Introduction
Delirium is an acute confusional state, also defined
as acute brain failure or dysfunction. The pathophysiological
mechanism behind delirium is not yet well understood. It is
frequently observed in elderly individuals and in hospital settings
(1,2).
Delirium is provoked by the transient disruption of
regular neuronal activity and is associated with a slower recovery,
increased mortality and morbidity, and a decreased quality of life
(3).
According to the criteria of Diagnostic and
Statistical Manual of Mental Disorders, fifth edition (DSM-5)
(4), the diagnosis of delirium
requires a disturbance in attention, which develops acutely, is not
explained by pre-existing dementia, and does not occur in the
context of a reduced level of arousal, with one additional
disturbance in cognition and evidence of an underlying organic
disorder. Patients may experience hallucinations and manifest
abnormal psychomotor behavior and a sleep-wake cycle (4).
Delirium can be described as hyperactive, hypoactive
or a combination of both. Hyperactive delirium includes
restlessness (for example, pacing), agitation, rapid mood changes
or hallucinations and is more easily recognizable, while
hypoactive, which includes a reduced motor activity, sluggishness
and abnormal drowsiness, can pass unrecognized, despite being the
most frequent among elderly patients, who usually manifest it with
lethargy and a general slowness (5).
Delirium occurs in 85% of cases in palliative care
settings, in up to 25% of patients post-surgery and in 50% of
patients following major surgery (6). Beyond an older age and long-term
hospitalization, other risk factors associated with the development
of delirium are the male sex, underlying undiagnosed dementia,
alcohol abuse, impairment in vision and/or hearing and depression
(6,7).
Previous studies have suggested cerebral
desaturation as a risk factor for the development of delirium
(8-10),
and it has been observed that the frequency of delirium is
increased in intensive care units (ICUs) (11).
The appearance of severe acute respiratory syndrome
coronavirus 2 (SARS-CoV-2) abruptly led to a pandemic, particularly
due to its transmission mode (12)
and the onset of numerous variants (13,14).
This rapidly led to an increase in the number of hospitalizations.
The respiratory syndrome consequent to coronavirus disease 2019
(COVID-19) (15), similar to the
one caused by the first SARS-CoV, led to a sudden need in oxygen
therapy, ventilation and admission to ICUs.
A number of complications, such as electrolytic
impairment or macular rash, have been linked to SARS-CoV-2
infection (16-22).
Neurological and psychiatric complications due to COVID-19 have
also been described, such as obsessive-compulsive disorder or motor
dysfunction (23,24). Researchers have already proven an
increase in the number of episodes of delirium during the COVID-19
pandemic, mostly related to ICU admissions, long-term
hospitalization and hypoxemia (25). Other aspects that have been found
to be associated with an increased risk of developing delirium are
the use of benzodiazepines, opioids, vasopressors, fever, smoking,
a history of cardiovascular diseases, dialysis and thromboembolic
illnesses (26). In some cases,
the very same strategies and treatments for COVID-19, such as the
use of the prone position can contribute to the development of
delirium (27). Another important
issue that has come to light with the COVID-19 pandemic is the
isolation of positive patients, who have been unable to visit or
come into contact with their families during the hospitalization
period. All these factors have contributed to the development of
delirium, particularly considering the more frail members of the
population, such as the elderly (28-40).
Even though it is certainly more frequent among
elderly patients, delirium concomitant to SARS-CoV-2 has been also
observed in younger age groups (41) and even in pediatric cases (42-44).
Moreover, it has been observed in some specific categories of
patients who are considered to be more frail, such as pregnant
women and immunocompromised individuals; thus, this should be
considered in the concept of delirium (45-47).
In some cases, it has been indicated that delirium may be the
primary and sometimes, the only presenting symptom of COVID-19
(48-51).
Since the first cases of COVID-19, different
manifestations of neuropathology secondary to the infection, such
as anosmia and ageusia have been observed. There are a number of
hypotheses regarding the pathophysiology of delirium in COVID-19,
including the ability of SARS-CoV-2 to directly invade the central
nervous system via the olfactory bulb, and it has been suggested
that it may preferentially target the frontal lobes (52), or indirectly via the oxidative
stress caused by the release of pro-inflammatory cytokines
(53,54) microvascular damage (55), metabolic and/or endocrine
dysfunctions and organ insufficiency (56,57).
In the study by Cuperlovic-Cul et al
(58), a difference was noted in
polyamines in patients with delirium and an association between the
SARS-CoV-2 spike protein and monoamine oxidase was postulated.
Therefore, it can be hypothesized that the development of delirium
is a result of both environmental and organic factors (59).
The study by Batra et al (60) demonstrated that persistent viral
shedding in patients was associated with in-hospital delirium
episodes and a higher mortality rate. Notably, in the study by Dias
et al (61), delirium was
not found to have a higher prevalence in the COVID-19 group
compared with the non-COVID-19, while it appeared to manifest in a
more severe form in the COVID-19 group.
Delirium has been shown to be associated with a
higher mortality rate in patients hospitalized for SARS-CoV-2
infection (62-66),
prolongation in hospital stay (67), an impairment in physical functions
(68) and cognitive impairment
even after physical recovery from infection (69).
Despite being so widely diffused, delirium remains a
challenging diagnosis and it is of utmost importance to develop
tools to help physicians recognize this condition. A consistent
barrier in recognizing delirium is the underlying dementia,
particularly considering that the patients with a major risk of
developing delirium are the elderly, who may already have cognitive
impairment. This poses the difficulty of a juxtaposition of both
neurocognitive impairment and it usually leads to a misdiagnosis or
the non-recognition of delirium. Two valid instruments for the
diagnosis of delirium are the Confusion Assessment Method-ICU
(CAM-ICU) and the Intensive Care Delirium Screening Checklist
(ICDSC), both developed for delirium screening in non-verbal
patients in ICUs (70). Another
tool with a high sensitivity and moderate specificity is the 4AT
score (71).
A critical aspect of the neuropsychiatric
consequences due to COVID-19 is the issue of the ‘forgotten ones’,
namely all the individuals dismissed from hospital following
recovery from COVID-19. It is known that SARS-COV-2 infection may
lead to long-term alterations, which have been commonly defined as
‘long covid’ (72). Even though it
often manifests with mild symptoms, in some cases, severe
complications may occur post-COVID-19, as in the case described in
the study by Hara et al (73); in that study, a patient developed
post-COVID-19 encephalitis presenting with delirium as a first
manifestation. Unrelated to the hospitalization, yet still an
important consequence of the COVID-19 pandemic, is the effect of
the lockdowns on elderly individuals, who are more susceptible to
developing delirium in response to the amount of stress and
anxiety, brought on by the feelings of isolation (74).
The aim of the present study was to evaluate the
psychiatric risks related to hospitalization and to acute viral
infections, such as COVID-19. It is of utmost importance to take
into account the possibilities of developing delirium, particularly
in elderly patients. An acute episode could not only lead to
adverse consequences for health workers and the patients
themselves, as in the case of the hyperactive form, but can also
compromise the prognosis and the rehabilitation of hospitalized
individuals.
