Introduction
The prevalence of urinary incontinence increases
with age, markedly affecting daily activities, such as working,
traveling, physical exercise and sexual function, ultimately
reducing quality of life (1,2). The
International Continence Society (ICS) defines urinary incontinence
as the involuntary leakage of urine (3). Urinary incontinence caused by
diabetes mellitus is closely related to neuropathy and detrusor
myopathy, where prolonged hyperglycemia damages the nerves
innervating the bladder and sphincter, reduces bladder contractions
and leads to abnormal detrusor function, impairing urinary function
(4).
According to Liu et al (1), individuals with blood glucose levels
>92 mg/dl and glycated hemoglobin (HbA1c) levels ≥6.5%
experience an increased severity of stress urinary incontinence and
urgency urinary incontinence. Good glycemic control, with blood
glucose levels <86 mg/dl and HbA1c levels <5.7%, may reduce
the incidence of urinary incontinence (1). A recent study found that diabetic
patients had an increased bladder wall thickness due to diabetic
neuropathy, which forces the bladder muscles to work harder to
expel urine, leading to trabeculation. This process weakens bladder
contractions and ultimately results in urinary incontinence
(5).
However, there are limited studies available
investigating the association between random blood glucose (RBG)
and HbA1c levels with urinary incontinence in the elderly,
particularly in Asian populations (6,7).
Therefore, the present study aimed to examine the association
between RBG and HbA1c levels and the severity of urinary
incontinence using the International Consultant Incontinence
Questionnaire-Urinary Incontinence Short Form (ICIQ-UISF) in
elderly individuals (8).
Patients and methods
Study design and study
participants
During the period between August, 2024 and October,
2024, research data were collected from the medical records of
elderly respondents aged ≥60 years who sought treatment at the
Department of Urology or the Department of Internal Medicine of
Prof. Dr. Chairuddin P. Lubis Hospital, located in Medan, North
Sumatra, Indonesia. This hospital is a public university-affiliated
hospital and serves as a referral center for urological and
internal medicine cases, across Medan city and its surrounding
regions.
The present study was designed as an observational,
cross-sectional, correlation-based study and was conducted in
accordance with the ethical principles of the Health Research
Ethics Committee of Universitas Sumatera Utara, Medan, Indonesia.
At the Department of Urology, elderly patients aged ≥60 years who
had been diagnosed with urinary incontinence were selected, while
at the Department of Internal Medicine, elderly patients aged ≥60
years with a history of type 2 diabetes mellitus were included. To
minimize selection bias, patients who had received prior treatment
for urinary incontinence, patients with a history of smoking, heart
failure medication use, neurological disorders, urinary tract
problems, or constipation were excluded from the study. Respondents
who met the inclusion criteria were contacted via telephone to
directly administer the ICIQ-UISF form to determine the presence of
urinary incontinence and to assess the severity of their
condition.
In the present study, the study sample was obtained
using a non-probability sampling method, specifically consecutive
sampling. Consecutive sampling involves including all subjects who
met the inclusion criteria at Prof. Dr. Chairuddin P. Lubis
Hospital until the required sample size was achieved. The sample
size was calculated using Slovin's formula, resulting in a total of
100 research subjects with a 95% confidence interval and a 5%
margin of error. While this sample size was relatively small for a
correlation study, it was deemed appropriate based on practical
considerations and the study's methodological framework.
RBG and HbA1c levels were obtained directly from the
medical records of the patients. These laboratory results were
collected as part of routine clinical assessments at Prof. Dr.
Chairuddin P. Lubis Hospital and were not self-reported. Blood
glucose levels were measured using standardized biochemical assays
in the laboratory of the hospital to ensure accuracy and
reliability.
ICIQ-UISF
The questions that were asked over the telephone to
the respondents are listed in Table
I. There were a total of four questions, of which the first
three questions had scores, and those were calculated to assess
whether the respondent experiences urinary incontinence and to
evaluate the severity. Moreover, the fourth question was used to
determine the timing of urinary leakage or the type of incontinence
the respondent is experiencing.
 | Table IInternational Consultant Incontinence
Questionnaire-Urinary Incontinence Short Form (ICIQ-UISF) (6). |
Table I
International Consultant Incontinence
Questionnaire-Urinary Incontinence Short Form (ICIQ-UISF) (6).
