Introduction
Osteopetrosis is a rare bone disease, with an
estimated prevalence of 1 case in every 20,000 people (1). This disease, caused by metabolic
imbalances resulting from genetic mutations, was first reported in
1904 by the German radiologist Heinrich Albers-Schönberg, as
reviewed by Bollerslev (2) and
García et al (3). Within one
of a limited number of reports on this disease, García et al
(3) demonstrated osteomyelitis of
the mandible in a patient with osteopetrosis. The
pathophysiological mechanism of the disease involves an
osteoclastic dysfunction that results in an impaired bone
resorption ability; as a result, bone modeling and remodeling are
inhibited. The cortical bone mass is therefore able to increase in
density and develop into a hard, marble consistency when the
medullary bone is remodelled. Two types of osteopetrosis exist:
Malignant and benign, categorized based on mortality rate, and
disease severity is highly heritable (1). Malignant osteopetrosis, or autosomal
recessive osteopetrosis has a poor prognosis associated with
fatality in infancy. Patients with ARO demonstrate a survival rate
of 7%, even subsequent to curative treatment such as allogenic
hemopoietic stem cell transplantation (4). Currently, it is understood that
autosomal dominant osteopetrosis (ADO) is a relatively benign
disorder caused by a missense mutation in the ClCN7 gene (5). Benign osteopetrosis typically has a
late onset in children and adults, the symptoms are milder and
prognosis is better than in malignant osteopetrosis.
However, curative care is not available for patients
with the benign form, thus only supportive care is provided.
Osteopetrosis is difficult to treat and can cause complications,
such as chronic osteomyelitis and bone fractures, as a result of
poor blood supply and iatrogenic fractures. As there is no cure,
symptom management is important in order to increase the patient
survival rates.
The current study presents a case of chronic
mandibular osteomyelitis and a maxillary sinusitis-generated
fistula of benign osteopetrosis. The current recommended treatment
options include high-dose systemic antibiotics, debridement of the
necrotic region and hyperbaric oxygen (HBO) therapy (3). However, the current report describes
treatment without the use of high-dose antibiotics or HBO therapy,
a justified approach due to the insufficiency of the blood supply
to the bone. Treatment of the debrided fistula, which included
repeated flushing and cleaning using nasal endoscopy every 2 weeks
in the acute infected period, was successful. Subsequently, a
fistula developed through granuloma formation. Therefore, the
present study investigated whether the debridement and drainage of
pus from fistulas generated by maxillary sinusitis and chronic
osteomyelitis is an effective treatment method.
Case report
In December 2014, a 50-year-old Chinese female was
admitted to the Xiamen Chang Gung Hospital (Xiamen, China) for the
evaluation and treatment of chronic purulent nasal discharge in the
left side of the nose. The patient reported that the discharge
appeared 3 years previously, following a tooth extraction from the
left side of the mouth. Physical examination revealed red swelling
in the left mandible. Intraoral examination revealed exposed
necrotising bone in the left maxillary region, sixth, seventh and
eighth tooth agenesis in the upper left side and fistula formation.
The pus had accumulated in the mouth and the left side of the nose
in the fistula, generated as a result of maxillary sinusitis.
