|
1
|
Dunn GP, Old LJ and Schreiber RD: The
three Es of cancer immunoediting. Annu Rev Immunol. 22:329–360.
2004.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Abbott M and Ustoyev Y: Cancer and the
immune system: The history and background of immunotherapy. Semin
Oncol Nurs. 35(150923)2019.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Kennedy LB and Salama AKS: A review of
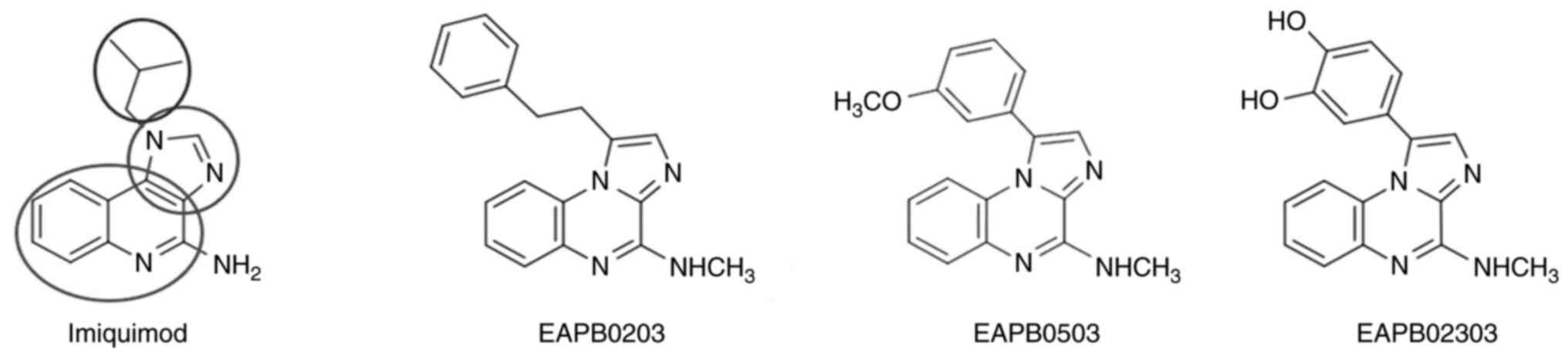
cancer immunotherapy toxicity. CA Cancer J Clin. 70:86–104.
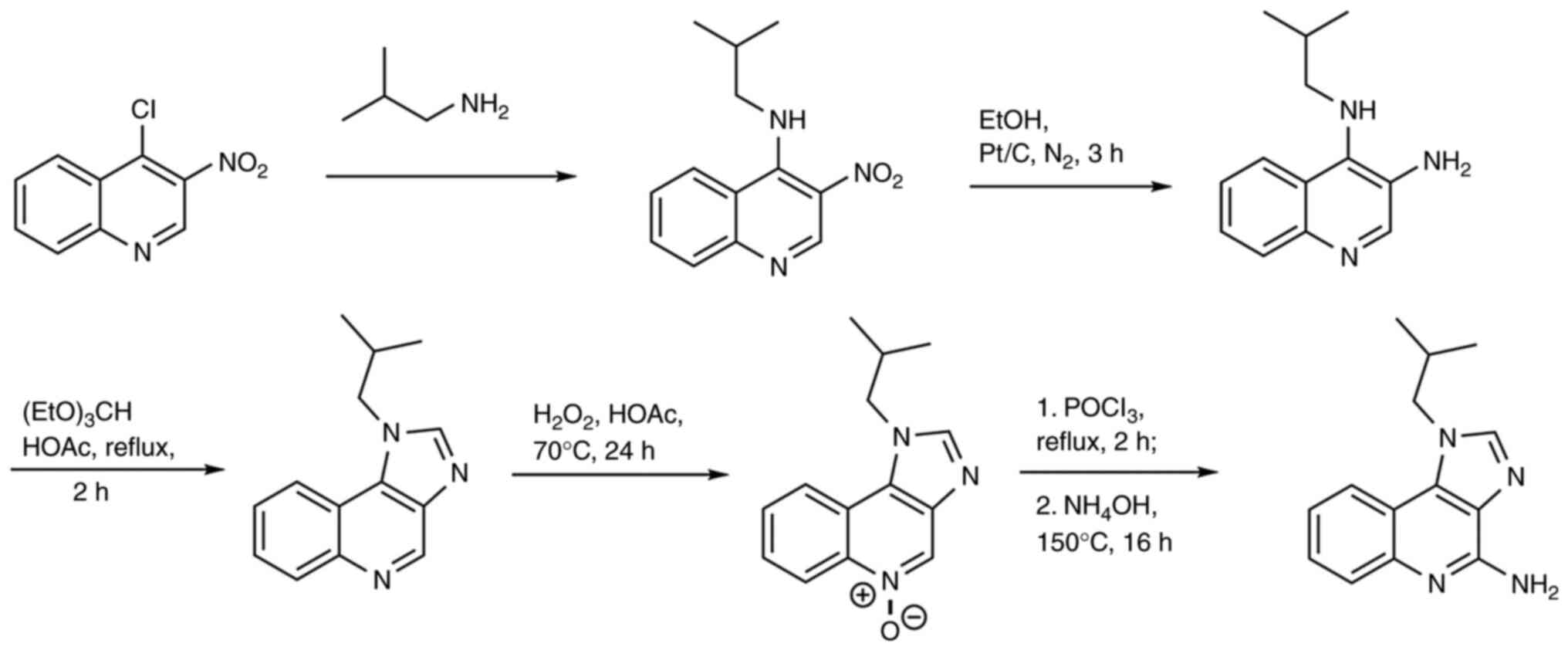
2020.PubMed/NCBI View Article : Google Scholar
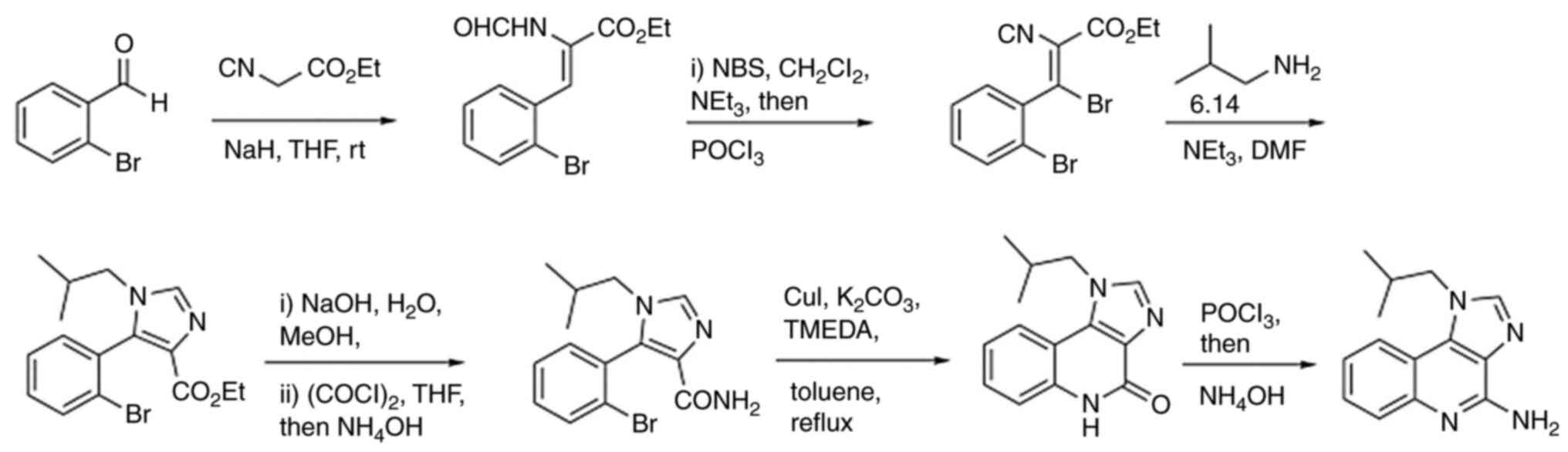
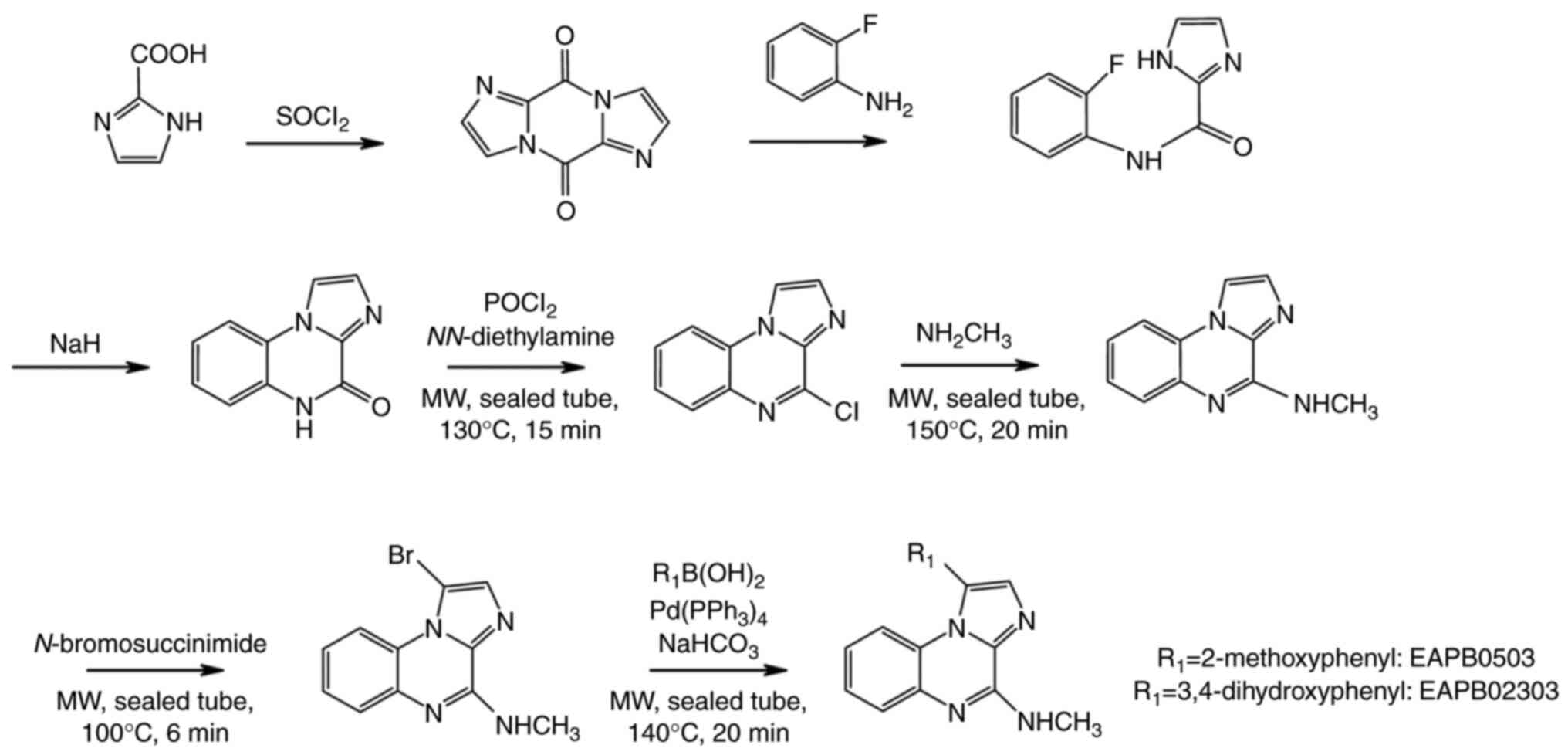
|
|
4
|
Avorn J: Learning about the safety of
drugs-a half-century of evolution. N Engl J Med. 365:2151–2153.
