Introduction
Mucinous tubular and spindle cell carcinoma (MTSCC)
is a rare variant of renal cell carcinoma (1). This form of renal cell carcinoma
(RCC) is predominately observed in adults and is generally
considered an indolent variant with a better prognosis relative to
the other forms of RCC (2-4).
The tumor has a very specific histological finding consisting of
tubular and spindle cells within a mucinous stroma as a background
(2). A method which can be used to
differentiate MTSCC from other forms of RCC, such as clear cell and
papillary RCC, is to perform magnetic resonance imaging (MRI),
since MTSCC tends to grow more avidly, while also exhibiting
gradual progressive enhancement (5). The amount of spindle and tubular
cells can vary; however, they always tend to exhibit a low nuclear
grade (3). Since MTSCC was
classified as its own specific identity by the World Health
Organization (WHO) in 2004, <100 cases have been reported in the
literature, rendering this an extremely rare disease (1,6). The
present study reports a rare case of MTSCC in the right kidney.
Case report
A 69-year-old male presented to the Urology Clinic
at Smart Health Tower (Sulaimani, Iraq) with a 3-month history of
abdominal and back pain. He also complained of frequent urination,
although he was without fever, and did not exhibit rigor or
vomiting. He was also a known case of hypertension, for which he
was administered 10 mg amlodipine tablets (calcium channel blocker)
twice daily. The patient had a history of a prior cortical lesion
in the right kidney 3 years prior to his presentation, which was
suspicious of RCC on imaging, for which a partial nephrectomy was
performed; the subsequent histopathological examination indicated a
simple fibrotic renal cyst. Upon examination, the patient was found
to have right-sided loin pain with tenderness, although there was
no sign of a palpable mass. A complete blood count showed a normal
level of white blood cells (4.8/µl), red blood cells (98 mg/dl), a
hemoglobin level of 12.5 g/dl and a mean corpuscle volume of 88 fl
(indicating normocytic anemia) with a mild decrease in the platelet
count (142/µl). Further blood analyses revealed negative viral
markers (HBsAg and hepatitis C virus), a urea level of 31 mg/dl and
