Introduction
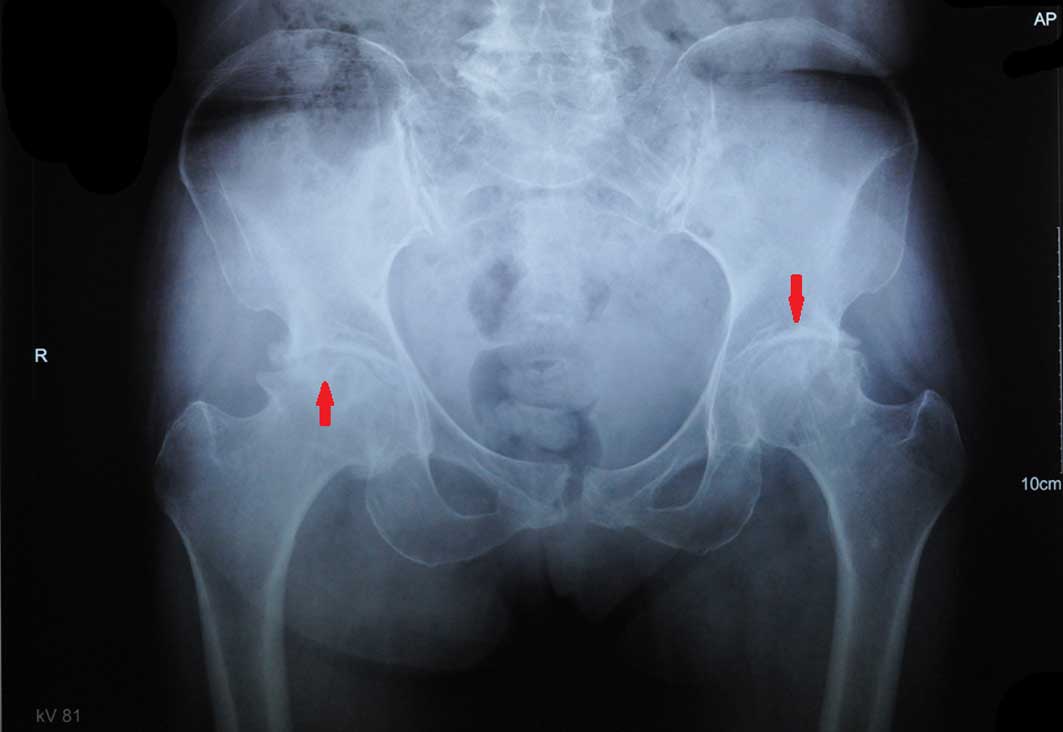
Osteoarthritis is a commonly occurring disease, with
the clinical manifestations of joint pain, swelling and progressive
loss of function (Fig. 1).
Osteoarthritis increases in prevalence with age and is estimated
that 40% of people >70 years old are affected by this disease
(1). Synovial inflammation is
associated with a number of the signs and symptoms of
osteoarthritis, including joint swelling and effusion (2). This multifactorial disease is
characterized by destruction of the articular cartilage and
subchondral bone alterations (3).
The degeneration of the joints is a major cause of disability,
which reduces the quality of life. Clinically speaking,
degeneration particularly affects the large weight-bearing joints
of the legs, namely the hips and knees, but can potentially affect
any joint of the body, including the hands and spine (4,5). The
manifestations of the disease can vary in severity, but the
majority of patients do not require major interventions and receive
only intermittent symptom relief. However, in certain patients, the
disease progresses rapidly, leading to disability and ultimately
joint replacement (6). Current
treatments for osteoarthritis, such as non-steroidal
anti-inflammatory drugs, are administered to provide symptomatic
relief but lack efficacy in controlling the progression of the
disease (7,8).
Vitamin E has various biological functions that have
been attributed to its ability to protect an organism against the
damaging effects of free radicals by acting as a lipid-based
radical chain reaction terminator (9). Vitamin E is a fat-soluble,
water-insoluble, light yellow oil, that is stable to heat and
acids, but rather unstable under alkali conditions, in which it is
slowly oxidized. It can be found in the nonsaponifiable fractions
of vegetable oils and plays various important roles, for example,
as an antioxidant and anti-apoptotic agent, in numerous
physiological and pathological conditions (10). Various theories on the pathology of
osteoarthritis are being investigated that may lead to new
therapeutic options. These relate to the role of skeletal muscle
(11–14), the effect of nucleic acid metabolism
(15,16), sex gland functions (17–19), the
action of stable mast cells (20,21) and
the importance of the subchondral vascular system (9,22,23) in
osteoarthritis and its progression. In the present review, the
possibility that vitamin E may be able to delay the progression of
osteoarthritis was explored through studying the potential role of
this nutritional factor in each of these mechanisms. The
association between the antioxidation effect (24) of vitamin E and these mechanisms in
osteoarthritis (25) is also
explored.
