Introduction
Diabetes mellitus (DM) is a risk factor for the
development of cancer (1,2). There may be a difference in the
increase of the risk of cancer among the organs in DM, and the
increased risk of developing cancer of the liver and pancreas has
been noted in both males and females with DM (3,4). The
association of DM with cancer has been investigated in cohort
studies using large-scale populations and in case-control study
(5-8).
The association of DM with cancer has not yet been examined using
autopsy records.
Autopsy cases in Japan have been recorded and
published as the Annual of the Pathological Autopsy Cases in Japan
by Japanese Society of Pathology since 1960(9). Each autopsy record contains clinical
and pathological diagnoses. Pathological diagnosis includes the
diagnosis that developed during the lifetime of the patient. Even
in cases in which DM was not clinically evident during the
patient's lifetime, a diagnosis of DM is made at the time of
autopsy, depending on the pathological findings. The pathological
diagnosis contains the present and past history of cancers and
includes detailed histological data on cancer and latent cancer
found at the autopsy.
In the present study, the association of DM with
cancers was investigated using the autopsy records between 2005 and
2009 in Japan. The odds ratios (ORs) for cancers in DM cases were
estimated. Although the study may warrant careful interpretation,
the increase in the ORs of hepatocellular carcinoma (HCC) was
verified using the autopsy records. To the best of our knowledge,
the present study is the first to elucidate the association of DM
with cancers using autopsy records.
Materials and methods
Autopsy records and selection of
cases
The Annual of Pathological Autopsy Cases in Japan
has been published by the Japanese Society of Pathology. The
portable document format (PDF) of the autopsy records published
between 2005 and 2009 was used in the present study (9). The use of the PDF files was permitted
by the Information Committee of the Japanese Society of Pathology.
Autopsy records of the age, sex, clinical diagnosis, pathological
diagnosis of one autopsy case were converted to a spreadsheet file.
A total of 83,829 cases were recorded in the Annual of Pathological
Autopsy Cases in Japan between 2005 and 2009. All records were
reviewed by two authors (RW and SKi).
The following cases were excluded from the
estimation of ORs: i) Cases that were not published and lacked a
description of age, sex and diagnosis; ii) cases of hermaphrodites;
iii) cases of regional dissection of the head, chest, or abdomen
and postmortem biopsy; iv) fetuses, stillborn infants; and v) cases
<40 years of age for the comparison with the previous cohort and
case-control studies (5-8),
in which ORs for cancers in DM were estimated in individuals ≥40
years.
Identification of diabetes mellitus
and cancer cases
The cases of DM and cancer were identified by a text
search. DM cases were identified by the words ‘diabetes’, ‘diabetes
mellitus’, ‘DM’, ‘insulin dependent diabetes mellitus (IDDM)’,
‘non-insulin dependent diabetes mellitus (NIDDM)’, ‘type 1
diabetes’, ‘type 2 diabetes’, ‘Kimmelstiel-Wilson syndrome’ and
‘diabetic nephropathy’ in clinical and pathological diagnoses. The
cases without DM was designated as non-DM.
Cancers were identified by the combination of the
words ‘cancer’ or ‘carcinoma’ and the words of the organs
‘thyroid’, ‘lung’, ‘stomach’, ‘colon’, ‘rectum’, ‘breast’,
‘kidney’, ‘uterus’, ‘ovary’ and ‘prostate’. Histological subtypes
were taken into consideration in the liver and pancreas. HCC was
identified by the words ‘hepatocellular carcinoma’ and ‘HCC’.
Intrahepatic cholangiocarcinoma (ICC) was identified by the words
‘intrahepatic cholangiocarcinoma’, ‘cholangiocellular carcinoma
(CCC)’, ‘ICC’ and ‘CCC’. Invasive ductal carcinoma (IDC) of the
pancreas was identified by the words ‘pancreatic ductal carcinoma’,
‘pancreas cancer’, ‘pancreas adenocarcinoma’, and by the
combination of ‘invasive ductal carcinoma’ and ‘ductal carcinoma’
with ‘pancreas’.