Case report
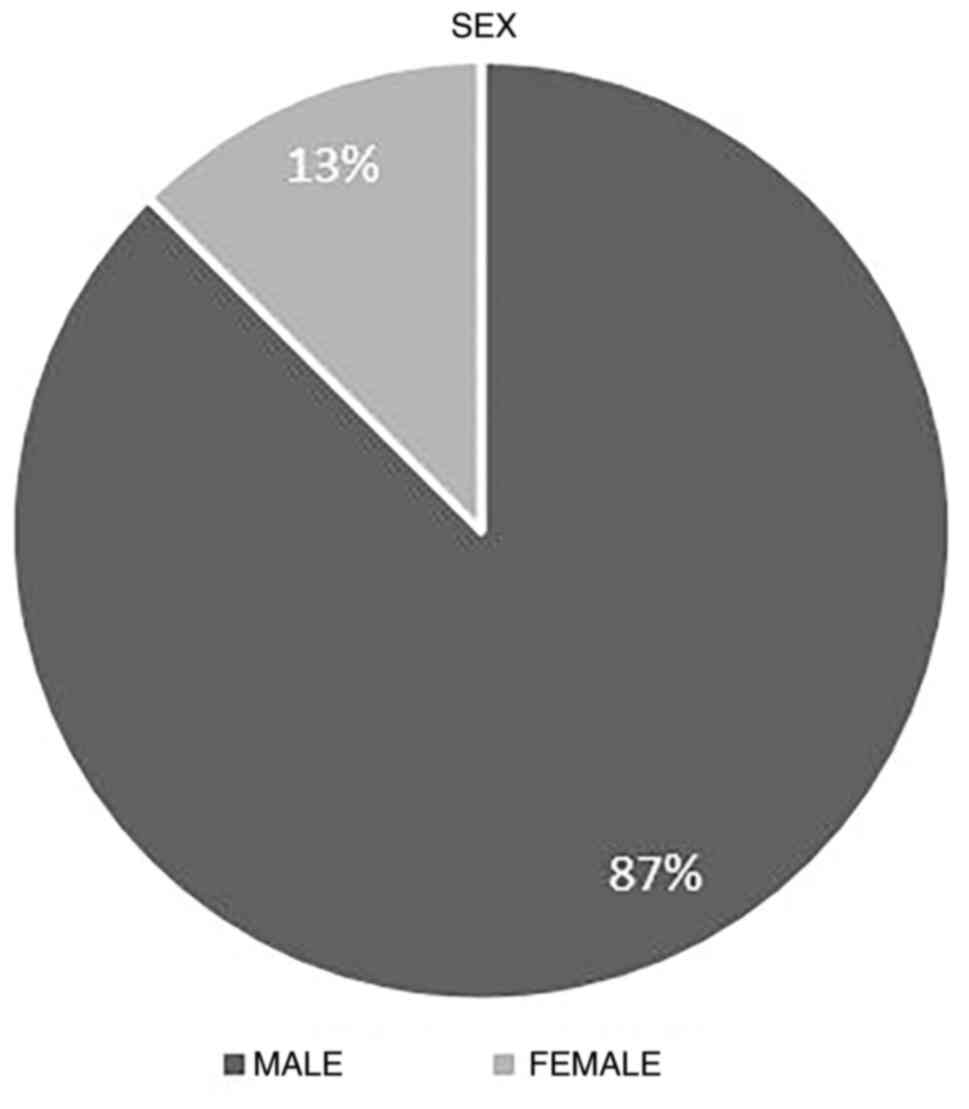
Between March, 2020 and May, 2022, in the Infectious
Diseases Unit of the ‘Gaetano Martino’ University Hospital in
Messina, 8 patients hospitalized for SARS-CoV-2 infection presented
delirium. The male sex was the most prevalent one, with a 7:1 ratio
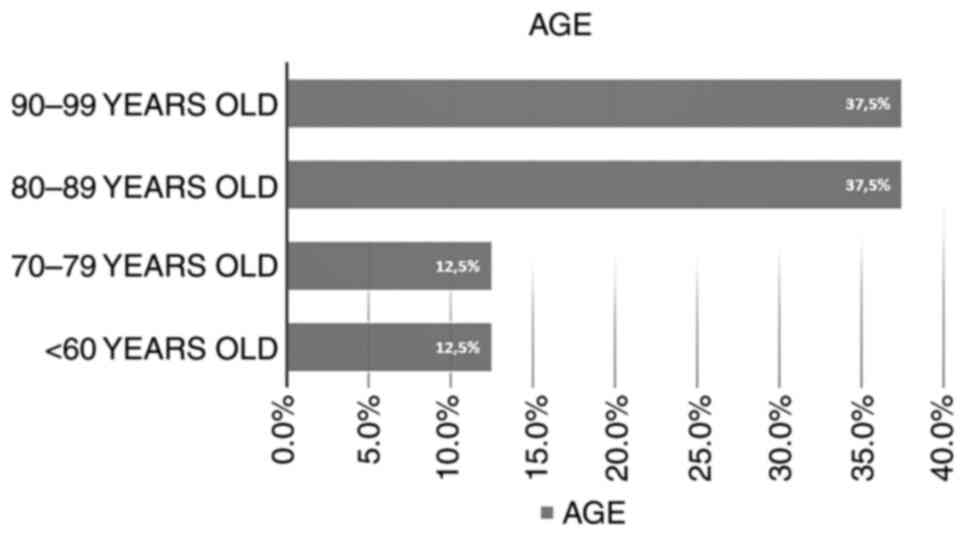
(Fig. 1). The mean age of the
patients was 81.7±4 years (Fig.
2). The characteristics of the 8 patients are presented in
Table I. In total, 5 patients
(cases 2, 3, 4, 5 and 8) presented the feature of mild age-related
dementia.
 | Table ICharacteristics of the 8 patients in
the present study. |
Table I
Characteristics of the 8 patients in
the present study.
| Case no. | Age, years | Sex | Comorbidities | SARS-CoV-2
vaccination | Hospitalization
days | Need for
O2 DH | COVID-19
therapy | Days between
admission and delirium | Outcome |
|---|
| 1 | 80 | M | | No | 25 | Yes |
Casirivimab/imdevimab | 2 | CR |
| 2 | 90 | M | DM, CV diseases;
COPD | No | 30 | Yes | | 14 | VR |
| 3 | 90 | M | | No | 12 | No | | 36 | CR |
| 4 | 86 | M | DM, CV diseases;
COPD | Yes | 15 | Yes | | 1 | Deceased |
| 5 | 87 | M | DM, CV disease,
psychosis | Yes | 56 | Yes | | 38 | Deceased |
| 6 | 58 | M | PD | No | 16 | No | Azithromycin,
hydroxychloroquine | 8 | VR |
| 7 | 70 | F | Cancer | No | 22 | Yes | | 2 | VR |
| 8 | 93 | M | | No | 13 | Yes | | 9 | CR |
A total of 2 patients had at least two shots of the
SARS-CoV-2 vaccine, while 6 patients were not vaccinated. In
addition, 2 patients had a history of type II diabetes,
cardiovascular diseases and chronic obstructive pulmonary disease,
1 patient had type II diabetes and cardiovascular disease, 1
patient had a history of cancer, and 1 patient had Parkinson's
disease. Only 1 patient had a psychiatric comorbidity prior to
hospitalization, as he was diagnosed with an unspecified psychosis
and received chronic therapy with lorazepam, promazine and
tiapride.
