer cells. Cell Mol Life Sci. 78:5397–5413.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Wang D, Chen D, Liang L and Hu J: The
circZEB1/miR-337-3p/OGT axis mediates angiogenesis and metastasis
via O-GlcNAcylation and up-regulating YBX1 in breast cancer.
Heliyon. 10:e340792024. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Babae N, Bourajjaj M, Liu Y, Van Beijnum
JR, Cerisoli F, Scaria PV, Verheul M, Van Berkel MP, Pieters EH,
Van Haastert RJ, et al: Systemic miRNA-7 delivery inhibits tumor
angiogenesis and growth in murine xenograft glioblastoma.
Oncotarget. 5:6687–6700. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Weis SM and Cheresh DA: Tumor
angiogenesis: Molecular pathways and therapeutic targets. Nat Med.
17:1359–1370. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Lynch TP, Ferrer CM, Jackson SR, Shahriari
KS, Vosseller K and Reginato MJ: Critical role of O-linked
β-N-acetylglucosamine transferase in prostate cancer invasion,
angiogenesis, and metastasis. J Biol Chem. 287:11070–11081. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Zhu Q, Zhou L, Yang Z, Lai M, Xie H, Wu L,
Xing C, Zhang F and Zheng S: O-GlcNAcylation plays a role in tumor
recurrence of hepatocellular carcinoma following liver
transplantation. Med Oncol. 29:985–993. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Duan F, Wu H, Jia D, Wu W, Ren S, Wang L,
Song S, Guo X, Liu F, Ruan Y and Gu J: O-GlcNAcylation of RACK1
promotes hepatocellular carcinogenesis. J Hepatol. 68:1191–1202.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Luo B, Soesanto Y and McClain DA: Protein
modification by O-linked GlcNAc reduces angiogenesis by inhibiting
Akt activity in endothelial cells. Arterioscler Thromb Vasc Biol.
28:651–657. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Li X, Peng X, Zhang C, Bai X, Li Y, Chen
G, Guo H, He W, Zhou X and Gou X: Bladder cancer-derived small
extracellular vesicles promote tumor angiogenesis by inducing
HBP-related metabolic reprogramming and SerRS O-GlcNAcylation in
endothelial cells. Adv Sci (Weinh). 9:e22029932022. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Hanahan D: Hallmarks of cancer: New
dimensions. Cancer Discov. 12:31–46. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Shen S, Shao Y and Li C: Different types
of cell death and their shift in shaping disease. Cell Death
Discov. 9:2842023. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Scimeca M, Rovella V, Palumbo V, Scioli
MP, Bonfiglio R, Tor Centre, Melino G, Piacentini M, Frati L,
Agostini M, et al: Programmed cell death pathways in
cholangiocarcinoma: Opportunities for targeted therapy. Cancers
(Basel). 15:36382023. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
D'Artista L and Seehawer M: Cell Death and
survival mechanisms in cholangiocarcinogenesis. Am J Pathol.
195:470–479. 2025. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Li M, Duan F, Pan Z, Liu X, Lu W, Liang C,
Fang Z, Peng P and Jia D: Astragalus polysaccharide promotes
doxorubicin-induced apoptosis by reducing O-GlcNAcylation in
hepatocellular carcinoma. Cells. 12:8662023. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Barkovskaya A, Seip K, Prasmickaite L,
Mills IG, Moestue SA and Itkonen HM: Inhibition of O-GlcNAc
transferase activates tumor-suppressor gene expression in
tamoxifen-resistant breast cancer cells. Sci Rep. 10:169922020.
