Introduction
Anti-neutrophil cytoplasmic antibodies (ANCAs) are
autoantibodies produced by the immune system, which mistakenly
target and attack proteins within an individual's neutrophils
(1). Using indirect fluorescence
antibody testing, ANCAs are typically classified as either
myeloperoxidase (MPO)-ANCA, proteinase 3 (PR3)-ANCA and
atypical-ANCA (1). The clinical
significance of the two common types or ANCA subsets, MPO-ANCA and
PR3-ANCA, differs; MPO-ANCA is often associated with microscopic
polyarteritis, necrotizing glomerulonephritis and Churg-Strauss
syndrome, whereas PR3-ANCA is found primarily in patients
exhibiting granulomatosis with polyangiitis (previously Wegener's
granulomatosis) (1). The association
between MPO-ANCA and lung fibrosis has also been demonstrated
(2,3).
The present case report describes a patient with elevated serum
levels of MPO-ANCA and PR3-ANCA, which decreased during the
postoperative course. To the best of our knowledge, this is the
first case to show a decrease in elevated serum levels of the two
types of ANCA following treatment for lung cancer.
Case report
A 71-year-old woman with arthralgia and lung
fibrosis was referred to Mito Kyodo General Hospital (Mito, Japan)
for a mass that was incidentally observed on a chest radiograph.
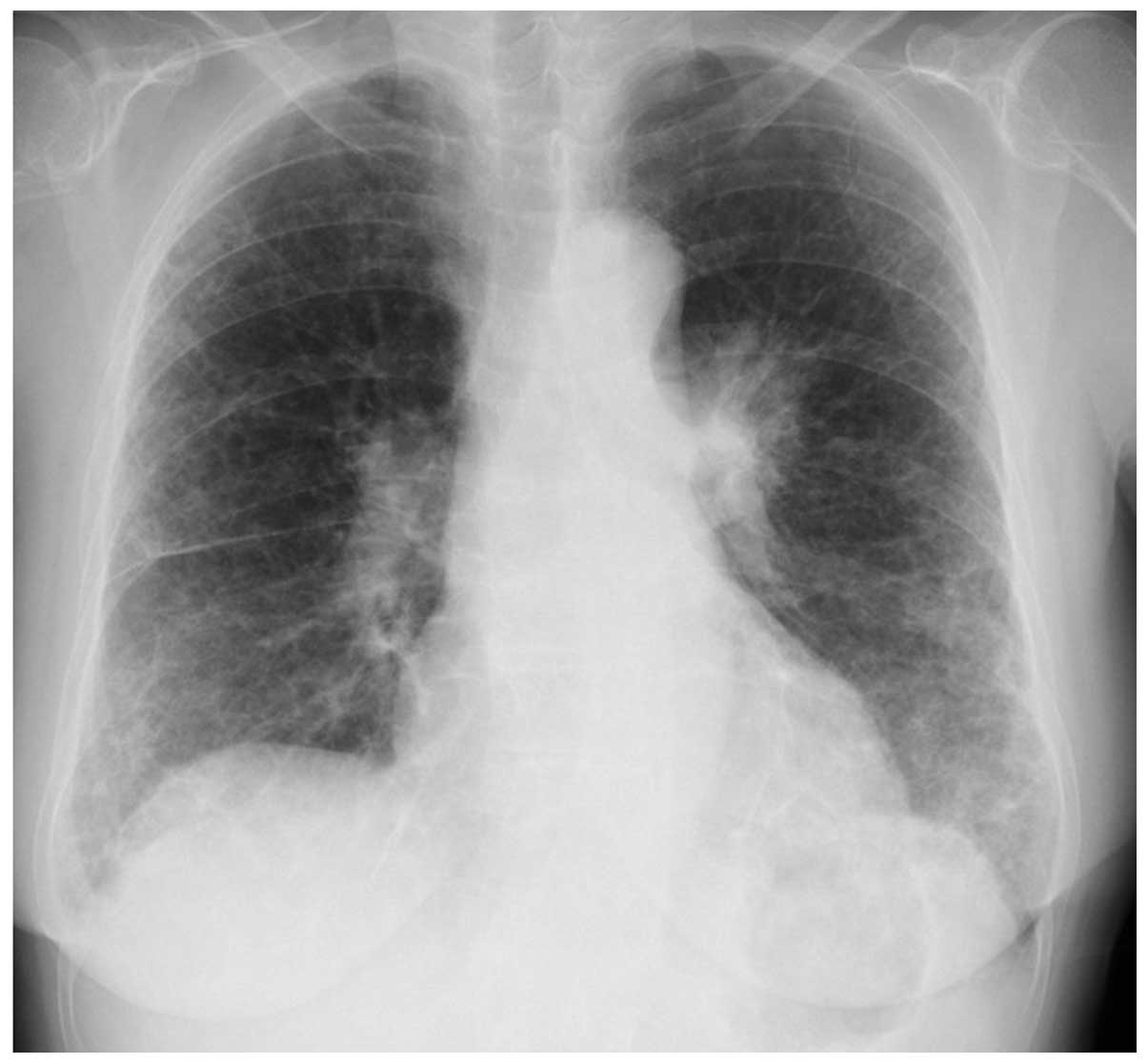
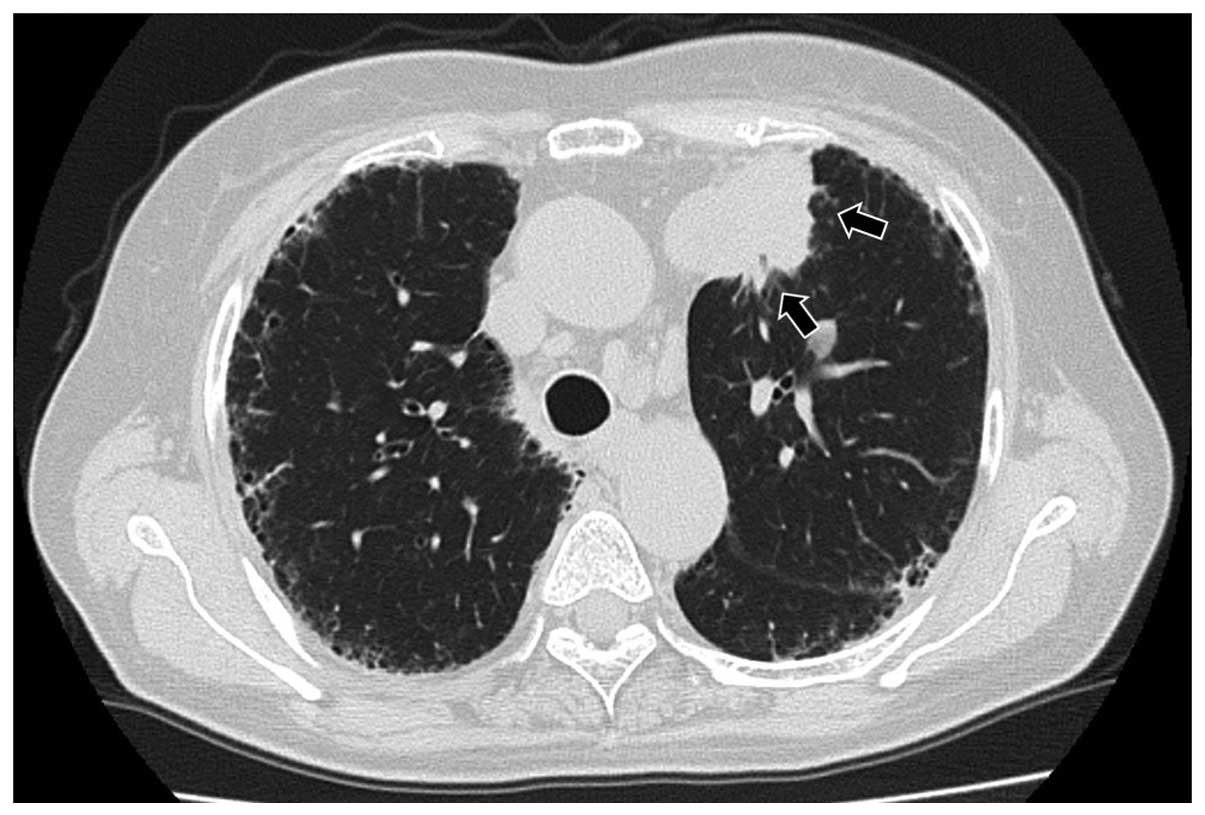
The chest radiograph and a computed tomography scan showed
ground-glass opacity and honeycombing in the lower lobes of the
lungs, and a nodule in the left upper lobe of the lung (Figs. 1 and 2).
