Introduction
Takayasu's arteritis (TA) is a chronic inflammatory
disease with an unknown origin, which usually affects the aorta and
its primary branches. TA typically occurs prior to the age of 40
years and has a morbidity of 0.6% (1). The aetiopathogenesis of the disease has
not been clarified yet. Infections, autoimmunity and genetic
factors have been examined as aetiologic factors. The treatment of
TA begins with pharmacological control of the acute arteritis in
order to induce clinical remission, followed by treatment of
vascular abnormalities (2). The
arteries suffering from TA are characterized by the proliferation
of intima, focal leukocytic infiltration of the tunica media and
degeneration of the external elastic lamina, leading to vessel wall
thickening, vessel stenosis and occlusion, which are the most
common presenting features (3,4).
However, aneurysmal dilatations occur less frequently (2) and arterial dissection is considerably
rare (5), can produce a wide range
of symptoms and typically presents with severe chest or back pain
(6). Aortic dissection in the common
carotid artery is an unusual pathologic characteristic of TA and
has been rarely reported (7). The
present study describes an atypical case of chronic aortic
dissection in the common carotid artery in a patient with TA.
Case report
A 25-year-old male patient with a history of TA for
10 years, and had received glucocorticoid treatment, was referred
to the General Hospital, Tinjin Medical University (Tianjin, China)
in December 2014 due to chest tightness, shortness of breath and
hemoptysis, without fever, fatigue or headaches. On admission,
clinical examination was unremarkable, aside from increased heart
rate of 115 bpm and elevated blood pressure of 192/100 mmHg. There
was no appreciable discrepancy in the blood pressure between the
arms and no sign of acute limb ischemia, while all the peripheral
pulses of the patient were present. Echocardiography revealed heart
failure, indicated by a decreased ejection fraction and cardiac
index. Lung and abdominal examination findings were normal, and no
abnormality was reported in the computed tomography and magnetic
resonance angiography scans of the cerebrovascular and neurologic
systems. Hematological analyses exhibited an elevated erythrocyte
sedimentation rate (ESR) of 37 mm/h (normal value, 0–15 mm/h) and
serum C-reactive protein level of 7.79 mg/dl (normal value, 0–0.8
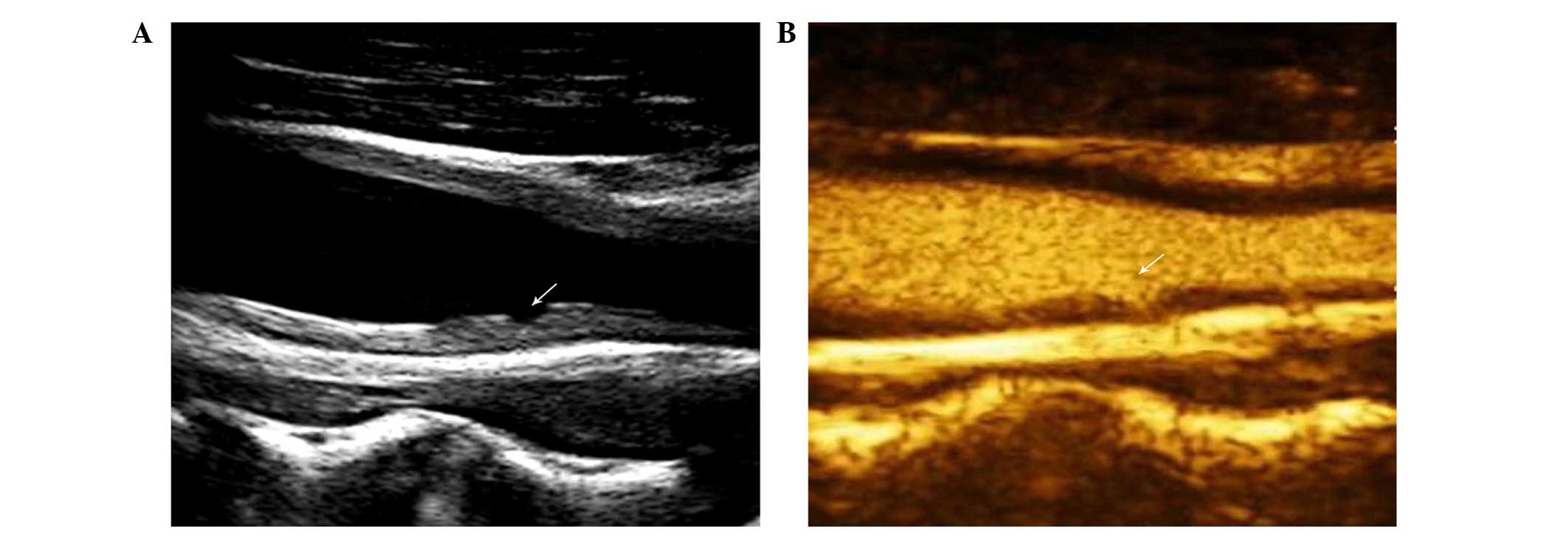
mg/dl). On carotid sonography, the patient's bilateral common
carotid arteries presented mild long-segment, homogeneous,
circumferential wall thickening, as well as a decrease in lumen
diameter (left, 35% stenosis; right, 43% stenosis) and dissection
in the left common carotid artery (Fig.
