Introduction
Hypertrophic cardiomyopathy (HCM) is a common
sarcomere gene mutation-caused clinical hereditary heart disease
mainly characterized by autosomal dominant inheritance and
asymmetric hypertrophy in the left ventricle and interventricular
septum (1). HCM can be expressed as
chest tightness, syncope, chest pain, palpitations and dyspnoea
(2). The left ventricular of HCM
patients usually show irregular geometry structure, and the unique
structure and function can lead to the reduced left ventricular and
stroke volume. Pathological manifestations include myocardial
hypertrophy and local fibrosis, and myocardial fiber was disorderly
arranged, resulting in lower left ventricular compliance and
diastolic dysfunction (3). More than
60% of HCM patients showed familial hereditary, while sporadic only
accounted for about 30%. Left ventricular systolic and diastolic
function plays an important role in the diagnosis, treatment and
prognosis evaluation of HCM. Although two-dimensional
echocardiography can provide some information, measurement error is
large, resulting in poor accuracy and repeatability. Accurate and
effective detection of left ventricular diastolic/systolic function
in patients with HCM is important for the treatment and prognosis
of this disease. Real-time three-dimensional ultrasound is a new
imaging technique, compared with the traditional two-dimensional
ultrasound, single-hearted real-time three-dimensional ultrasound
can obtain full volume and seamless images, so as to more
intuitively and accurately evaluate ventricular diastolic/systolic
function of HCM patients, and its repeatability is satisfactory,
and can serve as a complement to two-dimensional ultrasound
(4,5). At present, studies on the relationship
between left ventricular diastolic and systolic dyssynchrony are
still lacking. In the present study, single-cardiac real-time
three-dimensional ultrasonography was performed for all the
patients to investigate the relationship between left ventricular
diastolic and systolic dyssynchrony in HCM to provide references
for the treatment of HCM.
Materials and methods
General information
A total of 52 patients with HCM were selected from
July 2016 to June 2017 to serve as observation group. Inclusion
criteria: i) With clinical manifestations and echocardiography
results in line with HCM diagnostic criteria (6); ii) with stage III diastolic dysfunction
according to the diagnostic criteria established by American
Society of Echocardiography (ASE); and iii) patients signed
informed consent. Exclusion criteria for the study were: i)
Received surgery in recent 6 months; and ii) complicated with
hypertension, pulmonary heart disease and malignant tumor. A total
of 52 cases of healthy people were selected in the same period to
serve as the control group. This study was reviewed and approved by
the Ethics Committee of Jining No. 1 People's Hospital (Jining,
China). Patients provided written informed consent. There was no
significant difference in general information between the two
groups (P>0.05) (Table I).
 | Table I.General information of patients. |
Table I.
General information of patients.
|
| Groups |
|
|
|---|
|
|
|
|
|
|---|
| Items | Observation n=52 | Control n=52 | t/χ2 | P-value |
|---|
| Age (years) | 30–78 | 30–75 |
|
|
| Sex
(male/female) | 29/23 | 27/25 | 0.039 | 0.844 |
| Average age
(years) | 52.76±6.45 | 53.15±7.13 | 0.293 | 0.770 |
| BMI
(kg/m2) | 23.73±2.14 | 24.07±1.86 | 0.865 | 0.389 |
| Cultural level |
|
|
|
|
| Junior high school
and below | 11 (21.16) | 12 (23.08) | 0.168 | 0.919 |
| High school and
secondary school | 21 (40.38) | 19 (36.54) |
|
|
| College and
above | 20 (38.46) | 21 (40.38) |
|
|
Methods
ACUSON SC2000 ultrasonic diagnostic apparatus
(Siemens, Erlangen, GER) was used. 4Z1c full volume probe
frequency: 2.8 MHz. Scanning angle: 90°×90°, Scanning depth: 15–16
cm, volume fraction ≥12 frame/sec. The left lateral position was
taken. Conventional two-dimensional ultrasonography was used to
measure left ventricular ejection fraction (LVEF), left ventricular
end-diastolic volume (LVEDV) and left ventricular end-systolic
volume (LVESV) 3 times, and average values were calculated. ECG was
connected to record the electrocardiogram and collect the
three-dimensional images of three complete cardiac cycles at the
end of the breath. Full volume images of the heart and its
corresponding three-plane cutting images were collected. The data
were analyzed by LVA analysis software, and left ventricle was
divided into 16 segments. Related parameters including LVEDV,
LVESV, LVEF, end-systolic/diastolic sphericity index (ESSI/EDSI),
systolic dyssynchrony index (SDI), diastolic dyssynchrony index
(DDI), dispersion end systole (DISPES), diastolic dyssynchrony
index-late (DDI-late) and dispersion end diastole (DISPED-late)
were obtained. The segment volume-time curve was also obtained.