In total, 6 patients out of the 8 patients required
oxygen implementation, 2 patients did not need it and were
maintained in room air, and no patient required mechanical
ventilation. The mean duration of hospitalization was 23.6±6 days,
with the longest time being 56 days and the shortest time being 12
days (Table I).
As regards COVID-19 therapy, low molecular weight
heparin (LMWH) was administered to all patients. In addition, 1
patient was treated with azithromycin and hydroxychloroquine for
thromboembolic prophylaxis, and 1 patient received monoclonal
antibody therapy with casirivimab/imdevimab (Table I).
In total, 6 patients (cases 1, 2, 4, 5, 7 and 8)
received corticosteroids for respiratory impairment, 4 patients (1,
2, 4 and 7) received dexamethasone and 2 (5 and 8) patients
received methylprednisolone. These patients were also treated with
omeprazole for the duration of the corticosteroid therapy. Insulin
therapy was administered to 3 patients who were diabetic.
Moreover, 5 patients (cases 1, 2, 3, 7 and 8) were
treated with antibiotics for infections which occurred during
hospitalization; the antibiotics used were meropenem, cefepime,
amoxicillin/clavulanate and trimethoprim/sulfamethoxazole. The
chronic therapies administered are listed in Table II.
 | Table IIChronic therapies used in the
patients. |
Table II
Chronic therapies used in the
patients.
| Medication | Patients (case
nos.) |
|---|
| Cardioaspirin | 6 (2, 3, 4, 6, 7
and 8) |
| Atorvastatin | 5 (2, 4, 5, 6 and
8) |
| Bisoprolol | 4 (1, 4, 5 and
8) |
| Nebivolol | 4 (1, 2, 4 and
7) |
| Furosemide | 4 (1, 4, 5 and
6) |
| Fondaparinux | 2 (2 and 4) |
| Canrenone | 2 (6 and 7) |
|
Lorazepam/delorazepam/clonazepam | 2 (5 and 8) |
| Finasteride | 1(7) |
| Nifedipine | 1(7) |
| Allopurinol | 1(1) |
| Pramipexole | 1(5) |
| Safinamide | 1(5) |
| Vortioxetine | 1(5) |
| Pregabalin | 1(1) |
| Promazine | 1(8) |
| Tiapride | 1(7) |
During hospitalization blood analyses were performed
routinely. In total, 2 patients (cases 4 and 5) exhibited
alterations in glycaemia (251 and 337 mg/dl) upon admission and
maintained a slightly altered level of hematic glucose during the
whole period of hospitalization. Furthermore, patient 1 exhibited
an abnormal renal function, with creatinine levels of 2,8 mg/dl and
azotemia levels of 123 mg/dl upon admission, which improved during
hospitalization. In another case (case 8), a worsening of renal
function was observed during hospitalization. An increase in
procalcitonin levels (max 10 ng/ml) was observed in cases 1, 2, 3,
7 and 8, who developed infection during hospitalization. C reactive
protein levels were found to be altered in 6 patients (cases 1, 2,
3, 4, 7 and 8), with a minimum level of 1,50 mg/dl and a maximum
level of 10,5 mg/dl. Of note, in case 6, a decrease in hemoglobin
(8,9 g/dl) levels was observed in the blood analyses performed the
day after the delirium episode. No significant alterations were
found in the levels of other laboratory markers performed during
hospitalization, such as transaminases, cholestasis indices,
coagulation factors and a urine analysis.
In total, 4 patients (cases 2, 3, 6 and 7) were
discharged with a negative nasopharyngeal swab (RT-PCR) for
SARS-CoV-2: the mean time of viral shedding was 26.5±2 days, with
the longest time being 35 days and the shortest time being 18 days.
The mean number of days between the admission and the occurrence of
delirium was 13.7±3, with the longest being 38 days, and the
shortest being 1 day.
A delirium episode began with an abrupt
manifestation of aggressiveness and violence: The patients, who
were previously compliant, suddenly removed vascular accesses,
oxygen masks and exhibited verbal aggressiveness, thus insulting
health workers; 7 patients (cases 1, 2, 3, 4, 5, 7 and 8) used
vulgar language, which had never been used by them before, as also
confirmed by the families of the patients. In 3 cases (1, 3 and 5),
the patients destroyed the room furniture and every other object
they could reach. In all the cases, delirium manifested with a
strong refusal to receive medical examination, or therapies and
food. A total of 3 patients (cases 3, 6 and 7) experienced
hallucinations referring to the presence of other individuals in
the room and objects that were not effectively present, and 2
patients (3 and 7) also referred to hearing voices of other
individuals. In addition, 1 patient (case 8) manifested self-harm
and started beating and scratching himself and patient 5 presented
persecutory delusions and suicidal ideation.
In all cases, delirium presented as hyperactive.
Although, it should be mentioned that 1 patient (case 6) manifested
a general slowness and became unresponsive immediately following a
hyperactive delirium episode.
According to standard clinical practice,
non-pharmacological interventions, such as verbal reassurance and
orientation, were used at first. When it was deemed safe for health
workers to intervene, as a first line pharmacologic treatment and
according to psychiatric consultation, intramuscular tiapride (100
mg) was administered alone in 3 cases (patients 1, 3 and 4) and in
association with haloperidol (1 mg) in case 7, promazine (25 mg)
was administered alone in case 8, in association with valproate
sodium at 300 mg in case 5 and with aripiprazole in another case
(patient 2), and in case 6, aripiprazole alone was administered at
increasing doses.
A complete resolution of delirium with no other
recurrences was obtained in 3 cases (patients 3, 4 and 6). In 5
cases (1, 2, 5, 7 and 8), the patients had a recurrence of
delirium. As second-line therapy, valproate sodium, promazine and
tiapride were administered. In addition, 2 patients out of the 8
patients had a clinical recovery and were discharged to a COVID-19
low intensity cure facility, 4 patients had a virological recovery
and 2 patients did not survive.
Discussion
With a mean age of 81.7±4 years and a huge
prevalence of the male sex, the cases described in the present
study appear to follow the evidence in the literature, which report
a greater risk of developing delirium in males and among the
elderly, a well as among patients hospitalized for COVID-19
(75-79).
Even though individuals with pre-existing
psychiatric disorders appear to have a major risk of developing
delirium (80), among the patients
described herein, 1 patient had a history of psychiatric disorders.
Age-related dementia was present in the majority of patients in the
present study. Thus, it is considered that dementia and other types
of neurocognitive age-related impairment are precipitating factors
for delirium (6).
In the patients described in the present study,
COVID-19 was the dominant cause capable of triggering delirium,
since the other conditions either alone, or in combination, would
probably have not been sufficient to cause this; i.e., in a
population of patients of the same age and comorbidities, the
prevalence of delirium would have been significantly lower.
Moreover, the presence of comorbidities found during
viral infections can facilitate the onset of an acute confusional
state (28,81,82).
In a previous Chinese case study (83), the prevalence of some comorbidities
was hypertension (16.9%), other cardiovascular diseases (53.7%)
cerebrovascular diseases (1.9%), diabetes (8.2%), hepatitis B
infections (1.8%), chronic obstructive pulmonary disease (1.5%),
chronic kidney diseases (1.3%), tumors (11.1%) and immunodeficiency
(0.2%). Those individuals who require ICU-level care, are the ones
who can easily develop delirium.