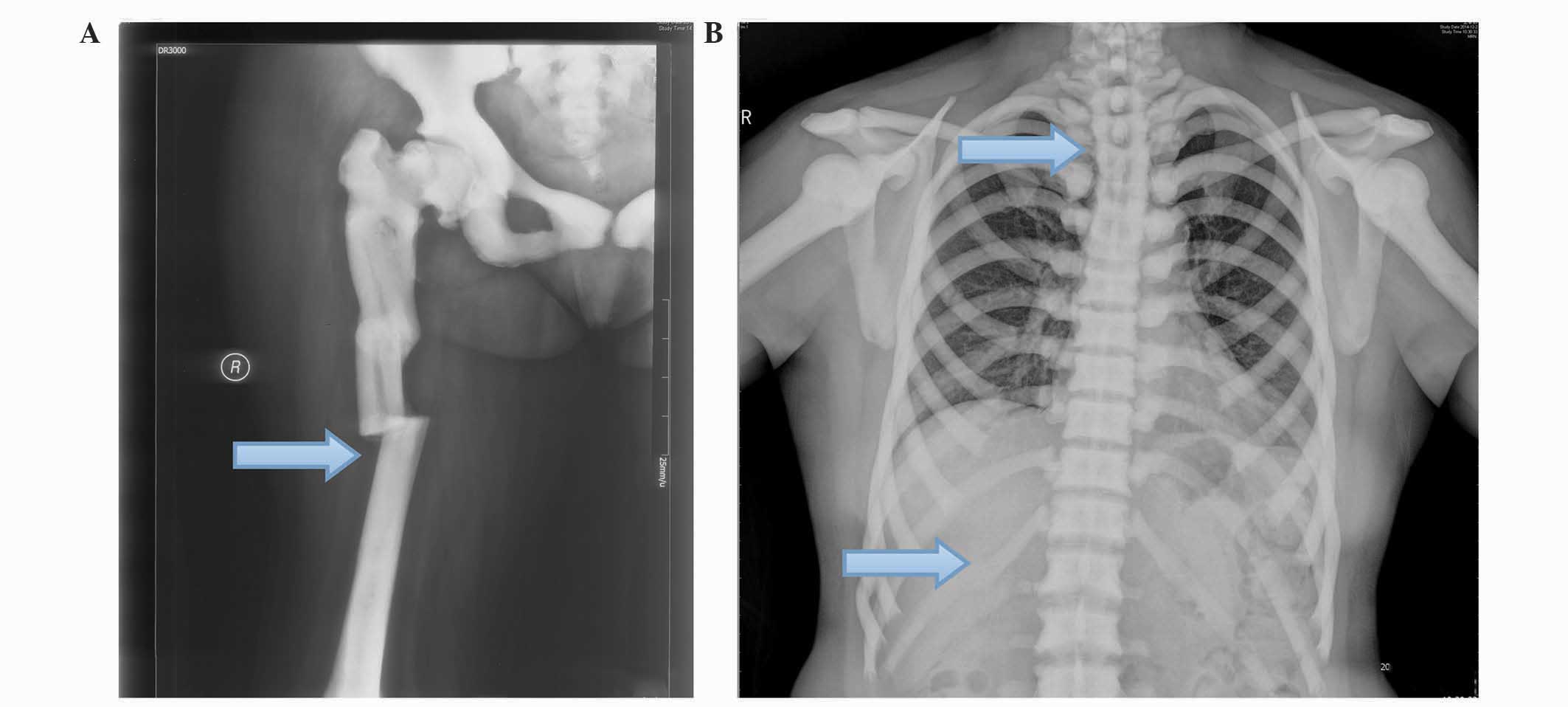
Previous medical history revealed that the patient was diagnosed
with osteopetrosis at the age of 19 years old, with six rib,
femoral and thoracic vertebra bone fractures (Fig. 1). The patient did not accept any
treatment for the osteopetrosis, but was fitted with a plaster cast
for 6 weeks. However, the patient developed splenomegaly due to
secondary bone marrow suppression, subsequent to which the spleen
was resected. Written informed consent was obtained from the
patient for these and the following procedures. Examination of the
patient's family history revealed that her older sibling was
diagnosed with osteopetrosis at the age of 23 years old, but the
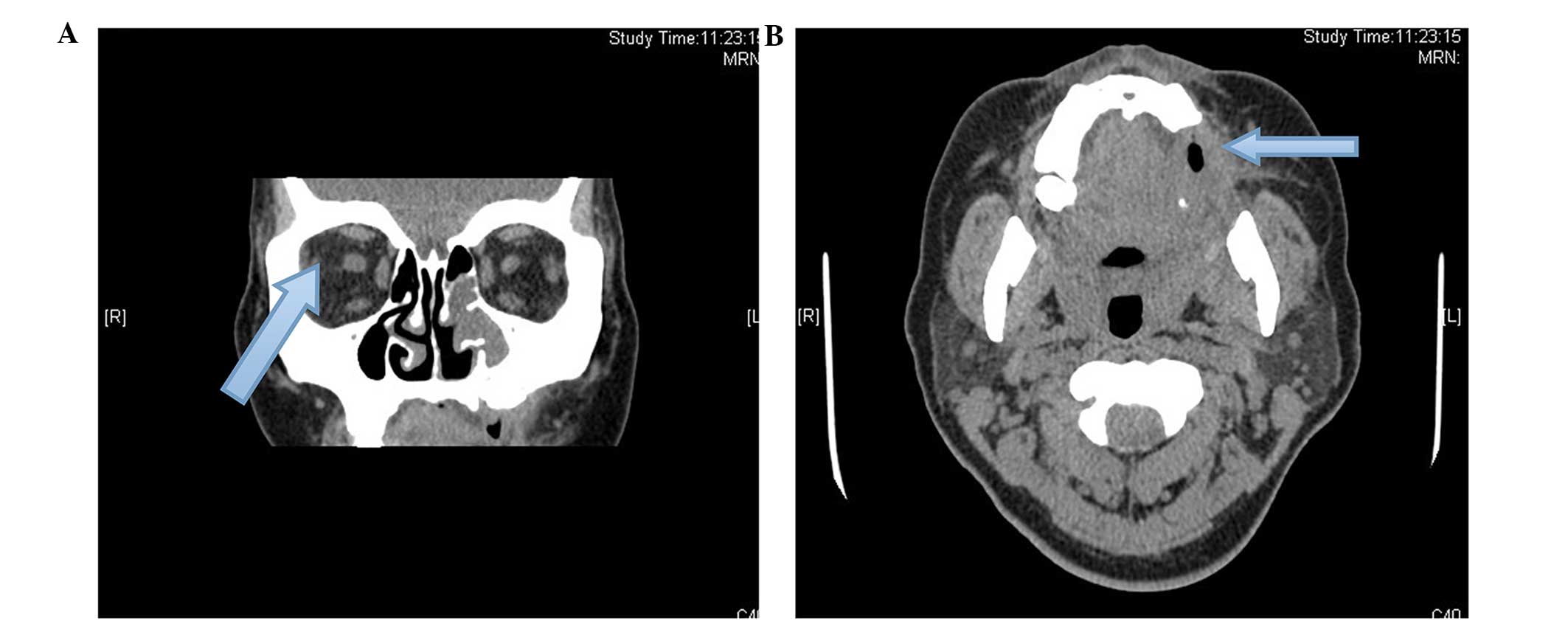
patient's child had not developed the disease. Non-contrast
computed tomography scans (GE Healthcare Life Sciences, Chalfont,
UK) displayed evidence of low bone density in the posterior left
side of the mandible with destruction of the vestibular cortex that
