Introduction
Perinatal care remains a major health concern among
mothers and children worldwide. In Japan, 99% of women plan to give
birth in obstetrics facilities, clinics and hospitals, under the
care of obstetricians. When obstetric complications arise, a
considerable proportion of pregnant and parturient women are sent
from referring facilities (primary maternity clinics, midwifery
homes, or district and general hospitals) to Emergency Obstetric
and Neonatal Care (EONC) centers by the ambulance or
doctor-helicopter service (1). In
line with the government policy in Japan, the ambulance functions
as an emergency transfer team and works 24 h a day, every day.
Preterm birth is one of the most important complications of
pregnancy and plays a major role in neonatal mortality and
morbidity (2-4).
Furthermore, major causes of direct maternal deaths from pregnancy
complications include peripartum hemorrhage, amniotic fluid
embolism, pulmonary embolism and preeclampsia (5,6).
The current maternal mortality rate in Japan, which is estimated to
be approximately 4 in 100,000 deliveries, is similar to that
observed in other developed countries (6). Previous researchers have identified
that inappropriate referral is an important factor associated with
maternal mortality and morbidity (5).
A shortage of obstetrician resources and excessive
workloads have been encountered in Japan, which may limit the
provision of comprehensive EONC and affect the quality of care
(7). In 2006, a serious incident
related to interfacility transfer (IFT) occurred in Nara
Prefecture, Japan. The patient suffered from a severe headache and
loss of consciousness following the onset of labor. Finally, 18
hospitals refused care and treatment due to the lack of
availability of both a maternal bed and a neonatal bed, as well as
due to the obstetricians' increased workload. The patient was thus
transferred outside of Nara Prefecture (Out-of-Nara transfer) and
died of intracranial hemorrhage after the patient was transferred
and following the attempted transfers to other hospitals which did
not accept the patient. Realizing the above situation, the
Governmental Organization in Nara prefecture has established the
Council for Perinatal Care (CPC) Committee, with responsibility for
reorganizing the IFT system and initiating a population-based
perinatal and neonatal registry. At the time, the EONC centers
often lacked human resources to safely manage women with severe
maternal and fetal complications. Since 2007, in order to improve
the obstetric and neonatal care, the CPC Committee put forward a
number of recommendations regarding the effective communication
between referring facilities and referred facilities.
The aim of this study was to assess the impact of a
newly established IFT system and medical coverage of IFT cases from
2006 to 2017.
Data collection and methods
A newly established IFT system
We used nationwide data in the vital statistics in
Japan on the estimated population of 1,356,950 and 9,626 expected
deliveries per year in Nara Prefecture in 2017 (the vital
statistics published by Ministry of Health, Labor and Welfare in
Japan, 2018; https://www.mhlw.go.jp/toukei/saikin/hw/jinkou/kakutei16/index.html
and http://www.stat.go.jp/data/ssds/).
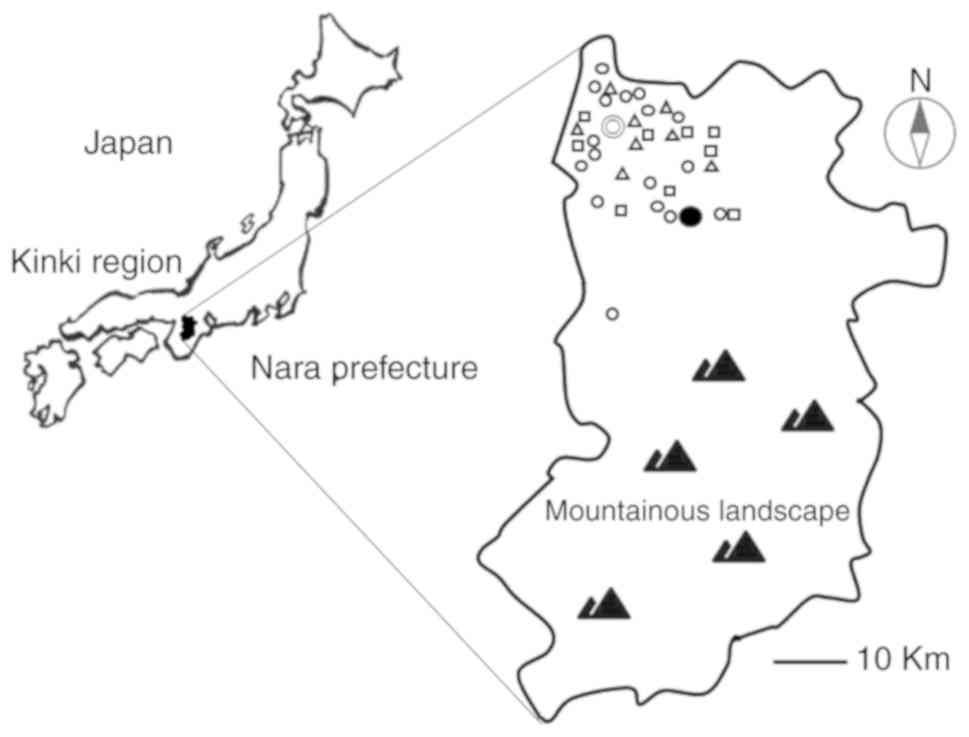
Nara prefecture is an inland prefecture located in Kinki region.
The geographical features in Nara Prefecture are basically a basin
and mountainous region. The northern part is low and flat, and
there are no barriers in accessing medical services. By contrast,
the southern part is mostly mountainous landscape. The habitants
live in hard-to-reach mountainous areas and have difficulties in
accessing medical services. Women plan to give birth in one of four
settings: Freestanding obstetrician-led clinics (approximately
54.2% of all births), freestanding midwife-led units (2.2%), the
prefectural-level district and general hospitals (28.9%), and a
tertiary hospital (14.7%). In 2006, at the beginning of this study,
there were four prefectural-level hospitals [Nara Medical
University (NMU), Nara Prefecture General Medical Center (NPGMC),
Tenri Hospital and Kindai University Nara Hospital] which have
specialist obstetric, pediatric, anesthetic and emergency services
onsite, seven district and general hospitals with the functioning
operation theater for obstetric and gynecological care, 17 primary
clinics staffed by obstetricians and nine midwifery homes (primary
level maternity units staffed by trained midwives). The majority of
the hospitals and clinics were located in the northern part of the
prefecture. The locations of the primary clinics, midwifery homes,
district and general hospitals, NMU and NPGMC are illustrated in
Fig. 1.