The majority of the patients in the present study
required oxygen supplementation, in some cases limited to a
low-flow nasal cannula; however, in some cases, oxygenation had to
be implemented at a high flow due to severe desaturation. This may
support the hypothesis that cerebral desaturation may trigger
delirium and that the need for oxygen supplementation is also
related to delirium (8-10,25).
Considering the therapies administered for COVID-19,
all the patients described herein were treated with LMWH for
thromboembolic prophylaxis. In the study by D'Ardes et al
(84), a protective role of LMWH
in the development of delirium was suggested. Notably, in the
present study, it did not play a protective role in preventing
delirium.
Other than drugs, the time of hospitalization has
been one of the main factors associated with the development of
delirium in hospital settings. As aforementioned, long-term
hospitalization is strongly associated with the development of
delirium (6,7); however, in the present study, it is
interesting to observe that the median time passed between
admission and the episode of delirium was 13 days, and in in 3
cases, delirium occurred after 1 or 2 days after admission. This
suggests that, while long-term hospitalization plays a critical
role, pre-existing features may lead to the onset of delirium,
despite the time in hospital.
There does not appear to be a prevalence of
hyperactive vs. hypoactive delirium, although it also appears that
there is a higher frequency of hypoactive delirium in the elderly
population. Nevertheless, both forms were observed in hospital
settings during the COVID-19 pandemic (85,86).
Of note, all the patients described herein manifested a hyperactive
form of delirium, exhibiting verbal and physical aggressiveness
towards the health workers. Verbal and physical aggressiveness
towards health workers can be considered, in psychopathological
terms, a form of hetero-aggressiveness or heterodirect
aggressiveness, which is a feature of hyperactive delirium, that is
characterized itself by an aggressive behavior, according to DSM-5
(87-90).
However, it is possible that some cases of hypoactive delirium have
passed undiagnosed and have been resolved without the use of
medications.
The treatment for delirium is controversial,
particularly considering that some primary medications may be
contraindicated due to the concomitant SARS-CoV-2 infection, with
particular attention to the antivirals, even though no notable
interactions have been reported (91). Specifically, haloperidol,
risperidone and quetiapine may expose the patients to certain
adverse effects of antivirals, due to their increased concentration
(71). Given the high distress of
patients admitted to hospital and in a enforced isolation,
behavioral therapy should be the first-line treatment for the
prevention of delirium. As regards pharmacological therapy, the
Italian Society of Psychiatry suggested a number of therapeutic
options for delirium during COVID-19(92), as presented in Table III.
 | Table IIITreatment recommendations for
delirium during the COVID-19 pandemic, as recommended by the
Italian Society of Psychiatry. |
Table III
Treatment recommendations for
delirium during the COVID-19 pandemic, as recommended by the
Italian Society of Psychiatry.
| Delirium therapy in
COVID-19 |
| Dexmetodimin (for
patients in the ICU): Alpha-2 agonist, sedative
anxiolytic-analgesic that does not cause respiratory
depression |
| Tiapride: Useful if
the patient is agitated (hyperkinetic delirium) and receiving
therapy with lopinavir/ritonavir. |
| Promazine via
intramuscular (if not contraindicated for coagulation
problems) |
| Aripiprazole:
Useful for hypokinetic delirium |
| Haloperidol: Low
risk of respiratory depression |
| Avoid
benzodiazepines unless delirium tremens is suspected |
The treatment options suggested in previous studies
include melatonin, in order to regulate the wake-sleep cycle,
valproic acid or trazodone and dopamine agonist (93). In a letter by Khosravi (94), quetiapine was proposed as a safe
therapy for delirium in the ICU.
The management of psychiatric drugs, their possible
interactions with COVID-19 therapeutics and the concomitant
necessity for psychological treatment are the main issues in
treating delirium, particularly in ICU settings (95-97).
Thus, the assessment and treatment of delirium in hospitalized
patients with COVID-19 requires a multidisciplinary effort and
collaboration (98).
The drugs most frequently used in the cases
described herein were promazine, haloperidol and tiapride. It is
noteworthy to observe that only 3 patients had a complete
resolution of delirium, while the majority experienced a
recurrence, despite therapies. The recurrence of delirium may be
caused by the environmental factors that still pose a huge font of
distress to hospitalized individuals, including isolation, the lack
of communication, the limitations in motility and the treatments
for underlying illnesses and COVID-19 itself. Therefore, the
implementation of the quality of life, as a multidisciplinary
effort, of patients hospitalized for COVID-19 is necessary to
achieve a resolution or, at least, avoid the repercussions of
delirium (98).
In the cases described in the present study, the
mortality rate was 25%, which is a critical indicator of how
delirium can play a role in the mortality of hospitalized patients,
as demonstrated by other studies (62-66).
It is imperative to create protocols and take action
in order to prevent delirium. While some aspects are not
modifiable, such as patient comorbidities or visiting restrictions,
an improvement could be made regarding the wake-sleep cycle of the
patients, considering the use of melatonin in treatment. The food
intake also is a critical variable and a more balanced diet may
play a positive role during the hospital stay of patients. The
psychological aspect is probably the most crucial one; engaging the
patients in conversations or implementing the use of psychologists
and/or the digital system to maintain communications with families
while in COVID-19 wards may improve the quality of life and the
mental status of hospitalized patients (99-101).
In conclusion, in this period when SARS-CoV-2 has
imposed enforced isolation, hospitalization and the need for
oxygen, it is of primary importance to develop tools to diagnose
delirium more effectively, including the less evident forms, and to
take measures to improve the environmental factors that may
contribute to delirium, with particular attention to behavioral
therapy.
Acknowledgements
The authors would like to thank Dr Aldo Sitibondo,
of the Unit of Infectious Diseases, University of Messina, Messina,
Italy, for providing a critical clinical point of view on the
manuscript.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
YR, EVR, CM, GN, VC and CPS conceptualized the
study. YR, CM and VC were involved in the writing of the original
draft and in manuscript preparation. EVR, CM, VC and GN were
involved in the writing, reviewing and editing of the manuscript.
VC was involved in visualization/impagination. GN supervised the
study. YR and GN confirm the authenticity of all the raw data. All
authors have read and approved the final version of the
manuscript.
Ethics approval and consent to
participate
Written informed consent has been obtained from the
patients described in the present case report. In the 2 cases which
were then deceased, written consent was obtained from the patients
prior to their death.
Patient consent for publication
Written informed consent has been obtained from the
patients for the publication of their data. In the 2 cases which
were then deceased, written consent was obtained from the patients
prior to their death.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Mattison MLP: Delirium. Ann Intern Med.
173:ITC49–ITC64. 2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Hshieh TT, Inouye SK and Oh ES: Delirium
in the Elderly. Psychiatr Clin North Am. 41:1–17. 2018.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Maldonado JR: Acute brain failure:
Pathophysiology, diagnosis, management, and sequelae of delirium.
Crit Care Clin. 33:461–519. 2017.PubMed/NCBI View Article : Google Scholar
|
|
4
|
American Psychiatric Association:
Diagnostic and statistical manual of mental disorders. 5th edition.
American Psychiatric Association, Washington, DC, 2013.
|
|
5
|
Ely EW, Shintani A, Truman B, Speroff T,
Gordon SM, Harrell FE Jr, Inouye SK, Bernard GR and Dittus RS:
Delirium as a predictor of mortality in mechanically ventilated
patients in the intensive care unit. JAMA. 291:1753–1762.
