Introduction
Chronic obstructive pulmonary disease (COPD) is a
chronic inflammatory disease resulting from intensified
inflammatory responses to noxious particles or gases in the airways
or lung. Complications associated with COPD usually occur due to
intrapulmonary inflammatory exudations. As a result, the newly
modified Global Initiative for Chronic Obstructive Lung Disease
(2011 Version) recommendations have emphasized the importance of
complications in the comprehensive evaluation of COPD (1).
Since the respiratory and intestinal tracts have
similar mucosal structures and physiological characteristics, COPD
is to some extent associated with inflammatory diseases of the
intestinal mucosa, such as inflammatory bowel disease (IBD)
(2). Studies have indicated that, in
addition to commonly shared risk factors (such as smoking), COPD
increases the prevalence of IBD among COPD patients via mechanisms
such as inflammatory responses and dysregulation of
protease/anti-protease activity (3).
Furthermore, patients with IBD complicated by COPD have a
significantly higher mortality rate (2.5–3.5 times), as compared
with IBD alone (4). Rutten et
al (5) found in their recent
study that patients with COPD exhibit increased intestinal
permeability, intestinal epithelial damage and destruction of the
integrity of the intestinal mucosal barrier. These observations
suggest that structural and functional changes in the gut may be
caused by systemic damage associated with the complications of
COPD. However, the mechanisms underlying the development of
COPD-induced intestinal damage in patients with COPD remains
unclear. In order to address this issue, the present observational
study of the structural and functional changes of the intestinal
mucosal barrier was conducted using a rat model of COPD, with the
aim of providing evidence useful in the diagnosis and treatment of
COPD and its complications.
Materials and methods
Materials and animals
A total of 40 healthy male specific pathogen-free
Sprague-Dawley rats (Division of Comparative Medicine, Nanjing
Jinling Hospital, Nanjing, China) with a mean weight of 150±12 g
were evenly randomized into the control and COPD groups (n=20 per
group). The 8-week rats were clean grade and were bred in the
Medical Experiment Animal Center of Jinling Hospital. All rats were
maintained in a specific-pathogen free environment, ventilated with
clean air at 20–25°C and 40–70% relative humidity throughout the
study with a 12-h light/dark cycle. Following one week of
conditioning, rats were randomly divided into control group (clean
air-exposed only) and COPD groups. At all times, excluding the
smoke exposure period, water and food were provided ad
libitum. Chambers and cages were washed on a daily basis. Rats
were visually observed twice daily. Cigarettes delivering 11 mg
tar, 0.9 mg nicotine and 14 mg carbon monoxide (Nanjing Cigarette
Factory, Nanjing, China) were used. The other reagents and devices
included: Occludin (sc-5562) and zona occludens-1 (ZO-1; sc-10804)
specific antibodies (Santa Cruz Biotechnology, Inc., Dallas, TX,
USA); β-actin antibody (TDY051; TDY Biotech Co., Ltd., Beijing,
China); horseradish peroxidase (HRP)-conjugated goat anti-rabbit
secondary antibody (074-1506; KPL, Inc., Gaithersburg, ML, USA); UV
spectrophotometer 52-P; Shanghai Xianke Instrument Co., Ltd.,
Shanghai, China), diamine oxidase (DAO) standard (Sigma-Aldrich,
St. Louis, MO, USA), lactulose standard (National Institute for
Food and Drug Control, Beijing, China), D-mannitol standard
(Shanghai Yuanye Biotechnology Co., Ltd., Shanghai, China), high
performance liquid chromatography (HPLC) system (Waters
Corporation, Milford, MA, USA), rat tumor necrosis factor-α (TNF-α)
enzyme-linked immunosorbent assay (ELISA) kit (Sigma-Aldrich), rat
interleukin-8 (IL-8) ELISA kit (Sigma-Aldrich) and rat interferon-γ
(IFN-γ) ELISA kit (Sigma-Aldrich). The study protocol was approved
by the ethics committee of Nanjing Jinling Hospital.
Establishment of the rat model of
COPD
The rat model of COPD was established using the
sidestream cigarette smoke method described by Zheng et al
(6) and Li et al (7). The rats were kept in a cigarette smoke
(CS) chamber (70×40×30 cm) with two 5×5 cm vents. CS was produced
by five simultaneously lit cigarettes twice a day and the vents
were opened every 15 min. The rats were exposed to the sidestream
cigarette smoke for 2 h per day and 5 days per week continuously
for 6 months. With the exception of restraint in a similar CS
chamber, no other treatments were administered to the rats in the
control group. Rats from the two groups were able to move without
restraint and were allowed free access to drinking water and
food.
Staining of the lung and intestinal
tissues
Rats were anesthetized with 2% pentobarbital sodium
at a dose of 30 mg/kg and then sacrificed by exsanguination from
the heart. Serum samples were harvested from the rats following
sacrifice and were stored at −80°C until they were required to
measure DAO. Subsequently, the right-upper lung and jejunum (5 cm
below the Treitz ligament) were harvested and fixed by immersion in
10% neutral formalin for a 24 h. Finally, after consecutive
procedures of paraffin-embedding, generation of serial sections
(thickness, 4 µm), dewaxing, hematoxylin and eosin (H&E)
staining, dehydration, deparaffinization with xylene and mounting,
the sections were observed with the use of light microscopy.
