1. Introduction
The Coronavirus Disease 2019 (COVID-19) was declared
a public health emergency of international concern by the World
Health Organization (WHO) on January 30, 2020. Eventually, it was
classified as the COVID-19 pandemic on March 11, 2020(1). At the time of the writing of the
present review, the global pandemic of COVID-19 has been present
for approximately 3 months worldwide. Since the first case was
identified in the city of Wuhan, Hubei Province in China, some
individuals suffered from the symptoms of pneumonia, although the
cause of the disease was unclear at that time. Eventually,
researchers in China isolated the agent of the disease and
published the whole genome of the virus. The virus identified has
only an 80-90% similarity with SARS-CoV from bats, shares a 79%
sequence identity with SARS-CoV in 2002 and a 50% similarity with
MERS-CoV in 2012(2). Therefore,
the WHO announced that pneumonia symptoms are caused by the novel
coronavirus and it was named SARS-CoV-2. The characteristics of
this novel coronavirus also differ from those of previously
identified coronaviruses that cause severe pneumonia, such as
SARS-CoV and MERS-CoV.
Coronaviruses are known to circulate among mammals
and birds; however, the virus was probably transmitted to humans by
another animal. In humans, coronaviruses cause respiratory tract
infections that can be mild for 4 genera of the virus
(Alpha, Beta, Gamma and
Deltacoronavirus) (3,4),
such as in some cases of the common cold (other possible causes,
for example, rhinoviruses). However, other types, such as SARS-CoV
and MERS-CoV can be lethal and can cause major outbreaks of severe
pneumonia (5). Recently, the novel
coronavirus or SARS-CoV-2 has caused the COVID-19 pandemic
(6). SARS-CoV, MERS-CoV and
SARS-CoV-2 cause severe respiratory tract infections and are
zoonotic pathogens, which begin in infected animals and are
transmitted from animals to humans, and can be transmitted,
moreover, from human to human. There are currently 7 types of
coronaviruses, including the novel coronavirus, SARS-CoV-2. Common
signs of COVID-19 infection include respiratory symptoms, fever,
cough, shortness of breath and breathing difficulties. In more
severe cases, the infection can cause pneumonia, severe acute
respiratory syndrome, kidney failure and even death (7,8).
Extensive research is being conducted in order to
obtain a deeper understanding of this novel coronavirus. Efforts
are being made to identify strategies with which to prevent and
break the chain of transmission. The characterisation of SARS-CoV-2
is not similar to that of SARS-CoV in 2002 and MERS-CoV in 2012.
First, SARS-CoV-2 is the most contagious virus among the
coronaviruses group. This has been proven by the continuously
increasing number of positive cases over the course of merely 3
months until >1,000,000 individuals who were affected (up to the
time of the writing of the present review). On the other hand,
SARS-CoV in 2002 and MERS-CoV in 2012 caused only 8,098 and 2,494
cases, respectively (9,10). The number of COVID-19 cases will
continue to increase for an undetermined amount of time this year.
Moreover, the estimated early range of the reproductive rate (R0)
of COVID-19 is from 2.6 to 4.71, indicating that new cases are
increasing by 2-4-fold each day (11). COVID-19 may spread between
individuals before any symptoms appear, rendering its
identification and control difficult.
As it is common in the course of infections, there
is a delay between the time of viral infection of an individual and
the time point at which the individual develops symptoms (the
disease onset). This is known as the incubation period. The
incubation period for COVID-19 is typically 5 to 6 days, but may
range from 2 to 14 days (12,13).
The transmission of COVID-19 to multiple hosts may be relatively
easy during the incubation period (pre-symptomatic period) compared
with SARS-CoV and MERS-CoV. Moreover, the number of asymptomatic or
mildly symptomatic individuals following infection is relatively
high for COVID-19, but fairly low for SARS-CoV and MERS-CoV. Thus,
it is a difficult to carry out the isolation and contact tracing of
individuals infected with COVID-19. Second, the transmission of
SARS-CoV-2 slightly differs from that of SARS-CoV and MERS-CoV. The
latter two viruses are mainly transmitted through direct contact
with individuals who have symptoms, such as by travelling to or
residing in an area where SARS-CoV and MERS-CoV have recently
spread, coming in close contact with infected patients and visiting
or attending healthcare facilities where SARS-CoV and MERS-CoV have
spread (14). For COVID-19,
however, there are two major methods through which the virus is
considered to disseminate, namely, from individual to individual
through respiratory droplets when an infected individual coughs,
sneezes or talks, as well as from contact with contaminated
surfaces, where the virus can survive for hours up to even days at
a time. From contaminated surfaces, the transmission of the virus
can take place when an individual touches a surface or object that
has the virus on it and subsequently touches their eyes, nose or
mouth (15). Furthermore, the WHO
states that in the context of COVID-19, airborne transmission may
be possible in specific circumstances and settings, in which
procedures or support treatments that generate aerosols are
performed (16). Third, most
reported SARS-CoV and MERS-CoV cases exhibited severe respiratory
illnesses requiring hospitalisation; however, approximately 20% of
the patients had mild or no symptoms. Fever, chills, myalgia and
cough were common. However, COVID-19 infection has led to 80% of
asymptomatic cases or those with mild to moderate symptoms and, 20%
severe and critical cases (17).
Fourth, the case fatality rate (CFR) of COVID-19 is likely not
higher compared with that of SARS-CoV and MERS-CoV. The CFR of
COVID-19 is globally indicated to be approximately 2-3%. This is
lower than the CFR of SARS-CoV and MERS-CoV, measured at
approximately 9.6 and 34%, respectively (18). Nevertheless, the COVID-19 pandemic
still continues to spread. The CFR may also increase, depending on
the total number of positive cases and deaths. COVID-19 has
recently become a major threat; therefore, urgent action to combat
the virus according to characterisation of the virus itself is
required, and it is also important to have knowledge of the
characterisation of the infected host. In the present review,
information on the spread and pattern of COVID-19 cases related to
the characterisation of the infected host, namely the level of
illness, symptoms, vulnerable groups (age, sex and health status)
and fatality rate is presented. Furthermore, urgent actions, as a
step of public health interventions, which are expected to prevent
the spread of COVID-19 in communities are also discussed.
2. Data collection methods
The present review analysed data on COVID-19
published on the Statista, WHO and Worldometer databases on April
4, 2020 sourced from countries worldwide (19-21).
In the present review, the data analysed are presented in the form
of a figure, a graph or diagram. In addition, some articles
(22-28)
were included in the present review to compare certain indicators
of COVID-19 cases published globally by websites, such as Statista,
WHO and Worldometer (19-21).
