Introduction
Hepatocellular carcinoma (HCC) is the fifth most
common cancer in men and the seventh in women worldwide, and it
ranks third among the total number of deaths from cancer (1). HCC is particularly prevalent in Africa
and eastern/south eastern Asia. Surgical resection and liver
transplantation remains the optimal therapeutic strategy for the
treatment of HCC. However, due to poor liver conditions, such as
cirrhosis and liver dysfunction, only a minority of HCC patients
are eligible for surgical intervention, and access to
transplantation is limited by the scarcity of donor organs
(2,3). Furthermore, the majority of HCC
patients are diagnosed during the late or end stages, thus missing
the best opportunity for surgical resection. In addition,
recurrence and metastasis are frequently detected in patients who
undergo surgical resection and the postoperative 5-year survival
rate remains low at 30–40% (4).
Therefore, it is of great importance that the potential initial
molecular mechanisms of HCC progression are investigated in order
to identify biomarkers that may be used to evaluate whether HCC
patients are at high risk of metastasis or recurrence.
MicroRNAs (miRs) are a family of single-stranded,
highly conserved, non-coding functional RNAs (5,6). As
>50% of human miRs are located at fragile sites or in
cancer-associated genomic regions (7), they may be used as novel biomarkers for
the assessment of cancer and potential therapeutic targets. It has
previously been reported that miRs act as tumor suppressive genes
and oncogenes (8). Various studies
have been performed to investigate the association between miRs and
human tumors (9–11). Several metastasis-associated miRs
have been detected in HCC, including miR-338, miR-19a and miR-122a
(12). miR-132, which is located on
human chromosome 17p13.3, has been associated with various human
cancers including osteosarcoma, colorectal cancer (13,14),
breast cancer (15,16), pancreatic cancer (17–20),
prostate cancer (21), gastric
cancer (22) and glioma (23,24).
Furthermore, Wei et al (25)
also investigated the association between miR-132 and hepatitis B
virus (HBV)-associated HCC. However, this study only included 20
paired samples and did not investigate the association between
miR-132 and clinicopathological factors or recurrence in patients
with HCC. To the best of our knowledge, there has been no
investigation of the association between miR-132 levels and
recurrence in any previous study to date. Therefore, a large cohort
is required to validate the clinical significance of miR-132 in
patients with HCC.
In the present study, reverse
transcription-quantitative polymerase chain reaction (RT-qPCR) was
performed to assess the expression levels of miR-132 in HCC
patients. Subsequently, the associations between miR-132 expression
levels, clinical parameters and recurrence were investigated in
patients with HCC.
Materials and methods
Patients and tissue samples
A total of 95 formalin-fixed, paraffin embedded
(FFPE) HCC tissues and their matched adjacent non-cancerous liver
tissues were obtained from patients who underwent surgery in the
Department of Hepatobiliary Surgery at the First Affiliated
Hospital of Guangxi Medical University (Nanning, China) between
March 2010 and December 2011. The mean age of the enrolled patients
was 52 years (range, 29–82 years), and the mean size of the tumors
was 6.4 cm (range, 1–11 cm). Pathologic diagnosis was independently
performed by two experienced pathologists. A total of 75 men and 20
women were enrolled in the present study. The characteristics of
the patients are shown in Table I.
None of the patients had previously received preoperative
treatments and the present hepatectomy was the first for each
patient. The study protocol was approved by the Research Ethics
Committee of the First Affiliated Hospital of Guangxi Medical
University. Written informed consent was obtained from each
patient.
 | Table I.Association between the expression of
miR-132 and clinicopathological features in patients with HCC. |
Table I.
Association between the expression of
miR-132 and clinicopathological features in patients with HCC.