Western blot analysis of tight
junction proteins in the intestinal tissues
Proteins were extracted from the intestinal tissues
of the rats from the two groups by protein lysis. Proteins lysates
were then stored in Eppendorf tubes at −130°C. Total protein
concentrations were determined by UV spectrophotometry. Equal
amounts of total proteins (20µg) were then separated using 10%
sodium dodecyl sulfate-polyacrylamide gel electrophoresis and
transferred to polyvinylidene difluoride (PVDF) membranes. The PVDF
membranes were then blocked using 5% skimmed milk with shaking at
room temperature for 1 h. The primary occludin, ZO-1 and β-actin
antibodies (1:1,000) were dissolved in Tris-buffered saline and
Tween 20 (TBST) with 5% skimmed milk and incubated with the
membrane at 4°C overnight. They were then washed three times with
TBST using a shaker at room temperature, for 5 min each time. The
HRP-conjugated goat anti-rabbit secondary antibody was diluted with
TBST (1:3,000), incubated with the membrane for 30 min at room
temperature, and then the membrane was washed three times using
TBST with shaking at room temperature, for 5 min each time.
Exposure of the images was conducted using enhanced
chemiluminescence and the scanned images were archived. Analysis of
the optical density of each band was conducted using AlphaEaseFC
4.0 system analysis software (Protein Simple, San Jose, CA, USA).
Protein levels were expressed as the integrated density ratio of
the corresponding protein to the internal control (β-actin).
Measurement of the urinary lactulose
to mannitol ratio (L/M)
Oral infusions of lactulose (100 mg) and mannitol
(50 mg) were administered to 10 rats from each group. These rats
were then kept in separate cages without food and samples of their
urine were collected 6 h later. A method has been developed for the
simultaneous determination of lactulose and mannitol in urine by
HPLC (8), and was used in the
current study. Following ultrafiltration and deionization, urine
samples were analyzed with a LiChrospher® NH2 column
(4.6×250 mm, internal diameter, 5 µm), a mixture of acetonitrile
and water (722:8, volume ratio) as the mobile phase and a
refractive index detector. Column temperature was 30°C. During the
mobile phase, a flow rate of 1 ml/min was used (differential
detector: internal heating, 37°C; sensitivity, 32, time constant,
1.0; scale factor, 20; and injection volume, 10 µl). The excretion
of urinary lactulose and mannitol was determined and the L/M value
was calculated.
Determination of serum DAO
activity
A 3.3-ml volume of reaction buffer consisting 3 ml