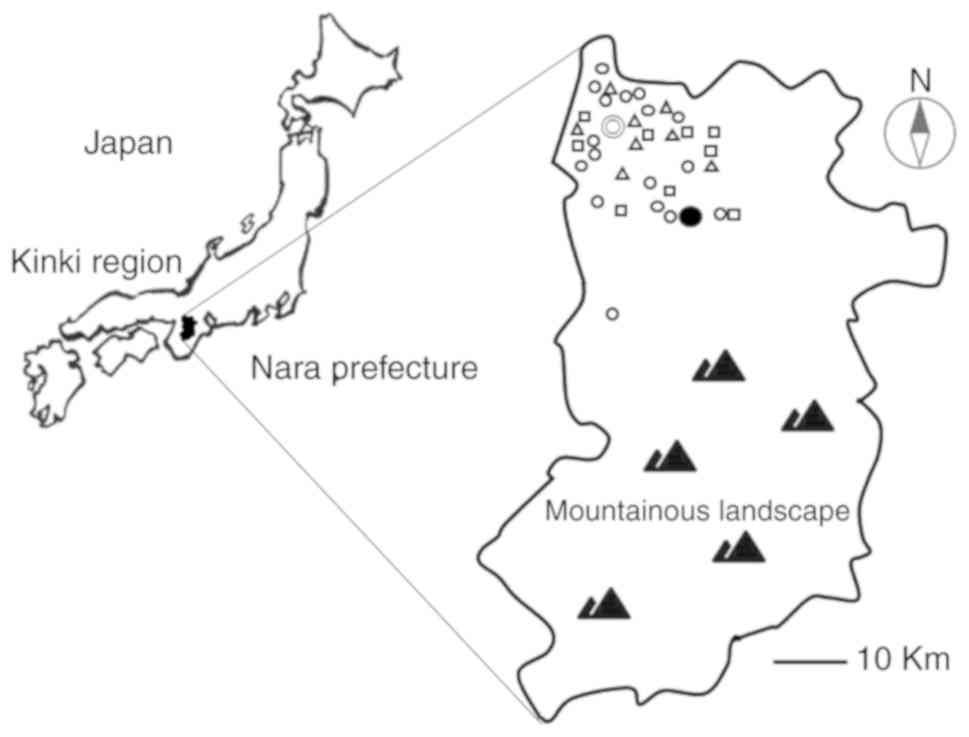 | Figure 1.Map of Nara Prefecture showing the
location of primary maternity clinics (n=16), midwifery homes
(n=8), or district and general hospitals (n=9), and the EONC
centers in 2017. In the map, the symbols indicate the following: ○,
Primary maternity clinics (n-16); Δ, midwifery homes (n-8); □,
district and general hospitals (n=9); ●, NMU; ⦾, NPGMC (EONC
centers). EONC centers, emergency obstetric and neonatal care
centers; NMU, Nara Medical University; NPGMC, Nara Prefecture
General Medical Center. |
Obstetricians in obstetrics-gynecology clinics and
professional midwives contribute to an uncomplicated physiological
birth. They sometimes confront unmet needs for emergency obstetric
care unavailable at their clinics, midwifery homes, or district and
general hospitals. When women are diagnosed as having maternal and
fetal complications, they are referred to EONC centers for
appropriate care. EONC was available in only two of 11 hospitals;
one is a tertiary care facility hospital of NMU (located in the
central part of the prefecture) and the other is a
prefectural-level hospital of NPGMC (located in the northern
district of the prefecture). Multiple barriers at the time,
including workforce shortage (shortage of obstetricians and nursing
staffs), reduced service capability after standard working hours,
excessive workloads of obstetricians, EONC center crowding and
hospital bed shortage and poor collaboration between NMU and NPGMC,
led the lack of availability and access to timely and appropriate
emergency obstetric care. The emergency ambulance was available;
however, an obstetrician of referring facilities or the land
ambulance crew in charge of IFT had to often identify a transfer
destination by oneself. A majority of specialists, including
obstetricians, neonatologists and gynecologists, had unresolved
problems with respect to job stress and had the negative impact of
job-related satisfaction, work-family conflict and working in a
rural area. Before 2006, there was a major public health concern in
perinatal care due to an inadequate IFT program and the low
referral coverage of complicated deliveries. The conflicts emerged
between government and obstetricians at the point of the process of
and policy recommendations for improving perinatal care management
systems.
First, under the leadership of the government, the
CPC Committee was set up to combat the various problems that
obstruct perinatal care. To combat the issue of IFTs, the CPC
Committee set up and reorganized the EONC centers in the tertiary
NMU Hospital as Comprehensive Centers for Perinatal Medicine in
2008 and then NPGMC hospital as Regional Centers for Perinatal
Medicine in 2010, respectively. Two EONC centers were reorganized
through the selection, integrated arrangements and concentration of
obstetric facilities, and requested to build a 24-h communication
network system for the transfer of women with obstetric
complications from referring facilities to the EONC centers. To
ensure sufficient medical coverage at all times, the traditional
overnight on-call and standby duties were assigned to obstetricians
in NMU and NPGMC. Specialized maternal and neonatal care services
were offered in a separate maternal-fetal intensive care unit
(MFICU) and neonatology unit (NICU). We proposed a team composed of
specialists from multiple disciplines (maternal-fetal medicine,
perinatology, neonatology, gynecology with surgical skills,
obstetric anesthesiology, interventional radiology, cardiology,
pulmonology, advanced midwives and nurse specialists etc.). With
this team-based approach, they strongly cooperated with each other
to establish a support system. Further attempts were approached
with careful triage protocol development. The CPC Committee has
achieved a consensus that preterm labor/birth and premature rupture
of membranes between 22+0 and 27+6 weeks of gestation requires an
intensive care in the NMU Hospital, while preterm labor with a
gestational age of >28 weeks with an estimated fetal body weight
>1,000 g is managed by prolonged tocolytic regimens in the NPGMC
Hospital. Since it is very difficult to save the lives of newborns,
pregnant women with a gestational age of <22+0 weeks do not
require an intensive care in EONCs. If women fulfilled the specific
referral criteria (Table I), they
have to be properly transferred from referring facilities to either
of the two EONC centers by an ambulance, with the distance between
1 and 20 km (up to 0.7 h drive one way to the furthest clinics). At
the start of the IFT program, full or optimal coverage of
complicated deliveries had not yet been achieved.
