Introduction
Deficient alveolar bone with horizontal and vertical
ridge imperfections encountered due to tooth extraction, advanced
periodontitis, dehiscence and window defects, or congenitally
missing teeth, present esthetic and functional challenges for
implant placement poses a constant challenge (1,2).
Therefore, in order to restore function using implant therapy in a
prosthetically favorable position, it is necessary to perform ridge
augmentation using predictable approaches, such as guided bone
regeneration (GBR), prior to, or during implant placement (3). Bone grafting is complicated by bone
resorption. The use of bone grafting materials in combination with
barrier membranes has been suggested as a strategy with which to
mitigate this disadvantage by employing the GBR approach. It
involves creating a space beneath the barrier membrane that is then
filled with new bone.
For GBR procedures, a variety of resorbable and
non-resorbable membranes have been employed (4). Enhancing membrane characteristics,
such as biocompatibility, cell occlusiveness (isolation), space
maintenance and bio-integration with the surrounding tissue, during
osteogenesis can benefit regenerated tissues (5). Although resorbable membranes do not
require a second surgical re-entry, their rate of resorption can
have a significant impact on the amount of regenerated bone
(6). The most often used
non-resorbable membranes are polytetrafluoroethylene (PTFE) and
titanium mesh (Ti-mesh). These function as a rigid barrier with
less risk of complications and tissue biocompatibility (7). Boyne et al (8) introduced the Ti-mesh in 1969 for the
repair of major osseous defects due to its stiffness and good
biocompatibility; hence it is widely employed in a variety of
surgical operations (8). For ridge
enhancement, von Arx et al (9) recommended using the Ti-mesh with
autogenous bone. The appropriate stiffness of the mesh maintains
room for new bone development, while minimizing graft displacement
and mucosal compression. In comparison to resorbable membranes, the
Ti-mesh maintains space, enables the three-dimensional restoration
of bone deformities due to the enhanced rigidity and microporous
structure, facilitating vascularity and is less vulnerable to
bacterial contamination (10). The
major drawback associated with the Ti-mesh is its exposure, which
may lead to complications related to bone regeneration (11). While autogenous bone is considered
to be the gold standard in alveolar reconstructive procedures, it
has a major drawback of limited availability and proclivity for
resorption (12). Hence, grafts
obtained from other sources, such as xenografts are favored, due to
their availability in larger volumes and desired particle size
enabling better graft manipulation during the GBR procedure
(13). Additionally, properties,
such as biocompatibility, scaffold formation (osteoconduction), the
moderate resorption rate and the capacity to preserve bone gain
volume render xenografts more suitable for use in large
reconstructive procedures (14).
Evidence from previous studies has demonstrated that ridge
augmentation performed using xenografts has been proven to be a
more predictable approach for achieving bone regeneration in the
deficient alveolar process due to their ability of stable space
maintenance (15,16). Hence, GBR performed in extensive
alveolar defects using xenografts and non-resorbable membranes has
been shown to be associated with successful outcomes (15,16).
During the GBR procedure with simultaneous implant
placement, it is necessary to create a space between the implant
and surrounding soft tissues and it should be maintained for an
appropriate duration to prevent the migration of non-osteogenic
tissues into the area (17).
Multilayered platelet-rich fibrin (PRF) can be used as a membrane
for the graft material and it provides a barrier effect for new
bone regeneration. There have been various attempts to change the
structure of PRFs and create new formulations since its launch in
2001(18). PRF, which was
introduced by Miron et al in 2017(19), is one of the recently created
formulations. Injectable-PRF (i-PRF), is a liquid formulation that
is prepared using shorter and slower centrifugal speeds, is simple
to handle, and can be combined with contemporary biomaterials.
Furthermore, circulating stem cells have been discovered in i-PRF,
which may improve its regenerative potential (20).
The present case report study focuses on the
clinical and radiographic aspects of GBR employing personalized
titanium mesh and xenograft in the maxillary anterior region with
simultaneous implant placement. Since soft tissue stability is
critical for long-term success, i-PRF and collagen membrane was
used to augment the soft tissue surrounding the implant during the
second surgical exposure.
Case report
A 27-year-old systemically healthy male patient
reported at the Department of Periodontology, SRM Dental College,
Chennai, Tamil Nadu, India, with mobility in the upper right
anterior region with a history of trauma in the upper anterior
region 2 years prior. A clinical examination revealed grade III
mobility according to the tooth mobility index published by Miller
in 1950(21) in relation to tooth
no. 11. The patient was advised for the extraction of tooth no. 11,
followed by implant prosthetic rehabilitation. An informed consent
was obtained from the patient for the treatment procedure. After 4
weeks of healing, the edentulous site in relation to tooth no.