2004.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Marcantonio ER: Delirium in hospitalized
older adults. N Engl J Med. 377:1456–1466. 2017.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Cipriani G, Danti S, Nuti A, Carlesi C,
Lucetti C and Di Fiorino M: A complication of coronavirus disease
2019: Delirium. Acta Neurol Belg. 120:927–932. 2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Susano MJ, Dias M, Seixas FS, Vide S,
Grasfield R, Abelha FJ, Crosby G, Culley DJ and Amorim P:
Association among preoperative cognitive performance, regional
cerebral oxygen saturation, and postoperative delirium in older
portuguese patients. Anesth Analg. 132:846–855. 2021.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Xue FS, Liu SH and Hou HJ: Association
between postoperative delirium and cerebral oxygen desaturation in
older patients undergoing cardiac surgery. Comment on Br J Anaesth
2020; 124: 146-53. Br J Anaesth. 127:e98–e99. 2021.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Eertmans W, De Deyne C, Genbrugge C,
Marcus B, Bouneb S, Beran M, Fret T, Gutermann H, Boer W, Vander
Laenen M, et al: Association between postoperative delirium and
postoperative cerebral oxygen desaturation in older patients after
cardiac surgery. Br J Anaesth. 124:146–153. 2020.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Stollings JL, Kotfis K, Chanques G, Pun
BT, Pandharipande PP and Ely EW: Delirium in critical illness:
Clinical manifestations, outcomes, and management. Intensive Care
Med. 47:1089–1103. 2021.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Vella F, Senia P, Ceccarelli M, Vitale E,
Maltezou H, Taibi R, Lleshi A, Venanzi Rullo E, Pellicanò GF,
Rapisarda V, et al: Transmission mode associated with coronavirus
disease 2019: A review. Eur Rev Med Pharmacol Sci. 24:7889–7904.
2020.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Lai A, Bergna A, Menzo S, Zehender G,
Caucci S, Ghisetti V, Rizzo F, Maggi F, Cerutti F, Giurato G, et
al: Circulating SARS-CoV-2 variants in Italy, October 2020-March
2021. Virol J. 18(168)2021.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Lai A, Bergna A, Caucci S, Clementi N,
Vicenti I, Dragoni F, Cattelan AM, Menzo S, Pan A, Callegaro A, et
al: Molecular tracing of SARS-CoV-2 in Italy in the first three
months of the epidemic. Viruses. 12(798)2020.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Ceccarelli M, Berretta M, Venanzi Rullo E,
Nunnari G and Cacopardo B: Differences and similarities between
severe acute respiratory Syndrome (SARS)-CoronaVirus (CoV) and
SARS-CoV-2. Would a rose by another name smell as sweet? Eur Rev
Med Pharmacol Sci. 24:2781–2783. 2020.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Meduri A, Oliverio GW, Mancuso G,
Giuffrida A, Guarneri C, Venanzi Rullo E, Nunnari G and Aragona P:
Ocular surface manifestation of COVID-19 and tear film analysis.
Sci Rep. 10(20178)2020.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Guarneri C, Rullo EV, Pavone P, Berretta
M, Ceccarelli M, Natale A and Nunnari G: Silent COVID-19: What your
skin can reveal. Lancet Infect Dis. 21:24–25. 2021.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Pirisi M, Rigamonti C, D'Alfonso S,
Nebuloni M, Fanni D, Gerosa C, Orrù G, Venanzi Rullo E, Pavone P,
Faa G, et al: Liver infection and COVID-19: the electron microscopy
proof and revision of the literature. Eur Rev Med Pharmacol Sci.
25:2146–2151. 2021.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Guarneri C, Venanzi Rullo E, Gallizzi R,
Ceccarelli M, Cannavò SP and Nunnari G: Diversity of clinical
appearance of cutaneous manifestations in the course of COVID-19. J
Eur Acad Dermatol Venereol. 34:e449–e450. 2020.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Ceccarelli M, Marino A, Cosentino F,
Moscatt V, Celesia BM, Gussio M, Bruno R, Rullo EV, Nunnari G and
Cacopardo BS: Post-infectious ST elevation myocardial infarction
following a COVID-19 infection: A case report. Biomed Rep.
16(10)2022.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Longhitano E, Nardi C, Calabrese V,
Messina R, Mazzeo G, Venanzi Rullo E, Ceccarelli M, Chatrenet A,
Saulnier P, Torreggiani M, et al: Hypernatraemia and low eGFR at
hospitalization in COVID-19 patients: A deadly combination. Clin
Kidney J. 14:2227–2233. 2021.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Calabrese V, Micali C, Russotto Y, Laganà
N, Gullotta C, Pisano A, Santoro D, Nunnari G and Venanzi Rullo E:
Arteriovenous fistula thrombosis in hemodialysis patients with
COVID-19: Epiphenomenon or marker of severe clinical disease? G
Ital Nefrol. 39:2022–vol3. 2022.PubMed/NCBI
|
|
23
|
Pavone P, Ceccarelli M, Marino S, Caruso
D, Falsaperla R, Berretta M, Rullo EV and Nunnari G: SARS-CoV-2
related paediatric acute-onset neuropsychiatric Syndrome. Lancet
Child Adolesc Health. 5:e19–e21. 2021.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Buccafusca M, Micali C, Autunno M, Versace
AG, Nunnari G and Musumeci O: Favourable course in a cohort of
Parkinson's disease patients infected by SARS-CoV-2: A
single-centre experience. Neurol Sci. 42:811–816. 2021.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Kotfis K, Williams Roberson S, Wilson JE,
Dabrowski W, Pun BT and Ely EW: COVID-19: ICU delirium management
during SARS-CoV-2 pandemic. Crit Care. 24(176)2020.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Santos CJ, Nuradin N, Joplin C, Leigh AE,
Burke RV, Rome R, McCall J and Raines AM: Risk factors for delirium
among SARS-CoV-2 positive veterans. Psychiatry Res.
309(114375)2022.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Woolley B: The COVID-19 conundrum: Where
both the virus and treatment contribute to delirium. Geriatr Nurs.
42:955–958. 2021.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Pun BT, Badenes R, Heras La Calle G, Orun
OM, Chen W, Raman R, Simpson BK, Wilson-Linville S, Hinojal
Olmedillo B, Vallejo de la Cueva A, et al: Prevalence and risk
factors for delirium in critically ill patients with COVID-19
(COVID-D): A multicentre cohort study. Lancet Respir Med.
9:239–250. 2021.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Rogers JP, Chesney E, Oliver D, Pollak TA,
McGuire P, Fusar-Poli P, Zandi MS, Lewis G and David AS:
Psychiatric and neuropsychiatric presentations associated with
severe coronavirus infections: A systematic review and
meta-analysis with comparison to the COVID-19 pandemic. Lancet
Psychiatry. 7:611–627. 2020.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Garcez FB, Aliberti MJR, Poco PCE,
Hiratsuka M, Takahashi SF, Coelho VA, Salotto DB, Moreira MLV,
Jacob-Filho W and Avelino-Silva TJ: Delirium and adverse outcomes
in hospitalized patients with COVID-19. J Am Geriatr Soc.