 | Table ICriteria for ambulance referrals to
EONC centers of women at risk of or with an obstetric
complication. |
Table I
Criteria for ambulance referrals to
EONC centers of women at risk of or with an obstetric
complication.
| Maternal complication
with or without organ dysfunction: |
| | Cardiovascular or
renal pathologies, severe hypertension or stroke, diabetes, asthma,
appendicitis, enterocolitis, and infections. |
| Specified critical
interventions: |
| | Need massive blood
transfusion, ventilation and hysterectomy |
| Obstetric
complications: |
| | Prematurity <36
weeks gestation |
| | Premature rupture of
membranes <36 weeks gestation |
| | Hypertensive
disorders of pregnancy/Preeclampsia/eclampsia |
| | Placental
abruption |
| | Placenta previa |
| | Multiple
pregnancy |
| | Pregnant women
without antenatal health care |
| | Non-reassuring fetal
status |
| | Fetal growth
restriction |
| | Intrauterine fetal
death |
| | Malpresentation of
the fetus/umbilical cord |
| | Abdominal pain during
pregnancy |
| | Bleeding during
pregnancy |
| | Postpartum
hemorrhage |
| | Postpartum
sepsis |
Second, there is growing interest in the
effectiveness of task shifting that is an important government
policy option to improve workforce shortages of an obstetrician
(8). Professional midwives have
provided obstetric care and reproductive healthcare for normal
deliveries under the guidance of obstetricians. Since 2011,
midwives in NMU Hospitals were responsible for labor and delivery
care in a low-risk midwifery-led unit. The intense, hands-on
training has been provided in order to improve their skills in the
study meetings of the Japan Association of Obstetricians and
Gynecologists and Japan Academy of Midwifery of Nara
prefecture.
Third, the government programs employed an
obstetrician as a transfer coordinator. Telephone-based services by
a transfer coordinator can provide valuable informational and
practical support for IFTs. A five-point demand was proposed based
on the agreement by the CPC Committee as follows: i) An
obstetrician, midwife, or nurse in referring facilities rides in
the ambulance for the care in principle. The ambulances are well
equipped with a means of communication, EONC treatment protocols, a
patient stretcher, oxygen, drugs, ECG monitor and pulse oximeter
that could be administered in the ambulance by the accompanying
medical staffs en route to emergency obstetric hospitals. ii) In
2015, full-scale 24-h communication network began using
telephone-based services by a transfer coordinator. The
implementation of an emergency referral network includes an
efficient coordination by a transfer coordinator and an effective
communication. Without taking a labor in the referring facilities,
the transfer coordinator can understand an obstetrician's need,
taking each facility's limitations and acceptance into
consideration and can objectively identify a destination. An
optimal combination of the definitive destination avoiding delay
and any necessary support to manage the patient can be provided
over the cell phone to the ambulance medical staffs by the transfer
coordinator. iii) If all beds are filled with patients in EONC
centers, the IFT patient will be transferred from the referring
facilities to emergency obstetric hospitals outside of the
prefecture limits (the Out-of-Nara transfer). iv) If the ambulance
arrives at the referring facilities following vaginal delivery, the
woman and neonate will be transferred to emergency hospitals, even
though she does not require emergency postpartum care. v) Our
effective emergency medical services system includes a timely
dispatch of one ambulance car with special equipment such as a
portable incubator for neonatal transport stationed at the NPGMC
hospital. Ambulance use is free of charge.
Finally, perinatal health registries were developed
in Nara prefecture in 1997. In 2006, the government established a
standing committee to focus on emergency perinatal care. The Board
of the CPC Committee was authorized to design, approve and finance
observational studies in relevant scientific fields to ensure the
quality of community perinatal care services. A hospital-based
perinatal registry was collected, validated, managed, analyzed and
published, which was conducted by an underlying organization of the
CPC Committee at an annual meeting. The publication of the ‘Annual
Report of the Epidemiology and Management regarding Emergency
Obstetric and Neonatal Care’ is a project initiated by the
Committee (http://www.pref.nara.jp/46607.htm). Recent summary
data published through releasing an annual report would be helpful
to strengthen collaboration among critical care staffs and
physicians.
Study design and population
This is a retrospective time series study using a
longitudinal design between January, 2006 and December, 2017. All
facilities were invited to participate in the registry. There are
35 hospitals with deliveries in Nara Prefecture and only 4
hospitals (NMU, NPGMC, Tenri Hospital and Kindai University Nara
Hospital) accept patients with obstetric and neonatal
complications. Transferred patients were defined as either patients
that transported from the primary facilities to EONC centers or
those with the Out-of-Nara transfer. The annual number of and
reasons for IFTs was registered in the CPC Committee during the
study period.