View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Wu J, Tan Z, Li H, Lin M, Jiang Y, Liang
L, Ma Q, Gou J, Ning L, Li X and Guan F: Melatonin reduces
proliferation and promotes apoptosis of bladder cancer cells by
suppressing O-GlcNAcylation of cyclin-dependent-like kinase 5. J
Pineal Res. 71:e127652021. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Deng X, Yi X, Huang D, Liu P, Chen L, Du Y
and Hao L: ROCK2 mediates osteosarcoma progression and TRAIL
resistance by modulating O-GlcNAc transferase degradation. Am J
Cancer Res. 10:781–798. 2020.PubMed/NCBI
|
|
108
|
Wang L, Chen S, Zhang Z, Zhang J, Mao S,
Zheng J, Xuan Y, Liu M, Cai K, Zhang W, et al: Suppressed OGT
expression inhibits cell proliferation while inducing cell
apoptosis in bladder cancer. BMC Cancer. 18:11412018. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Yu FY, Zhou CY, Liu YB, Wang B, Mao L and
Li Y: miR-483 is down-regulated in gastric cancer and suppresses
cell proliferation, invasion and protein O-GlcNAcylation by
targeting OGT. Neoplasma. 65:406–414. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Wen T, Hou K, Li Z, Li L, Yu H, Liu Y, Li
Y and Yin Z: Silencing β-linked N-acetylglucosamine transferase
induces apoptosis in human gastric cancer cells through PUMA and
caspase-3 pathways. Oncol Rep. 34:3140–3146. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Asthana A, Ramakrishnan P, Vicioso Y,
Zhang K and Parameswaran R: Hexosamine biosynthetic pathway
inhibition leads to AML cell differentiation and cell death. Mol
Cancer Ther. 17:2226–2237. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Lee SJ, Lee DE, Choi SY and Kwon OS:
OSMI-1 enhances TRAIL-induced apoptosis through ER stress and NF-κB
signaling in colon cancer cells. Int J Mol Sci. 22:110732021.
View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Ferrer CM, Lynch TP, Sodi VL, Falcone JN,
Schwab LP, Peacock DL, Vocadlo DJ, Seagroves TN and Reginato MJ:
O-GlcNAcylation regulates cancer metabolism and survival stress
signaling via regulation of the HIF-1 pathway. Mol Cell.
54:820–831. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Loison I, Pioger A, Paget S, Metatla I;
OrgaRES Consortium, ; Vincent A, Abbadie C and Dehennaut V:
O-GlcNAcylation inhibition redirects the response of colon cancer
cells to chemotherapy from senescence to apoptosis. Cell Death Dis.
15:7622024. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Leonel AV, Alisson-Silva F, Santos RCM,
Silva-Aguiar RP, Gomes JC, Longo GMC, Faria BM, Siqueira MS,
Pereira MG, Vasconcelos-Dos-Santos A, et al: Inhibition of
O-GlcNAcylation reduces cell viability and autophagy and increases
sensitivity to chemotherapeutic temozolomide in glioblastoma.
Cancers (Basel). 15:47402023. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Ben Ahmed A, Scache J, Mortuaire M,
Lefebvre T and Vercoutter-Edouart AS: Downregulation of O-GlcNAc
transferase activity impairs basal autophagy and late endosome
positioning under nutrient-rich conditions in human colon cells.
Biochem Biophys Res Commun. 724:1501982024. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Zhu Y, Shan X, Safarpour F, Erro Go N, Li
N, Shan A, Huang MC, Deen M, Holicek V, Ashmus R, et al:
Pharmacological inhibition of O-GlcNAcase enhances autophagy in
brain through an mTOR-independent pathway. ACS Chem Neurosci.
9:1366–1379. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Jo YK, Park NY, Park SJ, Kim BG, Shin JH,
Jo DS, Bae DJ, Suh YA, Chang JH, Lee EK, et al: O-GlcNAcylation of
ATG4B positively regulates autophagy by increasing its hydroxylase
activity. Oncotarget. 7:57186–57196. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Shi Y, Yan S, Shao GC, Wang J, Jian YP,
Liu B, Yuan Y, Qin K, Nai S, Huang X, et al: O-GlcNAcylation
stabilizes the autophagy-initiating kinase ULK1 by inhibiting
chaperone-mediated autophagy upon HPV infection. J Biol Chem.
298:1023412022. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Sun QH, Wang YS, Liu G, Zhou HL, Jian YP,
Liu MD, Zhang D, Ding Q, Zhao RX, Chen JF, et al: Enhanced O-linked
glcnacylation in Crohn's disease promotes intestinal inflammation.
