Introduction
A phyllodes tumor (PT) is a rare type of breast
tumor known for its diverse biological behavior, which can range
from benign to malignant forms. A number of PTs are known for their
rapid growth and are classified as fibroepithelial neoplasms with a
tendency for local recurrence (1).
PTs comprise up to ~0.3 to 1% of all primary breast tumors.
Although they can occur at any age, they are most frequently
observed in women between 30 and 50 years of age (2).
PTs were initially described in 1838 by Johannes
Müller, who named them cystosarcoma phyllodes due to their
leaf-like (phyllodial) projections into cystic spaces and their
sarcoma-like stromal features (3).
However, this term is somewhat misleading, as up to 70% of these
tumors follow a benign course and cystic degeneration is uncommon
(1). In 1931, the first case of a
malignant PT that had spread to the lungs was documented,
highlighting the potential of the tumor for malignancy (4).
Recent studies indicate that ~10 to 15% of PTs are
malignant. Malignant PTs have a high risk of local recurrence,
occurring in up to 30% of cases, and they also have the potential
to metastasize. PTs >10 cm in size are referred to as ‘giant’
PTs and comprise ~20% of all cases (1).
PTs are categorized as benign, borderline, or
malignant based on a combination of histological features,
including stromal cellularity, nuclear abnormalities, mitotic
count, stromal overgrowth, necrosis, heterologous sarcomatous
elements and tumor margins (5).
Th present study describes the case of a 40-year-old
female patient with a rapidly growing, giant, ulcerative malignant
PT. The report follows the CaReL guidelines, and all references
cited were evaluated for relevance (6,7).
Case report
Patient information
A 40-year-old female patient presented to Smart
Health Tower (Sulaymaniyah, Iraq) with a rapidly growing mass in
her left breast for a 2-month duration. She had no significant past
medical or surgical history and no family history of breast cancer.
An analysis of her obstetric history revealed gravida 2, para 2 and
abortion 0. She had a total lactation history of 2 years.
Clinical findings
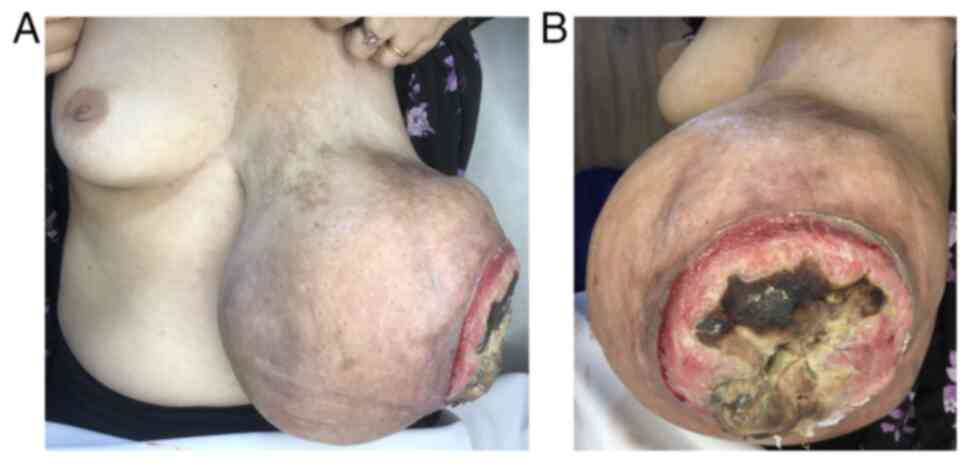
Upon a clinical assessment, the left breast was
found to be markedly enlarged, pendulous and significantly
asymmetrical compared to the right breast, with the lower position
attributed to the weight and extent of the underlying mass.
Palpation revealed a hard, irregular and fixed mass, measuring
~24x20x17 cm occupying the majority of the breast parenchyma.
Centrally, there was a large, well-demarcated ulcerative lesion
measuring ~10-12 cm in diameter. The ulcer surface was necrotic
with areas of black eschar and friable granulation tissue, and a
purulent, foul-smelling discharge, accompanied by zones of active
bleeding. The overlying skin was erythematous, edematous and
indurated, with diffuse discoloration and no evidence of peau
d'orange or satellite lesions. The nipple-areolar complex was
completely obscured and retracted, likely due to the extensive
involvement of the lesion (Fig.