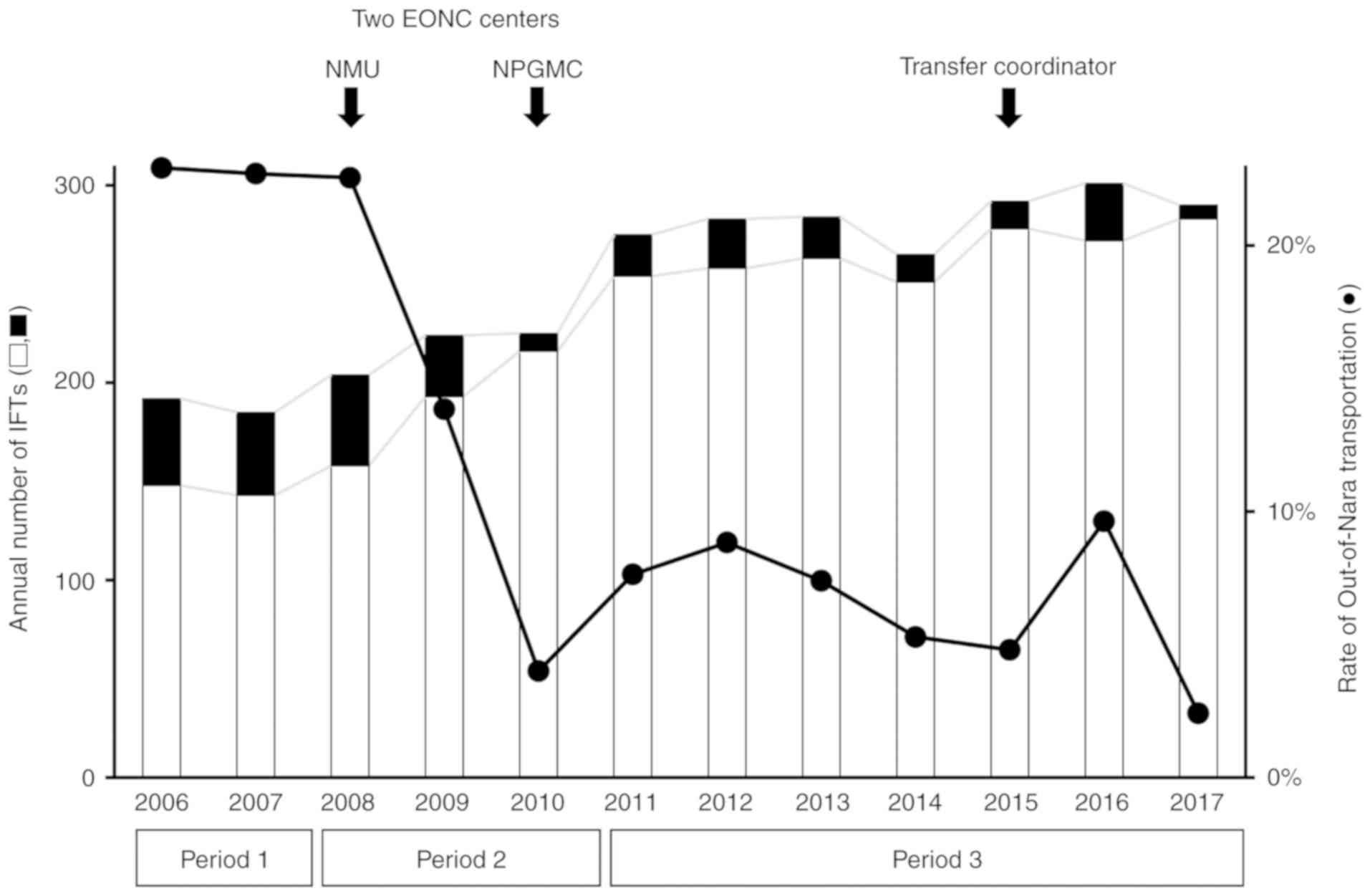
The patients were divided into three periods
according to the reorganization date as follows: Between 2006-2007
(before reorganization, Period 1), 2008-2010 (one reorganization,
Period 2) and between 2011-2017 (two reorganization and an
efficient coordination, Period 3). During Period 2, the NMU EONC
center officially commenced in order to improve the maternal and
neonatal care system. During Period 3, the NPGMC EONC center was
also officially commenced and IFTs were then timely coordinated by
a transfer operator who can identify a transfer destination.
Transfer coordinators would be required to keep the entire
management smooth and safe and facilitate prompt transfer to the
definitive destination avoiding delay at the emergency.
Data collection
All reporting data forms were completed by
obstetricians and midwives and mailed to the Board of the CPC
Committee on a yearly basis. The Committee members transferred the
data to an electronic database for future statistical evaluation.
The database was subsequently double checked to confirm whether
patients had been reported by both sending and receiving hospitals.
Any disagreements were resolved by confirming the ambulance call
log books and the electronic patient database at NMU and NPGMC
hospitals. Furthermore, data were independently extracted from the
paramedic and coordinator's reports for all IFTs. The IFT data and
reason for transfer were collected from the administrative database
operated by the CPC Committee. To assess the quality of medical
practice in Nara Prefecture, maternal and perinatal mortality was
confirmed from data provided by National Statistics Center
(https://www.e-stat.go.jp/).
Statistical analysis
To assess the impact of the newly established IFT
system, the number and rate of IFTs and Out-of-Nara transportation
were compared among the three periods. Analyses were performed
using commercially available software packages (SPSS Statistics for
Windows version 17.0; IBM Corp. and Medcalc for Windows version
11.4.2.0; Medcalc) (Stata version 16.0, StataCorp LLC, TX). Values
of P<0.05 were deemed to indicate statistically significant
differences. Linear regression analysis was used for the comparison
of differences in each data between each year and the three
periods.
Results
Information regarding the annual
number of obstetric units, obstetrician-gynecologists and NICU and
GCU beds
During the study period, 129,482 deliveries were
recorded in our database. There were approximately 10,000
deliveries per year (a maximum of 11,659 in 2006 and a minimum of
9,626 in 2017). The number of deliveries significantly decreased by
17.4% between 2006 and 2017 (P<0.0001). The annual numbers of
obstetric units, obstetrician-gynecologists and NICU and GCU beds
are presented in Table II. The
number of obstetric units in Nara Prefecture did not change between
2006 and 2017. The number of obstetrician-gynecologists increased
annually (P=0.0132) and between the three periods (P<0.0001).