2011.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Wu Y, Yang Z, Cheng K, Bi H and Chen J:
Small molecule-based immunomodulators for cancer therapy. Acta
Pharm Sin B. 12:4287–4308. 2022.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Kumar AR, Devan AR, Nair B, Vinod BS and
Nath LR: Harnessing the immune system against cancer: Current
immunotherapy approaches and therapeutic targets. Mol Biol Rep.
48:8075–8095. 2021.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Liu SV, Reck M, Mansfield AS, Mok T,
Scherpereel A, Reinmuth N, Garassino MC, Carpeno JD, Califano R,
Nishio M, et al: Updated overall survival and PD-L1 subgroup
analysis of patients with extensive-stage small-cell lung cancer
treated with Atezolizumab, Carboplatin, and Etoposide (IMpower133).
J Clin Oncol. 39:619–630. 2021.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Vaddepally RK, Kharel P, Pandey R, Garje R
and Chandra AB: Review of indications of FDA-approved immune
checkpoint inhibitors per NCCN guidelines with the level of
evidence. Cancers (Basel). 12(738)2020.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Chen XY, Li YD, Xie Y, Cao LQ, Ashby CR
Jr, Zhao H and Chen ZS: Nivolumab and relatlimab for the treatment
of melanoma. Drugs Today (Barc). 59:91–104. 2023.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Kang C: Retifanlimab: First approval.
Drugs. 83:731–737. 2023.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Di Trolio R, Simeone E, Di Lorenzo G,
Grimaldi AM, Romano A, Ayala F, Caracò C, Mozzillo N and Ascierto
PA: Update on PEG-interferon α-2b as adjuvant therapy in melanoma.
Anticancer Res. 32:3901–3909. 2012.PubMed/NCBI
|
|
12
|
Qureshi YA, Karp CL and Dubovy SR:
Intralesional interferon alpha-2b therapy for adnexal Kaposi
sarcoma. Cornea. 28:941–943. 2009.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Rallis KS, Corrigan AE, Dadah H, George
AM, Keshwara SM, Sideris M and Szabados B: Cytokine-based cancer
immunotherapy: Challenges and opportunities for IL-10. Anticancer
Res. 41:3247–3252. 2021.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Lamb YN: Pexidartinib: First Approval.
Drugs. 79:1805–1812. 2019.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Hemmi H, Kaisho T, Takeuchi O, Sato S,
Sanjo H, Hoshino K, Horiuchi T, Tomizawa H, Takeda K and Akira S:
Small anti-viral compounds activate immune cells via the TLR7
MyD88-dependent signaling pathway. Nat Immunol. 3:196–200.
2002.PubMed/NCBI View
Article : Google Scholar
|
|
16
|
Kamath P, Darwin E, Arora H and Nouri K: A
review on imiquimod therapy and discussion on optimal management of
basal cell carcinomas. Clin Drug Investig. 38:883–899.
2018.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Tyring S: Imiquimod applied topically: A
novel immune response modifier. Skin Therapy Lett. 6:1–4.
2001.PubMed/NCBI
|
|
18
|
Courbet A, Bec N, Constant C, Larroque C,
Pugniere M, Messaoudi SE, Zghaib Z, Khier S, Deleuze-Masquefa C and
Gattacceca F: Imidazoquinoxaline anticancer derivatives and
imiquimod interact with tubulin: Characterization of molecular
microtubule inhibiting mechanisms in correlation with cytotoxicity.
PLoS One. 12(e0182022)2017.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Moarbess G, Deleuze-Masquefa C, Bonnard V,
Gayraud-Paniagua S, Vidal JR, Bressolle F, Pinguet F and Bonnet PA:
In vitro and in vivo anti-tumoral activities of
imidazo[1,2-a]quinoxaline, imidazo[1,5-a]quinoxaline, and
pyrazolo[1,5-a]quinoxaline derivatives. Bioorg Med Chem.
16:6601–6610. 2008.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Deleuze-Masquefa C, Moarbess G, Khier S,
David N, Gayraud-Paniagua S, Bressolle F, Pinguet F and Bonnet PA:
New imidazo[1,2-a]quinoxaline derivatives: Synthesis and in vitro
activity against human melanoma. Eur J Med Chem. 44:3406–3411.
2009.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Kwong A, Sanlorenzo M, Rappersberger K and
Vujic I: Update on advanced melanoma treatments: Small molecule
targeted therapy, immunotherapy, and future combination therapies.
