Introduction
In patients with benign central airway stenosis or
obstruction, surgical resection/anastomosis is the optimal
treatment: However, only 50% of patients can undergo resection
(1). Therefore, stenting is
required for the treatment of patients with benign airway stenosis
or obstruction (1). An airway
stent is used to improve symptoms and quality of life. In addition,
airway stenting is used as palliative treatment to improve lung
function in patients with central airway stenosis or obstruction
due to thoracic malignancies (2-4),
as central airway stenosis or obstruction can result from tumor
invasion or extrinsic tumor compression (5,6).
However, the decision for stent placement in an airway should be
undertaken carefully, as stenting is associated with serious risks,
such as bleeding, airway obstruction during the procedure, or
misplacement or migration from the desired location (5). In particular, care should be taken in
selecting the types of stenting according to the indications for
patients with benign central airway stenosis or obstruction
(5). Therefore, the indications
for stent placement in patients with benign disease should be based
on a risk-benefit analysis.
Reports on stenting for airway stenosis or
obstruction due to malignant disease are relatively common;
however, limited data are available on stenting for patients with
central airway stenosis or obstruction due to benign disease, as
there are only a few studies available on the long-term outcomes of
patients with benign disease who have undergone airway stenting
(1,7). As the outcomes for patients with
benign disease may differ from those of patients with malignant
disease (7), and a number of
issues related to stenting for benign central airway stenosis or
obstruction remain unknown (8),
the accrual of data on stenting related to benign disease is
warranted. The aim of the present study was to identify the
clinical features and outcomes of patients with airway stenosis or
obstruction due to benign disease who underwent stenting
procedures.
Materials and methods
Patients
The present study was approved by the Ethics
Committee of Toho University Omori Medical Center (M19151). The
present study retrospectively analyzed clinical data from 19
patients with stents for benign airway stenosis or obstruction who
underwent treatment at Toho University Omori Medical Center from
1998 to 2018, and compared the data with those of patients with
stents for central airway stenosis or obstruction due to malignant
disease. The following parameters were investigated from the
medical records obtained from Toho University Omori Medical Center:
Sex, age, disease, types of stents, complications, treatment after
stenting and patient outcome.
Complications associated with
stenting
The following complications were evaluated as
positive if treatment via bronchoscopy was required: Granulations,
halitosis, infection, mucoid impaction, tumor ingrowth, stent
fracture, stent malposition, or stent migration. Bleeding caused by
stenting was considered positive if hemostatic agents were
administered or bronchoscopic treatment was required. Infections,
stent fracture and airway rupture were considered related to
stenting if confirmed by bronchoscopy. Halitosis was considered
positive if patients did not have halitosis prior to stenting, but
developed it after stenting.
Outcomes
The outcomes of patients following stenting for
airway stenosis or obstruction due to benign or malignant disease
were compared.
Statistical analysis
Fisher's exact test was used to compare binomial
proportions in frequency of complication by type. The χ2
test was used to assess differences between sex, type of stent,
treatments in patients' characteristics, complications of stenting,
and cases undergoing ≥2 procedures. Mann-Whitney U test was used to
assess differences in age in the patient characteristics. Survival
times were measured from the date of the first stent treatment
until the date of death or the last follow-up, and were estimated
by the Kaplan-Meier method. Kaplan-Meier graphs were compared by
the log-rank test. A P-value <0.05 was considered to indicate a
statistically significant difference.
Results
The patient characteristics are presented in
Table I. Of the patients with
benign disease, a significantly higher proportion were females,
whereas this was not the case in patients with malignant disease
(Table I). The difference between
the types of stents (silicon vs. metallic) used in patients with
benign vs. those with malignant disease was not significant.
 | Table ICharacteristics of patients with
airway stenosis/obstruction. |
Table I
Characteristics of patients with
airway stenosis/obstruction.
