Introduction
The anatomy of the tracheobronchial tree has been
thoroughly investigated over the past hundred years using
anatomical dissections and bronchography. Various congenital
abnormalities can affect the bronchi, lungs, and their vascular
supply. These anomalies in bronchial anatomy can include atypical
origins, missing branches, extra branches, and congenital
diverticula (1). In contrast to
the numerous variations found in lobar or segmental bronchial
subdivisions, it is rare for abnormal bronchi to originate from the
trachea or main bronchi. Significant bronchial abnormalities
include the accessory cardiac and tracheal bronchus (TB) (2). TB is an abnormal bronchus that
emerges directly from the lateral wall of the trachea above the
carina, providing air to the upper lobes. First described by
Sandifort in 1785, it is typically an asymptomatic anatomical
variation that is often discovered incidentally during a chest
computed tomography (CT) scan or bronchoscopy (3). The average incidence rate of TB is
0.1-2% in the general population. It is typically found on the
right side of the trachea and is more common among males (4). Patients with congenital tracheal
stenosis (TS) sometimes exhibit this abnormality, with the
occurrence of TB in these patients varying from 11.9 to 24.7%
(5). The congenital TS is a
markedly rare malformation characterized by complete annular
tracheal rings, which is in contrast to the typical C-shaped
tracheal cartilages. It is estimated to affect ~1 in 64,500 live
births, accounting for merely 0.3-1% of all laryngotracheal
stenosis subtypes (6). However,
accurately determining the incidence of congenital TS poses
challenges, as numerous patients remain undiagnosed due to
diagnostic uncertainties among practitioners and high mortality
rates before definitive diagnosis (7). Another type of congenital pulmonary
anomaly is pulmonary sequestration (PS), typically identified
during childhood or adolescence. These non-functional masses of
pulmonary tissue lack connection to the tracheobronchial tree and
are nourished by an abnormal systemic artery. Similar to tracheal
bronchi, they commonly present no symptoms and are usually
discovered incidentally (4,8). The
PS is rare, accounting for ~1 to 6% of all congenital lung
anomalies. It can often remain undetected during prenatal and early
childhood (9). The present study
describes an extremely rare case of simultaneous TB, congenital TS
and PS in a single patient. It is organized according to the CaReL
guidelines (10). All studies
referenced herein were evaluated for eligibility (11).
Case report
Patient information
A 4-year-old boy presented to the Emergency Room at
Smart Health Tower (Sulaymaniyah, Iraq) with shortness of breath
and stridor. The patient had a history of frequent episodes of the
same issue since birth and had been misdiagnosed with asthma. The
management plan included inhaled corticosteroids as the primary
treatment and short-acting beta-agonists, particularly during
asthma attacks or severe symptoms.
Clinical findings
A clinical examination revealed tachypnea
(respiratory rate, 30 cycles/min) and audible stridor, with a
temperature of 37.9˚C. Hematological investigations revealed
elevated white blood cell counts (13,000 cells/mm³) and C-reactive
protein levels (15 mg/dl).
