1. Introduction
Light amplification by stimulated emission of
radiation (termed laser), introduced in the 1960s by Maiman has
been a breakthrough in the field of dentistry (1). Lasers can broadly be classified, on
the type of tissue adaptability into hard-tissue lasers, such as
neodymium-doped yttrium aluminum garnet (Nd:YAG), Er:YAG and
carbon-dioxide, and soft-tissue lasers, such as diode lasers
(2). While hard-tissue lasers are
more versatile as regards their application, they are more costly
and run a risk of causing thermal injury to the pulp (3).
The diode laser, running on the principle of a
semi-conductor is compact, affordable and versatile in its
application for soft tissue procedures and biostimulation. Its
application has been tried and tested over a number of years in the
field of dentistry and more specifically, in periodontology
(3). It has multiple settings for
various wavelength applications. Lower wavelengths (630-810 nm) are
appropriate for use in techniques, such as antibacterial
photodynamic therapy, while higher wavelengths (940-980 nm) are
used for bacterial decontamination, soft tissue curettage in
periodontal pockets and photobiomodulation (PBM) therapy.
2. Mechanisms of action of lasers
Lasers produce a single, coherent and monochromatic
light through stimulated emission in a medium excited by an
external energy source. Mirrors reflect and amplify photons, with a
partially reflecting mirror, at an angle, narrowing the light to a
focused beam prepared to emerge (4).
The wavelength is primarily determined by the
composition of its active medium, namely gas, crystal or a solid
semiconductor. Out of the four possible interactions which can
occur, that include reflection, transmission, scattering and
absorption, the latter is the most ideal for its application
(5). Once absorbed, the
temperature rises, producing photochemical effects. Protein
denaturation occurs at temperatures ranging from 60 to 100˚C.
Beyond this range, water ablation or vaporization occurs. In the
event that the temperature exceeds 200˚C, all water content is lost
and dehydration results in burning (Fig. 1).
Diode lasers
Diode lasers are packed into a conveniently sized
and portable device, allowing for an easier application across
different procedures in the field of dentistry. A diode laser is
primarily a solid semiconductor comprised of aluminium, gallium,
arsenide and indium. This is used to convert the input electrical
energy to produce light of varying wavelengths. These are further
readily absorbed by chromophores, such as melanin and hemoglobin
present in the soft tissue, allowing for ideal application. The use
of diode lasers in hard tissue, however, is not practically
applicable, as they exhibit poor absorption by hydroxyapatite,
predominantly observed in enamel. The flexible fiber optic fiber
aids in delivering treatment rays to the desired area (6). The treatment plan determines the use
of either continuous or pulsed modes and that of contact and
non-contact applications.
Over the years, ample research has been performed to
further investigate diode lasers, and various advantages have been
suggested. Compared to more conventional techniques, such as the
use of scalpels, diode lasers provide higher precision, a more
bloodless field, and thus, improved visualization, and the
placement of suture is obsolete. Diode lasers also provide an
excellent post-operative recovery period with minimal bleeding,
swelling and pain (7).
However, the use of diode lasers is not without
disadvantages. The equipment is costly, and is thus not accessible
to all dental clinics. Their use is also associated a risk of
morbidities, such as damage to the eye in the case that appropriate
protection is not used; thus, specialized training is required for
the use of diode lasers (8).