Evaluation criteria
Patient's diastolic functions were determined
according to the criteria established by ASE: Level I: E/A ratio
<0.8, E peak deceleration time (DT) >200 ms, E/EA ratio ≤8,
slightly damaged diastolic function; Level II: >0.8 E/A ratio
<1.5, >160 DT ≤200 ms, ≥9 E/EA ratio <12, false normal
diastolic function; and Level III: ≥2 E/A ratio, DT >160 ms, ≤13
E/EA ratio, restrictive filling (7).
During real-time three-dimensional ultrasound
examination, the left ventricle was divided into 16 segments, and
the diastolic volume-time curve of those 16 segments was obtained
automatically by software. LVEF, LVEDV, LVESV, EDSI, DDI-late,
DISPED-late, ESSI, SDI and DISPES were determined.
Statistical analysis
The data were processed using SPSS19.0 (SPSS, Inc.,
Chicago, IL, USA) software. Measurement data were expressed as mean
± standard deviation, and processed by t-test. Enumeration data
were expressed as rate, and processed by χ2 test.
Correlation analyses were performed using Pearson's correlation
coefficient analysis. P<0.05 was considered to indicate a
statistically significant difference.
Results
Comparison of results of two- and
three-dimensional ultrasonography
Results of left ventricular function tests in 52
patients with HCM showed that the values of LVEF, LVEDV and LVESV
in two-dimensional ultrasonography were significantly higher than
those in three-dimensional ultrasonography (P<0.05) (Table II).
 | Table II.Comparison of results of
two-dimensional and three-dimensional ultrasonography. |
Table II.
Comparison of results of
two-dimensional and three-dimensional ultrasonography.
| Methods | Cases | LVEF (%) | LVEDV (ml) | LVESV (ml) |
|---|
| Two-dimensional
ultrasonography | 52 | 59.52±3.42 | 104.97±3.84 | 50.76±3.46 |
| Three-dimensional
ultrasonography | 52 | 53.78±3.56 | 99.13±3.86 | 43.87±3.27 |
| t-test |
| 8.385 | 7.735 | 10.436 |
| P-value |
| <0.001 | <0.001 | <0.001 |
HCM morphological characteristics
Wall thickness of 16 segments of the two groups was
measured and results showed that the hypertrophy of HCM was
irregular, and left ventricular hypertrophy could occur in any
part, such as anterior wall apex, lateral wall apex and left
ventricular apex hypertrophy. In 52 HCM patients, 43 cases (82.69%)
were unsymmetrical hypertrophy of interventricular septum, 6
(11.54%) were apical hypertrophy and 3 were homogeneous hypertrophy
(5.77%).