The number of NICU and GCU beds increased annually (P=0.0149).
 | Table IIThe number of the patient transfers to
the EONC centers. |
Table II
The number of the patient transfers to
the EONC centers.
| | Period 1 | Period 2 | Period 3 | | |
|---|
| Year | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | Total | Significance |
|---|
| Population of Nara
Prefecture | 1,416,323 | 1,410,825 | 1,405,074 | 1,400,951 | 1,400,738 | 1,395,687 | 1,389,690 | 1,383,549 | 1,376,466 | 1,364,950 | 1,356,950 | 1,348,257 | 16,648,826 |
P<0.05a,b |
| Number of
deliveries | 11,659 | 11,456 | 11,224 | 10,898 | 11,164 | 10,995 | 11,021 | 10,752 | 10,257 | 10,414 | 10,016 | 9,626 | 129,482 |
P<0.05a,b |
| Number of IFTs | 192 | 185 | 204 | 224 | 225 | 275 | 283 | 284 | 265 | 292 | 301 | 290 | 3,020 |
P<0.05a,b |
|
Average on
Period (95% CI) | 188.5
(144.0-233.0) | 217.7
(188.2-247.1) | 284.3
(273.4-295.2) | | |
| Number of patients
transferred to facilities within Nara Prefecture | 148 | 143 | 158 | 193 | 216 | 254 | 25 | 263 | 251 | 278 | 272 | 283 | 2,717 |
P<0.05a,b |
|
The number
of patients transferred to NMU | 114 | 67 | 83 | 130 | 153 | 146 | 157 | 156 | 107 | 125 | 106 | 128 | 1,472 | n.s. |
|
Number of
patients transferred to NPGMC | 20 | 84 | 65 | 60 | 63 | 106 | 100 | 105 | 141 | 147 | 148 | 146 | 1,185 |
P<0.05a,b |
|
Number of
patients transferred to other facilities in Nara | 14 | 15 | 10 | 3 | 0 | 2 | 1 | 2 | 3 | 6 | 18 | 9 | 83 | n.s. |
| Number of
Out-of-Nara transfers | 44 | 42 | 46 | 31 | 9 | 21 | 25 | 21 | 14 | 14 | 29 | 7 | 155.4 |
P<0.05a |
|
Average on
Period (95% CI) | 43.0
(30.3-55.7) | 28.7
(-17.6-74.9) | 18.7
(11.8-25.6) | | |
| Out-of-Nara rate
(%) | 22.9 | 22.7 | 22.5 | 13.8 | 4.0 | 7.6 | 8.8 | 7.4 | 5.3 | 4.8 | 9.6 | 2.4 | 5.1 |
P<0.05a,b |
|
Average on
Period (95% CI) | 22.8
(21.5-24.2) | 13.5
(9.6-36.5) | 6.6 (4.2-8.9) | | |
| Number of obstetric
units (total) | 36 | 36 | 36 | 36 | 36 | 36 | 36 | 37 | 36 | 36 | 35 | 35 | | n.s. |
|
Prefectural-level
hospitals | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | | |
|
General
hospitals | 7 | 7 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 7 | 7 | 7 | | |
|
Primary
clinics | 17 | 17 | 18 | 18 | 18 | 18 | 18 | 19 | 19 | 17 | 16 | 16 | | |
|
Midwifery
homes | 8 | 8 | 9 | 9 | 9 | 9 | 9 | 9 | 8 | 8 | 8 | 8 | | |
| Number of
obstetrician-gynecologists of four prefectural-level hospitals
(total) | 31 | 35 | 40 | 39 | 40 | 43 | 43 | 44 | 44 | 43 | 46 | 49 | |
P<0.05a,b |
|
Nara Medical
University (NMU) | 12 | 15 | 20 | 19 | 21 | 22 | 22 | 24 | 22 | 22 | 25 | 25 | | |
|
Nara
Prefecture General Medical Center (NPGMC) | 6 | 7 | 7 | 7 | 7 | 9 | 9 | 9 | 10 | 10 | 10 | 12 | | |
|
Tenri
Hospital | 8 | 8 | 8 | 8 | 4 | 4 | 4 | 3 | 4 | 5 | 5 | 5 | | |
|
Kindai
University Nara Hospital | 5 | 5 | 5 | 5 | 8 | 8 | 8 | 8 | 8 | 6 | 6 | 7 | | |
| Number of NICU and
GCU beds (total) | 34 | 40 | 40 | 40 | 40 | 40 | 40 | 40 | 40 | 39 | 63 | 78 | |
P<0.05a |
|
Nara Medical
University (NMU) | 15 | 21 | 21 | 21 | 21 | 21 | 21 | 21 | 21 | 21 | 45 | 45 | | |
|
Nara
Prefecture General Medical Center (NPGMC) | 9 | 9 | 9 | 9 | 9 | 9 | 9 | 9 | 9 | 9 | 9 | 24 | | |
|
Kindai
University Nara Hospital | 10 | 10 | 10 | 10 | 10 | 10 | 10 | 10 | 10 | 9 | 9 | 9 | | |
| Number of maternal
deaths | 2 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 2 | 0 | 0 | 6 | n.s. |
|
Perinatal
mortality rate (per 1,000 births) | 6.2 | 4.2 | 5.5 | 5.2 | 3.3 | 5.1 | 3.3 | 4.4 | 3.8 | 5.2 | 3.7 | 4.7 | | |
|
Average on
Period (95% CI) | 5.2
(-7.5-17.9) | 4.7 (1.7-7.6) | 4.3 (3.6-5.0) | | |
| Incidence of
prolonged mechanical ventilation (%) | ND | 38.2 | 44.8 | 47.1 | 49.5 | 44.3 | 48.7 | 43 | 54.1 | 56.9 | 37.5 | 23 | | n.s. |
|
Average on
Period (95% CI) | 38.2 | 47.1
(41.3-53.0) | 43.9
(33.4-54.4) | | |
The annual number of IFTs from the
referring facilities to EONC centers
The CPC Committee databases (2006-2017) were used to
identify an annual trend analysis of the IFTs and Out-of-Nara
transfer. The number of deliveries significantly decreased by 17.4%
between 2006 and 2017 (P<0.0001). The number of the patient
transfers to the EONC centers is presented in Table II and Fig. 2. Among a total of 129,482
deliveries, 3,020 were transferred to the EONC centers (2.33%). Of
the 3,020 IFTs, 1,472 (48.7%) and 1,185 (39.2%) patients were
transferred to NMU and NPGMC, respectively. The annual IFT number
and rate increased from 192 (1.6%) per 11,659 deliveries in 2006 to
290 (3.0%) per 9,626 deliveries in 2017 (P<0.0001), resulting in
a 82.4% increase in the number of cases. The patients were divided
into three periods to assess the effects of these organizational
changes on IFTs. The number of IFTs significantly increased from
188.5 cases (95% CI, 144.0-233.0) per year in Period 1 to 217.7
cases (188.2-247.1) in Period 2 and 284.3 cases (273.4-295.2) in
Period 3 (P<0.0001).
