Introduction
The von Willebrand factor (vWF) is a large
multimeric plasma glycoprotein produced by endothelial cells and
megakaryocytes (1). vWF can be
secreted through a constitutive pathway following synthesis, or by
a regulated pathway involving storage and release by secretagogues
(2,3). Although platelets secrete vWF, plasma
vWF levels have been shown to depend almost entirely on vWF from
endothelial cells (4). A large
amount of vWF is stored in Weibel-Palade bodies in endothelial
cells and released towards the lumen of blood vessels in response
to various stimuli (5,6). In blood circulation, vWF is well known
for its role in homeostasis, where it binds to platelet receptor
glycoprotein Ib and to the constituents of the sub-endothelial
connective tissue (4,7). vWF also binds to blood coagulation
factor VIII, another blood clotting protein, and acts as its
carrier in the circulation (8). In
addition to homeostasis, vWF has recently been recognized as a
critical regulator in angiogenesis, inflammation and cell
proliferation (9–11).
The vWF gene is located on chromosome 12p and
comprises 52 exons spanning ~178 kb of genomic sequence (12). Mutations in the vWF gene are
responsible for von Willebrand disease, a bleeding disorder that
prolongs the blood clotting process (13). The vWF gene is also a marker of
endothelial cell heterogeneity as demonstrated by the existence of
regional variations in vWF protein and mRNA levels within the
vascular tree (14). The
vascular-bed specific expression of vWF is regulated by a group of
distinct signaling pathways, each communicating with different
regions of the promoter (15,16). In
pathological conditions such as sepsis, diabetes and cancer
development, vWF expression in endothelial cells is regulated by
specific groups of transcription factors (17–21).
The plasma levels of vWF have been found to be
associated with cardiovascular diseases, particularly myocardial
infarction (MI) (22,23). MI is a common cause of mortality; as
of 2008, >3,000,000 individuals exhibited ST elevation MIs and
4,000,000 non-ST elevation MIs every year worldwide (24). As a result of inadequate coronary
artery blood flow, MI triggers ischemic responses, which include
myocyte death, endothelial cell dysfunction and abnormal tissue
repair with fibrosis (25). To date,
no clinical marker is available for the accurate assessment of this
process (26). Plasma vWF
concentration has been shown to be increased in patients with acute
MI (AMI) (27,28). However, other studies have reported
that no difference in the vWF levels was identified between
patients with MI and the controls (29,30). It
is therefore necessary to accurately assess the plasma vWF level
during MI.
In the present study, a rat model of ST-elevation
AMI was established, and the plasma vWF level in the cardiac and
peripheral blood was examined at different time-points. The plasma
level of TNF-α, an inflammatory cytokine, was also examined and the
effects of TNF-α on vWF secretion and expression in cultured
endothelial cells were investigated. The data obtained may be
important for evaluating the association between plasma vWF and AMI
progression.
Materials and methods
Animal model
Fifty-seven male Wistar rats (age, 8 weeks; weight,
280–300 g) were obtained from the Animal Center of Shandong
University (Jinan, China) and randomized into four groups:
Sham-operated and MI 1-h, 24-h and 7-day groups. Each group
contained 12–15 rats. Following anesthesia with 3% sodium
pentobarbital (30 mg/kg intraperitoneally; Sigma-Aldrich, St.
Louis, MO, USA), the rats were intubated via tracheotomy and
ventilated with a small-animal ventilator (HX-300S; Chengdu TME
Technology Co., Chengdu, China). The heart was exposed through left
fourth intercostal lateral thoracotomy, and the AMI model was
induced by permanently ligating the left anterior descending artery
~2 mm from its origin as previously described (31,32). At
each time-point, ~5-µl blood samples were collected from the
coronary sinus and inferior vena cava using a 30-gauge needle.
Electrodes were attached to the four limbs for electrocardiography,
and successful creation of AMI was verified by ST-segment elevation
shown by electrocardiography. The rats of the sham-operated group
underwent thoracotomy and pericardiotomy without coronary artery
ligation. The study was approved by the Animal Care and Use
Committee of Shandong University and all procedures involving
animals were conducted in accordance with the Guide for the Care
and Use of Laboratory Animals of the National Institutes of Health
(publication no. 85–23, revised 1996).
Masson's trichrome staining
Masson's trichrome staining was performed as
previously described (33). Briefly,
the rats of the MI 7-day group were decapitated following blood
collection. Subsequently, their hearts were removed, washed and
fixed in Bouin's solution [Tiangen Biotech (Beijing) Co.,
Ltd.,China] for 2 h. They were then embedded in optimum cutting
temperature compound (Tissue-Tek; Miles Laboratories, Inc.,
Elkhart, IN, USA) by dry ice-ethanol bath. The frozen-embedded rat
hearts were transversely sectioned (6 µm) and stained with
Weigert's iron hematoxylin (Shanghai Jinpan Biotech Co., Ltd.,
Shanghai, China) for 10 min, then washed and stained in 1%
ponceau-acetic acid solution (mixture of equal volumes of 0.5%
ponceau 2R in 1% acetic acid and 0.5% acid fuchsin in 1% acetic
acid) for 5 min. Following washing with phosphate-buffered saline
(PBS), the sections were incubated with 1% phosphomolybdic acid for
5 min and counterstained light green. The images were captured
under an Olympus FSX200 microscope (Olympus Corporation, Tokyo,
Japan).
ELISA
The rat blood samples were centrifuged at 1,075 × g
for 2 min at 4°C, and the supernatant (blood plasma) was collected.
Then, the plasma samples were diluted 1:20 with PBS for the
detection of vWF and TNF-α protein levels using a vWF ELISA kit
(Ramco Laboratories Inc., Stafford, TX, USA) and a TNF-α Rat ELISA
kit (Abcam, Cambridge, MA, USA), respectively. For cell culture,
HUVECs were grown to confluence and serum/growth factor-free media
containing 0, 10 or 50 ng/ml TNF-α (Miltenyi Biotec, Bergisch
Gladbach, Germany) was applied. At each time-point, the media were
collected for detection of the vWF protein level using the vWF
ELISA kit. The measurements were performed 4 times (n=4).