phosphate-buffered saline (0.2 M, pH 7.2), 0.1 ml (4 µg)
horseradish peroxidase, 0.1 ml o-dianisidine dihydrochloride
(500 pg) methanol solution, and 0.1 ml substrate solution
(containing 175 pg cadaverine dihydrochloride) was added to each
well of a 6-well plate. A 0.5-ml volume of serum sample was then
added to each well for analysis. The blank control and a
concentration gradient of standard substance were also added. DAO
values were calculated automatically with a microplate reader
detecting the optical density at 436 nm.
Measurement of cytokines secreted by
the intestinal tissues
One small segment (length, 2cm) of the intestine
sample from each rat was harvested for the measurement of cytokine
production. After being cut along the mesentery, the intestinal
tissue samples were soaked and washed in cold normal saline (NS) to
remove the blood. The tissues were then weighed after drying on
filter papers. Subsequently, each tissue sample was placed into a
5-ml beaker containing a volume of 0.86% cold NS equal to six times
the weight of the sample. Following homogenization of the tissue
and washing using a volume of 0.86% cold NS equal to three times
the original weight of the intestinal sample, samples of the tissue
homogenates (10% suspension) were prepared and stored at −20°C. The
levels of TNF-α, IL-8 and IFN-γ in the homogenates were determined
using ELISA kits according to the manufacturer's protocol.
Statistical analysis
Data were analyzed using SPSS version 13.0 software
(SPSS, Inc., Chicago, IL, USA). Enumeration data were expressed as
means ± standard deviation and analyzed by independent sample
t-tests. P<0.05 was considered to indicate a statistically
significant difference.
Results
Establishment of the rat model of
COPD
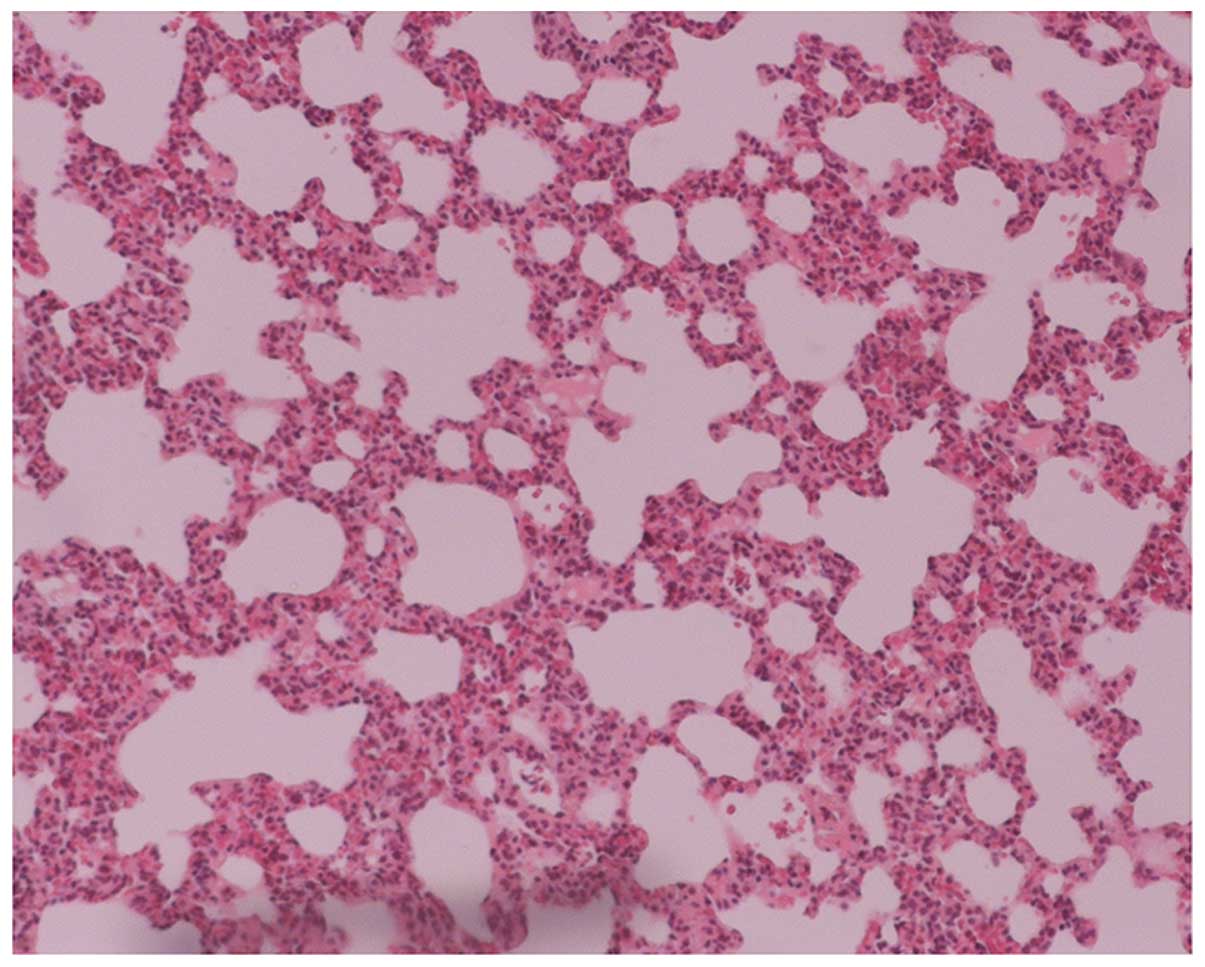
The lung histopathology indicated normal pulmonary
structures, an absence of inflammatory infiltration in the small
airways and structural integrity of the alveolar wall (Fig. 1) in the control group. However, in
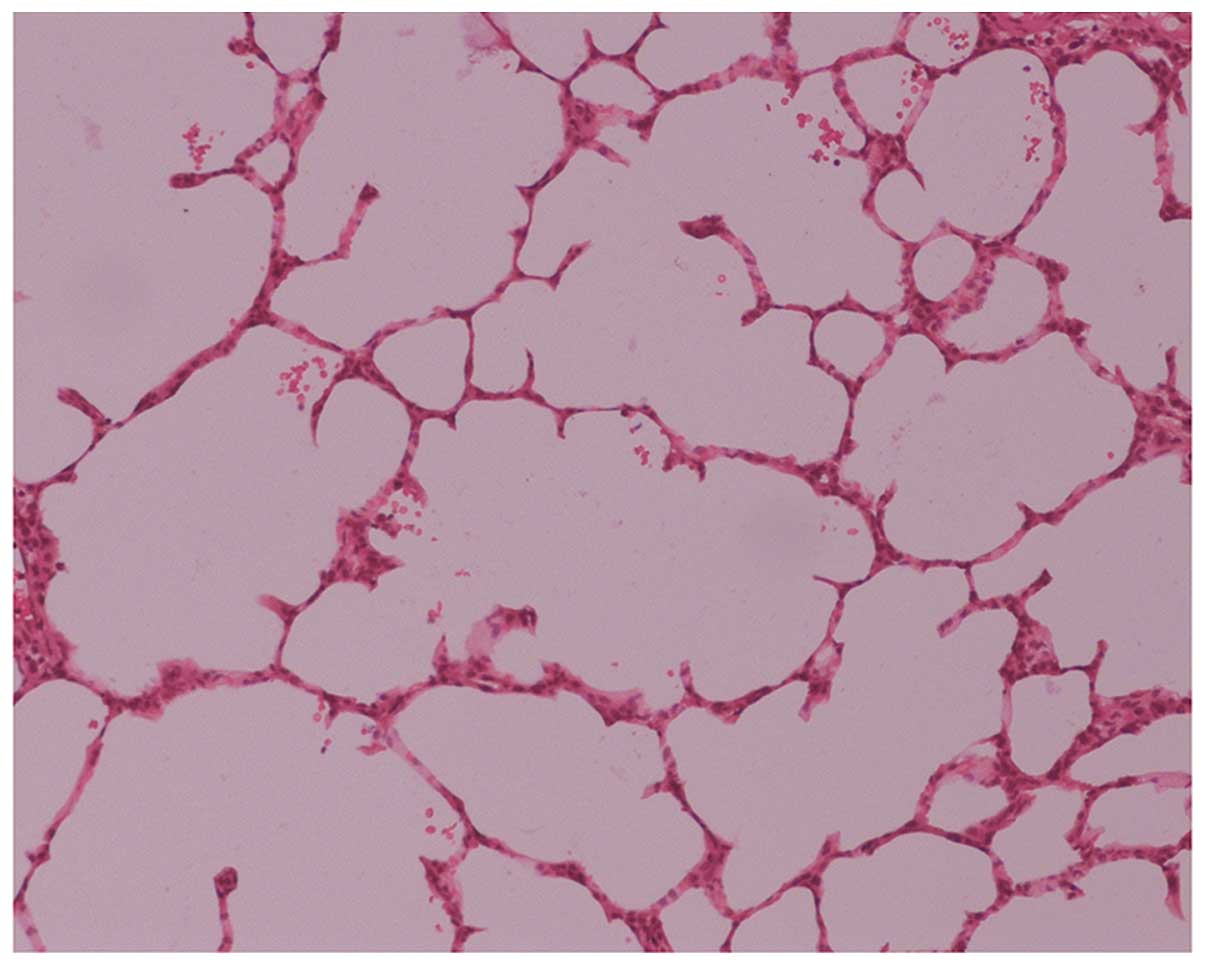
the COPD group, a large amount of monocyte and lymphocyte
infiltration at and around the small airway walls was observed,
with thinning of the alveolar wall, ruptured alveolar septa,
interstitial pulmonary congestion and edema, reduced blood vessel
density, enlarged and deformed alveoli, and formation of bullae due
to alveolar fusion (Fig. 2). These
results indicated the presence of emphysema and other pathological
changes in the rats from the COPD group and confirmed the
successful establishment of the rat model of COPD.