| Question | Frequency | Score |
|---|
| How often do you leak
urine? | Never | 0 |
| | About once a week or
less often | 1 |
| | Two or three times a
week | 2 |
| | About once a day | 3 |
| | Several times a
day | 4 |
| | All the time | 5 |
| How much urine do you
usually leak? | None | 0 |
| | A small amount | 2 |
| | A moderate
amount | 4 |
| | A large amount | 6 |
| Overall, how much
does leaking urine interfere with your everyday life? Please answer
a number between 0 (not at all) and 10 (a great deal) | 0 | 0 |
| | 1 | 1 |
| | 2 | 2 |
| | 3 | 3 |
| | 4 | 4 |
| | 5 | 5 |
| | 6 | 6 |
| | 7 | 7 |
| | 8 | 8 |
| | 9 | 9 |
| | 10 | 10 |
| When does urine
leak? | Never | |
| | Leaks before you can
get to the toilet | |
| | Leaks when you cough
or sneeze | |
| | Leaks when you are
sleep | |
| | Leaks when you have
finished urinating and are dressed | |
| | Leaks for no obvious
reason | |
| | Total score | |
Statistical analysis
All statistical analyses were conducted using IBM
SPSS Statistics version 24.0 (IBM Corp.). The Kolmogorov-Smirnov
test was used to assess the normality of continuous variables,
including RBG, HbA1c, urinary incontinence scores, and age if none
of the variables were normally distributed; therefore, continuous
data are presented as the median and interquartile range (IQR).
Categorical variables, such as the severity of urinary incontinence
and response distributions from the ICIQ-UISF questionnaire, are
expressed as frequencies and percentages. The strength and
direction of the association between RBG, HbA1c, age and the
severity of urinary incontinence (ICIQ-UISF score) were assessed
using Spearman's rank correlation coefficient (ρ). Correlation
coefficients were interpreted as weak (ρ<0.30), moderate (ρ≥0.30
and ρ<0.60), or strong (ρ≥0.60). A P-value <0.05 was
considered to indicate a statistically significant difference.
Results
Distribution of the characteristics of
the study respondents
The research results obtained from 100 respondents
are presented in Table II. It was
found that the majority of respondents experienced symptoms of
urinary incontinence, with a percentage of 82%, while those who did
not experience urinary incontinence accounted for 18%.
 | Table IIDistribution of respondent
characteristics. |
Table II
Distribution of respondent
characteristics.
| Variable | No. of
respondents | Percentage |
|---|
| ICIQ-UISF scores | | |
|
No urinary
incontinence | 18 | 18 |
|
Mild | 12 | 12 |
|
Moderate | 24 | 24 |
|
Severe | 36 | 36 |
|
Very
severe | 10 | 10 |
|
Median
(IQR) | 10.50
(4.00-16.75) |
| Random blood sugar
(RBG) | | |
|
Diabetes
(RBG ≥200 mg/dl) | 100 | 100 |
|
Median
(IQR) | 274.00
(245.25-333.00) |
| HbA1c | | |
|
Diabetes
(HbA1c ≥6.5% ) | 100 | 100 |
|
Median
(IQR) | 8.50
(7.30-10.88) |
| Age | | |
|
Young-old
(60-74 years) | 88 | 88 |
|
Old (75-90
years) | 12 | 12 |
|
Oldest-old
(>90 years) | 0 | 0 |
|
Median
(IQR) | 66.00
(63.00-69.75) |
Furthermore, from the 100 respondents whose urinary
incontinence severity was measured using the ICIQ-UISF scores,
those with severe urinary incontinence ranked the highest with a
percentage of 36%, followed by those with a moderate degree of
incontinence at 24%. Those without urinary incontinence accounted
for 18%, while those with mild urinary incontinence accounted for
12%, and those with very severe urinary incontinence accounted for
10% of the study participants.
The majority of the respondents in the present study
were in the young-old age group (60-74 years), comprising 88%. This
was followed by the old age group (75-90 years) at 12%; no
respondents were found in the oldest-old age group (>90
years).
Based on the normality test results, none of the
variables followed a normal distribution. Therefore, for the
distribution table, RBG, HbA1c, urinary incontinence score and age
are reported as the median and IQR.