Comparison of cardiac function, left
ventricular diastolic function, left ventricular systolic function,
diastolic volume-time curve of 16 segments between two groups
LVEF of observation was significantly lower than
that of control group, while LVEDV, LVESV, E/A and E/Ea were
significantly higher in observation than in control group
(P<0.05) (Table III). EDSI,
DDI-late and DISPED-late were significantly higher in the
observation than in the control group (P<0.05) (Table IV). ESSI, SDI and DISPES in
observation were significantly higher than those in the control
group (P<0.05) (Table V). The
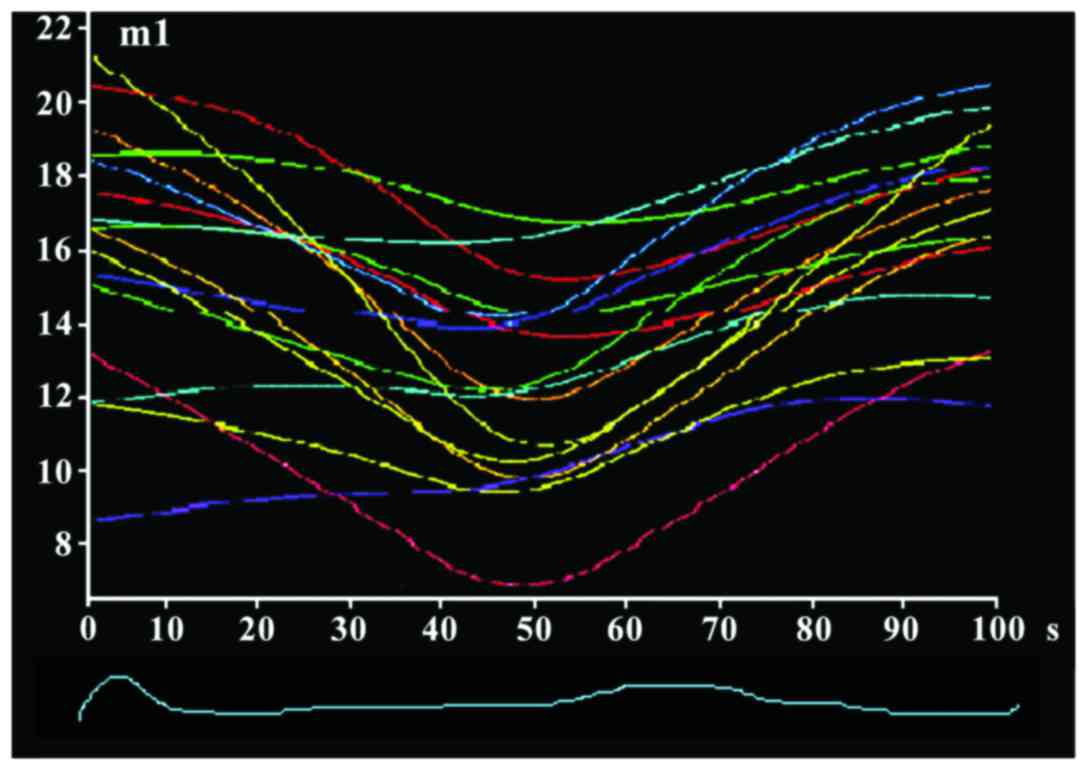
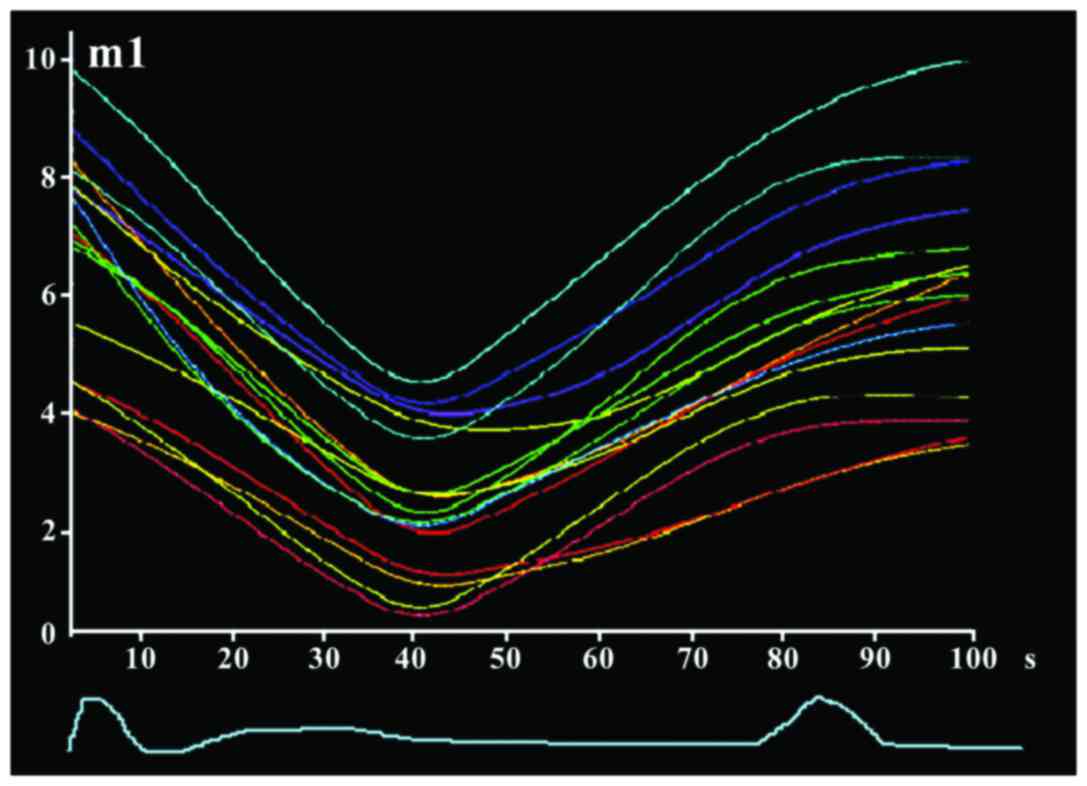
16-segment time-volume curve of observation group was disordered
without synchronization (Fig. 1),
while the curve of control group was regular and smooth with
synchronization (Fig. 2).
 | Table III.Comparison of cardiac function between
the two groups of patients. |
Table III.
Comparison of cardiac function between
the two groups of patients.
| Groups | Cases | LVEF (%) | LVEDV (ml) | LVESV (ml) | E/A | E/Ea |
|---|
| Control | 52 | 62.73±3.68 | 91.97±3.64 | 36.76±3.18 | 1.35±0.23 | 7.35±1.16 |
