Introduction
Venous malformations are common vascular
malformations observed in clinical practice, mostly congenital
venous dysplasia, with an incidence of approximately 1% in the
population, of which approximately 7% of cases are adolescents.
Superficial vascular malformations are mostly characterized by skin
discolorations, with cyan-purple-colored lesions appearing on the
skin. However, some venous malformations occur deeper into the
muscle layer, and patients often exhibit symptoms of swelling and
tenderness. As the boundary of the venous malformation is not
clear, the curative effects of surgical resection are limited, and
relapse is relatively common. Thus, the effective treatment of
venous malformations has posed a significant issue in the field of
vascular surgery (1,2).
According to Puig's classification (3), venous malformations are classified
into the following 4 types: Type I, no obvious venous reflux; type
II, normal venous reflux; type III, thickening of the venous
reflux; type IV, vascularization and thickening of the malformation
cavity. Simple sclerotherapy for type I malformations can achieve
good therapeutic outcomes. However, as some type II, III and IV
malformations exhibit rapid venous reflux, good therapeutic
outcomes cannot be achieved with sclerosing agent alone. Increasing
the dose of the sclerosing agent also increases the risk of
complications. However, traditional surgical resection is gradually
retiring from the first-line treatment, since it is easy to cause
skin flap edema post-operatively, as well as necrosis and a high
recurrence rate (4,5). For the treatment of such venous
malformations, in recent years, percutaneous coil packing +
anhydrous ethanol treatment has been gradually used in clinical
practice, which has a definite effect and is widely accepted by
experts. However, the surgery involves interventional procedures,
and has absolute contraindications for patients allergic to
contrast agents (6). With the
application of certain novel medical devices, the application of
radiofrequency (RF) ablation in the treatment of venous
malformations has been frequently reported. This method is
minimally invasive and is currently favored clinically. Note that
when the lesion is adjacent to the nerve area, radiofrequency
surgery is associated with a risk of direct thermal injury to the
nerve and post-operative neuroedema (7).
Based on previous cases of venous malformations
treated by ultrasound-guided RF in the department of vascular
surgery at the authors' institution, the present study compared the
clinical data of patients who underwent coil packing and sclerosing
agent injection guided by conventional digital subtraction
angiography (DSA) in the same period, aiming to explore the
therapeutic effects of the 2 different methods in type II, III and
IV venous malformations.
Patients and methods
Study subjects
From September, 2018 to July, 2019, 53 patients with
type II, III and IV venous malformations were admitted to the
Department of Vascular Surgery, Southwest Hospital of Army Medical
University. According to the inclusion and exclusion criteria
(Table I), 41 patients were
finally enrolled in the present study, including 16 males and 25
females, aged between 6-45 years, with an average age of 26.40±6.35
years. The procedures and the complete treatment process were
explained in detail to the patients and their family members,
including the complications and associated costs; the surgical
method used for each patient was selected by the patients
themselves. Both treatment methods were explained in detail to the
patients and each patient voluntarily selected the treatment
option. All surgeries were performed by physicians with
intermediate professional titles or above at the department of
vascular surgery who had been engaged in vascular surgery or
related specialties for >5 years. After obtaining informed
consent for participating and publishing the images with their
features from all patients, the study protocol was approved by the
Ethics Committee of Southwest Hospital of Third Military Medical
University.
 | Table IInclusion and exclusion criteria used
in the present study for patient selection. |
Table I
Inclusion and exclusion criteria used
in the present study for patient selection.
| Inclusion
criteria | Exclusion
criteria |
|---|
| 1. Patients who fully
understand the purpose of the study, and actively cooperated with
the therapist | 1. Patients with
other severe diseases and contraindications related to ultrasound
or angiography (4 patients) |
| 2. Complete relevant
clinical data | 2. Incomplete
relevant clinical data (5 patients) |
| 3. Post-operative
regular reexamination and complete related data | 3. Those who refused
to cooperate with this study (1 patient) |
| | 4. Loss to follow-up
(2 patients) |
Treatment strategies i) Percutaneous
or arterial coil packing + anhydrous ethanol treatment
The surgery was performed in the DSA room, and
patient was placed in a supine position. In the case of a dorsal
malformation, the patient was placed in prone position during the
surgery. Following general anesthesia, routine disinfection and
draping were performed. Iodixanol contrast agent (Visipaque, GE
Healthcare) was used. In total, 17 patients underwent routine
catheterization angiography from the femoral artery and
trans-arterial angiography. A total of 12 patients exhibited no
obvious femoral artery pulsation touched on the body surface. As
there may be individual differences in the morphology of femoral
artery in anatomy, ultrasound is needed to locate the femoral
artery. According to the size of the malformation nest and the
diameter of the drainage vein, the diameter and quantity of the
coils (Visipaque, GE Healthcare) placed were determined for
tamponade. The total volume of anhydrous ethanol was controlled at
0.5 ml/kg body weight (some small veins were injected with 1%
polidocanol). Anhydrous ethanol emulsifier (anhydrous
ethanol:iodized oil, 5:1 v/v) was injected into the malformation
cavity under DSA fluoroscopy, and the injection was terminated
after the malformation cavity was filled with contrast agent under
fluoroscopy (8). Using anhydrous
ethanol with lipiodol was instrumental in thrombus formation by
local anesthesia injection, facilitating the surgical process.