Wien Med Wochenschr. 169:314–322. 2019.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Zghaib Z, Guichou JF, Vappiani J, Bec N,
Hadj-Kaddour K, Vincent LA, Paniagua-Gayraud S, Larroque C,
Moarbess G, Cuq P, et al: New imidazoquinoxaline derivatives:
Synthesis, biological evaluation on melanoma, effect on tubulin
polymerization and structure-activity relationships. Bioorg Med
Chem. 24:2433–2440. 2016.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Moarbess G, El-Hajj H, Kfoury Y, El-Sabban
ME, Lepelletier Y, Hermine O, Deleuze-Masquéfa C, Bonnet PA and
Bazarbachi A: EAPB0203, a member of the imidazoquinoxaline family,
inhibits growth and induces caspase-dependent apoptosis in T-cell
lymphomas and HTLV-I-associated adult T-cell leukemia/lymphoma.
Blood. 111:3770–3777. 2008.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Saliba J, Deleuze-Masquéfa C, Iskandarani
A, El Eit R, Hmadi R, Mahon FX, Bazarbachi A, Bonnet PA and Nasr R:
EAPB0503, a novel imidazoquinoxaline derivative, inhibits growth
and induces apoptosis in chronic myeloid leukemia cells. Anticancer
Drugs. 25:624–632. 2014.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Nabbouh AI, Hleihel RS, Saliba JL, Karam
MM, Hamie MH, Wu HCJM, Berthier CP, Tawil NM, Bonnet PAA,
Deleuze-Masquefa C and El Hajj HA: Imidazoquinoxaline derivative
EAPB0503: A promising drug targeting mutant nucleophosmin 1 in
acute myeloid leukemia. Cancer. 123:1662–1673. 2017.PubMed/NCBI View Article : Google Scholar
|
|
26
|
El Hajj R, Youness HB, Lachaud L, Bastien
P, Masquefa C, Bonnet PA, El Hajj H and Khalifeh I: EAPB0503: An
Imiquimod analog with potent in vitro activity against cutaneous
leishmaniasis caused by Leishmania major and Leishmania tropica.
PLoS Negl Trop Dis. 12(e0006854)2018.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Baumann M and Baxendale IR: An overview of
the synthetic routes to the best selling drugs containing
6-membered heterocycles. Beilstein J Org Chem. 9:2265–2319.
2013.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Rudy SJ: Imiquimod (Aldara): Modifying the
immune response. Dermatol Nurs. 14:268–270. 2002.PubMed/NCBI
|
|
29
|
Miller RL, Gerster JF, Owens ML, Slade HB
and Tomai MA: Imiquimod applied topically: A novel immune response
modifier and new class of drug. Int J Immunopharmacol. 21:1–14.
1999.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Smith KJ, Hamza S and Skelton H: The
imidazoquinolines and their place in the therapy of cutaneous
disease. Expert Opin Pharmacother. 4:1105–1119. 2003.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Deleuze-Masquefa C, Gerebtzoff G, Subra G,
Fabreguettes JR, Ovens A, Carraz M, Strub MP, Bompart J, George P
and Bonnet PA: Design and synthesis of novel
imidazo[1,2-a]quinoxalines as PDE4 inhibitors. Bioorg Med Chem.
12:1129–1139. 2004.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Del Rosso JQ: Topical imiquimod therapy
for actinic keratosis: Is long-term clearance a realistic benefit?
J Clin Aesthet Dermatol. 1:44–47. 2008.PubMed/NCBI
|
|
33
|
Oumata N, Nguyen PH, Beringue V, Soubigou
F, Pang Y, Desban N, Massacrier C, Morel Y, Paturel C, Contesse MA,
et al: The toll-like receptor agonist imiquimod is active against
prions. PLoS One. 8(e72112)2013.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Sidky YA, Borden EC, Weeks CE, Reiter MJ,
Hatcher JF and Bryan GT: Inhibition of murine tumor growth by an
interferon-inducing imidazoquinolinamine. Cancer Res. 52:3528–3533.
1992.PubMed/NCBI
|
|
35
|
Sauder DN, Skinner RB, Fox TL and Owens
ML: Topical imiquimod 5% cream as an effective treatment for
external genital and perianal warts in different patient
populations. Sex Transm Dis. 30:124–128. 2003.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Yokogawa M, Takaishi M, Nakajima K,
Kamijima R, Digiovanni J and Sano S: Imiquimod attenuates the
growth of UVB-induced SCC in mice through Th1/Th17 cells. Mol
Carcinog. 52:760–769. 2013.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Spaner DE, Miller RL, Mena J, Grossman L,
Sorrenti V and Shi Y: Regression of lymphomatous skin deposits in a
chronic lymphocytic leukemia patient treated with the toll-like
receptor-7/8 agonist, imiquimod. Leuk Lymphoma. 46:935–939.
2005.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Raman VS, Duthie MS, Fox CB, Matlashewski
G and Reed SG: Adjuvants for Leishmania vaccines: From models to
clinical application. Front Immunol. 3(144)2012.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Hamie M, Najm R, Deleuze-Masquefa C,
Bonnet PA, Dubremetz JF, El Sabban M and El Hajj H: Imiquimod
targets toxoplasmosis through modulating host toll-like
receptor-MyD88 signaling. Front Immunol. 12(629917)2021.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Arevalo I, Ward B, Miller R, Meng TC,
Najar E, Alvarez E, Matlashewski G and Llanos-Cuentas A: Successful
treatment of drug-resistant cutaneous leishmaniasis in humans by
use of imiquimod, an immunomodulator. Clin Infect Dis.
33:1847–1851. 2001.PubMed/NCBI View
Article : Google Scholar
|
|
41
|
Miranda-Verastegui C, Tulliano G, Gyorkos
TW, Calderon W, Rahme E, Ward B, Cruz M, Llanos-Cuentas A and
Matlashewski G: First-line therapy for human cutaneous
leishmaniasis in Peru using the TLR7 agonist imiquimod in
combination with pentavalent antimony. PLoS Negl Trop Dis.