a creatinine level of 1.02 mg/dl. Prothrombin time, partial
thromboplastin time, international normalized ratio and all the
liver function tests yielded results which were within the normal
range.
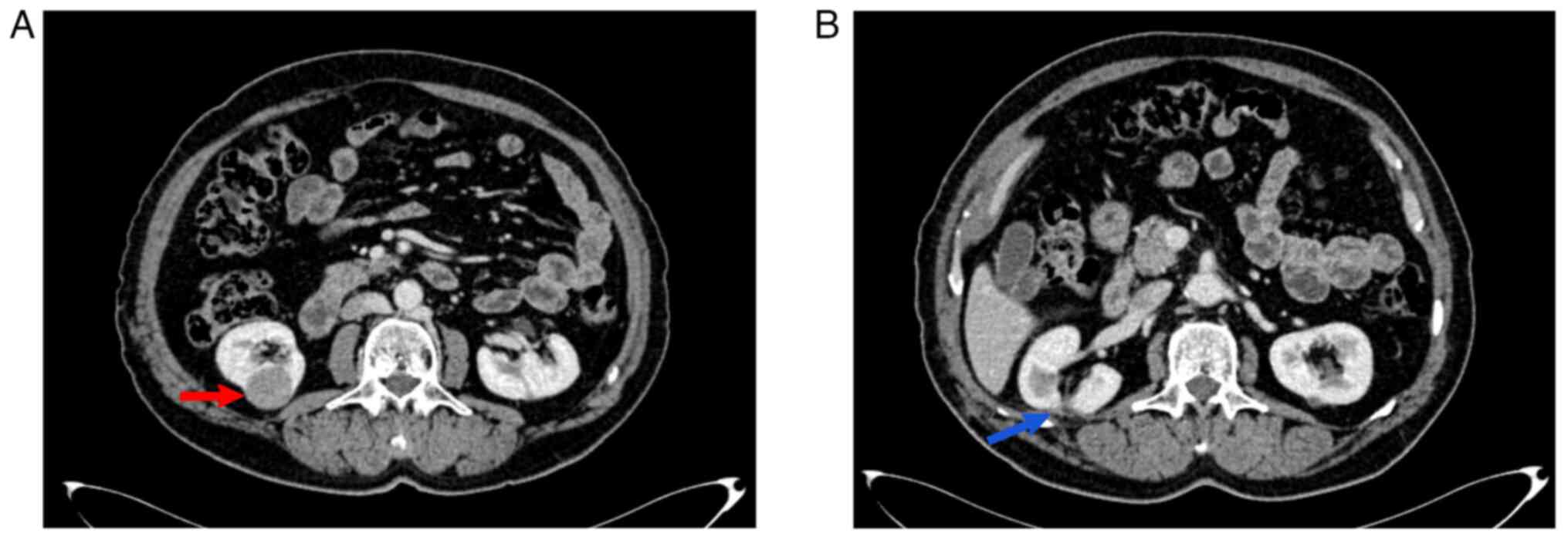
An abdominal ultrasound showcased a well-defined
hypoechoic lesion, which measured 23x26 mm, found on the lateral
aspect of the right kidney. A computed tomography (CT) scan of the
chest, abdomen and pelvis with contrast material revealed evidence
of a well-defined exophytic mass (3x3 cm) within the lower pole of
the right kidney (it was stage T1a on the CT scan) (Fig. 1). The mass exhibited minimal
enhancement at the arterial phase with more enhancement in the
venous phase (equivocal enhancement) and no renal vascular
invasion; the overall picture was suggestive of RCC. Under general
anesthesia, the patient underwent a right partial nephrectomy, with
the patient lying in the left lateral position, a right subcostal
incision was made, and the kidney was found to be severely adhered
to the surrounding peritoneum. All adhesions were released by the
surgeon. Despite the CT scan indicating the mass in the lower pole,
the mass was found to be located in the mid-pole of the right
kidney intraoperatively. Bleeding was encountered due to a small
parenchymal tear which was controlled and sutured. The renal
pedicle was identified and bulldog forceps were placed. Following
the partial nephrectomy of the mid-pole mass in the right kidney,
positive margins were indicated in the intraoperative frozen
section. This led the surgeon to further excise extra tissue from
the base of the tumor in order for it to be sent for a
histopathological evaluation. The warm ischemic time was measured
and recorded as 12 min. Following excision, hemostasis was secured,
a corrugate drain was placed and the wound was closed in layers.
The resected mass had a gross appearance of a smooth capsular
surface with a solid glistening grey color and few foci of
necrosis. The mass had <1 cm of renal parenchyma on both of its
lateral sides, although no parenchymal tissue was found centrally.
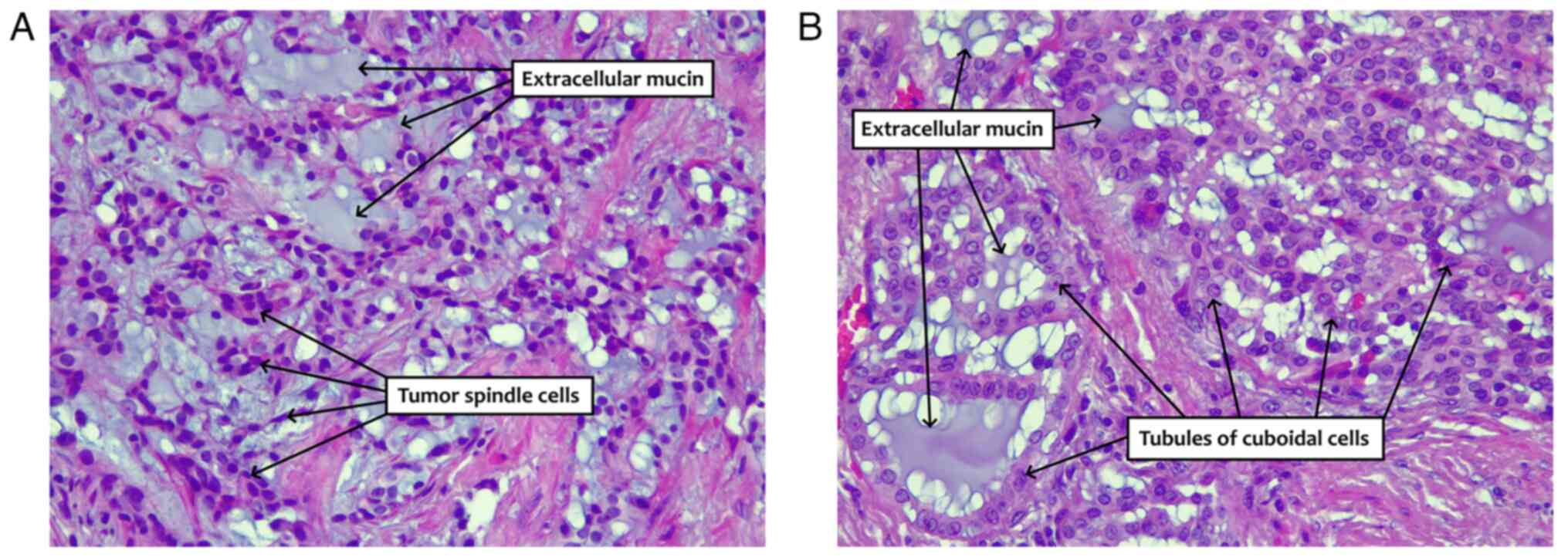
The histopathological examination was performed at Anwar Shekha
Medical City; the specimen was formalin-fixed and