EBioMedicine. 53:1026932020. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Guo B, Liang Q, Li L, Hu Z, Wu F, Zhang P,
Ma Y, Zhao B, Kovács AL, Zhang Z, et al: O-GlcNAc-modification of
SNAP-29 regulates autophagosome maturation. Nat Cell Biol.
16:1215–1226. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Pellegrini FR, De Martino S, Fianco G,
Ventura I, Valente D, Fiore M, Trisciuoglio D and Degrassi F:
Blockage of autophagosome-lysosome fusion through SNAP29
O-GlcNAcylation promotes apoptosis via ROS production. Autophagy.
19:2078–2093. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Zhou F, Yang X, Zhao H, Liu Y, Feng Y, An
R, Lv X, Li J and Chen B: Down-regulation of OGT promotes cisplatin
resistance by inducing autophagy in ovarian cancer. Theranostics.
8:5200–5212. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
124
|
Ruan HB, Ma Y, Torres S, Zhang B, Feriod
C, Heck RM, Qian K, Fu M, Li X, Nathanson MH, et al:
Calcium-dependent O-GlcNAc signaling drives liver autophagy in
adaptation to starvation. Genes Dev. 31:1655–1665. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
125
|
Zhang H, Zhang J, Dong H, Kong Y and Guan
Y: Emerging field: O-GlcNAcylation in ferroptosis. Front Mol
Biosci. 10:12032692023. View Article : Google Scholar : PubMed/NCBI
|
|
126
|
Tang J, Long G, Hu K, Xiao D, Liu S, Xiao
L, Zhou L and Tao Y: Targeting USP8 inhibits O-GlcNAcylation of
SLC7A11 to promote ferroptosis of hepatocellular carcinoma via
stabilization of OGT. Adv Sci (Weinh). 10:e23029532023. View Article : Google Scholar : PubMed/NCBI
|
|
127
|
Liu H, Fu Y, Tang L, Song B, Gu W, Yang H,
Xiao T, Wang H and Chen P: O-GlcNAc-modified HOXA9 suppresses
ferroptosis via promoting UBR5-mediated SIRT6 degradation in
nasopharyngeal carcinoma. Neoplasia. 62:1011422025. View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Li Q, Cheng Y, Yang C, Tian M, Wang X, Li
D, Li X, Qu J, Zhou S, Zheng L and Tong Q: Targeting the exonic
circular OGT RNA/O-GlcNAc transferase/forkhead box C1 axis inhibits
asparagine- and alanine-mediated ferroptosis repression in
neuroblastoma progression. Research (Wash D C).
8:07032025.PubMed/NCBI
|
|
129
|
Yang Z, Wei X, Ji C, Ren X, Su W, Wang Y,
Zhou J, Zhao Z, Zhou P, Zhao K, et al: OGT/HIF-2α axis promotes the
progression of clear cell renal cell carcinoma and regulates its
sensitivity to ferroptosis. iScience. 26:1081482023. View Article : Google Scholar : PubMed/NCBI
|
|
130
|
Li X, Gong W, Wang H, Li T, Attri KS,
Lewis RE, Kalil AC, Bhinderwala F, Powers R, Yin G, et al: O-GlcNAc
transferase suppresses inflammation and necroptosis by targeting
receptor-interacting serine/threonine-protein kinase 3. Immunity.
50:576–590.e6. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
131
|
Zhang B, Li MD, Yin R, Liu Y, Yang Y,
Mitchell-Richards KA, Nam JH, Li R, Wang L, Iwakiri Y, et al:
O-GlcNAc transferase suppresses necroptosis and liver fibrosis. JCI
Insight. 4:e1277092019. View Article : Google Scholar : PubMed/NCBI
|
|
132
|
Brindley PJ, Bachini M, Ilyas SI, Khan SA,
Loukas A, Sirica AE, Teh BT, Wongkham S and Gores GJ:
Cholangiocarcinoma. Nat Rev Dis Primers. 7:652021. View Article : Google Scholar : PubMed/NCBI
|
|
133
|
Labib PL, Goodchild G and Pereira SP:
Molecular pathogenesis of cholangiocarcinoma. BMC Cancer.