Data retrieved from each article were collected, and certain
indicators are listed in Table I
and marked in bold font as the first, second and third most common
in the individuals infected. The present review also discusses the
efforts made for COVID-19 prevention that were recommended by the
WHO and implemented by several countries.
 | Table ISeven articles included in the present
review for the comparison of data published in web by Statista, WHO
and Worldometer. |
Table I
Seven articles included in the present
review for the comparison of data published in web by Statista, WHO
and Worldometer.
| Study no. | Article
title/(Ref.) | No. of cases | Data on age | Data on sex (%) | Data on symptoms
(%) | Data on laboratory
tests | Data on comorbidities
(%) |
|---|
| 1. | Characteristics and
outcomes of 21 critically ill patients with COVID-19 in Washington
State (22) | 21 | Mean age, 70 years
(range, 43-92 years) | Male (52)
Female (48) | Cough 11 (47.6)
Shortness of breath 17 (76.2) Fever 11 (52.4) Temperature, mean
(range), 37.6̊C (35.3-39.2) | White blood cell
count, /µl 9,365 (2,890-16,900) Absolute lymphocyte count,
/µl 889 (200-2,390) Hemoglobin, g/dl 11.4 (8.0-13.7)
Platelet count, x103/µl 215 (52-395) | Total with ≥1
comorbidity 18 (85.7): Asthma 2 (9.1) Chronic obstructive
pulmonary disease 7 (33.3) Congestive heart failure 9 (42.9)
Diabetes 7 (33.3) Rheumatologic disease 1 (4.8) Obstructive
sleep apnea 6 (28.6) Chronic kidney disease 10 (47.6)
End-stage kidney disease 2 (9.5) History of solid organ transplant
2 (9.5) Cirrhosis 1 (4.8) Immunosuppression 3 (14.3) |
| 2. | Clinical
characteristics of 138 hospitalized patients with 2019 novel
coronavirus-infected pneumonia in Wuhan, China (23) | 138 | Median age, 56 years
(interquartile range, 42-68; range, 22-92 years) | Male 75 (54.3)
Female 63 (45.7) | Fever 136 (98.6)
Fatigue 96 (69.6) Dry cough 82 (59.4) Anorexia 55 (39.9)
Myalgia 48 (34.8) Dyspnea 43 (31.2) Expectoration 37 (26.8)
Pharyngalgia 24 (17.4) Diarrhea 14 (10.1) Nausea 14 (10.1)
Dizziness 13 (9.4) Headache 9 (6.5) Vomiting 5 (3.6) Abdominal pain
3 (2.2) | White blood cell
count, x109/l 3.5-9.5 Platelet count,
x109/l 125-350 Lymphocyte count,
x109/l 1.1-3.2 | Comorbidities 64
(46.4): Hypertension 43 (31.2) Cardiovascular disease 20 (14.5)
Diabetes 14 (10.1) Malignancy 10 (7.3) Cerebrovascular disease
7 (5.1) COPD 4 (2.9) Chronic kidney disease 4 (2.9) Chronic liver
disease 4 (2.9) HIV infection 2 (1.4) |
| 3. | Epidemiologic and
clinical characteristics of novel coronavirus infections involving
13 patients outside Wuhan, China (24) | 13 | Mean age, 34 years
(range, 34-48 years) | Male 10(77)
Female 3(23) | Maximum temperature,
˚C 38.4 (0.883), Mean (SD) Cough 6 (46.2) Productive cough 2
(15.4) Rhinorrhea 1 (7.7) Myalgia 3 (23.1) Diarrhea 1 (7.7)
Upper airway congestion 8 (61.5) Headache 3 (23.1) | Hemoglobin, g/l 147
(12.1) Hematocrit, % 43.2 (3.36) Platelets, x109/l
199 (72.5) WBCs, x109/l 5.83 (2.32) | No data |
| 4. | Epidemiologic
features and clinical course of patients infected with SARS-CoV-2
in Singapore (25) | 18 | Median age, 47
years (range, 31-73 years) | Male 9(50)
Female 9(50) | Fever 13(72)
Cough 15(83) Shortness of breath 2(11) Rhinorrhea 1(6) Sore
throat 11(61) Diarrhea 3(17) | WBCs,
x109/l 4.6 (1.7-6.3) Hemoglobin, g/dl 13.5 (11.7-17.2)
Platelets, x109/l 159 (116-217) Neutrophils,
x109/l 2.7 (0.7-4.5) Lymphocytes,
x109/l 1.2 (0.8-1.7) | No data |
| 5. | Risk factors
associated with acute respiratory distress syndrome and death in
patients with coronavirus disease 2019 pneumonia in Wuhan, China
(26) | 201 | Median age, 51
years (range, 43-60 years) ≥65 40 (19.9) <65 161 (80.1) | Male 128
(63.7) female 73 (36.3) | Fever 188 (93.5)
Cough 163 (81.1) Productive cough 83 (41.3) Dyspnea 80 (39.8)
Fatigue or myalgia 65 (32.3) | White blood cells,
x109/ml 5.94 (3.80-9.08) Neutrophils, x109/ml
4.47 (2.32-7.70) Lymphocytes, x109/ml 0.91
(0.60-1.29) Platelets, x109/ml 180.00
(137.00-241.50) | Comorbidities
Hypertension 39 (19.4) Diabetes 22 (10.9) Cardiovascular disease
8 (4.0) Liver disease 7 (3.5) Nervous system disease 7 (3.5)
Chronic lung disease 5 (2.5) Chronic kidney disease 2 (1.0)
Endocrine system diseases 2 (1.0) Tumor 1 (0.5) |
| 6. | Clinical features
of patients infected with 2019 novel coronavirus in Wuhan, China
(27) | 41 | Median age, 49
years (range, 41-58 years | Male 30(73)
Female 11(27) | Fever 40(98)
Cough 31(76) Myalgia (muscle pain) or fatigue 18(44) Sputum
production 11/39(28) Headache 3/38(8) Haemoptysis 2/39(5) Diarrhea
1/38(3) | White blood cell
count, x109 per liter 6.2 (4.1-10.5) Neutrophil count,
x109 per liter 5.0 (3.3-8.9) Lymphocyte count,
x109 per liter 0.8 (0.6-1.1) Haemoglobin, g/l 126.0
(118.0-140.0) Platelet count, x109 per liter 164.5
(131.5-263.0) | Any comorbidity
13(32): Diabetes 8(20) Hypertension 6(15) Cardiovascular disease
6(15) Chronic obstructive pulmonary disease 1(2) Malignancy
1(2) Chronic liver disease 1(2) |
| 7. | Epidemiological and
clinical characteristics of 99 cases of 2019 novel coronavirus
pneumonia in Wuhan, China: A descriptive study (28) | 99 | Mean age (SD) 55.5
years (13.1) (range, 21-82 years) | Male 67(68)
Female 32(32) | Fever 82(83)
Cough 81(82) Shortness of breath 31(31) Muscle ache 11(11)
Confusion 9(9) Headache 8(8) Sore throat 5(5) Runny nose 4(4) Chest
pain 2(2) Diarrhea 2(2) Nausea and vomiting 1(1) | Leucocytes
(x109 per liter; normal range 3.5-9.5) 7.5 (3.6)
Increased 24, Decreased 9 Neutrophils (x109 per liter;
normal range 1.8-6.3) 5.0 (3.3-8.1) Increased 38 Lymphocytes
(x109 per liter; normal range 1.1-3.2) 0.9 (0.5)
Decreased 35 Platelets (x109 per liter; normal range
125.0-350.0) 213.5 (79.1) Increased 4, Decreased 12 Haemoglobin
(g/l; normal range 130.0-175.0) 129.8 (14.8) Decreased 50 | Any 33(33): ARDS
17(17) Acute renal injury 3(3) Acute respiratory injury 8(8)
Septic shock 4(4) Ventilator-associated pneumonia 1(1) |
The data of COVID-19 cases obtained from Statista
(19), WHO (20) and Worldometer (21) included the total number of cases
(active infection, recoveries and deaths), grouped by age, sex, the
level of illness and comorbidities from some countries that have
been affected. In the present review, the number of COVID-19 cases
in Indonesia is also shown; however, the characterisation of cases
based on factors such as age, sex and comorbidities was not yet
available of the data published on April 4, 2020, both on
international and national websites (19-21,29).