Cell culture
Human umbilical vascular endothelial cells (HUVECs)
were purchased from the American Type Culture Collection (Manassas,
VA, USA) and maintained in endothelial growth media (EGM-2)
supplemented with EGM™-2-MV bullet kit (Lonza, Basel, Switzerland)
and containing antibiotics (100 IU/ml penicillin and 100 µg/ml
streptomycin), in humidified air at 37°C with 5%
CO2.
Reverse transcription-quantitative
polymerase chain reaction (RT-qPCR)
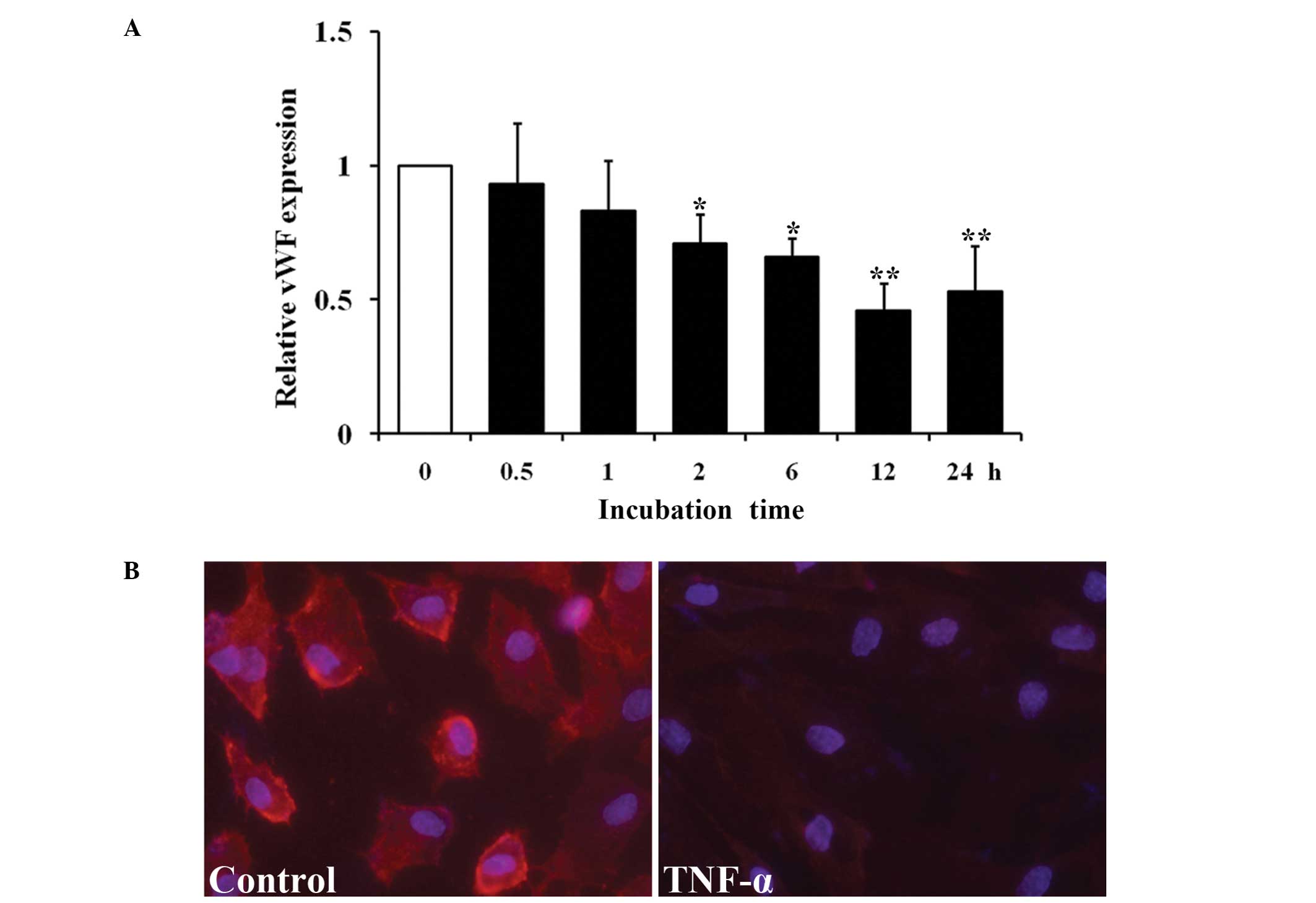
Total RNA was isolated from HUVECs treated with 10
ng/ml TNF-α at 37°C at each time-point (0, 0.5, 1, 2, 6, 12 and 24
h) using the RNeasy Mini kit (Qiagen, Hilden, Germany). cDNA was
synthesized using the High Capacity RNA-to-cDNA Master Mix (Applied
Biosystems-Life Technologies, Carlsbad, CA, USA). RT-qPCR was
performed using SYBR Green master mixes (Life Technologies) with a
ViiA7 Real-Time PCR system (Life Technologies). All PCR reactions
were repeated in triplicate. The relative expression of vWF was
calculated using GAPDH as an endogenous internal control. The
primer sequences are listed in Table
I.
 | Table I.Reverse transcription-quantitative
polymerase chain reaction primer sequences. |
Table I.
Reverse transcription-quantitative
polymerase chain reaction primer sequences.
| Gene |
Sense/antisense | Primer
sequence | Size (bp) | Tm (°C) |
|---|
| vWF | Sense |
CGGCTTGCACCATTCAGCTA | 90 | 61.5 |
|
| Antisense |
TGCAGAAGTGAGTATCACAGCCATC |
|
|
| GAPDH | Sense |
TGATGACATCAAGAAGGTGGTGAAG | 240 | 57.9 |
|
| Antisense |
TCCTTGGAGGCCATGTGGGCCAT |
|
|
Immunofluorescence
HUVEC monolayers grown on fibronectin-coated glass
chamber slides were exposed to 0 or 10 ng/ml TNF-α. After 24 h, the
media was aspirated and the monolayers were washed with PBS
containing 100 mM L-glycine, fixed with 4% paraformaldehyde, and
re-washed with PBS. Immunofluorescence assay was performed using a
primary polyclonal rabbit anti-human vWF antibody (cat. no.,
A008229; dilution, 1:200; Dako, Glostrup, Denmark) and an Alexa
Fluor® 546 polyclonal anti-rabbit secondary antibody (cat. no.,
A-11035; dilution,1:200; Life Technologies). The cells were
incubated with the primary antibody overnight at 4°C, washed with
PBS and then incubated with the secondary antibody for 1 h at room
temperature. Photographic images of the slides were captured using
an Olympus FSX200 microscope (Olympus Corporation) with an
excitation wavelength of 546 nm.