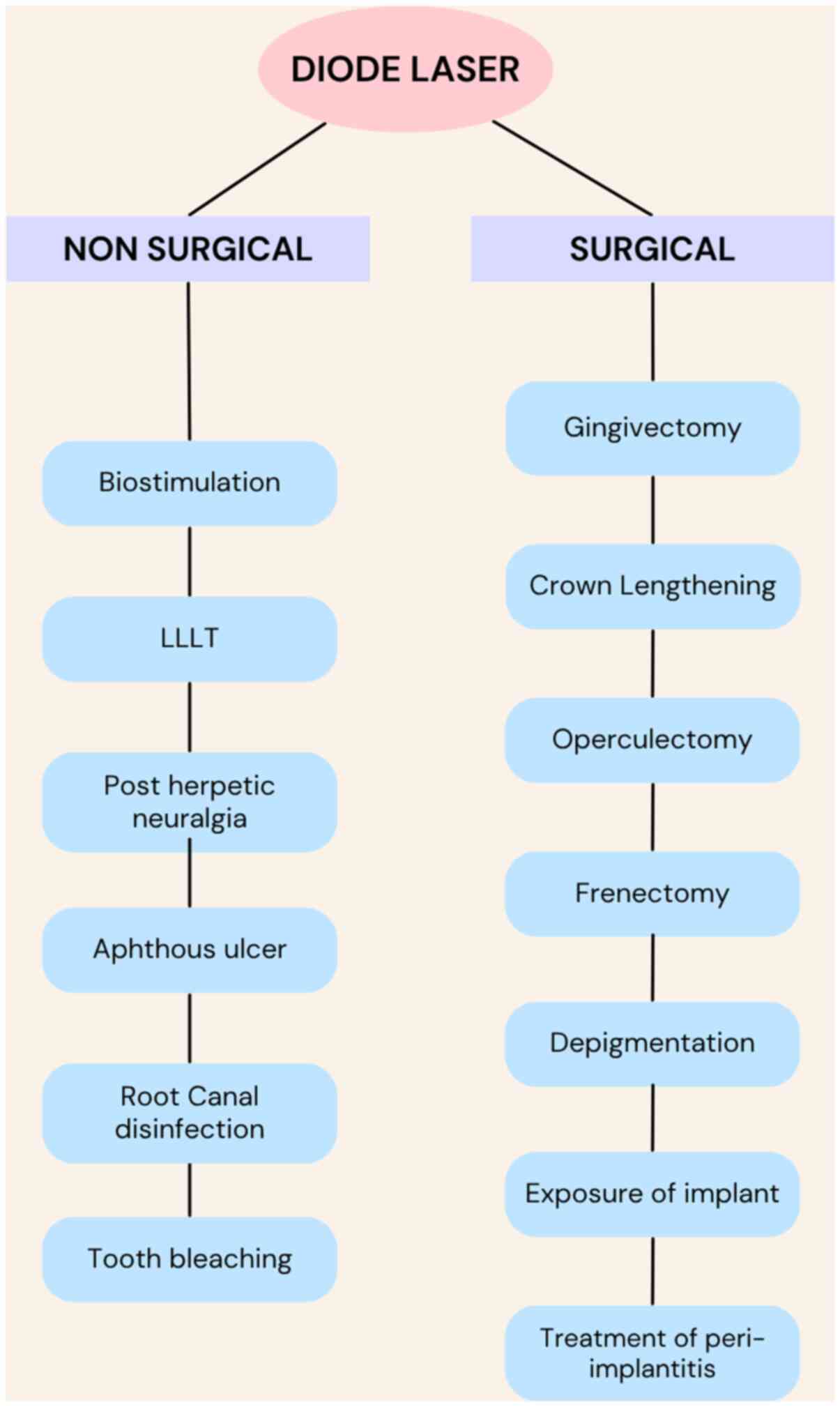
Below, the use of diode lasers in dentistry is discussed.
Crown lengthening
Diode lasers can be applied to various procedures,
such as in case of inadequate crown length prior to crown
placement, for the restoration of subgingival caries or fracture
exposure and for the correction of gummy smile (9). However due to a lack of hard-tissue
applications, it cannot only be used in cases where there is a wide
band of keratinized tissue and optimal space between the alveolar
crest and cementoenamel junction. The use of diode lasers is
proposed to be a more safe and effective alternative to the
traditional scalpel, as these lasers minimize bleeding and improve
post-operative pain according, to the visual analogue score
(10).
