Introduction
Spontaneous inferior epigastric artery hemorrhage
(SIEAH) is a rare condition and can lead to rectus sheath hematoma
(RSH), and may thus prove potentially fatal condition (1-5).
Bleeding can lead to hematoma and tamponade; therefore, this
episode may be self-limited (2,6-8).
However, in some cases, hemorrhaging can result in hypovolemic
shock or even death. Anticoagulant therapy has been reported to be
a risk factor of mortality (1,3,4).
Other risk factors of SIEAH include hypertension, pregnancy,
atherosclerosis, obesity, the use of corticosteroids, thrombophilia
and leukemia (1,5,8).
Initially, conservative treatment, including blood transfusion,
anticoagulation therapy and coagulation parameter correction, is
the most commonly used treatment (1,2,4,9,10).
However, in some patients with an unstable hemodynamic status,
invasive intervention is indicated (2,4,9,10).
In some selected cases, compared with open surgery, transcatheter
arterial embolization (TAE) can be a relatively safe and effective
modality for the termination of bleeding (2,9,10).
The present study describes two cases that underwent anticoagulant
therapy and developed spontaneous inferior epigastric artery (IEA)
bleeding. Both cases were successfully dealt with using TAE.
Case reports
Case 1
A 72-year-old male subject with hypertension and
coronary artery disease was diagnosed with sigmoid colon cancer
(clinical stage, cT3N1M0; stage IIIB), and sigmoid colectomy was
subsequently performed. A few hours post-surgery, the patient was
diagnosed with acute myocardial infarction. Considering the fasting
status following colorectal surgery, a heparin pump was initially
applied and this was then switched to oral antiplatelet agents
(clopidogrel, 75 mg daily; aspirin, 100 mg daily).
On post-operative day 10, the patient suffered from
bleeding from the operative wound with hypovolemic shock. The
hemoglobin level decreased from 12.0 to 9.2 g/dl. Laboratory data
revealed a normal prothrombin time (PT) and the international
normalized ratio (INR) was 1.03 (range, 0.85-1.15). Computed
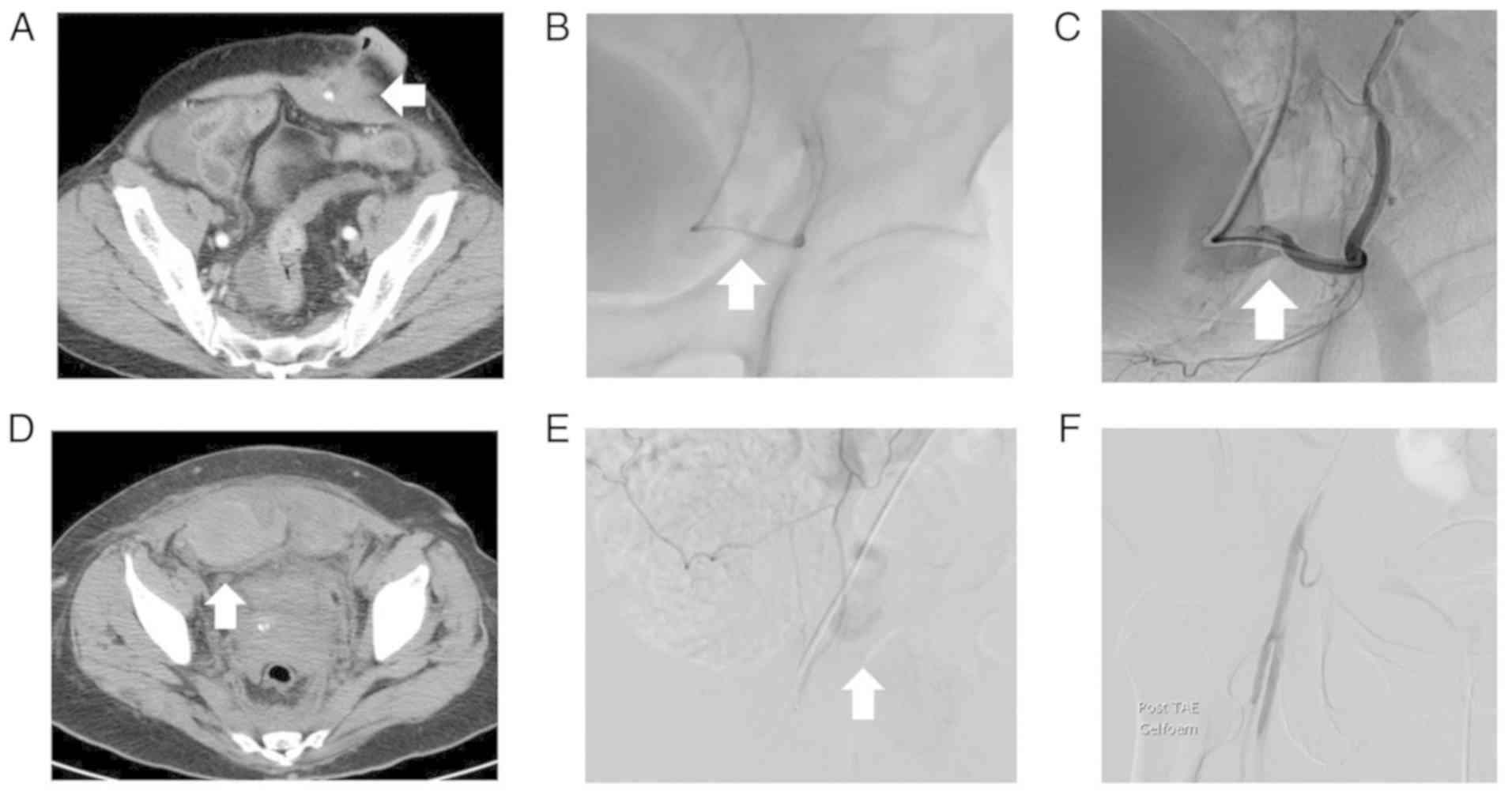
tomography (CT) revealed contrast extravasation on the left lower
abdominal wall (Fig. 1A).
Subsequent angiography revealed active bleeding from the left IEA