paraffin-embedded. The sections were cut using a microtome to a
thickness of 4 µm and stained with conventional hematoxylin and
eosin stain (MilliporeSigma). The procedure was performed at room
temperature for 65 min using a Tissue-Tek Prisma Plus Automated
slide stainer (Sakura Finetek Europe B.V.). The microscope used for
examination was an Olympus BX-51 microscope with a camera adaptor
(Olympus U-TV0.5XC-3) (Olympus Corporation) for obtaining images.
The histopathological examination revealed the renal mass
containing long tubules and a cord-like growth pattern of uniform,
bland, and low cuboidal cells in an eosinophilic, focally
vacuolated cytoplasm (Fig. 2). The
stroma had myxoid foci and a bubbly appearance with extracellular
mucin. A confirmed diagnosis of MTSCC was made with a pathological
staging of T1aNxMx. The post-operative interval transpired without
noteworthy incidents. Subsequently, a CT scan of the thoracic,
abdominal and pelvic regions was conducted at 3 months
post-operatively, indicating the absence of both recurrence and
distant metastasis.
Discussion
MTSCC, is a rare subtype of RCC, comprising 1-4% of
all RCCs (6-8).
This rare subtype was initially described by Lopez-Beltran et
al (6). The lesion
predominantly affects females with a 2-4:1 female-to-male ratio and
has an average age at onset of 53 years. Despite its rarity, the
youngest reported case was in a 13-year-old boy with rapid disease
progression and eventual fatality due to metastasis (2).
MTSCC is often asymptomatic, discovered incidentally
during imaging for unrelated issues (2). However, it may present with
non-specific symptoms, such as abdominal and back pain, as observed
in the patient described in the present study. In numerous
instances, the identification of MTSCC can be suggested by
analyzing a combination of CT/MRI features. Notably, the presence
of slow enhancement with a plateau in dynamic contrast-enhanced
CT/MRI, coupled with intermediate to high T2 signal intensity that
contrasts with low apparent diffusion coefficient values on MRI, is
indicative of this specific diagnosis (9). The patient described herein exhibited
a 3x3 cm solid mass in the lower pole of the right kidney,
demonstrating more venous phase enhancement compared to the minimal
arterial phase enhancement.