ICIQ-UISF scores of the study
respondents
The distribution of the answers of the respondents
to the questions in the ICIQ-UISF are presented in Table III. These were as follows:
 | Table IIIDistribution of International
Consultant Incontinence Questionnaire-Urinary Incontinence Short
Form (ICIQ-UISF) question scores. |
Table III
Distribution of International
Consultant Incontinence Questionnaire-Urinary Incontinence Short
Form (ICIQ-UISF) question scores.
| | | | Respondents |
|---|
| No | Question | Frequency | No. of
respondents | % |
|---|
| 1 | How often do you leak
urine? | Never | 18 | 18 |
| | | About once a week or
less often | 37 | 37 |
| | | Two or three times
a week | 16 | 16 |
| | | About once a
day | 1 | 1 |
| | | Several times a
day | 3 | 3 |
| | | All the time | 25 | 25 |
| 2 | How much urine do
you usually leak? | None | 18 | 18 |
| | | A small amount | 55 | 55 |
| | | A moderate
amount | 10 | 10 |
| | | A large amount | 17 | 17 |
| 3 | Overall, how much
does leaking urine interfere with your everyday life? Please answer
a number between 0 (not at all) and 10 (a great deal) | 0 | 18 | 18 |
| | | 1 | 21 | 21 |
| | | 2 | 3 | 3 |
| | | 3 | 2 | 2 |
| | | 4 | 0 | 0 |
| | | 5 | 14 | 14 |
| | | 6 | 0 | 0 |
| | | 7 | 2 | 2 |
| | | 8 | 4 | 4 |
| | | 9 | 0 | 0 |
| | | 10 | 36 | 36 |
| 4 | When does urine
leak? | Never | 18 | 18 |
| | | Leaks before you
can get to the toilet | 10 | 10 |
| | | Leaks when you
cough or sneeze | 20 | 20 |
| | | Leaks when you are
sleep | 3 | 3 |
| | | Leaks when you have
finished urinating and are dressed | 32 | 32 |
| | | Leaks for no
obvious reason | 17 | 17 |
Question 1, frequency of urinary leakage: The
majority of the respondents experienced episodes of urinary leakage
with varying frequencies. A total of 37% of the respondents
reported leaking urine once a week or less often, followed by 25%
who experienced continuous leakage. Additionally, 18% of the
respondents reported no urinary incontinence, 16% experienced
leakage two or three times a week, 3% several times a day, and 1%
once a day.
Question 2, volume of urine leaked during urinary
incontinence: The majority of the respondents (55%) reported a
small amount of urine leakage, followed by 18% who did not
experience urinary incontinence, 17% who reported a large amount,
and 10% who reported a moderate amount.
Question 3, impact on quality of life: The
assessment of the impact of urinary incontinence on quality of life
varied among respondents. The majority (36%) had a score of 10,
followed by 21% with a score of 1, and 18% who reported no urinary
incontinence. Other responses included 14% with a score of 5, 4%
with a score of 8, 3% with a score of 2, and 2% each for scores 3
and 7. No respondents gave scores of 4, 6, or 9.
Question 4, timing of urinary leakage: The majority
of the respondents (32%) reported experiencing urinary leakage
after urinating and dressing, followed by 20% who experienced
leakage while coughing or sneezing. Additionally, 18% reported no
urinary incontinence, 17% experienced leakage without any obvious
reason, 10% leaked before reaching the toilet, and 3% experienced
leakage while sleeping.
Severity of urinary incontinence
As demonstrated in Table IV, out of the 100 respondents
tested, 18% did not experience urinary incontinence, followed by
those with mild incontinence (12%), moderate incontinence (24%),
severe incontinence (36%), and the remaining respondents
experiencing very severe incontinence (10%). The median urinary
incontinence score was 10.50, suggesting that, on average, patients
experienced a moderate level of urinary incontinence.
 | Table IVProportion of ICIQ-UISF among the
participants. |
Table IV
Proportion of ICIQ-UISF among the
participants.