Vitamin E maintains skeletal muscle which
may slow down the rate of joint degeneration
Vitamin E is essential for the structural and
functional maintenance of skeletal muscle (11,12). A
study by Chang et al indicated that vitamin E influences the
training-induced adaptation of glutathione peroxidase (GPX) and
superoxide dismutase (SOD) activities in rat skeletal muscle
(11); in rats, the deprivation of
vitamin E increased the exercise-induced elevation in GPX activity
and inhibited exercise-induced SOD activity (14). A study conducted by Baumgartner et
al showed that mild oxidative stress led to activation of the
intrinsic pathway of apoptosis and death in skeletal muscle cells,
which was reduced by supplementation of the culture medium with
vitamin E (26). The effects of
vitamin E on muscle have been suggested to be of greater importance
than those on fertility (27). A
deficiency of vitamin E causes muscular dystrophy and morphologic
changes in various tissues, accompanied by increased oxygen
consumption and alterations in chemical composition and functional
behavior of the muscle. Creatine elimination then is increased,
which is hypothesized to be the result of an inability of the
skeletal muscle to utilize creatine (28). A study of joint degeneration in
rabbits conducted by Rehan Youssef et al indicated that
quadriceps weakness is a risk factor for osteoarthritis through its
functional implications on joint loading, and leads to the onset
and progression of osteoarthritic changes in the patellofemoral
joint (13). The contribution of
muscle weakness to joint loading and the progression of
osteoarthritis has been confirmed in humans (29).
Vitamin E has a gene regulatory function
that may delay the development of osteoarthritis
In animals, vitamin E deficiency causes derangement
of nucleic acid metabolism (30,31).
These results show that serum vitamin E is a determinant of bone
mass through its regulation of osteoclast fusion. Data discussed in
a review by Azzi et al support evidence of a gene regulatory
function of vitamin E (9); this
comprises the observation of an elevated output of the purine
metabolite allantoin in vitamin E-deficient rabbits, and changes in
the levels of tissue nucleic acids. Hartman et al conducted
a study of exercise-induced DNA damage in human subjects using DNA
strand breaks in white blood cells as a biomarker (16), and found that supplementation with
vitamin E for 2 weeks was effective in reducing DNA damage after an
incremental exercise test to exhaustion. In a study conducted by
Baskin et al (32), following
3 days of endurance training in sled dogs, supplementation with
vitamin E and lutein for 1 month was associated with a reduction in
oxidative DNA damage, as demonstrated by decreased levels of
7,8-dihydro-8-oxo-2′-deoxyguanosine (8-OHdG) in the plasma, whereas
untreated dogs showed an increase in 8-OHdG levels. Various nuclear
changes can be observed in tissues that are severely affected by a
deficiency of vitamin E (30).
Cell-based assays demonstrated that α-tocopherol stimulates
osteoclast fusion, independent of its antioxidant capacity, by
inducing the expression of dendritic-cell-specific transmembrane
protein. This protein is an essential molecule for osteoclast
fusion, which occurs via the activation of mitogen-activated
protein kinase 14 (p38) and microphthalmia-associated transcription
factor, as well as via its direct recruitment to the Tm7sf4
promoter (a gene encoding DC-STAMP) (30). There is a strong hereditary component
to osteoarthritis, reflected by high heritability estimates from
twin studies (33). Thus, the gene
regulatory function of vitamin E is likely to play an important
role in delaying the progression of osteoarthritis. As insights
into the molecular mechanisms involved in the initiation and
progression of osteoarthritis are gained, certain pathways involved
in joint metabolism, including Wnt/β-catenin, discoidin domain
receptor 2 and proteinase-activated receptor-2 pathways are being
closely examined and their relevance to osteoarthritis evaluated
(7).
