|
1
|
Rist CL, Arriola CS and Rubin C:
Prioritizing zoonoses: A proposed one health tool for collaborative
decision-making. PLoS One. 9(e109986)2014.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Tiwari R, Kumar H, Dutt T, Singh BP,
Pachaiyappan K and Dhama K: Future challenges of food security and
sustainable livestock production in India in the changing climatic
scenario. Asian J Anim Vet Adv. 9:367–384. 2014.
|
|
3
|
Lindahl JF and Grace D: The consequences
of human actions on risks for infectious diseases: A review. Infect
Ecol Epidemiol. 5(30048)2015.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Tomley FM and Shirley MW: Livestock
infectious diseases and zoonoses. Philos Trans R Soc B Biol Sci.
364:2637–2642. 2009.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Esposito MM, Turku S, Lehrfield L and
Shoman A: The impact of human activities on zoonotic infection
transmissions. Animals (Basel). 13(1646)2023.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Sm E, Altilmisani NM, Albishri F, Gad HA,
Al-Dubai TA and Al-Wesabi EO: Overview of quality control and
safety in public health pest laboratory in Jeddah, Saudi Arabia.
Int J Agric Biosci. 13:92–100. 2024.
|
|
7
|
Dhama K, Dhama K, Chakraborty S, Tiwari R,
Kumar A, Rahal A, Latheef SK, Wani MY and Kapoor S: Avian/Bird flu
virus: Poultry pathogen having zoonotic and pandemic threats: A
review. J Med Sci. 13:301–315. 2013.
|
|
8
|
Han BA, Kramer AM and Drake JM: Global
patterns of zoonotic disease in mammals. Trends Parasitol.
32:565–577. 2016.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Sayed E, Altilmisani NM, Albishri F, Ahmed
A, Elkhalifa SM, Al-Dubai TA and Al-Wesabi EO: Prevalence and
zoonotic potential of parasites in wild rats in Jeddah City, Saudi
Arabia. Int J Vet Sci. 13:232–240. 2024.
|
|
10
|
Morwal S and Sharma SK: Bacterial
zoonosis-A public health importance. J Dairy Vet Anim Res. 5:56–59.
2017.
|
|
11
|
Tounta DD, Nastos PT and Tesseromatis C:
Human activities and zoonotic epidemics: A two-way relationship.
The case of the COVID-19 pandemic. Glob Sustain. 5(e19)2022.
|
|
12
|
Tazerji SS, Nardini R, Safdar M, Shehata
AA and Duarte PM: An overview of anthropogenic actions as drivers
for emerging and re-emerging zoonotic diseases. Pathogens.
11(1376)2022.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Subedi D, Farhan MHRF, Niraula A, Shrestha
P, Chandran D, Acharya KP and Ahmad M: Avian influenza in low and
middle-income countries (LMICs): Outbreaks, vaccination challenges
and economic impact. Pak Vet J. 44:9–17. 2024.
|
|
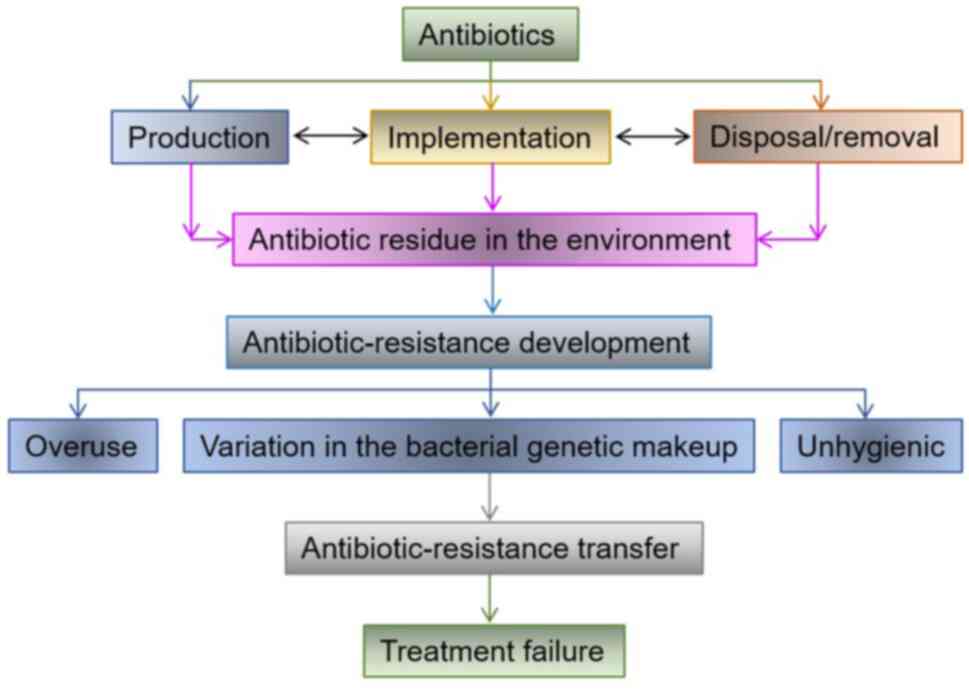
14
|
Mujahid U, Ahmad M, Mujahid A, Narayan E,
Rehman SU, Iqbal HMN and Ahmed I: Recent outbreak of Marburg virus;
a global health concern and future perspective. Eur J Clin
Microbiol Infect Dis. 43:209–211. 2024.PubMed/NCBI View Article : Google Scholar
|
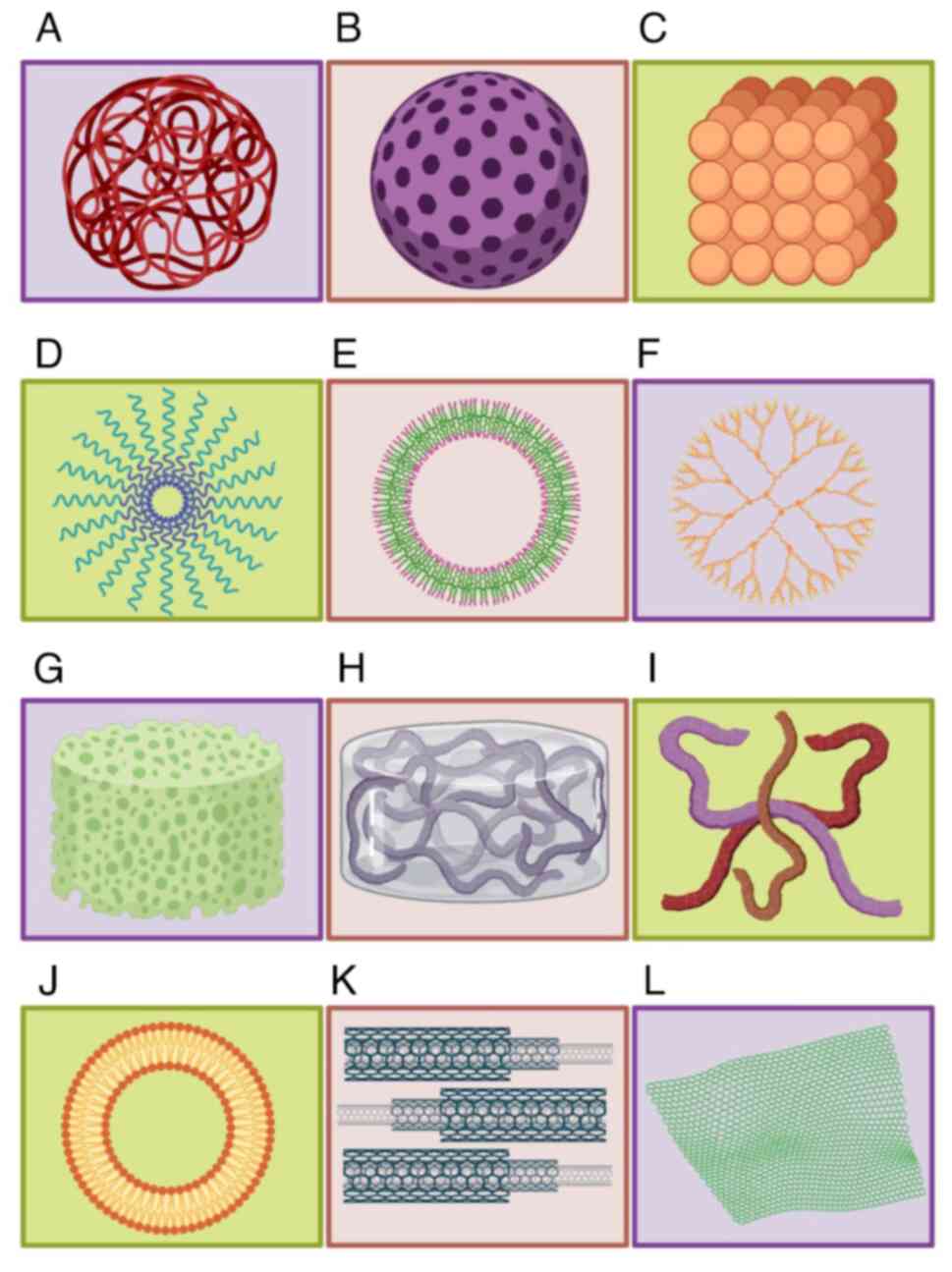
