Introduction
Endoscopic retrograde cholangiopancreatography
(ERCP) is widely performed as the diagnostic and therapeutic tool
intended for patients with pancreato-biliary diseases. The
frequency of ERCP for elderly patients is increasing in accordance
with the overall aging of the population worldwide (1). To date, ERCP has been known to be
associated with severe adverse events, such as pancreatitis,
gastrointestinal bleeding and perforation (1). Although it has been reported that
ERCP can be safely performed in elderly patients (2-6),
the clinical status of these patients varies due to comorbidities,
nutritional status, cognition, etc., which causes endoscopists to
debate whether or not ERCP should be performed. The Eastern
Cooperative Oncology Group (ECOG) scale of performance status (PS)
is widely used for the quantification of the general well-being and
daily life activities of patients (7). Elderly patients with a decreased PS
are a high-risk group, and the efficacy and safety of ERCP for
these patients is unclear. Thus, the aim of this study was to
elucidate the efficacy and safety of ERCP in elderly patients with
a PS of 3-4, compared to those with a PS of 0-2, hospitalized in
Saiseikai Chuwa Hospital.
Patients and methods
Study design
The present study was conducted at Saiseikai Chuwa
Hospital, Sakurai, Nara, Japan. This hospital is located in a rural
district in Nara, and the average age of patients in this area is
very high. The records of the patients, who underwent ERCP in this
facility from April, 2017 to April, 2018, were retrospectively
analyzed. In total, 146 patients (232 procedures) underwent ERCP,
patients aged <75 years were excluded, and 94 patients (158
procedures) were enrolled in this study. The patients were divided
into the PS 0-2 group and PS 3-4 group. For both groups, clinical
characteristics were analyzed, such as age, sex, PS, primary
disease for ERCP, the prevalence rate of moderate or severe
cholangitis [assessed by the severity assessment of acute
cholangitis per the Tokyo Guidelines 13 (TG13) (8)], the use of antithrombotic drugs,
history of gastrectomy and the Charlson comorbidity index (CCI)
(9), which is a weighted index
that assigns a different risk score (from 1 to 6) to 22 conditions
and their related relative risk of 1-year mortality. Clinical
outcomes were analyzed, such as performed procedures, the number of
ERCPs for each patient, the technical success rate, adverse events
caused by ERCPs, admission periods and fatal cases occurred within
30 days following ERCP.
Procedures
In the facility, 5 gastroendoscopists performed
ERCP. All ERCP procedures were performed by one operator and at
least one assistant among 5 gastroendoscopists. A rule was
established to complete the ERCP procedures within 1 h from scope
insertion for all patients, as the ERCP procedure bears the risk of
adverse events, such as pancreatitis, even when performed by
endoscopic specialists, and it is estimated that a lengthy
procedure bears the risk of adverse events following ERCP.
According to the TG13 flowchart (10), not all procedures are performed in
a single session for patients with moderate or severe cholangitis.
In the first session, only endoscopic drainage was performed,
followed, after the improvement of cholangitis, by other procedures
such as endoscopic lithotomy. The TJF-260V (Olympus Medical Systems
Co.) and ED-450XL8/B (FUJIFILM Co.) endoscopes were used, and for
patients who had Billroth II or Roux-en Y reconstructions, the
SIF-H290S (Olympus Medical Systems Co.) was used, which is a
short-type single-balloon-assisted endoscope useful for ERCP in
patients with altered gastrointestinal anatomy (11). For all procedures, carbon dioxide
(CO2) insufflation was used during ERCP to reduce
post-procedural pain and abdominal distension (12,13). For the purposes of sedation during
ERCP, midazolam and pentazocine were used, monitoring vital signs
and the degree of sedation, all the while increasing the sedation
if necessary.
Definition
The PS score (7)
was labeled according to information on the general status prior to
admission.
Severity assessment of
cholangitis
The severity of cholangitis was assessed by the
severity assessment of acute cholangitis as per the Tokyo
Guidelines 2013(8). The adverse
events caused by ERCP procedures are defined as follows: i)
Pancreatitis: The onset of new abdominal pain with at an least
3-fold elevation of serum amylase levels following ERCP; ii)
hyperamylasemia: At least a 3-fold elevation of serum amylase
levels following ERCP, without abdominal pain; and iii) biliary
infection, including cholangitis, cholecystitis and liver abscess.