Statistical analysis
Identified cases were stratified into two strata of
age: Between 40 and 69 years, and ≥70 years. The distribution of
age was analyzed using the Chi-square test. Age-adjusted ORs and
95% confidence intervals (CIs) of cancers were estimated with the
logistic regression method. Analyses were performed using RStudio
(RStudio, Inc., https://www.rstudio.com). P-values <0.05 were
considered to indicate statistically significant differences.
Results
Autopsy cases
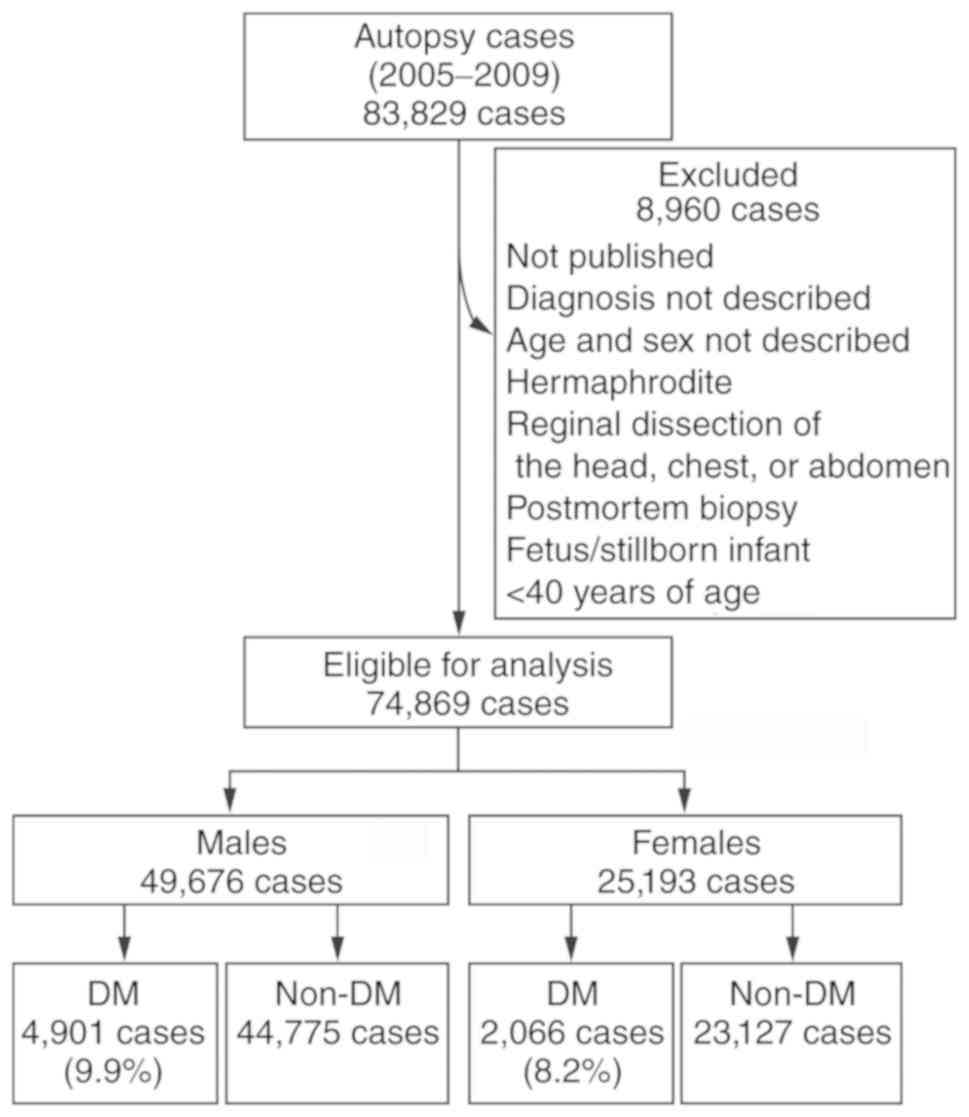
Among the 83,829 cases, a total 8,960 cases were
excluded. The excluded cases were as follows: Cases that were not
published and lacked a description of age, sex and diagnosis (427
cases); cases of hermaphrodites (5 cases); cases of regional
dissection of the head, chest, or abdomen and postmortem biopsy
(1,314 cases); fetuses, stillborn infants (3,533 cases); and cases
younger than 40 years of age (3,681 cases). Finally, 74,869 were
eligible for the analysis (Fig.