Furthermore, data from published articles were collected (22-28)
in order to compare with the total data published on websites, such
as Statista, WHO and Worldometer (19-21)
from countries affected by COVID-19. Eventually, these data may
enhance our understanding of the pattern of individuals infected by
COVID-19, such as the level of illness, symptoms, vulnerable groups
(age, sex and health status) and the fatality rate. The
presentation of these data may be used to consider the efforts to
determine which responses will be the most effective in the
COVID-19 crisis.
3. Summary of data obtained
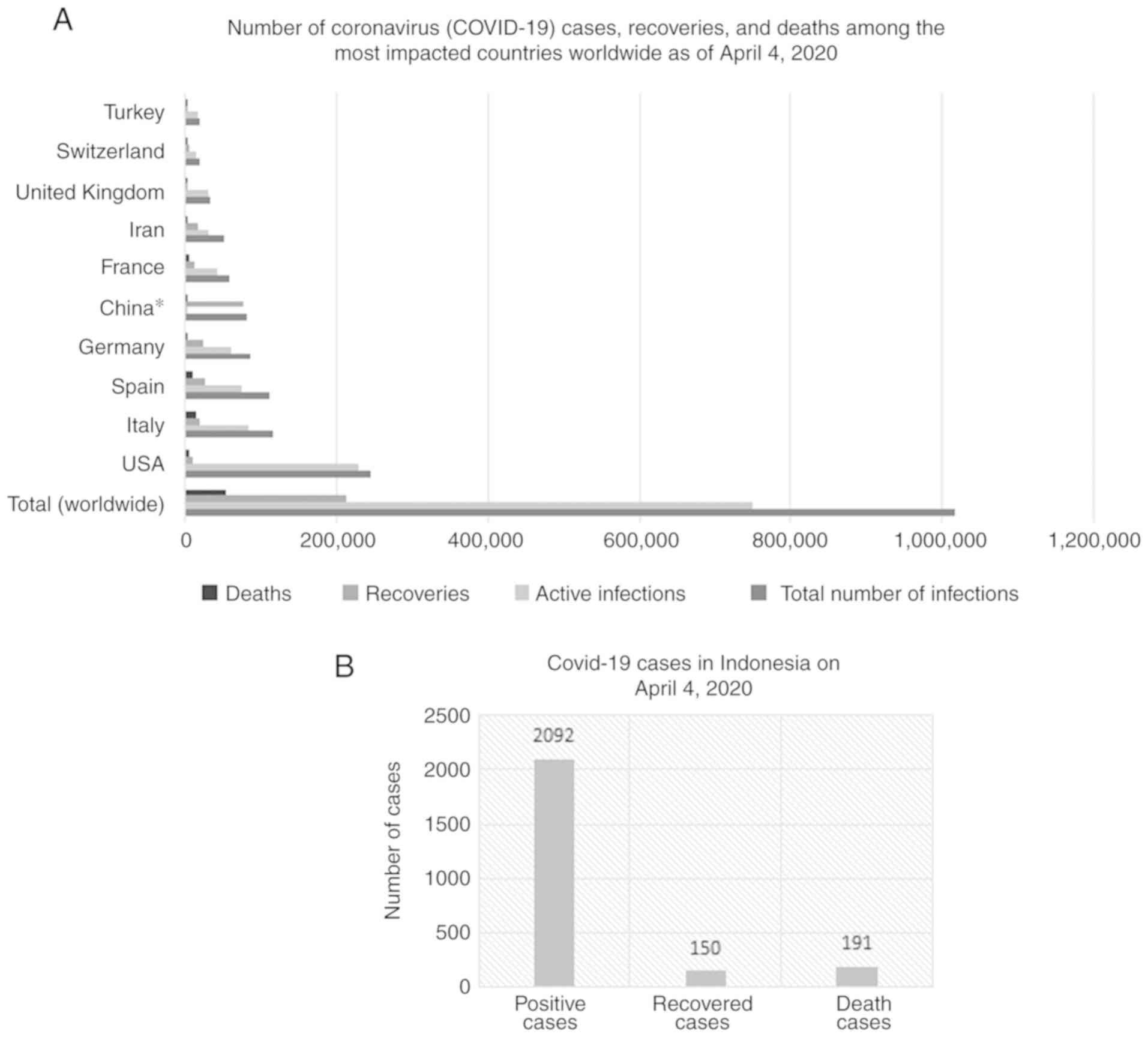
In the present review, data were collected on the
following: i) Updated data until April 4, 2020 of the total number
of COVID-19 cases for the 10 most affected countries, namely the
USA, Italy, Spain, Germany, China, France, Iran, UK, Switzerland
and Turkey, as well as the number of COVID-19 cases in Indonesia;
ii) descriptions of the symptoms and levels of illness from
COVID-19 cases; iii) demographic information on the age and sex of
COVID-19 cases; and iv) death rate by age and comorbidities. The
present review aimed to determine the characteristics of hosts
infected with COVID-19 based on categories such as age, sex,
symptoms, comorbidities and levels of illness. Moreover, these
characteristics may encourage general awareness in an effort to
prevent and avoid the spread of COVID-19 and the rising mortality
rate.
4. Pattern of COVID-19 cases
The spread of COVID-19 is currently increasing
worldwide outside the Chinese mainland. By contrast, the number of
COVID-19 cases in China has significantly decreased. Some countries
have exhibited a notable increase in COVID-19 cases as of April 4,
2020, the confirmed cases and deaths in countries, such as the USA,
Italy, Spain and Germany have exceeded the number of cases in
China. Currently, China is ranked 5th among the countries with
COVID-19 cases worldwide. The total number of COVID-19 cases,
active infections, recoveries and deaths globally reported
worldwide up to April 4, 2020 by Statista were 1,016,395, 750,024,
213,133 and 53,238, respectively (19). These data were collected over a
period of 3 months (Fig. 1A). The
highest number of active infections was in the USA, while the
highest number of deaths was in Italy. Moreover, in Indonesia, the
number of COVID-19 cases, recoveries and deaths, was approximately
2,092, 150 and 191, respectively (Fig.
1B). Even though the number of cases in Indonesia remains low,
an awareness of the widespread cases is required.