Out-of-Nara transfer rates
There was a marked decrease in the incidence of the
Out-of-Nara transfer, ranging from 22.9% in 2006 to 2.4% in 2017
(10.0% per year on average, P=0.0057). The annual IFT rate of the
Out-of-Nara transfer decreased by 89.6% between 2006 (22.9%) and
2017 (2.4%, P=0.0011). The medical coverage of complicated
obstetric cases at the EONC centers was estimated to be 77.1%
(148/192) in 2006 and 97.6% (283/290) in 2017. A significant
decrease in the Out-of-Nara transfer rate was shown from 22.8% (95%
CI, 21.5-24.2) in Period 1 to 13.5% (9.6-36.5) in Period 2 and 6.6%
(4.2-8.9) in Period 3 (P=0.0065).
Top reasons for IFTs
The most common reasons for IFTs to the EONC centers
were preterm labor (36.7%), followed by premature rupture of
membranes (PROM) (20.0%), hypertensive disorders of pregnancy (HDP)
(8.7%), postpartum hemorrhage (PPH) (8.3%), placental abruption
(4.0%) (Table III).
 | Table IIIMain reasons for patient transfer to
the EONC centers, Nara prefecture, Japan. |
Table III
Main reasons for patient transfer to
the EONC centers, Nara prefecture, Japan.
| Reasons for patient
transfer | n 3,043 | (%) (100) |
|---|
| Preterm labor | 1,118 | (36.7) |
| PROM | 609 | (20.0) |
| HDP | 265 | (8.7) |
| PPH | 254 | (8.3) |
| Placental
abruption | 123 | (4.0) |
| Placenta
previa | 89 | (2.9) |
| Non-reassuring
fetal status | 69 | (2.3) |
| FGR | 58 | (1.9) |
| HELLP syndrome | 51 | (1.7) |
| Pregnant women
without antenatal health care | 35 | (1.2) |
| Threatened
abortion | 23 | (0.8) |
| Others | 349 | (11.5) |
Maternal and perinatal mortality
In addition, we estimated the annual change in
incidence of maternal and perinatal outcomes before and after the
reorganization of the EONCs. We queried the CPC Committee registry
for the medical records of maternal death, perinatal mortality, and
adverse clinical outcomes, including NICU length of stay, the need
for inotropes and prolonged mechanical ventilation. It was found
that maternal death (P=0.926), perinatal mortality rate (P=0.947)
and adverse clinical outcomes (P=0.518) between 2006-2017 did not
change prior to and after the reorganization (Table II). Six maternal deaths were
registered in 2006 (n=2, postpartum hemorrhage and dilated
cardiomyopathy), 2012 (n=2, Group A streptococcal infection and
malignant lymphoma), and 2015 (n=2, brain stroke and aortic
dissection), respectively. Since maternal mortality was rare
throughout the period studied, no association was observed between
maternal mortality and vehicle-dispatch data. Furthermore, the
perinatal mortality rate exhibited no significant difference
between the periods studied [Period 1, 5.2 (95% CI, -7.5-17.9);
Period 2, 4.7 (1.7-7.6); and Period 3, 4.3 (3.6-5.0)]. We finally
investigated adverse clinical outcomes of the deliveries prior to
and after the reorganization. Both NICU length of stay and duration
of mechanical ventilation may be associated with a trend towards
neonatal mortality and morbidity. The duration of mechanical
ventilation, but not the NICU length of stay, was recorded in the
CPC committee database. The incidence of prolonged mechanical
ventilation was unchanged before and after the reorganization.
Discussion
In this study, a prefecture-based observational
study was conducted for a period of 12 years. This study assessed
the impact of the newly established IFT system and medical coverage
of complicated obstetric cases at two EONC centers. The timespan
was divided into three periods (before reorganization, one
reorganization and two reorganizations). The IFT rate significantly
increased from 1.7% (Period 1) to 2.4% (Period 2) and finally to
2.9% (Period 3) (P<0.0001). In contrast to these changes, the
Out-of-Nara transfer rate significantly declined from 22.7% (Period
1) to 7.8% (Period 2) and finally to 5.7% (Period 3) (P=0.0065).
The key findings of this study were as follows: i) The IFT rates
significantly increased over the study period; and ii) the
Out-of-Nara transfer rate markedly declined after the
reorganization of the EONC centers. The combination of the
reorganization of the EONC centers and the implementation of an
emergency referral network, including an efficient coordination
using telephone-based services by a transfer coordinator and an
effective communication, can facilitate the IFTs of women who
urgently require emergency obstetric care.