1).
Based on the Vital Statistics of Japan Final Data,
General Mortality (10), the total
number of deaths was 5,560,852 between 2005 and 2009 in Japan. The
number of deaths of those ≥40 years was 5,425,379. Thus, the cases
eligible for the analysis corresponded to 1.4% of deceased
individuals ≥40 years.
Among the 74,869 records, 49,676 were males and
25,193 were females (Fig. 1). A
total of 6,967 cases (9.3%) were identified as DM. DM was noted in
4,901 men (9.9%) and 2,066 women (8.2%). The cases were stratified
into two strata: Between 40 and 69 years, and ≥70 years. The
distribution of the numbers of cases by age did not differ
significantly between DM and non-DM in both males and females
(Tables I and II).
 | Table INumber of cancer cases and odds ratios
in males. |
Table I
Number of cancer cases and odds ratios
in males.
| Cases | DM | Non-DM | Age-adjusted OR (95%
CI) | P-value |
|---|
| Total no. of
cases | 4,901 | 44,775 | | |
| Age
(years)a |
|
40-69 | 2,145 | 19,108 | | |
|
≥70 | 2,756 | 25,667 | | |
| Cancers |
|
Thyroid | 90 | 823 | 1.00 (0.80-1.24) | 0.982 |
|
Lung | 465 | 6,749 | 0.59 (0.54-0.65) | <0.001 |
|
Stomach | 336 | 4,226 | 0.71 (0.63-0.80) | <0.001 |
|
Colon/rectum | 327 | 3,197 | 0.93 (0.83-1.05) | 0.256 |
|
Liver |
|
HCC | 414 | 3,076 | 1.25 (1.12-1.39) | <0.001 |
|
ICC | 38 | 480 | 0.72 (0.52-1.00) | 0.043 |
|
Pancreas
IDC | 182 | 1,607 | 1.04 (0.89-1.21) | 0.663 |
|
Biliary
tract | 58 | 921 | 0.57 (0.44-0.75) | <0.001 |
|
Kidney | 86 | 781 | 1.01 (0.80-1.26) | 0.959 |
|
Prostate | 349 | 3,835 | 0.82 (0.74-0.93) | <0.001 |
|
Multiple
cancers | 328 | 3,776 | 0.78 (0.70-0.88) | <0.001 |
 | Table IINumber of cancer cases and ORs in
females. |
Table II
Number of cancer cases and ORs in
females.
| Cases | DM | Non-DM | Age-adjusted OR (95%
CI) | P-value |
|---|
| Total no. of
cases | 2,066 | 23,127 | | |
| Age
(years)a |
|
40-69 | 699 | 8,174 | | |
|
≥70 | 1,367 | 14,953 | | |
| Cancers |
|
Thyroid | 77 | 797 | 1.09 (0.86-1.38) | 0.497 |
|
Lung | 104 | 1,672 | 0.68 (0.55-0.83) | <0.001 |
|
Stomach | 62 | 1,283 | 0.52 (0.40-0.68) | <0.001 |
|
Colon/rectum | 104 | 1,453 | 0.79 (0.64-0.96) | 0.017 |
|
Liver |
|
HCC | 117 | 1,077 | 1.22 (1.00-1.49) | 0.045 |
|
ICC | 9 | 229 | 0.44 (0.22-0.85) | 0.005 |
|
Pancreas
IDC | 88 | 954 | 1.03 (0.83-1.29) | 0.776 |
|
Biliary
tract | 42 | 665 | 0.69 (0.51-0.95) | 0.017 |
|
Kidney | 18 | 212 | 0.95 (0.59-1.54) | 0.837 |
|
Breast | 63 | 945 | 0.74 (0.57-0.96) | 0.020 |
|
Uterus | 25 | 437 | 0.64 (0.43-0.96) | 0.023 |
|
Multiple
cancers | 75 | 971 | 0.86 (0.67-1.09) | 0.191 |
Odds ratio for cancers in males
The ORs for cancer in males are presented in
Table I. The age-adjusted ORs for
cancers of the thyroid, colon/rectum and kidney were comparable.