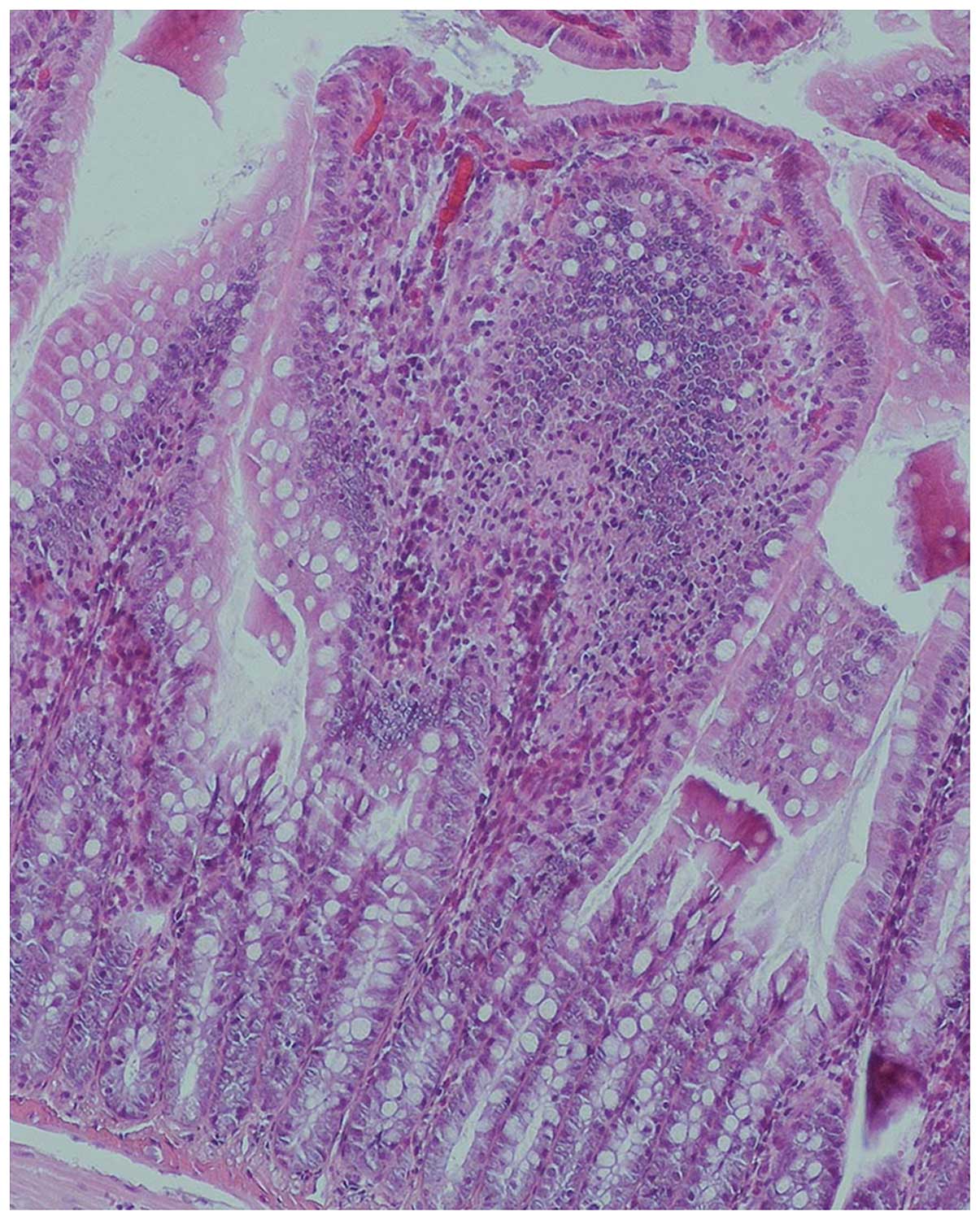
Evaluation of the intestinal
samples
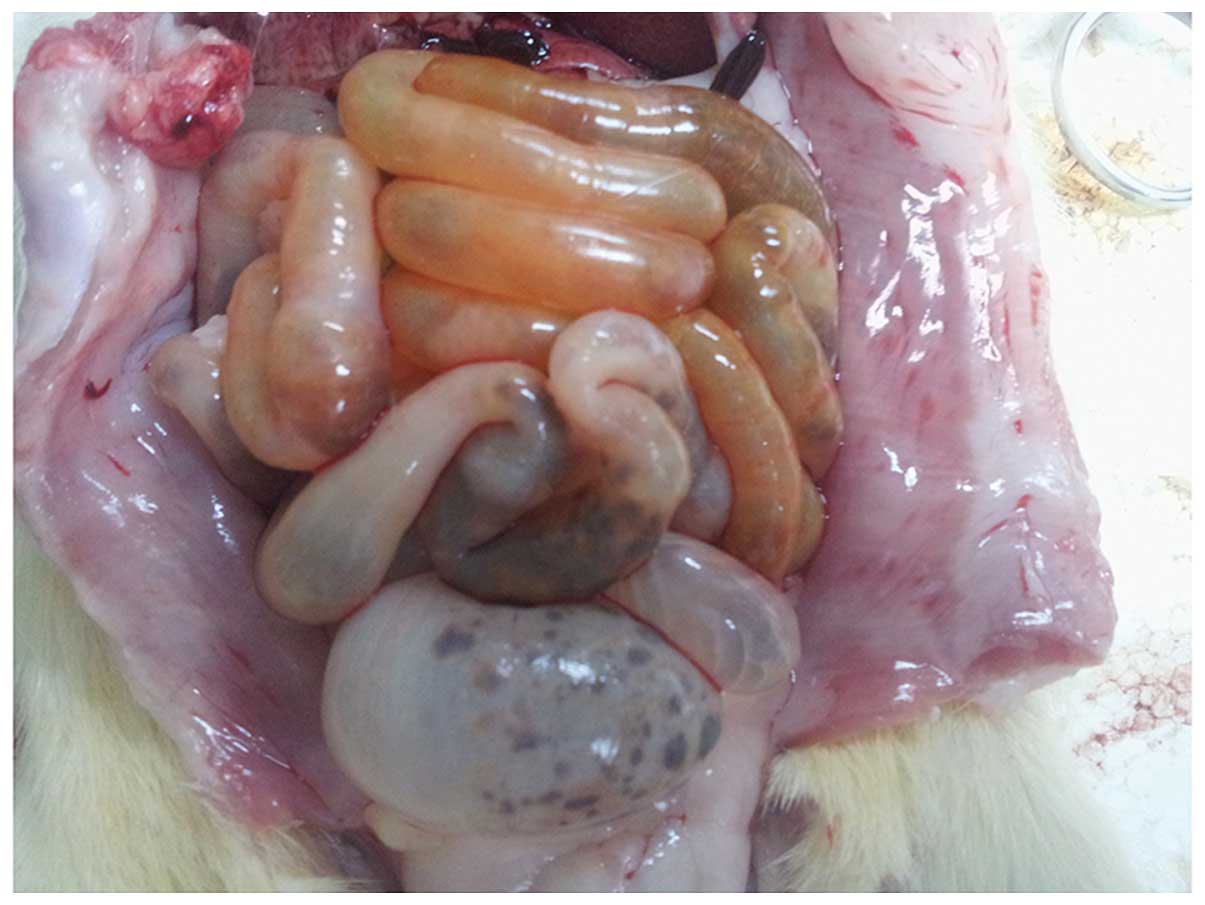
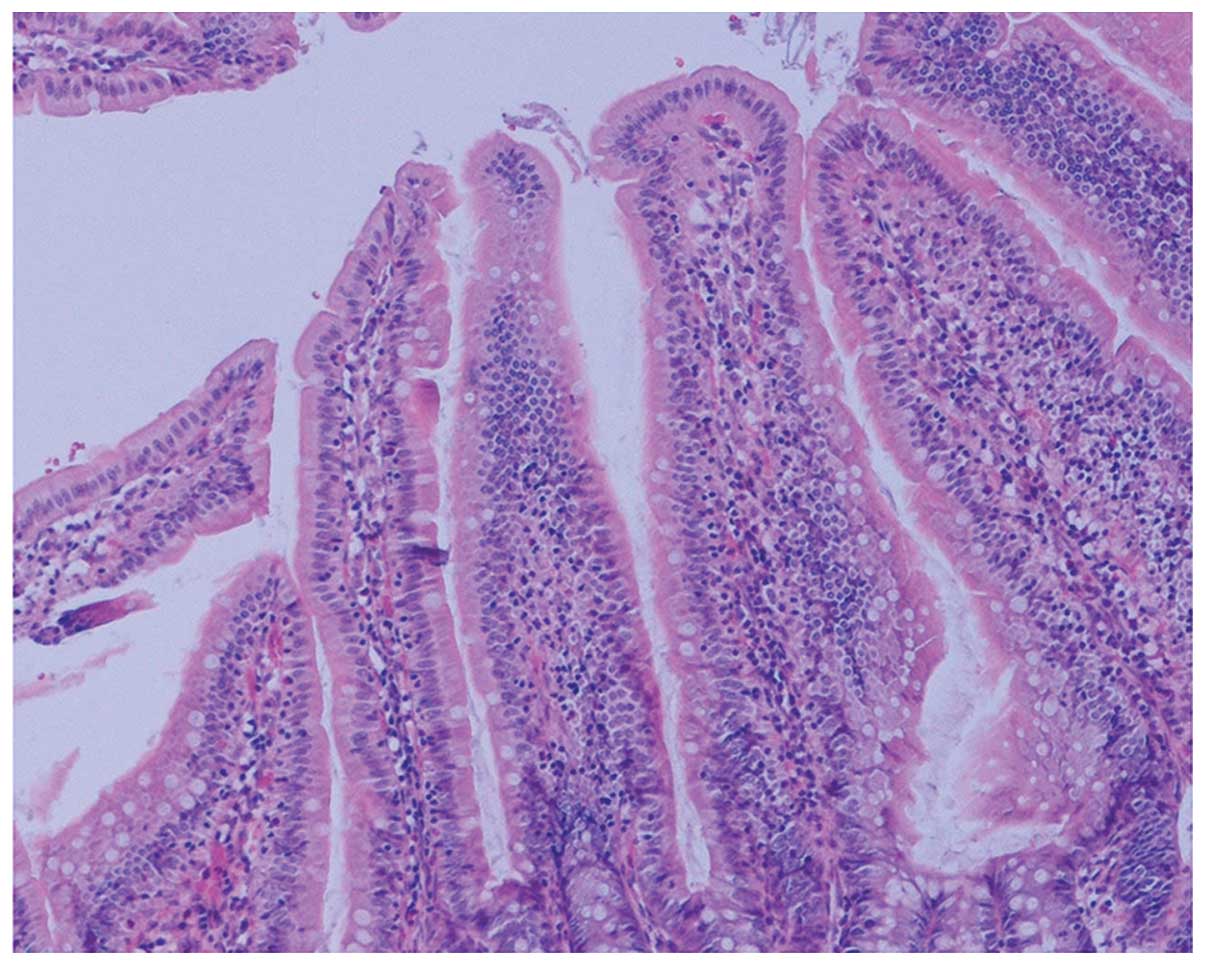
Gross observation indicated significant swelling of
the gut in the rats of the COPD group compared with that in the
normal rats, with darkened and gray mucosa in the former (Figs. 3 and 4). Under light microscopy, neutrophil
infiltration of the intestinal mucosa, structural damage to the
epithelium and pathological changes characterized by regional
epithelial shedding and reduction in the number of intestinal villi
were observed in the rats of the COPD group. By contrast, no
evident pathological changes were observed in the intestinal mucosa
of rats from the control group (Figs.