Statistical analysis
Data are expressed as the mean ± standard error. An
unpaired, two-tailed Student's t-test was used for the comparison
between means. The SPSS 17.0 software for Windows (SPSS Inc.,
Chicago, IL, USA) was used for the statistical analysis. P<0.05
was considered to indicate a statistically significant
difference.
Results
Model establishment
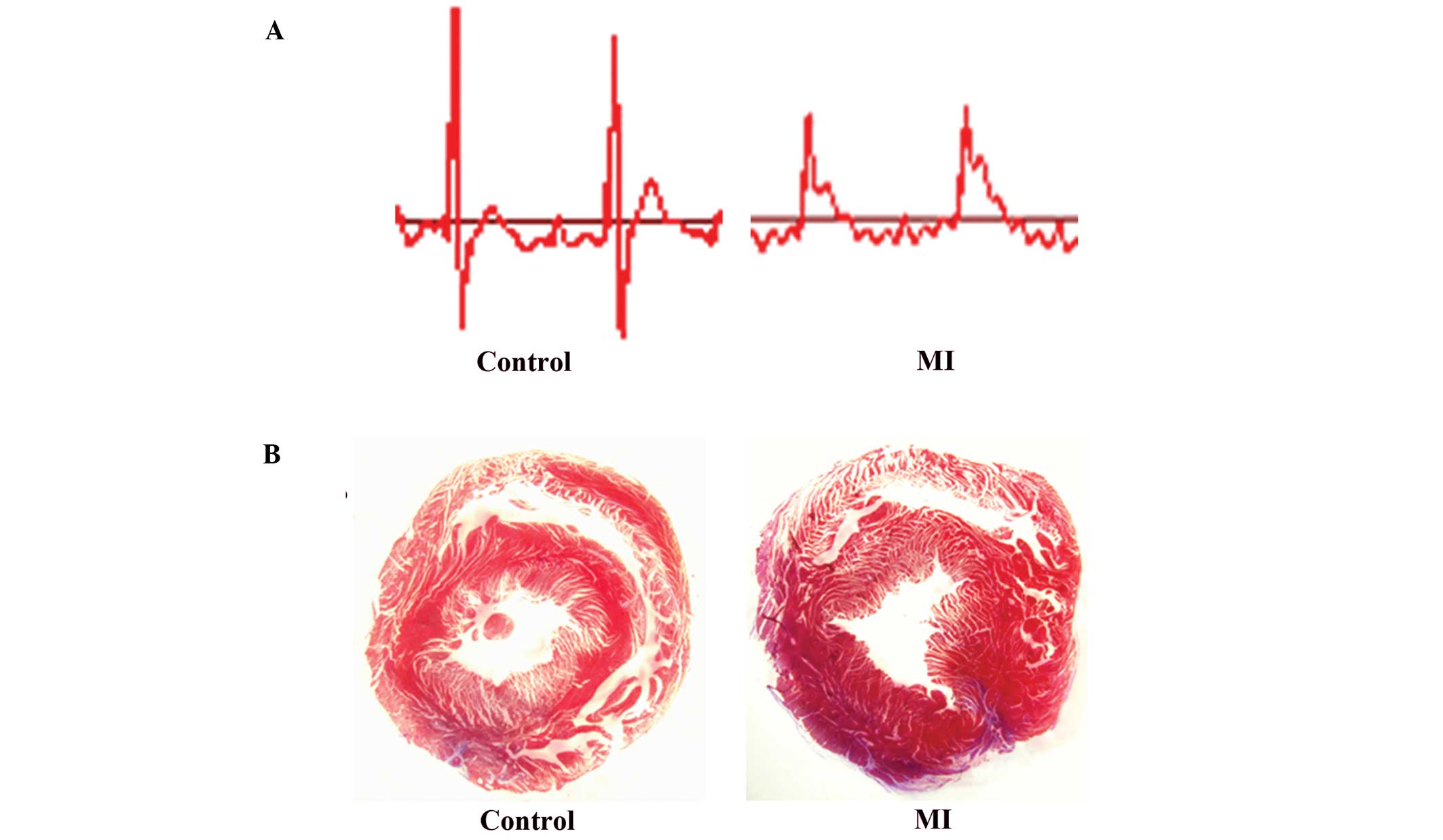
The establishment of the AMI model was confirmed by
the significant ST-segment elevation shown on electrocardiography
(Fig. 1A). Following blood sample
collection at each time-point, the rats were sacrificed and the
hearts were extracted to verify the effects of AMI. The Masson's
trichrome staining results of the sections of the cardiac tissues
from the rats of the AMI model after 7 days are shown in Fig. 1. In these sections, the normal
myocardium was stained red, while the region of fibrosis that
caused infarction damage was stained blue. In the sham-operated
control group, only the perivascular area was stained light blue
(Fig. 1B). By contrast, the
infarcted zone of the AMI group contained a large quantity of blue
fibrotic tissues (Fig. 1B),
suggesting that the AMI model has been successfully developed in
the Wistar rats.