Gingival depigmentation
In the case of severely pigmented gingiva, a
surgical periodontal procedure may be used to reduce or remove the
zones of hyperpigmentation with the aid of a scalpel, high-speed
handpiece, cryosurgery or electrosurgery (11). Diode lasers have been proven to be
a single-step alternative. They eliminate the need for a
periodontal dressing, as their use is associated with a more rapid
healing process, with reduced pain and discomfort (12). A higher esthetic appearance is
expected when using the diode laser for gingival depigmentation
compared to the CO2 laser. The application of the diode
laser at pulsed mode may be recommended for gingival
depigmentation, as its use is associated with improved esthetic
outcomes and requires a smaller amount of time to achieve results
(13). The increasing esthetic
demands of individuals require the removal of hyperpigmented
gingival areas to create a confident and appealing smile, which can
be easily attained using a laser. As regards clinical significance,
the use of a laser is an effective tool which requires a smaller
amount of time to obtain results. The use of lasers is also
associated with lower levels of pain and discomfort, as well as a
more rapid healing process, and delayed repigmentation compared
with the use of scalpels or electrosurgery for gingival
depigmentation (14).
Exposure of unerupted and partially
erupted teeth
Lasers are also used for soft tissue removal over
unexposed or partially erupted teeth, for the placement of
orthodontic brackets or the removal of an operculum. They have an
added advantage over surgery in sealing small blood vessels and
lymphatic vessels. There is also minimal tissue shrinkage in laser
procedures, and thus, less scarring. The need for suturing is also
eliminated in the majority of cases, as healing occurs by secondary
intention (15).
Removal of tissue overgrowth
Fibrous hyperplasia is often observed due to
chronically ill-fitting dentures. To resume the use of dentures,
overgrowth removal is necessary (16). Diode lasers exhibit positive
results along with suitable homeostasis and less post-operative
pain. They can also be utilized to obtain biopsy specimens
(17).
Frenectomies
A high labial frenum can cause severe discomfort and
pain, in which case its removal may be indicated (18). For a relatively painless, bloodless
procedure with reduced post-surgical complications, diode lasers
can be used. The use of diode lasers is also particularly useful in
ankyloglossia. In these cases, a thick band of frenal attachment is
observed from the floor of the mouth until the tip of the tongue.
The excision of this band of tissue is essential for free tongue
movement (19).
Implant dentistry
Implant dentistry has been revolutionized over the
past few years. It has been striving to replace more redundant
techniques (20). In such a field,
diode lasers have been proven to be an immense success. They are
particularly useful in the second-stage of implant surgeries, as
they provide an efficient, safe, bloodless and painless procedure
(21). Diode lasers have also been
proven to be useful for the removal of peri-implant soft tissue and
the decontamination of failing implants. Various studies have been
conducted in this field of study that prove that diode
laser-assisted implant exposure eliminates the need for local
anesthesia (22).
However, the duration of surgery, healing time,
post-operative pain and overall success of the implant exhibit
similar results to those of scalpel surgery. Following treatment
for peri-implantitis with lasers, there is also a lack of
re-osseointegration observed with the use of lasers. There is also
a concern raised regarding the overheating of the implant surface,
followed by melting which can be a crucial drawback (23).
Wound healing
Biostimulation is another term for low-level laser
therapy (LLLT). Research indicates that a small amount of laser
energy (2 J/cm2) encourages the growth of fibroblasts,
whereas larger doses (16 J/cm2) inhibit their
proliferation (24). The rise in
fibroblast growth and movement leads to greater strength in healed
wounds. Research indicates that within the initial 72 h following
radiation exposure, biostimulation through LLLT leads to the
increased proliferation and maturation of human osteoblast-like
cells. In fact, a synergistic effect of laser use in combination
with ozonized substances has been demonstrated (25).
Photoactivated disinfection (PAD)
Low-level laser energy from a diode lasers functions
as a photo-activator of oxygen releasing dyes, such as Methylene
blue. This has been shown to cause membrane and DNA damage to
microorganisms when activated (26).