Vitamin E maintains sex organ functions
which may delay the progression of osteoarthritis
Vitamin E has important effects on the reproductive
system. Free radicals and reactive oxygen species, such as hydroxyl
radicals, superoxide and hydrogen peroxides, can cause lipid
peroxidation (18). Deficiency of
vitamin E may lead to damage of the reproductive organs, resulting
in conditions such as testicular damage, degenerative spermatogonia
and degeneration of the seminiferous tubules (34). A study in goats conducted by Hong
et al found that vitamin E supplementation improved the
weight of the epididymis, the density and diameters of convoluted
seminiferous tubules, spermatogenic cell density and epididymis
ductule diameters, particularly when administered at dosages of 80
and 320 IU/day (19). A study
conducted by Rao et al to investigate nickel- and/or
chromium-induced toxicity in the mouse ovary suggested that vitamin
E exerted a protective effect by preventing lipid peroxidation and
protecting the antioxidant system (35). Sex organs play a vital role in
secretion. Estrogens have been proposed to act as protective
factors by certain authors, but as pathogenic determinants of
osteoarthritis by others (36).
While the effects of hormone replacement therapy (HRT) in
osteoarthritis appear to be modest, some large observational
studies have concluded that when administered over a prolonged
period, HRT may exert a beneficial effect on the structural
progression of osteoarthritis, particularly in the lower limbs
(37).
Vitamin E regulates mast cell stability
which may reduce inflammation associated with osteoarthritis
Mast cells are a unique type of immune cell that can
be activated by various non-immune processes, including acute
stress (38), and participate in a
variety of inflammatory diseases affecting the skin and joints
(39). The role of mast cells in the
immune system involves interaction with B and T cells and the
release of mediators (such as IL-4, IL-5 and IL-6) involved in the
activation of other cells (such as granulocytes and mast cells)
(40). Mast cells are reported to be
present in joints (41), and they
are suggested to be involved in inflammatory arthritis (42). It has also been reported that mast
cells are required for autoimmune arthritis (43). Hyperactivity of mast cells and their
uncontrolled accumulation in tissues increases the release of
inflammatory mediators contributing to the pathogenesis of several
diseases, including arthritis and asthma (40). Natural vitamin E analogs have
differing modulatory effects on signal transduction and gene
expression in various cell lines; in mast cells, vitamin E affects
protein kinase C, protein phosphatase 2A and protein kinase B,
which leads to the modulation of proliferation, apoptosis,
secretion and migration; therefore, it is possible that, by
modulating signal transduction and gene expression, vitamin E
prevents diseases with mast cell involvement (21). Mast cell activation is a feature of
osteoarthritis, and carboxypeptidase, chymase and tryptase exhibit
distinct patterns of release and clearance in the synovial fluid of
patients with osteoarthritis (20).
The inflammation associated with osteoarthritis may be reduced by
vitamin E.
Vitamin E protects the subchondral vascular
system which may reduce the necrosis and remodeling of
osteoarthritis
There is evidence indicating that impaired
microvascular blood flow, which may arise due to various
combinations of pro-coagulant factors, can result in symptomatic
osteoarthritis (44). While the
survival of articular chondrocytes depends largely on the diffusion
of nutrients from the synovial fluid, the osteocytes in subchondral
bone obtain nourishment from a well-developed capillary plexus
(23,45). In cases of osteoarthritis, synovial
and subchondral vascular engorgement results in necrosis and the
gradual remodeling of tissue (46).
Vitamin E, along with a network of cellular antioxidant mediators,
including catalases and superoxide dismutase, plays a role in the
elimination of lipid-soluble free radicals through its action as a
free radical scavenger (9).
Furthermore, vitamin E is involved in the regulation of certain
cellular events, such as the cell cycle progression of vascular
smooth muscle cells, the expression of adhesion molecules, the
deposition of extracellular matrix and aggregation of platelets
(47). In addition, it attenuates
capillary endothelial swelling in ischemic and remote muscle
(24). It has also been reported
that vitamin E protects vascular walls from damage by limiting cell
proliferation, and by assisting in the stabilization of a fibrous
cap through its effects on components of the extracellular matrix
(48).
Conclusion
Osteoarthritis is a chronic degenerative joint
disorder characterized by destruction of the articular cartilage,
subchondral bone alterations and synovitis (1). It is a multifactorial disorder in which
ageing, genetic, hormonal and mechanical factors are major
contributors to progression (2).
Osteoarthritis occurs as a clinical syndrome when these etiological
factors result in joint damage of sufficient severity to impair
function and produce symptoms. Current treatments are focused on
symptomatic relief but they lack efficacy to control the
progression of this disease, which is a leading cause of
disability.
Vitamin E is a free radical scavenger, which is able
to prevent the oxidation of various readily oxidized substances.