was suggestive of a fistula, resulting from chronic osteomyelitis
with maxillary sinusitis (Fig. 2).
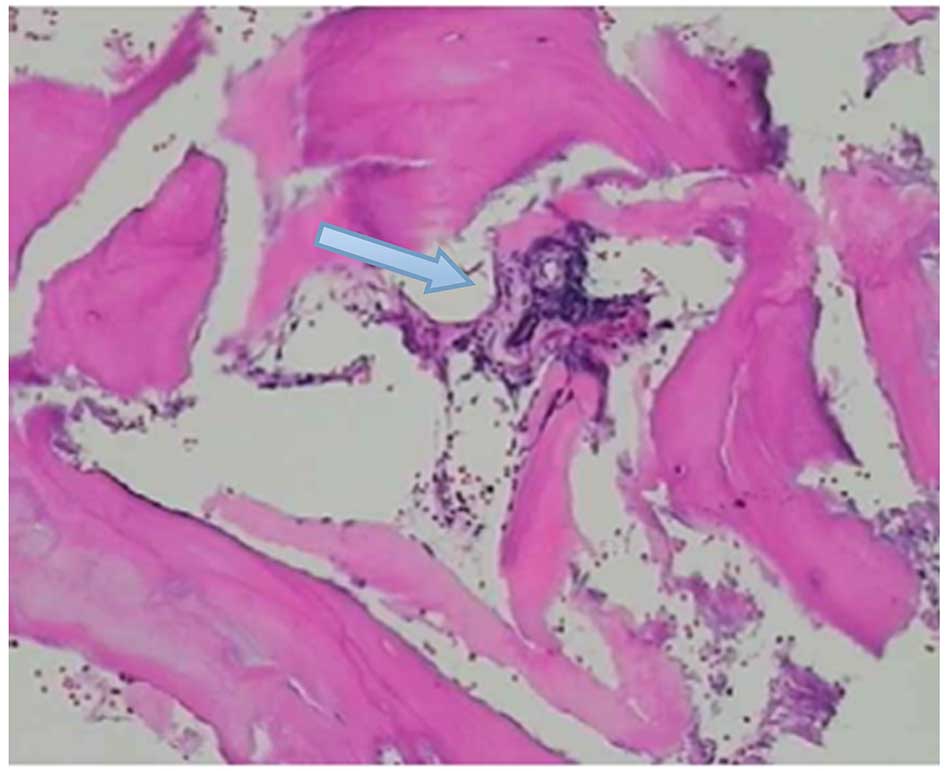
Subsequently, a bone marrow puncture, hematoxylin and eosin
staining and brightfield imaging of these structures were
performed. The medullary cavity was obliterated and the bone marrow
was reported to be suppressed, determined by hematoxylin and eosin
staining using an Olympus BX51 brightfield microscope (Fig. 3). The sequestra were removed and
debridement of the necrotic region was performed via nasal
endoscopy, without antibiotics or any other form of treatment A
month later, intravenous low-strength antibiotic therapy (1 g
cefazolin, every 8 h; Mosinter Group, Ltd., Ningbo, China) was
administered for a week, and the fistula was flushed and drained of
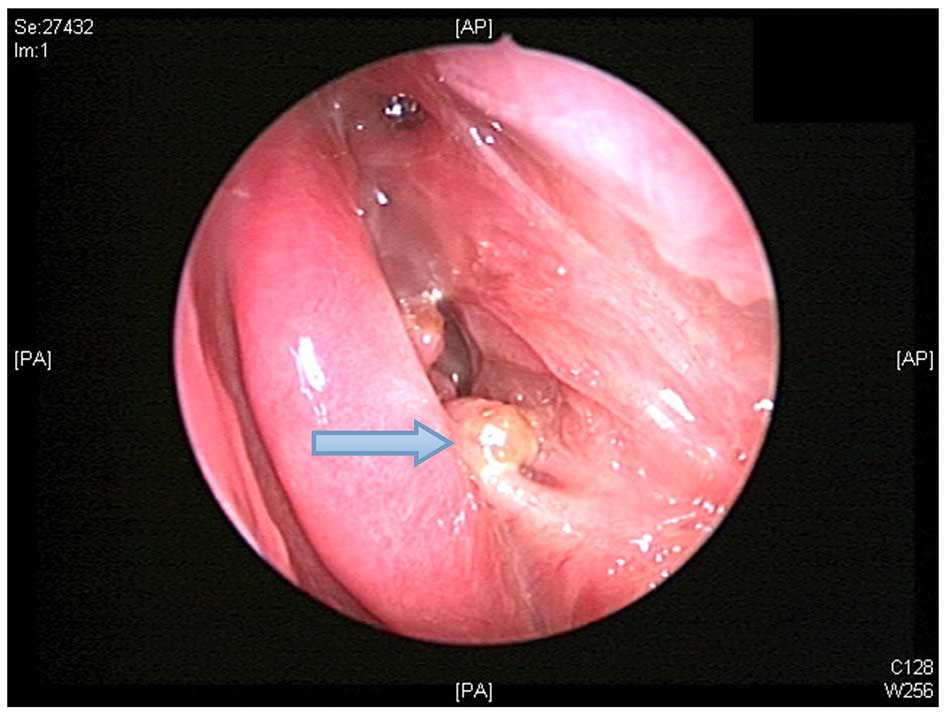
pus via nasal endoscopy every 2 weeks. After a week, the infection
had been successfully treated without the necessity of additional
antibiotic treatment, chronic osteomyelitis was resolved and the
fistula was replaced with fresh granulation after 2 months
(Fig. 4).
Discussion
Osteopetrosis is a rare hereditary disease caused by
an imbalance in bone metabolism, resulting from decreased
osteoclast activity (6). This leads
to a lack of bone remodeling, which can result in a high mortality
rate in children within the first 10 years of their life (6). Early onset osteopetrosis is known as
severe infantile malignant autosomal recessive disease, or
intermediate mild autosomal recessive disease (6). This condition is typically fatal as a
result of anemia with congestive heart failure or sepsis due to
bone overgrowing in the bone marrow space. In adults, the same
disease is known as benign ADO with a late onset, and has a lower
mortality rate (3). At present, the
curative treatment for malignant osteopetrosis is allogenic
hemopoietic stem cell transplantation (4); however, only supportive care is
available for benign osteopetrosis (7). Therefore, symptom management of benign
osteopetrosis is important to increase the patient survival
rates.