branches (Fig. 1B). To achieve
hemostasis, superselective catheterization and conducted
transarterial embolization we performed using Gelfoam
(SURGIFOAM®, Ethicon). Bleeding was successfully
terminated following the procedure (Fig. 1C). Owing to the state of shock of
the patient, he was referred to the surgical intensive care unit.
The patient was discharged on post-operative day 23. Written
informed consent was provided by the patient.
Case 2
A 58-year-old female with a history of mitral and
tricuspid valve replacement received anticoagulant therapy with
warfarin (3 mg/day). She visited the Outpatient Department at
Kaohsiung Medical University Chung-Ho Memorial Hospital and
complained of a productive cough and abdominal pain. A physical
examination revealed a tender mass on the lower abdominal area.
Laboratory data revealed mildly prolonged PT/INR as 1.44 (range,
0.85-1.15). Initially, conservative treatment was applied with bed
rest and ice pack application. However, the symptoms persisted, and
the hemoglobin level decreased from 10.7 to 9.3 g/dl. CT findings
revealed hematoma in the bilateral lower abdominal wall with
persistent bleeding (Fig. 1D).
Subsequent angiography revealed contrast extravasation from the
right IEA (Fig. 1E).
Superselective embolization was performed with Gelfoam
(SURGIFOAM®, Ethicon) pledgets (Fig. 1F). Post-operatively, the recovery
course was uneventful. The patient was discharged on post-operative
day 7. Written informed consent was provided by the patient. A
summary of the 2 cases is presented in Table I.
 | Table ISummary of the two cases of SIEAH. |
Table I
Summary of the two cases of SIEAH.
| Age (years)/sex | Underlying
disease | Anticoagulant | Laboratory data | Bleeding point | Embolization |
|---|
| 72/male | Acute myocardial
infarction | Heparin, clopidogrel,
aspirin | Normal | Left IEA | Gelfoam |
| 58/female | Post MVR and TVR | Warfarin | Prolonged PT/INR | Right IEA | Gelfoam |
Discussion
RSH accounts for 1-2% of acute abdominal syndrome
cases (2,5,8,11).
Although its incidence is rare, certain studies have reported a
high mortality rate of up to 25% with anticoagulant therapy
(2,4,11,12).
The etiology of RSH includes trauma, intensive muscle contractions,
and iatrogenic and anticoagulant therapy (2,3,5,12,13).