19:1852019. View Article : Google Scholar : PubMed/NCBI
|
|
134
|
Leone V, Ali A, Weber A, Tschaharganeh DF
and Heikenwalder M: Liver inflammation and hepatobiliary cancers.
Trends Cancer. 7:606–623. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
135
|
Ouyang M, Yu C, Deng X, Zhang Y, Zhang X
and Duan F: O-GlcNAcylation and its role in cancer-associated
inflammation. Front Immunol. 13:8615592022. View Article : Google Scholar : PubMed/NCBI
|
|
136
|
Yang WH, Park SY, Nam HW, Kim DH, Kang JG,
Kang ES, Kim YS, Lee HC, Kim KS and Cho JW: NFkappaB activation is
associated with its O-GlcNAcylation state under hyperglycemic
conditions. Proc Natl Acad Sci USA. 105:17345–17350. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
137
|
Ali A, Kim SH, Kim MJ, Choi MY, Kang SS,
Cho GJ, Kim YS, Choi JY and Choi WS: O-GlcNAcylation of NF-κB
promotes lung metastasis of cervical cancer cells via upregulation
of CXCR4 expression. Mol Cells. 40:476–484. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
138
|
Yang YR, Kim DH, Seo YK, Park D, Jang HJ,
Choi SY, Lee YH, Lee GH, Nakajima K, Taniguchi N, et al: Elevated
O-GlcNAcylation promotes colonic inflammation and tumorigenesis by
modulating NF-κB signaling. Oncotarget. 6:12529–12542. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
139
|
Pathak S, Borodkin VS, Albarbarawi O,
Campbell DG, Ibrahim A and van Aalten DM: O-GlcNAcylation of TAB1
modulates TAK1-mediated cytokine release. EMBO J. 31:1394–1404.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
140
|
Kawauchi K, Araki K, Tobiume K and Tanaka
N: Loss of p53 enhances catalytic activity of IKKbeta through
O-linked beta-N-acetyl glucosamine modification. Proc Natl Acad Sci
USA. 106:3431–3436. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
141
|
Li X, Zhang Z, Li L, Gong W, Lazenby AJ,
Swanson BJ, Herring LE, Asara JM, Singer JD and Wen H:
Myeloid-derived cullin 3 promotes STAT3 phosphorylation by
inhibiting OGT expression and protects against intestinal
inflammation. J Exp Med. 214:1093–1109. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
142
|
Freund P, Kerenyi MA, Hager M, Wagner T,
Wingelhofer B, Pham HTT, Elabd M, Han X, Valent P, Gouilleux F, et
al: O-GlcNAcylation of STAT5 controls tyrosine phosphorylation and
oncogenic transcription in STAT5-dependent malignancies. Leukemia.
31:2132–2142. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
143
|
Jin H, He H, Li J, Liu X, Cai Q, Shi J,
Hao Z and He J: Mannose Inhibits NSCLC growth and inflammatory
microenvironment by regulating gut microbiota and targeting
OGT/hnRNP R/JUN/IL-8 axis. Int J Biol Sci. 21:1566–1584. 2025.
View Article : Google Scholar : PubMed/NCBI
|
|
144
|
Hinshaw DC, Hanna A, Lama-Sherpa T, Metge
B, Kammerud SC, Benavides GA, Kumar A, Alsheikh HA, Mota M, Chen D,
et al: Hedgehog signaling regulates metabolism and polarization of
mammary tumor-associated macrophages. Cancer Res. 81:5425–5437.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
145
|
Hinshaw DC, Benavides GA, Metge BJ, Swain
CA, Kammerud SC, Alsheikh HA, Elhamamsy A, Chen D, Darley-Usmar V,
Rathmell JC, et al: Hedgehog signaling regulates Treg to Th17
conversion through metabolic rewiring in breast cancer. Cancer
Immunol Res. 11:687–702. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
146
|
Das S, Bailey SK, Metge BJ, Hanna A,
Hinshaw DC, Mota M, Forero-Torres A, Chatham JC, Samant RS and
Shevde LA: O-GlcNAcylation of GLI transcription factors in
hyperglycemic conditions augments Hedgehog activity. Lab Invest.