| Clinical factor | Total no. of patients
136 | No. of patients with
benign disease 19 | No. of patients with
malignant disease 117 | P-value |
|---|
| Age | | | | |
|
Mean | 63 | 57 | 64 | 0.4817 |
| Sex | | | | |
|
Male:female | 94:42 | 8:11 | 86:31 | 0.0131 |
| Type of stent | | | | 0.2915 |
|
Silicon | 60 | 11 | 49 | |
|
Metallic | 76 | 8 | 68 | |
| Treatment | 167 | 35 | 132 | <0.0001 |
|
Placement | 135 | 18 | 117 | |
|
Replacement | 10 | 6 | 4 | |
|
Additional | 9 | 3 | 6 | |
|
placement | | | | |
|
Removed | 9 | 6 | 3 | |
|
Repositioned | 3 | 2 | 1 | |
|
Cleaned | 1 | 0 | 1 | |
Of the 19 patients with benign disease, central
airway stenosis or obstruction due to long-term intubation,
tracheostomy, traffic accident, surgery for infection, tuberculosis
and goiter resulted in stenting for 8 patients, 7 patients, 1, 1, 1
and 1 patient, respectively (Table
II). The differences between complication rates and types of
complication in patients with benign disease vs. those with
malignant disease were not significant (Tables III and IV).
 | Table IIReasons for stenting in patients with
benign disease. |
Table II
Reasons for stenting in patients with
benign disease.
| Group | No. of patients |
|---|
| Benign disease | 19 |
| After intubation | 8 |
| After
tracheostomy | 7 |
| Traffic accident | 1 |
| After surgery for
infection | 1 |
| Infection
(tuberculosis) | 1 |
| Goiter | 1 |
 | Table IIIComplications of stenting. |
Table III
Complications of stenting.
| Group | Total no. of
patients | No. of patients with
benign disease | No. of patients with
malignant disease | P-value |
|---|
| Positive for
complication | 33 | 6 | 27 | 0.6077 |
| Negative for
complication | 103 | 13 | 90 | |
 | Table IVFrequency of complication by type. |
Table IV
Frequency of complication by type.
| Group | Total no. of
patients | No. of patients with
benign disease | No. of patients with
malignant disease | P-value |
|---|
| Airway rupture | 0 | 0 | 0 | - |
| Bleeding | 2 | 0 | 2 | >0.9999 |
| Granulation | 9 | 2 | 7 | 0.6129 |
| Halitosis | 3 | 1 | 2 | 0.3656 |
| Infection | 3 | 0 | 3 | >0.9999 |
| Mucoid impaction | 14 | 2 | 12 | >0.9999 |
| Stent fracture | 0 | 0 | 0 | - |
| Stent
malposition | 2 | 1 | 1 | 0.2608 |
| Stent migration | 11 | 3 | 8 | 0.1837 |
| Total | 44 | 9 | 35 | |
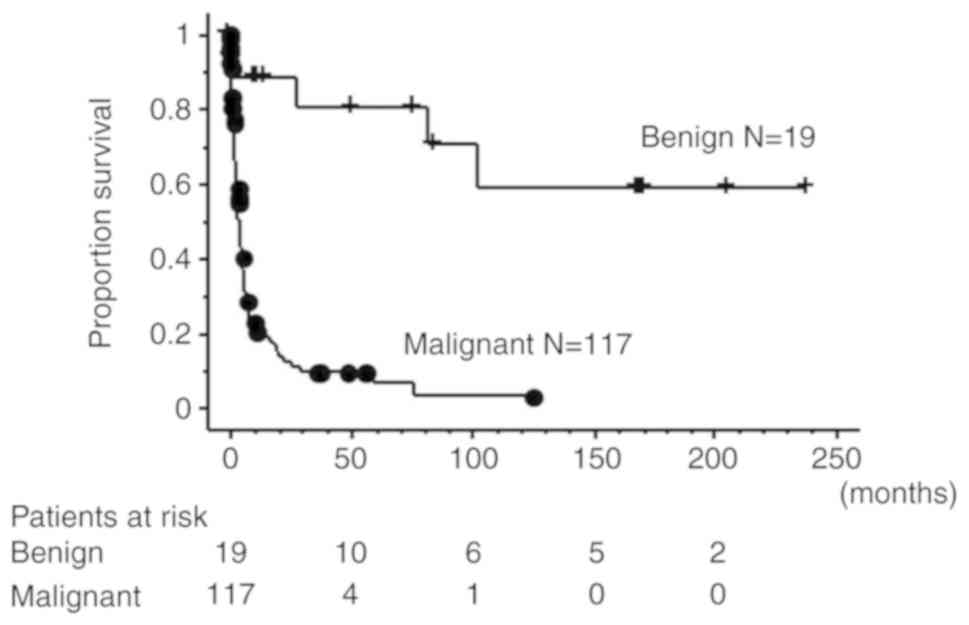
The median follow-up times of patients with stents
due to benign and malignant central airway stenosis or obstruction
were 51 (benign: Range, 0.164-239,) months and 3 (malignant: Range,
0.066-125) months, respectively. The 5-year survival rates were
80.5 and 6.3% in patients with benign and malignant stenosis or
obstruction, respectively. The 10-year survival rates were 58.7 and
3.1% in patients with benign and malignant stenosis or obstruction,
respectively. Patients with benign disease had a significantly