| | ICIQ-UISF (no. of
participants) | |
|---|
| | No urinary
incontinence | Mild | Moderate | Severe | Very severe | Total |
|---|
| Diabetic
patients | 18 | 12 | 24 | 36 | 10 | 100 |
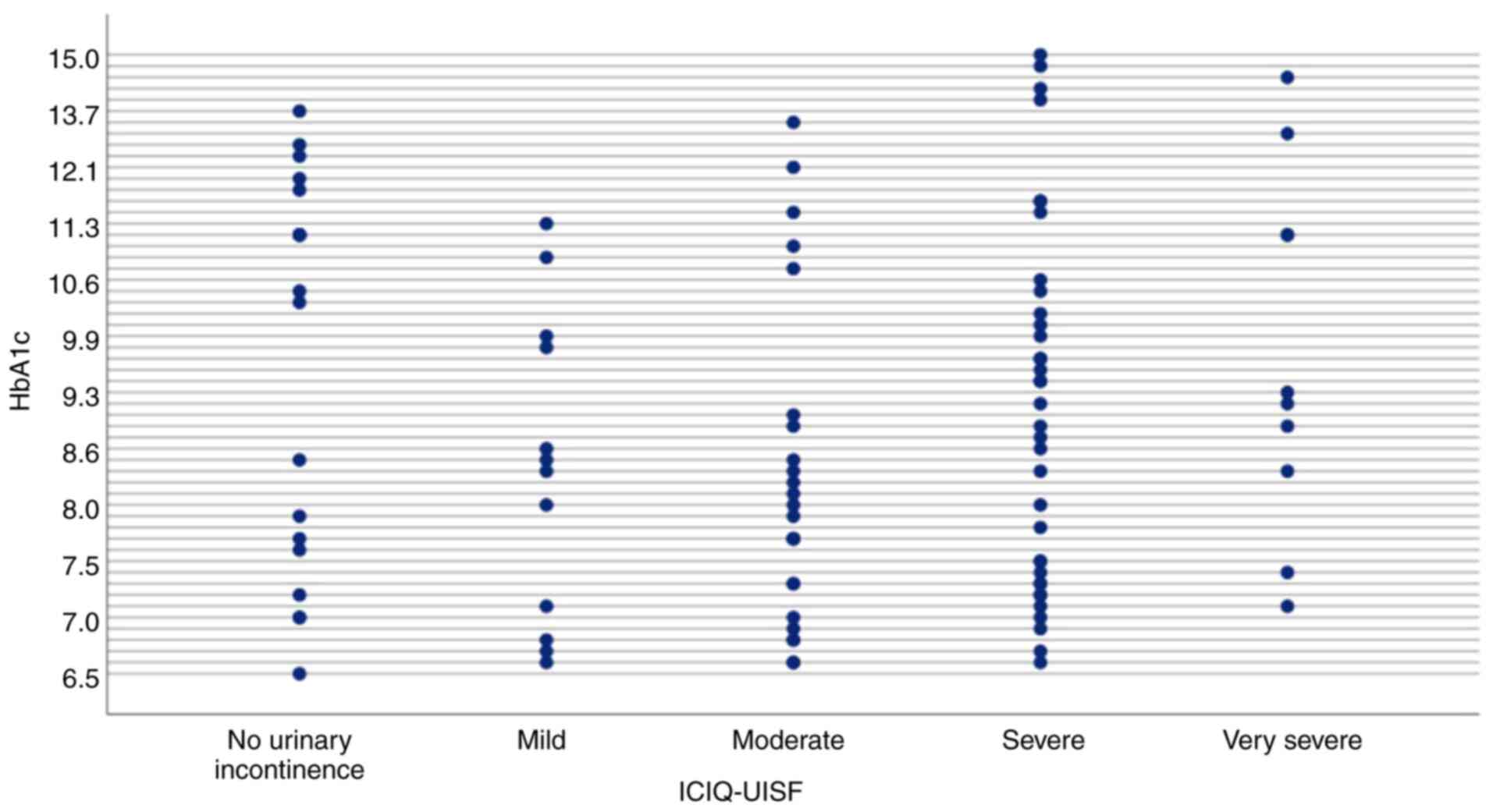
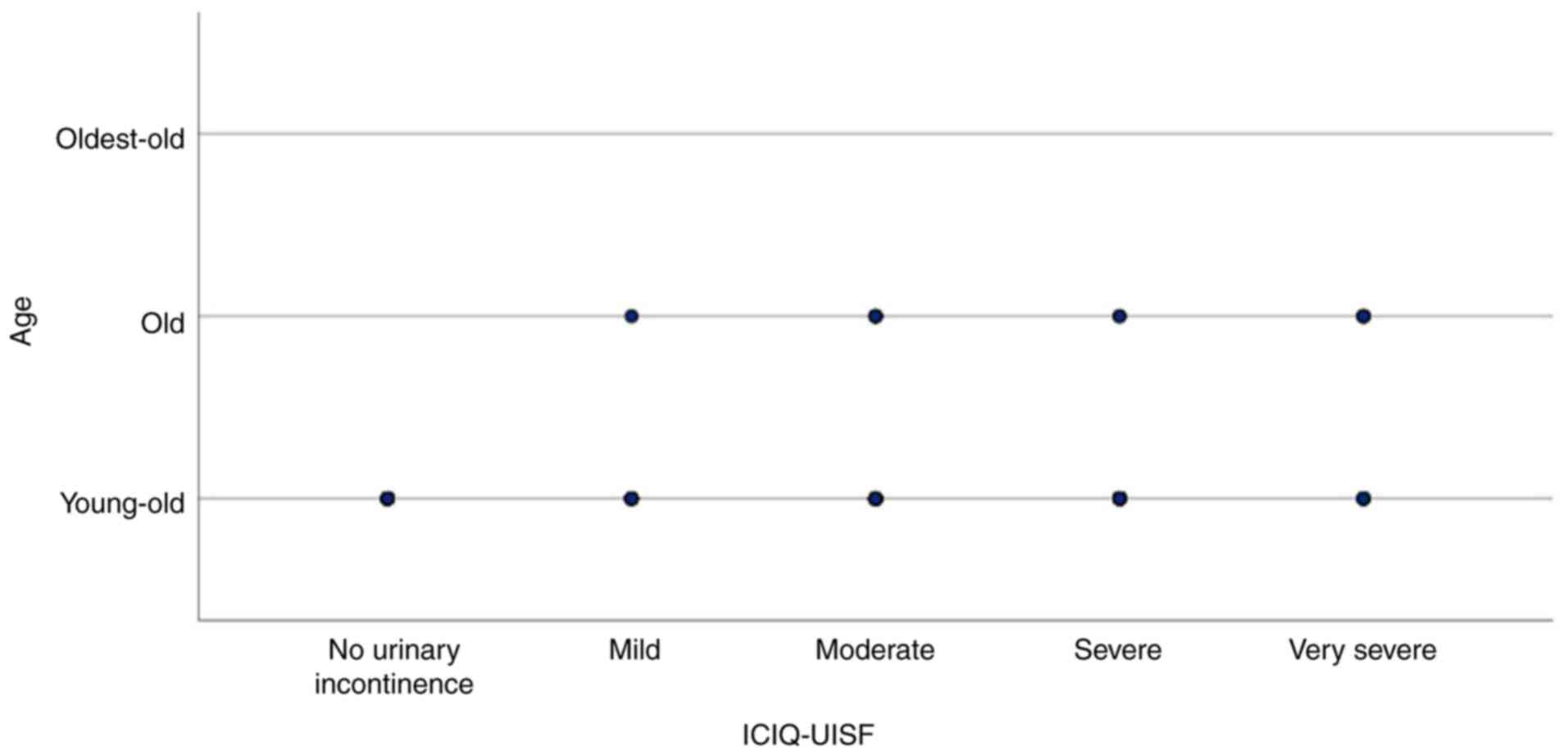
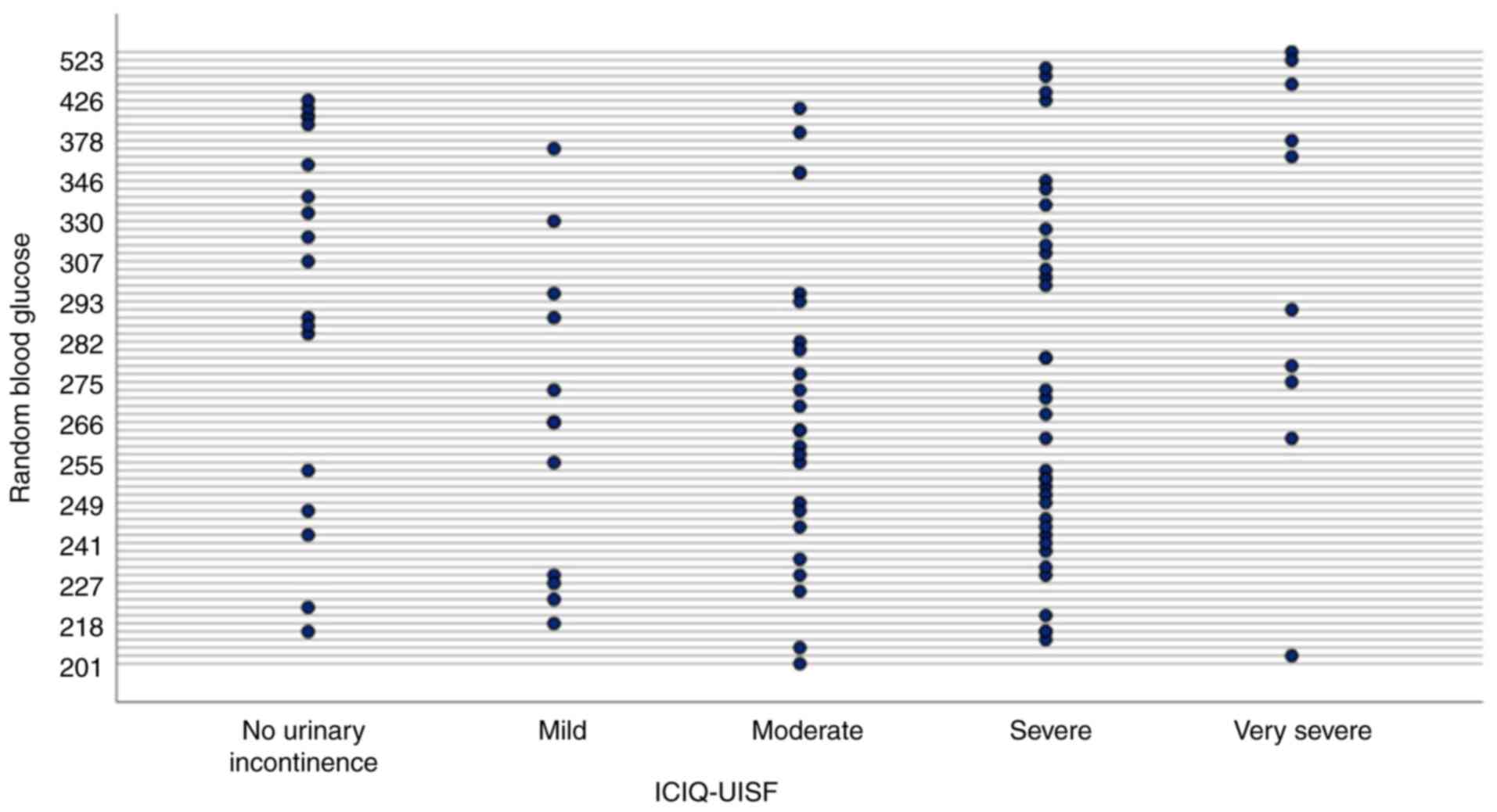
Correlation between the ICIQ-UISF
score and independent variables
The results of the correlation analysis between the
ICIQ-UISF score and three independent variables (RBG, HbA1c levels
and age) are presented in Table V
and Fig. 1, Fig. 2 and Fig. 3. Spearman's correlation analysis
revealed a very weak negative correlation between RBG levels and
the urinary incontinence score (ρ=-0.016, P=0.877), which was not
statistically significant (P>0.05), indicating no meaningful
association (Table V and Fig. 3). Similarly, the HbA1c levels
exhibited a weak positive correlation with the urinary incontinence
score (ρ=0.047, P=0.641), although this correlation was also not
significant (P>0.05), suggesting no substantial link (Table V and Fig. 1). By contrast, age exhibited a