Diagnostic approach
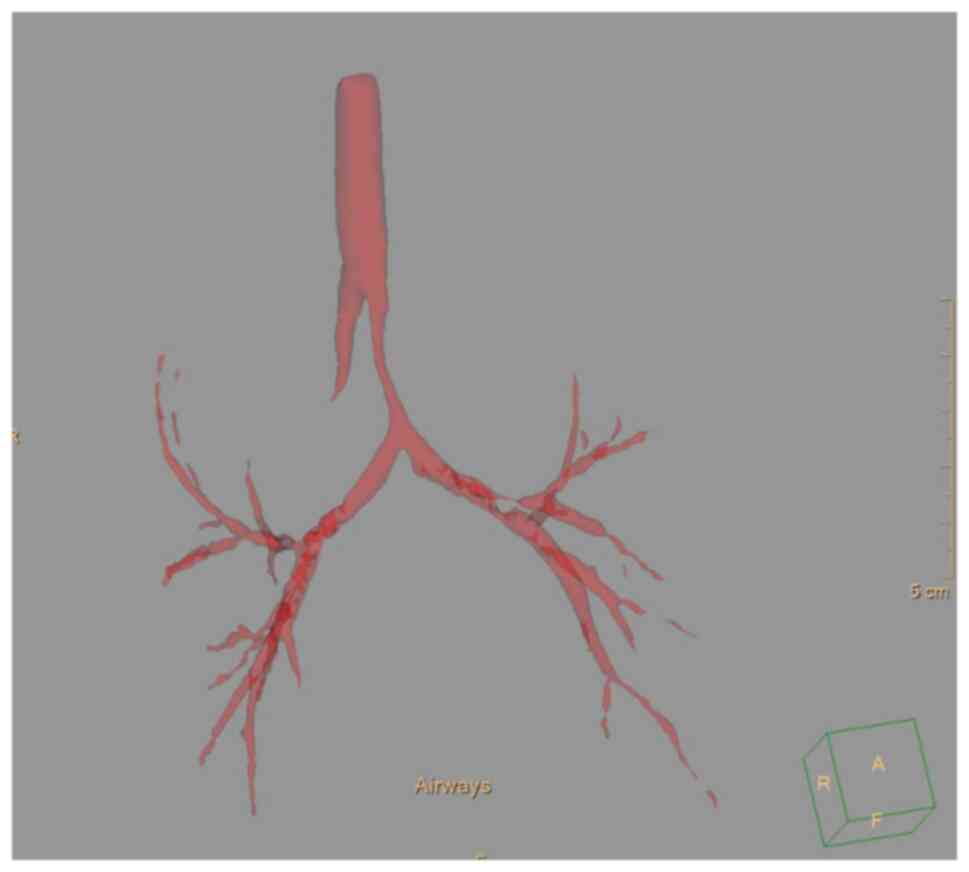
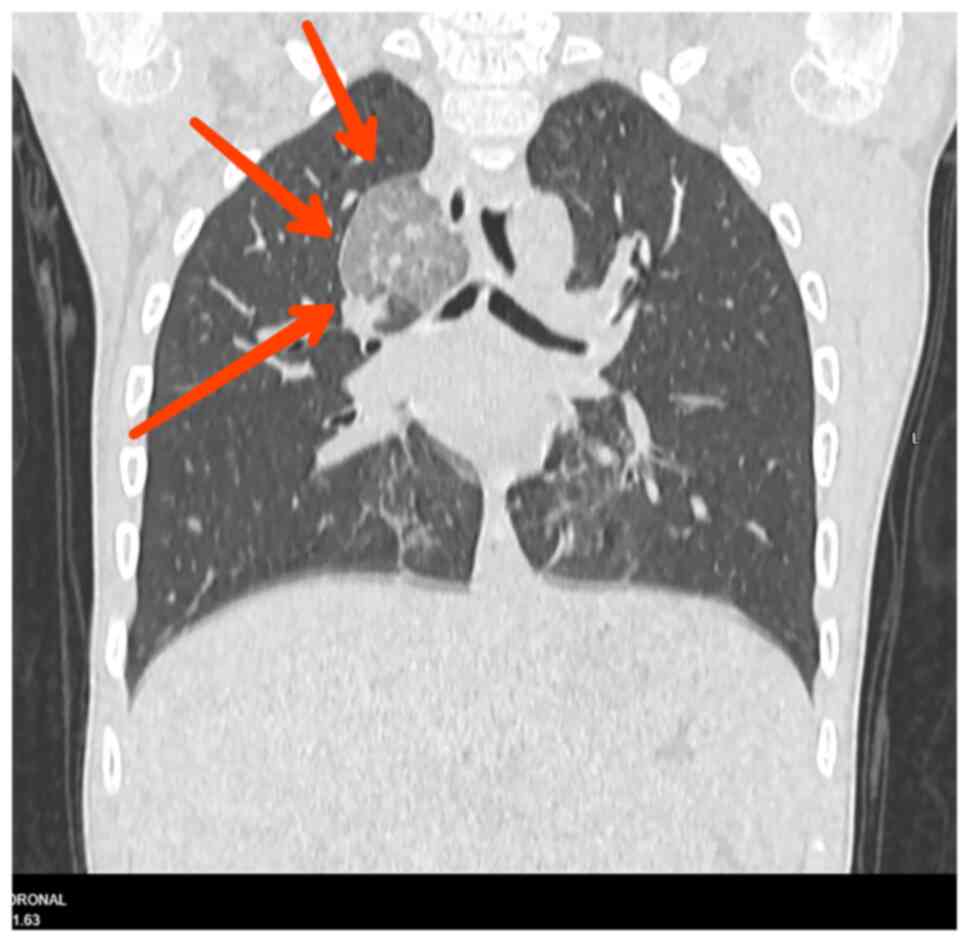
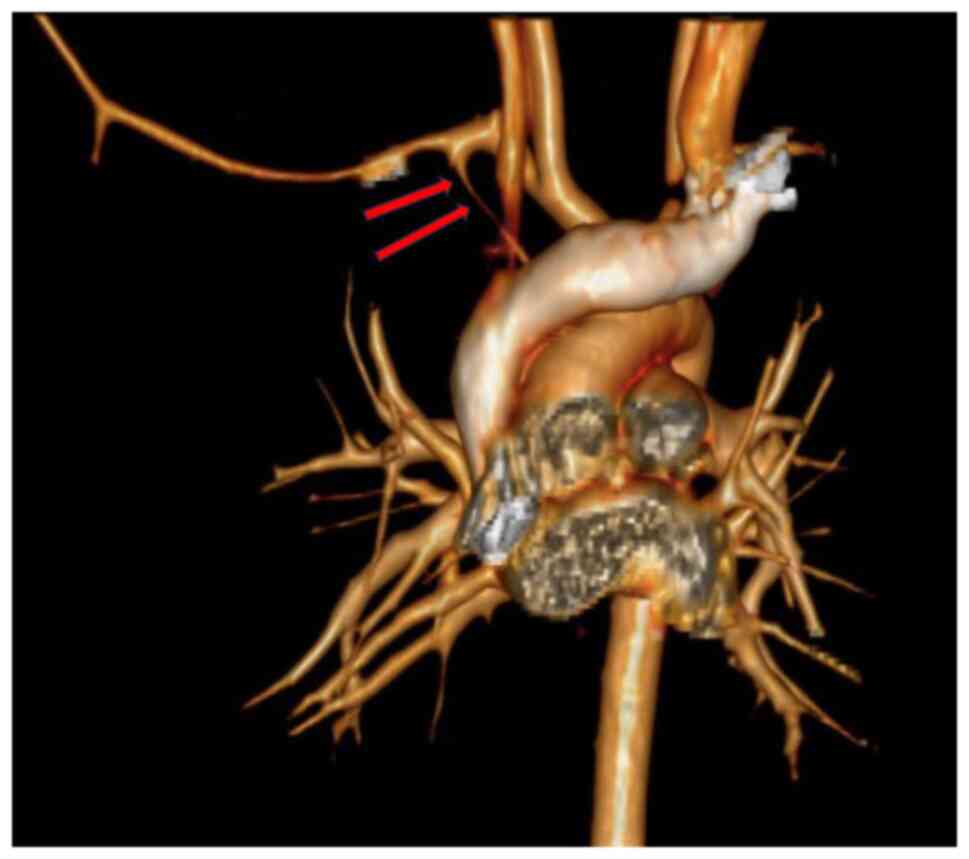
A subsequent chest CT scan revealed a TB and severe
TS beginning just below the TB and extending to the carina.
Notably, the TB was supplying additional lobar sequestration on the
right side of the lung (Fig. 1,
Fig. 2 and Fig. 3).
Therapeutic interventions
The patient received resuscitation with oxygen
therapy, intravenous (IV) fluids, IV antibiotics and a low dose of
steroid (4 mg dexamethasone x2). Surgery was planned.
