Introduction
Topical ocular anesthetics are typically safe when
used appropriately. However, their widespread use has revealed a
potential to cause severe toxicity, abuse and addiction.
Keratopathy is a common manifestation of topical ophthalmic drug
abuse, and results in intense pain, loss of vision, refractory
central corneal epithelial defects, ring keratitis, degenerative
keratopathy with epithelial cell shedding, stromal infiltration,
and may lead to corneal melting and perforation, with poor
prognosis (1,2). Abuse of topical ocular anesthetics is
rare and serious toxicities are not frequently reported. In
numerous cases, the symptoms of toxic keratopathy are mistaken for
another disease. Mooren's ulcer is an idiopathic, chronic,
non-infectious, painful ulcerative keratitis with a characteristic
undermined opaque central edge. The ulcerative lesion with
overhanging edges typically initially presents on the periphery of
the cornea and often spreads progressively to the entire
circumference or towards the centre of the cornea (3,4). The
disease may also be recurrent in nature and involve one or both
eyes. The common manifestations of topical ophthalmic drug abuse
keratopathy include intense pain, loss of vision, refractory
central corneal epithelial defects, ring keratitis, degenerative
keratopathy with epithelial cell shedding, stromal infiltration,
and may lead to corneal melting and perforation, with poor
prognosis (1,2). Here we report a typical case of toxic
keratopathy presented as binocular corneal annular melt and
perforation, subsequent to the abuse of lidocaine, tetracaine and
dexamethasone (DEX) eye drops, the manifestations of which are
similar to those of Mooren's ulcer.
Case report
The patient was a 38-year-old male physician with
severe pain and decline of vision in the left and right eyes for
six months. He had treated himself with sodium hyaluronate eye
drops (Santen Pharmaceutical Co., Ltd., Shenzhen, China), lidocaine
eye drops (Tianjin Jin Yao Amino Acid Co., Ltd., Tianjin, China)
and DEX eye drops (Shandong Xinhua Pharmaceutical Co., Ltd., Henan,
China) hourly for the previous six months. However, the
deterioration of his eyes continued and the patient began to
self-administer tetracaine eye drops (Zhejiang Jiuxu Pharmaceutical
Co., Ltd., Hangzhou, China) once per hour during the two weeks
prior to being admitted to the Department of Ophthalmology at First
Hospital of Jilin University (Changchun, China). Written informed
consent was obtained from the patient for publication of this case
report and accompanying images. The present study was approved by
the Human Ethics Committee of Jilin University, (Changchun, China)
and written informed consent was obtained from the patient.
The patient had a history of intermittent use of