68:2440–2446. 2020.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Helms J, Kremer S, Merdji H, Schenck M,
Severac F, Clere-Jehl R, Studer A, Radosavljevic M, Kummerlen C,
Monnier A, et al: Delirium and encephalopathy in severe COVID-19: A
cohort analysis of ICU patients. Crit Care. 24(491)2020.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Skipper AW and Zanetos J: The importance
of delirium before and after COVID-19. J Gerontol Nurs. 47:3–5.
2021.PubMed/NCBI View Article : Google Scholar
|
|
33
|
de Sousa Moreira JL, Barbosa SMB, Vieira
JG, Chaves NCB, Felix EBG, Feitosa PWG, da Cruz IS, da Silva CGL
and Neto MLR: The psychiatric and neuropsychiatric repercussions
associated with severe infections of COVID-19 and other
coronaviruses. Prog Neuropsychopharmacol Biol Psychiatry.
106(110159)2021.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Kennedy M, Helfand BKI, Gou RY, Gartaganis
SL, Webb M, Moccia JM, Bruursema SN, Dokic B, McCulloch B, Ring H,
et al: Delirium in older patients with COVID-19 presenting to the
emergency department. JAMA Netw Open. 3(e2029540)2020.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Forget MF, Del Degan S, Leblanc J, Tannous
R, Desjardins M, Durand M, Vu TTM, Nguyen QD and Desmarais P:
Delirium and inflammation in older adults hospitalized for
COVID-19: A cohort study. Clin Interv Aging. 16:1223–1230.
2021.PubMed/NCBI View Article : Google Scholar
|
|
36
|
M AS, E DP and Jl AM: Delirium in
hospitalized COVID-19 patients: A case series. Psychiatry Res.
305(114245)2021.PubMed/NCBI View Article : Google Scholar
|
|
37
|
García-Grimshaw M, Chiquete E,
Jiménez-Ruiz A, Vidal-Mayo JJ, Grajeda-González SL, Vargas-Martínez
MLÁ, Toapanta-Yanchapaxi LN, Valdés-Ferrer SI, Chávez-Martínez OA,
Marché-Fernández OA, et al: Delirium and associated factors in a
cohort of hospitalized patients with coronavirus disease 2019. J
Acad Consult Liaison Psychiatry. 63:3–13. 2022.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Turan Ş, Poyraz BÇ, Aksoy Poyraz C,
Demirel ÖF, Tanrıöver Aydın E, Uçar Bostan B, Demirel Ö and Ali RK:
Characteristics and outcomes of COVID-19 inpatients who underwent
psychiatric consultations. Asian J Psychiatr.
57(102563)2021.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Watne LO, Tonby K, Holten AR, Olasveengen
TM, Romundstad LG and Neerland BE: Delirium is common in patients
hospitalized with COVID-19. Intern Emerg Med. 16:1997–2000.
2021.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Maeker É and Maeker-Poquet B: Delirium, a
possible typical presentation of COVID-19 in the elderly. Soins
Gerontol. 26:10–15. 2021.PubMed/NCBI View Article : Google Scholar : (In French).
|
|
41
|
Haddad PM, Alabdulla M, Latoo J and Iqbal
Y: Delirious mania in a patient with COVID-19 pneumonia. BMJ Case
Rep. 14(e243816)2021.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Bauer SC, Moral F, Preloger E, Spindler A,
Roman M, Logan A, Sandage SJ, Manak C and Mitchell M: Pediatric
COVID-19 delirium: Case report of 2 adolescents. WMJ. 120:131–136.
2021.PubMed/NCBI
|
|
43
|
Castro REV, Rodríguez-Rubio M,
Magalhães-Barbosa MC and Prata-Barbosa A: Pediatric delirium in
times of COVID-19. Rev Bras Ter Intensiva. 33:483–486.
2022.PubMed/NCBI View Article : Google Scholar : (In English,
Portuguese).
|
|
44
|
Gasnier M, Choucha W, Radiguer F, Bougarel
A, Faulet T, Kondarjian C, Thorey P, Baldacci A, Ballerini M, Ait
Tayeb AEK, et al: Acute objective severity of COVID-19 Infection
and psychiatric disorders 4 months after hospitalization for
COVID-19. J Clin Psychiatry. 83(21br14179)2021.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Di Giacomo E, Colmegna F, Santorelli M,
Pessina R, D'Amico E, Marcatili M, Dakanalis A, Pavone F, Fagiolini
A and Clerici M: Delirium in the ‘young’ covid-19 patient (<65
years): Preliminary clinical indications. Riv Psichiatr. 56:85–92.
2021.PubMed/NCBI View Article : Google Scholar : (In Italian).
|
|
46
|
Facciolà A, Micali C, Visalli G, Venanzi
Rullo E, Russotto Y, Laganà P, Laganà A, Nunnari G and Di Pietro A:
COVID-19 and pregnancy: Clinical outcomes and scientific evidence
about vaccination. Eur Rev Med Pharmacol Sci. 26:2610–2626.
2022.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Ceccarelli M, Nunnari G, Celesia BM,
Pellicanò GF, Venanzi Rullo E, Berretta M and Santi Cacopardo B:
Editorial-Coronavirus disease 2019 and people living with HIV:
Clinical considerations Eur Rev Med. Pharmacol Sci. 24:7534–7539.
2020.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Butt I, Sawlani V and Geberhiwot T:
Prolonged confusional state as first manifestation of COVID-19. Ann
Clin Transl Neurol. 7:1450–1452. 2020.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Beach SR, Praschan NC, Hogan C, Dotson S,
Merideth F, Kontos N, Fricchione GL and Smith FA: Delirium in
COVID-19: A case series and exploration of potential mechanisms for
central nervous system involvement. Gen Hosp Psychiatry. 65:47–53.
2020.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Zazzara MB, Penfold RS, Roberts AL, Lee
KA, Dooley H, Sudre CH, Welch C, Bowyer RCE, Visconti A, Mangino M,
et al: Probable delirium is a presenting symptom of COVID-19 in
frail, older adults: A cohort study of 322 hospitalised and 535
community-based older adults. Age Ageing. 50:40–48. 2021.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Tyson B, Shahein A, Erdodi L, Tyson L,
Tyson R, Ghomi R and Agarwal P: Delirium as a presenting symptom of
COVID-19. Cogn Behav Neurol. 35:123–129. 2022.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Toniolo S, Di Lorenzo F, Scarioni M,
Frederiksen KS and Nobili F: Is the frontal lobe the primary target
of SARS-CoV-2? J Alzheimers Dis. 81:75–81. 2021.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Harapan BN and Yoo HJ: Neurological
symptoms, manifestations, and complications associated with severe
acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and
coronavirus disease 19 (COVID-19). J Neurol. 268:3059–3071.
2021.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Pensato U, Muccioli L, Cani I, Janigro D,
Zinzani PL, Guarino M, Cortelli P and Bisulli F: Brain dysfunction
in COVID-19 and CAR-T therapy: Cytokine storm-associated
encephalopathy. Ann Clin Transl Neurol. 8:968–979. 2021.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Østergaard L: SARS CoV-2 related
microvascular damage and symptoms during and after COVID-19:
Consequences of capillary transit-time changes, tissue hypoxia and
inflammation. Physiol Rep. 9(e14726)2021.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Velásquez-Tirado JD, Trzepacz PT and
Franco JG: Etiologies of delirium in consecutive COVID-19
inpatients and the relationship between severity of delirium and
COVID-19 in a prospective study with follow-up. J Neuropsychiatry
Clin Neurosci. 33:210–218. 2021.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Schneider F, Agin A, Baldacini M, Maurer
L, Schenck M, Alemann M, Solis M, Helms J, Villette C, Artzner T,
et al: Acute-onset delirium in intensive care COVID patients:
Association of imperfect brain repair with foodborne
micro-pollutants. Eur J Neurol. 28:3443–3447. 2021.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Cuperlovic-Culf M, Cunningham EL,
Teimoorinia H, Surendra A, Pan X, Bennett SAL, Jung M, McGuiness B,
Passmore AP, Beverland D and Green BD: Metabolomics and
computational analysis of the role of monoamine oxidase activity in
delirium and SARS-COV-2 infection. Sci Rep.
