Introduction
Pancreatic head cancer is one of the most malignant
digestive system tumors worldwide, which greatly contributes to the
increasing overall morbidity and mortality (1). Radical resection remains the
potential curative treatment for long-term survival. If the margins
of the specimens are all negative, an R0 resection may be achieved
(2-4).
Local recurrence around the superior mesenteric artery (SMA) is a
frequent outcome following resection, even in patients with
resectable pancreatic head cancer, which is defined as a tumor
which does not touch the artery, according to the National
Comprehensive Cancer Network (NCCN) guidelines (5). Therefore, radical dissection with a
reticular pattern around the SMA in resectable cancer of the
pancreatic head is vital in order to achieve a better
prognosis.
Due to the difficulty of the procedure and the
complex anatomical association of the organs and tissues around the
head of pancreas, the traditional surgical resection often causes
incomplete tumor resection and a high recurrence rate (6-8).
In order to avoid the shortcomings of conventional surgery, the
superior mesenteric arterial approach is recommended; this involves
the exploration of the mesenteric vessels first, and subsequently
to determine whether radical pancreaticoduodenectomy (PD) can be
performed (9). In the 1990s, Nakao
and Takagi (10) and Leach et
al (11) first described the
application of priority artery exposure in PD. In 2001, Machado
et al (12) tried the
posterior approach for PD, and indicated that this approach had
great advantages for patients with portal vein invasion who
required resection and reconstruction. In 2006, Pessaux et
al (13) first proposed the
application of the priority artery approach for PD. After this
time, the term ‘arterial priority approach’ was used worldwide, and
this procedure was adopted in PD to evaluate the main vascular
invasion before entering the irreversible surgical procedure.
The superior mesenteric arterial approach has been
reported to have the advantage of improving the R0 resection rate;
however, little is known about its effects on resectable pancreatic
head cancer. Thus, the present study aimed to determine the
function and efficacy of the superior mesenteric artery-first
approach for resectable pancreatic head cancer by comparing the
post-operative complications and patient survival.
Patients and methods
Patient screening
Data from patients with resectable pancreatic head
cancer were retrospectively collected and analyzed based on the
relevant inclusion/exclusion criteria. The patients underwent
radical PD with or without the superior mesenteric artery-first
approach at Beijing Chaoyang Hospital (Beijing, China) from
January, 2011 to December, 2019. Informed consent was obtained from
the patients and their family members. The study complied with the
Declaration of Helsinki and was approved by the Ethics Committee of
Beijing Chaoyang Hospital (No. 2020-D-302). The participants
provided written informed consent to participate in this study.
The inclusion criteria were as follows: i) An age
range between 18-80 years; ii) a pathologically confirmed diagnosis
of pancreatic ductal adenocarcinoma; iii) no distant metastasis;
iv) the pre-operative assessment of resectable pancreatic cancer
according to the NCCN 2020 guidelines (5); v) the provision of informed consent;
vi) complete availability of clinical and pathological data. The
exclusion criteria were as follows: i) Portal vein invasion
>180˚ or celiac artery invasion; ii) pathologically confirmed
non-adenocarcinoma pancreatic cancer; iii) pre-operative
neoadjuvant therapy; iv) incomplete clinicopathological data.
Patient grouping and definition
According to the surgical technique, the patients
were divided into two groups as follows: The arterial approach
group and the conventional approach group.
The inferior infracolic superior mesenteric
artery-first approach was performed as previously reported
(14): A transverse arc incision
was performed in the superior abdomen followed by exploration. The
SMA was gradually separated and exposed after opening the serosa of
the mesenteric root in the lower colon. The first jejunal artery
and the inferior pancreaticoduodenal artery were then ligated. The
SMA was separated from the tumor and skeletonized. The 14th group
lymph nodes and retroperitoneal nerve connective tissue were
removed. If the SMA could be dissociated to its origin in abdominal
aorta smoothly, it was concluded that a radical resection could be
achieved. If the SMA was found to be seriously invaded and
difficult to dissociate, the surgery was abandoned. The choice of
modus operandi needed to be individualized according to the
patient's situation. Finally, the gastrocolic ligament was incised
and the anterior lobe of transverse mesocolon was dissociated to
enter the lesser omental cavity. The stomach, pancreas, jejunum and
bile duct were resected accordingly, and pancreaticojejunostomy,
choledochojejunostomy, gastrointestinal anastomosis and
enterojejunostomy were performed in turn.