1).
Diagnostic approaches
An ultrasonography of the left breast demonstrated
the marked enlargement and replacement of normal parenchyma by a
large heterogeneous mass with prominent internal vascularity. A
sizable ulceration was identified in the lower outer quadrant,
accompanied by diffuse skin thickening. These findings were highly
suggestive of a locally advanced breast malignancy. An axillary
ultrasound revealed two suspicious lymph nodes (LNs) in level I,
with no abnormal nodes observed in levels II, III, or the
supraclavicular region. The lesion was assigned a Breast Imaging
Reporting and Data System (BI-RADS) category of 5. A mammography of
the right breast demonstrated no architectural distortion,
suspicious mass, or microcalcifications, and was categorized as M1.
Imaging of the left breast could not be obtained due to the
presence of a large, ulcerated mass. A contrast-enhanced computed
tomography (CT) scan of the chest, abdomen and pelvis revealed no
evidence of distant metastasis. A core needle biopsy (CNB) of the
left breast mass revealed a fibroepithelial lesion with stromal
smooth muscle (myoid) differentiation. Fine-needle aspiration of
the left axillary LNs yielded negative results for malignant cells.
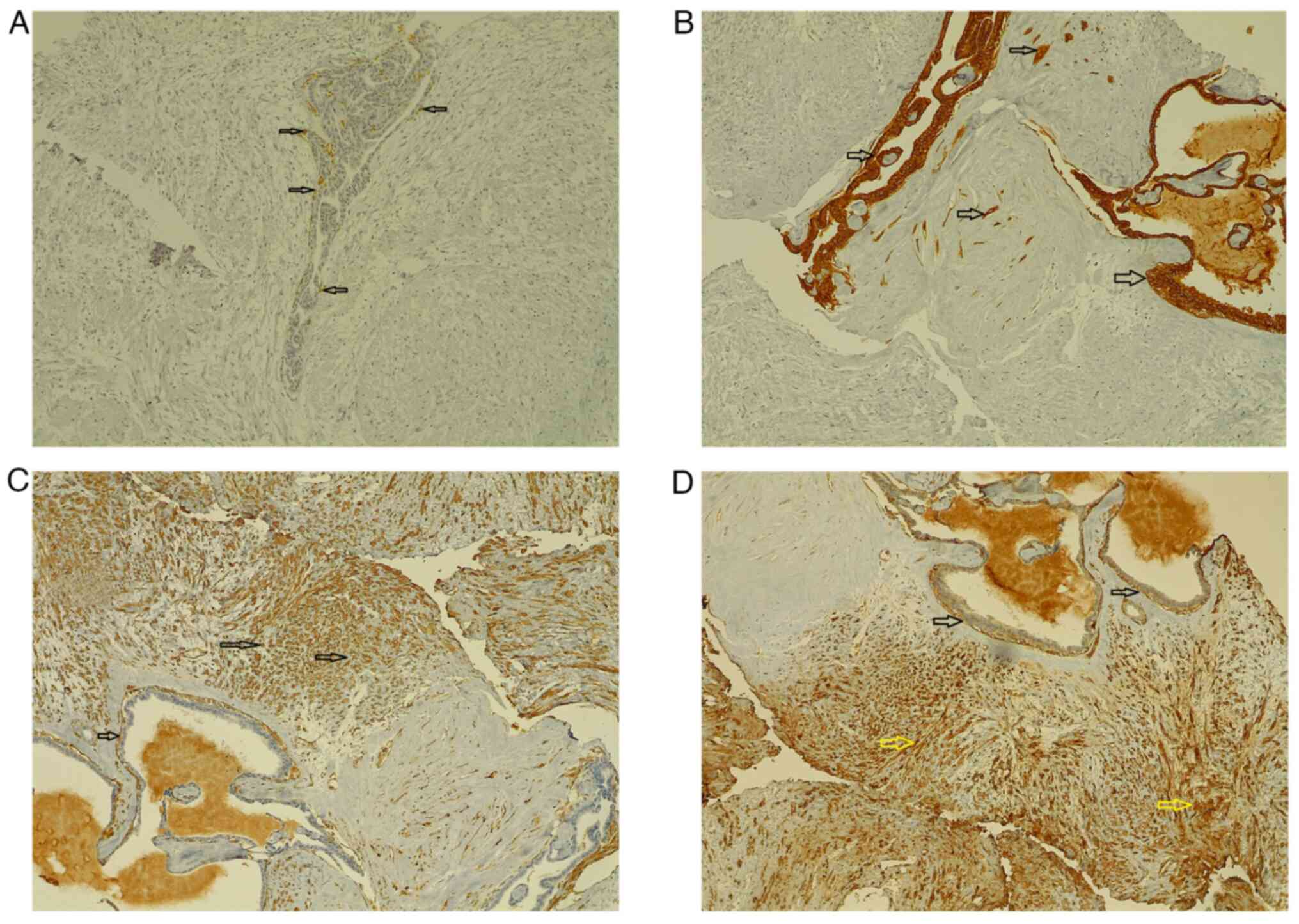
An immunohistochemical analysis was performed. For
immunohistochemical analysis, 4-5 µm-thick sections were cut from
formalin-fixed, paraffin-embedded (FFPE) tissue blocks using a
Sakura Accu-Cut SRM microtome. Permeabilization was not required
since the analyzed targets were membrane and cytoplasmic antigens.