The onset of the adverse events was evidenced after the ERCP
procedures and did not exist before the ERCP procedures. Liver
dysfunction is defined as the elevation of L-aspartate
aminotransferase (AST) and L-alanine aminotransferase (ALT) that
were at normal levels before the ERCP procedures and were found to
be above normal levels after the ERCP procedures in the absence of
any other cause. Mallory-Weiss syndrome is defined as the
laceration of gastroesophageal junction caused by nausea or
vomiting with or following ERCP procedures.
Statistical analysis
Comparisons between the study groups were performed
with the Wilcoxon signed-rank test for quantitative variables and
the Chi-square test for qualitative variables. A P-value <0.05
was considered to indicate a statistically significant difference.
All statistical analyses were performed using IBM SPSS statistics
version 22 (IBM Corp.).
Results
Clinical characteristics
The clinical characteristics of the patients in both
groups are presented in Table I.
A total of 94 patients (158 procedures) who were over 75 years old
and underwent ERCP were divided into 2 groups as follows: The PS
0-2 group with 73 patients (116 procedures), and the PS 3-4 group
with 21 patients (42 procedures). The average age did not differ
significantly between the 2 groups. The ERCP rate in females was
significantly higher in the PS 3-4 group than in the PS 0-2 group.
The numbers of patients for each PS were 31 for PS 0, 36 for PS 1,
6 for PS 2, 4 for PS 3 and 17 for PS 4. Of note, the prevalence
rates of moderate or severe cholangitis and the CCI were
significantly higher in the PS 3-4 group than in the PS 0-2 group.
The rate of anti-thrombotic drug use did not differ between the
groups. In the PS 0-2 group, 9 patients had undergone gastrectomy
(3 patients with Billroth I reconstruction, 3 patients with
Billroth II reconstruction and 3 patients with Roux-en-Y
reconstruction); however, in the PS 3-4 group, no patients had
undergone gastrectomy. In both groups, no patients had undergone
pancreaticoduodenectomy or choledochojejunostomy. The majority of
the indications for ERCP in both groups were choledocholithiasis
and malignant biliary obstruction (Table II).
 | Table IBaseline characteristics in elderly
patients with both PS 0-2 and 3-4. |
Table I
Baseline characteristics in elderly
patients with both PS 0-2 and 3-4.
| Variable | All patients (94
patients, 158 procedures) | PS 0-2 group (73
patients, 116 procedures) | PS 3-4 group (21
patients, 42 procedures) | P-value |
|---|
| Age, median
(range) | 84 (75-98) | 84 (75-96) | 86 (78-98) | N.S. |
| Sex, rate of female
(%) | 52.1 | 43.8 | 80.9 | P=0.003 |
| Performance status,
0/1/2/3/4 | 31/36/6/4/17 | 31/36/6/0/0 | 0/0/0/4/17 | - |
| Prevalence rate of
moderate or severe cholangitis, n (%) | 29 (30.9) | 14 (19.1) | 15 (71.4) | P<0.001 |
| Charlson comorbidity
index, median (range) | 1 (0-7) | 1 (0-7) | 2 (1-3) | P=0.001 |
| Antithrombotic drug
therapy, n (%) | 34 (36.2) | 28 (38.4) | 6 (28.6) | N.S. |
| Altered
gastrointestinal anatomy, Billroth I, II, Roux-en-Y | 3/3/3 | 3/3/3 | 0/0/0 | - |
 | Table IIIndications for ERCP in elderly
patients with both PS 0-2 and 3-4. |
Table II
Indications for ERCP in elderly
patients with both PS 0-2 and 3-4.