The conventional approach was performed as follows:
Kocher incision exploration was performed to free the pancreatic
head and duodenum area, to evaluate the the resectability of the
tumor, to skeletonize the common hepatic artery, celiac trunk,
superior mesenteric transarterial in turn, and to clean the
surrounding lymph tissue. The gastric body and pancreatic body, and
jejunum and bile duct were cut off, respectively. Subsequently,
pancreaticojejunostomy, choledochojejunostomy, gastrointestinal
anastomosis and enterojejunostomy were performed.
Parameters and follow-up
The intraoperative parameters were as follows:
Duration of surgery, intraoperative blood loss and intraoperative
blood transfusion. The post-operative conditions examined were the
following: Pathological examination results, complications and
recovery. The follow-up protocol included telephone and outpatient
follow-up. The follow-up time was as of March, 2021 to June,
2021.
Statistical analysis
Normal quantitative parameters are expressed as the
mean ± standard deviation, while the median (interquartile range)
was used for non-normal quantitative parameters. Fisher's exact
test was used for categorical variables, while the independent
samples unpaired t-test and Mann-Whitney U test were employed for
normal quantitative variables and non-normal quantitative
variables, respectively. The Kaplan-Meier method was used to
calculate the survival curve. The log-rank test was used to compare
the differences in the survival rates of patients between the two
groups. All data were analyzed by SPSS 24.0 software (IBM Corp.). A
value of P<0.05 was considered to indicate a statistically
significant difference.
Results
A total of 204 patients were enrolled in the present
study, including 122 males and 82 females with an average age of
63.9 years. The most common symptoms noted were asymptomatic
jaundice (65.2%), abdominal pain (27.9%) and atypical
gastrointestinal symptoms (1.5%); a total of 5.4% of the patients
underwent routine checkups. The pre-operative characteristics of
the patients are summarized in Table
I. There was a similar distribution of sex, age, smoking stats,
diabetes, biliary drainage and carbohydrate antigen 19-9 between
the two groups (P>0.05).
 | Table IComparison of the pre-operative
parameters of the patients in the two groups. |
Table I
Comparison of the pre-operative
parameters of the patients in the two groups.
| Parameter | Arterial approach
group (n=94) | Conventional approach
group (n=110) | P-value |
|---|
| Sex, n (%) | | | 0.425 |
|
Male | 59 (62.8%) | 63 (57.3%) | |
|
Female | 35 (37.2%) | 47 (42.7%) | |
| Age, years; n
(range) | 64 (57-67) | 66 (57-72) | 0.671 |
| Symptom, n (%) | | | |
|
Asymptomatic
jaundice | 63 (67.0%) | 70 (63.6%) | 0.613 |
|
Abdominal
pain | 27 (28.7%) | 30 (27.3%) | 0.818 |
|
Atypical
gastrointestinal symptoms | 1 (1.1%) | 2 (1.8%) | 0.656 |
|
Routine
checkups | 3 (3.2%) | 8 (7.3%) | 0.198 |
| Smoking status, n
(%) | | | 0.822 |
|
Yes | 37 (39.4%) | 45 (40.9%) | |
|
No | 57 (60.6%) | 65 (59.1%) | |
| Diabetes, n (%) | | | 0.570 |
|
Yes | 24 (25.5%) | 32 (29.1%) | |
|
No | 70 (74.5%) | 78 (70.9%) | |
| Biliary drainage, n
(%) | | | 0.095 |
|
Yes | 35 (37.2%) | 29 (26.4%) | |
|
No | 59 (62.8%) | 81 (73.6%) | |
| Carbohydrate antigen
19-9 (U/ml), n (%) | | | 0.148 |
|
≤37 | 19 (20.2%) | 14 (12.7%) | |
|
>37 | 75 (79.8%) | 96 (87.3%) | |
The operative parameters and post-operative
complications of the two groups are presented in Table II. All patients completed the
surgery successfully and no peri-operative mortality occurred.