|
15
|
Ahmad M, Ahmed I, Satapathy P, Asumah MN
and Padhi BK: Re-emergence of the Lassa virus in Africa: A global
health concern. Int J Surg. 109:1044–1045. 2023.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Hing S, Narayan EJ, Thompson RCA and
Godfrey SS: The relationship between physiological stress and
wildlife disease: Consequences for health and conservation. Wildl
Res. 43:51–60. 2016.
|
|
17
|
Alotaibi BA, Muddassir M, Alotaibi MR,
Azeem MI and Alsanhani A: Assessing university students knowledge
and awareness about COVID-19 infection symptoms and preventive
measures in, Saudi Arabia. Int J Agric Biosci. 12:208–215.
2023.
|
|
18
|
Okamatsu M, Hiono T, Kida H and Sakoda Y:
Recent developments in the diagnosis of avian influenza. Vet J.
215:82–86. 2016.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Islam MT, Roy S, Talukdar H, Shammi SA and
Ahmed S: Sero-prevalence and associated risk factors of avian
influenza virus infection in backyard chicken at Sylhet region,
Bangladesh. Int J Vet Sci. 13:362–368. 2024.
|
|
20
|
Stone H, Jindal M, Lim S, Dawson R,
Quigley A, Scotch M and MacIntyre CR: Potential pathways of spread
of highly pathogenic avian influenza A/H5N1 clade 2.3.4.4b across
dairy farms in the United States medRxiv: 2024.05.02.24306785,
2024.
|
|
21
|
Ahmed A, Saqlain S, Rasool A, Muhammad S
and Umar S: Avian influenza virus (H5N1) was not detected among
dairy cattle and farm workers in Pakistan. Influenza Other Respi
Viruses. 18(e13317)2024.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Hu X, Saxena A, Magstadt DR, Gauger PC,
Burrough E, Zhang J, Siepker C, Mainenti M, Gorden PJ, Plummer P
and Li G: Highly pathogenic avian influenza A (H5N1) clade 2.3.4.4b
virus detected in dairy cattle bioRxiv: 2024.04.16.588916,
2024.
|
|
23
|
Briand FX, Souchaud F, Pierre I, Beven V,
Hirchaud E, Hérault F, Planel R, Rigaudeau A, Bernard-Stoecklin S,
Van der Werf S, et al: Highly pathogenic avian influenza A(H5N1)
clade 2.3.4.4b virus in domestic cat, France, 2022. Emerg Infect
Dis. 29:1696–1698. 2023.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Uyeki TM, Milton S, Hamid CA, Webb CR,
Presley SM, Shetty V, Rollo SN, Martinez DL, Rai S, Gonzales ER, et
al: Highly pathogenic avian influenza A(H5N1) virus infection in a
dairy farm worker. N Engl J Med. 390:2028–2029. 2024.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Putri DD, Handharyani E, Soejoedono RD,
Setiyono A and Etriwati : Newcastle disease polyclonal
antibodies as candidate reagents in immunohistochemistry diagnostic
test and passive immunization. Int J Vet Sci. 13:259–265. 2024.
|
|
26
|
Reynolds DL, Simpson EB and Hille MM:
Evidence for antibody dependent enhancement for an avian
coronavirus. Int J Vet Sci. 13:707–711. 2024.
|
|
27
|
Chomel BB, Belotto A and Meslin FX:
Wildlife, exotic pets, and emerging zoonoses. Emerg Infect Dis.