3(e491)2009.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Arevalo I, Tulliano G, Quispe A, Spaeth G,
Matlashewski G, Llanos-Cuentas A and Pollack H: Role of imiquimod
and parenteral meglumine antimoniate in the initial treatment of
cutaneous leishmaniasis. Clin Infect Dis. 44:1549–1554.
2007.PubMed/NCBI View
Article : Google Scholar
|
|
43
|
Walter A, Schäfer M, Cecconi V, Matter C,
Urosevic-Maiwald M, Belloni B, Schönewolf N, Dummer R, Bloch W,
Werner S, et al: Aldara activates TLR7-independent immune defence.
Nat Commun. 4(1560)2013.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Kono T, Kondo S, Pastore S, Shivji GM,
Tomai MA, McKenzie RC and Sauder DN: Effects of a novel topical
immunomodulator, imiquimod, on keratinocyte cytokine gene
expression. Lymphokine Cytokine Res. 13:71–76. 1994.PubMed/NCBI
|
|
45
|
Weber A, Zimmermann C, Mausberg AK,
Kieseier BC, Hartung HP and Hofstetter HH: Induction of
pro-inflammatory cytokine production in thymocytes by the immune
response modifiers Imiquimod and Gardiquimod. Int Immunopharmacol.
17:427–431. 2013.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Wolf IH, Kodama K, Cerroni L and Kerl H:
Nature of inflammatory infiltrate in superficial cutaneous
malignancies during topical imiquimod treatment. Am J
Dermatopathol. 29:237–241. 2007.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Wong JG, Toole JWP, Demers AA, Musto G and
Wiseman MC: Topical 5% imiquimod in the treatment of lentigo
maligna. J Cutan Med Surg. 16:245–249. 2012.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Schon M and Schon MP: The antitumoral mode
of action of imiquimod and other imidazoquinolines. Curr Med Chem.
14:681–687. 2007.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Schon MP and Schon M: The small-molecule
immune response modifier imiquimod-its mode of action and clinical
use in the treatment of skin cancer. Expert Opin Ther Targets.
10:69–76. 2006.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Bilu D and Sauder DN: Imiquimod: Modes of
action. Br J Dermatol. 149 (Suppl 66):5–8. 2003.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Levine E.N.a.V., Role of Topical Therapy:
Imiquimod. 2017.
|
|
52
|
Wagstaff AJ and Perry CM: Topical
imiquimod: A review of its use in the management of anogenital
warts, actinic keratoses, basal cell carcinoma and other skin
lesions. Drugs. 67:2187–2210. 2007.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Megyeri K, Au WC, Rosztoczy I, Raj NB,
Miller RL, Tomai MA and Pitha PM: Stimulation of interferon and
cytokine gene expression by imiquimod and stimulation by Sendai
virus utilize similar signal transduction pathways. Mol Cell Biol.
15:2207–2218. 1995.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Sauder DN: Immunomodulatory and
pharmacologic properties of imiquimod. J Am Acad Dermatol.
43:S6–S11. 2000.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Schon MP, Schon M and Klotz KN: The small
antitumoral immune response modifier imiquimod interacts with
adenosine receptor signaling in a TLR7- and TLR8-independent
fashion. J Invest Dermatol. 126:1338–1347. 2006.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Majewski S, Marczak M, Mlynarczyk B,
Benninghoff B and Jablonska S: Imiquimod is a strong inhibitor of
tumor cell-induced angiogenesis. Int J Dermatol. 44:14–19.
2005.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Denning DP and Hirose T: Anti-tubulins
DEPendably induce apoptosis. Nat Cell Biol. 16:741–743.
2014.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Schön MP and Schön M: Immune modulation
and apoptosis induction: Two sides of the antitumoral activity of
imiquimod. Apoptosis. 9:291–298. 2004.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Bong AB, Bonnekoh B, Franke I, Schön MP,
Ulrich J and Gollnick H: Imiquimod, a topical immune response
modifier, in the treatment of cutaneous metastases of malignant
melanoma. Dermatology. 205:135–138. 2002.PubMed/NCBI View Article : Google Scholar
|
|
60
|
Heikkinen AK and Susitaival P: Severe
systemic reaction to topical imiquimod. Acta Derm Venereol.
91:594–595. 2011.PubMed/NCBI View Article : Google Scholar
|
|
61
|
Cannon PS, O'Donnell B, Huilgol SC and
Selva D: The ophthalmic side-effects of imiquimod therapy in the
management of periocular skin lesions. Br J Ophthalmol.
95:1682–1685. 2011.PubMed/NCBI View Article : Google Scholar
|
|
62
|
Benson E: Imiquimod: Potential risk of an
immunostimulant. Australas J Dermatol. 45:123–124. 2004.PubMed/NCBI View Article : Google Scholar
|
|
63
|
Somani N, Martinka M, Crawford RI, Dutz JP
and Rivers JK: Treatment of atypical nevi with imiquimod 5% cream.
Arch Dermatol. 143:379–385. 2007.PubMed/NCBI View Article : Google Scholar
|
|
64
|
Hanna E, Abadi R and Abbas O: Imiquimod in
dermatology: An overview. Int J Dermatol. 55:831–844.
2016.PubMed/NCBI View Article : Google Scholar
|
|
65
|
Rosen T: Limited extent AIDS-related
cutaneous Kaposi's sarcoma responsive to imiquimod 5% cream. Int J
Dermatol. 45:854–856. 2006.PubMed/NCBI View Article : Google Scholar
|
|
66
|
Ezzell TI, Fromowitz JS and Ramos-Caro FA:
Recurrent pyogenic granuloma treated with topical imiquimod. J Am
Acad Dermatol. 54 (5 Suppl):S244–S245. 2006.PubMed/NCBI View Article : Google Scholar
|
|
67
|
Barba AR, Kapoor S and Berman B: An open
label safety study of topical imiquimod 5% cream in the treatment
of Molluscum contagiosum in children. Dermatol Online J.