Blood loss and blood transfusion in the arterial approach group
were less than those in the conventional approach group. The
differences in the duration of the surgery between the two groups
was not statistically significant. A total of 82 cases (40.2%) had
post-operative complications. Diarrhea occurred in 31 cases (33.0%)
in the arterial approach group and in 18 cases (16.4%) in the
conventional approach group (P<0.05). The incidence of the total
rate of post-operative complications, pancreatic fistula, gastric
emptying disorder, abdominal infection, abdominal hemorrhage,
biliary fistula, pulmonary infection, gastrointestinal bleeding and
liver abscess in the two groups was similar.
 | Table IIComparison of operative details and
complications between the two groups. |
Table II
Comparison of operative details and
complications between the two groups.
| Parameters | Arterial approach
group (n=94) | Conventional approach
group (n=110) | P-value |
|---|
| Blood loss, ml;
amount (range) | 500 (400,600) | 600 (400,800) | 0.001 |
| Blood
transfusion | | | 0.001 |
|
Yes | 14 (14.9%) | 54 (49.1%) | |
|
No | 80 (85.1%) | 56 (50.9%) | |
| Duration of surgery
(h) | 9.4±2.0 | 9.0±1.7 | 0.173 |
| Post-operative
complications, n (%) | 38 (40.4%) | 44 (40.0%) | 0.951 |
|
Pancreatic
fistula, n (%) | 13 (27.1%) | 18 (16.4%) | 0.615 |
|
Biochemical
leakage, n (%) | 6 (6.4%) | 8 (7.3%) | 0.802 |
|
Grade B
pancreatic fistula, n (%) | 3 (3.2%) | 5 (4.5%) | 0.620 |
|
Grade C
pancreatic fistula, n (%) | 4 (4.3%) | 5 (4.5%) | 0.920 |
|
Gastric
emptying disorder, n (%) | 14 (14.9%) | 27 (24.5%) | 0.086 |
|
Abdominal
infection, n (%) | 4 (4.3%) | 7 (6.4%) | 0.506 |
|
Abdominal
hemorrhage, n (%) | 2 (2.1%) | 9 (8.2%) | 0.056 |
|
Biliary
fistula, n (%) | 1 (1.1%) | 5 (4.5%) | 0.142 |
|
Pulmonary
infection, n (%) | 1 (1.1%) | 1 (0.9%) | 0.911 |
|
Gastrointestinal
bleeding, n (%) | 0 | 2 (1.8%) | 0.189 |
|
Liver
abscess, n (%) | 0 | 1 (0.9%) | 0.354 |
|
Diarrhea, n
(%) | 31 (33.0%) | 18 (16.4%) | 0.006 |
The histological and post-operative parameters are
summarized in Table III. A
higher rate of R0 resection and a higher number of lymph nodes
harvested were achieved in the arterial approach group (P<0.05).
The comparison of the tumor diameter, tumor differentiation, tumor
stage, lymph node metastasis, adjuvant chemotherapy and
post-operative hospitalization duration did not yield significant
differences. In addition, regional recurrence in the arterial
approach group was significantly less than that in the conventional
approach group. The comparison of hepatic, peritoneal, pulmonary
and skeletal metastases did not reveal any significant
differences.
 | Table IIIComparison of the histological and
post-operative parameters between the two groups. |
Table III
Comparison of the histological and
post-operative parameters between the two groups.
| Parameters | Arterial approach
group (n=94) | Conventional
approach group (n=110) | P-value |
|---|
| Tumor diameter
(cm) | 3.0±1.2 | 3.1±1.1 | 0.517 |
| Tumor
differentiation, n (%) | | | 0.860 |
|
Low | 31 (33.0%) | 35 (31.8%) | |
|
Medium-high | 63 (67.0%) | 75 (68.2%) | |
| Tumor stage, n
(%) | | | |
|
I | 47 (50.0%) | 42 (38.2%) | 0.090 |
|
II | 23 (24.5%) | 37 (33.6%) | 0.152 |
|
III | 24 (25.5%) | 31(28.2%) | 0.671 |
| Lymph node
metastasis, n (%) | | | 0.160 |
|
Yes | 57 (60.6%) | 77 (70.0%) | |
|
No | 37 (39.4%) | 33 (30.0%) | |
| R0 resection, n
(%) | | | 0.003 |
|
Yes | 91 (96.8%) | 93 (84.5%) | |
|
No | 3 (3.2%) | 17 (15.5%) | |
| Lymph nodes
harvested, n (range) | 19 (11-24) | 13 (8-20) | 0.024 |
| Adjuvant
chemotherapy, n (%) | | | 0.711 |
|
Yes | 42 (44.7%) | 52 (47.3%) | |
|
No | 52 (55.3%) | 58 (52.7%) | |
| Post-operative
duration of hospitalization (days), n (range) | 17 (15,22) | 17 (16,24) | 0.285 |
| Type of recurrence,
n (%) | 64 (68.1%) | 93 (84.5%) | 0.005 |
| Regional
recurrence, n (%) | 9 (9.6%) | 28 (25.5%) | 0.003 |
| Hepatic metastasis,
n (%) | 33 (35.1%) | 35 (31.8%) | 0.620 |
| Peritoneal
metastasis, n (%) | 17 (18.1%) | 23 (20.9%) | 0.613 |
| Pulmonary
metastasis, n (%) | 3 (3.2%) | 4 (3.6%) | 0.862 |
| Skeletal
metastases, n (%) | 2 (2.1%) | 3 (2.7%) | 0.783 |
Univariate analysis and multivariate analysis of
long-term survival for patients with pancreatic head cancer are
summarized in Table IV. In the
univariate analysis, sex, age, blood loss, blood transfusion and
adjuvant chemotherapy had no significant effect on the prognosis of
patients. Carbohydrate antigen 19-9, tumor differentiation, the
nature of resection, tumor stage and the artery-first approach were
included in the multivariate analysis. The results revealed that
tumor differentiation, tumor stage and the artery-first approach
could influence the prognosis of patients.