vWF levels in blood plasma
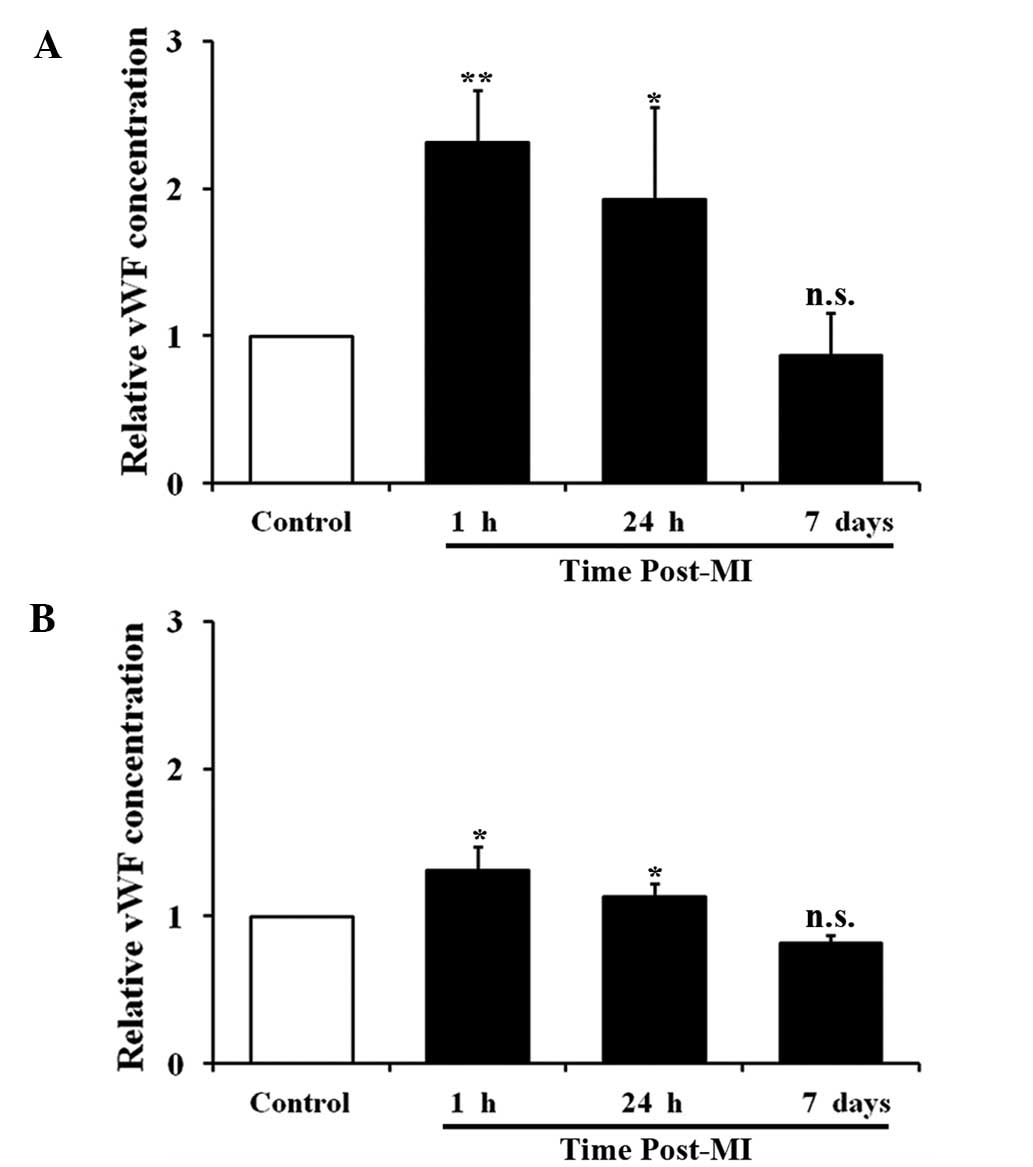
The concentrations of vWF in blood plasma were
detected using ELISA. As shown in Fig.
2, the level of vWF in the cardiac blood collected from the
coronary sinus underwent a 1.31-fold increase (P<0.01) at 1 h
and a 0.88-fold increase (P<0.05) at 24 h following AMI, but
decreased to normal levels by day 7. The level of vWF in the
peripheral blood collected from the inferior vena cava underwent a
0.37-fold increase at 1 h (P<0.05) and a 0.18-fold increase at
24 h (P<0.05), but decreased to normal levels at day 7. Thus,
following AMI, the concentrations of vWF in the cardiac and
peripheral blood increased, peaked at 1 h and then gradually
decreased to normal levels. At the peak level, the increase of vWF
in the peripheral blood (0.37-fold) was considerably smaller than
that in the cardiac blood (1.31-fold), suggesting that vWF was
secreted from the heart following MI and diluted through the
circulatory system.
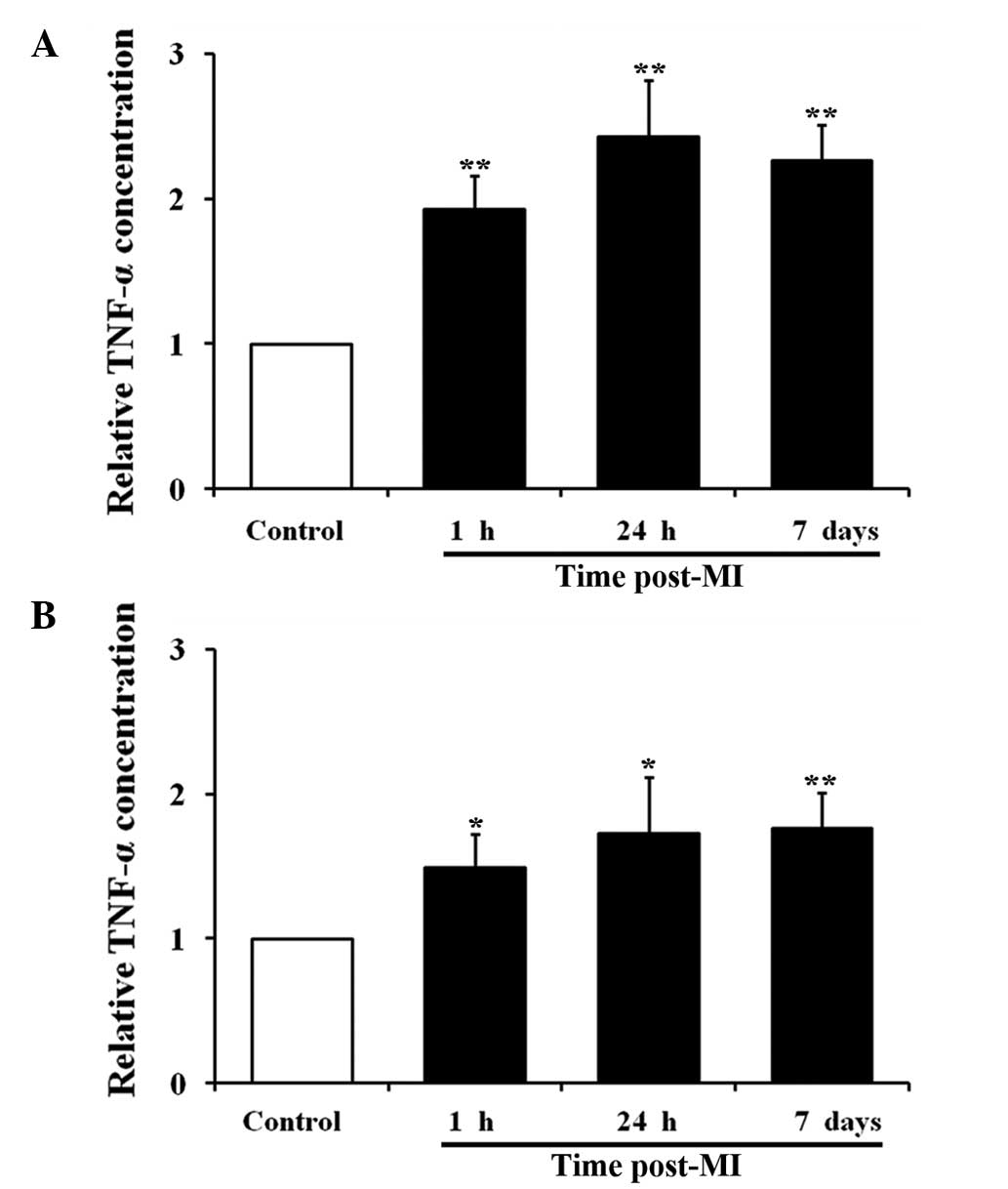
TNF-α levels in blood plasma
TNF-α, a pro-inflammatory cytokine, regulates vWF
expression in the vasculature (34).
The concentration of TNF-α in the blood plasma collected from the
rat model of AMI was examined. The cardiac plasma level of TNF-α
was increased at 1 h (0.89-fold; P<0.05), 24 h (1.32-fold;
P<0.05) and 7 days (1.23-fold; P<0.05) after AMI. The