Endogenous peroxidase activity was blocked using hydrogen peroxide
(Dako, Agilent Technologies, Inc.) for 7-10 min at room
temperature. The slides were then incubated with the primary
antibodies for 45 min at room temperature. The secondary antibody
(Dako horseradish peroxidase conjugate) was applied for 45 min at
room temperature, followed by chromogen development with
diaminobenzidine (DAB) for 5-10 min. Counterstaining was performed
using Hematoxylin Gill II (MilliporeSigma) for 2-5 min at room
temperature, then dehydrated through graded alcohols and cleared in
xylene. Imaging was performed using a standard light microscope at
x20 and x40 magnification. p63 staining was negative in both the
ductal and stromal cells, but positive in the myoepithelial cells.
AE1/AE3 was negative in spindle cells and positive in benign ductal
epithelial components. Smooth muscle actin (SMA) and smooth muscle
myosin heavy chain (SMMHC) were both positive in the stromal cells,
exhibiting strong cytoplasmic staining, supporting smooth muscle
differentiation (Fig. 2).
Therapeutic interventions
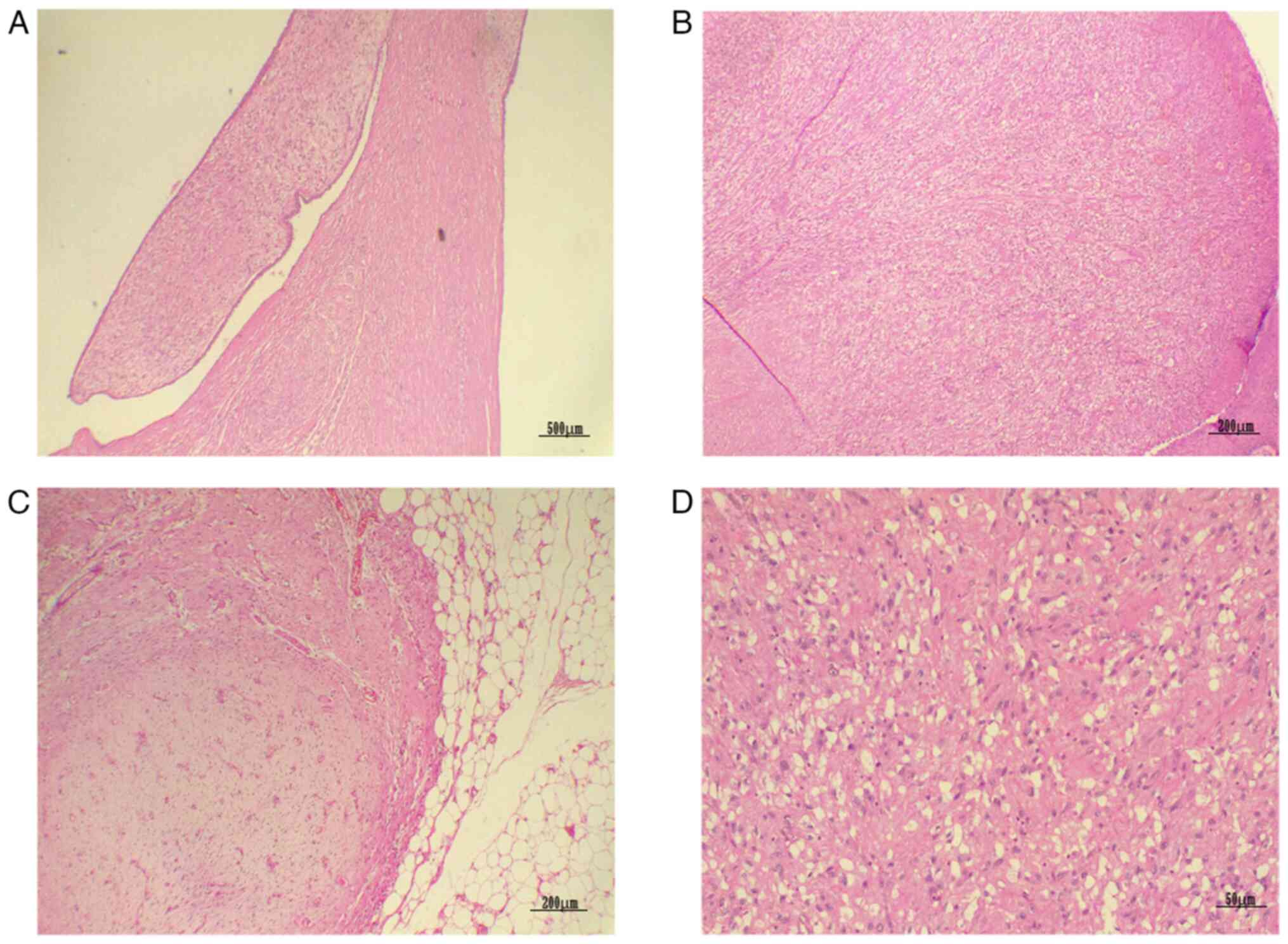
Following a multidisciplinary team discussion, the
decision was made to perform a wide local excision of the left
breast mass. A post-operative histopathological analysis was
performed on 5-µm-thick paraffin-embedded sections. The sections
were fixed in 10% neutral buffered formalin at room temperature for
24 h and then stained with hematoxylin and eosin (H&E; Bio
Optica Co.) for 1-2 min at room temperature. The sections were then
examined under a light microscope (Leica Microsystems GmbH). The
histopathological analysis confirmed the diagnosis of a malignant