 | Table IVUnivariate analysis and multivariate
analysis of the long-term survival of patients with pancreatic head
cancer. |
Table IV
Univariate analysis and multivariate
analysis of the long-term survival of patients with pancreatic head
cancer.
| | Univariate
analysis | Multivariate Cox
regression analysis |
|---|
| Factor | Median survival
time (months) | χ2
value | P-value | RR value | 95% CI | P-value |
|---|
| Sex | 20 | 2.418 | 0.120 | | | |
|
Male | 17 | | | | | |
|
Female | 31 | | | | | |
| Age (years) | 20 | 0.029 | 0.864 | | | |
|
≤60 | 20 | | | | | |
|
>60 | 20 | | | | | |
| Carbohydrate
antigen 19-9 (U/ml) | 22 | 4.627 | 0.031 | 1.198 | 0.729-1.969 | 0.476 |
|
≤37 | 41 | | | | | |
|
>37 | 21 | | | | | |
| Blood loss (range,
ml) | 20 | 1.821 | 0.110 | | | |
|
≤500 | 23 | | | | | |
|
>500 | 19 | | | | | |
| Blood
transfusion | 21 | 0.202 | 0.821 | | | |
|
Yes | 29 | | | | | |
|
No | 14 | | | | | |
| Tumor
differentiation | 20 | 1.778 | 0.037 | 0.645 | 0.455-0.916 | 0.014 |
|
Low | 18 | | | | | |
|
Medium-high | 27 | | | | | |
| Nature of
resection | 20 | 11.952 | 0.001 | 1.069 | 0.548-2.085 | 0.845 |
|
R0 | 28 | | | | | |
|
R1 | 8 | | | | | |
| Adjuvant
chemotherapy | 20 | 0.120 | 0.729 | | | |
|
Yes | 20 | | | | | |
|
No | 19 | | | | | |
| Tumor stage | 22 | 51.018 | 0.000 | 0.431 | 0.281-0.662 | 0.001 |
|
I | 30 | | | | | |
|
II | 23 | | | | | |
|
III | 15 | | | | | |
| Artery-first
approach | 24 | 10.824 | 0.017 | 1.694 | 1.2-2.391 | 0.003 |
|
Yes | 34 | | | | | |
|
No | 19 | | | | | |
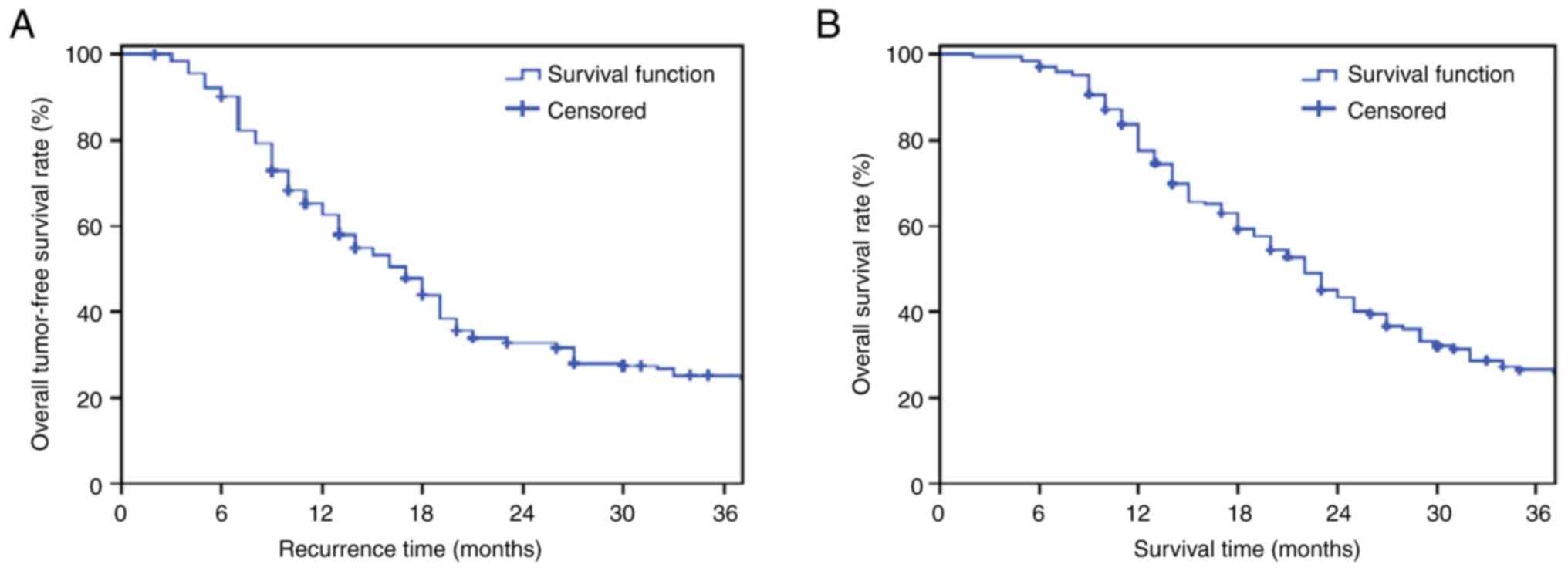
As of March 2021, the overall median survival rate
was 24 months, and the median tumor-free survival rate was 17
months. The 1-, 2- and 3-year overall tumor-free survival rates
were 62.8, 35.2 and 27.9% (Fig.
1A); and the 1-, 2- and 3-year overall survival rates were
