1. Introduction
As of September 19, 2020, the coronavirus disease
2019 (COVID-19) pandemic has spread globally, leading to >30
million confirmed cases and 943,433 deaths (1). A large-scale analysis from China
found that 81% of those infected were either asymptomatic or had
mild disease, with a case fatality rate of 2.3%. However, patients
requiring intensive care unit (ICU) care and those with acute
respiratory distress syndrome (ARDS) had high fatality rates of 49
and 52.4%, respectively (2-4).
Although there are different therapies available for the management
of patients with COVID-19, no specific antiviral therapy exists
thus far. The various therapeutic interventions are mostly
supportive therapies. Due to the extreme shortage of medical
resources, the treatment of patients critically ill with
COVID-19-associated pneumonia remains a major challenge for
clinicians. Since the adverse outcomes of patients with COVID-19
are the main cause of medical burden (2), the key intervention for the control
of COVID-19 is to reduce the occurrence of adverse outcomes.
It has been reported that severe acute respiratory
syndrome (SARS) coronavirus and SARS-CoV-2 have 79.5% genetic
homology and similar clinical manifestations characterized by rapid
progression to ARDS (5). However,
at the early stages, a number of patients with COVID-19 present
with atypical symptoms, including mild pharyngeal pain, dizziness,
anorexia and silent hypoxemia, without significant signs of
respiratory distress (6). In
effect, this delays treatment, aggravates the disease progression
of COVID-19, and increases the risk of disease transmission to
others, including healthcare workers, as vigilance is relaxed
(7-9).
In addressing this clinical dilemma, it was found that early oxygen
therapy and less activity during the asymptomatic period may reduce
the chances of the deterioration of the condition of patients
before viral shedding begins.
While performing tracheal intubation in a patient
considered to be a super-spreader of SARS coronavirus in 2003, the
author, XL, became infected. She received continuous oxygen therapy
as soon as possible and remained in bed. She had no obvious
symptoms of respiratory distress, inconsistent with her progressing
and severe chest X-ray manifestations, which were similar to those
of patients with COVID-19 reported by Pan et al (7). Some patients in the same ward
considered it unnecessary to receive oxygen therapy and remain in
bed, as they felt relatively well. However, they developed marked
respiratory distress and were subsequently admitted to the ICU.
This suggested that further attention should be paid to activity
restriction and early oxygen therapy during the asymptomatic
period.
2. Link between activity restriction and the
severity of COVID-19
Wang et al (9) reported that patients with severe
COVID-19 in Wuhan who required care in the ICU were of an older age
than patients with mild COVID-19, were more likely to have dyspnea
and anorexia, and had more underlying comorbidities, including
hypertension, diabetes, cardiovascular disease and cerebrovascular
disease. Moreover, in the early stages of infection, the severe
cases exhibited milder atypical symptoms and a longer interval from
disease onset to hospital admission. Although many patients with
COVID-19 are asymptomatic, and they do not undergo any activity
restriction prior to exhibiting profound symptoms of hypoxemia,
rapid deterioration can occur without proportional signs of
respiratory distress, which is known as ‘happy’ hypoxemia (10). Thus, inadequate attention may be
paid to critically ill patients who present with atypical symptoms
in the early stages, resulting in a lack of sufficient rest and
oxygen therapy.
By contrast, numerous patients with an exposure
history from Wuhan and/or contact with confirmed cases were
diagnosed with COVID-19. The time from the onset to the
confirmation of infection was shorter in patients with mild
disease, and this may be attributable to the policy on isolation
and medical observation that restricted patient activity, and
ensured rapid diagnosis (11).
Moreover, the rate of severely affected cases significantly
increased when hospital admission was delayed (9,12-18);
this inspired the research interests of the authors, since
hospitalization is associated with limited patient activities and
oxygen treatment is available (Table
I). Patients with infection are ‘hypermetabolic’ in the early
stages of the insult as the body initially fights to defend itself
(19). However, with a prolonged
insult, there is a progressive reduction in oxygen consumption in
severely affected patients (20).