The ORs for cancers of the lung, stomach, biliary tract and
prostate were significantly decreased in the DM cases. The OR for
HCC was significantly increased (1.25; 95% CI, 1.12-1.39,
P<0.001) in DM, whereas the OR for ICC was decreased (0.72; 95%
CI, 0.52-1.00, P<0.05). The OR for IDC of the pancreas was not
considered increased (1.04; 95% CI, 0.89-1.21, P=0.663). The OR for
multiple cancers was decreased (0.78; 95% CI, 0.70-0.88,
P<0.001) in males.
Odds ratio for cancers in females
The ORs for cancer in females are presented in
Table II. The age-adjusted ORs
for cancers of the thyroid and kidney were comparable. The ORs for
cancers of the lung, stomach, colon/rectum, breast and uterus were
decreased in DM cases. The OR for HCC in DM was significantly
increased (1.22; 95% CI: 1.00-1.49, P<0.05). The OR for ICC was
decreased (0.44; 95% CI, 0.22-0.85, P<0.05). The OR for IDC of
the pancreas was not considered increased (1.03; 95% CI, 0.83-1.29,
P=0.776). The OR for multiple cancers was comparable in women
(0.86; 95% CI, 0.67-1.09, P=0.191).
Discussion
The present study is the first, to the best of our
knowledge, to investigate the association of DM with cancer using
autopsy records. In the liver, the age-adjusted OR for HCC was
significantly increased (1.25 and 1.22) in males and females with
DM, respectively. On the other hand, the OR for ICC was decreased
(0.72 and 0.44) in males and females with DM, respectively. The
difference in OR between histological subtypes of cancers in the
liver was demonstrated. The ORs for cancers of other organs in DM
appeared to be reduced in males and females. The use of autopsy
records for the estimation of OR for cancers may warrant careful
consideration.
In previous cohort studies in Japan, ‘cancer’ of the
liver was identified by International Classification of Diseases
(ICD) code C22 (Table III)
(5-7).
The ICD code C22 includes all histological subtypes of malignant
tumor of the liver, the precise risk of the histological subtype
was unclear. In a case-control study, the increase in OR for HCC
was estimated from the cases with HCC (8). Although the ORs were lower than those
in previous studies in Japan, the significant increase in OR for
HCC in DM using autopsy records was in line with that of previous
studies. The increase in OR for HCC was noted in both males and
females in the present study. The association of DM with HCC was
confirmed in the present study using autopsy records from the
Annual of Pathological Autopsy Cases in Japan.
 | Table IIIOdds ratios of cancers of the liver in
DM. |
Table III
Odds ratios of cancers of the liver in
DM.
| | OR (95% CI) | |
|---|
| Author | No. of cases | Age (years) | Study design | Case selection | DM (%) | Males | Females | (Refs.) |
|---|
| Inoue et
al | 97,771 | 40-69 | Cohort | ICD C22 | 6.7 | 2.37 (1.76-3.20) | 2.09 (1.09-4.02) | (5) |
| Khan et
al | 56,881 | 40-79 | Cohort | ICD C22.0-9 | 5.8 | 2.30
(1.47-3.59) | 2.70
(1.20-6.05) | (6) |
| Kuriki et
al | 59,440 | 40-80 | Cohort | ICD C22 | 4.2 | 2.04
(1.48-2.80) | 2.27
(1.08-4.77) | (7) |
| Matsuo | 444 | 40-75 | Case-control | HCC | 15.8 | 2.52
(1.27-5.02) | 4.20
(0.81-21.81) | (8) |
| Present study | 74,869 | 40-104 |
Cross-sectional | HCC | 9.3 | 1.25
(1.12-1.39) | 1.22
(1.00-1.49) | |
The ORs estimated in the present study appeared to
be decreased. The increase in the risk of developing ICC in DM was
suggested by a previous study (11). The increase in the risk of
developing pancreatic cancer in DM was also previously suggested in
cohort studies in Japan (5-7);
however, the increase in OR for IDC of the pancreas was not noted
in the present study. This may be in part due to the fact that the
cases were selected by ICD code C25 in previous studies (5-7).