1A). On color Doppler sonography, the dissected artery was
filled with blood and the peak systolic velocity (PSV) of the
artery was as high as 305 cm/sec (normal range, 91.3±20.7 cm/sec).
Additionally, contrast-enhanced ultrasound examination with sulfur
hexafluoride (1.5 ml; Bracco Group, Milan, Italy) showed uniform
enhancement of contrast agent between the dissection and
intravascular (Fig. 1B). For
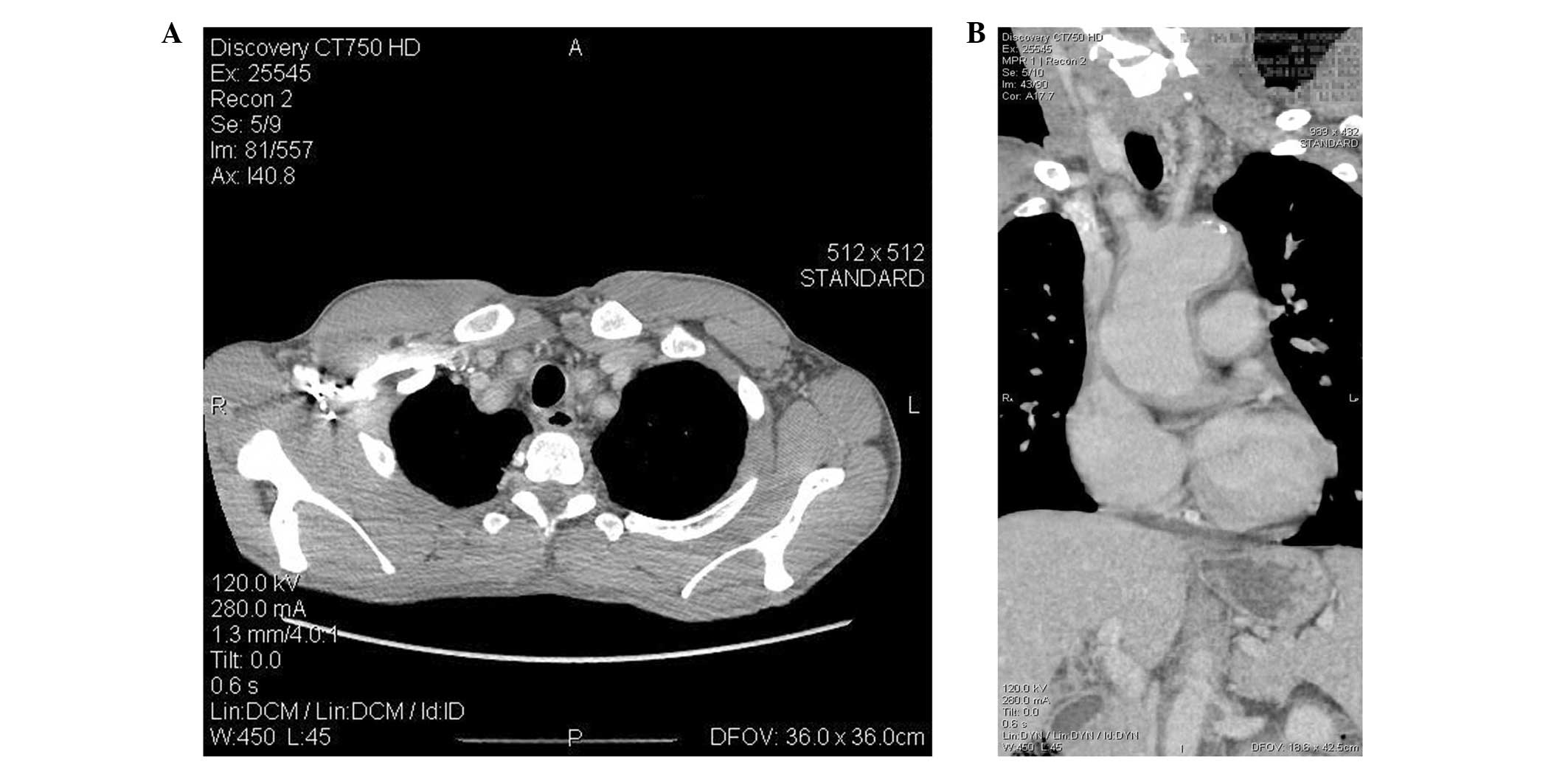
evaluation of the systemic large-artery involvement, computed
tomographic angiography using ioversol contrast agent (20 ml;
Jiangsu Hengrui Medicine Co., Lianyungang, China) was performed and
revealed diffuse wall thickening and stenosis of the left
subclavian artery, common carotid arteries, right brachiocephalic
trunk, diaphragm aorta, abdominal aorta, renal arteries and
superior mesenteric arteries (Fig. 2A
and B). A diagnosis was made, concluding TA involving the left
subclavian artery, common carotid arteries, right brachiocephalic
trunk, diaphragm aorta, abdominal aorta, renal arteries and
superior mesenteric arteries.
The patient was treated with furosemide (20 mg daily
for 5 days followed by dosage adjustments; Zhaohui Pharmaceutical
Co., Ltd., Shanghai, China), nifedipine (20 mg twice daily; Talison
Pharmaceutical Co., Ltd., Zhejiang, China), prednisone (1 mg/kg
daily, gradually reduced; Xinyi Pharmaceutical Co., Ltd., Shanghai,
China) and cyclophosphamide (2 mg daily, gradually reduced; Jin Shi
Pharmaceutical Co., Ltd., Tianjin, China) and no surgical
interventions were performed. The symptoms of chest tightness and
shortness of breath were resolved after three days following
admission and hypertension was controlled. After the patient was
discharged, follow-up once every two months within six months was
performed, followed by 6 monthly visit to hospital. During the
follow-up period, there was no obvious clinical symptoms, and the