13:6–11. 2007.PubMed/NCBI View Article : Google Scholar
|
|
28
|
World Zoonoses Day: Most emerging
infectious diseases originate in animals. Source Texas Vet Med
Assoc, 2018.
|
|
29
|
Dhama K, Chakraborty S, Tiwari R, Verma
AK, Saminathan M, Amarpal Malik YS, Nikousefat Z, Javdani M and
Khan RU: A concept paper on novel technologies boosting production
and safeguarding health of humans and animals. Res Opin Anim Vet
Sci. 4:353–370. 2014.
|
|
30
|
Christaki E: New technologies in
predicting, preventing and controlling emerging infectious
diseases. Virulence. 6:558–565. 2015.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Rukambile E, Sintchenko V, Muscatello G,
Kock R and Alders R: Infection, colonization and shedding of
Campylobacter and Salmonella in animals and their contribution to
human disease: A review. Zoonoses Public Health. 66:562–578.
2019.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Williamson ED: Vaccines for emerging
pathogens: From research to the clinic. Clin Exp Immunol.
196:155–156. 2019.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Feng Z, Hag M El, Wang N, Qin T, Chen S
and Peng D: Negative regulation of RpoS-mediated STM1703 in biofilm
formation of salmonella pullorum. Pak Vet J. 43:25–32. 2023.
|
|
34
|
Nations United: World population
prospects. United Nations, 2017.
|
|
35
|
Delgado C, Rosegrant M, Steinfeld H, Ehui
S and Courbois C: Livestock to 2020: The next food revolution.
Outlook Agric. 30:27–29. 2001.
|
|
36
|
Jones PG and Thornton PK: Croppers to
livestock keepers: Livelihood transitions to 2050 in Africa due to
climate change. Environ Sci Policy. 12:427–437. 2009.
|
|
37
|
Mottet A, Teillard F, Boettcher P, Besi GD
and Besbes B: Review: Domestic herbivores and food security:
Current contribution, trends and challenges for a sustainable
development. Animal. 12:S188–S198. 2018.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Bengis RG, Kock RA and Fischer J:
Infectious animal diseases: The wildlife/livestock interface. Rev
Sci Tech. 21:53–65. 2002.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Miller RS, Farnsworth ML and Malmberg JL:
Diseases at the livestock-wildlife interface: Status, challenges,
and opportunities in the United States. Prev Vet Med. 110:119–132.
2013.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Wobeser GA: Essentials of Disease in Wild
Animals. Wiley-Blackwell, Hoboken, NJ, 2013.
|
|
41
|
Wiethoelter AK, Beltrán-Alcrudo D, Kock R
and Mor SM: Global trends in infectious diseases at the
wildlife-livestock interface. Proc Natl Acad Sci USA.
112:9662–9667. 2015.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Cárdenas L, Awada L, Tizzani P, Cáceres P
and Casal J: Characterization and evolution of countries affected
by bovine brucellosis (1996-2014). Transbound Emerg Dis.
66:1280–1290. 2019.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Dik I, Bulut O, Avci O, Hasoksuz M,
Palanci HS, Aslim HP and Bulut Z: Molecular detection and
characterization of bovine noroviruses from cattle in Konya,
Turkey. Pak Vet J. 43:67–72. 2023.
|
|
44
|
Alexander DJ: A review of avian influenza
in different bird species. Vet Microbiol. 74:3–13. 2000.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Velkers FC, Bouma A, Matthijs MGR, Koch G,
Westendorp ST and Stegeman JA: Outbreak of avian influenza H7N3 on
a Turkey farm in the Netherlands. Vet Rec. 159:403–405.
2006.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Alexander DJ: An overview of the
epidemiology of avian influenza. Vaccine. 25:5637–5644.
2007.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Mourya DT, Yadav PD, Ullas PT, Bhardwaj
SD, Sahay RR, Chadha MS, Shete AM, Jadhav S, Gupta N, Gangakhedkar
RR, et al: Emerging/re-emerging viral diseases & new viruses on
the Indian horizon. Indian J Med Res. 149:447–467. 2019.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Hayek MN: The infectious disease trap of
animal agriculture. Sci Adv. 8(eadd6681)2022.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Rohr JR, Barrett CB, Civitello DJ, Craft
ME, Delius B, DeLeo GA, Hudson PJ, Jouanard N, Nguyen KH, Ostfeld
RS, et al: Emerging human infectious diseases and the links to
global food production. Nat Sustain. 2:445–456. 2019.PubMed/NCBI View Article : Google Scholar
|
|
50
|
World Organisation for Animal Health
(OIE): Information on aquatic and terrestrial animal diseases: OIE,
Paris, 2021.
|
|
51
|
Abusalab S and Hamid M: Haemorrhagic
septicaemia: A general review. Sudan J Vet Res. 18:1–14. 2003.
|
|
52
|
Jelsma T, Wijnker JJ, Smid B, Verheij E,
van der Poel WHM and Wisselink HJ: Determination of intestinal
viral loads and distribution of bovine viral diarrhea virus,
classical swine fever virus, and peste des petits ruminants virus:
A pilot study. Pathogens. 10(1188)2021.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Karakurt E, Nuhoğlu H, Dağ S, Çelebi Ö,
Büyük F, Beytut E, Yıldız A, Kuru M and Akça D: Immunohistochemical
investigation of TNF-α and IFN-γ expressions in sheep fetuses with
brucellosis. Pak Vet J. 43:85–90. 2023.
|
|
54
|
Yi SW, Bui NA, Lee HS, Bui VN, Dao DT,
Nguyen TH, Lee HG, Jung YH, Hur TY and Oh SI: Age-dependent
cytokine expression in response to foot-and-mouth disease virus in
bovine peripheral blood mononuclear cells. Pak Vet J. 43:209–212.