11was inspected clinically, which revealed class III Siebert's
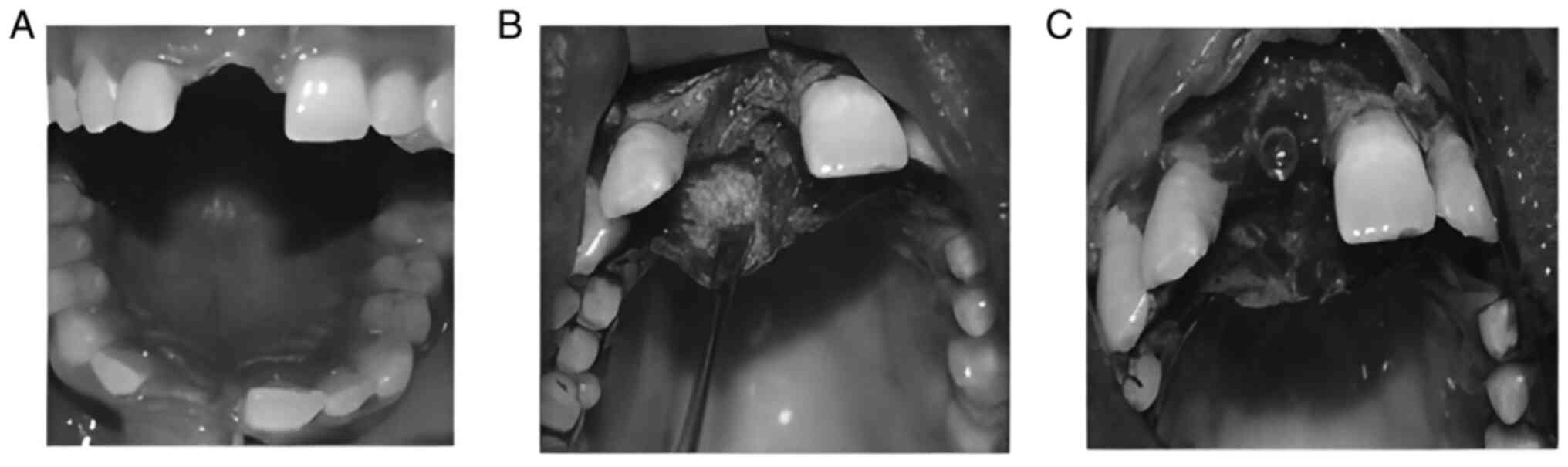
ridge defect (22) (Fig. 1A). A staged approach for implant
placement was planned following hard tissue augmentation using a
Ti-mesh and xenograft.
The intraoperative surgical procedures were as
follows: Under local anesthesia (Indoco Warren Lignox Lignocaine
2%), a paracrestal incision was performed and the full-thickness
mucosal periosteal flap was elevated extending from tooth nos. 12
to 21 (Fig. 1B). The reflection
was extended to expose the whole length of the facial cortical
plate of the alveolar ridge. The defect site was inspected
intraoperatively, an implant (ADIN Dental Implant System Ltd.) of
3.75 mm in width and a length of 13 mm was placed in the edentulous