ii) Radiofrequency ablation +
sclerotherapy
All patients who underwent RF were first localized
in the ultrasound department to draw a brief diagram. Detailed
information, such as drainage vessel and the diameter of the
vessel, were indicated on the body surface. The surgery was
performed during the day in an operating room. The patient was
placed in a supine position. The surgical site was routinely
disinfected and draped. Local anesthesia was performed at the
radiofrequency site. The drainage vein was examined by ultrasound,
and a radiofrequency needle was inserted after confirmation. The
tip of the needle was approximately 1 cm away from the normal vein
for radiofrequency ablation. After the drainage vein was closed by
ultrasound, the other drainage veins were again closed by ablation.
In the post-operative ultrasonography, sclerosing agent was
percutaneously injected (lauromacrogol or 3% polidocanol) if
venules with blood flow signals were found (9).
Evaluation of treatment efficacy
The duration of the surgery, treatment costs, blood
loss, duration of hospitalization and other routine clinical
indices were recorded in detail. Patients were requested to revisit
the hospital for re-examination at 2 weeks, 1 month, 36 months and
six months post-operatively. The follow-up period was completed in
January, 2020. Symptoms, pain degree, and the number and diameter
of the malformation cavity were recorded in detail. The criteria
for the evaluation of the efficacy of the treatments were as
follows: i) Effective: The malformation cavity continued to shrink,
symptoms were alleviated, 6 months after the re-examination of
ultrasound or contrast it was found that the malformed blood
vessels had disappeared, and the patient reported that the symptoms
had improved. If patients with recurrence were found at the
re-examination, and the above curative effects were achieved after
retreatment, treatment was regarded as effective; ii) Ineffective:
Malformed blood vessel malformation existed, symptoms were slightly
alleviated or not obvious. Malformed blood vessels could still be
observed at re-examination by ultrasound or magnetic resonance.
Changes in symptom reported by the patients were not significant.
The effective rate was calculated as follows: Effective
rate=effective cases/total no. of patients, as previously described
(10).
Statistical analysis
Measurement data are expressed as the means ±
standard deviation, and comparative analysis was performed using an
independent samples t-test or Mann-Whitney U test. Enumeration data
are expressed as a percentage (%) and the Chi-squared
(χ2) test was used for comparative analysis. All data
were analyzed and processed using SPSS 19.0 software. P<0.05
considered to indicate a statistically significant difference.
Results
A total of 41 cases were included in the present
study, of which 12 were treated with radiofrequency ablation of the
drainage vein and sclerotherapy, and 29 were treated with
DSA-assisted coil packing and sclerotherapy. All patients were
safely discharged without any severe post-operative
complications.
Comparison of clinical data in
general
Under the guidance of DSA, the average duration of
surgery was 96.34±19.68 min, the bleeding volume was 10.1±2.9 ml,
the treatment cost was 2,803±364 USD, the average number of coils
was 7.3 and anhydrous ethanol use was 7.0±3.5 ml. In total, 13
patients complained of pain post-operatively, and the pain was
relieved following the injection of painkillers, and the average
duration of hospitalization was 4.4±1.3 days. At 3 months
post-operatively, 4 patients were still found to have malformed
blood vessels upon re-examination. Ultrasound examination revealed
blood flow signals in the malformation cavity.
As regards the drainage venous radiofrequency
ablation + sclerotherapy group, the average duration of surgery was
40.08+7.15 min, the bleeding volume was 7.5±3.1 ml, the treatment
cost was 1,424±136 USD, the average puncture point was 4.4 and
polyethylene glycol (foam) use was 9±1.5 ml. In total, 6 patients
complained of pain post-operatively, and 8 patients exhibited
ecchymosis or pigmentation on their skin. The day ward model was
adopted. The patients remained in hospital for 1 h
post-operatively, and were discharged without any adverse
reactions. In the post-operative reexamination, thrombus formation
was observed in 4 cases, and the pain of pressing was relieved
slightly after a wet compress of 50% magnesium sulfate solution was
used, and blood flow signal was found in 9 cases. The detailed
results of the 2 treatments are presented in Table II.
 | Table IIStatistical data of the clinical cases
(n=41). |
Table II
Statistical data of the clinical cases
(n=41).