lidocaine and DEX eye drops in both eyes ten years previously. His
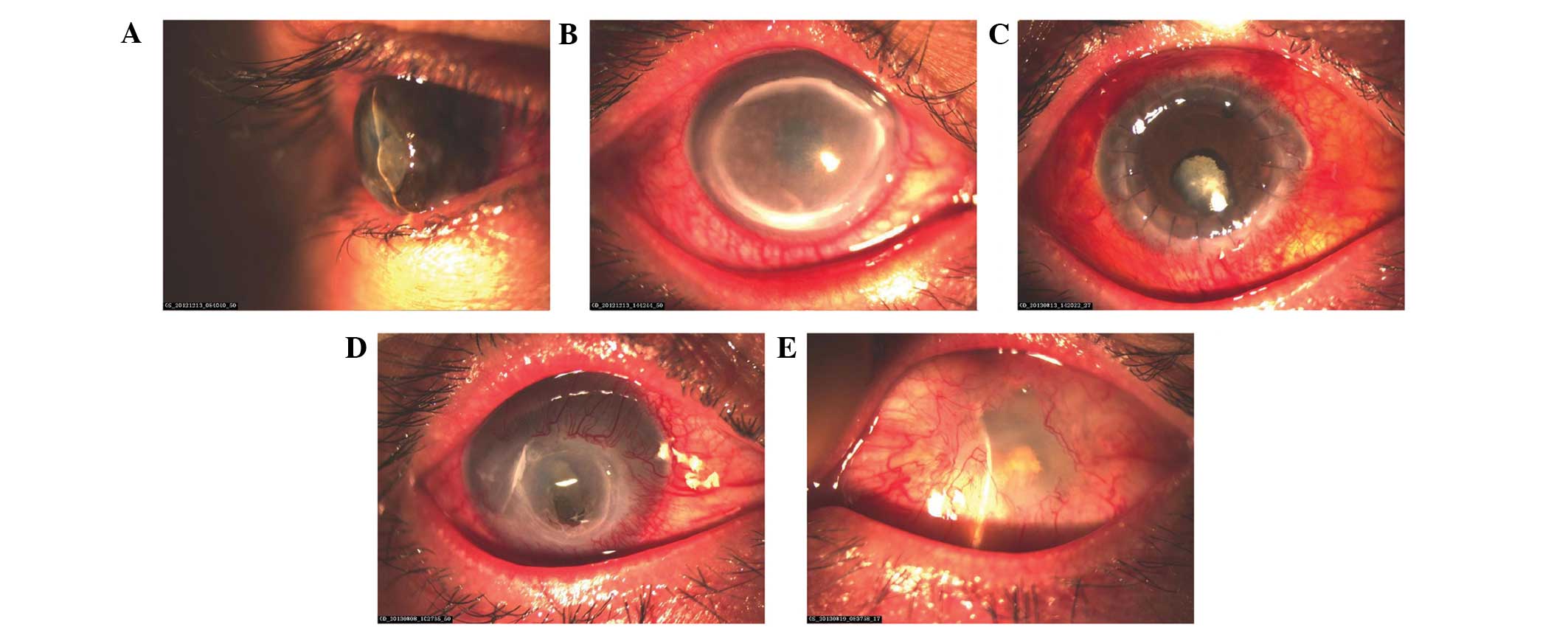
best-corrected visual acuities (BCVAs) (5) at admission were 20/32 in the right eye
and hand motion in the left eye. His right cornea exhibited annular
melting with Mooren-like full-thickness stromal infiltration at the
limbus; central corneal haze was also observed (Fig. 1A). His left cornea was completely
melted and iris prolapse was observed (Fig. 1B).
Use of the anesthetics and DEX eye drops was stopped
and an emergency keratoplasty was performed in his left eye
immediately following admission. The homogeneous allogeneic corneal
tissue was provided by the eye bank of the First Affiliated
Hospital of Jilin University. Following the surgery, the left eye
was treated with 4 drops per eye per day (one drop administered on
four separate occasions) 0.05% cyclosporine eye drops (North China
Pharmaceutical Co., Ltd., Shijiazhuang, China), 0.5% levofloxacin
eye drops and 0.1% sodium hyaluronate eye drops (Santen
Pharmaceutical Co., Ltd.) six times daily per eye, with one drop
administered on each occasion, and 100% autologous serum eye drops
three times daily per eye, administered as one drop on three
separate occasions. Eleven days postsurgery, the patient's BCVA of
the left eye was light perception. No corneal allograft rejection
was observed.
After release from the hospital, the patient did not
comply with follow-up. Eight months later, he presented again with
redness and loss of vision in the right eye of ~10 days duration.
The patient had self-administered tobramycin and DEX ointment
(Alcon; Novartis International AG, Basel, Switzerland) three times
per day since his release from the hospital, and used lidocaine eye
drops again to control pain. The patient was re-admitted to the
hospital and his BCVA was hand motion in the right eye. His right
cornea was gray and thin. A perforation ~3×2 mm in size and iris
prolapse at the inferior of the central cornea was observed; the
anterior chamber had disappeared (Fig.
1C).
A penetrating keratoplasty was immediately performed
in his right eye; the homogeneous allogeneic corneal tissue was
provided by our eye bank. After the surgery, the right eye was
treated with tacrolimus eye drops (Zhongshan Ophthalmic Center,
Zhongshan, China) and fluorometholone eye drops four times daily,
sodium hyaluronate eye drops (Santen Pharmaceutical Co., Ltd.) six
times daily, and atropine sulfate eye gel (Shenyang Xing Qi
Pharmaceutical Co., Ltd., Shenyang, China) three times daily.
Prior to hospital discharge, the patient's BCVAs
included counting fingers with use of the right eye and light
perception in the left eye. There was no allograft rejection
(Fig. 1D), and the bulbar
conjunctiva of the left eye proliferated and covered the majority
of the cornea (Fig. 1E).