peripheral plasma level of TNF-α was also increased at all
time-points as follows: 0.53-fold increase at 1 h (P<0.05),
0.71-fold increase at 24 h (P<0.05) and 0.72-fold increase at 7
days (P<0.01). During AMI, TNF-α was also produced in the heart
and diluted through the circulatory system. Unlike vWF, the level
of TNF-α peaked at 24 h, and a high level was maintained until day
7 after AMI (Fig. 3).
Effect of TNF-α on HUVECs
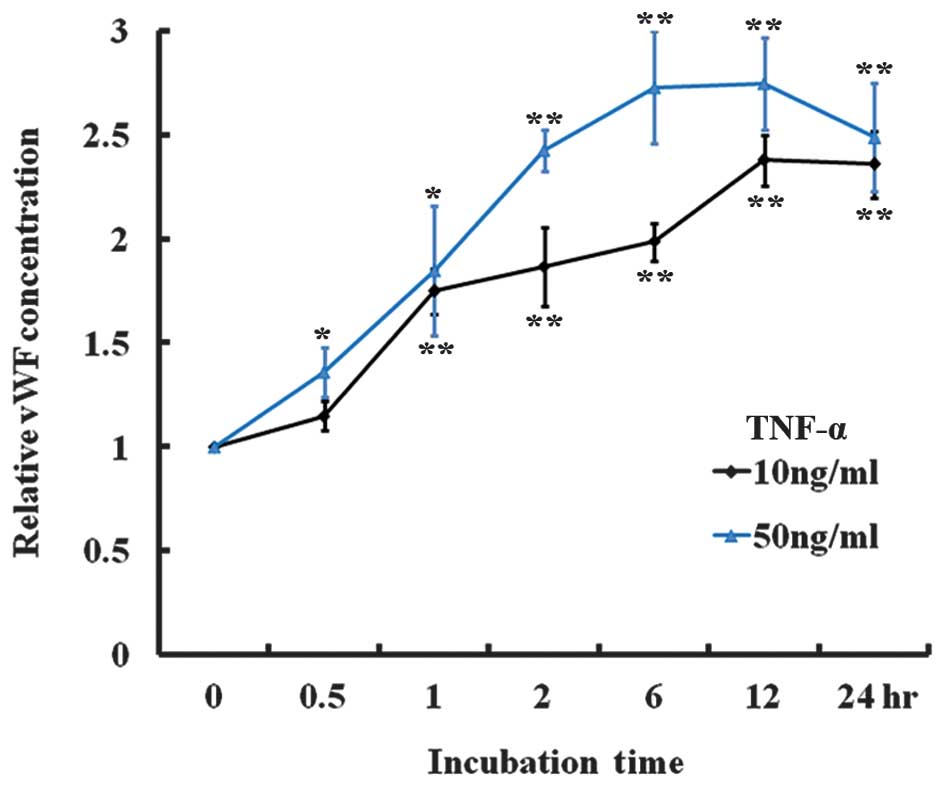
TNF-α was added to the medium of cultured HUVECs and
the vWF secretion in vitro was examined. Following treatment
with 10 or 50 ng/ml TNF-α, the level of vWF secreted into the
medium was significantly increased at all time-points (Fig. 4), suggesting that TNF-α stimulates
vWF secretion. In addition, vWF expression in the HUVECs treated
with 10 ng/ml TNF-α for 24 h was examined. RT-qPCR analysis
indicated that the mRNA level of vWF was significantly decreased at
2 h and continued to decrease until 24 h after treatment (Fig. 5A). An immunofluorescence assay using
a rabbit anti-human vWF antibody was performed on the HUVEC
monolayer. As shown on Fig. 5B, the
vWF protein was abundant on the membranes of the untreated cells
but its expression on the cells following a 24-h treatment with 10
ng/ml TNF-α was considerably reduced. Therefore, TNF-α treatment
increased the secretion of vWF by HUVECs, but decreased the
expression of vWF in the HUVECs.