Anticoagulant therapy is one of the major risk factors of RSH
(14). In a previous study, Cherry
and Mueller reviewed 126 RSH cases and found that 25% of the
patients received anticoagulant therapy (14). SIEAH is a relatively rare condition
of RSH (2,5). The pathophysiology of SIEAH remains
unclear. One hypothesis is unrecognized minor trauma, such as
cough, sneezing, or passive joint motion (8,9,11).
Patients with an advanced age are more susceptible to suffering
from SIEAH. The cause may be rectus sheath weakness or small vessel
atherosclerosis, or both (8,9,12,13).
Nevertheless, anticoagulant therapy is strongly associated with
SIEAH (5,8,11,13).
IEA pseudoaneurysm rupture is also a rare etiology
of RSH (15-17).
The majority of cases of IEA pseudoaneurysm rupture are iatrogenic,
such as the extraction of the retention suture, surgical trauma,
drain tube insertion or removal, and therapeutic paracentesis
(15,16). Color Doppler sonography can present
‘to-and-fro’ flow (16). CT and
angiography can also reveal pseudoaneurysm and bleeding (15-17).
In the present study, in case 1, the patient exhibited RSH on
post-operative day 10. Moreover, the left para-midline incision
wound was just beyond the extravasation point (Fig. 1A). Therefore, iatrogenic IEA
pseudoaneurysm rupture can be a possible cause of RSH. However,
angiography revealed no signs of pseudoaneurysm, only contrast
extravasation. Thus, it was considered that the bleeding episode
was SIEAH related to anticoagulant therapy.
The most common presentation of SIEAH is abdominal
pain (2,8,11,12),
which can become aggravated with the patient’s movements (2,3,5,8). The
typical finding during physical examination is an abdominal mass,
which does not cross the middle abdomen (2,3,5,7,8).
Peritoneal signs, such as muscle guarding or rebounding pain, may
be positive; therefore, the presentation can mimic that of acute
abdominal syndrome (3,7,8,11,12).
Laboratory data may reveal normal coagulation function even with
active bleeding (2,11). Bedside sonography can provide some
information on differential diagnosis; however, CT is the most
effective imaging modality (5,12).
Both sensitivity and specificity can reach 100% (2,3,5,11,12).
Since hematoma caused by SIEAH is confined to the
rectus sheath, bleeding can be self-limited. Thus, conservative
treatment with compression, the use of ice packs and blood
transfusion should be the appropriate initial treatments (2,3,5,12,13).
Invasive management, such as surgical intervention with hematoma
removal and ligation of the bleeding vessel, has been the most
standard treatment, particularly for correcting hemodynamic
instability (2,3,5,7,12).
However, locating the bleeding point in hematoma and muscle fiber
is difficult (9,10). Moreover, releasing the pressure of
hematoma may aggravate bleeding (9). In patients with severe comorbidities,
old age, or other associated injuries, the surgical intervention
may result in several complications. Hence, in some selected cases,
a minimally invasive procedure, such as TAE, may be the choice of
treatment for SIEAH (3,7,8,11).
Some studies have suggested that the shock status, such as
hypotension and tachycardia, is not a contraindication of TAE
(3,10). If the diagnosis of SIEAH is
definite, embolization can be performed to achieve hemostasis
(3,8,10,11).
In patients with SIEAH with unstable hemodynamic
status, to date, data suggesting that TAE is more suitable than
traditional open surgery are lacking (10,12).
However, it is suggested that with the improvement of the imaging
system and equipment, for selected patients with anticoagulant
therapy, TAE may be the optimal treatment, as with Case 1 in the
present study, for example. In a patient with old age and acute
myocardial infarction, TAE may be superior to open surgery as the
initial treatment.
In conclusion, the standard use of anticoagulant or
antiplatelet agents may induce severe bleeding episodes, such as
SIEAH. Although the condition is rare, it can be potentially
life-threatening. The diagnosis is mainly dependent on CT findings.
Surgery is a feasible treatment; however, it has some limitations.
In some selected patients receiving anticoagulant therapy, TAE, as
a minimally invasive procedure, may be the preferred treatment for
SIEAH.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
Data sharing is not applicable to this article, as
no datasets were generated or analyzed during the current
study.
Authors' contributions
YCC was involved in the management of the cases and
the preparation of the manuscript. CLH was involved in the
management of the cases. MCS perform the transcatheter arterial
embolization. JYW was involved in the management of the cases and
the critical appraisal and review of the manuscript. All authors
have read and approved the final manuscript.