weak, yet statistically significant positive correlation with the
urinary incontinence score (ρ=0.242, P=0.015; Table V and Fig. 2), suggesting that older individuals
tend to experience higher urinary incontinence scores. Although the
correlation is modest, it suggests that age-related factors may
contribute to the severity of urinary incontinence.
 | Table VCorrelation between ICIQ-UISF scores
and independent variables. |
Table V
Correlation between ICIQ-UISF scores
and independent variables.
| Variable | Spearman's ρ | P-value |
|---|
| RBG (mg/dl) | -0.016 | 0.877 |
| HbA1C (%) | +0.047 | 0.641 |
| Age (years) | +0.242 | 0.015a |
Discussion
The present study found no significant association
between HbA1c levels and urinary incontinence, consistent with the
findings in the study by Lee et al (6), which examined 6,026 diabetic women
and found no significant association between HbA1c levels and
urinary incontinence. However, HbA1c levels ≥9% were associated
with greater limitations in daily activities among individuals
already experiencing urinary incontinence compared to those with
HbA1c levels <6%. This suggests that poor glycemic control
worsens the impact of urinary incontinence on quality of life
rather than increasing its risk (9).
Similarly, a study in Turkey found no significant
differences in HbA1c levels between individuals with and without
urinary incontinence. Instead, factors such as body mass index and
medication use were stronger predictors (10). This supports the notion that
urinary incontinence is multifactorial, involving metabolic,
hormonal and mechanical factors. Furthermore, HbA1c reflects
glycemic control over the past 3 months, but may not capture
long-term diabetes effects.
Age is a key risk factor for prediabetes and type 2
diabetes mellitus, both of which increase urinary incontinence
severity (5). In the present
study, a weak, yet statistically significant positive correlation
was observed between age and ICIQ-UISF scores, suggesting that
urinary incontinence severity may worsen with age, albeit modestly.