| Information
parameter | Radiofrequency group
(n=12) | Spring coil group
group (n=29) | P-value |
|---|
| Age (years) | 27.33±7.86 | 26.19±5.62 | 0.896 |
| Course of disease
(months) | 28.96±8.24 | 30.13±8.75 | |
| Sex | | | 0.99 |
|
Male | 5 (12.2%) | 11 (26.8%) | |
|
Female | 7 (17.1%) | 18 (44.0%) | |
| Site of
malformation | | | 0.497 |
|
Head and
neck | 4 (9.7%) | 13 (31.7%) | |
|
Trunk and
limbs | 8 (19.5%) | 16 (39.0%) | |
| Puig's type | | | 0.234 |
|
II | 6 (14.6%) | 9 (21.9%) | |
|
III | 6 (14.6%) | 15 (36.6%) | |
|
IV | 0 (0%) | 5 (12.2%) | |
| Duration of surgery
(min) | 40.08±7.15 | 96.34±19.68 | <0.001 |
| Blood loss (ml) | 7.5±3.1 | 10.1±2.9 | 0.121 |
| Duration of
hospitalization (days) | 1.0±0.0 | 4.4±1.3 | <0.001 |
| Cost of treatment
(USD) | 1,424±136 | 2,803±364 | <0.001 |
| Post-operative
pain | 6 (50.0%) | 13 (44.8%) | 0.763 |
| Dose (ml) | 9.0±1.5 (stiffening
agent) | 7.0±3.5 (anhydrous