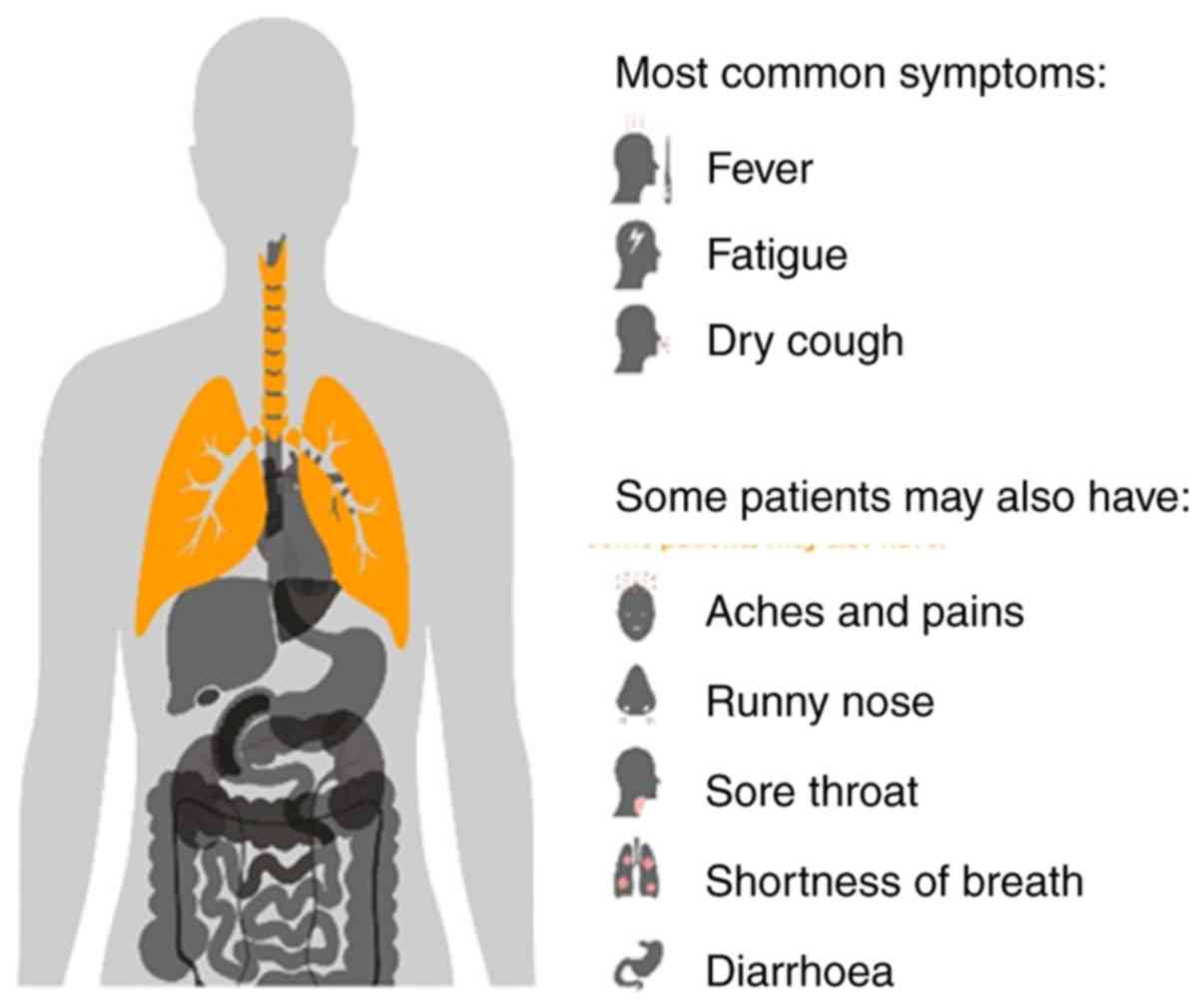
WHO has reported that the most common symptoms of
COVID-19 include fever, dry cough and fatigue. Some patients may
also have a runny nose, sore throat, headache, shortness of breath
and diarrhoea (Fig. 2) (30). These symptoms have been found at a
higher percentage in certain studies (Table I) (22-28).
When a pathogen of SARS-CoV-2 invades, the difference between
individuals and their health determines the race between how
rapidly the pathogen can spread within the body and how rapidly the
immune response can react without causing extensive organ damage.
COVID-19 may present with mild, moderate or severe illness. Among
the severe clinical manifestations, symptoms include severe
pneumonia, acute respiratory distress syndrome (ARDS), sepsis and
septic shock. In the total number of cases, there is a sudden
worsening of clinical conditions with rapid respiratory failure
after about a week. The criteria of severe respiratory
insufficiency and diagnostic criteria of sepsis and septic shock
can refer to reference (31).
Approximately 14% of infected individuals experience severe disease
and 5% become critically ill (Fig.
3) (32).
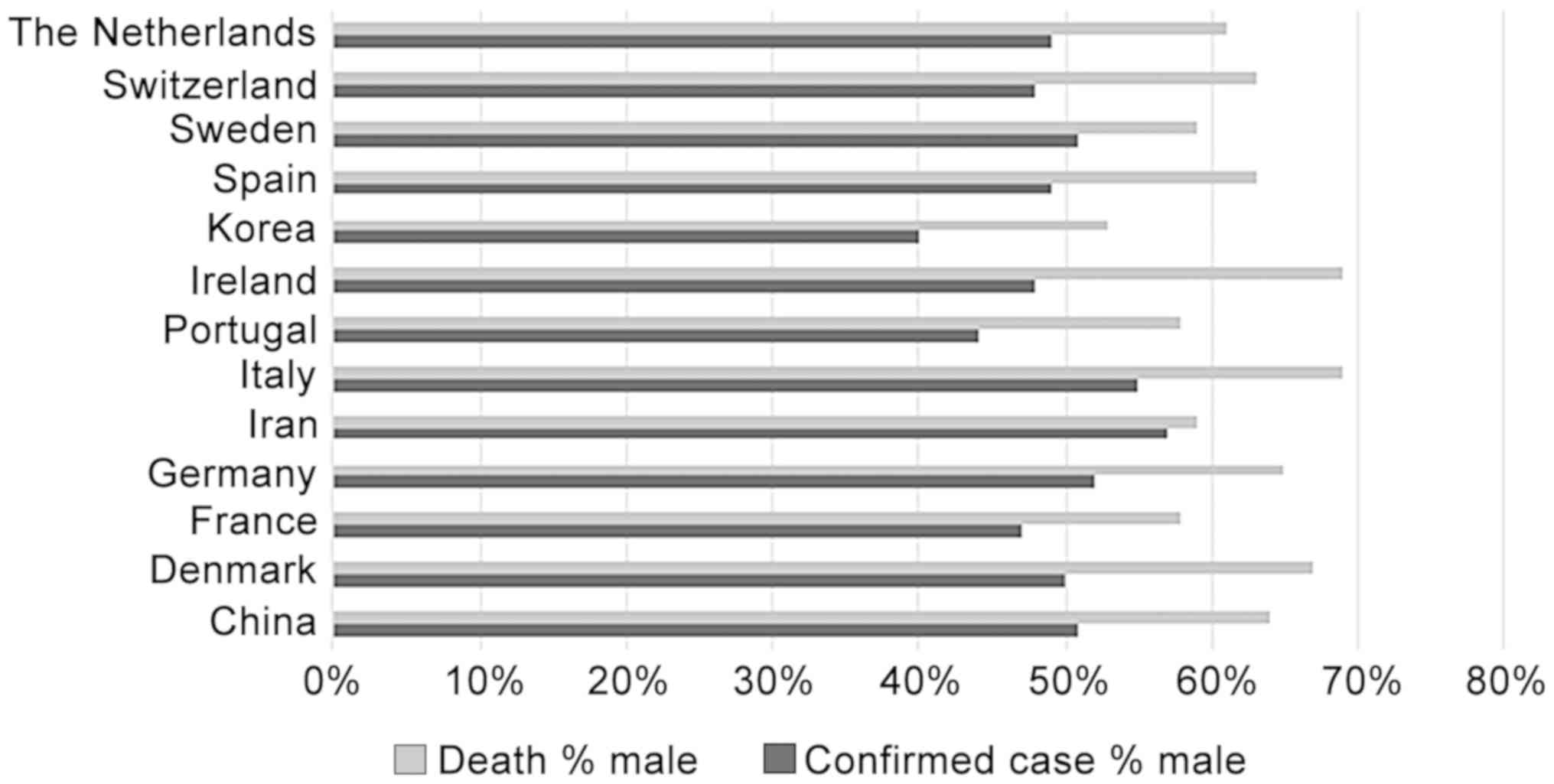
COVID-19 is the most infectious virus among the
coronavirus group, although it is not more lethal compared to the
other 2 strains of coronaviruses, SARS-CoV and MERS-CoV. Therefore,
the spread of COVID-19 is rapidly increasing, and the number of
deaths is also increasing. Furthermore, the present review observed
the characteristics of COVID-19 cases based on demographic
information, that is, the sex and age group of the individuals
infected with COVID-19. Although sex-disaggregated data for
COVID-19 have not exhibited a marked difference in the numbers of
cases between males and females to date, male patients seem to be
slightly greater in number than female patients in countries, such
as China, Germany, Iran, Italy and Sweden. By contrast, COVID-19
cases among female patients are slightly higher than those in male
patients in Denmark, France, Portugal, Ireland, Korea, Spain,
Switzerland and The Netherlands (Fig.