99:260–270. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
147
|
Chen L, Li Y, Song Z, Xue S, Liu F, Chang
X, Wu Y, Duan X and Wu H: O-GlcNAcylation promotes cerebellum
development and medulloblastoma oncogenesis via SHH signaling. Proc
Natl Acad Sci USA. 119:e22028211192022. View Article : Google Scholar : PubMed/NCBI
|
|
148
|
Rodrigues Mantuano N, Stanczak MA,
Oliveira IA, Kirchhammer N, Filardy AA, Monaco G, Santos RC,
Fonseca AC, Fontes M, Bastos CS Jr, et al: Hyperglycemia enhances
cancer immune evasion by inducing alternative macrophage
polarization through increased O-GlcNAcylation. Cancer Immunol Res.
8:1262–1272. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
149
|
Zhang HR, Li TJ, Yu XJ, Liu C, Wu WD, Ye
LY and Jin KZ: The GFPT2-O-GlcNAcylation-YBX1 axis promotes IL-18
secretion to regulate the tumor immune microenvironment in
pancreatic cancer. Cell Death Dis. 15:2442024. View Article : Google Scholar : PubMed/NCBI
|
|
150
|
Shi Q, Shen Q, Liu Y, Shi Y, Huang W, Wang
X, Li Z, Chai Y, Wang H, Hu X, et al: Increased glucose metabolism
in TAMs fuels O-GlcNAcylation of lysosomal cathepsin B to promote
cancer metastasis and chemoresistance. Cancer Cell.
40:1207–1222.e10. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
151
|
Alsheikh HAM, Metge BJ, Ha CM, Hinshaw DC,
Mota MSV, Kammerud SC, Lama-Sherpa T, Sharafeldin N, Wende AR,
Samant RS and Shevde LA: Normalizing glucose levels reconfigures
the mammary tumor immune and metabolic microenvironment and
decreases metastatic seeding. Cancer Lett. 517:24–34. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
152
|
Swamy M, Pathak S, Grzes KM, Damerow S,
Sinclair LV, van Aalten DM and Cantrell DA: Glucose and glutamine
fuel protein O-GlcNAcylation to control T cell self-renewal and
malignancy. Nat Immunol. 17:712–720. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
153
|
Lopez Aguilar A, Gao Y, Hou X, Lauvau G,
Yates JR and Wu P: Profiling of protein O-GlcNAcylation in murine
CD8+ effector- and memory-like T cells. ACS Chem Biol.
12:3031–3038. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
154
|
Qiu Y, Su Y, Xie E, Cheng H, Du J, Xu Y,
Pan X, Wang Z, Chen DG, Zhu H, et al: Mannose metabolism reshapes T
cell differentiation to enhance anti-tumor immunity. Cancer Cell.
43:103–121.e8. 2025. View Article : Google Scholar : PubMed/NCBI
|
|
155
|
Machacek M, Saunders H, Zhang Z, Tan EP,
Li J, Li T, Villar MT, Artigues A, Lydic T, Cork G, et al: Elevated
O-GlcNAcylation enhances pro-inflammatory Th17 function by altering
the intracellular lipid microenvironment. J Biol Chem.
294:8973–8990. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
156
|
Liu B, Salgado OC, Singh S, Hippen KL,
Maynard JC, Burlingame AL, Ball LE, Blazar BR, Farrar MA, Hogquist
KA and Ruan HB: The lineage stability and suppressive program of
regulatory T cells require protein O-GlcNAcylation. Nat Commun.
10:3542019. View Article : Google Scholar : PubMed/NCBI
|
|
157
|
Yuan Y, Wang L, Ge D, Tan L, Cao B, Fan H
and Xue L: Exosomal O-GlcNAc transferase from esophageal carcinoma
stem cell promotes cancer immunosuppression through up-regulation
of PD-1 in CD8+ T cells. Cancer Lett. 500:98–106. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
158
|
Perišić Nanut M, Pečar Fonović U, Jakoš T
and Kos J: The role of cysteine peptidases in hematopoietic stem
cell differentiation and modulation of immune system function.