| Variable | All patients (94
patients, 158 procedures) | PS 0-2 group (73
patients, 116 procedures) | PS 3-4 group (21
patients, 42 procedures) | P-value |
|---|
| Choledocholithiasis,
n (%) | 56 (59.6) | 46 (63.0) | 10 (47.6) | N.S. |
| Malignant biliary
obstruction, n (%) | 32 (34.0) | 24 (32.9) | 8 (38.1) | N.S. |
| Gallstone
pancreatitis, n (%) | 2 (2.1) | 0 (0.0) | 2 (9.5) | N.S. |
| Lemmel syndrome, n
(%) | 1 (1.1) | 0 (0.0) | 1 (4.8) | N.S. |
| Others, n (%) | 3 (3.2) | 3 (4.1) | 0 (0.0) | N.S. |
ERCP results
The ERCP results for both groups are presented in
Tables III-V. The performed procedures did not differ in either
group. In particular, endoscopic biliary stent (EBS) and endoscopic
lithotomy were frequently observed (Table III). Patients in the PS 3-4
group required frequent ERCP for one primary disease and longer
admission periods (Table V). The
reason was that patients in the PS 3-4 group had a higher
prevalence rate of moderate or severe cholangitis (Table I). Only biliary drainage was
performed for the first procedure, and other procedures such as
endoscopic lithotomy were performed following the improvement of
cholangitis. Moreover, a number of patients in the PS 3-4 group
were often discharged to the nursing facility. Thus, several
procedures and the adjustment of the discharge schedule required
longer admission periods. Subsequently, the technical success rate
for planned procedures was adequately high in both groups. There
were no cases that required the suspension of ERCP procedures due
to hypotension, bradycardia or respiratory depression caused by
oversedation. In the PS 3-4 group, all planned procedures were
completed (Table V). However, in
the PS 0-2 group, 5 cases failed to achieve bile duct or pancreatic
duct cannulation at the first ERCP. However, 3 cases were
completely successful at the second ERCP, and 2 cases were changed
to perform procedures under a non-endoscopic approach. One case
after Roux-en-Y reconstruction failed to reach the papilla of
Vater. Finally, the rate of adverse events caused by ERCP
procedures did not differ significantly in both groups (Table IV). There were no severe adverse
events, such as perforation and bleeding, which required endoscopic
hemostasis or blood transfusion. Although 5 cases of
post-ERCP-pancreatitis were observed only in the PS 0-2 group, they
were improved only by conservative therapy. Despite the rate of
adverse events by ERCP procedures not differing in both groups,
there were 2 fatal cases during the 30 days following ERCP in the
PS 3-4 group and no fatal cases in the PS0-2 group (Table V). The two fatal cases during 30
days following ERCP were the following.
 | Table IIIERCP procedures in elderly patients
with both PS 0-2 and 3-4. |
Table III
ERCP procedures in elderly patients
with both PS 0-2 and 3-4.
| Variable | All patients (94
patients, 158 procedures) | PS 0-2 group (73
patients, 116 procedures) | PS 3-4 group (21
patients, 42 procedures) | P-value |
|---|
| Endoscopic biliary
stent (EBS), n (%) | 69 (43.7) | 51(44.0) | 18 (42.9) | N.S. |
| Endoscopic
nasobiliary drainage (ENBD), n (%) | 6 (3.8) | 5 (4.3) | 1 (2.4) | - |
| Self expandable
metalic stent (SEMS), n (%) | 12 (7.6) | 9 (7.8) | 3 (7.1) | - |
| Endoscopic
sphincterotomy (EST), n (%) | 55 (34.8) | 40 (34.5) | 15 (35.7) | - |
| Endoscopic papillary
large balloon dilation (EPLBD), n (%) | 11 (7.0) | 8 (6.9) | 3 (7.1) | - |
| Endoscopic lithotomy,
n (%) | 58 (36.7) | 39 (33.6) | 19 (45.2) | - |
| SEMS cleaning, n
(%) | 2 (1.3) | 1 (0.9) | 1 (2.4) | - |
 | Table VPost-ERCP outcomes in elderly
patients with both PS 0-2 and 3-4. |
Table V
Post-ERCP outcomes in elderly
patients with both PS 0-2 and 3-4.