77.6, 46.3 and 29.2% (Fig. 1B).
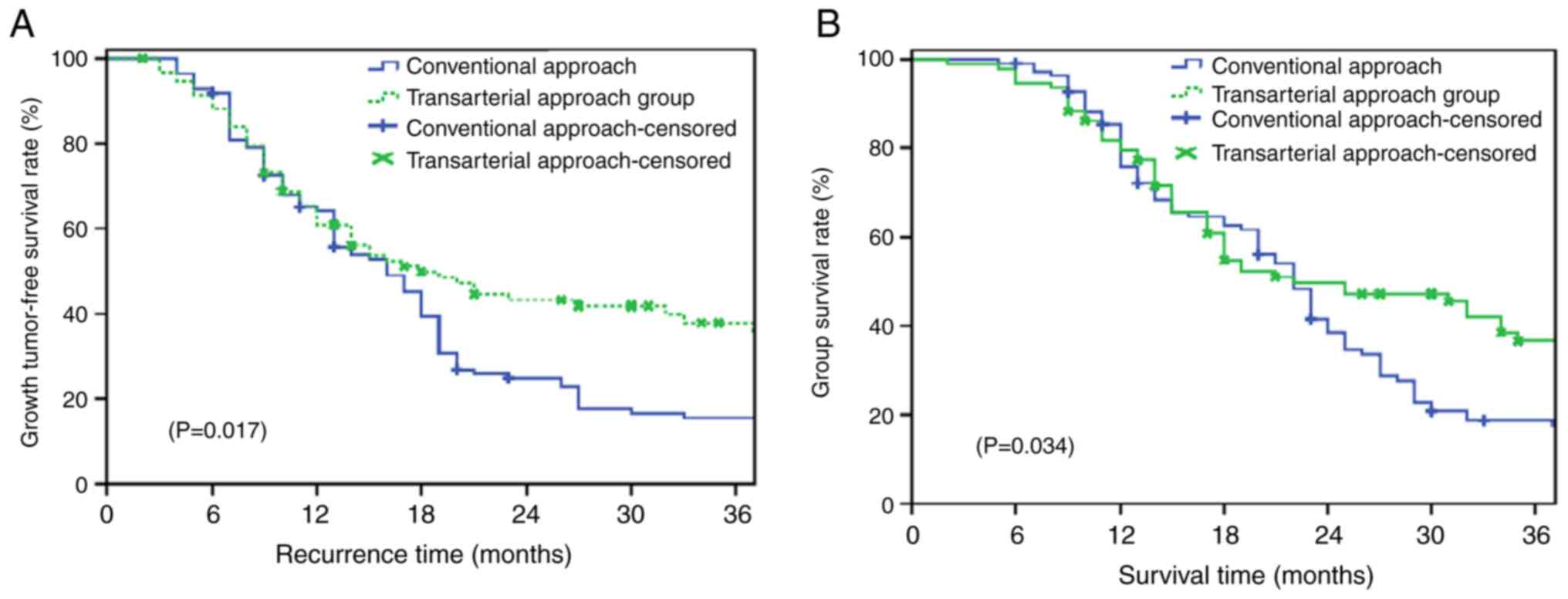
The median survival of the two groups was 26 and 23 months, and the
median tumor-free survival of the two groups was 18 and 16 months,
respectively. The 1-, 2- and 3-year tumor-free survival rates of
the patients in the arterial approach group were 60.9, 43.2 and
37.9%, respectively, and those of the patients in the conventional
approach group were 64.2, 24.9 and 15.6%, respectively (P=0.017;
Fig. 2A). Moreover, the 1-, 2- and
3-year overall survival rates of the patients in the arterial
approach group were 79.5, 49.7 and 36.7%, respectively, and those
of the patients in the conventional approach group were and 75.9,
38.6 and 18.7%, respectively (P=0.034; Fig. 2B).
Discussion
In the present study, it was found that patients
from the artery-first approach group had less bleeding and blood
transfusion, but a prolonged duration of surgery. However, the
number of lymph nodes dissected and the R0 resection rate were
higher, which could lead to the lower incidence of regional
recurrence, but to a higher incidence of post-operative diarrhea.
Furthermore, the present study demonstrated that tumor
differentiation, tumor stage and the artery-first approach could
independently affect the prognosis of patients. The lower the
differentiation, the higher the staging, the worse the prognosis.
Finally, the prolonged tumor-free time and overall survival time of
the patients in the artery-first approach group was observed.
According to the statistics of the American Cancer
Society in 2020, the 5-year survival rate of patients with
pancreatic head cancer was only 9% (15-17).
The only curative treatment for resectable pancreatic head cancer
is surgical resection, namely pancreatoduodenectomy. However, An R0
resection is usually difficult to achieve, and local recurrence is