7(20)2001.PubMed/NCBI
|
|
68
|
Díaz-Guimaraens B, Saceda-Corralo D,
Hermosa-Gelbard A, Moreno-Arrones ÓM, Dominguez-Santas M,
Suarez-Valle A and Vañó-Galván S: Imiquimod-enhanced immunotherapy
with diphencyprone for patients with alopecia areata. Dermatol
Ther. 35(e15516)2022.PubMed/NCBI View Article : Google Scholar
|
|
69
|
Palefsky JM, Lee JY, Jay N, Goldstone SE,
Darragh TM, Dunlevy HA, Rosa-Cunha I, Arons A, Pugliese JC, Vena D,
et al: Treatment of anal high-grade squamous intraepithelial
lesions to prevent anal cancer. N Engl J Med. 386:2273–2282.
2022.PubMed/NCBI View Article : Google Scholar
|
|
70
|
Al Fayez N, Rouhollahi E, Ong CY, Wu J,
Nguyen A, Böttger R, Cullis PR, Witzigmann D and Li SD:
Hepatocyte-targeted delivery of imiquimod reduces hepatitis B virus
surface antigen. J Control Release. 350:630–641. 2022.PubMed/NCBI View Article : Google Scholar
|
|
71
|
Daude M, Dinulescu M, Nguyen JM, Maillard
H, Duff FL, Machet L, Beylot-Barry M, Legoupil D,
Wierzbicka-Hainaut E, Bedane C, et al: Efficacy of imiquimod in the
management of lentigo maligna. J Eur Acad Dermatol Venereol.
27(10.1111/jdv.19141)2023.PubMed/NCBI View Article : Google Scholar
|
|
72
|
Chang SH, Lin PY, Wu TK, Hsu CS, Huang SW,
Li ZY, Liu KT, Kao JK, Chen YJ, Wong TW, et al: Imiquimod-induced
ROS production causes lysosomal membrane permeabilization and
activates caspase-8-mediated apoptosis in skin cancer cells. J
Dermatol Sci. 107:142–150. 2022.PubMed/NCBI View Article : Google Scholar
|
|
73
|
Urquhart JL and Weston WL: Treatment of
multiple trichoepitheliomas with topical imiquimod and tretinoin.
Pediatr Dermatol. 22:67–70. 2005.PubMed/NCBI View Article : Google Scholar
|
|
74
|
Cantisani C, Lazic T, Richetta AG, Clerico
R, Mattozzi C and Calvieri S: Imiquimod 5% cream use in
dermatology, side effects and recent patents. Recent Pat Inflamm
Allergy Drug Discov. 6:65–69. 2012.PubMed/NCBI View Article : Google Scholar
|
|
75
|
Pasadyn SR and Cain R: Topical imiquimod
induces severe weakness and myalgias after three applications: A
case report. J Clin Aesthet Dermatol. 12:58–59. 2019.PubMed/NCBI
|
|
76
|
Safadi MG, Hassan S, Patel V, Viglione M
and Zahner SL: Imiquimod-induced hypertrophic lupus
erythematosus-like reaction. Dermatol Online J.
28(10.5070/D328458526)2022.PubMed/NCBI View Article : Google Scholar
|
|
77
|
Li HO, Aw M and Glassman SJ:
Imiquimod-induced bullous pemphigoid: A case report. SAGE Open Med
Case Rep. 11(2050313x231164222)2023.PubMed/NCBI View Article : Google Scholar
|
|
78
|
Arias NM, Bonino CB, Feal PP, Rico MLP,
Peñaranda JMS and Osorio IV: Lupus-like reaction following
imiquimod treatment for actinic keratoses. Dermatol Ther.
35(e15700)2022.PubMed/NCBI View Article : Google Scholar
|
|
79
|
Raman J, Bisbee E, Missall TA and Saikaly
SK: A case of topical imiquimod induced fatigue. J Dermatolog
Treat. 33:3202–3204. 2022.PubMed/NCBI View Article : Google Scholar
|
|
80
|
McKinzie AH and Christman MA:
Imiquimod-associated localized skin ulceration in a patient with
uncontrolled diabetes. Obstet Gynecol. 140:316–319. 2022.PubMed/NCBI View Article : Google Scholar
|
|
81
|
Martins P, Jesus J, Santos S, Raposo LR,
Roma-Rodrigues C, Baptista PV and Fernandes AR: Heterocyclic
anticancer compounds: Recent advances and the paradigm shift
towards the use of nanomedicine's tool box. Molecules.
20:16852–16891. 2015.PubMed/NCBI View Article : Google Scholar
|
|
82
|
Kumar S, Bawa S and Gupta H: Biological
activities of quinoline derivatives. Mini Rev Med Chem.
9:1648–1654. 2009.PubMed/NCBI View Article : Google Scholar
|
|
83
|
Chu XM, Wang C, Liu W, Liang LL, Gong KK,
Zhao CY and Sun KL: Quinoline and quinolone dimers and their
biological activities: An overview. Eur J Med Chem. 161:101–117.
2019.PubMed/NCBI View Article : Google Scholar
|
|
84
|
Balderas-Renteria I, Gonzalez-Barranco P,
Garcia A, Banik BK and Rivera G: Anticancer drug design using
scaffolds of β-lactams, sulfonamides, quinoline, quinoxaline and
natural products. Drugs advances in clinical trials. Curr Med Chem.