5 and 6).
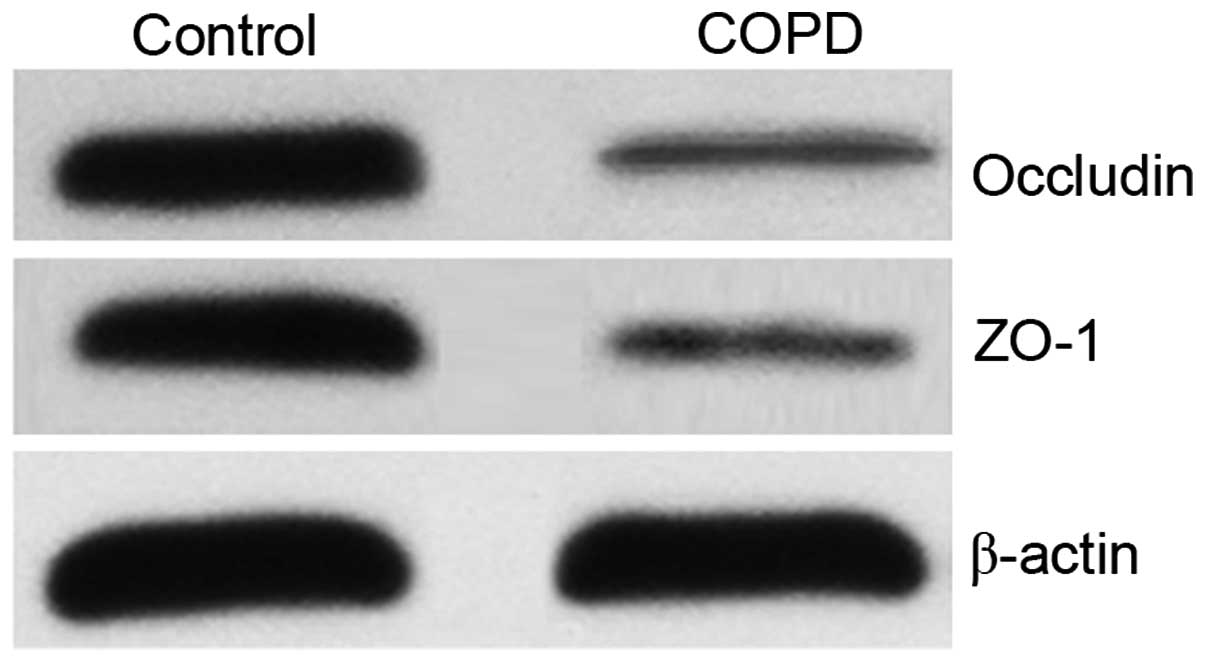
Expression of occludin and ZO-1
proteins in the intestinal tissues
As tight junction proteins (including occludin and
ZO-1) contributed to barrier function, the expression levels of
occludin and ZO-1 proteins were significantly reduced in the COPD
group, as compared with the control group (P<0.05; Fig. 7 and Table
I). This result indicated that the damage to the intestinal
barrier structure may contribute to intestinal barrier dysfunction
in COPD.
 | Table I.Relative intestinal expression of
occludin and ZO-1 protein in the two groups (%). |
Table I.
Relative intestinal expression of
occludin and ZO-1 protein in the two groups (%).
| Group | Occludin | ZO-1 |
|---|
| Control |
102.00±5.17 |
98.40±4.98 |
| COPD |
35.00±2.23a |
29.80±2.28a |
Evaluation of the intestinal mucosal
barrier function
Various molecular probes can be used to determine
the permeability of the intestinal mucosa; however, the results are
affected by numerous factors including gastrointestinal emptying
retardation, renal dysfunction and urine collection insufficiency
when a molecular probe is used alone. The accuracy of the results
can be greatly improved when two different molecular probes are
used simultaneously. In the present study, the urinary L/M value
and serum DAO levels were significantly higher in the COPD group
compared with those in the control group (both P<0.05; Table II). This result indicated that the
permeability of the intestinal mucosal barrier is increased and
intestinal mucosal barrier function is impaired in COPD.
 | Table II.Urinary L/M values and serum DAO
levels in the two groups. |
Table II.
Urinary L/M values and serum DAO
levels in the two groups.
| Group | L/M value | Serum DAO level
(ng/ml) |
|---|
| Control |
0.15±0.02 |
10.69±0.35 |
| COPD |
1.58±0.21a |
12.26±0.23a |
Measurement of cytokine levels in the
intestinal tissues
Intestinal inflammatory factors were examined to
identify the possible mechanism of intestinal barrier dysfunction
in COPD. The intestinal secretion levels of TNF-α, IL-8 and IFN-γ
were significantly higher in the COPD group compared with the
control group (P<0.05; Table
III). As cytokines are able to regulate intestinal tight
junctions under pathological states, this result indicated that
intestinal barrier dysfunction may occur in COPD, and may at least
partly function via the enhanced inflammatory response.
 | Table III.Intestinal expression levels of TNF-α,
IL-8 and IFN-γ in the two groups. |
Table III.