|
|
| Relative expression
of miRNA-132 (2−ΔΔCq) |
|---|
|
|
|
|
|---|
| Clinicopathological
features | N | Mean ± SD | t-value | P-value |
|---|
| Tissue |
|
| −5.731 | <0.001 |
|
Adjacent non-cancerous
liver | 95 | 2.7326±1.1475 |
|
|
|
HCC | 95 | 1.9245±0.7564 |
|
|
| Age |
|
| 0.696 | 0.488 |
| ≥50
years | 46 | 1.9804±0.8967 |
|
|
| <50
years | 49 | 1.8720±0.6006 |
| Gender |
|
| 0.381 | 0.704 |
|
|
|
Male | 75 | 1.9399±0.7858 |
|
|
|
Female | 20 | 1.8670±0.6490 |
|
|
|
Differentiation |
|
| 0.272 | 0.763 |
|
High | 6 | 1.9167±0.9745 |
|
|
|
Moderate | 60 | 1.8837±0.7898 |
|
|
|
Low | 29 | 2.0107±0.6522 |
|
|
| Size |
|
| 0.007 | 0.994 |
| <5
cm | 8 | 1.9233±0.8599 |
|
|
| ≥5
cm | 77 | 1.9248±0.7363 |
|
|
| Tumor nodes |
|
| 0.370 | 0.712 |
|
Single | 52 | 1.9508±0.7608 |
|
|
|
Multi | 43 | 1.8928±0.7588 |
|
|
| Metastasis |
|
| 2.193 | 0.031 |
| Without
metastasis | 46 | 2.0967±0.7740 |
|
|
| With
metastasis | 49 | 1.7629±0.7096 |
|
|
| Clinical TNM
stage |
|
| 2.323 | 0.022 |
|
I–II | 22 | 2.2455±0.7900 |
|
|
|
III–IV | 73 | 1.8278±0.7238 |
|
|
| Portal vein tumor
embolus |
|
| 0.261 | 0.794 |
| − | 63 | 1.9390±0.8197 |
|
|
| + | 32 | 1.8959±0.6243 |
|
|
| Vaso-invasion |
|
| −0.044 | 0.965 |
| − | 59 | 1.9219±0.8013 |
|
|
| + | 36 | 1.9289±0.6873 |
|
|
| Tumor capsular
infiltration |
|
| 2.264 | 0.026 |
| With
complete capsule | 45 | 2.1058±0.7603 |
|
|
| No
capsule or infiltration | 50 | 1.7614±0.7219 |
|
|
| HCV |
|
| 1.023 | 0.309 |
| − | 63 | 1.9811±0.7596 |
|
|
| + | 32 | 1.8131±0.7494 |
| HBV |
|
| 4.594 | <0.001 |
| − | 17 | 2.6176±0.9534 |
|
|
| + | 78 | 1.7735±0.6167 |
|
|
| AFP |
|
| −1.803 | 0.075 |
| − | 41 | 2.0722±0.8840 |
|
|
| + | 38 | 1.7634±0.5986 |
|
|
| Cirrhosis |
|
| −1.654 | 0.101 |
| − | 50 | 2.0452±0.7716 |
|
|
| + | 45 | 1.7904±0.7241 |
|
|
| NM23 |
|
| 2.146 | 0.034 |
| − | 20 | 2.2410±0.6714 |
|
|
| + | 75 | 1.8401±0.7594 |
|
|
| MTDH1 |
|
| −0.133 | 0.895 |
| − | 38 | 1.9055±0.8265 |
|
+/++/+++ | 51 | 1.9275±0.7251 |
|
|
|
MTDH2 |
|
| 0.187 | 0.852 |
|
-/+ | 50 | 1.9316±0.7788 |
|
|
|
++/+++ | 39 | 1.9008±0.7580 |
|
|
| P53 |
|
| 1.064 | 0.290 |
| − | 40 | 2.0212±0.6458 |
|
|
| + | 55 | 1.8542±0.8262 |
|
|
| P21 |
|
| 0.201 | 0.841 |
| − | 62 | 1.9360±0.7050 |
|
|
| + | 33 | 1.9030±0.8558 |
|
|
| VEGF |
|
| 0.431 | 0.667 |
| − | 25 | 1.9808±0.7791 |
|
|
| + | 70 | 1.9044±0.7528 |
|
|
| Ki-67 labeling
index |
|
| 2.893 | 0.005 |
|
Low | 47 | 2.1430±0.7889 |
|
|
|
High | 48 | 1.7106±0.6637 |
|
|
| MVD |
|
| 1.229 | 0.222 |
|
Low | 47 | 2.0206±0.7705 |
|
|
|
High | 48 | 1.8304±0.7381 |
|
|
RNA isolation and RT-qPCR
Total RNA was extracted from FFPE cancer
(OD260/280, 1.84–2.06) and adjacent non-cancerous liver
tissues (OD260/230, 1.90–2.04) using miRNeasy
FFPE kit (73504; Qiagen AB, Sollentuna, Sweden), according to
previous reports (26–29). Expression levels of miR-132 were
evaluated using RT and qPCR kits. In order to remove genomic DNA,
the following mixture with a total volume of 10.0 µl was used: 2.0
µl 5X gDNA Eraser buffer, 1.0 µl gDNA Eraser, and trace amount of
total RNA with extra RNase-free water. The mixture was maintained
at 42°C for 2 min and then at 4°C until further use. Reverse
transcription of total RNA into cDNA was performed with the TaqMan
MicroRNA Reverse Transcription kit (4366596; Applied Biosystems;
Thermo Fisher Scientific, Inc., Waltham, MA, USA) in a total volume
of 20.0 µl, including 10.0 µl from the previous step (removal of
genomic DNA), 4.0 µl 5X PrimeScript Buffer 2, 1.0 µl PrimeScript
RTEnzyme Mix I, 1.0 µl RT Primer Mix, and 4.0 µl RNase-free water.
qPCR analysis of miRNA was performed using a PCR7900 thermal cycler
(Applied Biosystems; Thermo Fisher Scientific, Inc.). RNU6B and
RNU48 were selected as endogenous controls. Primers were purchased
from Applied Biosystems (Thermo Fisher Scientific, Inc.) and the
respective sequences were as follows: miR-132,
UAACAGUCUACAGCCAUGGUCG; RNU6B,
CGCAAGGAUGACACGCAAAUUCGUGAAGCGUUCCAUAUUUUU; and RNU48,
GAUGACCCCAGGUAACUCUGAGUGUGUCGCUGAUGCCAUCACCGCAGCGCUCUGACC.