Front Immunol. 12:6802792021. View Article : Google Scholar : PubMed/NCBI
|
|
159
|
Božič J, Stoka V and Dolenc I: Glucosamine
prevents polarization of cytotoxic granules in NK-92 cells by
disturbing FOXO1/ERK/paxillin phosphorylation. PLoS One.
13:e02007572018. View Article : Google Scholar : PubMed/NCBI
|
|
160
|
Zhang N, Jiang H, Zhang K, Zhu J, Wang Z,
Long Y, He Y, Feng F, Liu W, Ye F and Qu W: OGT as potential novel
target: Structure, function and inhibitors. Chem Biol Interact.
357:1098862022. View Article : Google Scholar : PubMed/NCBI
|
|
161
|
Konrad RJ, Zhang F, Hale JE, Knierman MD,
Becker GW and Kudlow JE: Alloxan is an inhibitor of the enzyme
O-linked N-acetylglucosamine transferase. Biochem Biophys Res
Commun. 293:207–212. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
162
|
Liu TW, Zandberg WF, Gloster TM, Deng L,
Murray KD, Shan X and Vocadlo DJ: Metabolic inhibitors of O-GlcNAc
transferase that act in vivo implicate decreased O-GlcNAc levels in
leptin-mediated nutrient sensing. Angew Chem Int Ed Engl.
57:7644–7648. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
163
|
Pantaleon M, Tan HY, Kafer GR and Kaye PL:
Toxic effects of hyperglycemia are mediated by the hexosamine
signaling pathway and o-linked glycosylation in early mouse
embryos. Biol Reprod. 82:751–758. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
164
|
Gross BJ, Kraybill BC and Walker S:
Discovery of O-GlcNAc transferase inhibitors. J Am Chem Soc.
127:14588–14589. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
165
|
Liu Y, Ren Y, Cao Y, Huang H, Wu Q, Li W,
Wu S and Zhang J: Discovery of a low toxicity O-GlcNAc transferase
(OGT) inhibitor by structure-based virtual screening of natural
products. Sci Rep. 7:123342017. View Article : Google Scholar : PubMed/NCBI
|
|
166
|
Ortiz-Meoz RF, Jiang J, Lazarus MB, Orman
M, Janetzko J, Fan C, Duveau DY, Tan ZW, Thomas CJ and Walker S: A
small molecule that inhibits OGT activity in cells. ACS Chem Biol.
10:1392–1397. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
167
|
Martin SES, Tan ZW, Itkonen HM, Duveau DY,
Paulo JA, Janetzko J, Boutz PL, Törk L, Moss FA, Thomas CJ, et al:
Structure-based evolution of low nanomolar O-GlcNAc transferase
inhibitors. J Am Chem Soc. 140:13542–13545. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
168
|
Efimova EV, Appelbe OK, Ricco N, Lee SS,
Liu Y, Wolfgeher DJ, Collins TN, Flor AC, Ramamurthy A, Warrington
S, et al: O-GlcNAcylation enhances double-strand break repair,
promotes cancer cell proliferation, and prevents therapy-induced
senescence in irradiated tumors. Mol Cancer Res. 17:1338–1350.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
169
|
Huang YJ, Chen YT, Huang CM, Kuo SH, Liao
YY, Jhang WY, Wang SH, Ke CC, Huang YH, Cheng CM, et al: HIF-1α
expression increases preoperative concurrent chemoradiotherapy
resistance in hyperglycemic rectal cancer. Cancers (Basel).
14:40532022. View Article : Google Scholar : PubMed/NCBI
|
|
170
|
Ping X and Stark JM: O-GlcNAc transferase
is important for homology-directed repair. DNA Repair (Amst).
119:1033942022. View Article : Google Scholar : PubMed/NCBI
|
|
171
|
Na HJ, Akan I, Abramowitz LK and Hanover
JA: Nutrient-driven O-GlcNAcylation controls DNA damage repair
signaling and stem/progenitor cell homeostasis. Cell Rep.