site, primary stability was achieved and the cover screw was placed
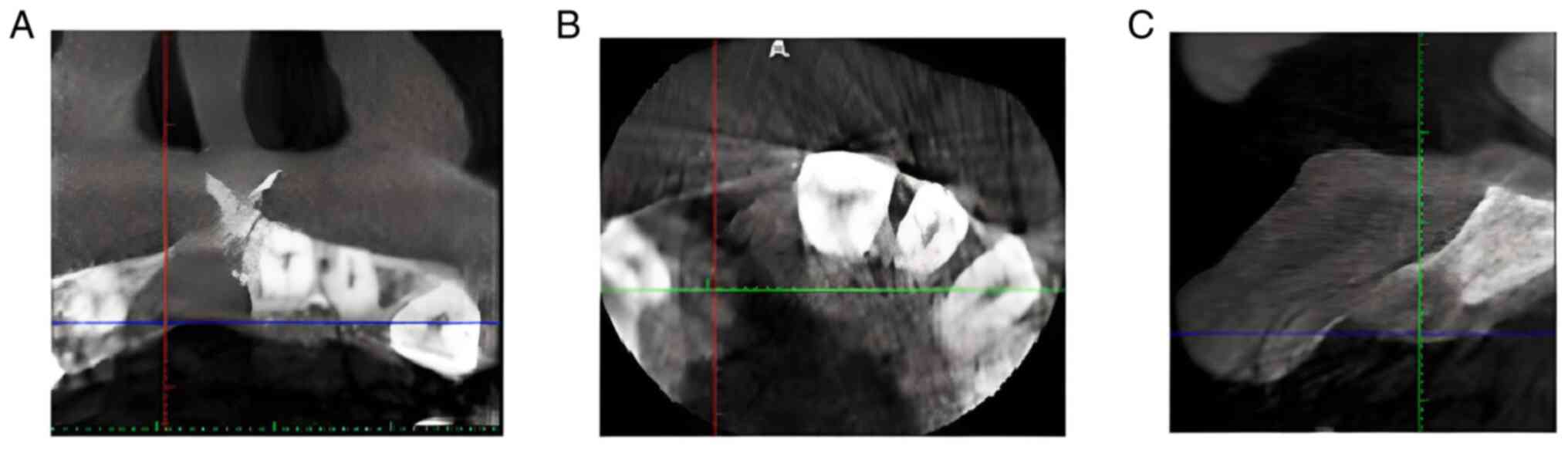
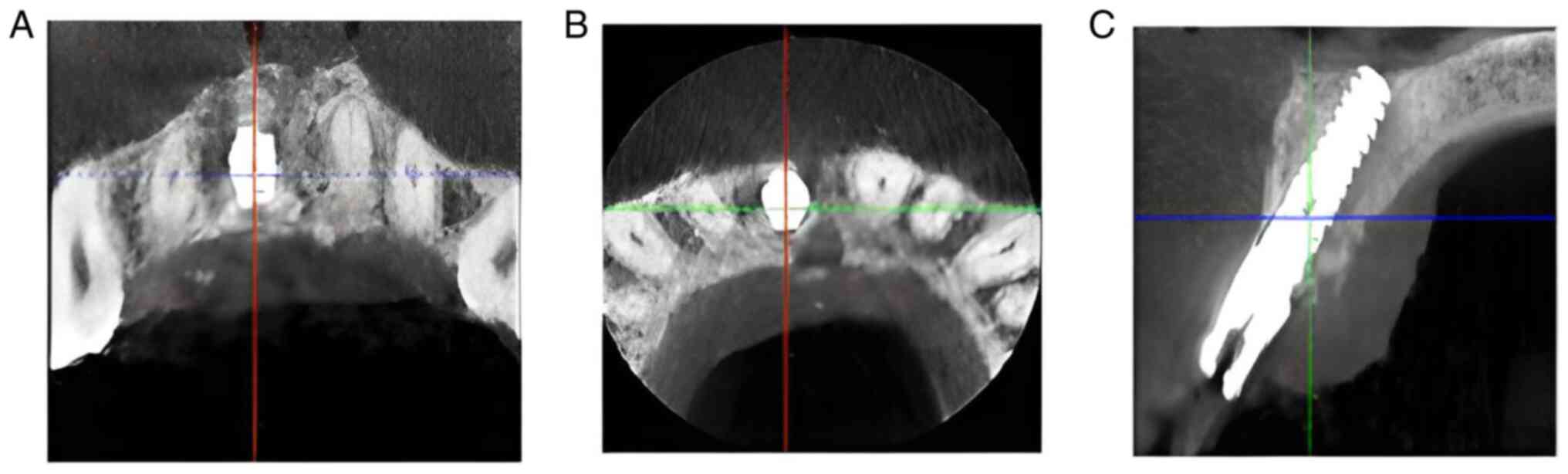
(Fig. 1C). Cone-beam computed
tomography (CBCT) was performed prior to surgery, which revealed
defect measurements of 3.6 and 10.9 mm in relation to horizontal
and vertical dimensions, respectively (Fig. 2). GBR was performed simultaneous to
implant placement, xenograft (Bio-Oss® particles,
Geistlich Pharma AG) was used along with rigid customized titanium
membrane for ridge augmentation. Depending on the size of the
alveolar defect and the future position of the prosthetic crown,
the required amount of bone augmentation required was planned and