The restriction of activity in the early stages of infection helps
to attenuate oxygen consumption and ensure sufficient energy supply
to important organs. This may provide an explanation for the
effectiveness of the quarantine policy in China, which recommends
rapid isolation or the hospitalization of patients to limit their
activity and oxygen consumption, resulting in the current reduction
in severe and critical cases of COVID-19 in China.
 | Table IAdverse outcomes of patients with
COVID-19 (rates of severe and critical cases and mortality). |
Table I
Adverse outcomes of patients with
COVID-19 (rates of severe and critical cases and mortality).
| Author | Total cases (n) | Study type | Study date range | Location | Groups (no. of
patients) | Proportion of severe
and critical cases | Mortality/% | OSTHA, median (IQR),
days | (Refs.) |
|---|
| Zhou et
al | 191 | Retrospective | December 29, 2019 to
January 31, 2020 | Wuhan | Non-survivor (54) vs.
survivor (137) | 63% Severe (35%)
Critical (28%) | 28.3% | 11 (8-14) | (13) |
| Huang et
al | 41 | Retrospective | December 31, 2019 to
January 2, 2020 | Wuhan | ICU (13) vs. non-ICU
(28) | 32% | 15% | 7 (4-8) | (14) |
| Wang et
al | 138 | Retrospective | January 1, 2020 to
January 28, 2020 | Wuhan | ICU (36) vs. non-ICU
(102) | 26.1% | 4.3% | 7 (4-8) | (9) |
| Guan et
al | 1,099 | Retrospective | Through January 29,
2020 | 31 Provinces | Severe (173) vs.
non-severe (926) | 15.7% | 1.36% | 3 (0-8) | (15) |
| Han et al | 108 | Retrospective | January 4 to February
3, 2020 | Wuhan | All mild | 0% | 0% | 1 (1-3) | (16) |
| Qian et
al | 91 | Retrospective | January 20 to
February 11, 2020 | Zhejiang | Severe (9) vs. mild
(82) | 10% | 0% | 1 (1-2) | (17) |
| Xu et al | 51 | Retrospective | January 23 to
February 18, 2020 | Changzhou | Imported (15)
Secondary (17) Tertiary (19) | 0% | 0% | CT was performed
immediately after symptom onset | (18) |
| Xu et al | 1 | Case report | January 21 to
February 3, 2020 | Wuhan | | Critical disease and
death | | 9 | (22) |
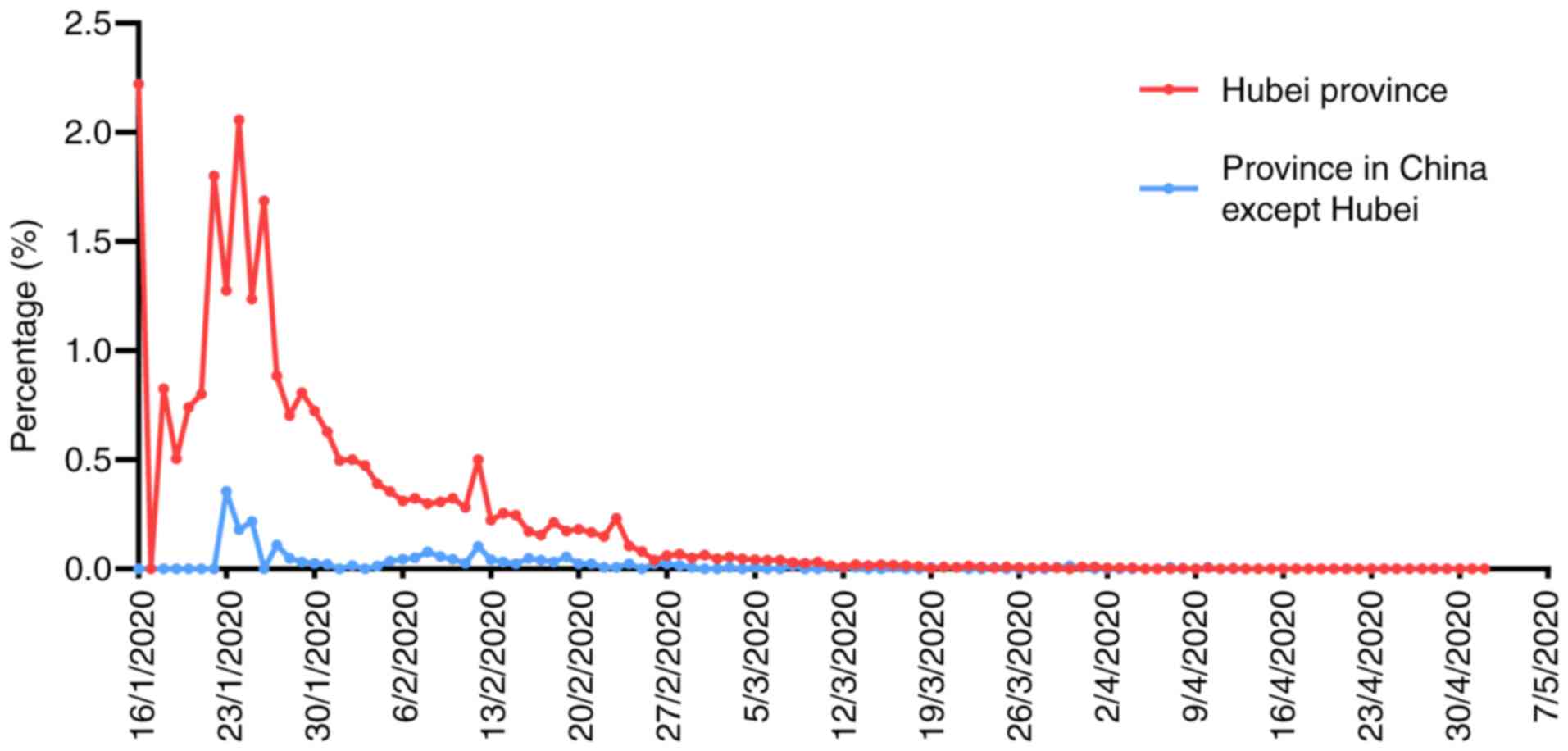
As shown in Figs. 1
and 2, the highest case fatality
rate in Hubei Province was 6.62%. However, the highest case
fatality rate in other provinces was only 0.9% during the same
period. After the COVID-19 outbreak in Hubei Province, other
provinces adopted strict anti-epidemic measures. Those who had been
in contact with confirmed cases were rapidly isolated. With the
strengthening of the quarantine measures in Hubei Province in the
later period of the epidemic, both the new cases and the case
fatality rate decreased. Thus, the disease severity of patients
with COVID-19 may be related to activity restriction (Fig. 2).
3. Importance of atypical symptoms and
earlier oxygen inhalation