NormFinder (MOMA, Aarhus, Denmark) and geNorm (genorm.cmgg.be) were
used to select RNU6B and RNU48 as endogenous controls. PCR primers
for miR-132, RNU6B and RNU48 were included in the TaqMan MicroRNA
assay kit (4427975; Applied Biosystems; Thermo Fisher Scientific,
Inc.). A PCR reaction system with a total volume of 20.0 µl was
employed, including 10.0 µl LightCycler 480 SYBR Green I Master
(Roche Diagnostics GmbH, Mannheim, Germany), 0.8 µl PCR forward
primer (10 µM), 0.8 µl PCR reverse primer (10 µM), 1.0 µl cDNA
template (<100 ng) and 7.4 µl RNase-free water. A LightCycler
480 (Roche Diagnostics GmbH) was used to perform PCR under the
following conditions: Pre-denaturation at 95°C for 5 min; 40 cycles
of 95°C for 10 sec, 60°C for 10 sec, and 72°C for 10 sec; analysis
of solubility curve at 95°C for 5 sec and 65°C for 1 min); and then
cooling at 40°C for 30 sec. Each reaction was performed in
triplicate. Relative mRNA expression levels of miR-132 were
calculated using the 2−ΔΔCq method (30).
Statistical analysis
Statistical analysis was conducted using SPSS 20.0
(IBM SPSS, Armonk, NY, USA) for Windows. Independent samples t-test
and one-way analysis of variance were used to determine the
differences between the groups. Data were presented as the mean
±standard deviation. Receiver operating characteristic (ROC) curve
was used to identify the predictive power of miR-132. Spearman
correlation analysis was performed to investigate the association
between miR-132 expression levels and clinicopathological
parameters. Kaplan-Meier and log-rank tests were performed to
assess the association between the expression levels of miR-132 and
recurrence in patients with HCC. All reported P-values were two
tailed, and P<0.05 was considered to indicate a statistically
significant difference.
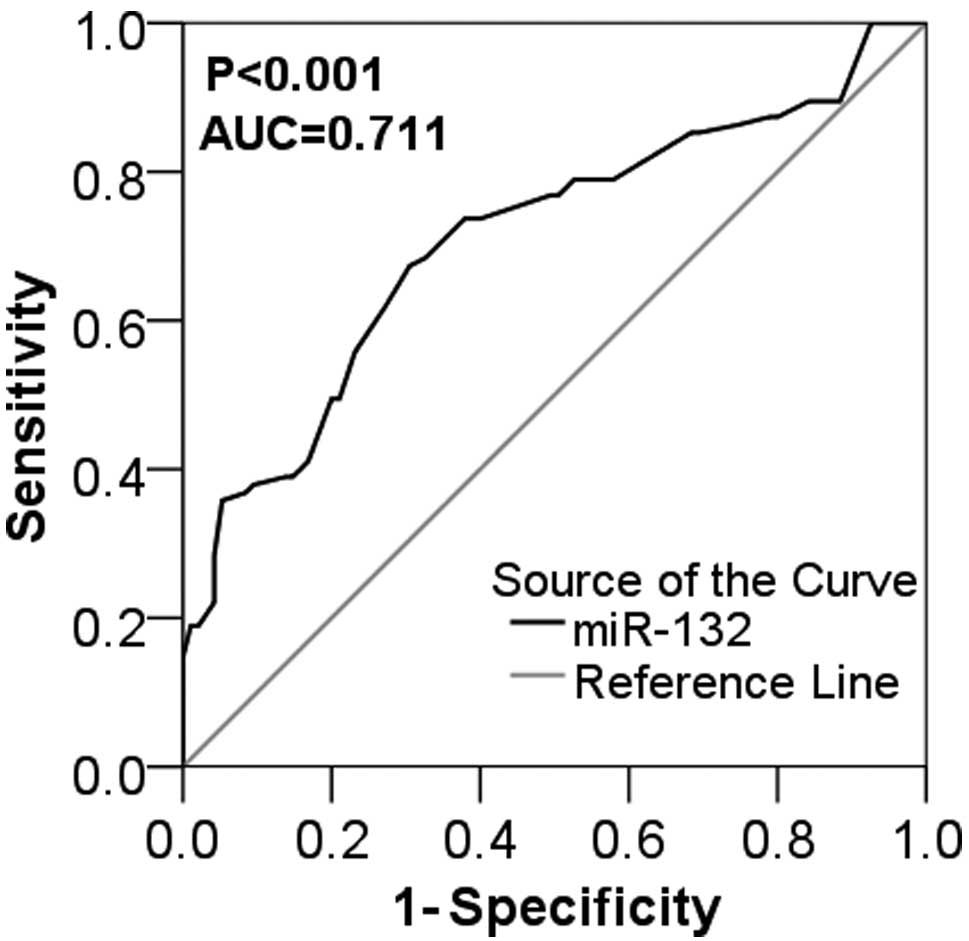
Results
miR-132 expression is downregulated in
HCC
Following normalization against RNU6B and RNU48
expression levels, the expression levels of miR-132 in HCC tissues
was demonstrated to be significantly decreased, as compared with
adjacent non-tumorous tissues (1.9245±0.7564 vs. 2.7326±1.1475;
P<0.001; Table I). The area under
curve (AUC) of ROC used to distinguish cancerous from non-cancerous
tissue was 0.711 for miR-132 expression [95% confidence interval
(CI), 0.637–0.785; P<0.001; Fig.