2023.
|
|
55
|
Akhtar T, Shahid S, Asghar A, Naeem MI,
Aziz S and Ameer T: Utilisation of herbal bullets against newcastle
disease in poultry sector of Asia and Africa (2012-2022). Int J
Agric Biosci. 12:56–65. 2023.
|
|
56
|
Du X, Gul ST, Ahmad L, Hussain R and Khan
A: Fowl typhoid: Present scenario, diagnosis, prevention and
control measures. Int J Agric Biosci. 12:172–179. 2023.
|
|
57
|
Afzal Z, Javed MT, Mohsin M, Ahmad HMW,
Saeed Z, Taimoor M, Aleem RA, Raza A, Ayub A, Israr F, et al: The
usefulness of glutaraldehyde coagulation test as a conjuncture test
in the diagnosis of tuberculosis in humans and animals. Agrobiol
Rec. 15:34–40. 2024.
|
|
58
|
Sarmykova M, Yespembetov B, Sambetbayev A,
Tileukhanov K, Kaldyrkaev A, Shestakov A, Melisbek A, Burashev Y,
Usserbayev B and Syrym N: Isolation and characterization of
bacteriophage streptococcus equi for application against horse
strangles. Int J Vet Sci. 13:691–699. 2024.
|
|
59
|
Verma AK, Dhama K, Chakraborty S, Kumar A,
Tiwari A, Rahal A, Mahima and Singh SV: Strategies for
combating and eradicating important infectious diseases of animals
with particular reference to India: Present and future
perspectives. Asian J Anim Vet Adv. 9:77–106. 2014.
|
|
60
|
Nii-Trebi NI: Emerging and neglected
infectious diseases: Insights, advances, and challenges. Biomed Res
Int. 2017(5245021)2017.PubMed/NCBI View Article : Google Scholar
|
|
61
|
Walker JW, Han BA, Ott IM and Drake JM:
Transmissibility of emerging viral zoonoses. PLoS One.
13(e0206926)2018.PubMed/NCBI View Article : Google Scholar
|
|
62
|
Watkins K: Emerging infectious diseases: A
review. Curr Emerg Hosp Med Rep. 6:86–93. 2018.PubMed/NCBI View Article : Google Scholar
|
|
63
|
Singh RK, Sharma GK, Mahajan S, Dhama K,
Basagoudanavar SH, Hosamani M, Sreenivasa BP, Chaicumpa W, Gupta VK
and Sanyal A: Foot-and-Mouth disease virus: Immunobiology, advances
in vaccines and vaccination strategies addressing vaccine
failures-an indian perspective. Vaccines (Basel).
7(90)2019.PubMed/NCBI View Article : Google Scholar
|
|
64
|
Yatoo MI, Parray R, Bashir ST, Bhat RA,
Gopalakrishnan A, Karthik K, Dhama K and Singh SV: Veterinary
quarterly contagious caprine pleuropneumonia-a comprehensive review
contagious caprine pleuropneumonia-a comprehensive review. Vet Q.
39:1–25. 2019.PubMed/NCBI View Article : Google Scholar
|
|
65
|
Kabir A, Kalhoro DH, Abro SH, Kalhoro MS,
Yousafzai1 HA, Shams S, Khan IU, Lochi GM, Mazari MQ, Baloch MW, et
al: Peste des petits ruminants: A review. Pure Appl Biol.
8:1214–1222. 2019.
|
|
66
|
World Health Organization (WHO): Influenza
A (H1N2) variant virus-Brazil. WHO, Geneva, 2021.
|
|
67
|
McKendrick AG: Studies on the theory of
continuous probabilities, with special reference to its bearing on
natural phenomena of a progressive nature. Proc London Math Soc.
S2-S13:401–416. 1914.
|
|
68
|
McCulloch K, Romero N, MacLachlan J,
Allard N and Cowie B: Modeling progress toward elimination of
hepatitis B in Australia. Hepatology. 71:1170–1181. 2020.PubMed/NCBI View Article : Google Scholar
|
|
69
|
Farr W: On the cattle plague. J Soc Sci.
1:349–351. 1866.
|
|
70
|
Snow J: On continuous molecular changes,
more particularly in their relation to epidemic diseases. Rev
Infect Dis. 7:441–447. 1985.
|
|
71
|
Kermack WO and Mckendrick AG: A
contribution to the mathematical theory of epidemics. Proc R Soc
London Ser A, Contain Pap a Math Phys Character. 115:700–721.
1927.
|
|
72
|
Kermack WO and Mckendrick AG:
Contributions to the mathematical theory of epidemics. II. -The
problem of endemicity. Proc R Soc London Ser A, Contain Pap a Math
Phys Character. 138:55–83. 1932.
|
|
73
|
Kermack WO and McKendrick AG:
Contributions to the mathematical theory of epidemics. III.-Further
studies of the problem of endemicity. Proc R Soc London Ser A,
Contain Pap a Math Phys Character. 141:94–122. 1933.
|
|
74
|
Kermack WO and McKendrick AG:
Contributions to the mathematical theory of epidemics-III. Further
studies of the problem of endemicity. Bull Math Biol. 53:89–118.
1991.PubMed/NCBI View Article : Google Scholar
|
|
75
|
Ferguson NM, Donnelly CA and Anderson RM:
The foot-and-mouth epidemic in Great Britain: Pattern of spread and
impact of interventions. Science. 292:1155–1160. 2001.PubMed/NCBI View Article : Google Scholar
|
|
76
|
Anderson I: Foot and mouth disease 2007: A
review and lessons learned., 2008.
|
|
77
|
Funk S, Camacho A, Kucharski AJ, Eggo RM
and Edmunds WJ: Real-time forecasting of infectious disease
dynamics with a stochastic semi-mechanistic model. Epidemics.