As stated in the literature, PAD has been found to
be particularly effective in killing bacteria, including
sub-gingival plaque in deep periodontal pockets, which are
generally known to be resistant to anti-microbial agents. It has
also been demonstrated to kill Gram-positive bacteria (including
methicillin-resistant Staphylococcus aureus), Gram-negative
bacteria, fungi and viruses. It is also now being used in the
disinfection of peri-mucositis and peri-implantitis (26).
Post-herpetic neuralgia and aphthous
ulcers
Post-herpetic neuralgia is a chronic painful
condition that occurs as a complication of herpes zoster virus
(27). It is generally observed
due to the reactivation of a varicella zoster virus found dormant
in a nerve cell near the spinal cord. This virus is commonly known
to cause chickenpox. Upon reactivation, it manifests as a painful
rash along the specific dermatome innervated by the spinal nerve
(27).
The condition is commonly known to be painful along
with hyperesthesia or even allodynia. LLLT has been demonstrated to
reduce this pain and enhance the healing process in these
conditions. In particular, in the case of recurrent herpes simplex
labialis lesions, photostimulation during the prodomal stage has
been shown to arrest the acceleration and progression of the
healing process and to reduce recurrence (28).
Root canal disinfection
Traditionally, root canal preparation is performed
with mechanical instrumentation using files and irrigants. In
vitro studies (29-31)
have suggested the use of laser irradiation following this to
increase the disinfection of deep radicular dentin. It has also
been associated with effective sealing of dentinal tubules,
eliminating Escherichia coli and Enterococcus
faecalis. This has also been suggested to increase the efficacy
of endodontic treatments (29-31).
Removal of periodontal pocket
lining
In the case of a periodontal pocket, scaling and
root planing are the primary steps for treatment. This helps remove
the inflamed gingival tissue and infected material present in the
pocket. Following this, the optical fiber of a diode laser can be
introduced into the pocket in ascending and descending movements,
while maintaining it parallel to the main access of the tooth root
(32). It is rotated around the
perimeter of each involved tooth. This helps to remove the pocket
lining, leading to a reduction of the periodontal pocket (33).
In their study, Assaf et al (34) used a diode laser in conjunction
with ultrasonic scaling for the treatment of gingivitis. The
results of their study revealed a significantly lower incidence of
bacteremia in the group treated with diode and ultrasonic therapy
(36%) compared with the group treated only with ultrasonic therapy
(68%) (34). In addition, it has
been suggested that in order to prevent bacteremia, particularly in
immuno-compromised patients, diode lasers should be used. For
example, Kamma et al (35)
confirmed that the total bacterial load in pockets was reduced
without the use of any systemic antibiotic therapy.
Tooth whitening
Laser lights enhance the efficacy of hydrogen
peroxide in the bleaching agent to a greater extent than
light-emitting-diodes (LEDs) (36). Teeth bleached with LEDs exhibit a
significant decrease in color intensity and appear gray, while
those treated with laser exhibit improved color intensity and less
grayness (37). Furthermore,
increased brightness and decreased sensitivity can be attained
using lasers to activate hydrogen peroxide (38).
3. Laser-assisted pediatric dentistry
Lasers have emerged as a valuable tool in pediatric
dentistry due to their minimally invasive nature, reduced need for
anesthesia and improved patient comfort. Diode lasers are commonly
used for soft tissue procedures, such as frenectomy, pulpotomy and
gingivoplasty. In children, lasers provide advantages, such as
reduced bleeding, a more rapid healing process and lower anxiety
levels compared to conventional techniques. Moreover, their
bactericidal properties enhance infection control in procedures
involving the pulp or soft tissues. However, careful parameter
selection is essential to avoid thermal damage, particularly in
immature or developing tissues (39).
PBM and anesthesia
PBM has gained increasing attention due to its
efficacy in pain reduction in various fields of dentistry. However,
available studies on the effects of PBM on injection pain in
children are minimal. A previous study examined the efficacy of PBM
with three different application parameters (doses) and topical
anesthesia in reducing injection pain and compared these results
with the placebo PBM and topical anesthesia in children during
supraperiosteal anesthesia administration; however, no differences
were found between the groups (P=0.109 and P=0.317). In addition,
in that study, the injection pain in children did not differ
compared to the placebo and PBM applied at a power of 0.3 W for 20,
30 and 40 sec (40).