related to a positive SMA margin. Kalisvaart et al (18) retrospectively reviewed 23/617
evaluated studies (n=3,815); local recurrence was observed in 7-69%
of the studies and the SMA margin (six studies) was positive in
15-35% of the studies. Moreover, local recurrence was more
frequently observed with a positive SMA margin (66 vs. 45%;
P=0.005). In addition, the abnormal origin and direction of the
artery can easily increase the risk of intraoperative injury,
massive hemorrhage and post-operative hepatic, intestinal and
biliary ischemia. The postoperative survival rate is not ideal
(19-21).
The aim of the artery-first approach is to explore the superior
mesenteric artery in the inferior infracolic to determine the
resectability of the tumor, cut off the blood supply of the tumor,
and then resect the specimen for routine anastomosis. It gives
priority to the evaluation of vascular invasion, and directly
determines whether radical resection can be implemented, which is
of utmost importance for the prognosis of patients (22,23).
In the present study, the inferior superior
mesenteric artery-first approach was performed, as previously
described (24). In the study by
Vallance et al (25), 80
patients underwent the posterior superior mesenteric artery-first
approach and the half-year survival rate was significantly higher
in these patients than those in the conventional approach group (95
vs. 80%), which was similar to the results of the present tsudy.
Furthermore, according to the study by Du et al (26), the R0 resection rate was improved
by the artery-first approach (85.71 vs. 62.50%), and the
post-operative tumor recurrence rate was significantly lower in
this group than that in the conventional approach group (7.14 vs.
28.13%); these findings were also in accordance with those of the
present study.