The capacity of vitamin E to act as a lipid-based radical
chain-breaking agent and thereby to protect against free-radical
attack is considered to underlie its effects in the body (49). However, alternative mechanisms of
action have also been proposed, particularly gene regulation.
Vitamin E has exhibited effects at the mRNA and protein levels,
which may be a result of the regulation of gene transcription, mRNA
stability, protein translation, protein stability and
post-translational events (50). The
potential role of vitamin E in a number of mechanisms is summarized
in the present review.
Vitamin E supplementation is safe when appropriate
doses are administered (51). In a
previous review, Kappus and Diplock summarized the tolerance,
toxicological considerations and safety of vitamin E (52). Doses of 100–300 mg/day were concluded
to be well tolerated and to cause no side effects. Doses of 200–400
mg/day have been recommended for use in food supplements, under
certain conditions, and higher doses of 400–2,000 mg/day do not
exhibit side effects in the majority of cases; only at very high
doses of 2,150 mg/day have side effects and intolerance been
increasingly noted. To investigate our hypothesis, that vitamin E
inhibits the progression of osteoarthritis, clinical studies should
be conducted in patients with osteoarthritis to assess the safety
of vitamin E supplementation, and to explore the effect of vitamin
E on the progression of osteoarthritis. As an alternative to oral
administration, vitamin E could also be administered by
intra-articular injection.
The observations summarized in the present review
suggest that vitamin E may have a potent therapeutic effect by
delaying the progression of osteoarthritis through the maintenance
of skeletal muscle, regulation of nucleic acid metabolism,
maintenance of sex organ function, stabilization of mast cells and
protection of the subchondral vascular system. Vitamin E may be an
effective and favorable treatment candidate for osteoarthritis,
leading to pain relief in patients.
References
|
1
|
Dieppe PA and Lohmander LS: Pathogenesis
and management of pain in osteoarthritis. Lancet. 365:965–973.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Benito MJ, Veale DJ, FitzGerald O, van den
Berg WB and Bresnihan B: Synovial tissue inflammation in early and
late osteoarthritis. Ann Rheum Dis. 64:1263–1267. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Goldring MB and Goldring SR:
Osteoarthritis. J Cell Physiol. 213:626–634. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kerkhof HJ, Doherty M, Arden NK, Abramson
SB, Attur M, Bos SD, Cooper C, Dennison EM, Doherty SA, Evangelou
E, et al: Large-scale meta-analysis of interleukin-1 beta and
interleukin-1 receptor antagonist polymorphisms on risk of
radiographic hip and knee osteoarthritis and severity of knee
osteoarthritis. Osteoarthritis Cartilage. 19:265–271. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Aigner T, Sachse A, Gebhard PM and Roach
HI: Osteoarthritis: Pathobiology-targets and ways for therapeutic
intervention. Adv Drug Deliv Rev. 58:128–149. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Luyten FP, Tylzanowski P and Lories RJ:
Wnt signaling and osteoarthritis. Bone. 44:522–527. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Alcaraz MJ, Megías J, García-Arnandis I,
Clérigues V and Guillén MI: New molecular targets for the treatment
of osteoarthritis. Biochem Pharmacol. 80:13–21. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Trijau S, Avouac J, Escalas C, Gossec L
and Dougados M: Influence of flare design on symptomatic efficacy
of non-steroidal anti-inflammatory drugs in osteoarthritis: A
meta-analysis of randomized placebo-controlled trials.
Osteoarthritis Cartilage. 18:1012–1018. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Azzi A, Gysin R, Kempná P, Ricciarelli R,
Villacorta L, Visarius T and Zingg JM: The role of alpha-tocopherol
in preventing disease: From epidemiology to molecular events. Mol
Aspects Med. 24:325–336. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Bourne N, Wathes DC, Lawrence KE, McGowan
M and Laven RA: The effect of parenteral supplementation of vitamin
E with selenium on the health and productivity of dairy cattle in
the UK. Vet J. 177:381–387. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Chang CK, Huang HY, Tseng HF, Hsuuw YD and
Tso TK: Interaction of vitamin E and exercise training on oxidative
stress and antioxidant enzyme activities in rat skeletal muscles. J
Nutr Biochem. 18:39–45. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Nunes VA, Gozzo AJ, Cruz-Silva I, Juliano
MA, Viel TA, Godinho RO, Meirelles FV, Sampaio MU, Sampaio CA and
Araujo MS: Vitamin E prevents cell death induced by mild oxidative
stress in chicken skeletal muscle cells. Comp Biochem Physiol C
Toxicol Pharmacol. 141:225–240. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Rehan Youssef A, Longino D, Seerattan R,
Leonard T and Herzog W: Muscle weakness causes joint degeneration
in rabbits. Osteoarthritis Cartilage. 17:1228–1235. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Clavel S, Farout L, Briand M, Briand Y and
Jouanel P: Effect of endurance training and/or fish oil
supplemented diet on cytoplasmic fatty acid binding protein in rat
skeletal muscles and heart. Eur J Appl Physiol. 87:193–201. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Abel K, Reneland R, Kammerer S, Mah S,
Hoyal C, Cantor CR, Nelson MR and Braun A: Genome-wide SNP
association: Identification of susceptibility alleles for
osteoarthritis. Autoimmun Rev. 5:258–263. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Hartmann A, Niess AM, Grünert-Fuchs M,
Poch B and Speit G: Vitamin E prevents exercise-induced DNA damage.