1] and the optimal cut-off value was 2.25. Thus, the results
indicated that miR-132 expression was downregulated in HCC.
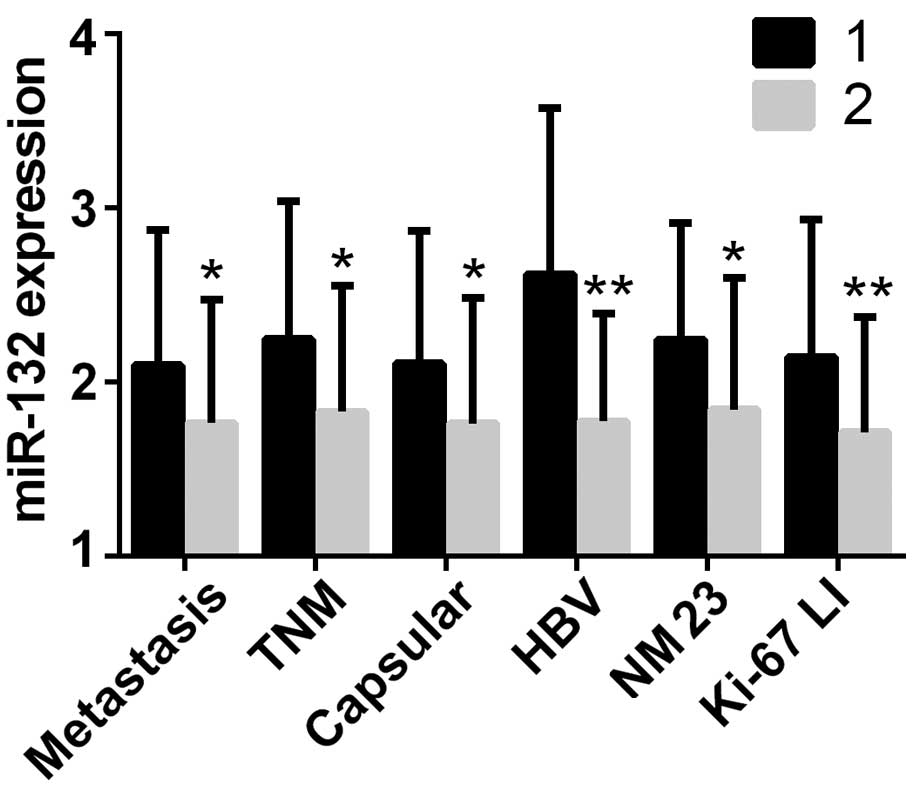
Association of miR-132 expression with
clinicopathological features in HCC patients. The associations
between miR-132 expression levels and pathological characteristics
were analyzed in order to better elucidate the potential role of
miR-132 in the development and progression of HCC. The results
suggested that the expression levels of miR-132 were significantly
decreased in HCC tissues with distant metastasis (P=0.031),
advanced clinical TNM stage (P=0.022) and tumor infiltration or no
capsule (P=0.026), as compared with the adjacent non-cancerous
tissues (Table I; Fig. 2). Similar outcomes were observed in
the HBV-positive group (P<0.001), NM23-expressed group
(P=0.034), and high Ki-67 labeling index (LI) group (P=0.005)
(Table I; Fig. 2). No significant differences were
detected in the expression levels of miR-132 and age, gender,
histological differentiation, tumor size, tumor nodes, portal vein
tumor embolus, micro-vascular invasion, hepatitis C virus,
α-fetoprotein, para-carcinoma cirrhosis, metadherin, p53, p21,
vascular endothelial growth factor, or microvessel density
(Table I). Spearman correlation
analysis was performed to investigate these associations. Positive
results were detected between the expression levels of miR-132 and
capsules (r=−0.207; P=0.044), HBV (r=−0.351;
P<0.001), NM23 (r=−0.220; P=0.032), and Ki-67 LI
(r=−0.264; P=0.010). The cut-off value for miR-132 was 2.15.
False positive and false negative rates were 0.22 and 0.556,
respectively. Therefore, the results revealed that miR-132
expression was associated with several clinical parameters in
HCC.