First, we highlight serious social and medical
issues related to emergency obstetric care and some of the
important factors to significantly reduce the number of the
Out-of-Nara transfer. Japan now faces serious medical issues,
including a shortage of physicians, an increase in the number of
females entering medicine and physician maldistribution between
medical departments (9). The
number of OB/GYN physicians, obstetricians and gynecologists, is
specifically decreasing. Furthermore, emerging evidence indicates
an increase in the incidence of obstetric complications in recent
years (2). The recent trend of
delayed parenthood and the associated use of assisted reproductive
technologies (ARTs) have led to the increased risk of obstetric
complications (4). There has been
an increase in the number of high-risk pregnant women who have
their first baby at an age >35 years. Other risk factors include
not only in vitro fertilization and embryo transfer
(IVF-ET), but also a pre-pregnancy BMI ≥30 kg/m2 or
<18 kg/m2, or a family history of hypertension or
diabetes (2).
The government has accelerated the selection and
concentration of obstetric facilities to cope with workforce
shortages and excessive workloads, including transfer or relocation
of services from one health care sector to EONC centers.
Policy-makers are facing acute shortages of obstetricians needed to
provide improved EONC services. Since 2007, the Japan Society of
Obstetrics and Gynecology (JSOG) created actionable recommendations
to implement the innovative and community relevant interventions
called the ‘selection and concentration’ of obstetric facilities
(8-10).
This was a political issue, in which the reorganization of the EONC
center should be considered to reduce the increased workload of
obstetricians, increase job satisfaction and improve maternal and
neonatal outcomes. Considering the fact that health workforce
shortage and increasing complicated delivery in Japan, the
reorganization of EONC facilities could be a possible policy
option. Two EONC centers (NMU in 2008 and NPGMC in 2010) were newly
reorganized in Nara Prefecture and staffed by specialists. In
almost one decade, larger and multispecialty groups have been
reorganized through the selection, integrated arrangements and
concentration of obstetric facilities. The reorganization has
overcome accessibility of complicated obstetric cases and emergency
care for women with obstetric and neonatal disabilities in the
referring facilities. Therefore, both a resolution of a shortage of
obstetricians with increased workload and the increased number of
EONC beds may have a positive impact on the decreased Out-of-Nara
transfer rate.
Second, perinatal emergencies remain a challenging
burden on emergency department staff (11-14).
IFTs may be a useful option to ensure a higher level of care than
that which is available at the referring clinic or hospital. The
CPC Committee held a series of meetings to implement a plan for
coordinating the care of high-risk pregnancies with emergency
obstetric conditions. An obstetric emergency care coordinator can
quickly assess the limitations of each facility and acceptance, and
can properly determine ENOC center suitable for a patient's
condition, allowing information to be shared among obstetricians
and neonatologists. Our policy is that ensuring an uneventful IFT
will prepare prompt arrangement of transport for the patient and
reduce delays in access to the EONC centers. Neither pregnant women
nor their families denied to be transferred to the EONC centers.
During Period 3, IFTs were carried out by a transfer coordinator
through an agreement between the NMU hospital and the CPC Committee
under a relational contract with the government. A modest
investment in the transfer coordination may reduce the
obstetrician's burden. Task shifting by a transfer coordinator is a
potential strategy to improve access to the EONC centers and
actualize the smooth management of the IFT system. This clinical
innovation may involve a sustainable change in the clinical
practice of emergency medicine, particularly in countries now
facing serious medical issues, such as a shortage of
obstetricians.
Third, the most common cause for IFTs was preterm
labor (37.0%), followed by premature rupture of membranes (PROM)
(20.2%), hypertensive disorders of pregnancy (HDP) (8.8%),
postpartum hemorrhage (PPH) (8.4%), placental abruption (4.0%).
Preterm delivery is considered to be the leading cause of neonatal
mortality and morbidity worldwide (3). Its prevention is an important
healthcare priority, but has been long-standing challenges. Since
neonatal outcomes are better for expectant mother transferred in
utero than those transferred ex utero (neonates), women
with pregnancy complications, including preterm birth, should be
transferred to the EONC centers as an in utero transfer
(15). In addition, we estimated
the annual change in incidence of the maternal death, perinatal
mortality rate and adverse clinical outcomes, including prolonged
mechanical ventilation, before and after the reorganization of the
EONCs. However, the timely response for emergency IFTs was not
associated with improved maternal-fetal outcomes. Due to the
increase in preterm delivery for maternal or fetal indications,
including preeclampsia or eclampsia, and intrauterine growth
restriction, premature infants may require longer positive pressure
ventilation.
Finally, we sought to identify other factors that
may have influenced the results of this study: For example, the
establishment of new hospitals inside Nara Prefecture,
transportation system changes (the spatiotemporal changes of new
expressway network), and changes in the criteria for
transportation. Nationwide, the number of obstetrics facilities
decreased during the study period. It is commonly believed that the
improvement of the expressway network exerts more widespread
influences on the emergency transportation. However, there were no
expressway infrastructure development plans in Nara Prefecture
throughout the study period. Furthermore, the IFT rate varies
according to the criteria for ambulance referrals to EONC centers
of women at risk of or with an obstetric complication. All of the
women who met these criteria in this study are shown in Table I. Therefore, it can be concluded
that the reorganization may be a primary factor of this change.
In conclusion, the findings of this study
demonstrate that i) progression of the selection, concentration and
intensification of obstetrics facilities may reduce the Out-of-Nara
transfer and acceptable referral coverage of complicated obstetric
cases; and that ii) transfer coordination by an IFT operator who
can quickly identify a transfer destination may provide an
effective doctor-to-doctor communication between referring
facilities and referred facilities.
In this study, we only analyzed the time trend data
based on the CPC Committee database and did not assess whether the
availability of the EONC centers is associated with an improved
outcome of severe obstetric complications, which may be a main
limitation of this study. Furthermore, this study did not evaluate
the quality of life and job satisfaction in obstetricians of
referring facilities and referred facilities. Koike et al
reported that the selection, concentration and intensification of
obstetrics facilities in fewer hospitals impairs patient access,
but EONC centers had a greater annual caseload and better staffing
than did those at non-specialized centers, which has the potential
advantages of better clinical outcomes (16). Further studies are required to
synthesize evidence regarding maternal and neonatal deaths, as well
as comprehensive outcome measurements, including an improvement of
quality of life of medical professionals.