PT exhibiting myoid differentiation (Fig. 3). The patient was subsequently
referred to the oncology team for further management and treatment
planning.
Follow-up and outcome
The patient received adjuvant external-beam
radiotherapy to the left breast following initial surgical
excision, using a 3D conformal technique. A total dose of 50 Gy was
delivered in 25 fractions (2 Gy per fraction) over a period of 5
weeks, followed by a tumor-bed boost of 10 Gy in 5 fractions, for a
cumulative dose of 60 Gy. The patient was maintained on regular
follow-up. At the 1-year follow-up, a breast ultrasonography
(images not available) revealed a focal hypoechoic area in the left
breast. A CNB was performed, revealing a fibroepithelial neoplasm
consistent with recurrent PT. Considering the recurrence, the
patient subsequently underwent a modified radical mastectomy. At
the 8-month post-operative follow-up, the patient remained
clinically stable with no evidence of disease recurrence.
Discussion
In the present study, a brief review of the
literature was also performed. A total of seven case reports
(2,5,8-12)
on malignant PTs of the breast were reviewed, published between
2024 and 2025 (Table I). The
patients were all female, with ages ranging from 19 to 73 years.
The majority of the cases (5 out of 7 cases) involved tumors in the
right breast, while 2 cases involved tumors in the left breast.
Tumor sizes varied widely, from 7.5x7x4.5 cm to as large as
55.5x36x50 cm (weighing 18.6 kg). Clinically, all cases presented
with rapid tumor growth. In several cases, rapid growth occurred
after a prolonged period of stable tumor size, with final
accelerated growth durations ranging from one to three months.