Intestinal expression levels of TNF-α,
IL-8 and IFN-γ in the two groups.
| Group | TNF-α (pg/ml) | IL-8 (pg/ml) | IFN-γ (ng/ml) |
|---|
| Control |
316.15±0.82 |
684.15±3.14 |
1.76±0.03 |
| COPD |
357.73±1.56a |
731.56±7.10a |
2.21±0.14a |
Discussion
COPD is a chronic inflammatory condition that is
caused by exposure of the airways and lung tissues to toxic gases
or particles. Inflammatory cell infiltration in the lungs of
patients with COPD comprises mainly alveolar macrophages,
neutrophils and CD8+ T cells that release multiple
inflammatory mediators including leukotriene B4, IL-8, and TNF-α.
This persistent inflammation is not restricted to the lung, but may
also lead to inflammation in extrapulmonary systems, resulting in
the occurrence of complications (9).
In the present study, significant inflammation of the intestinal
tissues was demonstrated in rats in association with COPD, together
with pathological changes of the intestines, such as neutrophil
infiltration and regional mucosal epithelial shedding. This
indicated the presence of increased inflammatory cell infiltration
of the mucosa and structural damage to the intestines of the rats
with COPD.
The intestinal mucosal barrier consists mainly of
epithelial junctional complexes between intestinal epithelial
cells. These junctions include adherens junctions and tight
junctions, which are critically responsible for the selective
regulation of the movement of water, ions and other small molecules
via the paracellular transportation pathway. Therefore, tight
junctions are an important part of the intestinal mucosal barrier
and the integrity of this barrier is one of the prerequisites of
its function. Tight junctions are formed by transmembrane proteins
(such as claudins, occludin and adhesion molecules) and
intracellular scaffold proteins (such as ZO and cingulin) (10). Several studies, including the one
conducted by Odenwald and Turner indicate that destruction of the
tight junction leads to structural changes and dysfunction of the
intestinal mucosal barrier (11).
The present study demonstrated that the expression levels of
occludin and ZO-1 proteins were significantly reduced in the
intestinal tissues of rats with COPD compared with those of normal
rats. These observations indicate destruction of the tight
junctions in the intestinal tissues of rats in the COPD group,
which might result in structural changes and dysfunction of the
intestinal mucosal barrier.
It is challenging to evaluate the intestinal mucosal
barrier function directly; however, commonly used indirect measures
are based on determinations of intestinal permeability, serum
D-lactate levels and serum DAO activity. DAO is the marker enzyme
of intestinal mucosal cells, which exists at low serum levels under
normal conditions but is released into the blood, increasing serum
levels, if these cells are damaged; therefore, DAO activity
reflects the degree of damage to the intestinal mucosa. Intestinal
permeability is determined mainly by using sugar probe molecules.
Since mannitol and lactulose have a high recycling rate and are
minimally affected by the intraluminal osmotic pressure, these
molecules are ideal sugar probes that have been widely applied to
determine the permeability of the intestinal mucosa (12). The urinary L/M ratio accurately
reflects intestinal permeability, with increased L/M values
indicating an increase in permeability and impaired intestinal
mucosal barrier function (8). The
results of the present study revealed that the serum DAO level and
urinary L/M value were both significantly increased in the rats of
the COPD group, indicating the presence of increased intestinal
permeability and impaired intestinal mucosal barrier function. By
detecting the plasma intestinal fatty acid binding protein levels
and urinary sucralose to erythritol ratios, Rutten et al
(5) demonstrated that enterocyte
damage and intestinal hyperpermeability occurred in patients with
COPD. Their results indicate the presence of structural changes and
dysfunction of the intestinal mucosal barrier in patients with
COPD, and the results of the present study are consistent with
these previous observations.
At present, although the pathogenesis of
COPD-induced intestinal mucosal barrier dysfunction in patients
with COPD remains unclear, inflammatory reactions are a possible
mechanism. It has previously been demonstrated that cytokines
regulate intestinal tight junctions under pathological states
(13). Cytokine-induced tight
junction dysfunction caused by immune activation or tissue
inflammation is considered to play an important role in the
occurrence and development of intestinal and other systemic
diseases (14). In the present
study, higher intestinal levels of IFN-γ, TNF-α and IL-8 were found
in the COPD group compared with those in normal rats, which
revealed that increased levels of cytokines and an elevated
inflammatory responses in the intestinal tissues of the rats with
COPD. Suzuki (15) and Yang et
al (16) found that IFN-γ causes
damage to tight junction structures by inducing the redistributed
expression and intracellular uptake of tight junction proteins,
while Amasheh et al (17) and
Ye et al (18) reported that
TNF-α causes structural changes of the tight junctions by promoting
the loss of claudin 1, increasing claudin 2 expression and
enhancing the degeneration of occludin and ZO-1. Increased tissue
levels of IL-8 have been found in patients with IBD, which could
contribute to the occurrence of mucosal damage and ulcers (19). The present study showed that the
intestinal expression levels of occludin and ZO-1 proteins were
reduced in the rats of the COPD group, which might be associated
with the increased levels of intestinal cytokines and further
damage to tight junctions. Therefore, it may be inferred that
structural and dysfunctional changes of the intestinal mucosal
barrier in patients with COPD are associated with enhanced
inflammatory responses. In addition, IFN-γ, TNF-α and IL-8 might be
important inflammatory mediators of the pathogenesis of COPD.