Aging-related physiological changes, such as reduced bladder
capacity, weakened pelvic floor muscles and impaired neurological
control, contribute to an increased severity of urinary
incontinence. However, older adults may be underrepresented in
healthcare assessments. Previous research suggests that physical
limitations, transportation challenges and caregiver dependence
reduce healthcare utilization (11). Goodwin et al (12) found that older individuals were
less likely to seek routine medical care due to mobility
restrictions and declining overall health, which may contribute to
variations in incontinence severity across different age groups in
clinical settings.
The present study also found no significant
association between RBG levels and urinary incontinence. A similar
study by Tambunan et al (13) reported only a weak positive
correlation and suggested that RBG does not adequately represent
diabetes duration or long-term glycemic control. Additionally,
other contributing factors likely play a more prominent role in
urinary incontinence. The same study noted that RBG accounted for
only 8% of ICIQ-UISF scores, while the remaining 92% was influenced
by other unexamined variables (10). Age, sex, obesity, pregnancy and
neurological disorders have also been identified as key
contributors to urinary incontinence prevalence. Lifestyle habits,
such as smoking and alcohol consumption were also found to
exacerbate the condition (14).
These findings reinforce that urinary incontinence results from
multiple interacting factors, rather than diabetes alone.
Glycemic variability, referring to fluctuations in
blood glucose over short and long periods, may have influenced the
results of the present study. Previous research highlights the
duration of diabetes as a crucial factor in glucose fluctuations,
which can impact urinary incontinence severity. Individuals with a
shorter duration of diabetes often experience daily glucose
fluctuations, whereas those with a longer disease duration exhibit
more stable glucose levels due to physiological adaptations over
weeks or months (15).
This may explain why RBG and HbA1c levels did not
consistently correlate with urinary incontinence severity as
assessed by the ICIQ-UISF in the present study. HbA1c, which
measures glycemic control over 3 months, may not be sufficiently
sensitive to detect short-term glucose fluctuations that more
immediately affect incontinence symptoms. Likewise, RBG, a
single-point measurement, does not capture long-term glycemic
trends. Therefore, undetected glucose fluctuations, not reflected
by HbA1c or RBG, may contribute to inconsistencies in the
association between diabetes and urinary incontinence.
The present study had certain limitations which
should be mentioned. First, the cross-sectional design prevents the
establishment of causal associations between glycemic control, age
and urinary incontinence severity. Second, the study was conducted
in a specific population, which may limit the generalizability of
the findings. In addition, potential biases of the present study
include the following: i) Selection bias: Participants were
recruited from a clinical setting, possibly excluding individuals
with urinary incontinence who did not seek medical care, leading to
an underestimation of its true prevalence. ii) Information bias:
The assessment of urinary incontinence severity relied on
self-reported ICIQ-UISF scores, which may introduce subjective
variability in responses. iii) Recall bias: Participants may have
inaccurately reported the onset or severity of their symptoms,
particularly in older individuals with cognitive decline, affecting
data accuracy. Further studies with larger, more diverse
populations are thus required to incorporate objective measures to
minimize bias and enhance reliability.
In conclusion, the present study found a weak but
significant association between age and urinary incontinence
severity, while no significant associations were observed with
HbA1c or RBG levels. These findings suggest that urinary
incontinence is influenced by multiple factors beyond glycemic
control. Future research is required to explore the role of
glycemic variability and other metabolic factors in the severity of
urinary incontinence.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
SS, SMW and MAM conceptualized the study. SS, SMW,
NSA and MAM were involved in data curation. SMW, MSS and MAM were
involved in the formal analysis.: SS, SMW and MAM were involved in
the investigative aspects of the study. SMW, MSS and NSA were
involved in the study methodology. SS, SMW and NSA were involved in
project administration. SMW, MSS and NSA provided all questionnaire
materials obtained from the official International Consultation on
Incontinence Questionnaire (ICIQ) resource website (https://iciq.net). The ICIQ-UISF form was processed
and scored by SS and MAM using standard spreadsheet software
(Microsoft Excel 2019) without any additional statistical plug-ins.
SMW, MSS and NSA supervised the study. SMW and MAM were involved in
data validation. SS, SMW and MSS were involved in visualization.
SMW, MSS and MAM were involved in the writing of the original draft
of the manuscript. SS, SMW and MAM were involved in the writing,
reviewing, and editing of the manuscript. All authors have read,
critically reviewed, and approved the final version of the
manuscript, and each author accepts responsibility for the
integrity and accuracy of the work as a whole. All authors
contributed to the study design, data collection, and manuscript
preparation. SMW and MAM confirm the authenticity of all the raw
data.