ethanol) | 0.319 |
Comparison of the efficacy of the 2
treatments
The effect of DSA-guided coil packing on the
treatment of venous malformations is definite. In particular, in
the treatment of more complex venous malformations, the drainage
speed of the vein is reduced to the greatest extent through the
filling of the spring coil. Only a small amount of deformed blood
vessels cannot be placed with the spring coil; thus, the injection
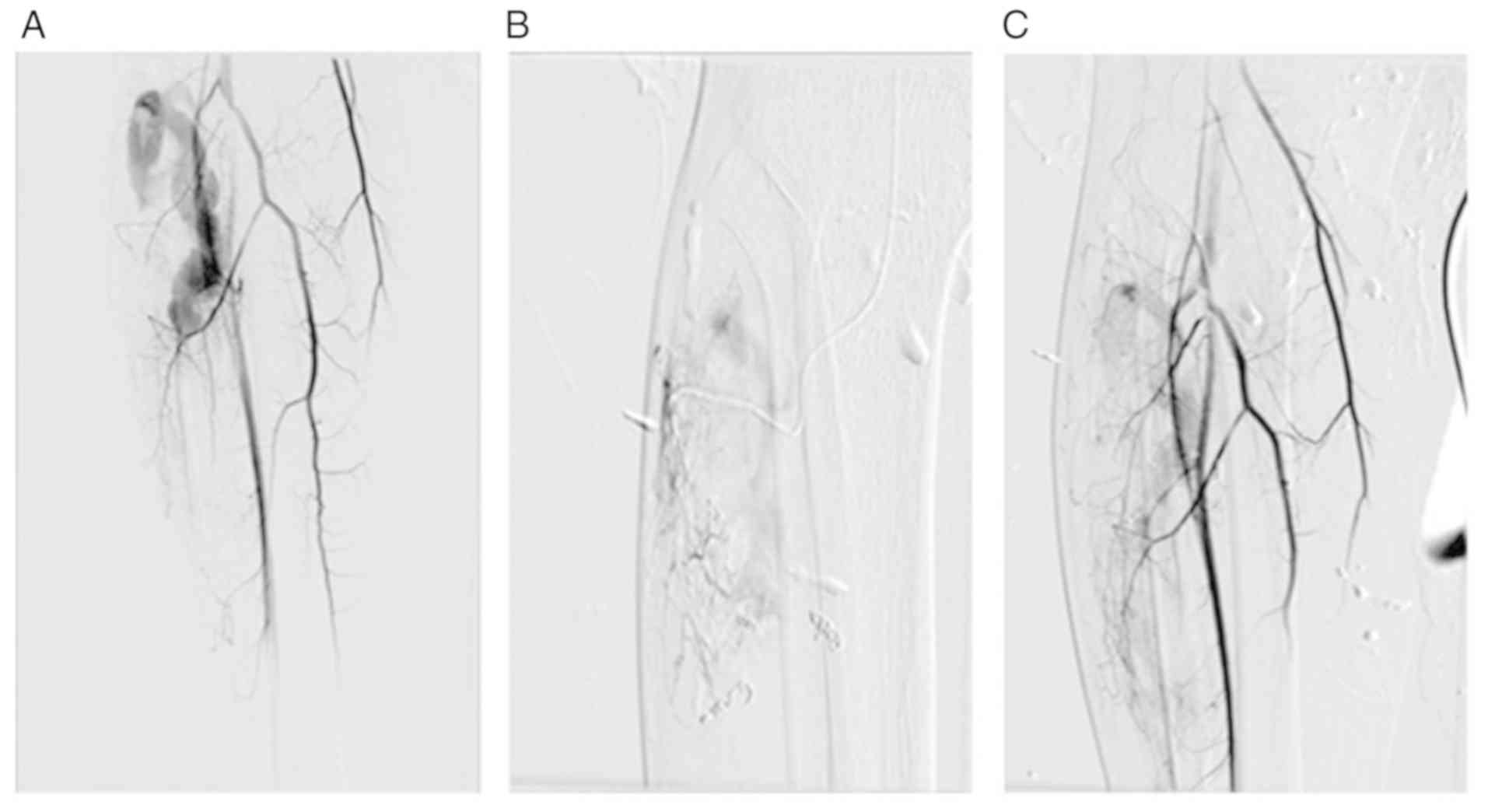
of anhydrous ethanol or polidocanol is necessary (Fig. 1). In the present study, there was
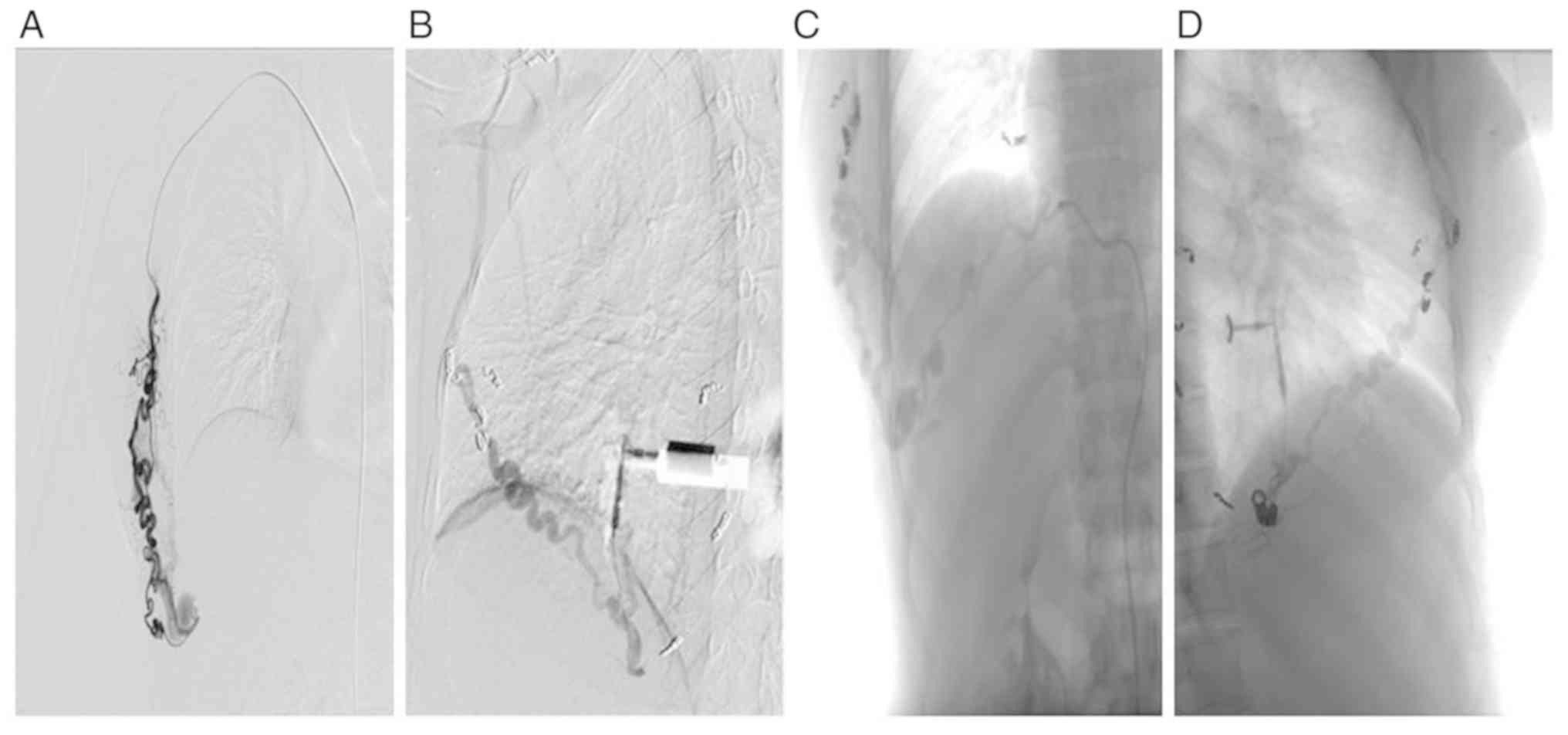
only one case of dorsal vascular malformation. After placing
multiple coils through multiple approaches, the abnormal vessels
were still observed in the angiography. It was not excluded that
the coils were not accurately placed in the malformation nest due
to some intraoperative causes (Fig.