4). As per the data shown in Fig.
4, the proportion of deaths among confirmed cases is higher in
males than in females (female data in Fig. 4 can be calculated by subtracting
the male data from 100%). This may be caused by the fact that the
rates of tobacco smoking are substantially higher among male than
female patients (33). Preliminary
reports of individuals with severe COVID-19 disease symptoms have
found associations with existing comorbidities, including
hypertension, cardiovascular disease and certain chronic lung
diseases, and these conditions tend to burden the male population
to a greater extent globally (34).
COVID-19 can infect all age groups with the same
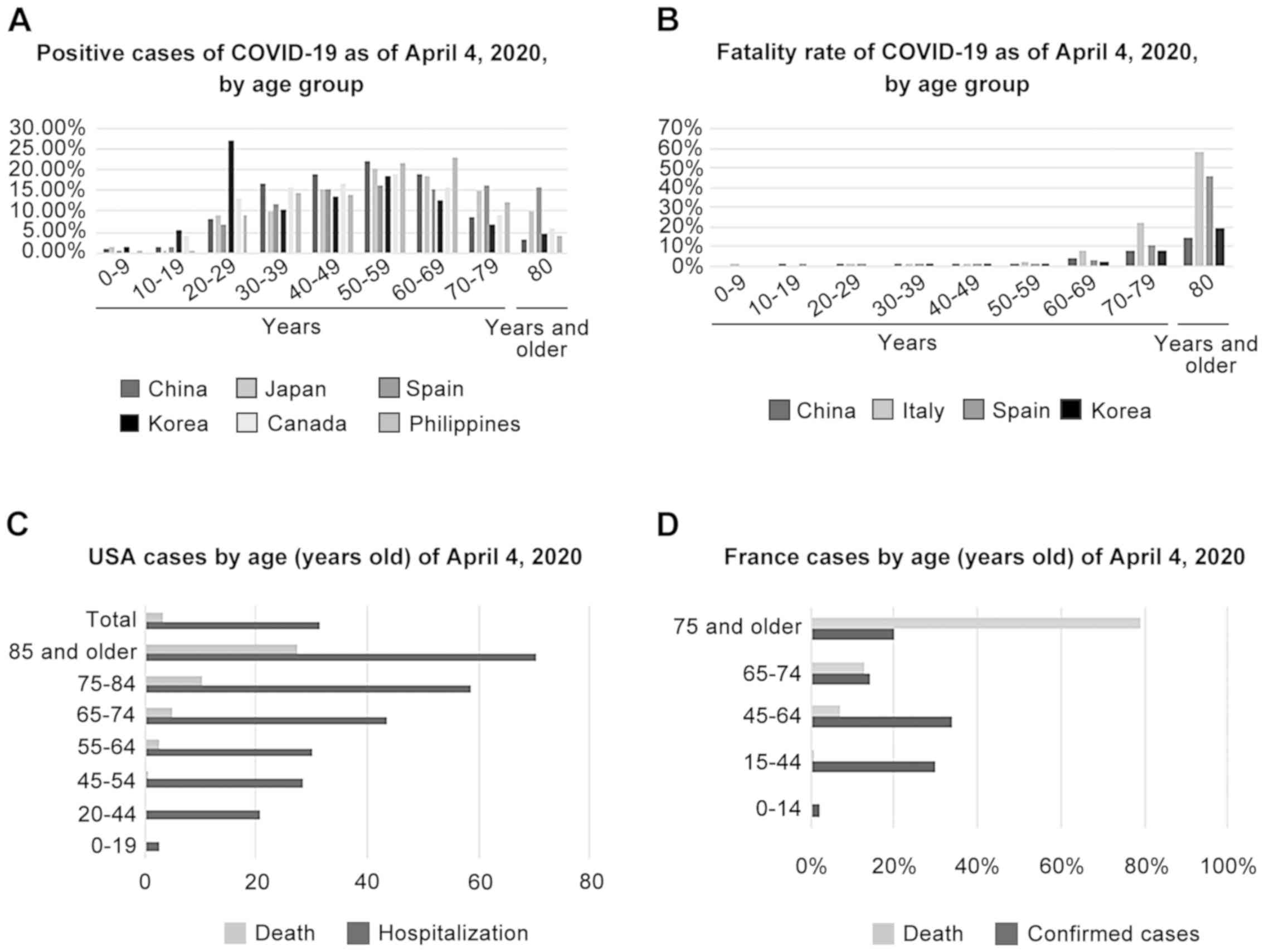
risk, particularly the ages 20-80 years (Fig. 5A, C and D);
however, the age group has an impact on deaths caused by the virus,
particularly in elderly individuals >60 years of age. The
greater the age, the higher the risk the individual has. The age
groups between 60-69, 70-79, 80 years and older have higher risks
of mortality in China, Italy, Spain and Korea. The highest number
of fatalities has been recorded in ages >80 years in these
countries (Fig. 5B). A similar
trend has also been observed in the USA and France (Fig. 5C and D). This is due to the fact that, in older
individuals, the body's immunity is weak compared with that of
younger individuals. Older individuals are vulnerable to infection,
not only by COVID-19, but also by other infectious diseases. The
human immune system has two sets of defences against viruses and
other pathogens. The first line of defence comprises cells termed
leukocytes that attack invading microbes within minutes to hours.
The second line is composed of precisely targeted antibodies and
T-cells that surge to the battlefront as late as several days
following infection. With advancing age, the body has fewer T-cells
and produces fewer virus-fighting chemicals. The cytokine barrage
varies somewhat by sex. A previous study demonstrated that older
males have more cytokine-producing cells than older females, who
have a greater number of and more effective B- and T-cells,
suggesting that elderly males generally fare worse than elderly
females as a result of a cytokine storm (35). Furthermore, previous studies have
indicated that the majority of children with COVID-19 have mild or
moderate clinical-type symptoms. In a study published in
Pediatrics, researchers conducted the first retrospective
epidemiologic analysis of disease spread and severity in 2,143
confirmed or possible paediatric COVID-19 infection cases reported
to the Chinese Centre for Disease Control and Prevention (China
CDC) from January 16 to February 8, 2020. Of the 2,143 cases, 731
(34.1%) were laboratory-confirmed and 1,412 (65.9%) were suspected.