31:1076322020. View Article : Google Scholar : PubMed/NCBI
|
|
172
|
Naimi A, Mohammed RN, Raji A, Chupradit S,
Yumashev AV, Suksatan W, Shalaby MN, Thangavelu L, Kamrava S,
Shomali N, et al: Tumor immunotherapies by immune checkpoint
inhibitors (ICIs); the pros and cons. Cell Commun Signal.
20:442022. View Article : Google Scholar : PubMed/NCBI
|
|
173
|
Zhu Q, Wang H, Chai S, Xu L, Lin B, Yi W
and Wu L: O-GlcNAcylation promotes tumor immune evasion by
inhibiting PD-L1 lysosomal degradation. Proc Natl Acad Sci USA.
120:e22167961202023. View Article : Google Scholar : PubMed/NCBI
|
|
174
|
Chen J, Zhao B, Dong H, Li T, Cheng X,
Gong W, Wang J, Zhang J, Xin G, Yu Y, et al: Inhibition of O-GlcNAc
transferase activates type I interferon-dependent antitumor
immunity by bridging cGAS-STING pathway. Elife. 13:RP948492024.
View Article : Google Scholar : PubMed/NCBI
|
|
175
|
Kumatori A, Tanaka K, Inamura N, Sone S,
Ogura T, Matsumoto T, Tachikawa T, Shin S and Ichihara A:
Abnormally high expression of proteasomes in human leukemic cells.
Proc Natl Acad Sci USA. 87:7071–7075. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
176
|
Chen L and Madura K: Increased proteasome
activity, ubiquitin-conjugating enzymes, and eEF1A translation
factor detected in breast cancer tissue. Cancer Res. 65:5599–5606.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
177
|
Arlt A, Bauer I, Schafmayer C, Tepel J,
Müerköster SS, Brosch M, Röder C, Kalthoff H, Hampe J, Moyer MP, et
al: Increased proteasome subunit protein expression and proteasome
activity in colon cancer relate to an enhanced activation of
nuclear factor E2-related factor 2 (Nrf2). Oncogene. 28:3983–3996.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
178
|
Soave CL, Guerin T, Liu J and Dou QP:
Targeting the ubiquitin-proteasome system for cancer treatment:
Discovering novel inhibitors from nature and drug repurposing.
Cancer Metastasis Rev. 36:717–736. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
179
|
Fricker LD: Proteasome inhibitor drugs.
Annu Rev Pharmacol Toxicol. 60:457–476. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
180
|
Zhang F, Su K, Yang X, Bowe DB, Paterson
AJ and Kudlow JE: O-GlcNAc modification is an endogenous inhibitor
of the proteasome. Cell. 115:715–725. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
181
|
Sekine H, Okazaki K, Kato K, Alam MM,
Shima H, Katsuoka F, Tsujita T, Suzuki N, Kobayashi A, Igarashi K,
et al: O-GlcNAcylation signal mediates proteasome inhibitor
resistance in cancer cells by stabilizing NRF1. Mol Cell Biol.
38:e00252–18. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
182
|
Hashimoto E, Okuno S, Hirayama S, Arata Y,
Goto T, Kosako H, Hamazaki J and Murata S: Enhanced O-GlcNAcylation
mediates cytoprotection under proteasome impairment by promoting
proteasome turnover in cancer cells. iScience. 23:1012992020.
View Article : Google Scholar : PubMed/NCBI
|
|
183
|
Zeidan Q, Tian JL, Ma J, Eslami F and Hart
GW: O-GlcNAcylation of ribosome-associated proteins is concomitant
with translational reprogramming during proteotoxic stress. J Biol
Chem. 300:1078772024. View Article : Google Scholar : PubMed/NCBI
|
|
184
|
Xia M, Wang S, Qi Y, Long K, Li E, He L,
Pan F, Guo Z and Hu Z: Inhibition of O-GlcNAc transferase
sensitizes prostate cancer cells to docetaxel. Front Oncol.