22:56–61. 2018.PubMed/NCBI View Article : Google Scholar
|
|
78
|
Keeling MJ, Woolhouse MEJ, Shaw DJ,
Matthews L, Chase-Topping M, Haydon DT, Cornell SJ, Kappey J,
Wilesmith J and Grenfell BT: Dynamics of the 2001 UK foot and mouth
epidemic: Stochastic dispersal in a heterogeneous landscape.
Science. 294:813–817. 2001.PubMed/NCBI View Article : Google Scholar
|
|
79
|
Hayama Y, Firestone SM, Stevenson MA,
Yamamoto T, Nishi T, Shimizu Y and Tsutsui T: Reconstructing a
transmission network and identifying risk factors of secondary
transmissions in the 2010 foot-and-mouth disease outbreak in Japan.
Transbound Emerg Dis. 66:2074–2086. 2019.PubMed/NCBI View Article : Google Scholar
|
|
80
|
Picado A, Guitian FJ and Pfeiffer DU:
Space-time interaction as an indicator of local spread during the
2001 FMD outbreak in the UK. Prev Vet Med. 79:3–19. 2007.PubMed/NCBI View Article : Google Scholar
|
|
81
|
Keeling MJ and Rohani P: Modeling
infectious diseases in humans and animals. Clin Infect Dis.
47:864–866. 2008.
|
|
82
|
Kleczkowski A, Hoyle A and Mcmenemy P: One
model to rule them all? Modelling approaches across OneHealth, for
human, animal and plant epidemics. Philos Trans R Soc Lond B Biol
Sci. 374(20180255)2019.PubMed/NCBI View Article : Google Scholar
|
|
83
|
Thompson RN and Brooks-Pollock E:
Detection, forecasting and control of infectious disease epidemics:
Modelling outbreaks in humans, animals and plants. Philos Trans R
Soc B Biol Sci. 374(20190038)2019.PubMed/NCBI View Article : Google Scholar
|
|
84
|
Hart WS, Hochfilzer LFR, Cunniffe NJ, Lee
H, Nishiura H and Thompson RN: Accurate forecasts of the
effectiveness of interventions against Ebola may require models
that account for variations in symptoms during infection.
Epidemics. 29(100371)2019.PubMed/NCBI View Article : Google Scholar
|
|
85
|
Looi LM and Chua KB: Lessons from the
Nipah virus outbreak in Malaysia. Malays J Pathol. 29:63–67.
2007.PubMed/NCBI
|
|
86
|
Mörner T, Obendorf DL, Artois M and
Woodford MH: Surveillance monitoring of wildlife diseases. Rev Sci
Tech. 21:67–76. 2002.PubMed/NCBI View Article : Google Scholar
|
|
87
|
Gronvall G, Boddie C, Knutsson R and Colby
M: One health security: An important component of the global health
security agenda. Biosecur Bioterror. 12:221–224. 2014.PubMed/NCBI View Article : Google Scholar
|
|
88
|
Corning S: World Organisation for animal
health: Strengthening veterinary services for effective one health
collaboration. Rev Sci Tech. 33:639–650. 2014.PubMed/NCBI View Article : Google Scholar
|
|
89
|
Brooks-Pollock E, de Jong MCM, Keeling MJ,
Klinkenberg D and Wood JLN: Eight challenges in modelling
infectious livestock diseases. Epidemics. 10:1–5. 2015.PubMed/NCBI View Article : Google Scholar
|
|
90
|
Metcalf CJE, Edmunds WJ and Lessler J: Six
challenges in modelling for public health policy. Epidemics.
10:93–96. 2015.PubMed/NCBI View Article : Google Scholar
|
|
91
|
Ezanno P, Andraud M, Beaunée G, Hoch T,
Krebs S, Rault A, Touzeau S, Vergu E and Widgren S: How mechanistic
modelling supports decision making for the control of enzootic
infectious diseases. Epidemics. 32(100398)2020.PubMed/NCBI View Article : Google Scholar
|
|
92
|
Craft ME, Beyer HL and Haydon DT:
Estimating the probability of a major outbreak from the timing of
early cases: An indeterminate problem? PLoS One.
8(e57878)2013.PubMed/NCBI View Article : Google Scholar
|
|
93
|
Thompson RN, Gilligan CA and Cunniffe NJ:
Detecting presymptomatic infection is necessary to forecast major
epidemics in the earliest stages of infectious disease outbreaks.
PLoS Comput Biol. 12(e1004836)2016.PubMed/NCBI View Article : Google Scholar
|
|
94
|
Thompson PN and Etter E: Epidemiological
surveillance methods for vector-borne diseases. Rev Sci Tech.
34:235–247. 2015.PubMed/NCBI View Article : Google Scholar
|
|
95
|
Saegerman C, Humblet MF, Leandri M,
Gonzalez G, Heyman P, Sprong H, L'Hostis M, Moutailler S, Bonnet
SI, Haddad N, et al: First expert elicitation of knowledge on
possible drivers of observed increasing human cases of tick-borne
encephalitis in Europe. Viruses. 15(791)2023.PubMed/NCBI View Article : Google Scholar
|
|
96
|
Ahmad M, Hussain A, Soomro MH and Jalbani
S: Leptospirosis: An overview. In: One Health Triad. vol. 2 Abbas
R, Saeed N, Younus M, Aguilar-Marcelino L and Khan A (eds.) Unique
Scientific Publishers, Faisalabad, Pakistan, pp41-46, 2023.
|
|
97
|
Wen N: Establishment and development of
the disease surveillance system. Immun Progr China. 3:31–37.