In conclusion, the combination of reorganization of
two emergency obstetric and neonatal care (EONC) centers and
implementation of an efficient coordination by a transfer operator
is imperative for the successful management of interfacility
transfers (IFTs) in Nara Prefecture, Japan.
Acknowledgements
The authors acknowledged members of the CPC
Committee, Nara Prefecture Government, including Toshiya Nishikubo
(Department of Neonatology, Nara Medical University), Tsunekazu
Kita (Department of Obstetrics and Gynecology, Nara Prefecture
General Medical Center Hospital), Hideki Minowa (Department of
Neonatology, Nara Prefecture General Medical Center Hospital),
Naoya Harada (Department of Obstetrics and Gynecology, Nara City
Hospital), Kiyoshi Fujiwara (Department of Obstetrics and
Gynecology, Tenri Hospital), Hidekazu Oi (Department of Obstetrics
and Gynecology, Kindai University Nara Hospital), Junji Tanji and
Takao Sanai (Nara Wide Area Fire Department) and Syuichiro Hayashi
(Welfare and Medical Department, Nara Prefectural Government). HK
and MA are members of the CPC Committee, Nara Prefecture
Government.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
TT, JA and KN collected data regarding the recent
trend of obstetric complications using the PubMed database. TS and
KN collected data regarding the number of the patient transfers to
the EONC centers and the Out-of-Nara transfer using the CPC
committee database and nation data in the vital statistics in
Japan. HK and MA contributed to the conception, design and
interpretation of this study. HK wrote the first draft of the
manuscript. The final version of the manuscript has been read and
approved by all authors.
Ethics approval and consent to
participate
This study was approved by the CPC Committee.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Hasegawa J, Ikeda T, Sekizawa A, Tanaka H,
Nakamura M, Katsuragi S, Osato K, Tanaka K, Murakoshi T, Nakata M
and Ishiwata I: Maternal Death Exploratory Committee in Japan and
the Japan Association of Obstetricians and Gynecologists:
Recommendations for saving mothers' lives in Japan: Report from the
maternal death exploratory committee (2010-2014). J Obstet Gynaecol
Res. 42:1637–1643. 2016.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Muto H, Yamamoto R, Ishii K, Kakubari R,
Takaoka S, Mabuchi A and Mitsuda N: Risk assessment of hypertensive
disorders in pregnancy with maternal characteristics in early
gestation: A single-center cohort study. Taiwan J Obstet Gynecol.
55:341–345. 2016.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Wang ML, Dorer DJ, Fleming MP and Catlin
EA: Clinical outcomes of near-term infants. Pediatrics.
114:372–376. 2004.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Johnson B and Chavkin W: Policy efforts to
prevent ART-related preterm birth. Matern Child Health J.
11:219–225. 2007.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Nair M, Kurinczuk JJ, Brocklehurst P,
Sellers S, Lewis G and Knight M: Factors associated with maternal
death from direct pregnancy complications: A UK national
case-control study. BJOG. 122:653–662. 2015.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Hasegawa J, Sekizawa A, Tanaka H,
Katsuragi S, Osato K, Murakoshi T, Nakata M, Nakamura M, Yoshimatsu
J, Sadahiro T, et al: Current status of pregnancy-related maternal
mortality in Japan: A report from the maternal death exploratory
committee in Japan. BMJ Open. 6(e010304)2016.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Ide H, Yasunaga H, Kodama T, Koike S,
Taketani Y and Imamura T: The dynamics of obstetricians and
gynecologists in Japan: A retrospective cohort model using the
nationwide survey of physicians data. J Obstet Gynaecol Res.
35:761–766. 2009.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Japan Society of Obstetrics and
Gynecology: Grand design 2015 (GD2015) renovation of the obstetrics
and gynecology healthcare system in Japan. Japan Society of
Obstetrics and Gynecology, Tokyo, 2015. http://shusanki.org/index.html.
Accessed April 20, 2019.
|
|
9
|
Ishikawa T, Ohba H, Yokooka Y, Nakamura K
and Ogasawara K: Forecasting the absolute and relative shortage of
physicians in Japan using a system dynamics model approach. Hum
Resour Health. 11(41)2013.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Matsumoto M, Koike S, Matsubara S, Kashima
S, Ide H and Yasunaga H: Selection and concentration of obstetric
facilities in Japan: Longitudinal study based on national census
data. J Obstet Gynaecol Res. 41:919–925. 2015.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Wiegers TA and de Borst J: Organisation of
emergency transfer in maternity care in the Netherlands. Midwifery.
29:973–980. 2013.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Eckstein M, Schlesinger SA and Sanko S:
Interfacility transports utilizing the 9-1-1 emergency medical
services system. Prehosp Emerg Care. 19:490–495. 2015.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Tayler-Smith K, Zachariah R, Manzi M, Van
den Boogaard W, Nyandwi G, Reid T, De Plecker E, Lambert V, Nicolai
M, Goetghebuer S, et al: An ambulance referral network improves
access to emergency obstetric and neonatal care in a district of
rural Burundi with high maternal mortality. Trop Med Int Health.
18:993–1001. 2013.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Wu O, Briggs A, Kemp T, Gray A, MacIntyre
K, Rowley J and Willett K: Mobile phone use for contacting
emergency services in life-threatening circumstances. J Emerg Med.
42:291–298.e3. 2012.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Chien LY, Whyte R, Aziz K, Thiessen P,
Matthew D and Lee SK: Canadian Neonatal Network: Improved outcome
of preterm infants when delivered in tertiary care centers. Obstet
Gynecol. 98:247–252. 2001.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Koike S, Matsumoto M, Ide H, Kashima S,
Atarashi H and Yasunaga H: The effect of concentrating obstetrics
services in fewer hospitals on patient access: A simulation. Int J
Health Geogr. 15(4)2016.PubMed/NCBI View Article : Google Scholar
|