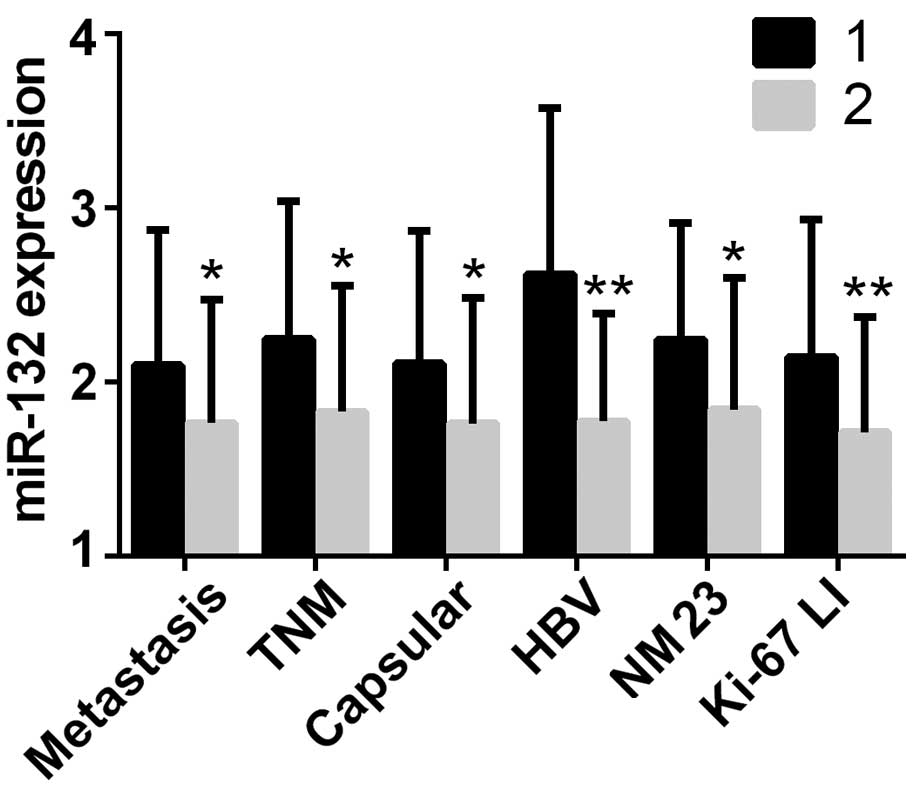 | Figure 2.Statistically significant
correlations between miR-132 expression levels and
clinicopathological parameters. miR-132 expression levels were
significantly downregulated in hepatocellular carcinoma tissues
with distant metastasis (P=0.031), advanced clinical TNM stage
(P=0.022) and tumor infiltration or no capsule (P=0.026), as well
as the hepatitis B virus (HBV)-positive group (P<0.001), the
NM23-expressed group (P=0.034), and the high Ki-67 labeling index
(LI) group (P=0.005). *P<0.05 and **P<0.01, vs. group 1.
Metastasis: 1, without metastasis; 2, with metastasis. TNM: 1,
I–II; 2, III–IV. Capsular: 1, with complete capsule; 2, no capsule
or infiltration. HBV: 1, HBV-negative; 2, HBV-negative. NM23: 1,
NM23-negative; 2, NM23-positive. Ki-67 LI: 1, low; 2, high. TNM,
tumor, node and metastatis; HBV, hepatitis B virus; NM23 |
Recurrence analysis
Median duration of follow-up was 32.78±1.43 months
(range, 2.68–68.00 months) for the patients who were successfully
followed up. Among the 70 HCC patients with recurrence data
included in the present study, 59 exhibited recurrent tumors and
data from 11 patients were not included due to subsequent
mortality, withdrawal or loss to follow-up. The median level of
miR-132 expression among the 70 patients followed up was 1.89.
Accordingly, 1.89 was used as a cut-off value to divide the 70
patients into two respective groups, low expression (<1.89;
n=35) and high expression (>1.89; n=35). The overall recurrent
period of the whole group was 57.10 months (95% CI, 51.46–62.73).
The recurrent period in the high expression group (58.68 months;
95% CI, 51.59–65.76) was longer than the low expression group
(50.95 months; 95% CI, 45.71–56.20) despite the limited statistical
significance (χ2=0.430; P=0.512 log-rank test). Thus,
the results demonstrated that the high miR-132 expression group
showed a longer recurrent period by ~8 months compared with the low
expression group.
Discussion
The expression of miR-132 in human cancer has
attracted a large amount of research. Its molecular mechanisms have
been studied in osteosarcoma (31),
colorectal cancer (13), pituitary
tumor (32), prostate cancer
(21), breast cancer (15), lung cancer (33,34) and
pancreatic cancer (17–19). The majority of studies have
demonstrated the suppressive role of miR-132 in different classes
of cancers via various novel molecule networks. For example by
repressing CCNE1 expression (31),
targeting zinc finger E-box-binding homeobox 2 (ZEB2) (13), Sox5 (32), hematological and neurological
expressed 1 (HN1) (15) or ZEB2
(33) and being methylation-silenced
and antimetastatic in PCa controlling cellular adhesion (21), as well as via the induction of
acetylcholinesterase-independent apoptosis (31). All of these studies mention
identified miR-132 as a tumor suppressor. However, a discrepancy in
the data was detected in pancreatic cancer. Luo et al
(19) demonstrated that
stem-cell-like BxPC-3-LN cells expressed lower levels of miR-132
than the parental BxPC-3 cells. Zhang et al (17) further supported this finding by
demonstrating the downregulation of miR-132 in pancreatic cancer
via promoter methylation.
Researchers have also investigated the clinical
significance of miR-132 in various tumors, where greater divergence
emerged by predominantly focusing on the different expression
levels of miR-132 between cancerous tissues and corresponding
non-cancerous tissues. miR-132 upregulation was observed in gastric
cancer (22), glioma (23,35) and
pancreatic cancer (18). Conversely,
miR-132 downregulation was detected in osteosarcoma (31,36),
colorectal cancer (13), ductal
carcinoma in situ of the breast (16), pancreatic cancer (17) and breast cancer (15), where lower levels of miR-132 were
observed in cancerous tissues, as compared with corresponding
non-cancerous tissues.