19:4377–4398. 2012.PubMed/NCBI View Article : Google Scholar
|
|
85
|
Afzal O, Kumar S, Haider MR, Ali MR, Kumar
R, Jaggi M and Bawa S: A review on anticancer potential of
bioactive heterocycle quinoline. Eur J Med Chem. 97:871–910.
2015.PubMed/NCBI View Article : Google Scholar
|
|
86
|
Bonilla-Ramirez L, Rios A, Quiliano M,
Ramirez-Calderon G, Beltrán-Hortelano I, Franetich JF, Corcuera L,
Bordessoulles M, Vettorazzi A, de Cerain AL, et al: Novel
antimalarial chloroquine- and primaquine-quinoxaline 1,4-di-N-oxide
hybrids: Design, synthesis, Plasmodium life cycle stage profile,
and preliminary toxicity studies. Eur J Med Chem. 158:68–81.
2018.PubMed/NCBI View Article : Google Scholar
|
|
87
|
Burguete A, Pontiki E, Hadjipavlou-Litina
D, Ancizu S, Villar R, Solano B, Moreno E, Torres E, Pérez S,
Aldana I and Monge A: Synthesis and biological evaluation of new
quinoxaline derivatives as antioxidant and anti-inflammatory
agents. Chem Biol Drug Des. 77:255–267. 2011.PubMed/NCBI View Article : Google Scholar
|
|
88
|
Fabian L, Porro MT, Gómez N, Salvatori M,
Turk G, Estrin D and Moglioni A: Design, synthesis and biological
evaluation of quinoxaline compounds as anti-HIV agents targeting
reverse transcriptase enzyme. Eur J Med Chem.
188(111987)2020.PubMed/NCBI View Article : Google Scholar
|
|
89
|
El Newahie AMS, Nissan YM, Ismail NSM, El
Ella DA, Khojah SM and Abouzid KAM: Design and synthesis of new
quinoxaline derivatives as anticancer agents and apoptotic
inducers. Molecules. 24(1175)2019.PubMed/NCBI View Article : Google Scholar
|
|
90
|
Patinote C, Deleuze-Masquéfa C, Kaddour
KH, Vincent LA, Larive R, Zghaib Z, Guichou JF, Assaf MD, Cuq P and
Bonnet PA: Imidazo[1,2-a]quinoxalines for melanoma treatment with
original mechanism of action. Eur J Med Chem.
212(113031)2021.PubMed/NCBI View Article : Google Scholar
|
|
91
|
Lafaille F, Banaigs B, Inguimbert N,
Enjalbal C, Doulain PE, Bonnet PA, Masquefa C and Bressolle FMM:
Characterization of a new anticancer agent, EAPB0203, and its main
metabolites: nuclear magnetic resonance and liquid
chromatography-mass spectrometry studies. Anal Chem. 84:9865–9872.
2012.PubMed/NCBI View Article : Google Scholar
|
|
92
|
Khier S, Deleuze-Masquéfa C, Moarbess G,
Gattacceca F, Margout D, Solassol I, Cooper JF, Pinguet F, Bonnet
PA and Bressolle FMM: Pharmacology of EAPB0203, a novel
imidazo[1,2-a]quinoxaline derivative with anti-tumoral activity on
melanoma. Eur J Pharm Sci. 39:23–29. 2010.PubMed/NCBI View Article : Google Scholar
|
|
93
|
Morjaria S, Deleuze-Masquefa C, Lafont V,
Gayraud S, Bompart J, Bonnet PA and Dornand J: Impairment of
TNF-alpha production and action by imidazo[1,2- alpha]
quinoxalines, a derivative family which displays potential
anti-inflammatory properties. Int J Immunopathol Pharmacol.
19:525–538. 2006.PubMed/NCBI View Article : Google Scholar
|
|
94
|
Lideikaitė A, Mozūraitienė J and
Letautienė S: Analysis of prognostic factors for melanoma patients.
Acta Med Litu. 24:25–34. 2017.PubMed/NCBI View Article : Google Scholar
|
|
95
|
Drobits B, Holcmann M, Amberg N, Swiecki
M, Grundtner R, Hammer M, Colonna M and Sibilia M: Imiquimod clears
tumors in mice independent of adaptive immunity by converting pDCs
into tumor-killing effector cells. J Clin Invest. 122:575–585.
2012.PubMed/NCBI View Article : Google Scholar
|
|
96
|
Chouchou A, Patinote C, Cuq P, Bonnet PA
and Deleuze-Masquéfa C: Imidazo[1,2-a]quinoxalines derivatives
grafted with amino acids: Synthesis and evaluation on A375 melanoma
cells. Molecules. 23(2987)2018.PubMed/NCBI View Article : Google Scholar
|
|
97
|
Quereux G and Dreno B: Fotemustine for the
treatment of melanoma. Expert Opin Pharmacother. 12:2891–2904.
2011.PubMed/NCBI View Article : Google Scholar
|
|
98
|
Hermine O, Ramos JC and Tobinai K: A
review of new findings in adult T-cell leukemia-lymphoma: A focus
on current and emerging treatment strategies. Adv Ther. 35:135–152.
2018.PubMed/NCBI View Article : Google Scholar
|
|
99
|
Tsukasaki K, Hermine O, Bazarbachi A,
Ratner L, Ramos JC, Harrington W Jr, O'Mahony D, Janik JE,
Bittencourt AL, Taylor GP, et al: Definition, prognostic factors,
treatment, and response criteria of adult T-cell leukemia-lymphoma:
A proposal from an international consensus meeting. J Clin Oncol.