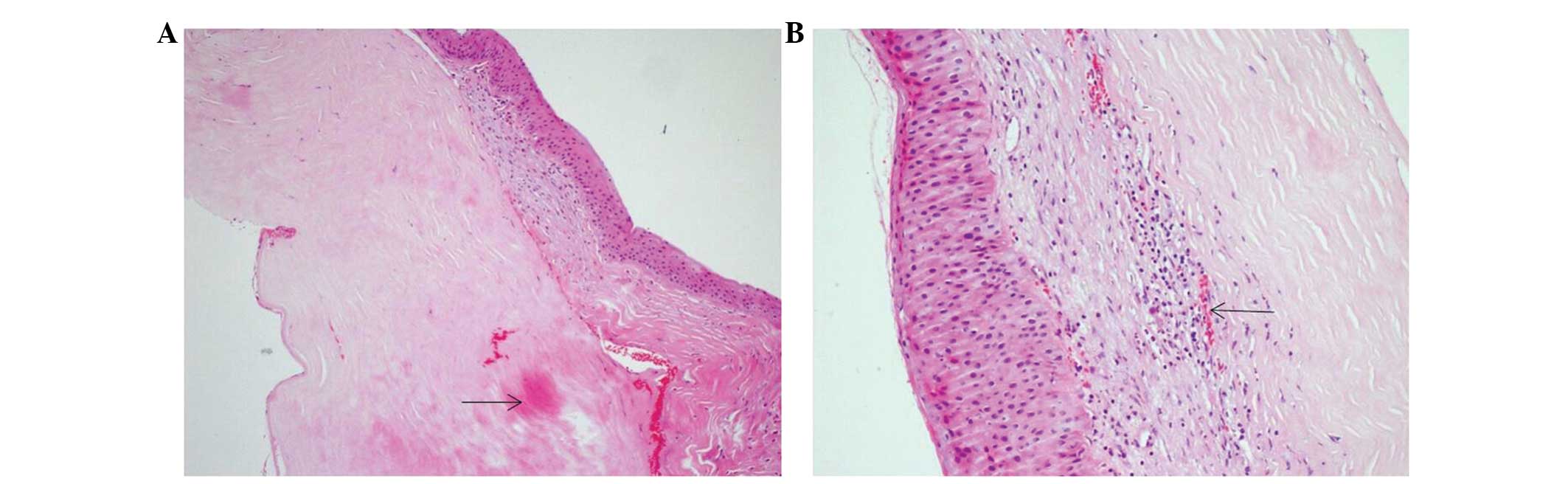
Hematoxylin and eosin staining was performed as
follows: Dewaxing formalin-fixed samples with xylene for 10 min,
followed by further dewaxing with xylene for 5 min. Next, samples
underwent two washes with absolute alcohol for 1 min each, followed
by 3 successive washes with 95, 90 and then 85% alcohol, each for 1
min. Subsequently, samples were washed with distilled tap water for
2 min, stained with hematoxylin for 1–5 min, washed with distilled
tap water for 1 min, then with 1% diluted ammonia water for 30 sec,
and again with distilled water for 1 min. Next, staining with eosin
for 20 sec to 5 min, washing with distilled water for 30 sec, then
successive rinses with 85, 90 and 95% alcohol for 20 sec, 30 sec
and 1 min, respectively. Further washes with 95% alcohol for 1 min,
and absolute alcohol twice each for 2 min. Finally, samples were
treated with xylene three times, each for 2 min. Next, samples were
fixed in rhamsan gum (neutral resin) sealing piece and cut into 2×2
cm sections 4 µm thick. Sections were then vieswed under an Olympus
BX50 microscope with magnification, ×50. Histology of the resection
of the right cornea revealed corneal epithelial hyperplasia,
neovascularization, hyaline degeneration of the corneal stroma,
with infiltration of neutrophils, lymphocytes and plasma cells
(Fig. 2A and B).
Discussion
In general, Mooren's ulcer is an idiopathic,
crescent-shaped peripheral corneal ulcer with grey white
infiltrate. The characteristic lesion begins in the periphery of
the cornea and spreads circumferentially (6). The leading edges of the ulcer are
undermined, infiltrated and de-epithelialized. In the present case,
we assume that the application of topical anesthetics altered the
antigens of a normal cornea and led to an autoimmune response.