The clinical application of miR-132 remains a hot
topic in associated research. According to Cote et al
(20), miR-132 expressed in plasma
may be used as a diagnostic test for pancreatic ductal
adenocarcinoma when in conjunction with other miRNAs; whereas Chung
et al (37) suggested that
the downregulation of miR-132 in serum may be considered as one of
the novel biomarkers in serous ovarian cancer. Furthermore, Salendo
et al (14) demonstrated that
miR-132 may be able to identify the chemoradiosensitivity of
colorectal cancer cells. As for its utilization in differential
diagnosis, Lages et al (24)
concluded that deregulated miR-132 may facilitate the proper
discrimination of oligodendroglioma from glioblastoma.
In the present study, RT-qPCR was performed to
detect the expression levels of miR-132 in 95 paired HCC and
adjacent non-cancerous liver tissues to explore correlations with
clinicopathological features. Only one previous study has
investigated miR-132 in HCC, which predominantly focused on the
role of miR-132 in the mechanism of HBV-mediated
hepatocarcinogenesis (25). The
present study focused on the correlations between miR-132 and
clinicopathological parameters, and a larger cohort of 95 patients
was investigated compared with only 20 in the previous study.
Furthermore, recurrent free survival analysis was performed in the
present study, which the previous research lacked.
Concerning the expression of miR-132 in HCC, the
present findings were consistent with those published by Wei et
al (25), as the expression of
miR-132 in HCC was significantly reduced, as compared with the
corresponding normal tissues (P<0.001). Wei et al
(25) suggested that the
downregulation of miR-132 may be modulated by HBx expression via
DNA methylation. This hypothesis may help to explain the present
results despite the difference that all their cancerous tissues
were HBV-associated HCC tissues and various HCC tissues were not
included. Meanwhile, the AUC of the expression level of miR-132 was
0.711 (95% CI, 0.637–0.785; P<0.001), which implied that miR-132
may be used as a reference index in the diagnosis of HCC.
In an attempt to further complement the study
conducted by Wei et al (25),
the correlations between miR-132 expression levels and major
clinicopathological features in HCC were explored, which was absent
in their study. Firstly, decreased expression levels of miR-132
were observed in HCC tissues with distant metastasis (P=0.031),
advanced clinical TNM stage (P=0.022) and tumor infiltration or no
capsule (P=0.026). These findings inferred a tumor-suppressing
role, which suggests that miR-132 may have a role in HCC
progression. Secondly, the associations between miR-132 expression
and other conventional biomarkers in HCC, including HBV, NM23 and
Ki-67, were also investigated. HBV infection is a common risk
factor for the development of HCC (38). Nm23 gene is a putative metastatic
suppressor gene (39) and Ki-67 LI
can be used to indicate cell proliferative activity (40). miR-132 expression levels were
significantly reduced in the HBV-positive (P<0.001),
NM23-expressed (P=0.034), and high Ki-67 LI (P=0.005) groups.
Spearman correlation analysis demonstrated positive results between
the expression of miR-132 and HBV (r=−0.351, P<0.001),
NM23 (r=−0.220, P=0.032), and Ki-67 LI (r=−0.264,
P=0.010). Taken together, these results demonstrated that the
expression of miR-132 was elevated in HCC cells with reduced cell
proliferation, indicated that miR-132 may be associated with cell
proliferation in HCC.
Recurrence analysis was also performed in the
present study. Followed-up patients demonstrated a median of
follow-up duration of 32.78±1.43 months (range, 2.68–68.00 months).
The cohort, which was composed of 59 cases with recurrent tumors
and recurrence data as well as 11 censored cases, exhibited an
overall recurrent duration of 57.10 months (95% CI, 51.46–62.73).
As to the recurrent period, the high expression group (>1.8900,
n=35) exhibited a longer duration of 58.68 months (95% CI,
51.59–65.76), as compared with the low expression group
(<1.8900; n=35) (50.95 months; 95% CI, 45.71–56.20) in spite of
the inferior statistical value (χ2=0.430; P=0.512
log-rank test).
The findings of the present study, which was the
first to include recurrent analysis to investigate the correlations
between miR-132 and mainstream clinicopathological characteristics
in HCC, indicated that miR-132 may be significantly decreased in
HCC and may perform as a tumor suppressive gene in HCC development.
Nevertheless, some limitations still exist. Firstly, limited
insights were emphasized in terms of the molecular mechanisms.
Given the similar results of decreased miR-132 published by Wei
et al (25), their theory
that downregulation of miR-132 may result from the HBx expression
via DNA methylation may also apply to the present study. Other
targets in previous research into miR-132 in cancer, such as ZEB2
(13), Sox5 (32), HN1 (15) and ZEB2 (33), should not be ignored since consistent
suppressive roles of miR-132 were observed. Furthermore, tissue
analysis was employed in the present study, which has various
disadvantages over non-invasive methods such as serum detection.
Future studies should aim to harvest tissue and serum samples of
HCC in order to investigate the molecular networks or mechanisms of
miR-132 in HCC with a larger cohort.