11(10629)2021.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Moretti P, Brufani F, Pierotti V, Pomili
G, Di Buò A, Giulietti C, Masini F, Tanku V, Bachetti MC, Menculini
G and Tortorella A: Neurotropism and neuropsychiatric symptomsi in
patients with COVID-19. Psychiatr Danub. 33 (Suppl 11):S10–S13.
2021.PubMed/NCBI
|
|
60
|
Batra A, Clark JR, Kang AK, Ali S, Patel
TR, Shlobin NA, Hoffman SC, Lim PH, Orban ZS, Visvabharathy L, et
al: Persistent viral RNA shedding of SARS-CoV-2 is associated with
delirium incidence and six-month mortality in hospitalized COVID-19
patients. Geroscience. 44:1241–1254. 2022.PubMed/NCBI View Article : Google Scholar
|
|
61
|
Dias R, Caldas JP, Silva-Pinto A, Costa A,
Sarmento A and Santos L: Delirium severity in critical patients
with COVID-19 from an infectious disease intensive care unit. Int J
Infect Dis. 118:109–115. 2022.PubMed/NCBI View Article : Google Scholar
|
|
62
|
Shao SC, Lai CC, Chen YH, Chen YC, Hung MJ
and Liao SC: Prevalence, incidence and mortality of delirium in
patients with COVID-19: A systematic review and meta-analysis. Age
Ageing. 50:1445–1453. 2021.PubMed/NCBI View Article : Google Scholar
|
|
63
|
Pranata R, Huang I, Lim MA, Yonas E, Vania
R and Kuswardhani RAT: Delirium and mortality in coronavirus
disease 2019 (COVID-19)-A systematic review and meta-analysis. Arch
Gerontol Geriatr. 95(104388)2021.PubMed/NCBI View Article : Google Scholar
|
|
64
|
Rebora P, Rozzini R, Bianchetti A,
Blangiardo P, Marchegiani A, Piazzoli A, Mazzeo F, Cesaroni G,
Chizzoli A, Guerini F, et al: Delirium in patients with SARS-CoV-2
infection: A multicenter study. J Am Geriatr Soc. 69:293–299.
2021.PubMed/NCBI View Article : Google Scholar
|
|
65
|
Hariyanto TI, Putri C, Hananto JE, Arisa
J, Fransisca V, Situmeang R and Kurniawan A: Delirium is a good
predictor for poor outcomes from coronavirus disease 2019
(COVID-19) pneumonia: A systematic review, meta-analysis, and
meta-regression. J Psychiatr Res. 142:361–368. 2021.PubMed/NCBI View Article : Google Scholar
|
|
66
|
Peterson A, Marengoni A, Shenkin S and
MacLullich A: Delirium in COVID-19: Common, distressing and linked
with poor outcomes. can we do better? Age Ageing. 50:1436–1438.
2021.PubMed/NCBI View Article : Google Scholar
|
|
67
|
Morandi A, Rebora P, Isaia G, Grossi E,
Faraci B, Gentile S, Bo M, Valsecchi MG, Deiana V, Ghezzi N, et al:
Delirium symptoms duration and mortality in SARS-COV2 elderly:
Results of a multicenter retrospective cohort study. Aging Clin Exp
Res. 33:2327–2333. 2021.PubMed/NCBI View Article : Google Scholar
|
|
68
|
Mcloughlin BC, Miles A, Webb TE, Knopp P,
Eyres C, Fabbri A, Humphries F and Davis D: Functional and
cognitive outcomes after COVID-19 delirium. Eur Geriatr Med.
11:857–862. 2020.PubMed/NCBI View Article : Google Scholar
|
|
69
|
Liu YH, Wang YR, Wang QH, Chen Y, Chen X,
Li Y, Cen Y, Xu C, Hu T, Liu XD, et al: Post-infection cognitive
impairments in a cohort of elderly patients with COVID-19. Mol
Neurodegener. 16(48)2021.PubMed/NCBI View Article : Google Scholar
|
|
70
|
Duggan MC, Van J and Ely EW: Delirium
assessment in critically Ill older adults: Considerations during
the COVID-19 Pandemic. Crit Care Clin. 37:175–190. 2021.PubMed/NCBI View Article : Google Scholar
|
|
71
|
Meagher D, Adamis D, Timmons S, O'Regan
NA, O'Keeffe S, Kennelly S, Corby C, Meaney AM, Reynolds P, Mohamad
M, et al: Developing a guidance resource for managing delirium in
patients with COVID-19. Ir J Psychol Med. 38:208–213.
2021.PubMed/NCBI View Article : Google Scholar
|
|
72
|
Rahman S and Byatt K: Follow-up services
for delirium after COVID-19-where now? Age Ageing. 50:601–604.
2021.PubMed/NCBI View Article : Google Scholar
|
|
73
|
Hara M, Kouda K, Mizoguchi T, Yokota Y,
Hayashi K, Gon Y and Nakajima H: COVID-19 post-infectious
encephalitis presenting with delirium as an initial manifestation.
J Investig Med High Impact Case Rep.
9(23247096211029787)2021.PubMed/NCBI View Article : Google Scholar
|
|
74
|
Aroos R, Wong BLL and Merchant RA: Delayed
health consequences of COVID-19 lockdown in an older adult. Age
Ageing. 50:673–675. 2021.PubMed/NCBI View Article : Google Scholar
|
|
75
|
Ragheb J, McKinney A, Zierau M, Brooks J,
Hill-Caruthers M, Iskander M, Ahmed Y, Lobo R, Mentz G and Vlisides
PE: Delirium and neuropsychological outcomes in critically Ill
patients with COVID-19: A cohort study. BMJ Open.
11(e050045)2021.PubMed/NCBI View Article : Google Scholar
|
|
76
|
Mendes A, Herrmann FR, Périvier S, Gold G,
Graf CE and Zekry D: Delirium in older patients with COVID-19:
Prevalence, risk factors, and clinical relevance. J Gerontol A Biol
Sci Med Sci. 76:e142–e146. 2021.PubMed/NCBI View Article : Google Scholar
|
|
77
|
Fabrazzo M, Russo A, Camerlengo A, Tucci
C, Luciano M, De Santis V, Perris F, Catapano F and Coppola N:
Delirium and cognitive impairment as predisposing factors of
COVID-19 infection in neuropsychiatric patients: A narrative
review. Medicina (Kaunas). 57(1244)2021.PubMed/NCBI View Article : Google Scholar
|
|
78
|
Ekmekyapar T, Ekmekyapar M, Tasci I, Sahin
L and Delen LA: Clinical features and predisposing factors of
delirium due to COVID-19 pneumonia in intensive care units. Eur Rev
Med Pharmacol Sci. 26:4440–4448. 2022.PubMed/NCBI View Article : Google Scholar
|
|
79
|
Pagali S, Fu S, Lindroth H, Sohn S, Burton
MC and Lapid M: Delirium occurrence and association with outcomes
in hospitalized COVID-19 patients. Int Psychogeriatr. 33:1105–1109.