Although oxygen therapy has been repeatedly
emphasized in patients with COVID-19, the optimal timing of oxygen
administration remains unclear (21); many clinicians still base their
treatment decisions on their experience and the criteria for oxygen
administration in other respiratory diseases. Xu et al
(22) reported the pathological
course of a fatal case who initially exhibited mild chills and dry
cough and continued to work. Although the patient in question
underwent high-flow oxygen therapy after developing hypoxemia, he
had impaired gaseous exchange in the lungs, which eventually caused
his death. SARS-CoV-2 mainly affects the lungs, resulting in
diffuse alveolar damage and a gelatinous mucus secretion of hyaline
membrane, thereby inhibits alveolar gas exchange (22). Once a patient develops significant
hypoxemia, it may be too late to provide oxygen therapy
(non-invasive or invasive ventilation); therefore, the optimum
timing of oxygen inhalation is critical. It is necessary to
increase the oxygen supply at an early stage before the virus
invades the lungs and hypoxemia occurs (1,8).
As mentioned above, numerous patients with COVID-19
only present atypical symptoms at the early stages of infection,
including silent hypoxemia without any significant signs of
respiratory distress (6). As a
result, such patients receive inadequate attention, leading to
rapid deterioration. It was hypothesized that the lack of timely
oxygen therapy and activity restriction was one of the main causes
of deterioration. Previous studies have confirmed that early oxygen
support may improve asymptomatic hypoxemia and reduce adverse
prognosis in infants hospitalized for acute lower respiratory tract
disease or laboratory animals under anesthesia (23,24).
Since the majority of patients with COVID-19 have a fever that
leads to partial energy loss and a high oxygen demand, the of
activities of patients should be restricted and pre-oxygenation
should be performed to ensure sufficient energy and oxygen supply
to vital organs (25). The
successful experience in China has indicated that aggressive oxygen
therapy to combat hypoxia is critical for the successful management
and treatment of patients with COVID-19 and for the reduction of
mortality.
4. Psychotherapy and music therapy for the
reduction of oxygen consumption
With limited knowledge about COVID-19, fear,
despair, anxiety, depression and irritability may prevail among
patients with COVID-19(26).
Negative emotions and psychological diseases may not only delay
recovery, but also pose challenges to treatment due to the
possibility of extreme behaviors, such as non-cooperation during
treatment (5). Psychotherapy and
music therapy may help patients to remain calm and may enhance
their confidence in overcoming the disease (27).