the dimensions of the Ti-mesh was customized according to the
defect. The titanium membrane was adapted to the adjacent bone
using titanium fixing microscrews to provide the tenting effect
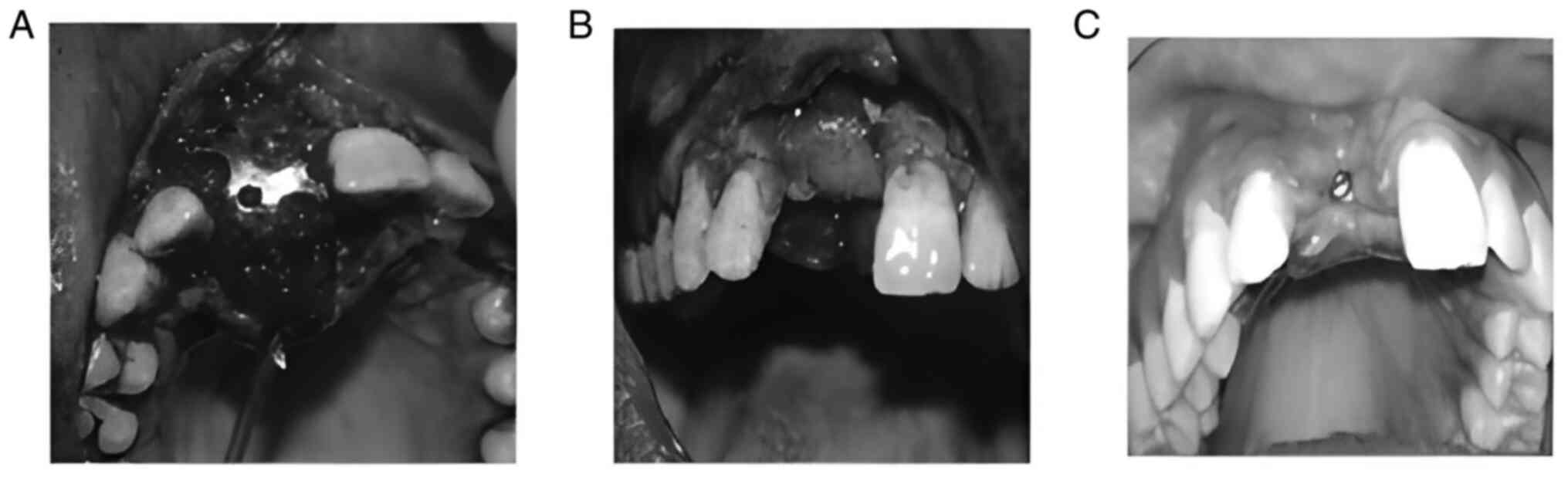
(Fig. 3A). The gap between the
Ti-mesh and the native bone was then filled with bone graft, the
graft was placed in an over contoured fashion to supplement its
final resorption. A resorbable collagen membrane
(PerioCol®, Eucare Pharmaceuticals Pvt. Ltd.) was placed
on a Ti-mesh and covered with PRF membranes (Fig. 3B). The flap was approximated and
secured with a 3-0 vicryl suture (Ethicon, Division of Johnson and
Johnson Ltd.). The patient was advised to take antibiotics and
analgesics, and was also provided instructions on oral hygiene.