better outcome than patients with malignant disease (Fig. 1, P<0.0001).
For 19 patients with benign disease, 35 stent
procedures were performed, which consisted of the following: A
total of 18 placements, 6 replacements, 3 additional stent
placements, 6 removals and 2 stents repositioned. One patient
underwent removal and replacement of the silicon stent in Toho
University Omori Medical Center following the placement of the
silicon stent in another hospital (Table V, case 4). The differences between
the types of treatments for patients with benign disease vs. those
with malignant disease were significant (Table I, P<0.0001). As regards the
number of procedures, 7 out of 19 patients with benign disease had
≥2 procedures and 13 out of 117 patients with malignant disease had
≥2 procedures; in addition, 6 out of 19 patients with benign
disease had ≥3 procedures, and only 2 of the 117 patients with
malignant disease had ≥3 procedures (Table V). Patients with benign disease
underwent significantly higher numbers of procedures (≥2 and ≥3)
than patients with malignant disease (Table VI; P=0.0096 and P<0.0001,
respectively).
 | Table VCases undergoing ≥2 procedures. |
Table V
Cases undergoing ≥2 procedures.
| Group | Reason for
obstruction | 1st operation | 2nd operation | 3rd operation | 4th operation | 5th operation |
|---|
| Benign disease | | | | | | |
|
Case 1 | Traffic
accident | Ultraflex | Dumon(ad) | Dumon(re) | | |
|
Case 2 | Tracheostomy | Dumon | Removal | | | |
|
Case 3 | Infection | Ultraflex | Ultraflex(ad) | Dumon(ad) | | |
|
Case 4 | Tracheostomy | [Dumon] | Removal | Dumon(re) | | |
|
Case 5 | Intubation | Dumon | Repositioned | Dumon(re) | Removal | |
|
Case 6 | Tracheostomy | Dumon | Removal | Dumon(re) | Dumon(re) | |
|
Case 7 | Tracheostomy | Dumon | Repositioned | Removal | T-tube(re) | Removal |
| Malignant
disease | | | | | | |
|
Case 1 | Thyroid cancer | Dumon | Dumon(re) | | | |
|
Case 2 | Lymphoma | Dumon | Ultraflex(ad) | | | |
|
Case 3 | Lung cancer | Ultraflex | Ultraflex(ad) | | | |
|
Case 4 | Lung cancer | Dumon | Removal | Ultraflex(re) | | |
|
Case 5 | Thyroid cancer | Ultraflex | Ultraflex(ad) | T-tube(ad) | | |
|
Case 6 | Lung cancer | Dumon | Removal | | | |
|
Case 7 | Lung cancer | Ultraflex | Ultraflex(ad) | | | |
|
Case 8 | Thyroid cancer | Ultraflex | Cleaned | | | |
|
Case 9 | Esophageal
cancer | Ultraflex | Ultraflex(ad) | | | |
|
Case 10 | Metastatic
cancer | Dumon | Removal | | | |
|
Case 11 | Malignant
schwannoma | Dumon | Ultraflex(re) | | | |
|
Case 12 | Lung cancer | Dumon | Repositioned | | | |
|
Case 13 | Esophageal
cancer | Dumon | Dumon(re) | | | |
 | Table VIDifferences between patients with
benign and malignant disease undergoing ≥2 and ≥3 procedures. |
Table VI
Differences between patients with
benign and malignant disease undergoing ≥2 and ≥3 procedures.