BI-RADS categories were reported in 5 cases, typically classified
as BI-RADS 4 or 5. The case in the present study aligns with the
reviewed cases in terms of clinical presentation, demonstrating a
strikingly rapid tumor growth over a short period, expanding to
24x20x17 cm within 2 months. However, it differs in tumor
laterality, arising in the left breast, which was less frequently
affected in the reviewed cases. Additionally, the lesion was
categorized as BI-RADS 5, reinforcing the high radiologic
suspicion, which is consistent with the reviewed cases of malignant
PTs.
 | Table ISummary of seven recently reported
cases of malignant phyllodes tumor. |
Table I
Summary of seven recently reported
cases of malignant phyllodes tumor.
| First author, year of
publication | Age, years/sex | Laterality | Tumor size (cm) | Presentation | Duration | BI-RADS | Treatment | IHC Markers | Metastasis |
Follow-up/outcome | (Refs.) |
|---|
| Ahmadi, 2025 | 19/F | Right | 24x12x7 | Rapid growth,
ulceration, bleeding | ~2 months of rapid
growth after stable years | BI-RADS 4 | Total right
mastectomy | Not reported | None | No adjuvant therapy,
close follow-up, no recurrence reported | (8) |
| Murcia, 2025 | 53/F | Right | 23x22x28 | Large, rapidly
growing mass | Rapid growth over the
past 2 months (present ~1 year) | BI-RADS 5 | Right mastectomy | Not reported | None | No detailed follow-up
given | (9) |
| Rumyantseva,
2025 | 73/F | Left | 25 | Large painless mass,
lymphadenopathy | Progressive growth
(duration not fully detailed) | Not reported | Excision with 1 cm
margin | Not reported | Regional
lymphadenopathy (possible reactive; exact status not fully
detailed) | Outcome not fully
detailed | (2) |
| Dong, 2024 | 48/F | Right | 25x10 | Rapid post-COVID
growth, ulceration, and anemia | Rapid growth in 3
months (stable for 6 years) | BI-RADS 4b | Modified radical
mastectomy | Not reported | None | No adjuvant therapy,
no recurrence at 9 months | (10) |
| Haddad (2024) | 24/F | Right | 7.5x7x4.5 | Rapid growth, pain,
and skin suffering | ~2 months of rapid
pro gressive growth | BI-RADS 4 | Partial mastectomy +
axillary dissection | Not reported | None | Adjuvant chemo- and
radiotherapy, no metastasis | (5) |
| Kaiser, 2024 | 66/F | Left | 55.5x36x50 | Giant mass, bleeding,
anemia, metastases | Rapid massive growth
in 1 month (after 5 years of neglect) | Not reported | Radical mastectomy,
chemo, radiotherapy | Not reported | Lung, brain, and bone
metastases | Stable disease at 18
months despite brain and bone metastasis | (11) |
| Vicentini, 2024 | 29/F | Right | 10x8x8 | Ulcerated mass,
axillary node metastasis | Mass since age 9,
rapid increase over 2 months | Not reported | Modified radical
mastectomy + axillary dissection | Positive P53, P63,
β-catenin; Ki-67 high (50%) | Axillary lymphnode
metastasis, lung nodules suspicious | Recurrence at 56
days, died at 6 months | (12) |
In patients with a large malignant PT, the rapid
growth of the tumor can cause varicose veins to appear on the
surface of the skin. This can result in poor blood circulation,
leading to tissue death, infection and the development of skin
ulcers. When the tumor or associated blood vessels rupture,
bleeding may occur. A malignant PT is also often accompanied by
systemic symptoms, such as anemia and severe weight loss, which may
be caused by the metabolic demands of the tumor, infections, or
bleeding (10). In advanced cases,
patients may develop cachexia, a condition that can lead to
multi-organ failure. Dong et al (10) reported a case in which the tumor of
the patient became enlarged rapidly and prominently, with surface
varicosities, bleeding and infection. The patient in their study
also exhibited signs of poor appetite, marked weight loss and
anemia (10). Similarly, the case
described herein presented with a large, ulcerated area containing
necrotic, foul-smelling tissue and active bleeding, features that
are characteristic of an aggressive malignant PT and their tendency
to cause skin breakdown due to pressure-induced necrosis.