4. Laser-tissue interactions and related
complications
Laser-tissue interactions in periodontal therapy are
governed by factors, such as wavelength, power density, pulse
duration and tissue characteristics. While lasers provide numerous
advantages, including precise cutting, hemostasis and minimal
postoperative discomfort, overexposure to laser energy can lead to
significant soft tissue complications. Excessive thermal energy can
cause coagulative necrosis, carbonization, or deep tissue burns,
leading to delayed wound healing and scarring. Moreover, prolonged
or improperly focused exposure can result in destruction of
adjacent healthy tissue, compromising the structural and functional
integrity of the periodontium. Overheating may also impair
microcirculation and fibroblast viability, essential for optimal
regeneration. In some cases, laser-induced edema, pain, or
ulceration has been reported due to excessive tissue ablation or
inadequate cooling. Therefore, strict adherence to recommended
laser parameters and technique is critical to avoid iatrogenic
injury and ensure therapeutic efficacy (41).
5. Advances in diode lasers
A dual-wavelength diode laser in dentistry has been
introduced that combines two distinct wavelengths, typically 450
and 808 nm, in order to provide a versatile approach to soft-tissue
procedures. This approach has certain advantages compared to
single-wavelength lasers, as it utilizes the unique properties of
each wavelength to achieve optimal coagulation, ablation and
healing (42).
A flexible optical fiber, typically in the form of a
handpiece, transmits the laser beams to the target area. The laser
can be used in both continuous and pulsed modes (pulse duration
ranging from 0.1 msec to infinity, with programmable frequencies up
to 10,000-20,000 Hz). The laser beam is delivered through optical
fibers with diameters ranging from 200 to 600 µm. The clinical
approach and treatment methods determine the selection between
continuous and pulsed modes, contact or non-contact tissue
application, and the specific type of tip recommended by the
manufacturer. A number of diode lasers allow for the adjustment of
parameters, such as power and frequency to minimize tissue damage
and enhance precision. The use of dual-wavelength lasers for
surgical purposes can lead to improved hemostatic cutting. In the
majority of cases, healing occurs by secondary intention with
minimal scar formation, eliminating the need for sutures.
Additionally, there is a significant reduction in post-operative
pain and inflammation, attributed to cellular biomodulation
resulting from residual energy transmission to the tissues during
the cutting action. By using both wavelengths, dual-wavelength
lasers can achieve a balance between coagulation and ablation,
potentially minimizing collateral damage and promoting more rapid
healing (42).
6. Conclusion and future perspectives
Diode laser technology and its various applications
in dentistry date back to several decades; however, it has been in
the past 10 years that diode lasers have gained a greater
prominence owing to the immense technical development achieved and
the materialization of affordable equipment for the dentist. All
these advancements have allowed for the current use of lasers in
numerous procedures to improve the performance of conventional
therapies; however, this is not sufficient. The use of different
diode laser therapies should be consolidated with further research.
In recent years, progress has been made in this regard, as it has
gained increasing prominence as an adjuvant therapy; however,
although there are several notable in vitro and clinical
studies available on the use of lasers (as aforementioned), further
research is warranted to address laser therapy from a different
perspective (43).
There is a possibility to match laser technology
with other recently introduced technology, such as smartphone
applications and artificial intelligence. It is desirable that
future studies evaluate long-term results to confirm the
effectiveness and use of diode lasers. Furthermore, studies
involving larger samples are warranted. The importance of lasers
should be explained by dental practitioners to make patients aware
of their existence and benefits. The ethical and legal implications
of the use of lasers should also be carefully considered. It would
also of interest to combine lasers with recently introduced
artificial intelligence software, which is an interesting and
current research topic (44,45).