The median patient age was 7 years (range, one day to 18 years) and
1,213 (56.6%) were boys. Using clinical signs, laboratory testing
and chest X-rays, the researchers classified 94 patients (4.4%) as
asymptomatic, 1,091 (50.9%) as having a mild disease and 831
(38.8%) as having a moderate illness (36). Other findings indicated that
COVID-19 symptoms among paediatric patients are much milder than
those in adults (37). Among
younger individuals, patients who have mild to moderate symptoms or
are asymptomatic can pose potential risks for the virus to be
transmitted to older individuals and furthermore, are likely to
become symptomatic cases, even leading to fatalities.
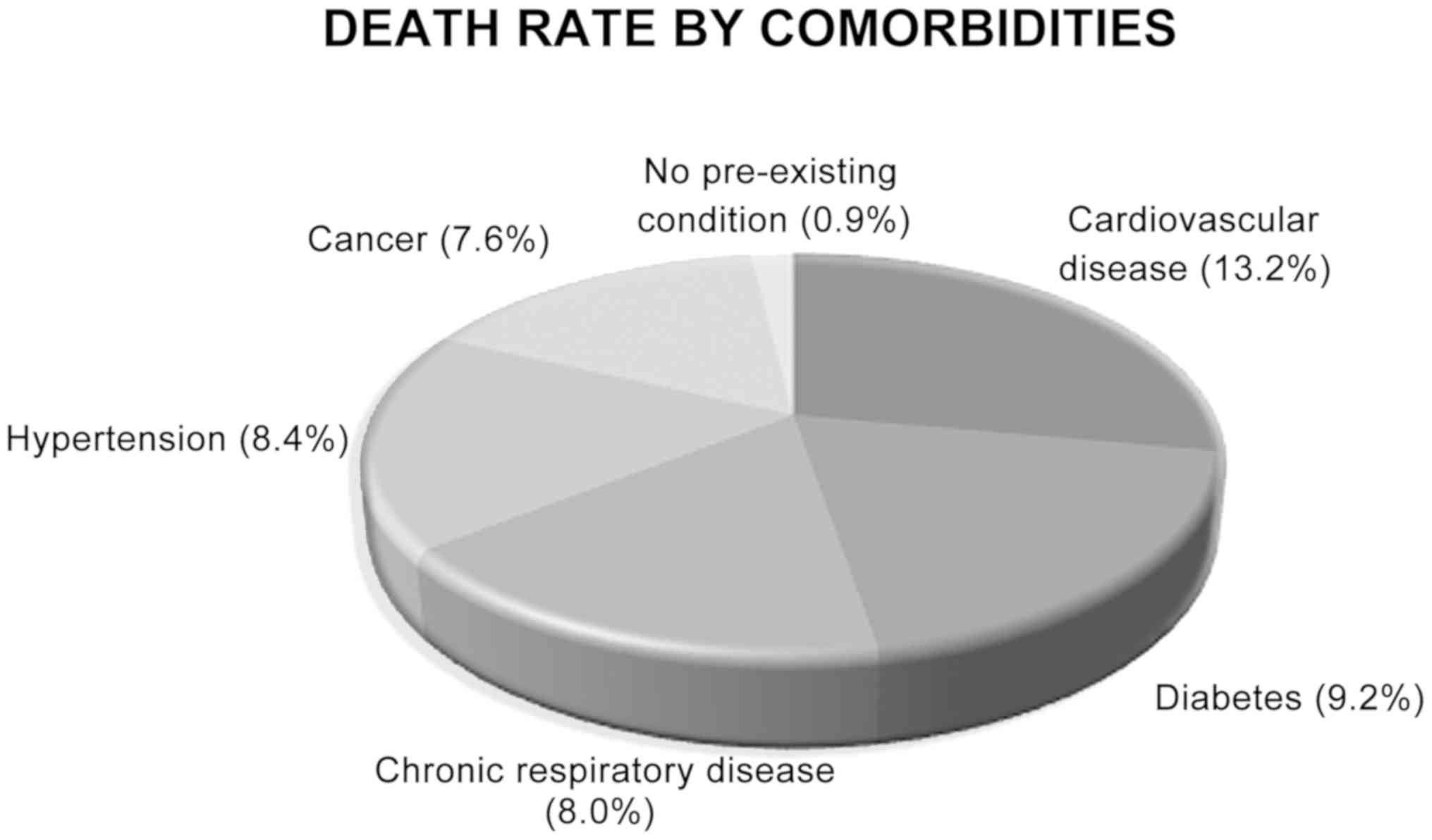
The older age group continues to be at risk of
severe diseases and death. Moreover, this condition can be worsened
by the comorbidities of older individuals. Compared to adults,
children rarely exhibit comorbidities, such as hypertension,
cardiovascular diseases, diabetes, etc. Early reports suggest that
illness severity and death caused by COVID-19 are associated with
age (>60 years old) and comorbid diseases (38). The data published by Statista
(19) revealed that cardiovascular
diseases, diabetes and hypertension are most commonly found
comorbidities in deaths caused by COVID-19 at 13.2, 9.2 and 8.4%,
respectively (Fig. 6). Similarly,
certain studies (22-28)
have demonstrated the comorbidities that contribute to illness
severity and deaths caused by COVID-19 (Table I). There are the unique
pathological features of COVID-19 cases in comparison with
non-COVID-19 caused pneumonia cases. The complete blood count (the
number of lymphocytes and platelets) was significantly decreased in
both severe and non-severe COVID-19 patients in comparison with
non-COVID-19 infected pneumonia patients, indicating that COVID-19
patients can have lymphopenia and thrombocytopenia (39). Certain studies (22-28)
included in the present review also demonstrated that the number of
lymphocytes and platelets notably decreased when compared to the
normal range of lymphocytes (1,000-4,800 in 1 µl of blood) and
platelet (150,000-450,000 in 1 µl of blood) counts.
5. Prevention and control of COVID-19
spreading
Scientists use the reproduction number (R0) to
describe the intensity of an infectious disease outbreak. If the R0
is <1, the disease will die out in a population as on average,
an infectious individual will transmit the disease to <1 other
susceptible individual. On the other hand, if the R0 is >1, the
disease will spread. A number of groups have estimated the R0 for
this novel coronavirus, SARS-CoV-2, to range between 2.6 to
4.71(11). As is known, the basic
properties of SARS-CoV-2 are yet unclear, and furthermore,
researchers consider that a number of mild cases or infections that
result in symptoms have been missed by surveillance, but
nevertheless have caused the spread of the disease. Moreover, the
susceptibility of the population affected by the infection is
unclear. SARS-CoV-2 spreads due to the ability of the virus to move
into new regions and communities. It encounters individuals with
varying health conditions that affect their susceptibility to
disease, as well as different social structures, both of which
affect its transmissibility. However, the majority of individuals
who have been infected with SARS-CoV-2 do recover.
Preventive measures are the current strategy used to
limit the rise in cases. Steps for prevention have been implemented
by certain countries and efforts have influenced the continued
spread of the virus, particularly for communities (40). These measures are the following: i)
Social and physical distancing, travel restrictions,
self-quarantine and lockdown; ii) personal and environmental
protection, such as the washing of hands, recommendations for
individuals with symptoms of acute airway infections to keep their
distance, covering one's mouth when coughing or sneezing and
disinfecting the surroundings, and wearing a mask; iii) enhancement
of the body's immune system through the consumption of nutritious
food, getting sufficient rest and taking supplements or vitamins;
iv) screening tests for tracing contact from positive cases; and v)
vaccine development.