Identifying the subtype of PTs is crucial, as it
helps predict the clinical course of the tumor: Benign forms may
recur locally, borderline types can also recur with a minimal risk
of metastasis, while malignant tumors carry a higher likelihood of
spreading (12). Mammography and
color Doppler ultrasound are the primary imaging modalities used
for evaluating PT. However, in the early stages, both techniques
often lack specific findings that clearly indicate the presence of
PT (10). In the case in the
present study, an ultrasonography revealed a large, heterogeneous
mass with internal blood flow and diffuse thickening of the skin,
features such as those reported by in the study by Murcia et
al (9), who observed that PTs
can resemble fibroadenomas and often lack distinctive imaging
characteristics to differentiate benign from malignant forms. In
the present study, a mammography could not be performed on the
affected breast due to the extensive size of the mass and the
presence of surface ulceration, an imaging limitation frequently
encountered in advanced tumors. A comparable situation was
described by Kaiser et al (11), where a PT had expanded to 55 cm.
These limitations in imaging underscore the importance of
histological examination for definitive diagnosis (11).
A definitive diagnosis of PTs requires a CNB, which
reveals characteristic histological features, including a leaf-like
architecture formed by stromal overgrowth that projects into
papillary structures resembling leaf blades (9). Fine needle aspiration has also been
considered a useful preoperative tool for diagnosing PTs.
Cytological findings typically include fibromyxoid stromal
fragments rich in spindle cells, along with clusters or sheets of
benign ductal epithelial cells without atypia, often accompanied by
myoepithelial cells (1). In the
case in the present study, CNB identified a fibroepithelial lesion
with stromal myoid differentiation, which raised the possibility of
a PT. Distinguishing PT from other fibroepithelial tumors, such as
fibroadenomas or metaplastic carcinoma, can be challenging before
surgery, as noted by Haddad et al (5). Immunohistochemical analysis was
essential in confirming the diagnosis in the present case. p63
staining was negative in both the ductal and stromal cells, but
remained positive in the myoepithelial cells. AE1/AE3 was positive
in the benign ductal epithelial components and negative in the
stromal cells. In contrast, the stromal cells showed strong,
diffuse cytoplasmic staining for SMA and SMMHC, supporting smooth
muscle differentiation (Fig. 2).
These findings are consistent with those reported by Lissidini
et al (1) (2022) and Haddad
et al (5), who emphasized
the critical role of immunohistochemistry in determining stromal
cell lineage and distinguishing malignant PTs from metaplastic
carcinomas, particularly in cases with prominent spindle cell
features.
Current management strategies for PTs reveal a lack
of consensus and limited evidence-based guidelines, particularly as
regards the optimal surgical margins required to achieve complete
excision and reduce the likelihood of recurrence. Traditionally,
treatment has involved wide local excision with margins >1 cm,
with tumor size often influencing the decision to proceed with
mastectomy. Malignant PTs are known for their aggressive nature,
with a high risk of local recurrence and potential for metastasis
to the lungs, bones and LNs. However, emerging data suggest that
margins <1 cm may be adequate for effective tumor removal,
potentially making breast-conserving surgery a viable option in
selected cases (8). In the case
presented herein, the patient underwent wide local excision. This
treatment approach is consistent with the current literature, which
emphasizes that complete surgical resection with negative margins
remains the primary method for managing malignant PTs. As
highlighted by Lissidini et al (1) and Haddad et al (5), the most critical factor influencing
local recurrence is the adequacy of surgical margins, with a
general recommendation of at least 1 cm. Due to the elevated risk
of recurrence, adjuvant radiotherapy was administered following the
initial excision. This decision aligns with findings from the study
by Kaiser et al (11), who
underscored the importance of radiotherapy in enhancing local
disease control, particularly for large or marginally resectable
tumors.
Despite initial aggressive local treatment, the
patient in the present study experienced a recurrence within 1
year, identified through follow-up imaging and confirmed by CNB.
Recurrence in malignant PTs is relatively common, with reported
rates as high as 30%, particularly in cases with inadequate
surgical margins or tumors characterized by high mitotic activity
and stromal overgrowth, as documented by Lissidini et al
(1) and Dong et al
(10). Given the recurrence, the
patient underwent a modified radical mastectomy, a more extensive
procedure involving the removal of the breast along with regional
LNs. While axillary LN metastasis in malignant PTs is uncommon, as
noted by Vicentini et al (12), LN dissection may be warranted in
select cases with clinically suspicious nodes. In the case in the
present study, a lymphadenectomy was performed due to suspicious
findings, but no LN metastases were identified on the
histopathological examination.