Follow-up and outcomes
The patient was lost to follow-up, and as a result,
the surgery was not performed (Table
I).
 | Table IChronological summary of clinical
events. |
Table I
Chronological summary of clinical
events.
| Time point | Clinical event |
|---|
| Since birth | Recurrent respiratory
distress and stridor. |
| Age 4 years | Emergency visit with
acute respiratory symptoms. |
| Upon
presentation | Chest CT scan
performed, revealing TB, TS and intralobar PS. |
| Shortly afterward (on
the same day of presentation) | Medical management
was initiated; symptoms improved. |
| Post-discharge | The patient was lost
to follow-up. |
Discussion
The typical development of the tracheobronchial tree
in humans commences between the 24th and 26th days of gestation. It
begins as a central protrusion on the front wall of the pharynx,
forming at the lower end of the laryngotracheal groove. (3) Between the 28th and 30th weeks of
gestation, the lung buds extend to form the primary bronchi. By the
36th day of gestation, all segmental bronchi are formed. TB is an
abnormal anatomical development characterized by various bronchial
anomalies originating from the trachea or main bronchi and directed
toward the upper lung lobes (3).
Alescio et al (12) linked TB formation to an
embryogenesis defect rather than a genetic abnormality. Their study
demonstrated that transplanting bronchial mesenchyme into the
tracheal epithelium led to TB (12).
Typically, TB manifests as a bronchus leading to the
right upper lobe, although instances of left tracheal bronchi have
been infrequently reported (13).
Studies utilizing bronchography and bronchoscopy have reported a
prevalence ranging from 0.1 to 2% for right TB, and 0.3 to 1% for
left TB (2). The study by Dave
et al (14) analyzed 1,021
rigid endoscopies of the trachea performed on children aged 0 to 6
years. The TB was identified in 11 cases. Of note, all detected TB
cases originated from the right lateral wall of the trachea
(14). In another study by Findik
(1), an average of 12,648 adult
patients underwent bronchoscopy in their clinic over a period of 10
years. Among these, 8 patients were diagnosed with right-sided TB
(1). Accordingly, the present
study found the TB on the right side of the trachea.
Of note, two primary types of TB have been
identified: Supernumerary and displaced tracheal bronchi. The
supernumerary type, considered relatively uncommon, is an accessory
bronchus. Conversely, a displaced bronchus originates from an
abnormal position and supplies one or more segments of the upper
lobe, typically the apical segment (15). The type of TB in the patient in the
present study was supernumerary.
The TB typically presents with either no or minimal
clinical symptoms. However, recent case reports have highlighted
associations with persistent atelectasis, hemoptysis, recurrent
pulmonary infection, bronchiectasis necessitating surgery of the
affected segment and instances of lung cancer (3,16,17).
Additionally, patients may exhibit symptoms such as persistent
cough, stridor and acute respiratory distress. These symptoms often
arise from retained secretions in the narrow bronchus, with
superadded infections as a contributing factor (3). The case presented herein suffered
from shortness of breath and stridor from birth.
TB should be considered in patients with recurrent
chest infections, persistent or chronic bronchitis and a persistent
cough. A chest X-ray may reveal an ectopic TB originating above the
carina, although this is not always the case, and additional
investigations are necessary to confirm the diagnosis (16). Bronchoscopy is considered an
invasive method for diagnosing TB, as it can reveal the opening of
the TB and other anomalies in the tracheobronchial tree.
Non-invasive diagnostic methods include a chest CT scan, the
preferred imaging modality for identifying this anomaly, as it can
accurately delineate the tracheal and bronchial anatomy (17,18).
In the case in the present study, a CT scan of the chest with 3D
reconstruction of the tracheobronchial tree revealed the presence
of TB and TS. The stenosis began just below the TB and extended
down to the carina. However, a CT scan of the chest with
intravenous contrast revealed sequestration on the right side of
the chest, located above the hilum.