2). The statistical data indicated that the overall treatment
efficacy was 96.5% (28/29, Table
III).
 | Table IIIComparative analysis of the treatment
efficacy of the 2 methods used. |
Table III
Comparative analysis of the treatment
efficacy of the 2 methods used.
| | Therapeutic
outcome | |
|---|
| Therapeutic
method | Effective | Ineffective | P-value |
|---|
| Radiofrequency
group | 8 | 4 | 0.033 |
| Spring coil
group | 28 | 1 | |
Ultrasound-guided radiofrequency ablation has a
positive effect in the malformation nest with clear drainage vein
and is easy to identify by ultrasound. The specific cycles of the
ablation process are determined by the sensitivity of venous
malformation to ablation. In the present study, the surgery was
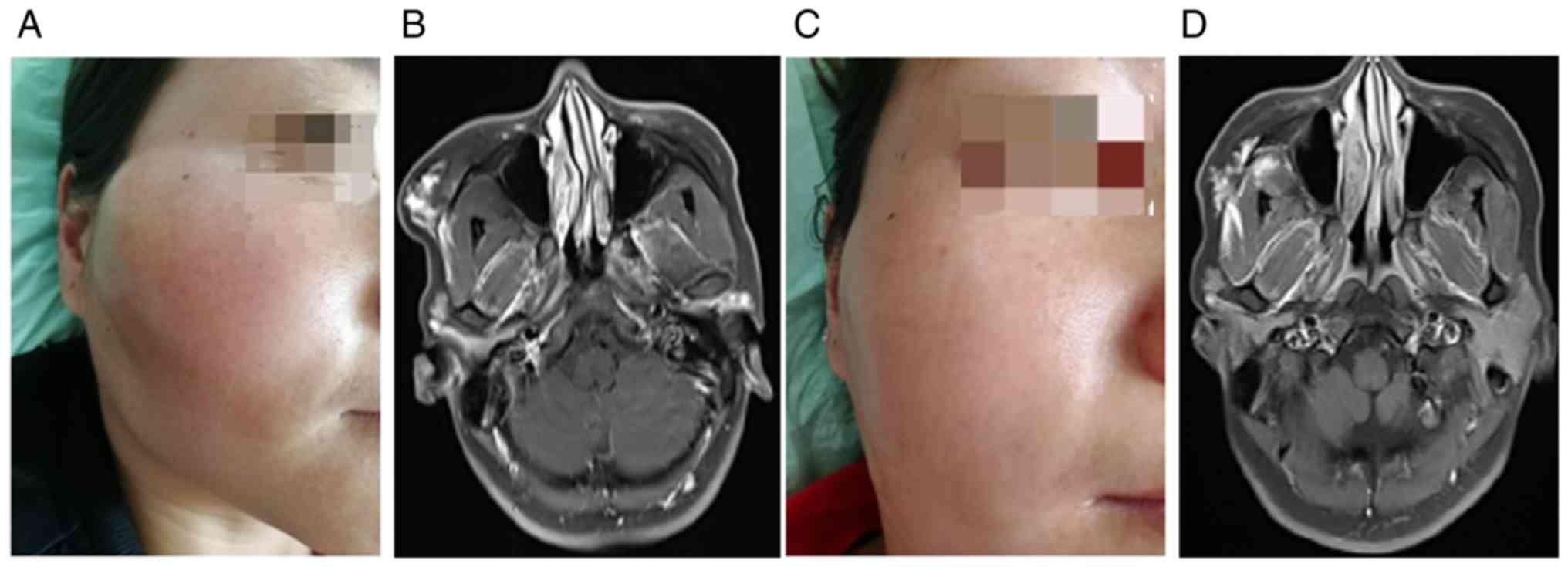
conducted in 12 patients. In a case of venous malformation on the
right side of the face, ultrasound revealed that several
malformation nests connected with the external jugular vein through
a drainage vein. Under guidance, the malformation cavity was closed
by radiofrequency and treated with a small amount of sclerosing
agent, achieving good results (Fig.