Since there were no symptoms of infection or inflammation during
the 2-week follow-up, the patient was instructed to continue the
oral hygiene routine with a soft-bristle toothbrush. The patient
was advised to be followed up at 6 weeks and 3 months; however, the
patient reported for the review appointment only after 4 months,
during which time, membrane exposure was evident (Fig. 3C) in the augmented site, and the
patient was advised to use topical antibiotics
(Hexidine®-ICPA Health Products Ltd.). The patient was
regularly followed-up until the second surgical appointment. Oral
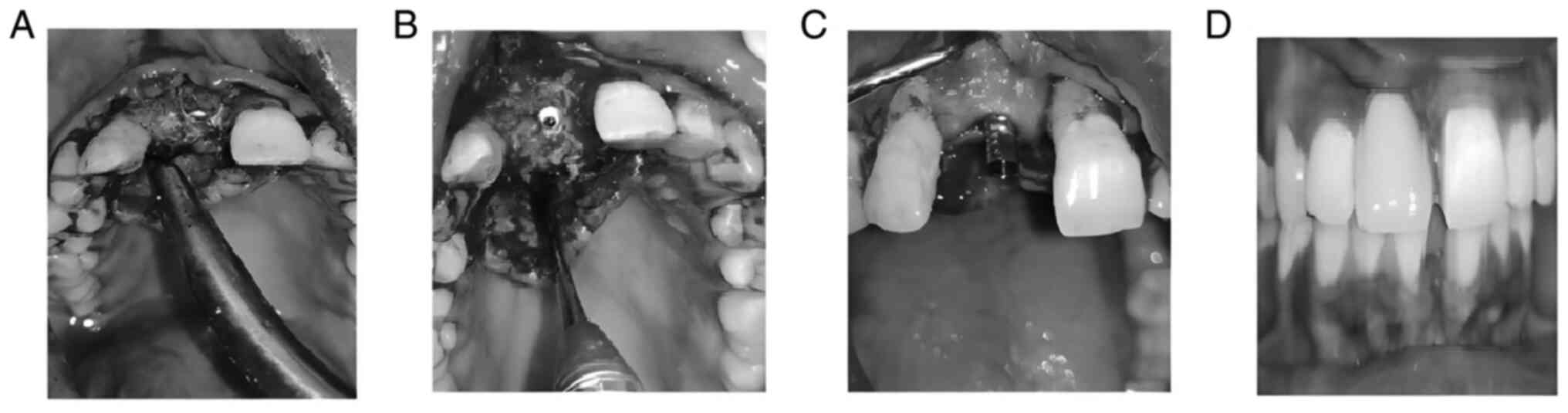
hygiene instructions were reinforced. After 5 months, during the
second stage of surgery, the Ti-mesh was removed thereby exposing
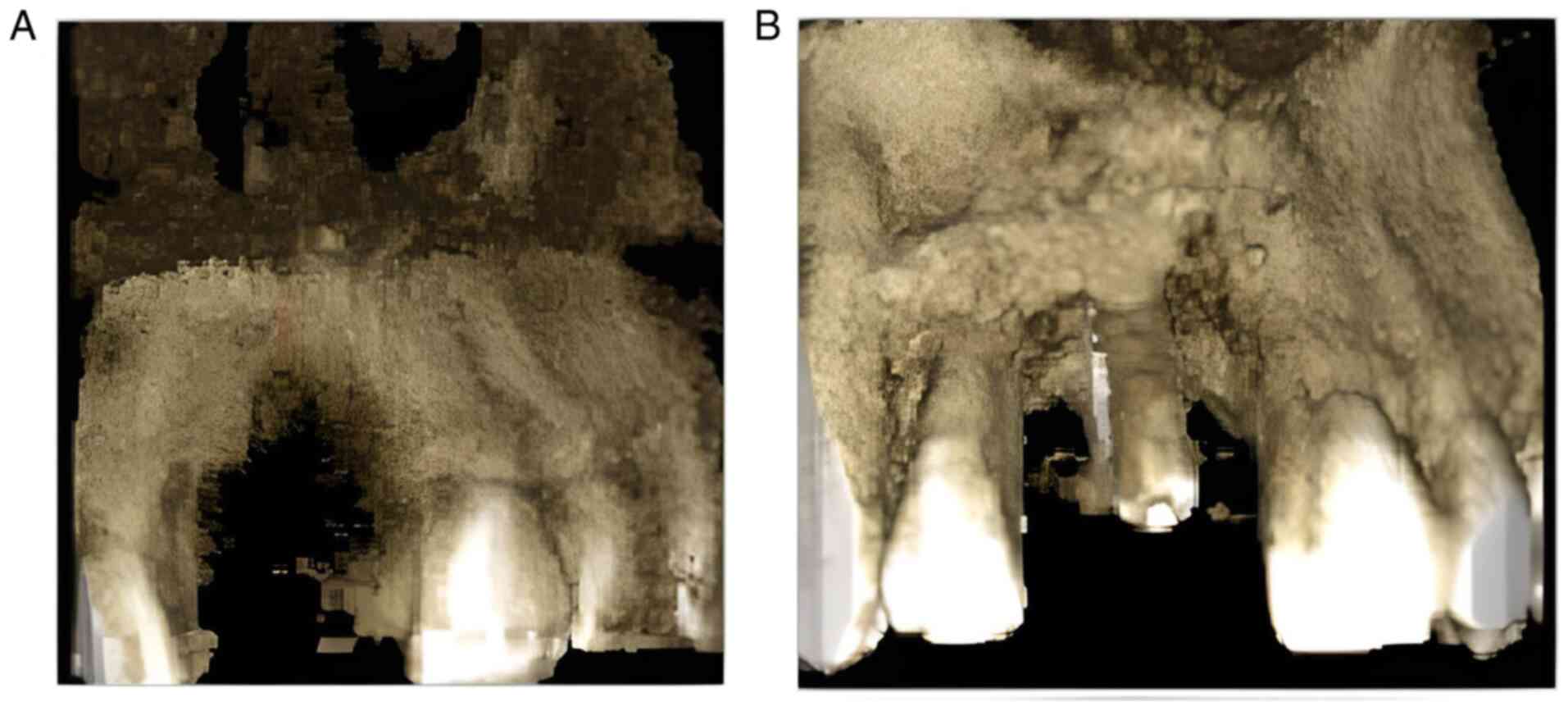
the implant (Fig. 4A). The newly
formed hard tissue was evident surrounding the implant (Fig. 4B). A collagen sponge
(Periocol™, Eucare Pharmaceuticals Private Ltd.)