Ethical approval and consent to
participate
Ethical approval for the present study was obtained
from the Health Research Ethics Committee of Universitas Sumatera
Utara (approval komiteetik@usu.ac.id; ethical approval no.
918/KEPK/USU/2024). All participants provided verbal informed
consent prior to participation in the study. During the telephone
interviews, respondents were asked for their consent to proceed
with the ICIQ-UISF form, and interviews were only conducted if
consent was explicitly granted.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Liu N, Xing L, Mao W, Chen S, Wu J, Xu B
and Chen M: Relationship between blood glucose and hemoglobin A1c
levels and urinary incontinence in women. Int J Gen Med.
14:4105–4116. 2021.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Chow PM, Chuang YC, Hsu KCP, Shen YC and
Liu SP: Impact of female stress urinary incontinence on quality of
life, mental health, work limitation, and healthcare seeking in
China, Taiwan, and South Korea (LUTS Asia): Results from a
cross-sectional, population-based study. Int J Womens Health.
14:1871–1880. 2022.PubMed/NCBI View Article : Google Scholar
|
|
3
|
D'Ancona CD, Haylen BT, Oelke M, Herschorn
S, Abranches-Monteiro L, Arnold EP, Goldman HB, Hamid R, Homma Y,
Marcelissen T, et al: An International Continence Society (ICS)
Report on the Terminology for Adult Male Lower Urinary Tract and
Pelvic Floor Symptoms and Dysfunction. Neurourol Urodyn.
38:433–477. 2019.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Zhang YX, Xu HN, Xia ZJ and Wu B: Analysis
of clinical interventional strategy for women with urinary
incontinence complicated with diabetes mellitus. Int Urogynecol J.
23:1527–1532. 2012.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Adegbehingbe OO, Ayoola O, Soyoye D and
Adegbehingbe A: Urinary bladder wall thickness in type 2 diabetes
mellitus patients. J Ultrason. 22:e12–e20. 2022.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Wang R, Lefevre R, Hacker MR and Golen TH:
Diabetes, glycemic control, and urinary incontinence in women.
Female Pelvic Med Reconstr Surg. 21:293–297. 2015.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Yıldırım ZK, Tekin C and Çaltek HÖ:
Diabetes subtypes and urinary incontinence in pregnancy: Role of
BMI and HbA1c. Istanbul Med J. 26:167–171. 2025.
|
|
8
|
International Consultation on Incontinence
Questionnaire-Urinary Incontinence Short Form (ICIQ-UI SF):
Questionnaire. ICIQ-UI SF, 2015. https://iciq.net/iciq-ui-sf.
|
|
9
|
Lee SJ, Karter AJ, Thai JN, Van Den Eeden
SK and Huang ES: Glycemic control and urinary incontinence in women
with diabetes mellitus. J Womens Health (Larchmt). 22:1049–1055.
2013.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Erdal GS and Erdal FS: The relation
between BMI and polypharmacy with urinary incontinence in diabetic
geriatric Patients. Grand J Urol. 1:14–7. 2021.
|
|
11
|
Mattson J: Transportation, distance, and
health care utilization for older adults in rural and small urban
areas. Transportation Research Record Journal of the Transportation
Research Board. 2265:192–199. 2011.
|
|
12
|
Goodwin VA, Low MSA, Quinn TJ, Cockcroft
EJ, Shepherd V, Evans PH, Henderson EJ, Mahmood F, Ni Lochlainn M,
Needham C, et al: Including older people in health and social care
research: Best practice recommendations based on the INCLUDE
framework. Age Ageing. 52(afad082)2023.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Tambunan NA, Firmansyah Y, Nathaniel F,
Wijaya DA and Yogie GS: Correlation Of Current Blood Sugar Levels
With The International Consultant Incontinence Questionnaire-Urine
Incontinence Short Form (ICIQ-UISF) Values In The Elderly Group.
Malahayati Health Stud J. 3:3668–3677. 2023.(In Indonesian).
|
|
14
|
Sangsawang B: Risk factors for the
development of stress urinary incontinence during pregnancy in
primigravidae: a review of the literature. Eur J Obstet Gynecol
Reprod Biol. 178:27–34. 2014.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Cavalot F: Do data in the literature
indicate that glycaemic variability is a clinical problem?
Glycaemic variability and vascular complications of diabetes.
Diabetes Obes Metab. 15 (Suppl 2):S3–S8. 2013.PubMed/NCBI View Article : Google Scholar
|