Other neoplasms, such as intraductal papillary mucinous neoplasm
and neuroendocrine neoplasms may be included in the code. If it is
taken into consideration that the OR for HCC is also lower than
those of the previous studies, the ORs estimated in the present
study may be underestimated, compared with those in the previous
studies, and the results warrant careful interpretation. In the
autopsy records from the Annual of Pathological Autopsy Cases in
Japan, the temporal sequence of diseases is not registered. It is
not feasible to estimate the ‘true’ risk of cancer development, and
the OR may need to be interpreted as the lifetime prevalence of
cancer in DM cases. The ORs were adjusted only by age in the
present study. The ORs were not adjusted with other important
confounding factors, such as smoking, body weight and occupation,
as these factors were not included in the records of the Annual of
Pathological Autopsy Cases in Japan. These factors may need to be
included in the Annual of Pathological Autopsy Records in Japan in
the future. The analyzed autopsy cases correspond 1.4% of mortality
between 2005 and 2009. There is a bias for the selection of autopsy
cases by attending doctors. These factors may affect the estimation
of OR.
According to the National Health and Nutrition
Survey in Japan 2007(12), the
prevalence of DM in Japanese individuals ≥40 years was estimated to
be 18.0% among males and 9.1% among females by the measurement of
HbA1c. In the present study, the percentage of DM was estimated as
9.9% among males and 8.2% among females. The percentage of DM in
the autopsy records was lower than that in the survey. However, the
percentage was higher than those in previous cohort studies, in
which DM was recorded in a self-report manner (Table III) (5-7).
In some recent cases of DM, the pathological changes associated
with DM may be subtle and overlooked. The pathological changes in
DM were carefully evaluated by pathologists and registered in
autopsy records. Although careful interpretation is required,
autopsy records are valuable for the epidemiological evaluation of
pathological alterations in DM cases.
Treatment with dipeptidyl peptidase (DPP)-IV
inhibitors and glucagon-like peptide (GLP)-1 agonists has been
suggested to induce the proliferation and dysplasia of ducts and
hyperplasia of endocrine cells based on materials from the Network
for Pancreatic Organ Donors with Diabetes (13). The pathological changes associated
with incretin-based therapy were not reproduced by an intensive
review of the same database (14).
The increase in the risk of developing ICC by incretin-based
therapy was not noted in a recent case-control study (15). In the present study, autopsy cases
were registered between 2005 and 2009, which was before DPP-IV
inhibitors had become available for the treatment of DM in Japan
(16). Therefore, the ORs in the
present study were not influenced by incretin-based therapy. DPP-IV
inhibitors are currently used for the treatment of DM in Japan. It
is plausible to examine the changes of diseases of the pancreas by
the autopsy records after 2009.
In conclusion, in the present study, the association
of DM with cancers was examined using the Annual of Pathological
Autopsy Cases in Japan. Although the ORs estimated from autopsy
records may warrant careful interpretation, the ORs of HCC were
increased in both males and females with DM. To the best of our
knowledge, this is the first study to demonstrate the association
of HCC with DM using autopsy records.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The data and material that support the findings of
this study are available from the corresponding author upon
reasonable request.