2019.
|
|
98
|
World Health Organization (WHO): Antiviral
use and the risk of drug resistance. WHO, Geneva, 2009.
|
|
99
|
Iqbal HMN: The quest for materials-based
hydrogels with antimicrobial and antiviral potentialities. Open
Virol J. 12:69–79. 2018.PubMed/NCBI View Article : Google Scholar
|
|
100
|
Jones JC, Yen HL, Adams P, Armstrong K and
Govorkova EA: Influenza antivirals and their role in pandemic
preparedness. Antiviral Res. 210(105499)2023.PubMed/NCBI View Article : Google Scholar
|
|
101
|
Nijhuis M, Van Maarseveen NM and Boucher
CAB: Antiviral resistance and impact on viral replication capacity:
Evolution of viruses under antiviral pressure occurs in three
phases. Handb Exp Pharmacol. 189:299–320. 2009.PubMed/NCBI View Article : Google Scholar
|
|
102
|
Herlocher ML, Truscon R, Elias S, Yen HL,
Roberts NA, Ohmit SE and Monto AS: Influenza viruses resistant to
the antiviral drug oseltamivir: Transmission studies in ferrets. J
Infect Dis. 190:1627–1630. 2004.PubMed/NCBI View
Article : Google Scholar
|
|
103
|
Smyk JM, Szydłowska N, Szulc W and
Majewska A: Evolution of influenza viruses-drug resistance,
treatment options, and prospects. Int J Mol Sci.
23(12244)2022.PubMed/NCBI View Article : Google Scholar
|
|
104
|
Malmsten M: Antimicrobial and antiviral
hydrogels. Soft Matter. 7:8725–8736. 2011.
|
|
105
|
Prasad M, Lambe UP, Brar B, Shah I, Ranjan
JM, Rao R, Kumar S, Mahant S, Khurana SK, Iqbal HMN, et al:
Nanotherapeutics: An insight into healthcare and multi-dimensional
applications in medical sector of the modern world. Biomed
Pharmacother. 97:1521–1537. 2018.PubMed/NCBI View Article : Google Scholar
|
|
106
|
Pham T, Loupias P, Dassonville-Klimpt A
and Sonnet P: Drug delivery systems designed to overcome
antimicrobial resistance. Med Res Rev. 39:2343–2396.
2019.PubMed/NCBI View Article : Google Scholar
|
|
107
|
Le LV, Mkrtschjan MA, Russell B and Desai
TA: Hang on tight: Reprogramming the cell with microstructural
cues. Biomed Microdevices. 21(43)2019.PubMed/NCBI View Article : Google Scholar
|
|
108
|
Iqbal HMN and Dhama K: Emerging pathogens
and bioactive materials: In Greening The 21st century biomedical
sciences. J Exp Biol Agric Sci. 6:296–306. 2018.
|
|
109
|
Iqbal HMN and Keshavarz T: Bioinspired
polymeric carriers for drug delivery applications. In: stimuli
responsive polymeric nanocarriers for drug delivery applications:
Volume 1: Types and triggers. Elsevier, pp377-404, 2018.
|
|
110
|
Rasheed T, Bilal M, Abu-Thabit NY and
Iqbal HMN: The smart chemistry of stimuli-responsive polymeric
carriers for target drug delivery applications. In: Stimuli
responsive polymeric nanocarriers for drug delivery applications:
Volume 1: Types and Triggers. Elsevier, pp61-99, 2018.
|
|
111
|
Raza A, Hayat U, Rasheed T, Bilal M and
Iqbal HMN: ‘Smart’ materials-based near-infrared light-responsive
drug delivery systems for cancer treatment: A review. J Mater Res
Technol. 8:1497–1509. 2019.
|
|
112
|
Raza A, Rasheed T, Nabeel F, Hayat U,
Bilal M and Iqbal H: Endogenous and exogenous stimuli-responsive
drug delivery systems for programmed site-specific release.
Molecules. 24(1117)2019.PubMed/NCBI View Article : Google Scholar
|
|
113
|
Berger J, Reist M, Mayer JM, Felt O,
Peppas NA and Gurny R: Structure and interactions in covalently and
ionically crosslinked chitosan hydrogels for biomedical
applications. Eur J Pharm Biopharm. 57:19–34. 2004.PubMed/NCBI View Article : Google Scholar
|
|
114
|
Kalshetti PP, Rajendra VB, Dixit DN and
Parekh PP: Hydrogels as a drug delivery system and applications: A
review. Int J Pharm Pharm Sci. 4:1–7. 2011.
|
|
115
|
Rodriguez VAM, Dhama K and Iqbal H:
Biomaterials-based hydrogels and their drug delivery
potentialities. Int J Pharmacol. 13:864–873. 2017.
|
|
116
|
Jaguezeski AM, Souza CF, Perin G, Reis JH,
Gomes TMA, Baldissera MD, Vaucher RA, de Andrade CM, Stefani LM,
Gundel SS, et al: Effect of free and nano-encapsulated curcumin on
treatment and energetic metabolism of gerbils infected by Listeria
monocytogenes. Microb Pathog. 134(103564)2019.PubMed/NCBI View Article : Google Scholar
|
|
117
|
Omwenga EO, Hensel A, Shitandi A and
Goycoolea FM: Chitosan nanoencapsulation of flavonoids enhances
their quorum sensing and biofilm formation inhibitory activities
against an E.coli Top 10 biosensor. Colloids Surfaces B
Biointerfaces. 164:125–133. 2018.PubMed/NCBI View Article : Google Scholar
|
|
118
|
da Cunha JA, de Ávila Scheeren C, Fausto
VP, de Melo LDW, Henneman B, Frizzo CP, de Almeida Vaucher R, de
Vargas AC and Baldisserotto B: The antibacterial and physiological
effects of pure and nanoencapsulated Origanum majorana essential
oil on fish infected with Aeromonas hydrophila. Microb Pathog.
124:116–121. 2018.PubMed/NCBI View Article : Google Scholar
|
|
119
|
Lopes LQS, de Almeida Vaucher R, Giongo
JL, Gündel A and Santos RCV: Characterisation and anti-biofilm
activity of glycerol monolaurate nanocapsules against Pseudomonas
aeruginosa. Microb Pathog. 130:178–185. 2019.PubMed/NCBI View Article : Google Scholar
|
|
120
|
Shin S, Ahmed I, Hwang J, Seo Y, Lee E,
Choi J, Moon S and Hong JW: A microfluidic approach to
investigating a synergistic effect of tobramycin and sodium dodecyl
sulfate on Pseudomonas aeruginosa biofilms. Anal Sci. 32:67–73.