Discussion
In the present study, a rat model of AMI was
successfully developed, which was validated by the ST-segment
elevation shown on electrocardiography and the results of Masson's
twrichrome staining on the cardiac tissues. The plasma level of
vWF, as determined by ELISA, was transiently increased following
AMI, and then decreased in the cardiac and peripheral blood, while
the level of TNF-α continuously increased until it peaked at 24 h
and remained elevated for 7 days. The in vitro experiments
indicated that TNF-α stimulated vWF secretion but inhibited the
expression of vWF in cultured endothelial cells. The present study,
therefore, partially elucidated the cause of the variation in human
plasma vWF levels during AMI and the underlying mechanisms.
The plasma level of vWF is a potential clinical
marker for AMI and may be a risk factor for recurrent myocardial
infarction (35). A number of
studies have investigated the associations between vWF plasma
levels and AMI events (22,23); however the results are inconsistent
and the conclusions remain controversial. The present study
determined the plasma level of vWF in a rat AMI model, and
indicated that vWF is transiently increased following AMI in the
cardiac and peripheral blood. This time-course is consistent with
the results of a clinical study that recorded the progression of
AMI precisely, and reported that the vWF concentration was
significantly increased at the onset stage of AMI and normalized 14
days following AMI (36). The
present findings suggest that a higher plasma level of vWF is
associated with the early stage but not the later stage of AMI. In
addition, the discrepancies between this and previous studies are,
at least partially, due to the different time-points of blood
collection from patients.
Inflammation plays an important role in AMI, and
TNF-α is the central regulator of inflammation (37,38). At
low levels, TNF-α exhibits a cardioprotective effect, whereas high
levels of TNF-α induce myocardial damage (39,40).
TNF-α is produced primarily by activated macrophages and expressed
by multiple cell types in the heart (41,42).
During AMI, the expression of TNF-α is increased in cardiac tissues
(43). In the present study, it was
found that the plasma level of TNF-α continuously increased during
the first 24 h and was maintained at a high level for the 7-day
period following AMI, suggesting that circulating TNF-α could be
associated with AMI. These results are consistent with the findings
of clinical studies, which support that observation that the TNF-α
level is higher in patients with AMI (25,44). The
increase in the level of TNF-α may be caused by both the
ischemia-induced damage of myocardial tissues and the late
consequences of tissue repair (40,45).
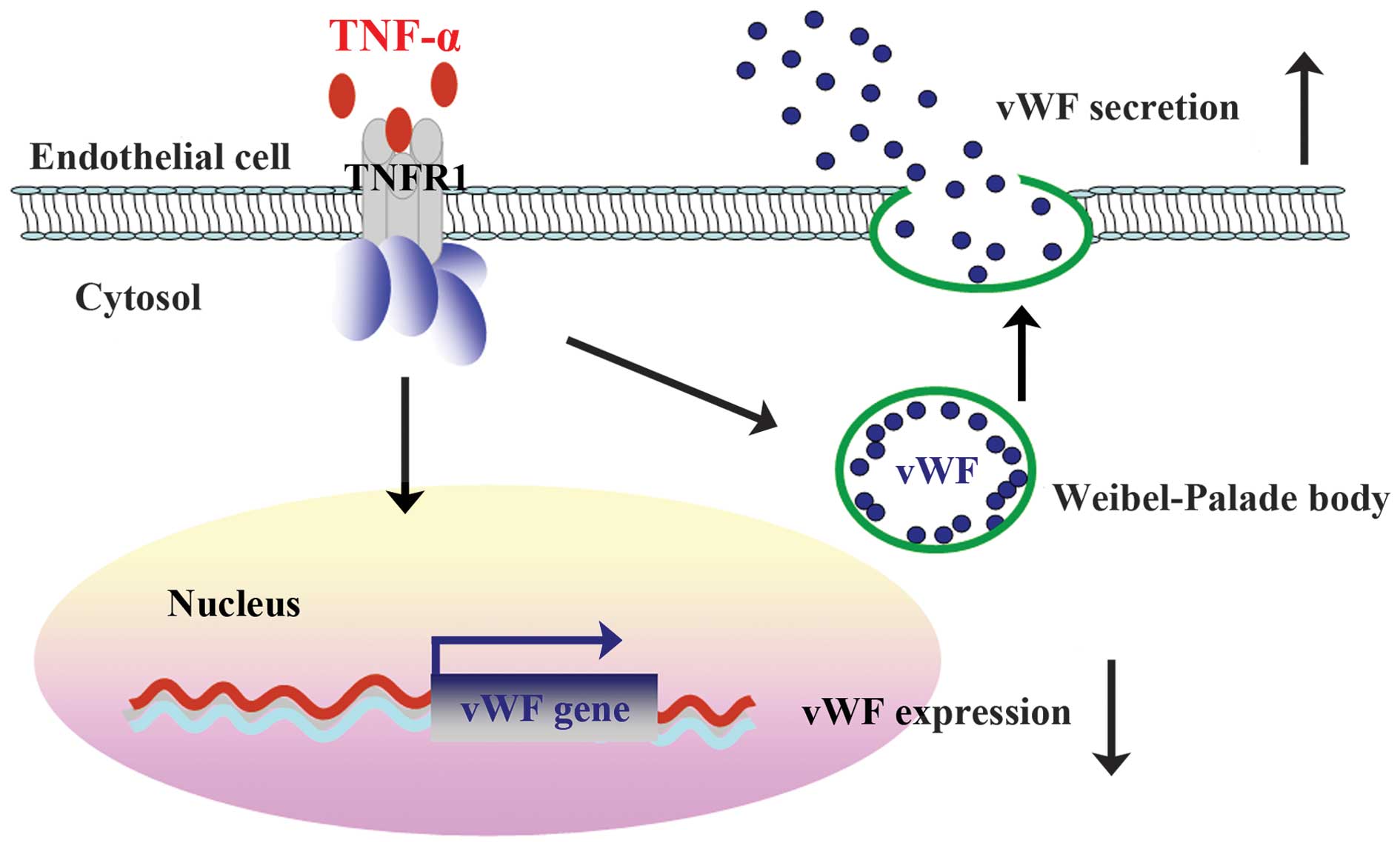
TNF-α in blood plasma interacts with its receptors
on the membrane of endothelial cells, triggers a collection of
signaling pathways and regulates various cellular processes
(46,47). In healthy humans, the intravenous
injection of recombinant TNF-α has been found to stimulate the
release of vWF from storage into the circulation, which is one of
the consequences of TNF-α-induced endothelial cell activation
(48). Through in vitro
experiments in the present study, it was also observed that
TNF-α-induced an increase in vWF secretion; however, TNF-α was
shown to downregulate the mRNA and protein expression of vWF
(Fig. 6). It has previously been
discovered that transcription factor GATA3 and ETS transcription
factor ERG are positive regulators of vWF expression (12,34).