TB may be linked with various congenital anomalies,
such as tracheal hypoplasia, TS, lobar emphysema, pulmonary cystic
lesions, cardiovascular disorders (particularly cyanotic cardiac
lesions), other bronchial tree abnormalities and Down syndrome
(19,20). Arslan et al (4) reported TB with PS and an azygos lobe
in a single case. Moreover, Morita et al (5) documented that out of 51 pediatric
patients with congenital TS who underwent tracheal reconstruction
at a single institution between January, 2006 and December, 2015,
14 patients had congenital TS associated with TB. In the present
case report, the patient was unexpectedly diagnosed with TB
associated with congenital TS and PS. To date, only six studies
(4,5,21-24),
including 41 cases of TB associated with congenital TS or PS, have
been reported (Table II). To the
best of our knowledge, the coexistence of these three anomalies in
a single case has not yet been reported in the literature.
 | Table IICases of tracheal bronchus associated
with either congenital tracheal stenosis or pulmonary sequestration
reported in the literature. |
Table II
Cases of tracheal bronchus associated
with either congenital tracheal stenosis or pulmonary sequestration
reported in the literature.
| Authors, year or
publication | Study design | No. of cases | Age | Sex (M/F) | Diagnostic
method | Co-occurrence | Management | (Refs.) |
|---|
| Arslan et al,
2013 | Case report | 1 | 53 years | 1/0 | Bronchoscopy and CT
scan | TB, PS and azygos
lobe | Conservative
treatment | (4) |
| Morita et al,
2016 | Case series | 13 | 4 monthsa | 8/5 | Bronchoscopy | TB and congenital
TS | Surgery | (5) |
| Loh et al,
2015 | Case report | 1 | 66 years | 0/1 | CT scan and 3-D
image | TB and congenital
TS | N/A | (21) |
| Wang et al,
2015 | Case series | 24 | 20.6
monthsa | 10/14 | CT scan | TB, congenital TS and
CHD | Surgery | (22) |
| Wong et al,
1998 | Case report | 1 | 2 years | 1/0 | Bronchoscopy | TB and congenital
TS | Conservative
treatment | (23) |
| Yamoto et al,
2020 | Case report | 1 | 37 weeks | 1/0 | CT scan | Bilateral TB and
congenital TS | Surgery | (24) |
The PS occurs in the population at a rate of
0.15-1.7% and is more common in males than females. Typically, it
is located in the inferior, posterior, and medial segments of the
left half of the thoracic cavity. In 74% of cases, it is supplied
by aberrant arteries originating from the thoracic aorta, and in
18.7% of cases, from the abdominal aorta (4). In the present case report, the PS was
located on the right side of the chest of a 4-year-old male child
above the hilum. The arterial supply came from the right subclavian
artery, and the venous drainage was to the superior vena cava.
The co-occurrence of congenital TS with TB ranges
from 11.9 to 24.7% of all congenital TS cases (5). The stenotic trachea is often located
near the right upper lobe bronchus (RULB), and preserving the RULB
complicates tracheal reconstruction for congenital TS when TB is
involved.
The optimal surgical approaches for congenital TS
with TB continues to be a matter of debate. This controversy
primarily arises from the diverse forms of congenital TS associated
with TB that have been documented (5). Congenital TS used to be associated
with mortality rates as high as 50%. However, various surgical
techniques have been developed to treat congenital TS, resulting in
more acceptable operative mortality rates (7-13%). Slide
tracheoplasty has been celebrated as a breakthrough in managing
congenital TS, achieving significantly improved outcomes. For
long-segment lesions, slide tracheoplasty has mostly replaced
tracheal patching with costal cartilage or pericardium due to the
high re-intervention rates associated with those methods.
Conversely, end-to-end anastomoses are typically used for patients
with short-segment congenital TS. Despite these advances,
surgically managing TS with abnormal bronchial branching or
involvement remains challenging (24). TB alone can often be observed when
asymptomatic, whereas symptomatic cases with recurrent pneumonia
typically necessitate resection of the affected lung segment
(segmentectomy or lobectomy) (25). PS is definitely managed through
surgical removal of the sequestered lobe or segment. Minimally
invasive techniques, including video-assisted or robotic
approaches, have been reported for PS, and uniportal segmentectomy
can effectively preserve normal lung parenchyma during resection
(26,27). In complex scenarios involving all
three anomalies, a multidisciplinary approach is essential. For
instance, airway reconstruction (slide tracheoplasty/bronchoplasty)
may be performed in stages or combined with pulmonary resection to
alleviate stenosis and excise the sequestration (4-6,8)
The case described in the present study illustrates
the diagnostic challenges posed by rare tracheobronchial anomalies,
particularly when they mimic more common conditions such as asthma.