In conclusion, the present study was the first to
investigate the associations between miR-132 and
clinicopathological parameters, including recurrence, in patients
with HCC. The results demonstrated that miR-132 is downregulated in
HCC. These findings strongly supported the hypothesis that miR-132
serves as a tumor suppressor in the development of HCC, and HCC
patients with downregulated miR-132 may suffer from poorer
outcomes. A subsequent study has been designed to investigate the
potential underlying mechanisms between HCC and miR-132 based on
the results from the present study.
Acknowledgements
The present study was supported by the Fund of
Guangxi Natural Scientific Research (grant no.
2013GXNSFBA019191).
References
|
1
|
Ferlay J, Shin HR, Bray F, Forman D,
Mathers C and Parkin DM: Estimates of worldwide burden of cancer in
2008: GLOBOCAN 2008. Int J Cancer. 127:2893–2917. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Schwartz M, Roayaie S and Konstadoulakis
M: Strategies for the management of hepatocellular carcinoma. Nat
Clin Pract Oncol. 4:424–432. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
El-Serag HB, Marrero JA, Rudolph L and
Reddy KR: Diagnosis and treatment of hepatocellular carcinoma.
Gastroenterology. 134:1752–1763. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Blum HE: Hepatocellular carcinoma: Therapy
and prevention. World J Gastroenterol. 11:7391–7400.
2005.PubMed/NCBI
|
|
5
|
Cho WC: OncomiRs: The discovery and
progress of microRNAs in cancers. Mol Cancer. 6:602007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Bartel DP: MicroRNAs: Genomics,
biogenesis, mechanism, and function. Cell. 116:281–297. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Calin GA, Sevignani C, Dumitru CD, Hyslop
T, Noch E, Yendamuri S, Shimizu M, Rattan S, Bullrich F, Negrini M
and Croce CM: Human microRNA genes are frequently located at
fragile sites and genomic regions involved in cancers. Proc Natl
Acad Sci USA. 101:2999–3004. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kent OA and Mendell JT: A small piece in
the cancer puzzle: microRNAs as tumor suppressors and oncogenes.
Oncogene. 25:6188–6196. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Li G, Shen Q, Li C, Li D, Chen J and He M:
Identification of circulating MicroRNAs as novel potential
biomarkers for hepatocellular carcinoma detection: A systematic
review and meta-analysis. Clin Transl Oncol. 17:684–693. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Zhang K, Zhang Y, Liu C, Xiong Y and Zhang
J: MicroRNAs in the diagnosis and prognosis of breast cancer and
their therapeutic potential (review). Int J Oncol. 45:950–958.
2014.PubMed/NCBI
|
|
11
|
Usó M, Jantus-Lewintre E, Sirera R,
Bremnes RM and Camps C: miRNA detection methods and clinical
implications in lung cancer. Future Oncol. 10:2279–2292. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Budhu A, Jia HL, Forgues M, Liu CG,
Goldstein D, Lam A, Zanetti KA, Ye QH, Qin LX, Croce CM, et al:
Identification of metastasis-related microRNAs in hepatocellular
carcinoma. Hepatology. 47:897–907. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Zheng YB, Luo HP, Shi Q, Hao ZN, Ding Y,
Wang QS, Li SB, Xiao GC and Tong SL: miR-132 inhibits colorectal
cancer invasion and metastasis via directly targeting ZEB2. World J
Gastroenterol. 20:6515–6522. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Salendo J, Spitzner M, Kramer F, Zhang X,
Jo P, Wolff HA, Kitz J, Kaulfuß S, Beißbarth T, Dobbelstein M, et
al: Identification of a microRNA expression signature for
chemoradiosensitivity of colorectal cancer cells, involving
miRNAs-320a, −224, −132 and let7g. Radiother Oncol. 108:451–457.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Zhang ZG, Chen WX, Wu YH, Liang HF and
Zhang BX: MiR-132 prohibits proliferation, invasion, migration, and
metastasis in breast cancer by targeting HN1. Biochem Biophys Res
Commun. 454:109–114. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Li S, Meng H, Zhou F, Zhai L, Zhang L, Gu
F, Fan Y, Lang R, Fu L, Gu L and Qi L: MicroRNA-132 is frequently
down-regulated in ductal carcinoma in situ (DCIS) of breast and
acts as a tumor suppressor by inhibiting cell proliferation. Pathol
Res Pract. 209:179–183. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Zhang S, Hao J, Xie F, Hu X, Liu C, Tong
J, Zhou J, Wu J and Shao C: Downregulation of miR-132 by promoter
methylation contributes to pancreatic cancer development.
Carcinogenesis. 32:1183–1189. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Park JK, Henry JC, Jiang J, Esau C, Gusev
Y, Lerner MR, Postier RG, Brackett DJ and Schmittgen TD: miR-132
and miR-212 are increased in pancreatic cancer and target the
retinoblastoma tumor suppressor. Biochem Biophys Res Commun.