27:453–459. 2009.PubMed/NCBI View Article : Google Scholar
|
|
100
|
Bazarbachi A, Suarez F, Fields P and
Hermine O: How I treat adult T-cell leukemia/lymphoma. Blood.
118:1736–1745. 2011.PubMed/NCBI View Article : Google Scholar
|
|
101
|
Cook LB, Fuji S, Hermine O, Bazarbachi A,
Ramos JC, Ratner L, Horwitz S, Fields P, Tanase A, Bumbea H, et al:
Revised adult T-cell leukemia-lymphoma international consensus
meeting report. J Clin Oncol. 37:677–687. 2019.PubMed/NCBI View Article : Google Scholar
|
|
102
|
Tsukasaki K, Marçais A, Nasr R, Kato K,
Fukuda T, Hermine O and Bazarbachi A: Diagnostic approaches and
established treatments for adult T cell leukemia lymphoma. Front
Microbiol. 11(1207)2020.PubMed/NCBI View Article : Google Scholar
|
|
103
|
El Hajj H, Tsukasaki K, Cheminant M,
Bazarbachi A, Watanabe T and Hermine O: Novel treatments of adult T
cell leukemia lymphoma. Front Microbiol. 11(1062)2020.PubMed/NCBI View Article : Google Scholar
|
|
104
|
Hehlmann R, Heimpel H, Hasford J, Kolb HJ,
Pralle H, Hossfeld DK, Queisser W, Löffler H, Hochhaus A and Heinze
B: Randomized comparison of interferon-alpha with busulfan and
hydroxyurea in chronic myelogenous leukemia. The german CML study
group. Blood. 84:4064–4077. 1994.PubMed/NCBI
|
|
105
|
Bisen A and Claxton DF: Tyrosine kinase
targeted treatment of chronic myelogenous leukemia and other
myeloproliferative neoplasms. Adv Exp Med Biol. 779:179–196.
2013.PubMed/NCBI View Article : Google Scholar
|
|
106
|
Krause DS and Van Etten RA: Bedside to
bench: Interfering with leukemic stem cells. Nat Med. 14:494–495.
2008.PubMed/NCBI View Article : Google Scholar
|
|
107
|
Okimoto RA and Van Etten RA: Navigating
the road toward optimal initial therapy for chronic myeloid
leukemia. Curr Opin Hematol. 18:89–97. 2011.PubMed/NCBI View Article : Google Scholar
|
|
108
|
Lagunas-Rangel FA, Chávez-Valencia V,
Gómez-Guijosa MA and Cortes-Penagos C: Acute myeloid
leukemia-genetic alterations and their clinical prognosis. Int J
Hematol Oncol Stem Cell Res. 11:328–339. 2017.PubMed/NCBI
|
|
109
|
Yilmaz M, Kantarjian H and Ravandi F:
Acute promyelocytic leukemia current treatment algorithms. Blood
Cancer J. 11(123)2021.PubMed/NCBI View Article : Google Scholar
|
|
110
|
Borthakur G and Kantarjian H: Core binding
factor acute myelogenous leukemia-2021 treatment algorithm. Blood
Cancer J. 11(114)2021.PubMed/NCBI View Article : Google Scholar
|
|
111
|
Molica M, Breccia M, Foa R, Jabbour E and
Kadia TM: Maintenance therapy in AML: The past, the present and the
future. Am J Hematol. 94:1254–1265. 2019.PubMed/NCBI View Article : Google Scholar
|
|
112
|
Kassim AA and Savani BN: Hematopoietic
stem cell transplantation for acute myeloid leukemia: A review.
Hematol Oncol Stem Cell Ther. 10:245–251. 2017.PubMed/NCBI View Article : Google Scholar
|
|
113
|
Lin WY, Fordham SE, Hungate E, Sunter NJ,
Elstob C, Xu Y, Park C, Quante A, Strauch K, Gieger C, et al:
Genome-wide association study identifies susceptibility loci for
acute myeloid leukemia. MedRxiv.
2021(2021.07.22.21259893)2021.PubMed/NCBI View Article : Google Scholar
|
|
114
|
Falini B, Brunetti L, Sportoletti P and
Martelli MP: NPM1-mutated acute myeloid leukemia: from bench to
bedside. Blood. 136:1707–1721. 2020.PubMed/NCBI View Article : Google Scholar
|
|
115
|
Wang AJ, Han Y, Jia N, Chen P and Minden
MD: NPM1c impedes CTCF functions through cytoplasmic
mislocalization in acute myeloid leukemia. Leukemia. 34:1278–1290.
2020.PubMed/NCBI View Article : Google Scholar
|
|
116
|
Skayneh H, Jishi B, Hleihel R, Hamie M, El
Hajj R, Deleuze-Masquefa C, Bonnet PA, El Sabban M and El Hajj H:
EAPB0503, an imidazoquinoxaline derivative modulates SENP3/ARF
mediated SUMOylation, and induces NPM1c degradation in NPM1 mutant
AML. Int J Mol Sci. 23(3421)2022.PubMed/NCBI View Article : Google Scholar
|
|
117
|
Sacks D and Noben-Trauth N: The immunology
of susceptibility and resistance to Leishmania major in mice. Nat
Rev Immunol. 2:845–858. 2002.PubMed/NCBI View
Article : Google Scholar
|
|
118
|
Ley SV and Thomas AW: Modern synthetic
methods for copper-mediated C(aryl)(bond)O, C(aryl)[bond]N, and
C(aryl)[bond]S bond formation. Angew Chem Int Ed Engl.
42:5400–5449. 2003.PubMed/NCBI View Article : Google Scholar
|