| Variable | All patients (94
patients, 158 procedures) | PS 0-2 group (73
patients, 116 procedures) | PS 3-4 group (21
patients, 42 procedures) | P-value |
|---|
| Numbers of ERCP for
one patient, average (range) | 1.7 (1-4) | 1.6 (1-4) | 2.0 (1-4) | P=0.003 |
| Admission period
(days), median (range) | 17 (4-98) | 15 (4-80) | 23 (10-98) | P<0.001 |
| Technical Success
Rate, % | 96.2 | 94.8 | 100 | N.S. |
| Fatal case in 30
days following ERCP, n | 2 | 0 | 2 | N.S. |
 | Table IVPost-ERCP complications in elderly
patients with both PS 0-2 and 3-4. |
Table IV
Post-ERCP complications in elderly
patients with both PS 0-2 and 3-4.
| Variable | All patients (94
patients, 158 procedures) | PS 0-2 group (73
patients, 116 procedures) | PS 3-4 group (21
patients, 42 procedures) | P-value |
|---|
| Total, n (%) | 25 (15.8) | 19 (16.4) | 6 (14.3) | N.S. |
| Pancreatitis, n
(%) | 5 (3.1) | 5 (4.3) | 0 (0.0) | - |
| Hyperamylasemia, n
(%) | 14 (8.9) | 10 (9.5) | 4 (9.5) | - |
| Biliary infection, n
(%) | 2 (1.3) | 1 (0.9) | 1 (2.4) | - |
| Liver dysfunction,
n (%) | 3 (1.9) | 3 (2.6) | 0 (0.0) | - |
| Mallory-Weiss
syndrome, n (%) | 1 (0.6) | 0 (0.0) | 1 (2.4) | - |
| Perforation, n
(%) | 0 (0.0) | 0 (0.0) | 0 (0.0) | - |
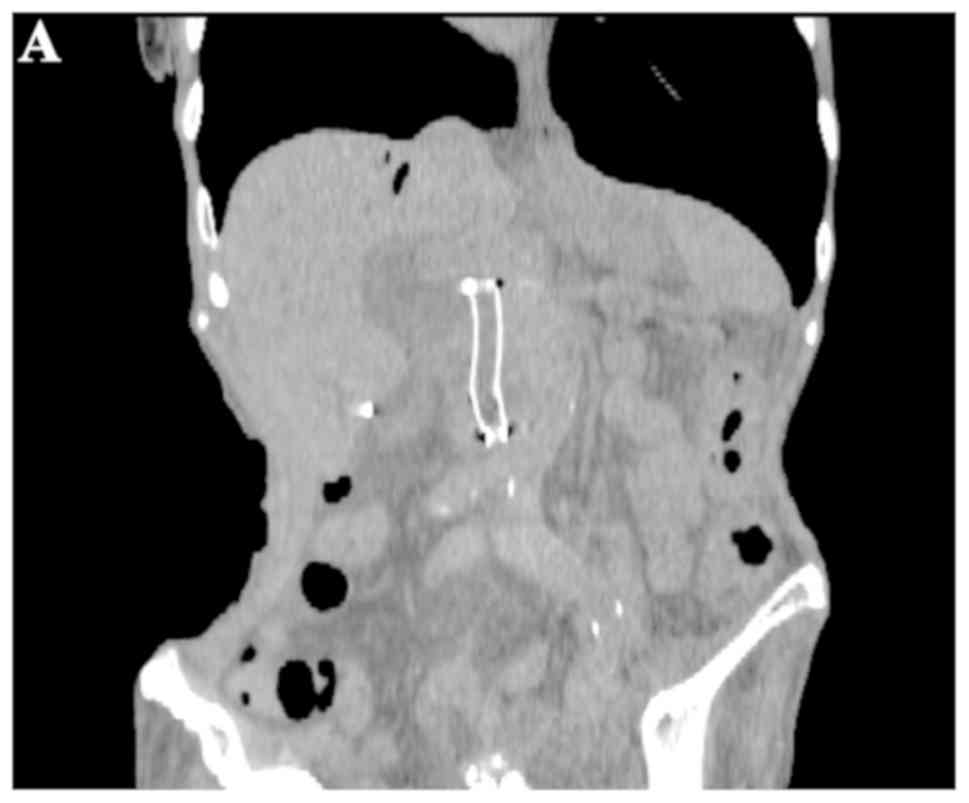
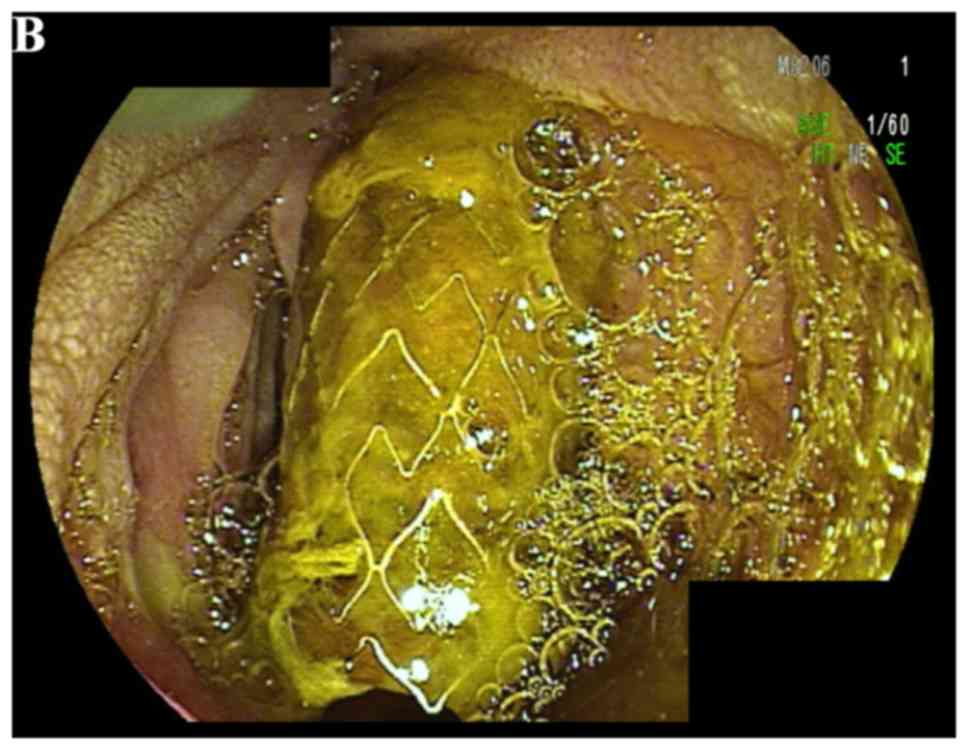
i) Case A: An 86-year-old female with PS 4
underwent placement of a covered-type self-expandable metallic