Ethics approval and consent to
participate
Written informed consent was provided by the
patients.
Patient consent for publication
The patients provided written informed consent for
the patient information to be published.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Romic I, Pavlek G, Mance M, Romic M and
Moric T: Fatal case of spontaneous rectus sheath hematoma caused by
anticoagulant and steroid therapy during hospital admission. Visc
Med. 34:225–227. 2018.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Ben Selma A and Genese T: Spontaneous
rectus sheath hematoma: An uncommon cause of acute abdominal pain.
Am J Case Rep. 20:163–166. 2019.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Azharuddin M, Gupta M and Maniar M:
Subcutaneous heparin leads to rectus sheath hematoma: A rare
complication. Cureus. 10(e2769)2018.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Stillman K and Kellar J: Rectus sheath
hematoma: An unfortunate consequence of novel anticoagulants. West
J Emerg Med. 16:420–421. 2015.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Takahashi K, Nihei T, Aoki Y, Nakagawa M,
Konno N, Munakata A, Okawara K and Kashimura H: Spontaneous rectus
sheath hematoma associated with warfarin administration: A case
report. J Rural Med. 14:245–248. 2019.PubMed/NCBI View
Article : Google Scholar
|
|
6
|
Ueno T, Nakamura T, Hikichi H, Arai A,
Suzuki C and Tomiyama M: Rectus sheath hematoma following
intravenous thrombolysis with recombinant tissue plasminogen
activator for cerebral infarction: A case report. J Stroke
Cerebrovasc Dis. 27:e237–e238. 2018.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Wick MC, Klocker J, Grundtman C, Jaschke W
and Chemelli AP: Transcatheter embolization for the management of
acute active inferior epigastric artery hemorrhages. J Endovasc
Ther. 20:561–567. 2013.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Buffone A, Basile G, Costanzo M, Veroux M,
Terranova L, Basile A, Okatyeva V and Cannizzaro MT: Management of
patients with rectus sheath hematoma: Personal experience. J Formos
Med Assoc. 114:647–651. 2015.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Sharafuddin MJ, Andresen KJ, Sun S, Lang
E, Stecker MS and Wibbenmeyer LA: Spontaneous extraperitoneal
hemorrhage with hemodynamic collapse in patients undergoing
anticoagulation: Management with selective arterial embolization. J
Vasc Interv Radiol. 12:1231–1234. 2001.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Basile A, Medina JG, Mundo E, Medina VG
and Leal R: Transcatheter arterial embolization of concurrent
spontaneous hematomas of the rectus sheath and psoas muscle in
patients undergoing anticoagulation. Cardiovasc Intervent Radiol.
27:659–662. 2004.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Hatjipetrou A, Anyfantakis D and
Kastanakis M: Rectus sheath hematoma: A review of the literature.
Int J Surg. 13:267–271. 2015.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Salemis NS: Spontaneous rectus sheath
hematoma presenting as acute surgical abdomen: An important
differential in elderly coagulopathic patients. Geriatr Gerontol
Int. 9:200–202. 2009.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Aktas H, Inci S, Dogan P and Izgu I:
Spontaneous rectus sheath hematoma in a patient treated with
apixaban. Intractable Rare Dis Res. 5:47–49. 2016.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Cherry WB and Mueller PS: Rectus sheath
hematoma: Review of 126 cases at a single institution. Medicine
(Baltimore). 85:105–110. 2006.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Sobkin PR, Bloom AI, Wilson MW, LaBerge
JM, Hastings GS, Gordon RL, Brody LA, Sawhney R and Kerlan RK Jr:
Massive abdominal wall hemorrhage from injury to the inferior
epigastric artery: A retrospective review. J Vasc Interv Radiol.
19:327–332. 2008.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Nichols-Totten K, Pollema T and Moncure M:
Pseudoaneurysm of the inferior epigastric artery: A rare
complication of laparoscopic ventral hernia repair. Surg Laparosc
Endosc Percutan Tech. 22:e25–e27. 2012.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Ruiz-Tovar J, Rubio M, Conde S, Morales V
and Martinez-Molina E: Inferior epigastric artery pseudoaneurysm:
Complication of surgical drain insertion. ANZ J Surg.
78(1139)2008.PubMed/NCBI View Article : Google Scholar
|