Mutat Res. 346:195–202. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Claassen H, Schicht M and Paulsen F:
Impact of sex hormones, insulin, growth factors and peptides on
cartilage health and disease. Prog Histochem Cytochem. 45:239–293.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kilarkaje N, Mousa AM, Al-Bader MM and
Khan KM: Antioxidants enhance the recovery of three cycles of
bleomycin, etoposide, and cisplatin-induced testicular dysfunction,
pituitary-testicular axis, and fertility in rats. Fertil Steril.
100:1151–1159. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Hong Z, Hailing L, Hui M and Guijie Z:
Effect of vitamin E supplementation on development of reproductive
organs in Boer goat. Anim Reprod Sci. 113:93–101. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Nakano S, Mishiro T, Takahara S, Yokoi H,
Hamada D, Yukata K, Takata Y, Goto T, Egawa H, Yasuoka S, et al:
Distinct expression of mast cell tryptase and protease activated
receptor-2 in synovia of rheumatoid arthritis and osteoarthritis.
Clin Rheumatol. 26:1284–1292. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Anogeianaki A, Castellani ML, Tripodi D,
Toniato E, De Lutiis MA, Conti F, Felaco P, Fulcheri M, Theoharides
TC, Galzio R, et al: Vitamins and mast cells. Int J Immunopathol
Pharmacol. 23:991–996. 2010.PubMed/NCBI
|
|
22
|
Babarina AV, Möllers U, Bittner K, Vischer
P and Bruckner P: Role of the subchondral vascular system in
endochondral ossification: Endothelial cell-derived proteinases
derepress late cartilage differentiation in vitro. Matrix Biol.
20:205–213. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Kiaer T: Bone perfusion and oxygenation:
Animal experiments and clinical observations. Acta Orthop Scand
Suppl. 257:1–41. 1994.PubMed/NCBI
|
|
24
|
Dai F, Chen WF and Zhou B: Antioxidant
synergism of green tea polyphenols with alpha-tocopherol and
L-ascorbic acid in SDS micelles. Biochimie. 90:1499–1505. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Bai B and Li Y: Danshen prevents articular
cartilage degeneration via antioxidation in rabbits with
osteoarthritis. Osteoarthritis Cartilage. 29:765–773. 2016.
|
|
26
|
Baumgartner HK, Gerasimenko JV, Thorne C,
Ashurst LH, Barrow SL, Chvanov MA, Gillies S, Criddle DN, Tepikin
AV, Petersen OH, et al: Caspase-8-mediated apoptosis induced by
oxidative stress is independent of the intrinsic pathway and
dependent on cathepsins. Am J Physiol Gastrointest Liver Physiol.
293:G296–G307. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Jukola E, Hakkarainen J, Saloniemi H and
Sankari S: Blood selenium, vitamin E, vitamin A and beta-carotene
concentrations and udder health, fertility treatments and
fertility. J Dairy Sci. 79:838–845. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Aoki MS, Lima WP, Miyabara EH, Gouveia CH
and Moriscot AS: Deleterious effects of immobilization upon rat
skeletal muscle: Role of creatine supplementation. Clin Nutr.
23:1176–1183. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Shelburne KB, Torry MR and Pandy MG:
Contributions of muscles, ligaments and the ground-reaction force
to tibiofemoral joint loading during normal gait. J Orthop Res.
24:1983–1990. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Fujita K, Iwasaki M, Ochi H, Fukuda T, Ma
C, Miyamoto T, Takitani K, Negishi-Koga T, Sunamura S, Kodama T, et
al: Vitamin E decreases bone mass by stimulating osteoclast fusion.