stent (SEMS) for biliary obstruction with pancreatic cancer. After
1 month of ERCP, she was admitted to the hospital for cholangitis
due to SEMS obstruction. She then underwent SEMS cleaning and
improved. However, she was readmitted for cholangitis due to a
recurrence of SEMS obstruction (Fig.
1A). The prolapsed, obstructed SEMS (Fig. 1B) was removed and replaced by an
EBS (Fig. 1C). Subsequently,
although cholangitis was improved, her general condition gradually
worsened due to anorexia caused by pancreatic cancer. As a result,
she died 26 days after ERCP.
ii) Case B: A 98-year-old male with PS 4
underwent placement of EBS for biliary obstruction with pancreatic
cancer (Fig. 2A). At 10 days
after ERCP, cholangitis with EBS obstruction occurred; The EBS
(across the papilla) was replaced with the plastic stent inside
[i.e., above the papilla (Fig.
2B, arrowheads)], and the cholangitis gradually improved.
However, at 10 days following stent replacement, he experienced a
hospital-acquired influenza infection. Thus, his general condition
worsened and he died 14 days after ERCP.
Discussion
The present study had two findings. First, ERCP for
elderly patients with a PS of 3-4, which is the highest risk group,
is effective and safe. Second, ERCP in elderly patients with a PS
of 3-4 may result in a fatal outcome caused by incidents unrelated
to the ERCP procedure.