patient remained on steroid treatment combined with
immunosuppressive therapy. Written informed patient consent was
obtained in the present study.
Discussion
TA is a rare clinical condition that is
characterized by chronic panarteritis of the aorta and its primary
branches, including the subclavian, common carotid, coronary and
renal arteries, and may result in localized stenoses, vascular
occlusion, dilatation and aneurysm formation (8). TA induces a variety of non-specific
inflammatory systemic signs and symptoms, such as fever, fatigue,
headaches, arthralgia, malaise and weight loss in the chronic phase
(9). In addition, it is
characterized by marked thickening of the aortic wall, with
fibrosis of the intima and adventitia. The thickening of the entire
vessel wall results in stiffness, and this is the primary sign
identified using imaging (10).
In the present study, the patient's clinical
symptoms were not evident, although his ESR was raised; this
indicated inflammatory activity. Chest tightness, shortness of
breath and hemoptysis may also be caused by heart failure. Color
Doppler sonography demonstrated homogeneous, mid-echoic,
circumferential wall thickening of the common carotid artery,
previously described as the macaroni sign', which is a
pathognomonic sign of TA (11). In
addition, an intimal dissection in the common carotid artery was
identified, which is not typically a unique imaging finding of TA.
The patient had a 10-year history of TA, resulting in increased
artery stiffness, which may increase the flow velocity of the
involved artery. Furthermore, chronic inflammation impelled the
lower wall elasticity and thus the intima was vulnerable to
denudation. The involved artery segment showed mild stenosis (35%);
however, the PSV was markedly accelerated (305 cm/s), indicating
severe stenosis. The high PSV observed in the current patient may
have resulted from increased arterial stiffness and decreased
elasticity.