406:518–523. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Luo G, Long J, Cui X, Xiao Z, Liu Z, Shi
S, Liu L, Liu C, Xu J, Li M and Yu X: Highly lymphatic metastatic
pancreatic cancer cells possess stem cell-like properties. Int J
Oncol. 42:979–984. 2013.PubMed/NCBI
|
|
20
|
Cote GA, Gore AJ, McElyea SD, Heathers LE,
Xu H, Sherman S and Korc M: A pilot study to develop a diagnostic
test for pancreatic ductal adenocarcinoma based on differential
expression of select miRNA in plasma and bile. Am J Gastroenterol.
109:1942–1952. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Formosa A, Lena AM, Markert EK, Cortelli
S, Miano R, Mauriello A, Croce N, Vandesompele J, Mestdagh P,
Finazzi-Agrò E, et al: DNA methylation silences miR-132 in prostate
cancer. Oncogene. 32:127–134. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Liu X, Yu H, Cai H and Wang Y: The
expression and clinical significance of miR-132 in gastric cancer
patients. Diagn Pathol. 9:572014. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Liu Q, Liao F, Wu H, Cai T, Yang L, Wang
ZF and Zou R: Upregulation of miR-132 expression in glioma and its
clinical significance. Tumour Biol. 35:12299–12304. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Lages E, Guttin A, El Atifi M, Ramus C,
Ipas H, Dupré I, Rolland D, Salon C, Godfraind C, de Fraipont F, et
al: MicroRNA and target protein patterns reveal physiopathological
features of glioma subtypes. PLoS One. 6:e206002011. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Wei X, Tan C, Tang C, Ren G, Xiang T, Qiu
Z, Liu R and Wu Z: Epigenetic repression of miR-132 expression by
the hepatitis B virus × protein in hepatitis B virus-related
hepatocellular carcinoma. Cell Signal. 25:1037–1043. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Gan TQ, Tang RX, He RQ, Dang YW, Xie Y and
Chen G: Upregulated MiR-1269 in hepatocellular carcinoma and its
clinical significance. Int J Clin Exp Med. 8:714–721.
2015.PubMed/NCBI
|
|
27
|
Pan L, Huang S, He R, Rong M, Dang Y and
Chen G: Decreased expression and clinical significance of miR-148a
in hepatocellular carcinoma tissues. Eur J Med Res. 19:682014.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Rong M, He R, Dang Y and Chen G:
Expression and clinicopathological significance of miR-146a in
hepatocellular carcinoma tissues. Ups J Med Sci. 119:19–24. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Rong M, Chen G and Dang Y: Increased
miR-221 expression in hepatocellular carcinoma tissues and its role
in enhancing cell growth and inhibiting apoptosis in vitro. BMC
Cancer. 13:212013. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(−Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Wang J, Xu G, Shen F and Kang Y: miR-132
targeting cyclin E1 suppresses cell proliferation in osteosarcoma
cells. Tumour Biol. 35:4859–4865. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Renjie W and Haiqian L: MiR-132, miR-15a
and miR-16 synergistically inhibit pituitary tumor cell
proliferation, invasion and migration by targeting Sox5. Cancer
Lett. 356:568–578. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
You J, Li Y, Fang N, Liu B, Zu L, Chang R,
Li X and Zhou Q: MiR-132 suppresses the migration and invasion of
lung cancer cells via targeting the EMT regulator ZEB2. PLoS One.
9:e918272014. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Zhang B, Lu L and Zhang X, Ye W, Wu J, Xi
Q and Zhang X: Hsa-miR-132 regulates apoptosis in non-small cell
lung cancer independent of acetylcholinesterase. J Mol Neurosci.
53:335–344. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Parker NR, Correia N, Crossley B, Buckland
ME, Howell VM and Wheeler HR: Correlation of MicroRNA 132
Up-regulation with an unfavorable clinical outcome in patients with
primary glioblastoma multiforme treated with radiotherapy plus
concomitant and adjuvant temozolomide chemotherapy. Transl Oncol.
6:742–748. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Yang J, Gao T, Tang J, Cai H, Lin L and Fu
S: Loss of microRNA-132 predicts poor prognosis in patients with
primary osteosarcoma. Mol Cell Biochem. 381:9–15. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Chung YW, Bae HS, Song JY, Lee JK, Lee NW,
Kim T and Lee KW: Detection of microRNA as novel biomarkers of
epithelial ovarian cancer from the serum of ovarian cancer
patients. Int J Gynecol Cancer. 23:673–679. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Kumar M, Kumar R, Hissar SS, Saraswat MK,
Sharma BC, Sakhuja P and Sarin SK: Risk factors analysis for
hepatocellular carcinoma in patients with and without cirrhosis: A
case-control study of 213 hepatocellular carcinoma patients from
India. J Gastroenterol Hepatol. 22:1104–1111. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Takada S and Koike K: Trans-activation
function of a 3′truncated X gene-cell fusion product from
integrated hepatitis B virus DNA in chronic hepatitis tissues. Proc
Natl Acad Sci USA. 87:5628–5632. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Koskinas J, Petraki K, Kavantzas N, Rapti
I, Kountouras D and Hadziyannis S: Hepatic expression of the
proliferative marker Ki-67 and p53 protein in HBV or HCV cirrhosis
in relation to dysplastic liver cell changes and hepatocellular
carcinoma. J Viral Hepat. 12:635–641. 2005. View Article : Google Scholar : PubMed/NCBI
|