In conclusion, the utilization of diode lasers in
oral soft tissue surgery is due to their simple application,
improved coagulation, elimination of suturing, reduced swelling and
pain, and their ability to address physiological gingival
pigmentation for aesthetic purposes. Diode lasers are a preferred
option for their swift action, enhanced de-epithelialization, lack
of bleeding and superior healing. Over the past 40 years, diode
lasers have been increasingly utilized in various dental
procedures, such as biostimulation for wounds, activating teeth
whitening gel, photodynamic disinfection and enhancing root canal
disinfection. Due to its affordable price and convenient size, this
optical scalpel is becoming increasingly popular among dentists in
dental clinics and hospitals.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
Not applicable.
Authors' contributions
All authors (DK, DGK, SS and AS) contributed to the
conception and design of the study. DK, SS and AS were involved in
manuscript preparation, and the collection and analysis of data
from the literature. DK wrote the first draft of the manuscript.
All authors commented on previous versions of the manuscript. All
authors have read and approved the final manuscript. Data
authenticity is not applicable.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Gross AJ and Hermann TR: History of
lasers. World J Urol. 25:217–220. 2007.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Center D: Application of laser in
dentistry: A brief review. J Adv Med Dental Sci Res. 9:2321–9599.
2021.
|
|
3
|
Luke AM, Mathew S, Altawash MM and Madan
BM: Lasers: A review with their applications in oral medicine. J
Lasers Med Sci. 10:324–329. 2019.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Maheshwari S, Jaan A, Vyaasini CS, Yousuf
A, Arora G and Chowdhury C: Laser and its implications in
dentistry: A review article. Curr Med Res Opin. 3:579–588.
2020.
|
|
5
|
Goldman L, Goldman B and Van-Lieu N:
Current laser dentistry. Lasers Surg Med. 6:559–562.
1987.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Aoki A, Mizutani K, Takasaki AA, Sasaki
KM, Nagai S, Schwarz F, Yoshida I, Eguro T, Zeredo JL and Izumi Y:
Current status of clinical laser applications in periodontal
therapy. Gen Dent. 56:674–687. 2008.PubMed/NCBI
|
|
7
|
Carroll L and Humphreys TR: Laser-tissue
interactions. Clin Dermatol. 24:2–7. 2006.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Desiate A, Cantore S, Tullo D, Profeta G,
Grassi FR and Ballini A: 980 nm diode lasers in oral and facial
practice: Current state of the science and art. Int J Med Sci.
6:358–364. 2009.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Camargo PM, Melnick PR and Camargo LM:
Clinical crown lengthening in esthetic zone. J Calif Dent Assoc.
35:487–98. 2007.PubMed/NCBI
|
|
10
|
Farista S, Kalakonda B, Koppolu P, Baroudi
K, Elkhatat EN and Dhaifullah E: Comparing laser and scalpel for
soft tissue crown lengthening: A clinical study. Glob J Health Sci.
8(55795)2016.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Kumar R, Jain G, Dhodapkar SV, Kumathalli
KI and Jaiswal G: The comparative evaluation of patient's
satisfaction and comfort level by diode laser and scalpel in the
management of mucogingival anomalies. J Clin Diagn Res. 9:56–58.
2015.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Roshn T and Nandakumar K: Anterior
esthetic gingival depigmentation and crown lengthening: Report of a
casese. J Contemp Dent Pract. 6:139–147. 2005.PubMed/NCBI
|
|
13
|
Moeintaghavi A, Ahrari F, Fallahrastegar A
and Salehnia A: Comparison of the effectiveness of CO2 and diode
lasers for gingival melanin depigmentation: A randomized clinical
trial. J Lasers Med Sci. 13(e8)2022.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Jagannathan R, Rajendran S, Balaji TM,
Varadarajan S and Sridhar LP: Comparative evaluation of gingival
depigmentation by scalpel, electrosurgery, and laser: A 14 months'
Follow-up study. J Contemp Dent Pract. 21:1159–1164.