The pathophysiology of dissection remains poorly
understood. A number of studies have suggested that patients with
artery dissection may have a genetically-determined weakness of the
vessel wall, and that environmental factors, such as acute
infection or minor trauma, may serve as triggers (12–14). The
intimal dissection in the common carotid artery may be associated
with chronic inflammation of the vessel wall, vulnerable intima and
hyperdynamic flow. This mechanism of chronic inflammation may
result in a moving intimal flap in the involved artery, which is
another unique character of intimal injury (15). In patients with an advanced stage of
TA, intimal defects may rarely occur as a result of stenosis, which
can cause insufficient blood flow to downstream vessels and
decreased blood flow velocity. Therefore, whether arterial intima
defects are unique to TA requires further study.
In conclusion, as one of the primary causes of
ischemic stroke in young adults, artery dissection requires early
identification and management (15).
Accordingly, regular follow-up is necessary for patients with
chronic TA, and strategies for the prevention of cerebrovascular
ischemia should be carefully designed when an artery dissection is
identified. Artery dissection in the common carotid artery is a
rare phenomena for patients with TA, and the exact mechanism is not
known, but is one of the as one of the primary causes of ischaemic
stroke in young adults. Further research is required in order to
improve the understanding of the underlying pathophysiology of TA
accompanied by common carotid artery dissection, to assess the
long-term outcome, and to provide treatment and prevention
strategies.
References
|
1
|
Sadurska E, Jawniak R, Majewski M and
Czekajska-Chehab E: Takayasu arteritis as a cause of arterial
hypertension. Case report and literature review. Eur J Pediatr.
171:863–869. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Maffei S, Di Renzo M, Bova G, Auteri A and
Pasqui AL: Takayasu's arteritis: A review of the literature. Intern
Emerg Med. 1:105–112. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hotchi M: Pathological studies on Takayasu
arteritis. Heart Vessels Suppl. 7:11–17. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Meini S, De Franco V, Auteri A and
Pieragalli D: Images in cardiovascular medicine. Takayasu's
arteritis: The 'macaroni sign'. Circulation. 114:e5442006.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Khalife T, Alsac JM, Lambert M, Messas E,
Van Huyen JP Duong, Bruneval P, Farahmand P, Julia P and Fabiani
JN: Diagnosis and surgical treatment of a Takayasu disease on an
abdominal aortic dissection. Ann Vasc Surg. 25:556.e1–556.e5. 2011.
View Article : Google Scholar
|
|
6
|
Gaul C, Dietrich W, Friedrich I, Sirch J
and Erbguth FJ: Neurological symptoms in type A aortic dissections.
Stroke. 38:292–297. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Wildburg G, Zahn R, Zander M, Schleiffer T
and Senges J: Takayasu arteritis - a rare differential diagnosis in
aortic dissection. A case report. Z Kardiol. 84:1033–1038.
1995.PubMed/NCBI
|
|
8
|
Direskeneli H, Aydin SZ and Merkel PA:
Assessment of disease activity and progression in Takayasu's
arteritis. Clin Exp Rheumatol. 29(1): Suppl 64. S86–S91.
2011.PubMed/NCBI
|
|
9
|
Vaideeswar P and Deshpande JR: Pathology
of Takayasu arteritis. A brief review. Ann Pediatr Card. 6:52–58.
2013. View Article : Google Scholar
|
|
10
|
Andrews J and Mason JC: Takayasu's
arteritis-recent advances in imaging offer promise. Rheumatology
(Oxford). 46:6–15. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Maeda H, Handa N, Matsumoto M, Hougaku H,
Ogawa S, Oku N, Itoh T, Moriwaki H, Yoneda S and Kimura K: Carotid
lesions detected by B-mode ultrasonography in Takayasu's arteritis:
'Macaroni sign' as an indicator of the disease. Ultrasound Med
Biol. 17:695–701. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Brandt T, Orberk E, Weber R, Werner I,
Busse O, Müller BT, Wigger F, Grau A, Grond-Ginsbach C and Hausser
I: Pathogenesis of cervical artery dissections: Association with
connective tissue abnormalities. Neurology. 57:24–30. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Schievink WI: Spontaneous dissection of
the carotid and vertebral arteries. N Engl J Med. 344:898–906.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Debette S and Leys D: Cervical-artery
dissections: Predisposing factors, diagnosis and outcome. Lancet
Neurol. 8:668–678. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Yang KK and Park JK: Chronic Takayasu
arteritis with a multifocal intimal defect and an intimal flap in
them common carotid artery. J Ultrasound Med. 32:2217–2219. 2013.
View Article : Google Scholar : PubMed/NCBI
|