The differential diagnosis was primary lung cancer and a nodule
with granulomatosis with polyangiitis. Laboratory analysis
demonstrated antinuclear antibodies were positive with a titer of
1:160 homogenous pattern, and a titer of 1:160 speckled pattern.
Serum levels of MPO-ANCA and PR3-ANCA were elevated to 60.3 and 7.5
U/ml, respectively (normal range, ≤3.5 IU/ml). A transbronchial
biopsy obtained from the lesion revealed a lung adenocarcinoma and
the patient underwent standard upper lobectomy of the left lung.
Written informed consent was obtained from the patient. The
postoperative period was not eventful and the postoperative
diagnosis was pT3N1M0, stage IIIA (according to the seventh edition
of the International Union Against Cancer TNM Staging System for
Lung Cancer), epidermal growth factor receptor mutation-negative
and anaplastic lymphoma receptor tyrosine kinase-negative fusion
gene. One month subsequent to the resection, MPO-ANCA and PR3-ANCA
serum levels had returned to 10.0 and <1.0 U/ml, respectively.
Antinuclear antibodies were positive, with a titer of 1:80
homogenous pattern and a titer of 1:80 speckled pattern. The
patient experienced an uneventful postoperative course for 6
months; however, developed lung and brain metastases, and succumbed
due to lung cancer 15 months after surgery.
Discussion
The presence of antibodies that react with
neutrophil cytoplasm in patients who had necrotizing
glomerulonephritis and small-vessel vasculitis was first reported
by Davies et al in 1982 (4). A
wide variety of pulmonary abnormalities, including alveolar
hemorrhage and pulmonary fibrosis, have been reported to be
associated with MPO-ANCA (5–7). Whereas the majority of patients with
granulomatosis with polyangiitis have elevated serum levels of
PR3-ANCA (8,9). It currently remains unknowns as to
whether there is a definite association between solid tumors and
elevated serum levels of ANCAs. Edgar et al (10) were the first to report an association
between solid tumors and ANCA-associated vasculitis. Thereafter,
Tatsis et al (11) evaluated
the frequencies and types of malignant diseases occurring before or
simultaneously with the diagnosis of patients positive for
PR3-ANCA. The authors reported that 23 of 477 patients that were
PR3-ANCA-positive had solid tumors; the most common malignant
disease was renal cell carcinoma and one patient had lung cancer
(11). Including this patient, to the
best of knowledge, there have been four ANCA-positive lung cancer
patients (Table I) (10–13). The
patients were the fifth and sixth decades, and were all male. Three
of the patients were positive for PR3-ANCA, and the others were
positive for MPO-ANCA. Two patients presented with squamous cell
carcinoma, and one patient had adenocarcinoma (and there was no
description for one patient). Two patients had renal impairment,
but none of the patients had pulmonary fibrosis. The patient in the
current study complained of arthralgia for 5 years and lung
fibrosis was detected on a chest radiograph taken 2 years before
referral to our department. Elevated serum levels of MPO-ANCA may
be associated with lung fibrosis in this patient. As the patient
presented with a mass on the chest radiograph, measurement of serum
PR3-ANCA levels was performed to rule out the possibility of
developing granulomatosis with polyangiitis. Notably, in the
present case, elevated PR3-ANCA and MPO-ANCA serum levels were
noted pretreatment, and decreases in the levels of the two types of
ANCA were observed postoperatively. Furthermore, titers of
antinuclear antibodies were observed to decrease during the
postoperative course. As shown in Table
I, decreases in the elevated serum levels of either MPO-ANCA or
PR3-ANCA following therapy for lung cancer were reported in two
patients (12,13). Navarro et al (12) reported a case of lung adenocarcinoma
with elevated MPO-ANCA serum levels and its decrease as a result of
therapy for lung cancer with prednisolone and cyclophosphamide.
Morisako et al (13) reported a
case with elevated levels of PR3-ANCA in a patient with advanced
squamous cell lung carcinoma, and the ANCA level was decreased
subsequent to successful chemotherapy. However, to the best of our
knowledge, the present case is the first to exhibit decreases in
elevated serum levels of the two types of ANCA due to therapy for
lung cancer. In certain cases of ANCA-associated vasculitis,
malignant disease may be a trigger for either the generation of
ANCAs or the development of vasculitis (10). In conclusion, together with the results
of previously reported cases (12,13),
elevated serum ANCA levels may be associated with the existence of
malignant disease, although the occurrence of the two types of ANCA
being elevated is rare. The present case provides information,
which may facilitate the diagnosis and treatment of similar cases
of patients presenting with these diseases.
 | Table I.ANCA-positive lung cancer
patients. |
Table I.