Diagnosing MTSCC can be complex due to its
histological similarity to papillary RCC. An immunohistochemical
evaluation, specifically negative staining for markers, such as
CD10, can help differentiate MTSCC from papillary RCC (5). Other differential diagnoses of MTSCC
include sarcomatoid RCC, mesenchymal tumors such as leiomyoma,
angiomyolipoma, inflammatory fibroblastic tumors and
juxtaglomerular cell tumors, which can be distinguished from MTSCC
by benefiting from their distinctive histological,
Immunohistochemical and molecular features (10). MTSCC generally has a mucinous
stroma and is composed of tubular and spindle cells (11). The tumor in the case presented
herein also displayed focal clusters of foamy macrophages, ~20%
necrosis and no rhabdoid differentiation, thus aiding in the
diagnosis. A gross examination usually reveals an encapsulated,
well-circumscribed tumor, which was consistent with the case in the
present study.
Although MTSCC was initially defined as a low-grade
neoplasm with a good prognosis by the WHO in 2004(6), its classification was revised in 2016
to omit the term ‘indolent course’ (12). The majority of cases have a benign
course; however, there are instances where the disease can be
aggressive, particularly when sarcomatoid changes are observed
(13). In such cases, the survival
rate may be <1 year, necessitating close follow-up following
surgical intervention (1,14). In the study conducted by Ged et
al (15) involving 25
patients, those displaying low-grade histological features
typically had localized tumors, and only 1 out of 20 of those
individuals developed recurrent metastatic disease. In contrast,
among the 5 patients who had underlying high-grade histological
features, all either developed or presented with metastatic
disease. The overall survival rate at 3 years following diagnosis
was found to be 84.8%. Notably, all the deaths were attributed to
metastatic disease (15).
The absence of a standardized treatment for MTSCC,
owing to its rarity, presents a significant clinical challenge.
Surgery, specifically partial nephrectomy, remains the primary
treatment option (16). For
metastatic disease, targeted therapies, such as the use of tyrosine
kinase inhibitors (such as sunitinib) have shown promise (17), while immunotherapies, such as
ipilimumab and nivolumab have resulted in complete remission in
some cases (18).
In conclusion, the case presented herein underscores
the importance of including MTSCC in the differential diagnoses for
RCC. Partial nephrectomy and tumor excision may have a good
outcome.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
RHA and SMA were major contributors to the
conception of the study. FHK designed the study and was involved in
the literature search. ASA and BAA obtained medical images,
participated in reviewing the literature, and preparing and
drafting the manuscript. RMA, AMA, AAA, JIH and LRAP critically
revised the manuscript, and were involved in analyzing the data and
advising on patient treatment. FHK and RHA confirm the authenticity
of all the raw data. All authors contributed equally to the
manuscript and have read and approved the final version of the
manuscript.
Ethics approval and consent to
participate
Written informed consent was obtained from the
patient for his participation in the present study.
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of the present case report and any
accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Kobari Y, Yoshida K, Minoda R, Fukuda H,
Hata K, Unagami K, Iizuka J, Ishida H, Nagashima Y and Takagi T:
Long-time survival of a renal transplant recipient with metastatic
mucinous tubular and spindle cell carcinoma: A case report. In
Vivo. 37:1394–1398. 2023.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Sharma K, Dhua A, Agarwala S and Kaushal
S: Mucinous tubular and spindle cell renal cell carcinoma
(MTSC-RCC) with an unusual presentation in a child. J Kidney Cancer
VHL. 9(6)2022.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Rahoui M, Boulma R and Khouni H: Renal
mucinous tubular and spindle cell carcinoma: A case report. Urol
Case Reports. 40(101889)2022.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Mahmood ZH, Mohemed FM, Fatih BN, Qadir AA
and Abdalla SH: Cancer publications in one year (2022); a
cross-sectional study': BMJ 1, 2023.
|
|
5
|
Takahashi H, Vikram R, Jimenez RE, Bolan
CW, Kawashima A, Karam JA and Takahashi N: MR characteristics of
mucinous tubular and spindle cell carcinoma (MTSCC) of the kidney:
Comparison with clear cell and papillary subtypes of renal cell
carcinoma. Abdom Radiol (NY). 46:5250–5259. 2021.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Lopez-Beltran A, Scarpelli M, Montironi R
and Kirkali Z: 2004 WHO classification of the renal tumors of the
adults. Eur Urol. 49:798–805. 2006.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Srigley JR, Delahunt B, Eble JN, Egevad L,
Epstein JI, Grignon D, Hes O, Moch H, Montironi R, Tickoo SK, et
al: The international society of urological pathology (ISUP)
vancouver classification of renal neoplasia. Am J Surg Pathol.