Anesthetic-induced keratopathy is progressive and is accompanied by
a injury of the corneal epithelium (7–9). Early
corneal damage can be identified on the first day of topical
application of an anesthetic, and is characterized as a smoothly
structured periphery and a pitted corneal surface. If not treated
or improperly treated for a number of days or weeks, infiltration
in the corneal stroma may appear along the rims of the area of
defected epithelium, forming a progressive ring lesion that can
lead to corneal ulceration, thinning and eventually perforation and
endophthalmitis (10,11). Prompt diagnosis is crucial, as
patients typically continue to use topical anesthetics for pain
management if no warning is given.
The mechanism underlying toxic keratopathy may
include damage of the corneal epithelial barrier and disruption of
re-epithelialization (6). A healthy
epithelial surface protects the cornea from potential infection and
the invasion of various microbial pathogens. Topical anesthetics
may paralyze corneal perception, reduce blink reflex and suppress
reflex weeping. This increases the duration of exposure of the
cornea to the air and promotes apoptosis (10), and therefore the ability of corneal
epithelial cells to resist infection and foreign bodies is
significantly reduced. In addition to initially compromising the
integrity of the corneal epithelial barrier, topical anesthetics
exert inhibitory effects on respiration, glucose metabolism and
mitosis of corneal epithelial cells, disrupting the process of
re-epithelialization (6,12,13).
With continued use of topical anesthetics, eventually the corneal
tissue may undergo necrosis, dissolution and perforation. Topical
anesthetics may also alter corneal antigens and lead to an
autoimmune response (14). The
increased immune activity and inflammatory cells further damage the
cornea, leading to a cycle of altered corneal antigens and
self-destruction (15–17).
DEX is an anti-inflammatory medication with low
corneal epithelial permeability. Excessive instillation of DEX eye
drops may lead to various complications (18), including glaucoma, optic nerve
damage, visual disturbance, sub-capsular cataract and corneal
thinning (19–21), and significantly delays corneal
re-epithelialization (22).
The prompt diagnosis and treatment of toxic
keratopathy is crucial to the clinical outcome. However, diagnosis
of keratopathy due to drug abuse is often delayed as the clinical
manifestations are common to other diseases such as acanthamoeba
keratitis, bacterial keratitis, viral keratitis and single cell
virus keratitis (23,24). Furthermore, the diagnosis may be
complicated if the patient cannot accurately identify the eye drops
they have used (25). A thorough
history and consideration of the specific eye drops used are
crucial for the accurate diagnosis of drug-induced keratopathy
(26).
Glossary
Abbreviations
Abbreviations:
|
BCVA
|
best corrected visual acuity
|
|
DEX
|
dexamethasone
|
References
|
1.
|
Ansari H, Garibaldi DC and Jun AS:
Anaesthetic abuse keratopathy as a manifestation of ocular
Munchausen's syndrome. Clin Experiment Ophthalmol. 34:81–83. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Yagci A, Bozkurt B, Egrilmez S, Palamar M,
Ozturk BT and Pekel H: Topical anesthetic abuse keratopathy: A
commonly overlooked health care problem. Cornea. 30:571–575.
2011.PubMed/NCBI
|
|
3.
|
Shinomiya K, Ueta M, Sotozono C, Inatomi
T, Yokoi N, Koizumi N and Kinoshita S: Immunohistochemical analysis
of inflammatory limbal conjunctiva adjacent to Mooren's ulcer. Br J
Ophthalmol. 97:362–366. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Ngan ND and Chau HT: Amniotic membrane
transplantation for Mooren's ulcer. Clin Experiment Ophthalmol.
39:386–392. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Murthy GVS and Johnson G: Chapter 1. The
Epidemiology of Eye Disease. Johnson GJ, Minassian DC, Weale RA and
West SK: 58:(3rd). Singapore: World Scientific Publishing Company.
82012.
|
|
6.
|
Chang YS, Tseng SY, Tseng SH and Wu CL:
Cytotoxicity of lidocaine or bupivacaine on corneal endothelial
cells in a rabbit model. Cornea. 25:590–596. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Tok OY, Tok L, Atay IM, Argun TC, Demirci
N and Gunes A: Toxic keratopathy associated with abuse of topical
anesthetics and amniotic membrane transplantation for treatment.