The ‘Voice of the Square Cabin’ music therapy has
been used by the Third Affiliated Hospital of Sun Yat-sen
University since the outbreak of the COVID-19 pandemic. The program
provides personalized online music therapy by utilizing music
artificial intelligence to provide all-round help to patients, in
combination with online psychotherapy and disease consultations.
Tranquilizing music can eliminate anxiety, dispel depression, and
reduce the heart rate and respiratory rate, thereby reducing oxygen
consumption (28). Moreover,
psychological counseling and proper nutrition are necessary to
provide in-depth treatment of COVID-19 patients.
5. Conclusions and future perspectives
The global COVID-19 pandemic will continue to affect
humanity until the development of an effective vaccine or specific
therapeutic drugs are made available. The present review article
provides new insight which may help minimize the loss of life and
prevent the development of severe disease. The present review
article discusses the hypothesis that restricting patient
activities, providing oxygen inhalation at the earlier stage of
infection, and reducing oxygen consumption, such as by reducing the
heart rate and respiratory muscle work, may result in a better
prognosis of patients with COVID-19.
Acknowledgements
The authors would like to thank Professor Yang
Qintai, Vice-President of the Third Affiliated Hospital of Sun
Yat-sen University, and Professor Yi Huimin, Director of the
Intensive Care Unit of the Third Affiliated Hospital of Sun Yat-sen
University for their careful assessment of the present review
article.
Funding
The present study was supported by the Natural
Science Foundation Project of Guangdong Province, China (no.
2018A030313618), and the Postdoctoral Science Foundation of China
(Grant nos. 2019M663260 and 2020T130148ZX).
Availability of data and materials
Not applicable.
Authors' contributions
XL and ZH contributed to the study design. XL and CC
wrote the manuscript. YG contributed to literature retrieval and
manuscript writing and to the preparation of the tables. JW
performed the literature search, figure production and manuscript
editing. YZ revised the manuscript. WY and ZH revised and edited
the manuscript. The manuscript has been read and approved by all
the authors; the requirements for authorship have been met; and
each author believes that the manuscript represents honest
work.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
World Health Organization. WHO Coronavirus
Disease (COVID-19) Dashboard. urihttps://covid19.who.int/simplehttps://covid19.who.int/.
Accessed Sep 19, 2020.
|
|
2
|
Wu Z and McGoogan JM: Characteristics of
and important lessons from the coronavirus disease 2019 (COVID-19)
outbreak in China: Summary of a report of 72314 cases from the
Chinese center for disease control and prevention. JAMA.
323:1239–1242. 2020.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Xie J, Tong Z, Guan X, Du B, Qiu H and
Slutsky AS: Critical care crisis and some recommendations during
the COVID-19 epidemic in China. Intensive Care Med. 46:837–840.
2020.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S,
Huang H, Zhang L, Zhou X, Du C, et al: Risk factors associated with
acute respiratory distress syndrome and death in patients with
coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern
Med. 180:934–943. 2020.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Coronaviridae Study Group of the
International Committee on Taxonomy of Viruses. The species severe
acute respiratory syndrome-related coronavirus: Classifying
2019-nCoV and naming it SARS-CoV-2. Nat Microbiol. 5:536–544.
2020.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Herrmann J, Mori V, Bates JHT and Suki B:
Modeling lung perfusion abnormalities to explain early COVID-19
hypoxemia. Nat Commun. 11(4883)2020.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Pan F, Ye T, Sun P, Gui S, Liang B, Li L,
Zheng D, Wang J, Hesketh RL, Yang L and Zheng C: Time course of
lung changes on chest CT during recovery from 2019 novel
coronavirus (COVID-19) pneumonia. Radiology.
295(200370)2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Zou L, Ruan F, Huang M, Liang L, Huang H,
Hong Z, Yu J, Kang M, Song Y, Xia J, et al: SARS-CoV-2 viral load
in upper respiratory specimens of infected patients. N Engl J Med.
382:1177–1179. 2020.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J,
Wang B, Xiang H, Cheng Z, Xiong Y, et al: Clinical characteristics
of 138 hospitalized patients with 2019 novel coronavirus-infected
pneumonia in Wuhan, China. JAMA. 323:1061–1069. 2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Dhont S, Derom E, Van Braeckel E, Depuydt
P and Lambrecht BN: The pathophysiology of ‘happy’ hypoxemia in
COVID-19. Respir Res. 21(198)2020.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Shi Y, Wang Y, Shao C, Huang J, Gan J,
Huang X, Bucci E, Piacentini M, Ippolito G and Melino G: COVID-19
infection: The perspectives on immune responses. Cell Death Differ.