As regards the first finding, as noted above, ERCP
for elderly patients with a PS of 3-4, which is the highest risk
group, is effective and safe. While ERCP is a useful procedure for
the diagnosis and therapy of pancreatic and biliary disease
(14), adverse events of ERCP
procedures, such as pancreatitis occasionally result in a fatal
outcome. Thus, ERCP procedures for high-risk patients should be
performed carefully. It is important to estimate preprocedural risk
factors accurately by means of objective clinical tools, applied to
elderly patients with comorbidity and possible procedure-related
adverse events, to produce satisfactory clinical ERCP outcomes
(15). Previously, a number of
studies have reported the safety and efficacy of ERCP for elderly
patients (2-6).
However, it is estimated that the risk factor for ERCP for elderly
patients is not only age, but also other clinical conditions. From
a geriatric perspective, the assessment of older patients is an
interdisciplinary process that should include multiple domains,
such as functional and nutritional status, cognition, the accurate
evaluation of comorbidity and many others (16). Thus, the assessment of the risk of
elderly patients is more complex. Park et al (17) reported that the Duke Activity
Status Index (DASI) is a useful predictor for overall serious
events related to ERCP. DASI is a valid measure of functional
capacity that can be obtained by answering a self-administered
questionnaire (18). However, the
calculation of DASI is known to be complex. Therefore, an easier
index is preferable for the determination of emergent ERCP
procedure indications. In the present study, the classification
from the Eastern Cooperative Oncology Group (ECOG) PS score was
used. The ECOG PS score is a simple and easy method used for the
assessment of general well-being, activities of daily life, and
tolerance for therapy (7).
Elderly patients with depressed PS are considered to be perhaps the
highest truly risk group because of the higher prevalence rate of
moderate to severe cholangitis and higher CCI, as described later.
To our knowledge, this is the first study on the safety and
efficacy of ERCP for elderly patients between good and depressed PS
groups. The present study indicated that ERCP is effective and safe
even for elderly patients with PS 3-4.
As regards the second finding, ERCP in elderly
patients with a PS of 3-4 may result in a fatal outcome caused by
incidents unrelated to the ERCP procedure. In the present study, 2
fatal cases occurred during the 30 days following ERCP in the PS
3-4 group, whereas no fatal cases occurred in the PS 0-2 group. One
patient's condition was exacerbated by anorexia caused by
pancreatic cancer, while another patient's condition was
exacerbated by hospital-acquired influenza infection. The general
condition of elderly patients with a decreased PS may be easily
deteriorated by anorexia or infection due to advanced malignant
tumors. Previously, Takahashi et al (19) also reported that patients with a
PS of 3-4 were likely to develop poor general conditions, such as
aspiration pneumoniae and heart failure following ERCP. Of note, in
the present study, both prevalence rates of moderate or severe
cholangitis and CCI in the PS 3-4 group were significantly higher
than in the PS 0-2 group. CCI is widely used for the assessment of
surgery indication or prognosis of other diseases (9,20-22).
In other words, a higher CCI indicates vulnerability in the general
condition due to several existing diseases. Thus, the general
condition of patients in the PS 3-4 group was likely to deteriorate
compared to that of the PS 0-2 group in the presence of
cholangitis. Moreover, incidents unrelated to the ERCP procedures,
such as an influenza infection, may deteriorate the general
condition of patients with a PS of 3-4 and may result in a fatal
outcome due to a higher CCI. However, the higher comorbidity
disease rate of the PS 3-4 group with moderate or severe
cholangitis indicates that elderly patients with a PS of 3-4
require biliary drainage compared to those with a PS of 0-2.
As mentioned above, ERCP is effective and safe for
elderly patients with not only a PS of 0-2, but also with a PS of
3-4. ERCP procedures should be performed for patients with a PS of
3-4 due to their moderate to severe cholangitis and their
vulnerability. However, even if ERCP procedures are successful,
careful attention should be paid to the clinical course of elderly
patients with a PS of 3-4.