Int J Ophthalmol. 8:938–944. 2015.PubMed/NCBI
|
|
8.
|
Dass BA, Soong HK and Lee B: Effects of
proparacaine on actin cytoskeleton of corneal epithelium. J Ocul
Pharmacol. 4:187–194. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Burns RP: Toxic effects of local
anesthetics. JAMA. 240:3471978. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
McGee HT and Fraunfelder FW: Toxicities of
topical ophthalmic anesthetics. Expert Opin Drug Saf. 6:637–640.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Patel M and Fraunfelder FW: Toxicity of
topical ophthalmic anesthetics. Expert Opin Drug Metab Toxicol.
9:983–988. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Atilla H, Tekeli O, Can B, Karel F and
Saran Y: Effects of intracameral lidocaine on ocular tissues. Clin
Experiment Ophthalmol. 31:73–77. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Catterall WA: Molecular mechanisms of
gating and drug block of sodium channels. Novartis Found Symp.
241:206–218; discussion 218–232. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Khakshoor H, Moshirfar M, Simpson RG,
Gharaee H, Vejdani AH, Christiansen SM, Edmonds JN and Behunin NL:
Anesthetic keratopathy presenting as bilateral Mooren-like ulcers.
Clin Ophthalmol. 6:1719–1722. 2012.PubMed/NCBI
|
|
15.
|
Chen HT, Chen KH and Hsu WM: Toxic
keratopathy associated with abuse of low dose anesthetic: A case
report. Cornea. 23:527–529. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Kintner JC, Grossniklaus HE, Lass JH and
Jacobs G: Infectious crystalline keratopathy associated with
topical anesthetic abuse. Cornea. 9:77–80. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Meyers-Elliott RH, Pettit TH and Maxwell
WA: Viral antigens in the immune ring of Herpes simplex stromal
keratitis. Arch Ophthalmol. 98:897–904. 1980. View Article : Google Scholar : PubMed/NCBI
|
|
18.
|
Swaminathan S, Vavia PR, Trotta F and
Cavalli R: Nanosponges encapsulating dexamethasone for ocular
delivery: Formulation design, physicochemical characterization,
safety and corneal permeability assessment. J Biomed Nanotechnol.
9:998–1007. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
19.
|
Ferrante P, Ramsey A, Bunce C and Lightman
S: Clinical trial to compare efficacy and side-effects of injection
of posterior sub-Tenon triamcinolone versus orbital floor
methylprednisolone in the management of posterior uveitis. Clin
Experiment Ophthalmol. 32:563–568. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
20.
|
Zhang JZ, Krenzer KL, López FJ and Ward
KW: Comparative effects of besifloxacin and other fluoroquinolones
on corneal reepithelialization in the rabbit. J Cataract Refract
Surg. 36:1049–1050. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
21.
|
Li CC and Chauhan A: Modeling ophthalmic
drug delivery by soaked contact lenses. Ind Eng Chem Res.
45:3718–3734. 2006. View Article : Google Scholar
|
|
22.
|
Piper SL, Laron D, Manzano G, Pattnaik T,
Liu X, Kim HT and Feeley BT: A comparison of lidocaine, ropivacaine
and dexamethasone toxicity on bovine tenocytes in culture. J Bone
Joint Surg Br. 94:856–862. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
23.
|
Ardjomand N, Faschinger C, Haller-Schober
EM, Scarpatetti M and Faulborn J: A clinico-pathological case
report of necrotizing ulcerating keratopathy due to topical
anaesthetic abuse. Ophthalmologe. 99:872–875. 2002.(In German).
View Article : Google Scholar : PubMed/NCBI
|
|
24.
|
Rosenwasser GO, Holland S, Pflugfelder SC,
Lugo M, Heidemann DG, Culbertson WW and Kattan H: Topical
anesthetic abuse. Ophthalmology. 97:967–972. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
25.
|
Katsimpris JM, Sarantoulakou M, Kordelou
A, Petkou D and Petropoulos IK: Clinical findings in patients with
topical anaesthetic abuse keratitis: A report of five cases. Klin
Monbl Augenheilkd. 224:303–308. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
26.
|
Lee JK and Stark WJ: Anesthetic
keratopathy after photorefractive keratectomy. J Cataract Refract
Surg. 34:1803–1805. 2008. View Article : Google Scholar : PubMed/NCBI
|