| No. of
procedures | Benign disease
(n=19) | Malignant disease
(n=117) | P-value |
|---|
| Patients with ≥2
procedures | 7 | 13 | 0.0096 |
| Patients with ≥3
procedures | 6 | 2 | <0.0001 |
Discussion
The findings of the present study indicated that
patients with benign disease obtained significantly better outcomes
after airway stenting than patients with malignant disease, and
patients with benign disease had significantly more frequent
operations than patients with malignant disease. These results
indicate that patients with benign central airway stenosis or
obstruction who undergo stenting might require multiple procedures,
and that physicians should plan for multiple treatments following
the first stent placement due to their promising outcomes. Although
retrospective studies on airway stenting have revealed risks and
complications after stenting (5,6), as
there are minimal data available on long-term outcomes, the present
study investigated the clinical features and outcomes of patients
with airway stenosis or obstruction due to benign disease.
Previous studies on airway stenting for benign
central airway obstruction have been retrospective and have
included few patients and short follow-up periods, as prospective
and large-scale studies were difficult to perform for airway
stenting (1,5). Saad et al examined the
clinical features of 21 patients with miscellaneous benign diseases
and 11 patients with airway complications following lung
transplantation (7). They reported
median follow-up durations of 336 days for patients with
miscellaneous benign diseases and 329 days for patients following
lung transplantation. Husain et al performed a retrospective
study on the Ultraflex metallic stent, and compared patients with
benign airway obstruction with patients with malignant airway
obstruction (1). They reported
that 10 of 12 patients with benign airway obstruction were alive
with a median survival of 1,017 days, ranging from 46 to 1,120
days, but not reaching the 5-year endpoint. Of the 2 patients with
benign diseases who passed away, 1 had severe Wegener
granulomatosis and the other had the comorbidities of pulmonary
fibrosis and cardiac failure (1).
By contrast, Saji et al examined 65 patients
with advanced lung cancer associated with central airway
obstruction and found a 1-year survival rate of 25.2% and a median
survival time of 6.2 months (9).
Furukawa et al examined 40 patients with advanced lung
cancer associated with central airway obstruction and found a
1-year survival rate of 14.3% and median survival time of 94 days
(3.1 months) (10). Lemaire et
al performed a retrospective study on 140 patients with
malignant tumor and malignant airway disease and found a 1-year
survival rate of 15% and median survival of 3.4 months after
stenting (11).
In 2005, the US Food and Drug Administration
recommended that metallic stents should be avoided for benign
central airway obstruction (5).
Although wire stents preserve the mucociliary escalator, permit a
larger airway lumen, and are more easily implanted than other
stents, some investigators have advised that wire stents should not
be used as patients with metallic stents placed for benign
tracheobronchial disease have a significantly higher complication
rate than patients with metallic stents placed for malignancy
(12-14).
Wire stents have also been found to be difficult to remove after
they have been in the patients for a long period of time (1). On the other hand, silicon stents have
such disadvantages as migration, small internal lumens and
impairment of the mucociliary escalator, although they have been
easy to remove (1). Although in
the present study, no significant differences were found in the
complications between silicon and metallic stents, long-term
survival and possible multiple stent-related procedures need to be
considered for patients with benign airway stenosis or
obstruction.
The present study has certain limitations. First,
this was a retrospective study. Second, the present study included
a small number of patients with benign central airway stenosis or
obstruction. However, despite these limitations, the findings were
significant.