reinforced with i-PRF was placed covering the buccal and lingual
aspects, around the implant, followed by flap advancement and flap
closure. Abutment placement was performed and a temporary
prosthesis was provided (Fig. 4C).
After 3 weeks of soft tissue healing, permanent restoration was
provided in relation to tooth no. 11 (Fig. 4D). At 6 months, the implant
exhibited satisfactory stability with no major biological
complications and post-operative CBCT evaluation revealed a ridge
dimension of 6.4 mm horizontally and 14 mm in the vertical
dimension of the ridge (Fig. 5).
The outcome of ridge augmentation along with implant placement was
evident when the bone gain was compared between the pre-operative
and post-operative CBCT (Fig.
6).
Discussion
Over the past decade, longitudinal studies have
emphasized that GBR is a successful and predictable technique for
clinicians to achieve vertical and horizontal ridge enhancement
(16). Using titanium mesh in
severely deficient alveolar ridges may provide a tenting effect and
stability for the graft structure and rigidity, used in this case
would provide the minimization of soft tissue in-growth into the
micro-perforation and maintain the permeability of nutrients, thus
promoting the attachment, migration and proliferation of
bone-forming cells involved in bone regeneration (23). Previous research has demonstrated
that alveolar defects, both vertical and horizontal ridge defects,
treated with titanium mesh exhibit predictable regenerative results
(7). However, the major drawback
of the Ti-mesh is the membrane exposure that may occur due to its
rigidity (11,24). The majority of studies have not
revealed any undesired regeneration results following mesh
placement (25,26). Xenografts were used due to the need
for a larger bone volume to fill the defect. A previous systematic
review reported that the implant survival for GBR was 95.5%, while
that for autologous grafts was 75% (16). In the present study, since
simultaneous implant placement along with GBR was performed,
implant dimensions were selected according to the available bone,
so that an implant insertion torque of 40 Ncm could be achieved.
After 5 months, the newly formed bone was clinically evident, the
implant was stable in position and CBCT revealed sufficient
horizontal and vertical dimensions. A previous histological
analysis revealed that xenografts can promote osteoblast
proliferation in its porous structure, facilitating angiogenesis
and early bone formation (27).
In the present case report study, the authors
attempted to perform ridge augmentation along with implant
placement using a rigid non-resorbable membrane primarily to
enhance the outcomes of GBR in cases of severe ridge deficiency and
optimal outcomes were successfully achieved in terms of bone gain
when comparing the pre-operative and post-operative CBCT.
Additionally, the augmentation of soft tissue was also considered
during the second surgical procedure to provide adequate soft
tissue support for the augmented ridge and to improve the esthetic
outcomes (23). Recent research on
i-PRF has revealed its ability to improve soft tissue thickness and
volume (20) with emphasis on
preventing peri-implant disease in the future. In the study by
Aprajita (28), GBR was performed
in the deficient maxillary anterior site using i-PRF and bone graft
simultaneously with implant placement; however, non-resorbable
membrane-like titanium was not used. Melek and Taalab (29) evaluated the effects of using i-PRF
as an adjunct to bone graft and collagen membrane for the
management of contained ridge defect at the time of extraction
before implant placement; i-PRF with its high growth factor content
may contribute to more favorable and predictable bone formation at
the grafted site. In conclusion, severe alveolar defects must be
treated with GBR prior to or simultaneous to implant placement
depending upon the remaining bone support and amount of soft tissue
thickness present.