Nat Med. 18:589–594. 2012. View
Article : Google Scholar : PubMed/NCBI
|
|
31
|
Ӧzer NK, Negis Y, Aytan N, Villacorta L,
Ricciarelli R, Zingg JM and Azzi A: Vitamin E inhibits CD36
scavenger receptor expression in hypercholesterolemic rabbits.
Atherosclerosis. 184:15–20. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Baskin CR, Hinchcliff KW, DiSilvestro RA,
Reinhart GA, Hayek MG, Chew BP, Burr JR and Swenson RA: Effects of
dietary antioxidant supplementation on oxidative damage and
resistance to oxidative damage during prolonged exercise in sled
dogs. Am J Vet Res. 61:886–891. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Spector TD, Perry LA and Jubb RW:
Endogenous sex steroid levels in women with generalised
osteoarthritis. Clin Rheumatol. 10:316–319. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Wilson MJ, Kaye D, Smith WE, Quach HT,
Sinha AA and Vatassery GT: Effect of vitamin E deficiency on the
growth and secretory function of the rat prostatic complex. Exp Mol
Pathol. 74:267–275. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Rao MV, Chawla SL and Sharma SR:
Protective role of vitamin E on nickel and/or chromium induced
oxidative stress in the mouse ovary. Food Chem Toxicol.
47:1368–1371. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Reginster JY, Kvasz A, Bruyere O and
Henrotin Y: Is there any rationale for prescribing hormone
replacement therapy (HRT) to prevent or to treat osteoarthritis?
Osteoarthritis Cartilage. 11:87–91. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Felson DT, Lawrence RC, Dieppe PA, Hirsch
R, Helmick CG, Jordan JM, Kington RS, Lane NE, Nevitt MC, Zhang Y,
et al: Osteoarthritis: New insights. Part 1: The disease and its
risk factors. Ann Intern Med. 133:635–646. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Theoharides TC: Mast cells and stress - a
psychoneuroimmunological perspective. J Clin Psychopharmacol.
22:103–108. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Theoharides TC and Cochrane DE: Critical
role of mast cells in inflammatory diseases and the effect of acute
stress. J Neuroimmunol. 146:1–12. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Zingg JM: Vitamin E and mast cells. Vitam
Horm. 76:393–418. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Gotis-Graham I, Smith MD, Parker A and
McNeil HP: Synovial mast cell responses during clinical improvement
in early rheumatoid arthritis. Ann Rheum Dis. 57:664–671. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Wooley DE: Mast cells in the rheumatoid
lesion-ringleaders or innocent bystanders? Ann Rheum Dis.
54:533–534. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Lee DM, Friend DS, Gurish MF, Benoist C,
Mathis D and Brenner MB: Mast cells: A cellular link between
autoantibodies and inflammatory arthritis. Science. 297:1689–1692.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Corrado A, Neve A and Cantatore FP:
Expression of vascular endothelial growth factor in normal,
osteoarthritic and osteoporotic osteoblasts. Clin Exp Med.
13:81–84. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Pedersen NW, Kiaer T, Kristensen KD and
Starklint H: Intraosseous pressure, oxygenation and histology in
arthrosis and osteonecrosis of the hip. Acta Orthop Scand.
60:415–417. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Ghosh P and Smith M: The role of
cartilage-derived antigens, pro-coagulant activity and fibrinolysis
in the pathogenesis of osteoarthritis. Med Hypotheses. 41:190–194.
1993. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Villacorta L, Azzi A and Zingg JM:
Regulatory role of vitamins E and C on extracellular matrix
components of the vascular system. Mol Aspects Med. 28:507–537.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Chiquet M, Renedo AS, Huber F and Flück M:
How do fibroblasts translate mechanical signals into changes in
extracellular matrix production? Matrix Biol. 22:73–80. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Azzi A and Stocker A: Vitamin E:
Non-antioxidant roles. Prog Lipid Res. 39:231–255. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Ricciarelli R, Zingg JM and Azzi A:
Vitamin E 80th anniversary: A double life, not only fighting
radicals. IUBMB Life. 52:71–76. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
WU J, Karlsson K and Danielsson Å: Effects
of vitamins E, C and catalase on bromobenzene- and hydrogen
peroxide-induced intracellular oxidation and DNA single-strand
breakage in Hep G2 cells. J Hepatol. 26:669–677. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Kappus H and Diplock AT: Tolerance and
safety of vitamin E: A toxicological position report. Free Radic
Biol Med. 13:55–74. 1992. View Article : Google Scholar : PubMed/NCBI
|