3). However, it was less effective on more complex venous
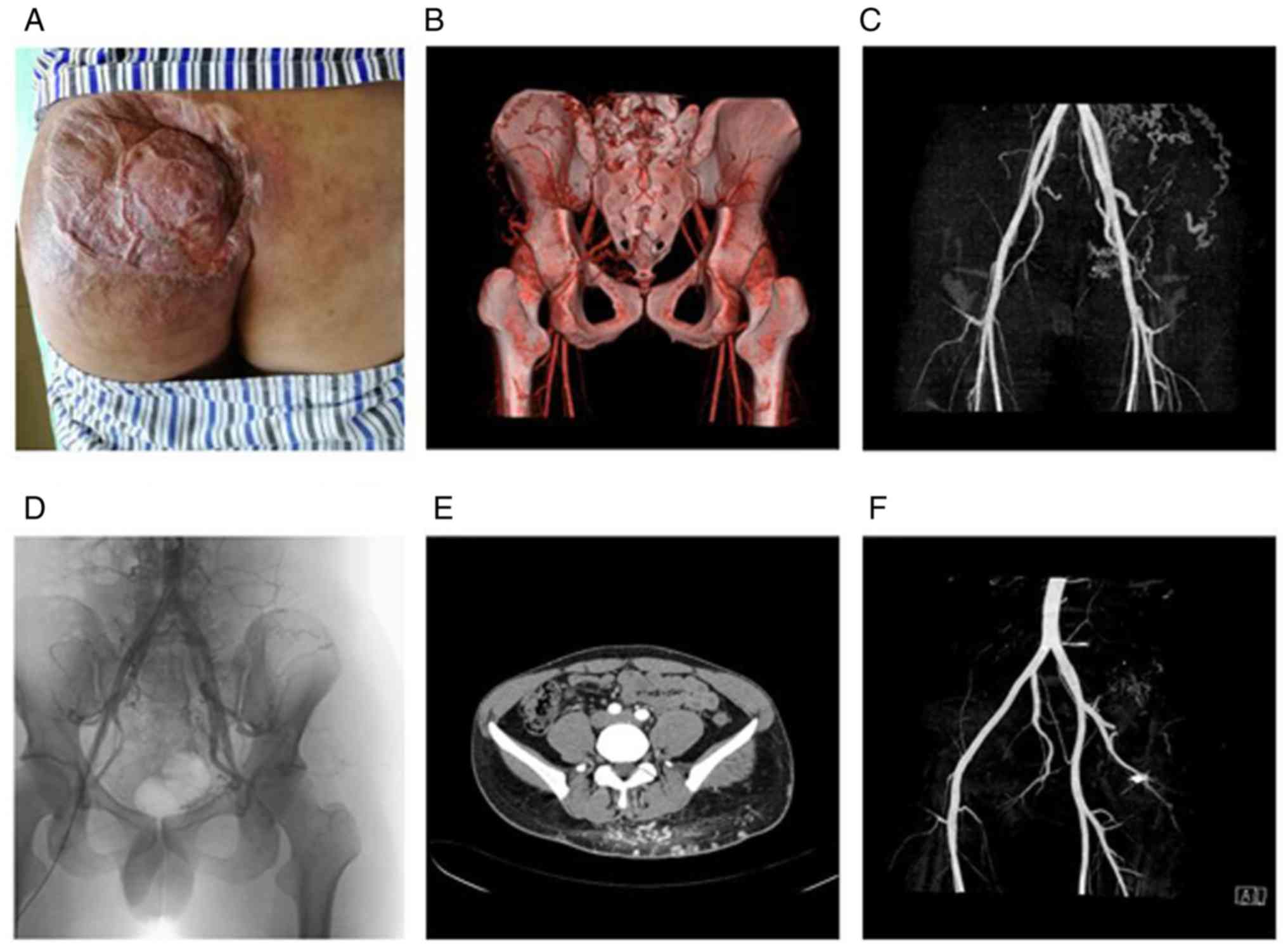
malformations. For example, in a case of venous malformation in the
buttock, given the large consumption of coils and increased costs,
radiofrequency ablation was used; however, the surgery aggravated
the ulcer. The patient complained of buttock pain, and the abnormal
blood vessels did not evidently disappear in the post-operative
angiography (Fig. 4). In addition,
there were 3 patients with recurrent deformities at only 1 week
post-operatively, which required radiofrequency again. The
statistical data indicated that the overall treatment efficacy was
66.7% (8/12, Table III).
Discussion
Type II, III and IV venous malformations exhibit
rapid blood reflux speed. During treatment, it is necessary to
block the drainage vein first, attenuate the flow rate and then
inject sclerosing agent to achieve an opitmal effect. The current
schemes of sealing drainage vein include surgical incision and
ligation, endoluminal spring coil embolization, percutaneous
puncture and spring coil packing, as well as ultrasound-guided
radiofrequency ablation of drainage vein (11). The authors used this procedure to
treat some patients in the early stages and did not obtain good
feedback on the effect. However, it remains controversial whether
all cases are suitable for coil embolization. The aim of the
present study was to explore the curative effects of these 2 types
of surgery for venous malformations by comparing cases undergoing
ultrasound and with those of radiofrequency in the same time
period, which provided reference for the clinical treatment of the
disease.
In the present study, the general clinical data were
mainly compared, such as the duration of surgery, treatment costs
and the duration of hospitalization. Through the comparison it was
found that regardless of the treatment cost or duration of surgery,
the duration of hospitalization of ultrasound-guided radiofrequency
was much lower than that of DSA, as the radiofrequency could be
completed under local anesthesia, and the trauma was small.