TNF-α inhibits the expression of these transcription factors in
endothelial cells (18,49), thus repressing the expression of vWF.
As the expression of vWF is decreased, the TNF-α-induced secretion
of vWF reaches a peak shortly afterwards and then decreases.
In conclusion, the present study found that the
plasma level of vWF is transiently elevated in a rat model of AMI,
which may result from a TNF-α-induced increase in vWF secretion and
reduction in vWF expression. The present results suggest that
plasma level of vWF may be a clinical marker of the early stage of
AMI. Future studies are required in order to elucidate the role of
vWF in the progression of AMI and the underlying mechanism.
Acknowledgements
This study was supported by a grant from the
National Natural Science Foundation of China (grant no. 81370269).
The authors are grateful for the funding received from the Shandong
Taishan Scholarship.
References
|
1
|
Ruggeri ZM: Von Willebrand factor,
platelets and endothelial cell interactions. J Thromb Haemost.
1:1335–1342. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Lenting PJ, Christophe OD and Denis CV:
von Willebrand factor biosynthesis, secretion and clearance:
Connecting the far ends. Blood. 125:2019–2028. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Sadler JE: von Willebrand factor assembly
and secretion. J Thromb Haemost. 7(Suppl 1): S24–S27. 2009.
View Article : Google Scholar
|
|
4
|
Kanaji S, Fahs SA, Shi Q, Haberichter SL
and Montgomery RR: Contribution of platelet vs. endothelial VWF to
platelet adhesion and hemostasis. J Thromb Haemost. 10:1646–1652.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Metcalf DJ, Nightingale TD, Zenner HL,
Lui-Roberts WW and Cutler DF: Formation and function of
Weibel-Palade bodies. J Cell Sci. 121:19–27. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Nightingale T and Cutler D: The secretion
of von Willebrand factor from endothelial cells; an increasingly
complicated story. J Thromb Haemost. 11(Suppl 1): S192–S201. 2013.
View Article : Google Scholar
|
|
7
|
Yee A and Kretz CA: Von Willebrand factor:
Form for function. Semin Thromb Hemost. 40:17–27. 2014.PubMed/NCBI
|
|
8
|
Lenting PJ, Pegon JN, Groot E and de Groot
PG: Regulation of von Willebrand factor-platelet interactions.
Thromb Haemost. 104:449–455. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Franchini M, Frattini F, Crestani S,
Bonfanti C and Lippi G: von Willebrand factor and cancer: A renewed
interest. Thromb Res. 131:290–292. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Lenting PJ, Casari C, Christophe OD and
Denis CV: von Willebrand factor: The old, the new and the unknown.
J Thromb Haemost. 10:2428–2437. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Randi AM, Laffan MA and Starke RD: Von
Willebrand factor, angiodysplasia and angiogenesis. Mediterr J
Hematol Infect Dis. 5:e20130602013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Jahroudi N and Lynch DC:
Endothelial-cell-specific regulation of von Willebrand factor gene
expression. Mol Cell Biol. 14:999–1008. 1994.PubMed/NCBI
|
|
13
|
Lillicrap D: von Willebrand disease:
Advances in pathogenetic understanding, diagnosis and therapy.
Blood. 122:3735–3740. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Yamamoto K, de Waard V, Fearns C and
Loskutoff DJ: Tissue distribution and regulation of murine von
Willebrand factor gene expression in vivo. Blood. 92:2791–2801.
1998.PubMed/NCBI
|
|
15
|
Aird WC, Jahroudi N, Weiler-Guettler H,
Rayburn HB and Rosenberg RD: Human von Willebrand factor gene
sequences target expression to a subpopulation of endothelial cells
in transgenic mice. Proc Natl Acad Sci USA. 92:4567–4571. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Aird WC, Edelberg JM, Weiler-Guettler H,
Simmons WW, Smith TW and Rosenberg RD: Vascular bed-specific
expression of an endothelial cell gene is programmed by the tissue
microenvironment. J Cell Biol. 138:1117–1124. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Bertagna A and Jahroudi N: The NFY
transcription factor mediates induction of the von Willebrand
factor promoter by irradiation. Thromb Haemost. 85:837–844.
2001.PubMed/NCBI
|
|
18
|
Liu J, Kanki Y, Okada Y, Jin E, Yano K,
Shih SC, Minami T and Aird WC: A +220 GATA motif mediates basal but
not endotoxin-repressible expression of the von Willebrand factor
promoter in Hprt-targeted transgenic mice. J Thromb Haemost.
7:1384–1392. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Mojiri A, Nakhaii-Nejad M, Phan WL, Kulak
S, Radziwon-Balicka A, Jurasz P, Michelakis E and Jahroudi N:
Hypoxia results in upregulation and de novo activation of von
Willebrand factor expression in lung endothelial cells.
Arterioscler, Thromb Vasc Biol. 33:1329–1338. 2013. View Article : Google Scholar
|
|
20
|
Kleinschmidt AM, Nassiri M, Stitt MS,
Wasserloos K, Watkins SC, Pitt BR and Jahroudi N: Sequences in
intron 51 of the von Willebrand factor gene target promoter
activation to a subset of lung endothelial cells in transgenic
mice. J Biol Chem. 283:2741–2750. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Nassiri M, Liu J, Kulak S, Uwiera RR, Aird
WC, Ballermann BJ and Jahroudi N: Repressors NFI and NFY
participate in organ-specific regulation of von Willebrand factor
promoter activity in transgenic mice. Arterioscler, Thromb Vasc
Biol. 30:1423–1429. 2010. View Article : Google Scholar
|
|
22
|
Paulinska P, Spiel A and Jilma B: Role of
von Willebrand factor in vascular disease. Hamostaseologie.