To the best of our knowledge, the present case
report is the first of its kind to attempt an innovative strategy
of soft tissue augmentation by the placement of a collagen sponge
infused with i-PRF in the GBR site that employed a Ti-mesh and
xenograft. This augmentation technique appears to be a
therapeutically viable method of restoring soft and hard tissue
deficiencies for implant placement in severely resorbed ridges.
However, long-term radiographic and histological studies evaluating
xenograft in conjunction with rigid membrane-like Ti-mesh are
warranted to assess bone quality and final implant treatment
outcomes.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
GK was involved in the conception and design of the
study, as well as in the acquisition, analysis and interpretation
of the patient's data. HP was involved in the analysis,
interpretation of the patient's data for the study and in the
drafting of the study. DP was involved in the conception of the
study and in the acquisition of patient data. GK and HP confirm the
authenticity of all the raw data. All authors have read and
approved the final manuscript.
Ethics approval and consent to
participate
Written informed consent was obtained from the
patient for inclusion in the study and investigations were carried
out following the rules of the Declaration of Helsinki of 1975.
Patient consent for publication
The patient provided written informed consent for
the publication images related to his case.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Sclar AG, Kannikal J, Ferreira CF, Kaltman
SI and Parker WB: Treatment planning and surgical considerations in
implant therapy for patients with agenesis, oligodontia, and
ectodermal dysplasia: Review and case presentation. J Oral
Maxillofac Surg. 67 (11 Suppl):S2–S12. 2009.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Aghaloo TL and Moy PK: Which hard tissue
augmentation techniques are the most successful in furnishing bony
support for implant placement? Int J Oral Maxillofac Implants. 22
(Suppl):S49–S70. 2007.PubMed/NCBI
|
|
3
|
Cucchi A, Chierico A, Fontana F, Mazzocco
F, Cinquegrana C, Belleggia F, Rossetti P, Soardi CM, Todisco M,
Luongo R, et al: Statements and recommendations for guided bone
regeneration: Consensus report of the guided bone regeneration
symposium held in Bologna, October 15 to 16, 2016. Implant Dent.
28:388–399. 2019.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Toledano-Osorio M, Toledano M,
Manzano-Moreno FJ, Vallecillo C, Vallecillo-Rivas M,
Rodriguez-Archilla A and Osorio R: Alveolar bone ridge augmentation
using polymeric membranes: A systematic review and meta-analysis.
Polymers (Basel). 13(1172)2021.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Rakhmatia YD, Ayukawa Y, Furuhashi A and
Koyano K: Current barrier membranes: Titanium mesh and other
membranes for guided bone regeneration in dental applications. J
Prosthodont Res. 57:3–14. 2013.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Cucchi A, Sartori M, Parrilli A, Aldini
NN, Vignudelli E and Corinaldesi G: Histological and
histomorphometric analysis of bone tissue after guided bone
regeneration with non-resorbable membranes vs resorbable membranes
and titanium mesh. Clin Implant Dent Relat Res. 21:693–701.
2019.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Briguglio F, Falcomatà D, Marconcini S,
Fiorillo L, Briguglio R and Farronato D: The use of titanium mesh
in guided bone regeneration: A systematic review. Int J Dent.
2019(9065423)2019.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Boyne PJ, Cole MD, Stringer D and Shafqat
JP: A technique for osseous restoration of deficient edentulous
maxillary ridges. J Oral Maxillofac Surg. 43:87–91. 1985.PubMed/NCBI View Article : Google Scholar
|
|
9
|
von Arx T, Hardt N and Wallkamm B: The
TIME technique: A new method for localized alveolar ridge
augmentation prior to placement of dental implants. Int J Oral
Maxillofac Implants. 11:387–394. 1996.PubMed/NCBI
|
|
10
|
Xie Y, Li S, Zhang T, Wang C and Cai X:
Titanium mesh for bone augmentation in oral implantology: Current
application and progress. Int J Oral Sci. 12(37)2020.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Lizio G, Corinaldesi G and Marchetti C:
Alveolar ridge reconstruction with titanium mesh: A
three-dimensional evaluation of factors affecting bone
augmentation. Int J Oral Maxillofac Implants. 29:1354–1363.