However, DSA surgery requires the puncture of the femoral artery;
thus, the surgical risk is relatively high. This is also the
advantage of ultrasound-guided radiofrequency therapy. As the
majority of the enrolled patients were cured after the first
treatment, the frequency of second surgery was low and it was
slightly difficult to perform a comparison. In the present study,
it was considered that both treatment methods were suitable for
almost all the venous system diseases if no surgical
contraindications are identified.
Treatment efficiency is the core index for the
evaluation of a treatment. In the present study, the efficacy of 2
groups of cases was evaluated, referring the criteria for treatment
efficacy in the treatment guidelines for vascular malformations
(12). The overall treatment
efficacy of DSA-guided venous malformation treatment was much
higher than that of radiofrequency. Under DSA, each drainage vein
is clearly displayed, including key information, such as drainage
blood speed, drainage vein diameter, etc. In the treatment process,
the spring coil can also be placed at the critical site accurately.
After the blood flow speed is reduced, the injection of a
sclerosing agent and effective compression can achieve a good
treatment effect. The reference vein diameter is used to select the
sclerosing agent. For the malformation nest with a diameter >5
mm, anhydrous ethanol is generally used. For a small one, foam
sclerotherapy is used, which has also been widely accepted by
experts (7). The key point of the
procedure is to place the spring coil in the correct position.
Whether through direct percutaneous puncture to the malformation
nest or through the femoral vein approach, the key is to fill the
malformation nest with a suitable diameter and a sufficient number
of coils. Spring coil tamponade under DSA angiography is a reliable
method for the treatment of vascular malformations at present.
Although the relevant reports may differ in the selection of
approach, auxiliary sclerosing agent, embolic material, the
surgical method and treatment principle are consistent (13).
With the popularization of radiofrequency, some
medical institutions have carried out ultrasound-assisted
radiofrequency ablation for the treatment of venous malformations;
however, the efficacy and indications remain unclear (9). The authors' department has carried
out radiofrequency in 12 cases of vein malformations; however, the
overall effect was worse than DSA. Ultrasonography has great
limitations; thus, it cannot clearly reveal the specific
information of each malformed blood vessel, and cannot accurately
guide the direction and depth of the radiofrequency needle. Due to
the high heat production of the needle, it causes edema of the
surrounding tissues and compresses other malformed blood vessels.
After the swelling disappears, revascularization occurs, which is
consistent with the reports from other institutions in China
(14). In the present study, in
this group, 3 patients experienced recurrence and the reappearance
of malformation at 1 week post-operatively, indicating that
radiofrequency has great limitations in the treatment of venous
malformations. It may however, be effective for venous
malformations with a small number of malformations and clear
layers. However, it had a limited effect for more complex venous
malformations, and the recurrence rate was higher than that of
coils under DSA angiography.
In the application of radiofrequency in the
treatment of venous malformations, some scholars consider that for
complex venous malformations, spring coil combined with
radiofrequency can achieve a better curative effect. Given the
complexity of venous malformations, available studies to date do
not provide clear indication criteria (15,16).
However, some scholars consider that multiple radiofrequency
treatments can achieve good results. Generally, the interval
between each treatment is approximately 2 weeks. Through
ultrasound, radiofrequency is applied immediately after identifying
the draining vein. In the present study, this method was also used
to treat 1 patient, achieving good results. At present, scholars in
China in related fields still have different opinions on the
indication of radiofrequency for venous malformations; thus,
further clinical research is warranted on this matter to clarify
all the related issues (17).
The present study still has some limitations:
Firstly, the sample size included was small, and thus the
statistical analysis results may be biased, limiting the
credibility of the findings. Secondly, the present study was
designed and carried out in a single center and thus, heterogeneity
was inevitable. The accuracy of the evaluation of surgical efficacy
under the guidance of the same standard at the same department may
be lower than that in a multi-center study. Thirdly, the present
study was a non-randomized controlled retrospective study, and the
evidence of the reliability of evidence-based medicine was
relatively weak. It should be noted that in the collection of
previous data, a small number of patients were not enrolled in the
study due to incomplete clinical data. It is worth considering
whether these data would have provided different results if they
were included in the statistical analysis (18,19).
In conclusion, the present study suggests that coil
packing under DSA angiography has obvious advantages in the
treatment of venous malformations, particularly for complex type
III and IV venous malformations. For type II venous malformations
with obvious relative malformed vessels, radiofrequency ablation
can be used.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article or are available from the
corresponding author on reasonable request.
Authors' contributions
SY was involved in the study design, data
acquisition, data analysis and interpretation, statistical
analysis, manuscript writing and drafting, manuscript editing and
manuscript reviewing. PL was involved in the study design, data
acquisition, and manuscript writing and drafting. LS was involved
in data acquisition, data analysis and interpretation, statistical
analysis and in revising the manuscript. CH was involved in data
analysis and interpretation, statistical analysis, and in the
writing and editing of the manuscript. YH was involved in the study
design, manuscript writing and drafting, manuscript editing,
manuscript revising and manuscript reviewing. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
The study protocol was approved by the Ethics
Committee of Southwest Hospital of Third Military Medical
University. Written informed consent was obtained from all
patients.