The present case report is distinguished by the rare
coexistence of extensive ulceration, recurrence following wide
local excision with adjuvant radiotherapy, and stromal myoid
differentiation within a giant malignant phyllodes tumor. These
uncommon features occurring together make the case a valuable
addition to the limited literature on the biological variability
and aggressive behavior of malignant phyllodes tumors. In
conclusion, the diagnosis and management of malignant PTs can be
challenging due to their rarity and unpredictable clinical
behavior. Even with aggressive treatment, these tumors carry a
significant risk of recurrence, highlighting the importance of
vigilant clinical follow-up and multidisciplinary care.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
FHK and LRAP were major contributors to the
conception of the study, as well as to the literature search for
related studies. AMS, SLT, HAN and MKA contributed to the clinical
management of the patient, assisted with data acquisition and
interpretation, and participated in the literature review and
manuscript preparation. ROM, HOB and SHH contributed to the
conception and design of the study, the literature review, the
critical revision of the manuscript, and the processing of the
table. SOA was the radiologist who assessed the case. AMA was the
pathologist who performed the diagnosis of the case. FHK and AMS
confirm the authenticity of all the raw data. All authors have read
and approved the final manuscript.
Ethics approval and consent to
participate
Written informed consent was obtained from the
patient for her participation in the present study.
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of the present case report and any
accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Lissidini G, Mulè A, Santoro A, Papa G,
Nicosia L, Cassano E, Ashoor AA, Veronesi P, Pantanowitz L, Hornick
JL and Rossi ED: Malignant phyllodes tumor of the breast: A
systematic review. Pathologica. 114:111–121. 2022.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Rumyantseva V, Slepukhova D, Sukhotko A,
Ankin A, Bumbu A and Covantsev S: Malignant phyllodes tumor
management-a case report. Acad J Health Sci. 40:75–79. 2025.
|
|
3
|
Müller J: On the finer structure and the
forms of morbid tumors. Berlin Gedruckt und verlegt bei, 1838.
|
|
4
|
Lee BJ and Pack GT: Giant intracanalicular
myxoma of the breast. Ann Surg. 93:250–268. 1931.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Haddad CF, de Oliveira Paiva AC, de Souza
Silva JP and Rodrigues IT: Malignant phyllodes tumor of the breast
in a young patient-case report. Mastology. 34(e20220043)2024.
|
|
6
|
Prasad S, Nassar M, Azzam AY,
García-Muro-San José F, Jamee M, Sliman RK, Evola G, Mustafa AM,
Abdullah HO, Abdalla AB, et al: CaReL Guidelines: A consensus-based
guideline on case reports and literature review (CaReL). Barw Med
J. 2:13–19. 2024.
|
|
7
|
Abdullah HO, Abdalla BA, Kakamad FH, Ahmed
JO, Baba HO, Nasih M, Bapir R, Rahim HM, Omar D, Kakamad SH, et al:
Predatory publishing lists: A review on the ongoing battle against
fraudulent actions. Barw Med J. 2:26–30. 2024.
|
|
8
|
Ahmadi N, Sajdlowska J, Shenasan P, Veltri
J and Moulayes N: Case report: Rapid growth of malignant phyllodes
tumor. J Surg Case Rep. 2025(rjaf082)2025.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Murcia DK, Tenreiro A, Kohlnhofer JA,
Wagner C and Monetto FP: Giant malignant phyllodes tumor: A case
report. Radiol Case Rep. 20:3719–3723. 2025.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Dong X, Song D, Ma J, Sun J and Wang X:
Massive malignant phyllodes tumor accompanied by anemia and
ulceration in the breast: A case report. Clin Case Rep.
12(e9096)2024.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Kaiser C, Abramian AV and Faridi A:
Surgical management and system therapy of the most giant known
malignant metastatic breast phyllodes tumor: A case report and
review of the literature. Oncol Res Treat. 47:145–148.
2024.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Vicentini G, Linhares JC, Borsari G and
Linhares HZ: Malignant phyllodes tumor of the breast with lymph
node metastasis: A case report. Mastology. 34(e20230008)2024.
|