However, the specific relationship between pulmonary and intestinal
inflammation in COPD requires further investigation. Moreover,
these observations raise the question of whether intestinal
inflammation and the damage and dysfunction of the intestinal
mucosal barrier could also be controlled by inhaled corticosteroid
therapy for intrapulmonary inflammation.
In summary, the results of the present study reveal
that increased intestinal inflammation resembling that in the lungs
is present in a rat model of COPD. These increased inflammatory
responses cause damage to the tight junction structures, resulting
in structural and functional changes of the intestinal mucosal
barrier. However, the specific association between pulmonary and
intestinal inflammation in COPD, in addition to the potential of
using inhaled corticosteroid therapy for intrapulmonary
inflammation to provide an effective treatment for associated
intestinal inflammation require further investigation.
Glossary
Abbreviations
Abbreviations:
|
COPD
|
chronic obstructive pulmonary
disease
|
|
DAO
|
diamine oxidase
|
|
IBD
|
inflammatory bowel disease
|
|
SD
|
Sprague-Dawley
|
|
HPLC
|
high performance liquid
chromatography
|
|
TNF-α
|
tumor necrosis factor-α
|
|
IFN-γ
|
interferon-γ
|
|
CS
|
cigarette smoke
|
|
H&E
|
hematoxylin and eosin
|
|
ECL
|
enhanced chemiluminescence
|
|
NS
|
normal saline
|
References
|
1
|
Abdool-Gaffar MS, Ambaram A, Ainslie GM,
Bolliger CT, Feldman C, Geffen L, Irusen EM, Joubert J, Lalloo UG,
Mabaso TT, et al: COPD Working Group: Guideline for the management
of chronic obstructive pulmonary disease - 2011 update. S Afr Med
J. 101:63–73. 2011.PubMed/NCBI
|
|
2
|
Mestecky J: The common mucosal immune
system and current strategies for induction of immune responses in
external secretions. J Clin Immunol. 7:265–276. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Garg P, Vijay-Kumar M, Wang L, Gewirtz AT,
Merlin D and Sitaraman SV: Matrix metalloproteinase-9-mediated
tissue injury overrides the protective effect of atrix
metalloproteinase-2 during colitis. Am J Physiol Gastrointest Liver
Physiol. 296:G175–G184. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Keely S, Talley NJ and Hansbro PM:
Pulmonary-intestinal cross-talk in mucosal inflammatory disease.
Mucosal Immunol. 5:7–18. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Rutten EP, Lenaerts K, Buurman WA and
Wouters EF: Disturbed intestinal integrity in patients with COPD:
Effects of activities of daily living. Chest. 145:245–252. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Zheng H, Liu Y, Huang T, Fang Z, Li G and
He S: Development and characterization of a rat model of chronic
obstructive pulmonary disease (COPD) induced by sidestream
cigarette smoke. Toxicol Lett. 189:225–234. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Li MM, Xin XF, Shao HT, Shi Y, Su X, Sun
WK, Sun H and Fang LP: The expressions of nerve growth factor and
its tyrosine kinase A receptor on alveolar macrophages in a rat
model of chronic obstructive pulmonary disease. Zhonghua Jie He He
Hu Xi Za Zhi. 35:601–605. 2012.(In Chinese). PubMed/NCBI
|
|
8
|
Liu H, Li W, Wang X, Li J and Yu W: Early
gut mucosal dysfunction in patients with acute pancreatitis.
Pancreas. 36:192–196. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Thomsen M, Dahl M, Lange P, Vestbo J and
Nordestgaard BG: Inflammatory biomarkers and comorbidities in
chronic obstructive pulmonary disease. Am J Respir Crit Care Med.
186:982–988. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Shen L: Tight junctions on the move:
Molecular mechanisms for epithelial barrier regulation. Ann NY Acad
Sci. 7:9–18. 2012. View Article : Google Scholar
|
|
11
|
Odenwald MA and Turner JR: Intestinal
permeability defects: Is it time to treat? Clin Gastroenterol
Hepatol. 11:1075–1083. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Tian R, Tan JT, Wang RL, Xie H, Qian YB
and Yu KL: The role of intestinal mucosa oxidative stress in gut
barrier dysfunction of severe acute pancreatitis. Eur Rev Med
Pharmacol Sci. 17:349–55. 2013.PubMed/NCBI
|
|
13
|
Cao M, Wang P, Sun C, He W and Wang F:
Amelioration of IFN-γ and TNF-α-induced intestinal epithelial
barrier dysfunction by berberine via suppression of MLCK-MLC
phosphorylation signaling pathway. PLoS One. 8:e619442013.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Turner JR: Intestinal mucosal barrier
function in health and disease. Nat Rev Immunol. 9:799–809. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Suzuki T: Regulation of intestinal
epithelial permeability by tight junctions. Cell Mol Life Sci.
70:631–659. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Yang S, Yu M, Sun L, Xiao W, Yang X, Sun
L, Zhang C, Ma Y, Yang H, Liu Y, et al: Interferon-γ-induced
intestinal epithelial barrier dysfunction by NF-kB/HIF-1α pathway.
J Interferon Cytokine Res. 34:195–203. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Amasheh M, Fromm A, Krug SM, Amasheh S,
Andres S, Zeitz M, Fromm M and Schulzke JD: TNFalpha-induced and
berberine-antagonized tight junction barrier impairment via
tyrosine kinase, Akt and NFkappaB signaling. J Cell Sci.
123:4145–4155. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Ye D, Guo S, Al-Sadi R and Ma TY: MicroRNA
regulation of intestinal epithelial tight junction permeability.
Gastroenterology. 141:1323–1333. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Műzes G, Molnár B, Tulassay Z and Sipos F:
Changes of the cytokine profile in inflammatory bowel diseases.
World J Gastroenterol. 18:5848–5861. 2012. View Article : Google Scholar : PubMed/NCBI
|