The present study reported the case of a patient
diagnosed with benign osteopetrosis at the age of 19 years, with
fractures identified based on presentation and radiology. In benign
osteopetrosis, the most common complications are chronic
osteomyelitis, occurring in 10% of cases involving the mandible
(3), and bone fractures, in 78% of
cases (8). The patient in the
current study presented with chronic purulent nasal discharge in
the left side of the nose, following tooth extraction from the left
side of the mouth 3 years earlier associated with chronic
osteomyelitis. Since the healing process in the bone is slow, it is
difficult to fight and prevent infection in osteopetrosis (1). In ADO, care must be taken when removing
the sequestra, since it is easy to create iatrogenic fractures due
to dense bone, which are difficult to repair once the bone is
fractured (9).
The current approaches of treating osteomyelitis in
osteopetrosis are controversial. Currently, administering a
high-dose of systemic antibiotics with debridement of the necrotic
region alongside HBO therapy is recommended (3). However, as the patient in the current
report presented with insufficient blood supply to the bone due to
osteopetrosis, the use of high-dose antibiotics was not suitable.
Instead, pus from the fistula was flushed and drained via nasal
endoscopy every 2 weeks for 1 month, subsequent to careful removal
of the sequestra and debridement of the necrotic region. Low dose
and intensity antibiotics were administered following debridement,
and the infection was cleared. To the best of our knowledge, this
is the first case report indicating that debridement with low doses
of antibiotics may be effective in the treatment of
osteopetrosis.
Notably, patients with osteopetrosis should be aware
of good dental care and oral hygiene. Decayed teeth should be
endodontically treated and tooth extraction should be avoided, if
possible, on the account of necrosis development. Currently, the
debridement field does not have a clear boundary regarding infected
bones. Care must therefore be taken when removing the necrotic bone
to prevent iatrogenic fractures, which may occur due to
inexperience of the surgeon (9). The
findings of the present study demonstrated that debridement and
drainage of pus from fistulas are important, and possibly a more
effective strategy compared with high-dose antibiotic usage alone
in osteopetrosis.
In conclusion, the complications of osteopetrosis
include bone fractures and chronic osteomyelitis, which are
difficult to treat. In a patient with osteopetrosis, tooth
extraction should be avoided to prevent these complications.
Currently, there is no cure for osteopetrosis and, therefore,
symptom management is important to increase the patient survival
rates. In the present study, it was demonstrated that debridement
and drainage of pus from fistulas may be more effective than
high-dose antibiotic usage in treating osteopetrosis.
References
|
1
|
Smith NH: Albers-Schönberg disease
(osteopetrosis). Report of a case and review of the literature.
Oral Surg Oral Med Oral Pathol. 22:699–710. 1966. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Bollerslev J: Autosomal dominant
osteopetrosis: Bone metabolism and epidemiological, clinical, and
hormonal aspects. Endocr Rev. 10:45–67. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
García CM, García MA, García RG and Gil
FM: Osteomyelitis of the mandible in a patient with osteopetrosis.
Case report and review of the literature. J Maxillofac Oral Surg.
12:94–99. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Juggins KJ, Walton GM and Patel M:
Osteomyelitis complicating osteopetrosis - a case report. Dent
Update. 28:509–511. 2001.PubMed/NCBI
|
|
5
|
Battaglia MA, Drigo P, Laverda AM,
Antolini A, Venuleo M, Miotti A and Pavone L: Juvenile
osteomyelitis and osteopetrosis. A case report. Minerva Stomatol.
40:125–127. 1991.(In Italian). PubMed/NCBI
|
|
6
|
Bollerslev J and Andersen PE Jr:
Radiological, biochemical and hereditary evidence of two types of
autosomal dominant osteopetrosis. Bone. 9:7–13. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Coudert AE, de Vernejoul MC, Muraca M and
Del Fattore A: Osteopetrosis and its relevance for the discovery of
new functions associated with the skeleton. Int J Endocrinol.
3721562015.PubMed/NCBI
|
|
8
|
Bénichou OD, Laredo JD and de Vernejoul
MC: Type II autosomal dominant osteopetrosis (Albers-Schönberg
disease): Clinical and radiological manifestations in 42 patients.
Bone. 26:87–93. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
van Hove RP, de Jong T and Nolte PA:
Autosomal dominant type I osteopetrosis is related with iatrogenic
fractures in arthroplasty. Clin Orthop Surg. 6:484–488. 2014.
View Article : Google Scholar : PubMed/NCBI
|