2020.PubMed/NCBI
|
|
15
|
Sarver DM and Yanosky M: Principles of
cosmetic dentistry in orthodontics: Part 2. Soft tissue laser
technology and cosmetic gingival contouring. Am J Orthod
Dentofacial Orthop. 127:85–90. 2005.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Chawla K, Lamba AK, Faraz F, Tandon S and
Ahad A: Diode laser for excisional biopsy of peripheral ossifying
fibroma. Dent Res J. 11:525–530. 2014.PubMed/NCBI
|
|
17
|
D'Arcangelo C, Di Nardo Di Maio F,
Prosperi GD, Conte E, Baldi M and Caputi S: A preliminary study of
healing of diode laser versus scalpel incisions in rat oral tissue:
A comparison of clinical, histological, and immunohistochemical
results. Oral Surg Oral Med Oral Pathol Oral Radiol Endod.
103:764–773. 2007.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Yadav RK, Verma UP, Sajjanhar I and Tiwari
R: Frenectomy with conventional scalpel and Nd: YAG laser
technique: A comparative evaluation. J Indian Soc Periodontol.
23:48–52. 2019.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Kalakonda B, Farista S, Koppolu P, Baroudi
K, Uppada U and Mishra A: Evaluation of patient perceptions after
vestibuloplasty procedure: A comparison of diode laser and scalpel
techniques. J Clin Diagn Res. 10:96–100. 2016.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Yeh S, Jain K and Andreana S: Using a
diode laser to uncover dental implants in secondstage surgery. Gen
Dent. 53:414–417. 2005.PubMed/NCBI
|
|
21
|
El-Kholey KE: Efficacy and safety of a
diode laser in secondstage implant surgery: A comparative study.
Int J Oral Maxillofac Surg. 43:633–638. 2014.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Gianfranco S, Francesco SE and Paul RJ:
Erbium and diode lasers for operculisation in the second phase of
implant surgery: A case series. Timisoara Med J. 60:117–123.
2010.
|
|
23
|
Grzech-Lesniak K: Making use of lasers in
periodontal treatment: A new gold standard? Photomed Laser Surg.
35:513–514. 2017.PubMed/NCBI View Article : Google Scholar
|
|
24
|
O'Neill JF, Hope CK and Wilson M: Oral
bacteria in Multi-species biofilms can be killed by red light in
the presence of toluidine blue. Lasers Surg Med. 31:86–90.
2002.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Scribante A, Gallo S, Pascadopoli M, Soleo
R, Di Fonso F, Politi L, Venugopal A, Marya A and Butera A:
Management of periodontal disease with adjunctive therapy with
ozone and photobiomodulation (PBM): A randomized clinical trial.
Photonics. 9(138)2022.
|
|
26
|
Husejnagic S, Lettner S, Laky M,
Georgopoulos A, Moritz A and Rausch-Fan X: Photoactivated
disinfection in periodontal treatment: A randomized controlled
clinical Split-mouth trial. J Periodontol. 90:1260–1269.
2019.PubMed/NCBI View Article : Google Scholar
|
|
27
|
To DS, Martins MA, Bussadori SK, Fernandes
KP, Tanji EY, Mesquita-Ferrari RA and Martins MD: Clinical
evaluation of low level laser treatment for recurring aphthous
stomatitis. Phtomed Laser Surg. 28 (Suppl 2):S85–S88.
2010.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Bladowski M, Konarska-Choroszucha H and
Choroszucha T: Comparison of treatment results of recurrent
aphthous stomatitis (RAS) with low-and high-power laser irradiation
vs. pharmaceutical method. J Oral Laser Applic. 4:191–209.