29:32–38. 2009.PubMed/NCBI
|
|
23
|
Spiel AO, Gilbert JC and Jilma B: von
Willebrand factor in cardiovascular disease: Focus on acute
coronary syndromes. Circulation. 117:1449–1459. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
White HD and Chew DP: Acute myocardial
infarction. Lancet. 372:570–584. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Hori M and Nishida K: Oxidative stress and
left ventricular remodelling after myocardial infarction.
Cardiovasc Res. 81:457–464. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
White HD, Thygesen K, Alpert JS and Jaffe
AS: Clinical implications of the third universal definition of
myocardial infarction. Heart. 100:424–432. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Peyvandi F, Hollestelle MJ, Palla R,
Merlini PA, Feys HB, Vanhoorelbeke K, Lenting PJ and Mannucci PM:
Active platelet-binding conformation of plasma von Willebrand
factor in young women with acute myocardial infarction. J Haemost.
8:1653–1656. 2010. View Article : Google Scholar
|
|
28
|
Goto S, Sakai H, Ikeda Y and Handa S:
Acute myocardial infarction plasma augments platelet thrombus
growth in high shear rates. Lancet. 349:543–544. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Jansson JH, Nilsson TK and Johnson O: von
Willebrand factor in plasma: A novel risk factor for recurrent
myocardial infarction and death. Br Heart J. 66:351–355. 1991.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Chion CK, Doggen CJ, Crawley JT, Lane DA
and Rosendaal FR: ADAMTS13 and von Willebrand factor and the risk
of myocardial infarction in men. Blood. 109:1998–2000. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Hu H, Xuan Y, Wang Y, Xue M, Suo F, Li X,
Cheng W, Li X, Yin J, Liu J and Yan S: Targeted NGF siRNA delivery
attenuates sympathetic nerve sprouting and deteriorates cardiac
dysfunction in rats with myocardial infarction. PloS One.
9:e951062014. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Wang Y, Liu J, Suo F, Hu HS, Xue M, Cheng
WJ, Xuan YL and Yan SH: Metoprolol-mediated amelioration of
sympathetic nerve sprouting after myocardial infarction.
Cardiology. 126:50–58. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Zhang WB, Du QJ, Li H, Sun AJ, Qiu ZH, Wu
CN, Zhao G, Gong H, Hu K, Zou YZ and Ge JB: The therapeutic effect
of rosuvastatin on cardiac remodelling from hypertrophy to fibrosis
during the end-stage hypertension in rats. J Cell Mol Med.
16:2227–2237. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Liu J, Yuan L, Molema G, Regan E, Janes L,
Beeler D, Spokes KC, Okada Y, Minami T, Oettgen P and Aird WC:
Vascular bed-specific regulation of the von Willebrand factor
promoter in the heart and skeletal muscle. Blood. 117:342–351.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Rutten B, Maseri A, Cianflone D, Laricchia
A, Cristell NA, Durante A, Spartera M, Ancona F, Limite L, Hu D, et
al: Plasma levels of active Von Willebrand factor are increased in
patients with first ST-segment elevation myocardial infarction: A
multicenter and multiethnic study. Eur Heart J Acute Cardiovasc
Care. 4:64–74. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Sakai H, Goto S, Kim JY, Aoki N, Abe S,
Ichikawa N, Yoshida M, Nagaoka Y and Handa S: Plasma concentration
of von Willebrand factor in acute myocardial infarction. Thromb
Haemost. 84:204–209. 2000.PubMed/NCBI
|
|
37
|
Frangogiannis NG, Smith CW and Entman ML:
The inflammatory response in myocardial infarction. Cardiovasc Res.
53:31–47. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Dinarello CA and Pomerantz BJ:
Proinflammatory cytokines in heart disease. Blood Purif.
19:314–321. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Hall G, Hasday JD and Rogers TB:
Regulating the regulator: NF-kappaB signaling in heart. J Mol Cell
Cardiol. 41:580–591. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Kleinbongard P, Schulz R and Heusch G:
TNFα in myocardial ischemia/reperfusion, remodeling and heart
failure. Heart Fail Rev. 16:49–69. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Mann DL: Tumor necrosis factor-induced
signal transduction and left ventricular remodeling. J Card Fail.
8(Suppl 6): S379–S386. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Bradham WS, Bozkurt B, Gunasinghe H, Mann
D and Spinale FG: Tumor necrosis factor-alpha and myocardial
remodeling in progression of heart failure: A current perspective.
Cardiovasc Res. 53:822–830. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Jacobs M, Staufenberger S, Gergs U, Meuter
K, Brandstätter K, Hafner M, Ertl G and Schorb W: Tumor necrosis
factor-alpha at acute myocardial infarction in rats and effects on
cardiac fibroblasts. J Mol Cell Cardiol. 31:1949–1959. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Blake GJ: Inflammatory biomarkers of the
patient with myocardial insufficiency. Curr Opin Crit Care.
9:369–374. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Schulz R, Aker S, Belosjorow S and Heusch
G: TNFalpha in ischemia/reperfusion injury and heart failure. Basic
Res Cardiol. 99:8–11. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Zhang H, Park Y, Wu J, Chen Xp, Lee S,
Yang J, Dellsperger KC and Zhang C: Role of TNF-alpha in vascular
dysfunction. Clin Sci (Lond). 116:219–230. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Madge LA and Pober JS: TNF signaling in
vascular endothelial cells. Exp Mol Pathol. 70:317–325. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
48
|
van der Poll T, van Deventer SJ,
Pasterkamp G, van Mourik JA, Büller HR and ten Cate JW: Tumor
necrosis factor induces von Willebrand factor release in healthy
humans. Thromb Haemost. 67:623–626. 1992.PubMed/NCBI
|
|
49
|
Umetani M, Mataki C, Minegishi N, Yamamoto
M, Hamakubo T and Kodama T: Function of GATA transcription factors
in induction of endothelial vascular cell adhesion molecule-1 by
tumor necrosis factor-alpha. Arterioscler Thromb Vasc Biol.
21:917–922. 2001. View Article : Google Scholar : PubMed/NCBI
|