The mesenteric approach was first developed for
pancreatoduodenectomy by Professor Akimasa Nakao (27). This approach allowed for the
dissection from the non-cancerous side and the determination of
both cancer-free margins and resectability followed by systematic
lymphadenectomy around the superior mesenteric artery. It also
enables the early ligation of the inferior pancreatoduodenal artery
and dorsal pancreatic artery branches from the superior mesenteric
artery, as well as the complete excision of the total mesopancreas,
which is considered to be the second portion of the pancreatic head
nerve plexus (27). Similar to the
present study, the artery-first approach was to explore along the
artery and in turn, dissect the perivascular tissue and lymph node
dissection during the exploration. Moreover, it was found that the
artery-first approach could make lymph node dissection more
thorough and comprehensive, expand the scope of lymph node
dissection, allow for an easier R0 resection, avoid residual lesion
tissue, reduce the risk of post-operative recurrence, improve the
tumor-free survival rate and improve the prognosis of patients. At
the same time, it reduced the times of moving tissues and organs,
which could reduce the tumor cell diffusion caused by moving.
Furthermore, the present study also demonstrated
that the patients who underwent the superior mesenteric
artery-first approach in the inferior infracolic region had less
intraoperative bleeding and blood transfusion. These results may be
due to the fact that the blood supply of the resected tissue was
ligated and cut first, which facilitated the subsequent organ
resection, reduced the bleeding caused by separating the venule
between uncinate process of pancreas and portal vein, and reduced
the blood transfusion. Moreover, the artery-first approach could
not only facilitate the judgement of its anatomical structure, but
also increased the accuracy of the operation for surgeons. However,
there were also some shortcomings in artery-first approach, such as
the prolonged duration of surgery and post-operative diarrhea; in
terms of the shortcomings, the general condition of the patients
during the surgery could be monitored, cooperating with
anesthesiologists to timely apply drugs, thus reducing the impact
of the long duration of the surgery on patients.
The main limitation of the present study was that it
presented the experience of a single center. The number of patients
in each subgroup was relatively small, which may limit the accuracy
of the assessment. Further studies, preferably random clinical
trials from multi-centers, are thus required to further confirm the
preliminary outcomes observed herein.
In conclusion, the present study demonstrated that
the inferior superior mesenteric artery approach improved the R0
resection rate, prolonged the post-operative survival time, reduced
recurrence and improved the prognosis of patients. It also reduced
intraoperative blood loss and blood transfusion, although it
increased the incidence of post-operative diarrhea. Further studies
are warranted in the future to validate these findings.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
JQZ conceived the study. SCL and FFW performed the
research and wrote the first draft of the manuscript. All authors
(FFW, SCL, ZYR, XZ, JQZ and QH) contributed to the design of the
study and to the interpretation of the results, and to further
drafts. JQZ and QH confirm the authenticity of all the raw data.
All authors have read and approved the final manuscript.
Ethics approval and consent to
participate
The study complied with the Declaration of Helsinki
and was approved by the Ethics Committee of Beijing Chaoyang
Hospital (No. 2020-D-302). The participants provided written
informed consent to participate in this study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Vincent A, Herman J, Schulick R, Hruban RH
and Goggins M: Pancreatic cancer. Lancet. 378:607–620.
2011.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Ansari D, Tingstedt B, Andersson B,
Holmquist F, Sturesson C, Williamsson C, Sasor A, Borg D, Bauden M
and Andersson R: Pancreatic cancer: Yesterday, today and tomorrow.
Future Oncol. 12:1929–1946. 2016.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Mouradides C, Taha A, Borbath I, Deprez PH
and Moreels TG: How to treat intestinal obstruction due to
malignant recurrence after Whipple's resection for pancreatic head
cancer: Description of 2 new endoscopic techniques. World J
Gastroenterol. 23:6181–6186. 2017.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Huang JL, Li WG, Chen FZ, Su ZJ, Li FM and
Liu B: The clinical impact of artery-first approach combined with
vascular resection and reconstruction in the treatment of
pancreatic head carcinoma. Zhonghua Zhong Liu Za Zhi. 39:225–230.
2017.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
5
|
Tempero MA: NCCN guidelines updates:
Pancreatic cancer. J Natl Compr Canc Netw. 17:603–605.
2019.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Jang JY, Kang JS, Han Y, Heo JS, Choi SH,
Choi DW, Park SJ, Han SS, Yoon DS, Park JS, et al: Long-term
outcomes and recurrence patterns of standard versus extended
pancreatectomy for pancreatic head cancer: A multicenter
prospective randomized controlled study. J Hepatobiliary Pancreat
Sci. 24:426–433. 2017.PubMed/NCBI View
Article : Google Scholar
|
|
7
|
Zhang JJ, Li QZ, Wang JH, Chen X, Ren S,
Ye DD, Zhang HF and Wang ZQ: Contrast-enhanced CT and texture
analysis of mass-forming pancreatitis and cancer in the pancreatic
head. Zhonghua Yi Xue Za Zhi. 99:2575–2580. 2019.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
8
|
Lin QJ, Yang F, Jin C and Fu DL: Current
status and progress of pancreatic cancer in China. World J
Gastroenterol. 21:7988–8003. 2015.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Kawai M, Hirano S and Yamaue H:
Artery-first approach for pancreaticoduodenectomy. J Hepatobiliary
Pancreat Sci. 25:319–320. 2018.PubMed/NCBI View
Article : Google Scholar
|
|
10
|
Nakao A and Takagi H: Isolated
pancreatectomy for pancreatic head carcinoma using catheter bypass
of the portal vein. Hepatogastroenterology. 40:426–429.