27:1451–1454. 2020.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Zhang X, Cai H, Hu J, Lian J, Gu J, Zhang
S, Ye C, Lu Y, Jin C, Yu G, et al: Epidemiological, clinical
characteristics of cases of SARS-CoV-2 infection with abnormal
imaging findings. Int J Infect Dis. 94:81–87. 2020.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z,
Xiang J, Wang Y, Song B, Gu X, et al: Clinical course and risk
factors for mortality of adult inpatients with COVID-19 in Wuhan,
China: A retrospective cohort study. Lancet. 395:1054–1062.
2020.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu
Y, Zhang L, Fan G, Xu J, Gu X, et al: Clinical features of patients
infected with 2019 novel coronavirus in Wuhan, China. Lancet.
395:497–506. 2020.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He
JX, Liu L, Shan H, Lei CL, Hui DSC, et al: Clinical characteristics
of coronavirus disease 2019 in China. N Engl J Med. 382:1708–1720.
2020.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Han R, Huang L, Jiang H, Dong J, Peng H
and Zhang D: Early clinical and CT manifestations of coronavirus
disease 2019 (COVID-19) pneumonia. AJR Am J Roentgenol.
215:338–343. 2020.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Qian GQ, Yang NB, Ding F, Ma AHY, Wang ZY,
Shen YF, Shi CW, Lian X, Chu JG, Chen L, et al: Epidemiologic and
clinical characteristics of 91 hospitalized patients with COVID-19
in Zhejiang, China: A retrospective, multi-centre case series. QJM.
113:474–481. 2020.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Xu T, Chen C, Zhu Z, Cui M, Chen C, Dai H
and Xue Y: Clinical features and dynamics of viral load in imported
and non-imported patients with COVID-19. Int J Infect Dis.
94:68–71. 2020.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Clark A, Imran J, Madni T and Wolf SE: .
Nutrition and metabolism in burn patients. Burns Trauma.
5(11)2017.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Kreymann G, Grosser S, Buggisch P,
Gottschall C, Matthaei S and Greten H: Oxygen consumption and
resting metabolic rate in sepsis, sepsis syndrome, and septic
shock. Crit Care Med. 21:1012–1029. 1993.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Wiersinga WJ, Rhodes A, Cheng AC, Peacock
SJ and Prescott HC: Pathophysiology, transmission, diagnosis, and
treatment of coronavirus disease 2019 (COVID-19): A review. JAMA.
324:782–793. 2020.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Xu Z, Shi L, Wang Y, Zhang J, Huang L,
Zhang C, Liu S, Zhao P, Liu H, Zhu L, et al: Pathological findings
of COVID-19 associated with acute respiratory distress syndrome.
Lancet Respir Med. 8:420–422. 2020.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Riccetto AG, Ribeiro JD, Silva MT, Almeida
RS, Arns CW and Baracat EC: Respiratory syncytial virus (RSV) in
infants hospitalized for acute lower respiratory tract disease:
Incidence and associated risks. Braz J Infect Dis. 10:357–361.
2006.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Rousseau-Blass F and Pang DS:
Hypoventilation following oxygen administration associated with
alfaxalone-dexmedetomidine-midazolam anesthesia in New Zealand
White rabbits. Vet Anaesth Analg. 47:637–646. 2020.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Singer M: Critical illness and flat
batteries. Crit Care. 21 (Suppl 3)(S309)2017.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Shi L, Lu ZA, Que JY, Huang XL, Liu L, Ran
MS, Gong YM, Yuan K, Yan W, Sun YK, et al: Prevalence of and risk
factors associated with mental health symptoms among the general
population in China during the coronavirus disease 2019 pandemic.
JAMA Network Open. 3(e2014053)2020.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Schmid W, Rosland JH, von Hofacker S,
Hunskår I and Bruvik F: Patient's and health care provider's
perspectives on music therapy in palliative care-an integrative
review. BMC Palliat Care. 17(32)2018.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Koelsch S and Jäncke L: Music and the
heart. Eur Heart J. 36:3043–3049. 2015.PubMed/NCBI View Article : Google Scholar
|