In conclusion, the present study found that the
majority of patients with benign central airway stenosis or
obstruction needed multiple stent-related procedures as the
patients had better outcomes than patients with malignant disease.
Therefore, airway stenting for patients with benign central airway
obstruction should be performed, while considering the need for
>1 stent-related procedure.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
AI, YA, AS, TS, SK, HO, KI, SS, YH and KT were
involved in the conception and design of the study. AI wrote the
manuscript. YA, AS, TS, SK, HO, KI, SS and YH collected data. KT
supervised the study. All authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
The present retrospective study was approved by the
Ethics Committee of Toho University Omori Medical Center
(M19151).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Husain SA, Finch D, Ahmed M, Morgan A and
Hetzel MR: Long-term follow-up of ultraflex metallic stents in
benign and malignant central airway obstruction. Ann Thorac Surg.
83:1251–1256. 2007.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Oviatt PL, Stather DR, Michaud G,
Maceachern P and Tremblay A: Exercise capacity, lung function, and
quality of life after interventional bronchoscopy. J Thorac Oncol.
6:38–42. 2011.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Ferrell B, Koczywas M, Grannis F and
Harrington A: Palliative care in lung cancer. Surg Clin North Am.
91:403–417. 2011.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Sökücü SN, Özdemir C, Tural Önür S, Dalar
L and Altın S: Comparison of silicon and metallic bifurcated stents
in patients with malignant airway lesions. Clin Respir J.
14:198–204. 2020.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Folch E and Keyes C: Airway stents. Ann
Cardiothorac Surg. 7:273–283. 2018.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Ost DE, Shah AM, Lei X, Godoy MCB, Jimenez
CA, Eapen GA, Jani P, Larson AJ, Sarkiss MG and Morice RC:
Respiratory infections increase the risk of granulation tissue
formation following airway stenting in patients with malignant
airway obstruction. Chest. 141:1473–1481. 2012.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Saad CP, Murthy S, Krizmanich G and Mehta
AC: Self-expandable metallic airway stents and flexible
bronchoscopy: Long-term outcomes analysis. Chest. 124:1993–1999.
2003.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Murgu SD, Egressy K, Laxmanan B, Doblare
G, Ortiz-Comino R and Hogarth DK: Central airway obstruction:
Benign strictures, tracheobronchomalacia, and malignancy-related
obstruction. Chest. 150:426–441. 2016.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Saji H, Furukawa K, Tsutsui H, Tsuboi M,
Ichinose S, Usuda J, Ohira T and Ikeda N: Outcomes of airway
stenting for advanced lung cancer with central airway obstruction.
Interact Cardiovasc Thorac Surg. 11:425–428. 2010.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Furukawa K, Ishida J, Yamaguchi G, Usuda
J, Tsutsui H, Saito M, Konaka C and Kato H: The role of airway
stent placement in the management of tracheobronchial stenosis
caused by inoperable advanced lung cancer. Surg Today. 40:315–320.
2010.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Lemaire A, Burfeind WR, Toloza E,
Balderson S, Petersen RP, Harpole DH Jr and D'Amico TA: Outcomes of
tracheobronchial stents in patients with malignant airway disease.
Ann Thorac Surg. 80:434–438. 2005.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Chung FT, Chen HC, Chou CL, Yu CT, Kuo CH,
Kuo HP and Lin SM: An outcome analysis of self-expandable metallic
stents in central airway obstruction: A cohort study. J
Cardiothorac Surg. 6(46)2011.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Guibert N, Saka H and Dutau H: Airway
stenting: Technological advancements and its role in interventional
pulmonology. Respirology: Mar 11, 2020 doi: 10.1111/resp.13801
(Epub ahead of print).
|
|
14
|
Serrano C, Laborda A, Lozano JM, Caballero
H, Sebastián A, Lopera J and de Gregorio MÁ: Metallic stents for
tracheobronchial pathology treatment. Cardiovasc Intervent Radiol.
36:1614–1623. 2013.PubMed/NCBI View Article : Google Scholar
|