12:9932432022. View Article : Google Scholar : PubMed/NCBI
|
|
185
|
Sun MX, An HY, Sun YB, Sun YB and Bai B:
LncRNA EBLN3P attributes methotrexate resistance in osteosarcoma
cells through miR-200a-3p/O-GlcNAc transferase pathway. J Orthop
Surg Res. 17:5572022. View Article : Google Scholar : PubMed/NCBI
|
|
186
|
Kwei KA, Baker JB and Pelham RJ:
Modulators of sensitivity and resistance to inhibition of PI3K
identified in a pharmacogenomic screen of the NCI-60 human tumor
cell line collection. PLoS One. 7:e465182012. View Article : Google Scholar : PubMed/NCBI
|
|
187
|
Wongprayoon P, Pengnam S, Srisuphan R,
Opanasopit P, Jirawatnotai S and Charoensuksai P: The correlation
between cellular O-GlcNAcylation and sensitivity to O-GlcNAc
inhibitor in colorectal cancer cells. PLoS One. 19:e03121732024.
View Article : Google Scholar : PubMed/NCBI
|
|
188
|
Pallasaho S, Gondane A, Kuivalainen A,
Girmay S, Moestue S, Loda M and Itkonen HM: Castration-resistant
prostate cancer cells are dependent on the high activity of CDK7. J
Cancer Res Clin Oncol. 149:5255–5263. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
189
|
Itkonen HM, Poulose N, Steele RE, Martin
SES, Levine ZG, Duveau DY, Carelli R, Singh R, Urbanucci A, Loda M,
et al: Inhibition of O-GlcNAc transferase renders prostate cancer
cells dependent on CDK9. Mol Cancer Res. 18:1512–1521. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
190
|
Shan X, Jiang R, Gou D, Xiang J, Zhou P,
Xia J, Wang K, Huang A, Tang N and Huang L: Identification of a
diketopiperazine-based O-GlcNAc transferase inhibitor sensitizing
hepatocellular carcinoma to CDK9 inhibition. FEBS J. 290:4543–4561.
2023. View Article : Google Scholar : PubMed/NCBI
|
|
191
|
Areewong S, Suppramote O, Prasopporn S and
Jirawatnotai S: Exploiting acquired vulnerability to develop novel
treatments for cholangiocarcinoma. Cancer Cell Int. 24:3622024.
View Article : Google Scholar : PubMed/NCBI
|
|
192
|
Carlson GP: Potentiation of carbon
tetrachloride hepatotoxicity in rats by pretreatment with
polychlorinated biphenyls. Toxicology. 5:69–77. 1975. View Article : Google Scholar : PubMed/NCBI
|
|
193
|
Dong W, Zhu Q, Yang B, Qin Q, Wang Y, Xia
X, Zhu X, Liu Z, Song E and Song Y: Polychlorinated biphenyl
quinone induces caspase 1-mediated pyroptosis through induction of
pro-inflammatory HMGB1-TLR4-NLRP3-GSDMD signal axis. Chem Res
Toxicol. 32:1051–1057. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
194
|
Brown AP, Schultze AE, Holdan WL,
Buchweitz JP, Roth RA and Ganey PE: Lipopolysaccharide-induced
hepatic injury is enhanced by polychlorinated biphenyls. Environ
Health Perspect. 104:634–640. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
195
|
National Toxicology Program, . Toxicology
and carcinogenesis studies of 2,3′,4,4′,5-pentachlorobiphenyl (PCB
118) (CAS No. 31508-00-6) in female harlan Sprague-Dawley rats
(gavage studies). Natl Toxicol Program Tech Rep Ser. 1–174.
2010.
|
|
196
|
National Toxicology Program, . NTP
toxicology and carcinogenesis studies of
3,3′,4,4′,5-pentachlorobiphenyl (PCB 126) (CAS No. 57465-28-8) in
female Harlan Sprague-Dawley rats (Gavage Studies). Natl Toxicol
Program Tech Rep Ser. 4–246. 2006.
|
|
197
|
Ovando BJ, Ellison CA, Vezina CM and Olson
JR: Toxicogenomic analysis of exposure to TCDD, PCB126 and PCB153:
Identification of genomic biomarkers of exposure to AhR ligands.
BMC Genomics. 11:5832010. View Article : Google Scholar : PubMed/NCBI
|