Social and physical distancing, travel restrictions,
self-quarantine and lockdown measures are aimed to avoid direct
contact with individuals infected with SARS-CoV-2 and help to
significantly reduce one's chances of being infected by aerosol
droplets. However, there is still a possibility for the virus to
contaminate surfaces that have been touched or coughed on by
infected individuals. Therefore, the aforementioned methods need to
be combined with other prevention steps, such as the sterilization
of surroundings using disinfectants or alcohol and the frequent
washing of hands. Some countries with an increasing number of
COVID-19 cases have applied not only social and physical
distancing, but have also imposed a lockdown. A lockdown is a state
of isolation or restricted access area as a security measure,
according to which individuals are prohibited from going out or
traveling in defined areas freely due to virus outbreaks. These
countries are China (in the Hubei province), Italy, India,
Malaysia, Philippines, Poland, Ireland, Spain, Denmark, Lebanon,
France, Belgium, New Zealand and El Salvador, where lockdowns were
implemented for a period of at least 14 days, as China previously
succeeded in decreasing their COVID-19 cases by imposing a
lockdown. Moreover, Korea, which had reported a significant number
of COVID-19 cases, successfully controlled the spread of infection
with social distancing without lockdown. However, in Korea,
aggressive testing has been carried out to evaluate the health of
individuals, even on the road. It becomes crucial to stop COVID-19
from spreading by contact-tracing positive cases, even the ones
that do not exhibit any symptoms. The key to the success of Korea
thus far has been its decision to respond aggressively from the
outset. Furthermore, Singapore, Hongkong and Taiwan banned
travellers from mainland China in the early stages of the outbreak
itself. Countries imposing containment and mitigation measures can
make a difference according to demographic, social, economic and
cultural conditions.
Notably, the immune system plays an important role
in COVID-19 infection. This immune system ultimately determines
whether the patient will fall ill, recover or die. In fact, the
majority of the deaths related to COVID-19 are caused by a
previously damaged immune system, not damage caused by the virus
itself. COVID-19 is known as a self-limiting disease, depending on
the body's immunity. Younger individuals can become infected by
COVID-19, exhibit mild to moderate symptoms and become cured.
Nevertheless, they can spread the virus with no exception to
parents or older individuals, whose condition can deteriorate
following infection. Therefore, social distancing along with
staying at home can help to protect vulnerable older and
immunocompromised populations who are at a higher risk of becoming
severely infected with COVID-19. Stopping the spread of COVID-19
throughout the population would protect those who have difficulties
in fighting the infection. The most important strategies for
individuals to undertake are to frequently wash their hands with
water and soap, use portable hand sanitizers, wear masks while
going outside and avoid making contact with their faces and mouths
after interacting with a possibly contaminated environment.
Healthcare workers who take care of infected individuals should
utilize contact and airborne precautions, including Personal
Protective Equipment (PPE), such as Negativity at Approximately 95
Milliseconds (N95) or Filtering FacePiece (FFP3) masks, eye
protection, gowns and gloves to prevent transmission of the
pathogen from patients and to other people. Moreover, scientific
research is developing a vaccine and drug for COVID-19. In recent
days, China has announced the first animal tests and researchers
from the University of Queensland in Australia have also announced
after completing the 3-week in vitro study, they have moved
on to animal testing. Furthermore, in the US, the National
Institute of Allergy and Infectious Diseases (NIAID) has announced
that a phase I trial has commenced for immunisation against the
novel coronavirus in the State of Washington. All efforts are being
taken to prevent widespread transmission.
6. Conclusion and future perspectives
The COVID-19 pandemic caused by a novel strain of
coronavirus is newly reported worldwide. The pandemic has occurred
for approximately 3 months; however, the number of new cases of
COVID-19 is still increasing. The disease characterisation of
COVID-19, as regards both the virus itself and the infected host,
is still under investigation, as several aspects of the virus
remain unclear. In numerous countries, efforts are underway to
prevent the transmission of this disease with interventions being
made based on the host and viral characteristics, while continuing
to investigate vaccines and therapeutic drugs. The majority of
countries affected by COVID-19 may be able to take effective
measures. A rapid response to COVID-19 spreading is required by all
countries in order to protect the groups at risk to avoid death
tolls. Unified efforts are required from all countries in order to
combat COVID-19 and prevent the virus from spreading.
Acknowledgements
The authors would like thank to Universitas
Airlangga for the facilities provided to search data or
information, such as subscription-based journals, etc. Thus, this
assisted the authors in their search for data sources for the
preparation of the present review.
Funding
No funding was received.
Availability of data and materials
All data used in the present review were obtained
from the Statista, WHO and Worldometer databases on April 4,
2020.
Authors' contributions
LNY and FS were involved in the conceptualisation of
the study, data curation and formal analysis, writing, reviewing
and editing of the manuscript. Both authors have read and approved
the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
World Health Organization: Available from:
https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports,
2020.
|
|
2
|
Lu R, Zhao X, Li J, Niu P, Yang B, Wu H,
Wang W, Song H, Huang B, Zhu N, et al: Genomic characterisation and
epidemiology of 2019 novel coronavirus: Implications for virus
origins and receptor binding. Lancet. 395:565–574. 2020.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Reed KD, Meece JK, Henkel JS and Shukla
SK: Birds, migration and emerging zoonoses: West nile virus, lyme
disease, influenza A and enteropathogens. Clin Med Res. 1:5–12.
2003.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Woo PC, Lau SK, Lam CS, Lai KK, Huang Y,
Lee P, Luk GS, Dyrting KC, Chan KH and Yuen KY: Comparative
analysis of complete genome sequences of three avian coronaviruses
reveals a novel group 3c coronavirus. J Virol. 83:908–917.
2009.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Fong IW: Emerging animal coronaviruses:
First SARS and now MERS. Emerging Zoonoses: Feb 8, 2017 (Epub ahead
of print). doi: 10.1007/978-3-319-50890-0_4.
|
|
6
|
World Health Organization:
Director-General's remarks at the media briefing on 2019-nCoV on 11
February 2020. World Health Organization [Internet]. 2020 [cited
2020 Feb 11]. Available from: https://www.who.int/dg/speeches/detail/who-director-general-s-remarks-at-the-media-briefing-on-2019-ncov-on-11-february-2020.
|
|
7
|
Hui DS, Azhar EI, Madani TA, Ntoumi F,
Kock R, Dar O, Ippolito G, Mchugh TD, Memish ZA, Drosten C, et al:
The continuing 2019-nCoV epidemic threat of novel coronaviruses to
global health-the latest 2019 novel coronavirus outbreak in Wuhan,
China. Int J Infect Dis. 91:264–266. 2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Centers for Disease Control and
Prevention: Symptoms of Novel Coronavirus (2019-nCoV). http://www.cdc.comhttps://www.cdc.com
[Internet]. [cited 2020 Jan 30]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/about/symptoms.html,
2020.
|
|
9
|
Centers for Disease Control and
Prevention: Frequently asked question about SARS. Centers for
Disease Control and Prevention [Internet]. Available from:
http://www.cdc.gov/sars/about/faq.html,
2005.
|
|
10
|
World Health Organization: Middle East
respiratory syndrome coronavirus (MERS-CoV). Available from:
http://www.who.int/emergencies/mers-cov/en.
|
|
11
|
Liu Y, Gayle AA, Wilder-Smith A and
Rocklöv J: The reproductive number of COVID-19 is higher compared
to SARS coronavirus. J Travel Med. 27(taaa021)2020.PubMed/NCBI View Article : Google Scholar
|
|
12
|
World Health Organization: Coronavirus
disease 2019 (COVID-19): Situation report, 29 [Internet]. [cited
2020 Feb 19]. Available from: https://apps.who.int/iris/handle/10665/331118,
2020.
|
|
13
|
World Health Organization: Q&A on
coronaviruses (COVID-19): How long is the incubation period for
COVID-19? [Internet]. [cited 2020 Feb 26]. Available from:
https://www.who.int/news-room/q-a-detail/q-a-coronaviruses,
2020.
|
|
14
|
Chowell G, Abdirizak F, Lee S, Lee J, Jung
E, Nishiura H and Viboud C: Transmission characteristics of MERS
and SARS in the healthcare setting: A comparative study. BMC Med.