Early recognition through advanced imaging and prompt referral to
specialized surgical centers are essential. The present case report
emphasizes the importance of heightened clinical awareness to
prevent misdiagnosis and delays in treatment. A limitation of the
present case report is that the patient was lost to follow-up and
was therefore unable to undergo further treatment.
In conclusion, the coexistence of TB, congenital TS
and PS is exceptionally rare and may easily be misdiagnosed as
common respiratory conditions such as asthma. It is essential to
consider such rare congenital anomalies in children presenting with
persistent stridor or unexplained respiratory symptoms.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
FHK and HKA were major contributors to the
conception of the study, as well as to the literature search for
related studies. SMA, KMH, HOK and BAM contributed to the clinical
management of the patient, assisted in data acquisition and
interpretation, and participated in the literature review and
manuscript preparation. HAN and SHM contributed to the conception
and design of the study, the literature review, the critical
revision of the manuscript, and the processing of the table. SHT
and RJR were the radiologists who performed the assessment of the
case. FHK and HKA assisted in diagnosing the patient, contributed
to the management of the patient, and participated in manuscript
review. FHK and HAN confirm the authenticity of all the raw data.
All authors have read and approved the final manuscript.
Ethics approval and consent to
participate
Written informed consent was obtained from the
patient's parent for this participation in the present study.
Patient consent for publication
Written informed consent was obtained from the
patient's parent for the publication of this case report and any
accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Findik S: Tracheal bronchus in the adult
population. J Bronchology Interv Pulmonol. 18:149–153.
2011.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Ghaye B, Szapiro D, Fanchamps JM and
Dondelinger RF: Congenital bronchial abnormalities revisited.
Radiographics. 21:105–119. 2001.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Eddine HJ and Arab WA: Tracheal bronchus:
Case report and literature review. SN Comprehensive Clinical
Medicine. 3:399–403. 2021.
|
|
4
|
Arslan S, Sabancioğullari V and Akkurt İ:
Concomitant occurrence of tracheal bronchus, pulmonary
sequestration and azygos lobe. Turk Gogus Kalp Damar Cerrahisi
Derg. 21(2):506–509. 2013.
|
|
5
|
Morita K, Yokoi A, Fukuzawa H, Hisamatsu
C, Endo K, Okata Y, Tamaki A, Mishima Y, Oshima Y and Maeda K:
Surgical intervention strategies for congenital tracheal stenosis
associated with a tracheal bronchus based on the location of
stenosis. Pediatr Surg Int. 32:915–919. 2016.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Herrera P, Caldarone C, Forte V, Campisi
P, Holtby H, Chait P, Chiu P, Cox P, Yoo SJ, Manson D and Kim PC:
The current state of congenital tracheal stenosis. Pediatr Surg
Int. 23:1033–1044. 2007.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Pellen G, Pandit C, Castro C, Robinson P,
Seton C, Fitzgerald DA, Waters K and Cheng AT: Use of non-invasive
ventilation in children with congenital tracheal stenosis. Int J
Pediatr Otorhinolaryngol. 127(109672)2019.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Alsumrain M and Ryu JH: Pulmonary
sequestration in adults: A retrospective review of resected and
unresected cases. BMC Pulm Med. 18:1–5. 2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Walker CM, Wu CC, Gilman MD, Godwin JD II,
Shepard JA and Abbott GF: The imaging spectrum of bronchopulmonary
sequestration. Curr Probl Diagn Radiol. 43:100–114. 2014.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Prasad S, Nassar M, Azzam AY, José FG,
Jamee M, Sliman RKA, Evola G, Mustafa AM, Abdullah HO, Abdalla BA,
et al: CaReL guidelines: A consensus-based guidelines on case
reports and literature review (CaReL). Barw Med J. 2:13–19.