Patient consent for publication
Written informed consent was obtained from the
patients for participating and publishing the images with their
features.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Clemens RK and Amann-Vesti BR: Vascular
malformations: New insights in classification and therapy. Dtsch
Med Wochenschr. 140:156–159. 2015.PubMed/NCBI View Article : Google Scholar : (In German).
|
|
2
|
Carqueja IM, Sousa J and Mansilha A:
Vascular malformations: Classification, diagnosis and treatment.
Int Angiol. 37:127–142. 2018.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Puig S, Casati B, Staudenherz A and Paya
K: Vascular low-flow malformations in children: Current concepts
for classification, diagnosis and therapy. Eur J Radiol. 53:35–45.
2005.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Abecassis IJ, Osbun JW and Kim L:
Classification and pathophysiology of spinal vascular
malformations. Handb Clin Neurol. 143:135–143. 2017.PubMed/NCBI View Article : Google Scholar
|
|
5
|
McCuaig CC: Update on classification and
diagnosis of vascular malformations. Curr Opin Pediatr. 29:448–454.
2017.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Benzar I: A diagnostic program of vascular
tumor and vascular malformations in children according to modern
classification. Acta Medica (Hradec Kralove). 60:19–26.
2017.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Langbroek GB, Horbach SE, van der Vleuten
CJ, Ubbink DT and van der Horst CM: Compression therapy for
congenital low-flow vascular malformations of the extremities: A
systematic review. Phlebology. 33:5–13. 2018.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Yesil S, Tanyildiz HG, Bozkurt C, Cakmakci
E and Sahin G: Single-center experience with sirolimus therapy for
vascular malformations. Pediatr Hematol Oncol. 33:219–225.
2016.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Ma LW, Levi B, Oppenheimer AJ and Kasten
SJ: Intralesional laser therapy for vascular malformations. Ann
Plast Surg. 73:547–551. 2014.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Eicker S, Turowski B, Steiger HJ and
Hänggi D: Diagnostic work-up and therapy of spinal vascular
malformations: An update. Nervenarzt. 81:719–726. 2010.PubMed/NCBI View Article : Google Scholar : (In German).
|
|
11
|
Müller-Wille R, Wildgruber M, Sadick M and
Wohlgemuth WA: Vascular anomalies (Part II): Interventional therapy
of peripheral vascular malformations. Rofo: Feb 7, 2018 (Online
ahead of print).
|
|
12
|
Mustak H, Ugradar S, Goldberg R and
Rootman D: Bevacizumab and Bleomycin combination for treatment of
orbital lymphatico-venous malformation recalcitrant to sclerosing
therapy alone. Clin Exp Ophthalmol. 46:815–816. 2018.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Abukawa H, Kono M, Hamada H, Okamoto A,
Satomi T and Chikazu D: Indications of potassium titanyl phosphate
laser therapy for slow-flow vascular malformations in oral region.
J Craniofac Surg. 28:771–774. 2017.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Eivazi B and Werner JA: Extracranial
vascular anomalies (hemangiomas and vascular malformations) in
children and adolescents-diagnosis, clinic, and therapy.
Laryngorhinootologie. 93 (Suppl 1):S185–S202. 2014.PubMed/NCBI View Article : Google Scholar : (In German).
|
|
15
|
Cornelis FH, Labrèze C, Pinsolle V, Le
Bras Y, Castermans C, Bader C, Thiebaut R, Midy D and Grenier N:
Percutaneous image-guided cryoablation as second-line therapy of
soft-tissue venous vascular malformations of extremities: A
prospective study of safety and 6-month efficacy. Cardiovasc
Intervent Radiol. 40:1358–1366. 2017.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Kucharska A, Józefczuk P, Ksiązyk M,
Labochka D and Banaszkiewicz A: Gastrointestinal vascular
malformations in patients with turner's syndrome: A systematic
review of case reports. Horm Res Paediatr. 90:39–43.
2018.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Gao Z, Zhang Y, Li W and Shi C:
Effectiveness and safety of polidocanol for the treatment of
hemangiomas and vascular malformations: A meta-analysis. Dermatol
Ther 31, 2018.
|
|
18
|
Wiesinger I, Jung W, Zausig N, Wohlgemuth
WA, Pregler B, Wiggermann P, Stroszczynski C and Jung EM:
Evaluation of dynamic effects of therapy-induced changes in
microcirculation after percutaneous treatment of vascular
malformations using contrast-enhanced ultrasound (CEUS) and time
intensity curve (TIC) analyses. Clin Hemorheol Microcirc. 69:45–57.
2018.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Iglesias Gordo J and Martínez García R:
Spinal dural arteriovenous fistulas: The most frequent vascular
malformations of the spinal cord. Radiologia. 60:237–249.
2018.PubMed/NCBI View Article : Google Scholar
|