Authors' contributions
RW and ZN designed the study. The conversion of PDF
files to Excel files and the reviewing of the data were performed
by RW and SKi. Statistical analyses were performed by RW, SKu and
KI. MK verified diabetic patients, and prepared the figure. All
authors proofread and approved the final manuscript for
publication.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Giovannucci E, Harlan DM, Archer MC,
Bergenstal RM, Gapstur SM, Habel LA, Pollak M, Regensteiner JG and
Ye D: Diabetes and cancer: A consensus report. Diabetes Care.
33:1674–1685. 2010.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Kasuga M, Ueki K, Tajima N, Noda M, Ohashi
K, Noto H, Goto A, Ogawa W, Sakai R, Tsugane S, et al: Report of
the Japan diabetes society/Japanese cancer association joint
committee on diabetes and cancer. Cancer Sci. 104:965–976.
2013.PubMed/NCBI View Article : Google Scholar
|
|
3
|
El-Serag HB, Hampel H and Javadi F: The
association between diabetes and hepatocellular carcinoma: A
systematic review of epidemiologic evidence. Clin Gastroenterol
Hepatol. 4:369–380. 2006.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Huxley R, Ansary-Moghaddam A, Berrington
de González A and Woodward M: Type-II diabetes and pancreatic
cancer: A meta-analysis of 36 studies. Br J Cancer. 92:2076–2083.
2005.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Inoue M, Iwasaki M, Otani T, Sasazuki S,
Noda M and Tsugane S: Diabetes mellitus and the risk of cancer:
Results from a large-scale population-based cohort study in Japan.
Arch Intern Med. 166:1871–1877. 2006.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Khan M, Mori M, Fujino Y, Shibata A,
Sakauchi F, Washio M and Tamakoshi A: Japan Collaborative Cohort
Study G. Site-Specific cancer risk due to diabetes mellitus
history: Evidence from the Japan collaborative cohort (JACC) study.
Asian Pac J Cancer Prev. 7:253–259. 2006.PubMed/NCBI
|
|
7
|
Kuriki K, Hirose K and Tajima K: Diabetes
and cancer risk for all and specific sites among Japanese men and
women. Eur J Cancer Prev. 16:83–89. 2007.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Matsuo M: Association between diabetes
mellitus and hepatocellular carcinoma: Results of a hospital- and
community-based case-control study. Kurume Med J. 50:91–98.
2003.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Japanese Society of Pathology: Annual
report of pathological autopsy cases in Japan 2005-2009. Japanese
Society of Pathology, Tokyo, 2006-2010.
|
|
10
|
Japanese Ministry of Health Labour and
Welfare: Vital statistics of Japan final data. General Mortality,
2009. https://www.e-stat.go.jp/.
|
|
11
|
Jing W, Jin G, Zhou X, Zhou Y, Zhang Y,
Shao C, Liu R and Hu X: Diabetes mellitus and increased risk of
cholangiocarcinoma: A meta-analysis. Eur J Cancer Prev. 21:24–31.
2012.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Japanese Ministry of Health Labour and
Welfare: The national health and nutrition survey in Japan, 2007.
https://www.mhlw.go.jp/bunya/kenkou/eiyou09/01.html.
|
|
13
|
Butler AE, Campbell-Thompson M, Gurlo T,
Dawson DW, Atkinson M and Butler PC: Marked expansion of exocrine
and endocrine pancreas with incretin therapy in humans with
increased exocrine pancreas dysplasia and the potential for
glucagon-producing neuroendocrine tumors. Diabetes. 62:2595–2604.
2013.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Harja E, Lord J and Skyler JS: An analysis
of characteristics of subjects examined for incretin effects on
pancreatic pathology. Diabetes Technol Ther. 15:609–618.
2013.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Giorda CB, Picariello R, Tartaglino B,
Nada E, Costa G and Gnavi R: Incretin-based therapy and risk of
cholangiocarcinoma: A nested case-control study in a population of
subjects with type 2 diabetes. Acta Diabetol. 57:401–408.
2020.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Goda M and Kadowaki T: Teneligliptin for
the treatment of type 2 diabetes. Drugs Today (Barc). 49:615–629.
2013.PubMed/NCBI View Article : Google Scholar
|