2016.PubMed/NCBI View Article : Google Scholar
|
|
121
|
Dua K, Gupta G, Rao NK and Bebawy M:
Nano-antibiotics: A novel approach in treating P. aeruginosa
biofilm infections. Minerva Med. 109(400)2018.PubMed/NCBI View Article : Google Scholar
|
|
122
|
Rozenbaum RT, Su L, Umerska A, Eveillard
M, Håkansson J, Mahlapuu M, Huang F, Liu J, Zhang Z, Shi L, et al:
Antimicrobial synergy of monolaurin lipid nanocapsules with
adsorbed antimicrobial peptides against Staphylococcus aureus
biofilms in vitro is absent in vivo. J Control Release. 293:73–83.
2019.PubMed/NCBI View Article : Google Scholar
|
|
123
|
Thomas V, Yallapu MM, Sreedhar B and
Bajpai SK: A versatile strategy to fabricate hydrogel-silver
nanocomposites and investigation of their antimicrobial activity. J
Colloid Interface Sci. 315:389–395. 2007.PubMed/NCBI View Article : Google Scholar
|
|
124
|
Rajchakit U and Sarojini V: Recent
developments in antimicrobial-peptide-conjugated gold
nanoparticles. Bioconjug Chem. 28:2673–2686. 2017.PubMed/NCBI View Article : Google Scholar
|
|
125
|
Kobayashi K, Yoon C, Oh SH, Pagaduan JV
and Gracias DH: Biodegradable thermomagnetically responsive soft
untethered grippers. ACS Appl Mater Interfaces. 11:151–159.
2019.PubMed/NCBI View Article : Google Scholar
|
|
126
|
Grewal TK, Majeed S and Sharma S:
Therapeutic implications of nano-encapsulated rifabutin,
azithromycin & ethambutol against experimental Mycobacterium
avium infection in mice. Indian J Med Res. 147:594–602.
2018.PubMed/NCBI View Article : Google Scholar
|
|
127
|
Mohid SA, Ghorai A, Ilyas H, Mroue KH,
Narayanan G, Sarkar A, Ray SK, Biswas K, Bera AK, Malmsten M, et
al: Application of tungsten disulfide quantum dot-conjugated
antimicrobial peptides in bio-imaging and antimicrobial therapy.
Colloids Surfaces B Biointerfaces. 176:360–370. 2019.PubMed/NCBI View Article : Google Scholar
|
|
128
|
Tsao CT, Chang CH, Lin YY, Wu MF, Wang JL,
Han JL and Hsieh KH: Antibacterial activity and biocompatibility of
a chitosan-gamma-poly(glutamic acid) polyelectrolyte complex
hydrogel. Carbohydr Res. 345:1774–1780. 2010.PubMed/NCBI View Article : Google Scholar
|
|
129
|
Tsao CT, Chang CH, Lin YY, Wu M, Wang JL,
Young T, Han JL and Hsieh K: Evaluation of chitosan/γ-poly(glutamic
acid) polyelectrolyte complex for wound dressing materials.
Carbohydrate Polymers. 84:812–819. 2011.
|
|
130
|
Bilal M, Rasheed T, Iqbal HMN, Li C, Hu H
and Zhang X: Development of silver nanoparticles loaded
chitosan-alginate constructs with biomedical potentialities. Int J
Biol Macromol. 105:393–400. 2017.PubMed/NCBI View Article : Google Scholar
|
|
131
|
Naeem MI, Rehman A, Zahid R, Tehseen U,
Arbab Z, Aziz S, Akhtar T, Ahmad HM, Ullah MR, Akram Q, et al: Use
of nanotechnology to mitigate antimicrobial resistance. Agrobiol
Rec. 13:16–33. 2023.
|
|
132
|
Bilal M, Zhao Y, Rasheed T, Ahmed I,
Hassan S, Nawaz M and Iqbal H: Biogenic nanoparticle-chitosan
conjugates with antimicrobial, antibiofilm, and anticancer
potentialities: Development and characterization. Int J Environ Res
Public Health. 16(598)2019.PubMed/NCBI View Article : Google Scholar
|
|
133
|
Alshubaily FA and Al-Zahrani MH: Appliance
of fungal chitosan/ceftriaxone nano-composite to strengthen and
sustain their antimicrobial potentiality against drug resistant
bacteria. Int J Biol Macromol. 135:1246–1251. 2019.PubMed/NCBI View Article : Google Scholar
|
|
134
|
Zhang CY, Gao J and Wang Z: Bioresponsive
nanoparticles targeted to infectious microenvironments for sepsis
management. Adv Mater. 30(e1803618)2018.PubMed/NCBI View Article : Google Scholar
|
|
135
|
Håkansson J, Ringstad L, Umerska A,
Johansson J, Andersson T, Boge L, Rozenbaum RT, Sharma PK, Tollbäck
P, Björn C, et al: Characterization of the in vitro, ex vivo, and
in vivo efficacy of the antimicrobial peptide DPK-060 used for
topical treatment. Front Cell Infect Microbiol.
9(174)2019.PubMed/NCBI View Article : Google Scholar
|
|
136
|
Thorgeirsdöttir TO, Thormar H and
Kristmundsottir T: Effects of polysorbates on antiviral and
antibacterial activity of monoglyceride in pharmaceutical
formulations. Pharmazie. 58:286–287. 2003.PubMed/NCBI
|
|
137
|
Kristmundsdóttir T, Árnadóttir SG,
Bergsson G and Thormar H: Development and evaluation of
microbicidal hydrogels containing monoglyceride as the active
ingredient. J Pharm Sci. 88:1011–1015. 1999.PubMed/NCBI View Article : Google Scholar
|
|
138
|
Thormar H, Bergsson G, Gunnarsson E,
Georgsson G, Witvrouw M, Steingrímsson O, De Clercq E and
Kristmundsdóttir T: Hydrogels containing monocaprin have potent
microbicidal activities against sexually transmitted viruses and
bacteria in vitro. Sex Transm Infect. 75:181–185. 1999.PubMed/NCBI View Article : Google Scholar
|
|
139
|
Rokhade AP, Patil SA and Aminabhavi TM:
Synthesis and characterization of semi-interpenetrating polymer
network microspheres of acrylamide grafted dextran and chitosan for
controlled release of acyclovir. Carbohydr Polym. 67:605–613.