2021.PubMed/NCBI View Article : Google Scholar
|
|
80
|
van Reekum EA, Rosic T, Sergeant A, Sanger
N, Rodrigues M, Rebinsky R, Panesar B, Deck E, Kim N, Woo J, et al:
Delirium and other neuropsychiatric manifestations of COVID-19
infection in people with preexisting psychiatric disorders: A
systematic review. J Med Case Rep. 15(586)2021.PubMed/NCBI View Article : Google Scholar
|
|
81
|
Dinakaran D, Manjunatha N, Naveen Kumar C
and Suresh BM: Neuropsychiatric aspects of COVID-19 pandemic: A
selective review. Asian J Psychiatr. 53(102188)2020.PubMed/NCBI View Article : Google Scholar
|
|
82
|
Munjal S, Ferrando SJ and Freyberg Z:
Neuropsychiatric aspects of infectious diseases: An update. Crit
Care Clin. 33:681–712. 2017.PubMed/NCBI View Article : Google Scholar
|
|
83
|
Guan WJ, Liang WH, Zhao Y, Liang HR, Chen
ZS, Li YM, Liu XQ, Chen RC, Tang CL, Wang T, et al: Comorbidity and
its impact on 1590 patients with COVID-19 in China: A nationwide
analysis. Eur Respir J. 55(2000547)2020.PubMed/NCBI View Article : Google Scholar
|
|
84
|
D'Ardes D, Carrarini C, Russo M, Dono F,
Speranza R, Digiovanni A, Martinotti G, Di Iorio A, Onofrj M,
Cipollone F and Bonanni L: Low molecular weight heparin in COVID-19
patients prevents delirium and shortens hospitalization. Neurol
Sci. 42:1527–1530. 2021.PubMed/NCBI View Article : Google Scholar
|
|
85
|
Martinotti G, Bonanni L, Barlati S, Miuli
A, Sepede G, Prestia D, Trabucco A, Palumbo C, Massaro A, Olcese M,
et al: Delirium in COVID-19 patients: A multicentric observational
study in Italy. Neurol Sci. 42:3981–3988. 2021.PubMed/NCBI View Article : Google Scholar
|
|
86
|
Boer H, Soekhai MTD, Renes MH, Schoevers
RA and Jiawan VCR: Neuropsychiatric manifestations of COVID-19 in
intensive care unit patients. Tijdschr Psychiatr. 63:509–513.
2021.PubMed/NCBI(In Dutch).
|
|
87
|
Haller J: Aggression, aggression-related
psychopathologies and their models. Front Behav Neurosci.
16(936105)2022.PubMed/NCBI View Article : Google Scholar
|
|
88
|
Merlo EM, Stoian AP, Motofei IG and
Settineri S: The role of suppression and the maintenance of
euthymia in clinical settings. Front Psychol.
12(677811)2021.PubMed/NCBI View Article : Google Scholar
|
|
89
|
Sweileh WM: Research trends and scientific
analysis of publications on burnout and compassion fatigue among
healthcare providers. J Occup Med Toxicol. 15(23)2020.PubMed/NCBI View Article : Google Scholar
|
|
90
|
Merlo EM, Stoian AP, Motofei IG and
Settineri S: Clinical psychological figures in healthcare
professionals: Resilience and maladjustment as the ‘Cost of Care’.
Front Psychol. 11(607783)2020.PubMed/NCBI View Article : Google Scholar
|
|
91
|
Arbelo N, López-Pelayo H, Sagué M, Madero
S, Pinzón-Espinosa J, Gomes-da-Costa S, Ilzarbe L, Anmella G, Llach
CD, Imaz ML, et al: Psychiatric clinical profiles and
pharmacological interactions in COVID-19 inpatients referred to a
consultation liaison psychiatry unit: A cross-sectional study.
Psychiatr Q. 92:1021–1033. 2021.PubMed/NCBI View Article : Google Scholar
|
|
92
|
Italian Society of Psychiatry:
Recommendations on activities and measures to contrasts and
contains SARS-CoV-19 virus. https://www.evidence-based-psychiatric-care.org/wp-content/uploads/2020/04/SARS-COV-19_Suppl_Speciale_Rivista_SIP_ita.pdf.pdf.
Acessed April 05, 2020.
|
|
93
|
Baller EB, Hogan CS, Fusunyan MA, Ivkovic
A, Luccarelli JW, Madva E, Nisavic M, Praschan N, Quijije NV, Beach
SR and Smith FA: Neurocovid: Pharmacological recommendations for
delirium associated with COVID-19. Psychosomatics. 61:585–596.
2020.PubMed/NCBI View Article : Google Scholar
|
|
94
|
Khosravi M: Letter to the editor:
Quetiapine safety in ICU delirium management among
SARS-CoV-2-infected patients. J Psychosom Res.
149(110598)2021.PubMed/NCBI View Article : Google Scholar
|
|
95
|
Marino A, Campanella E, Ceccarelli M,
Larocca L, Bonomo C, Micali C and Cacopardo B: (2022). Sarilumab
administration in patients with severe COVID-19: A report of four
cases and a literature review. World Acad Sci J 4, 24. https://doi.org/10.3892/wasj.2022.159.
|
|
96
|
Marino A, Pampaloni A, Scuderi D,
Cosentino F, Moscatt V and Ceccarelli M.: Cacopardo, B. (2020):
High-flow nasal cannula oxygenation and tocilizumab administration
in patients critically ill with COVID-19: A report of three cases
and a literature review. World Acad Sci J 2: 23. https://doi.org/10.3892/wasj.2020.64.
|
|
97
|
Ceccarelli M, Pavone P, Venanzi Rullo E
and Nunnari G: Comment on safety and efficacy of oral
lopinavir/ritonavir in pediatric patients with coronavirus disease:
A nationwide comparative analysis. Eur Rev Med Pharmacol Sci.
25:2473–2474. 2021.PubMed/NCBI View Article : Google Scholar
|
|
98
|
Syed S, Couse M and Ojha R: Management
challenges in patients with comorbid COVID-19 associated delirium
and serious mental illness-A case series. Int J Psychiatry Med.
56:255–265. 2021.PubMed/NCBI View Article : Google Scholar
|
|
99
|
Mota P: Delirium in COVID-19 elderly
patients: Raising awareness to the importance of its early
detection and therapeutic intervention. Acta Med Port.
34(318)2021.PubMed/NCBI View Article : Google Scholar : (In
Portuguese).
|
|
100
|
Radhakrishnan NS, Mufti M, Ortiz D, Maye
ST, Melara J, Lim D, Rosenberg EI and Price CC: Implementing
delirium prevention in the Era of COVID-19. J Alzheimers Dis.
79:31–36. 2021.PubMed/NCBI View Article : Google Scholar
|
|
101
|
Castro REV, Garcez FB and Avelino-Silva
TJ: Patient care during the COVID-19 pandemic: Do not leave
delirium behind. Braz J Psychiatry. 43:127–128. 2021.PubMed/NCBI View Article : Google Scholar
|