37:1469–1489. 2013.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Shen SS, Ro JY, Tamboli P, Truong LD, Zhai
Q, Jung SJ, Tibbs RG, Ordonez NG and Ayala AG: Mucinous tubular and
spindle cell carcinoma of kidney is probably a variant of papillary
renal cell carcinoma with spindle cell features. Ann Diagn Pathol.
13:39–46. 2009.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Cornelis F, Ambrosetti D, Rocher L, Derchi
LE, Renard B, Puech P, Claudon M, Rouvière O, Ferlicot S, Roy C, et
al: CT and MR imaging features of mucinous tubular and spindle cell
carcinoma of the kidneys. A multi-institutional review. Eur radiol.
27:1087–1095. 2017.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Nathany S and Monappa V: Mucinous tubular
and spindle cell carcinoma: A review of histopathology and clinical
and prognostic implications. Arch Pathol Lab Med. 144:115–118.
2020.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Pérez-González S, Del Rosario-Rodríguez V,
Feltes-Ochoa JA, Gimeno-Aranguez M, Alcojor-Ballesteros I and
Carrero-López VM: Mucinous tubular and spindle cell renal cell
carcinoma: Two novel cases and a literature review. Arch Esp Urol.
75:19–26. 2022.PubMed/NCBI(In Spanish).
|
|
12
|
Moch H, Cubilla AL, Humphrey PA, Reuter VE
and Ulbright TM: The 2016 WHO classification of tumours of the
urinary system and male genital organs-part A: renal, penile, and
testicular tumours. Eur Urol. 70:93–105. 2016.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Hatayama T, Sekino Y, Shikuma H, Mukai S,
Muto M, Miyamoto S, Sadahide K, Fukuoka K, Fuji S, Goto K, et al:
Case of renal mucinous tubular and spindle cell carcinoma with high
nuclear grade. IJU Case Rep. 2(193)2019.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Fukuta K, Nakanishi R, Moriyama T, Izaki
H, Kakimoto T, Oya T, Fukawa T, Yamaguchi K, Yamamoto Y, Takahashi
M, et al: High-grade renal mucinous tubular and spindle cell
carcinoma. Case Rep Oncol. 15:580–585. 2022.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Ged Y, Chen YB, Knezevic A, Donoghue MTA,
Carlo MI, Lee CH, Feldman DR, Patil S, Hakimi AA, Russo P, et al:
Mucinous tubular and spindle-cell carcinoma of the kidney: Clinical
features, genomic profiles, and treatment outcomes. Clin Genitourin
Cancer. 17:268–274. 2019.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Dincer E, Ipek OM, Kayipmaz SS and Akca O:
Solid renal mass in a transplanted allograft kidney: Mucinous
tubular and spindle cell renal cell carcinoma. J Coll Physicians
Surg Pak. 32:S192–S194. 2022.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Larkin J, Fisher R, Pickering L, Thway K,
Livni N, Fisher C and Gore M: Metastatic mucinous tubular and
spindle cell carcinoma of the kidney responding to sunitinib. J
Clin Oncol. 28:e539–e540. 2010.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Fuchizawa H, Kijima T, Takada-Owada A,
Nagashima Y, Okazaki A, Yokoyama M, Nishihara D, Ishida K and Kamai
T: Metastatic mucinous tubular and spindle cell carcinoma of the
kidney responding to nivolumab plus ipilimumab. IJU Case Rep.
4:333–337. 2021.PubMed/NCBI View Article : Google Scholar
|