2007.
|
|
140
|
Nair M, Jayant RD, Kaushik A and Sagar V:
Getting into the brain: Potential of nanotechnology in the
management of NeuroAIDS. Adv Drug Deliv Rev. 103:202–217.
2016.PubMed/NCBI View Article : Google Scholar
|
|
141
|
Fiandra L, Colombo M, Mazzucchelli S,
Truffi M, Santini B, Allevi R, Nebuloni M, Capetti A, Rizzardini G,
Prosperi D and Corsi F: Nanoformulation of antiretroviral drugs
enhances their penetration across the blood brain barrier in mice.
Nanomedicine. 11:1387–1397. 2015.PubMed/NCBI View Article : Google Scholar
|
|
142
|
Edagwa B, McMillan JE, Sillman B and
Gendelman HE: Long-acting slow effective release antiretroviral
therapy. Expert Opin Drug Deliv. 14:1281–1291. 2017.PubMed/NCBI View Article : Google Scholar
|
|
143
|
Zhang W, Wang M, Tang W, Wen R, Zhou S,
Lee C, Wang H, Jiang W, Delahunty IM, Zhen Z, et al:
Nanoparticle-laden macrophages for tumor-tropic drug delivery. Adv
Mater. 30(e1805557)2018.PubMed/NCBI View Article : Google Scholar
|
|
144
|
Mobo BHP, Rabinowitz PM, Conti LA and
Taiwo OA: Occupational health of animal workers. Human-Animal Med.
343–371. 2010.
|
|
145
|
Trinity L, Merrill SC, Clark EM, Koliba
CJ, Zia A, Bucini G and Smith JM: Effects of social cues on
biosecurity compliance in livestock facilities: Evidence from
experimental simulations. Front Vet Sci. 7(130)2020.PubMed/NCBI View Article : Google Scholar
|
|
146
|
Salman MD: The role of veterinary
epidemiology in combating infectious animal diseases on a global
scale: The impact of training and outreach programs. Prev Vet Med.
92:284–287. 2009.PubMed/NCBI View Article : Google Scholar
|
|
147
|
Alexandrino-Junior F, Silva KG, Freire
MCLC, Lione VD, Cardoso EA, Marcelino HR, Genre J, de Oliveira AG
and do Egito EST: A functional wound dressing as a potential
treatment for cutaneous leishmaniasis. Pharmaceutics.
11(200)2019.PubMed/NCBI View Article : Google Scholar
|
|
148
|
Amaral AC, Saavedra PHV, Souza ACO, de
Melo MT, Tedesco AC, Morais PC, Felipe MS and Bocca AL: Miconazole
loaded chitosan-based nanoparticles for local treatment of
vulvovaginal candidiasis fungal infections. Colloids Surfaces B
Biointerfaces. 174:409–415. 2019.PubMed/NCBI View Article : Google Scholar
|
|
149
|
Amaral AC, Bocca AL, Ribeiro AM, Nunes J,
Peixoto DL, Simioni AR, Primo FL, Lacava ZG, Bentes R,
Titze-de-Almeida R, et al: Amphotericin B in poly
(lactic-co-glycolic acid)(PLGA) and dimercaptosuccinic acid (DMSA)
nanoparticles against paracoccidioidomycosis. J Antimicrob
Chemother. 63:526–533. 2009.PubMed/NCBI View Article : Google Scholar
|
|
150
|
Yu Y, Peng L, Liao G, Chen Z and Li C:
Noncovalent complexation of amphotericin B with poly(β-Amino Ester)
derivates for treatment of C. Neoformans infection. Polymers
(Basel). 11(270)2019.PubMed/NCBI View Article : Google Scholar
|
|
151
|
Mehrizi TZ, Ardestani MS, Hoseini MH,
Khamesipour A, Mosaffa N and Ramezani A: Novel nano-sized chitosan
amphotericin B formulation with considerable improvement against
Leishmania major. Nanomedicine (Lond). 13:3129–3147.
2018.PubMed/NCBI View Article : Google Scholar
|
|
152
|
Kumar R, Pandey K, Sahoo GC, Das S, Das V,
Topno RK and Das P: Development of high efficacy peptide coated
iron oxide nanoparticles encapsulated amphotericin B drug delivery
system against visceral leishmaniasis. Mater Sci Eng C Mater Biol
Appl. 75:1465–1471. 2017.PubMed/NCBI View Article : Google Scholar
|
|
153
|
Heidari-Kharaji M, Taheri T, Doroud D,
Habibzadeh S and Rafati S: Solid lipid nanoparticle loaded with
paromomycin: In vivo efficacy against Leishmania tropica infection
in BALB/c mice model. Appl Microbiol Biotechnol. 100:7051–7060.
2016.PubMed/NCBI View Article : Google Scholar
|
|
154
|
Gupta PK, Jaiswal AK, Kumar V, Verma A,
Dwivedi P, Dube A and Mishra PR: Covalent functionalized
self-assembled lipo-polymerosome bearing amphotericin B for better
management of leishmaniasis and its toxicity evaluation. Mol Pharm.
11:951–963. 2014.PubMed/NCBI View Article : Google Scholar
|
|
155
|
Das S, Suresh P and Desmukh R: Design of
Eudragit RL 100 nanoparticles by nanoprecipitation method for
ocular drug delivery. Nanomedicine. 6:318–323. 2010.PubMed/NCBI View Article : Google Scholar
|
|
156
|
Sangeetha S, Venkatesh DN, Adhiyaman R,
Santhi K and Suresh B: Formulation of sodium alginate nanospheres
containing amphotericin b for the treatment of systemic
candidiasis. Trop J Pharm Res. 6:653–659. 2007.
|
|
157
|
Louie A, Deziel M, Liu W, Drusano MF,
Gumbo T and Drusano GL: Pharmacodynamics of caspofungin in a murine
model of systemic candidiasis: Importance of Persistence of
caspofungin in tissues to understanding drug activity. Antimicrob
Agents Chemother. 49:5058–5068. 2005.PubMed/NCBI View Article : Google Scholar
|