2014.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Sakkas A, Wilde F, Heufelder M, Winter K
and Schramm A: Autogenous bone grafts in oral implantology-is it
still a ‘gold standard’? A consecutive review of 279 patients with
456 clinical procedures. Int J Implant Dent. 3(23)2017.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Buser D, Dula K, Hess D, Hirt HP and
Belser UC: Localized ridge augmentation with autografts and barrier
membranes. Periodontol 2000. 19:151–163. 1999.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Hämmerle CH, Jung RE, Yaman D and Lang NP:
Ridge augmentation by applying bioresorbable membranes and
deproteinized bovine bone mineral: A report of twelve consecutive
cases. Clin Oral Implants Res. 19:19–25. 2008.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Meloni SM, Jovanovic SA, Pisano M, De Riu
G, Baldoni E and Tallarico M: One-stage horizontal guided bone
regeneration with autologous bone, anorganic bovine bone and
collagen membranes: Follow-up of a prospective study 30 months
after loading. Eur J Oral Implantology. 11:89–95. 2018.PubMed/NCBI
|
|
16
|
Aghaloo TL, Misch C, Lin GH, Iacono VJ and
Wang HL: Bone augmentation of the edentulous maxilla for implant
placement: A systematic review. Int J Oral Maxillofac Implants. 31
(Suppl):s19–s30. 2016.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Edelmayer M, Wehner C, Ulm C, Zechner W,
Shafer D and Agis H: Which substances loaded onto collagen
scaffolds influence oral tissue regeneration?-an overview of the
last 15 years. Clin Oral Investig. 24:3363–3394. 2020.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Fujioka-Kobayashi M, Miron RJ, Moraschini
V, Zhang Y, Gruber R and Wang HL: Efficacy of platelet-rich fibrin
on bone formation, part 2: Guided bone regeneration, sinus
elevation and implant therapy. Int J Oral Implantol (Berl).
14:285–302. 2021.PubMed/NCBI
|
|
19
|
Miron RJ, Fujioka-Kobayashi M, Hernandez
M, Kandalam U, Zhang Y, Ghanaati S and Choukroun J: Injectable
platelet rich fibrin (i-PRF): Opportunities in regenerative
dentistry? Clin Oral Investig. 21:2619–2627. 2017.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Abd El Raouf M, Wang X, Miusi S, Chai J,
Mohamed AbdEl-Aal AB, Nefissa Helmy MM, Ghanaati S, Choukroun J,
Choukroun E, Zhang Y and Miron RJ: Injectable-platelet rich fibrin
using the low speed centrifugation concept improves cartilage
regeneration when compared to platelet-rich plasma. Platelets.
30:213–221. 2019.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Miller SC: Textbook of Periodontia. 3rd
edition. The Blakiston Co., Philadelphia Toronto, 1950.
|
|
22
|
Seibert JS: Reconstruction of deformed,
partially edentulous ridges, using full thickness onlay grafts.
Part I. Technique and wound healing. Compend Contin Educ Dent.
4:437–453. 1983.PubMed/NCBI
|
|
23
|
Alagl AS and Madi M: Localized ridge
augmentation in the anterior maxilla using titanium mesh, an
alloplast, and a nano-bone graft: A case report. J Int Med Res.
46:2001–2007. 2018.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Uehara S, Kurita H, Shimane T, Sakai H,
Kamata T, Teramoto Y and Yamada S: Predictability of staged
localized alveolar ridge augmentation using a micro titanium mesh.
Oral Maxillofac Surg. 19:411–416. 2015.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Her S, Kang T and Fien MJ: Titanium mesh
as an alternative to a membrane for ridge augmentation. J Oral
Maxillofac Surg. 70:803–810. 2012.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Zeynalzadeh F and Zahedpasha A: Vertical
ridge augmentation by titanium mesh. In: Stevens MR, Ghasemi S and
Tabrizi R (eds). Innovative Perspectives In Oral And Maxillofacial
Surgery. Springer, Cham, pp259-265, 2021.
|
|
27
|
Su Z, Chen Y, Wang M and Mo A: Evaluation
of immediate implantation and provisionalization combined with
guided bone regeneration by a flap approach in the maxillary
esthetic zone: A retrospective controlled study. Materials (Basel).
14(3874)2021.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Aprajita B: Guided bone regeneration using
a platelet-rich fibrin membrane and sticky bone graft along with
implant placement in maxillary anterior region: A case report. J
Adv Med Dent Sci Res. 6(2)2018.
|
|
29
|
Melek LN and Taalab MR: The use of
injectable platelet rich fibrin in conjunction to guided bone
regeneration for the management of well contained ridge defect at
the time of extraction. Egypt Dent J. 63:1197–1208. 2017.
|