ANCA-positive lung cancer
patients.
| Author, year
(Refs.) | Age (years) | Gender | ANCA-positive | Pathology | Renal impairment | IPF | Lung cancer
therapy | ANCA improvement
post-treatment |
|---|
| Edgar et al,
1993 (10) | 62 | M | PR3-ANCA | SQ | Present | ND | BSC | ND |
| Tatsis et al,
1999 (11) | 63 | M | PR3-ANCA | ND | ND | ND | ND | ND |
| Navarro et al,
1994 (12) | 68 | M | MPO-ANCA | AD | Present | ND | Irradiation | Present |
| Morisako et
al, 2006 (13) | 57 | M | PR3-ANCA | SQ | Absent | Absent | Chemotherapy | Present |
| Present case | 70 | F | PR3-ANCA | AD | Absent | Present | Surgery | Present |
|
|
|
| MPO-ANCA |
|
|
|
|
|
References
|
1
|
Beauvillain C, Delneste Y, Renier G,
Jeannin P, Subra JF and Chevailler A: Antineutrophil cytoplasmic
autoantibodies: how should the biologist manage them? Clin Rev
Allergy Immunol. 35:47–58. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Hervier B, Pagnoux C, Agard C, Haroche J,
Amoura Z, Guillevin L and Hamidou MA: French Vasculitis Study
Group: Pulmonary fibrosis associated with ANCA-positive
vasculitides. Retrospective study of 12 cases and review of the
literature. Ann Rheum Dis. 68:404–407. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Yamada H: ANCA: Associated lung fibrosis.
Semin Respir Crit Care Med. 32:322–327. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Davies DJ, Moran JE, Niall JF and Ryan GB:
Segmental necrotising glomerulonephritis with antineutrophil
antibody: possible arbovirus aetiology? Br Med J (Clin Res Ed).
285:6061982. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Arimura Y, Minoshima S, Tanaka U, Fujii A,
Kobayashi M, Nakabayashi K, Kitamoto K and Nagasawa T: Pulmonary
involvement in patients with myeloperoxidase
specific-antineutrophil cytoplasmic antibody. Ryumachi. 35:46–55.
1995.(In Japanese). PubMed/NCBI
|
|
6
|
Homma S, Matsushita H and Nakata K:
Pulmonary fibrosis in myeloperoxidase antineutrophil cytoplasmic
antibody-associated vasculitides. Respirology. 9:190–196. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Gaudin PB, Askin FB, Falk RJ and Jennette
JC: The pathologic spectrum of pulmonary lesions in patients with
anti-neutrophil cytoplasmic autoantibodies specific for
anti-proteinase 3 and anti-myeloperoxidase. Am J Clin Pathol.
104:7–16. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Jennette JC and Falk RJ: Small-vessel
vasculitis. N Engl J Med. 337:1512–1523. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Jennette JC: Antineutrophil cytoplasmic
autoantibody-associated diseases: a pathologist's perspective. Am J
Kidney Dis. 18:164–170. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Edgar JD, Rooney DP, McNamee P and McNeill
TA: An association between ANCA positive renal disease and
malignancy. Clin Nephrol. 40:22–25. 1993.PubMed/NCBI
|
|
11
|
Tatsis E, Reinhold-Keller E, Steindorf K,
Feller AC and Gross WL: Wegener's granulomatosis associated with
renal cell carcinoma. Arthritis Rheum. 42:751–756. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Navarro JF, Quereda C, Rivera M, Navarro
FJ and Ortuño J: Anti-neutrophil cytoplasmic antibody-associated
paraneoplastic vasculitis. Postgrad Med J. 70:373–375. 1994.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Morisako T, Tsuchida F, Nakamura H, Ohishi
S and Matsuoka T: A case of squamous cell carcinoma of the lung
with a high titer of proteinase 3 antineutrophil cytoplasmic
antibody. Nihon Kokyuki Gakkai Zasshi. 44:139–143. 2006.(In
Japanese). PubMed/NCBI
|