1993.PubMed/NCBI
|
|
11
|
Leach SD, Davidson BS, Ames FC and Evans
FC: Alternative method for exposure of the retropancreatic
mesenteric vasculature during total pancreatectomy. J Surg Oncol.
61:163–165. 1996.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Machado MC, Penteado S, Cunha JE, Jukemura
J, Herman P, Bacchella T, Machado MA and Montagnini AL: Pancreatic
head tumors with portal vein involvement: An alternative surgical
approach. Hepatogastroenterology. 48:1486–1487. 2001.PubMed/NCBI
|
|
13
|
Pessaux P, Varma D and Arnaud JP:
Pancreaticoduodenectomy: Superior mesenteric artery first approach.
J Gastrointest Surg. 10:607–611. 2006.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Zhu J, Han D, Li X, Pan F, Ma J, Kou J,
Fan H, Lang R and He Q: Inferior infracolic ‘superior mesenteric
artery first’ approach with a no-touch isolation surgical technique
in patients with a borderline resectable cancer of the pancreatic
head. Ann Surg Oncol. 23 (Suppl 5):S976–S980. 2016.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Siegel RL, Miller KD and Jemal A: Cancer
statistics, 2018. CA Cancer J Clin. 68:7–30. 2018.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Chu LC, Goggins MG and Fishman EK:
Diagnosis and detection of pancreatic cancer. Cancer J. 23:333–342.
2017.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Saluja A and Maitra A: Pancreatitis and
pancreatic cancer. Gastroenterology. 156:1937–1940. 2019.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Kalisvaart M, Broadhurst D, Marcon F,
Pande R, Schlegel A, Sutcliffe R, Marudanayagam R, Mirza D,
Chatzizacharias N, Abradelo M, et al: Recurrence patterns of
pancreatic cancer after pancreatoduodenectomy: Systematic review
and a single-centre retrospective study. HPB (Oxford).
22:1240–1249. 2020.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Gedge K: Pancreatic cancer: A symptomless
killer. J Perioper Pract. 27:158–161. 2017.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Masiak-Segit W, Rawicz-Pruszyński K,
Skórzewska M and Polkowski WP: Surgical treatment of pancreatic
cancer. Pol Przegl Chir. 90:45–53. 2018.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Younan G, Tsai S, Evans DB and Christians
KK: Techniques of vascular resection and reconstruction in
pancreatic cancer. Surg Clin North Am. 96:1351–1370.
2016.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Hamner JB, White M, Crowder C and Singh G:
Resection of metachronous pancreatic cancer 4 years after
pancreaticoduodenectomy for stage III pancreatic adenocarcinoma.
World J Surg Oncol. 13(290)2015.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Wolpin BM: Pancreatic cancer. Hematol
Oncol Clin North Am. 29:13–14. 2015.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Jiang X, Yu Z, Ma Z, Deng H, Ren W, Shi W
and Jiao Z: Superior mesenteric artery first approach can improve
the clinical outcomes of pancreaticoduodenectomy: A meta-analysis.
Int J Surg. 73:14–24. 2020.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Vallance AE, Young AL, Pandanaboyana S,
Lodge JP and Smith AM: Posterior superior mesenteric artery first
dissection versus classical approach in pancreaticoduodenectomy:
Outcomes of a case-matched study. Pancreas. 46:276–281.
2017.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Du F, Wang X, Lin H and Zhao X:
Pancreaticoduodenectomy with arterial approach of total mesenteric
resection of the pancreas for pancreatic head cancer.
Gastroenterology Res. 12:256–262. 2019.PubMed/NCBI View
Article : Google Scholar
|
|
27
|
Nakao A: Isolated pancreatectomy using
mesenteric approach. J Hepatobiliary Pancreat Sci. 29:293–300.
2022.PubMed/NCBI View Article : Google Scholar
|