The present study had some limitations. First, it
was retrospectively performed in a single center, intended for
patients who underwent ERCP for short periods of time. Therefore,
the number of elderly patients with a PS of 3-4 was comparatively
lower. Additional prospective investigations for more cases are
necessary in the future. Second, this study was intended for
elderly patients with a PS of 3-4 who underwent ERCP. The clinical
course of elderly patients not undergoing ERCP was not
investigated, which may be a selective bias. Following this study,
it is necessary to investigate the clinical courses of all elderly
patients regardless of ERCP. Third, this study did not make
comparisons with younger patients. The efficacy and adverse events
of ERCP for younger patients with a PS of 3-4 need to be
investigated.
Overall, the present study clarified that the
technical success rate and complication rate in patients with PS
3-4 were comparable to those of patients with PS 0-2. Thus, ERCP
for elderly patients with a PS of 3-4 is effective and safe.
However, it should be noted that ERCP in patients with a PS of 3-4
may result in a fatal outcome caused by incidents unrelated to the
ERCP procedure.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The data of this study are available upon reasonable
request. The data are stored at Saiseikai Chuwa Hospital electronic
health record system, and the participant data were de-identified
in this study.
Authors' contributions
SA wrote the manuscript. SA, AD, HU, KM and KY were
the attending doctors for the patients. SA, AD, HU, KM conducted
the ERCP. HY contributed to the conception and design of the study.
AD organized the study and the report.
Ethics approval and consent to
participate
This is a retrospective observational study in
Saiseikai Chuwa Hospital, not an interventional trial. Thus, the
patients in this study were involved within general practice and
thus ethics approval and patient consent was not required.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Ukkonen M, Siiki A, Antila A, Tyrväinen T,
Sand J and Laukkarinen J: Safety and efficacy of acute endoscopic
retrograde cholangiopancreatography in the elderly. Dig Dis Sci.
61:3302–3308. 2016.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Galeazzi M, Mazzola P, Valcarcel B,
Bellelli G, Dinelli M, Pasinetti GM and Annoni G: Endoscopic
retrograde cholangiopancreatography in the elderly: Results of a
retrospective study and a geriatricians' point of view. BMC
Gastroenterol. 18(38)2018.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Tohda G, Ohtani M and Dochin M: Efficacy
and safety of emergency endoscopic retrograde
cholangiopancreatography for acute cholangitis in the elderly.
World J Gastroenterol. 22:8382–8388. 2016.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Yun DY, Han J, Oh JS, Park KW, Shin IH and
Kim HG: Is endoscopic retrograde cholangiopancreatography safe in
patients 90 years of age and older? Gut Liver. 8:552–556.
2014.PubMed/NCBI View
Article : Google Scholar
|
|
5
|
Behlül B, Ayfer S, Sezgin V, Altay K,
Mustafa C, Cem C, Bilge O, Fatih A, Emrah A, Zafer B, et al: Safety
of endoscopic retrograde cholangiopancreatography in patients 80
years of age and older. Prz Gastroenterol. 9:227–231.
2014.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Mohammad Alizadeh AH, Afzali ES, Shahnazi
A, Sanati A, Mirsattari D and Zali MR: Utility and safety of ERCP
in the elderly: A comparative study in Iran. Diagn Ther Endosc.
2012(439320)2012.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Oken MM, Creech RH, Tormey DC, Horton J,
Davis TE, McFadden ET and Carbone PP: Toxicity and response
criteria of the Eastern Cooperative Oncology Group. Am J Clin
Oncol. 5:649–655. 1982.PubMed/NCBI
|
|
8
|
Takada T, Strasberg SM, Solomkin JS, Pitt
HA, Gomi H, Yoshida M, Mayumi T, Miura F, Gouma DJ, Garden OJ, et
al: TG13: Updated Tokyo guidelines for the management of acute
cholangitis and cholecystitis. J Hepatobiliary Pancreat Sci.
20:1–7. 2013.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Charlson ME, Pompei P, Ales KL and
MacKenzie CR: A new method of classifying prognostic comorbidity in
longitudinal studies: Development and validation. J Chronic Dis.