13(210)2015.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Centers for Disease Control and
Prevention: How COVID-19 Spreads [Internet]. Available from:
https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/how-covid-spreads.html.
|
|
16
|
World Health Organization: Modes of
transmission of virus causing COVID-19: implications for IPC
precaution recommendations. Avalilable from: https://www.who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations,
2020.
|
|
17
|
World Health Organization: Similarities
and differences-COVID-19 and influenza [Internet]. 2020. Available
from: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200306-sitrep-46-covid-19.pdf?sfvrsn=96b04adf_2.
|
|
18
|
World Health Organization: Consensus
document on the epidemiology of severe acute respiratory syndrome
(SARS) [Internet]. Available from: https://apps.who.int/%0Airis/handle/10665/70863,
2003.
|
|
19
|
Statista. COVID-19/Coronavirus [Internet].
Available from: https://www.statista.com/page/covid-19-coronavirus.
|
|
20
|
World Health Organization: Coronavirus
disease (COVID-2019) situation reports [Internet]. Available from:
https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.
|
|
21
|
Worldometer. Covid-19 Coronavirus
Pandemic. Available from: https://www.worldometers.info/coronavirus/.
|
|
22
|
Arentz M, Yim E, Klaff L, Lokhandwala S,
Riedo FX, Chong M and Lee M: Characteristics and outcomes of 21
critically ill patients with COVID-19 in Washington State. JAMA.
323:1621–1614. 2020.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J,
Wang B, Xiang H, Cheng Z, Xiong Y, et al: Clinical characteristics
of 138 hospitalized patients with 2019 novel coronavirus-infected
pneumonia in Wuhan, China. JAMA. 323:1061–1069. 2020.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Chang D, Lin M, Wei L, Xie L, Zhu G, Dela
Cruz CS and Sharma L: Epidemiologic and clinical characteristics of
novel coronavirus infections involving 13 Patients outside Wuhan,
China. JAMA. 323:1092–1093. 2020.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Young BE, Ong SWX, Kalimuddin S, Low JG,
Tan SY, Loh J, Ng OT, Marimuthu K, Ang LW, Mak TM, et al:
Epidemiologic features and clinical course of patients infected
with SARS-CoV-2 in Singapore. JAMA. 323:1488–1494. 2020.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S,
Huang H, Zhang L, Zhou X, Du C, et al: Risk factors associated with
acute respiratory distress syndrome and death in patients with
coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern
Med: Mar 13, 2020 (Epub ahead of print).
|
|
27
|
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu
Y, Zhang L, Fan G, Xu J, Gu X, et al: Clinical features of patients
infected with 2019 novel coronavirus in Wuhan, China. Lancet.
395:497–506. 2020.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Chen N, Zhou M, Dong X, Qu J, Gong F, Han
Y, Qiu Y, Wang J, Liu Y, Wei Y, et al: Epidemiological and clinical
characteristics of 99 cases of 2019 novel coronavirus pneumonia in
Wuhan, China: A descriptive study. Lancet. 395:507–513.
2020.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Kemenkes RI: Coronavirus Disease 2019.
Available from: https://covid19.kemkes.go.id/situasi-infeksi-emerging/info-corona-virus/situasi-terkini-perkembangan-coronavirus-covid-19-5-april-2020/#.Xu0kymgzbIU,
2020.
|
|
30
|
World Health Organization: Media
Statement: Knowing the risks for COVID-19. Available from:
https://www.who.int/indonesia/news/detail/08-03-2020-knowing-the-risk-for-covid-19,
2020.
|
|
31
|
Kogan A, Segel MJ, Ram E, Raanani E,
Peled-Potashnik Y, Levin S and Sternik L: Acute respiratory
distress syndrome following cardiac surgery: Comparison of the
American-European consensus conference definition versus the Berlin
definition. Respiration. 97:518–524. 2019.PubMed/NCBI View Article : Google Scholar
|
|
32
|
World Health Organization: Consensus
document on the epidemiology of severe acute respiratory syndrome
(SARS) [Internet]. Available from: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200301-sitrep-41-covid-19.pdf?sfvrsn=6768306d_2,
2020.
|
|
33
|
Cai H: Sex difference and smoking
predisposition in patients with COVID-19. Lancet Respir Med.
8(e20)2020.PubMed/NCBI View Article : Google Scholar
|
|
34
|
GBD 2016 DALYs and HALE Collaborators.
Global, regional, and national disability-adjusted life-years
(DALYs) for 333 diseases and injuries and healthy life expectancy
(HALE) for 195 countries and territories, 1990-2016: A systematic
analysis for the global burden of disease study 2016. Glob Health
Met. 390:1260–1344. 2017.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Márquez EJ, Chung CH, Marches R, Rossi RJ,
Nehar-Belaid D, Eroglu A, Mellert DJ, Kuchel GA, Banchereau J and
Ucar D: Sexual-dimorphism in human immune system aging. Nat Commun.
11(751)2020.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Dong Y, Mo X, Hu Y, Qi X, Jiang F, Jiang Z
and Tong S: Epidemiological characteristics of 2143 pediatric
patients with 2019 coronavirus disease in China. Pediatrics.
145(e20200702)2020.
|
|
37
|
Qiu H, Wu J, Hong L, Luo Y, Song Q and
Chen D: Clinical and epidemiological features of 36 children with
coronavirus disease 2019 (COVID-19) in Zhejiang, China: An
observational cohort study. Lancet Infect Dis. 20:689–696.
2020.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Yuki K, Fujiogi M and Koutsogiannaki S:
COVID-19 pathophysiology: A review. Clin Immunol.
215(108427)2020.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Zheng Y, Huang Z, Ying G, Zhang X, Ye W,
Hu Z, Hu C, Wei H, Zeng Y, Chi Y, et al: Comparative study of the
lymphocyte change between COVID-19 and non-COVID-19 pneumonia cases
suggesting uncontrolled inflammation might not be the main reason
of tissue injury. MedRxiv, 2020.
|
|
40
|
Adhikari SP, Meng S, Wu YJ, Mao YP, Ye RX,
Wang QZ, Sun C, Sylvia S, Rozalle S, Raat H, et al: Epidemiology,
causes, clinical manifestation and diagnosis, prevention and
control of coronavirus disease (COVID-19) during the early outbreak
period: A scoping review. Infect Dis Poverty. 9(29)2020.PubMed/NCBI View Article : Google Scholar
|