2024.
|
|
11
|
Abdullah HO, Abdalla BA, Kakamad FH, Ahmed
JO, Baba HO, Hassan MN, Bapir R, Rahim HM, Omar DA, Kakamad SH, et
al: Predatory publishing lists: A review on the ongoing battle
against fraudulent actions. Barw Med J. 2:26–30. 2024.
|
|
12
|
Alescio T and Cassini A: Induction in
vitro of tracheal buds by pulmonary mesenchyme grafted on tracheal
epithelium. J Exp Zool. 150:83–94. 1962.PubMed/NCBI View Article : Google Scholar
|
|
13
|
O'Sullivan BP, Frassica JJ and Rayder SM:
Tracheal bronchus: A cause of prolonged atelectasis in intubated
children. Chest. 113:537–540. 1998.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Dave MH, Gerber A, Bailey M, Gysin C,
Hoeve H, Hammer J, Nicolai T and Weiss M: The prevalence of
tracheal bronchus in pediatric patients undergoing rigid
bronchoscopy. J Bronchology Interv Pulmonol. 21:26–31.
2014.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Siegel MJ, Shackelford GD, Francis RS and
McAlister WH: Tracheal bronchus. Radiology. 130:353–355.
1979.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Ikeno S, Mitsuhata H, Saito K, Hirabayashi
Y, Akazawa S, Kasuda H and Shimizu R: Airway management for
patients with a tracheal bronchus. Br J Anaesth. 76:573–575.
1996.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Ruchonnet-Metrailler I, Taam RA and de
Blic J: Presence of tracheal bronchus in children undergoing
flexible bronchoscopy. Respir Med. 109:846–850. 2015.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Manjunatha YC, Gupta AK and Gupta SK:
Subacute combined degeneration of the spinal cord in a child.
Indian J Pediatr. 78:240–241. 2011.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Aoun NY, Velez E, Kenney LA and Trayner
EE: Tracheal bronchus. Respir Care. 49:1056–1058. 2004.PubMed/NCBI
|
|
20
|
Reis JC, Martins CR, Otta LH, Tardelli MA
and Amaral JL: Complication related to tracheal bronchus in infant:
Case report. Rev Bras Anestesiol. 56:72–77. 2006.PubMed/NCBI View Article : Google Scholar : (In Portuguese).
|
|
21
|
Loh PS, Hashim SA, Aman RR, Lai LL and
Chan L: A challenging case of tracheal bronchus with concurrent
tracheal stenosis for one lung ventilation. Trends in Anaesthesia
and Critical Care. 5:136–139. 2015.
|
|
22
|
Wang S, Zhang H, Zhu L, Zhen J, Liu J and
Xu Z: Surgical management of congenital tracheal stenosis
associated with tracheal bronchus and congenital heart disease. Eur
J Cardiothorac Surg. 49:1201–1206. 2016.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Wong KS, Wang CR and Hsieh KH:
Demonstration of tracheal bronchus associated with tracheal
stenosis using direct coronal computed tomography. Pediatr
Pulmonol. 25:133–135. 1998.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Yamoto M, Fukumoto K and Urushihara N:
Tracheoplasty for congenital tracheal stenosis with bilateral
tracheal bronchus. Ann Thorac Cardiovasc Surg. 28:159–162.
2022.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Gullapalli D, Tangutoori S and Ganti SS:
Respiratory maze: An anatomical variant of tracheal bronchus.
Respirol Case Rep. 12(e01355)2024.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Lin TH, Huang WL, Chang CC, Yen YT, Lai
WW, Tseng YL and Chen YY: Uniportal video-assisted thoracoscopic
surgery lobectomy and segmentectomy for pulmonary sequestration. J
Thorac Dis. 10(3722)2018.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Mezzetti M, Dell'Agnola CA, Bedoni M,
Cappelli R, Fumagalli F and Panigalli T: Video-assisted
thoracoscopic resection of pulmonary sequestration in an infant.
Ann Thorac Surg. 61:1836–1838. 1996.PubMed/NCBI View Article : Google Scholar
|