40:373–383. 1987.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Miura F, Takada T, Strasberg SM, Solomkin
JS, Pitt HA, Gouma DJ, Garden OJ, Büchler MW, Yoshida M, Mayumi T,
et al: TG13 flowchart for the management of acute cholangitis and
cholecystitis. J Hepatobiliary Pancreat Sci. 20:47–54.
2013.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Tanisaka Y, Ryozawa S, Mizuide M,
Kobayashi M, Fujita A, Minami K, Kobatake T, Omiya K, Iwano H and
Araki R: Usefulness of the ‘newly designed’ short-type
single-balloon enteroscope for ERCP in patients with Roux-en-Y
gastrectomy: A pilot study. Endosc Int Open. 6:E1417–E1422.
2018.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Maple JT, Keswani RN, Hovis RM, Saddedin
EZ, Jonnalagadda S, Azar RR, Hagen C, Thompson DM, Waldbaum L and
Edmundowicz SA: Carbon dioxide insufflation during ERCP for
reduction of postprocedure pain: A randomized, double-blind,
controlled trial. Gastrointest Endosc. 70:278–283. 2009.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Nakamura K, Yamaguchi Y, Hasue T, Higa K,
Tauchi M, Toki M, Sugiyama M and Takahashi S: The usefulness and
safety of carbon dioxide insufflation during endoscopic retrograde
cholangiopancreatography in elderly patients: A prospective,
double-blind, randomized, controlled trial. Hepatogastroenterology.
61:2191–2195. 2014.PubMed/NCBI
|
|
14
|
Adler DG, Baron TH, Davila RE, Egan J,
Hirota WK, Leighton JA, Qureshi W, Rajan E, Zuckerman MJ, Fanelli
R, et al: ASGE guideline: The role of ERCP in diseases of the
biliary tract and the pancreas. Gastrointest Endosc. 62:1–8.
2005.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Mallery JS, Baron TH, Dominitz JA,
Goldstein JL, Hirota WK, Jacobson BC, Leighton JA, Raddawi HM, Varg
JJ II, Waring JP, et al: Complications of ERCP. Gastrointest
Endosc. 57:633–638. 2003.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Ellis G, Whitehead MA, O'Neill D,
Langhorne P and Robinson D: Comprehensive geriatric assessment for
older adults admitted to hospital. Cochrane Database Syst Rev.
2011(CD006211)2011.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Park TY, Choi JS, Oh HC, Kim JW, Do JH and
Jung YH: Assessment of safety of non-anesthesiologist-assisted
endoscopic retrograde cholangiopancreatography based on performance
status in elderly patients. J Gastroenterol Hepatol. 29:1943–1948.
2014.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Hlatky MA, Boineau RE, Higginbotham MB,
Lee KL, Mark DB, Califf RM, Cobb FR and Pryor DB: A brief
self-administered questionnaire to determine functional capacity
(the Duke Activity Status Index). Am J Cardiol. 64:651–654.
1989.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Takahashi K, Nihei T, Aoki Y, Nakagawa M,
Konno N, Munakata A, Okawara K and Kashimura H: Efficacy and safety
of therapeutic endoscopic retrograde cholangiopancreatography in
patients with native papillae with a performance status score of 3
or 4: A single-center retrospective study. J Rural Med. 14:226–230.
2019.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Endo I, Takada T, Hwang TL, Akazawa K,
Mori R, Miura F, Yokoe M, Itoi T, Gomi H, Chen MF, et al: Optimal
treatment strategy for acute cholecystitis based on predictive
factors: Japan-Taiwan multicenter cohort study. J Hepatobiliary
Pancreat Sci. 24:346–361. 2017.PubMed/NCBI View
Article : Google Scholar
|
|
21
|
Ando K, Doi T, Moody SY, Ohkuni Y, Sato S
and Kaneko N: The effect of comorbidity on the prognosis of acute
lung injury and acute respiratory distress syndrome. Intern Med.
51:1835–1840. 2012.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Naito Y, Sasaki H, Takamatsu Y, Kiyomi F
and Tamura K: Retrospective analysis of treatment outcomes and
geriatric assessment in elderly malignant lymphoma patients. J Clin
Exp Hematop. 56:43–49. 2016.PubMed/NCBI View Article : Google Scholar
|