2004.
|
|
29
|
de Souza EB, Cai S, Simionato MR and
Lage-Marques JL: High-power diode laser in the disinfection in
depth of the root canal dentin. Oral Surg Oral Med Oral Pathol Oral
Radiol Endod. 106:e68–e72. 2008.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Theodoro LH, Haypek P, Bachmann L, Garcia
VG, Sampaio JEC, Zezell DM and Eduardo Cde P: Effect of ER: YAG and
diode laser irradiation on the root surface: Morphological and
thermal analysis. J Periodontol. 74:838–843. 2003.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Menezes M, Prado M, Gomes B, Gusman H and
Simão R: Effect of phootodynamic therapy and non-thermal plasma on
root canal filling: Analysis of adhesion and sealer penetration. J
App Orl Sci. 25:396–403. 2017.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Caccianiga G, Rey G, Baldoni M, Caccianiga
P, Baldoni A and Ceraulo S: Periodontal decontamination induced by
light and not by heat: Comparison between oxygen high level laser
therapy (OHLLT) and LANAP. App Sci. 11(4629)2021.
|
|
33
|
Jha A, Gupta V and Adinarayan R: LANAP,
periodontics and beyond: A review. J Lasers Med Sci. 9:76–81.
2018.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Assaf M, Yilmaz S, Kuru B, Ipci SD, Noyun
U and Kadir T: Effect of the diode laser on bacteremia associated
with dental ultrasonic scaling: A clinical and microbiological
study. Photomed Laser Surg. 25:50–56. 2007.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Kamma JJ, Vasdekis VG and Romanos GE: The
effect of diode laser (980 nm) treatment on aggressive
periodontitis: Evaluation of microbial and clinical parameters.
Photomed Laser Surg. 27:11–9. 2009.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Dostalova T, Jelinkova H, Housova D, Sulc
J, Nemec M, Miyagi M, Junior AB and Zanin F: Diode laser-activated
bleaching. Brazi DentJ. 15 (Suppl 1):SI3–S18. 2004.PubMed/NCBI
|
|
37
|
Wetter NU, Walverde D, Kato IT and Eduardo
Cde P: Bleaching efficacy of whitening agents activated by xenon
lamp and 960-nm diode radiation. Photomed Laser Surg. 22:489–493.
2004.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Vildósola P, Bottner J, Avalos F, Godoy I,
Martín J and Fernández E: Teeth bleaching with low concentrations
of hydrogen peroxide (6%) and catalyzed by LED blue (450±10 nm) and
laser infrared (808±10 nm) light for in-office treatment:
Randomized clinical trial 1-yearfollow-up. J Esthet Restor Dent.
29:339–345. 2017.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Nazemisalman B, Farsadeghi M and
Sokhansanj M: Types of lasers and their applications in pediatric
dentistry. J Lasers Med Sci. 6:96–101. 2015.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Elbay M, Elbay ÜŞ, Kaya E and Kalkan ÖP:
Effects of photobiomodulation with different application parameters
on injection pain in children: A randomized clinical trial. J Clin
Pediatr Dent. 47:54–62. 2023.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Ansari MA, Erfanzadeh M and Mohajerani E:
Mechanisms of Laser-tissue interaction: II. tissue thermal
properties. J Lasers Med Sci. 4:99–106. 2013.PubMed/NCBI
|
|
42
|
Pergolini D, Del Vecchio A, Mohsen M,
Cerullo V, Angileri C, Troiani E, Visca P, Antoniani B, Romeo U and
Palaia G: Histological evaluation of oral soft tissue biopsy by
Dual-wavelength diode laser: An ex vivo study. Dent J (Basel).
13(265)2025.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Krishnan PA and Sukumaran A: Lasers and
their applications in the dental practice. Int J Dentistry Oral
Sci. 7:936–943. 2020.
|
|
44
|
Pascadopoli M, Zampetti P, Nardi MG,
Pellegrini M and Scribante A: Smartphone applications in dentistry:
A scoping review. Dent J (Basel). 11(243)2023.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Wang C, Yang J, Liu H, Yu P, Jiang X and
Liu R: Co-Mask R-CNN: Collaborative Learning-based method for tooth
instance segmentation. J Clin Pediatr Dent. 48:161–172.
2024.PubMed/NCBI View Article : Google Scholar
|