| Observation | 52 | 53.78±3.56 | 99.13±3.86 | 43.87±3.27 | 2.87±0.35 | 13.87±1.23 |
| t-test |
| 12.605 | 9.732 | 11.240 | 26.172 | 27.809 |
| P-value |
| <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
 | Table IV.Comparison of left ventricular
diastolic function between two groups (mean ± SD). |
Table IV.
Comparison of left ventricular
diastolic function between two groups (mean ± SD).
| Groups | Cases | EDSI | DDI-late | DISPED-late |
|---|
| Control | 52 | 41.52±3.19 | 5.18±0.78 | 21.25±1.16 |
| Observation | 52 | 50.64±3.73 | 7.89±0.95 | 27.64±1.58 |
| t-test |
| 13.399 | 15.898 | 23.508 |
| P-value |
| <0.001 | <0.001 | <0.001 |
 | Table V.Comparison of left ventricular
systolic function of two groups of patients (mean ± SD). |
Table V.
Comparison of left ventricular
systolic function of two groups of patients (mean ± SD).
| Groups | Cases | ESSI | SDI | DISPES |
|---|
| Control | 52 | 35.54±3.08 | 5.36±1.29 | 16.78±3.09 |
| Observation | 52 | 41.68±3.27 | 8.89±1.64 | 32.82±3.53 |
| t-test |
| 9.856 | 12.200 | 24.655 |
| P-value |
| <0.001 | <0.001 | <0.001 |
Correlation analysis between left
ventricular diastolic and systolic dyssynchrony
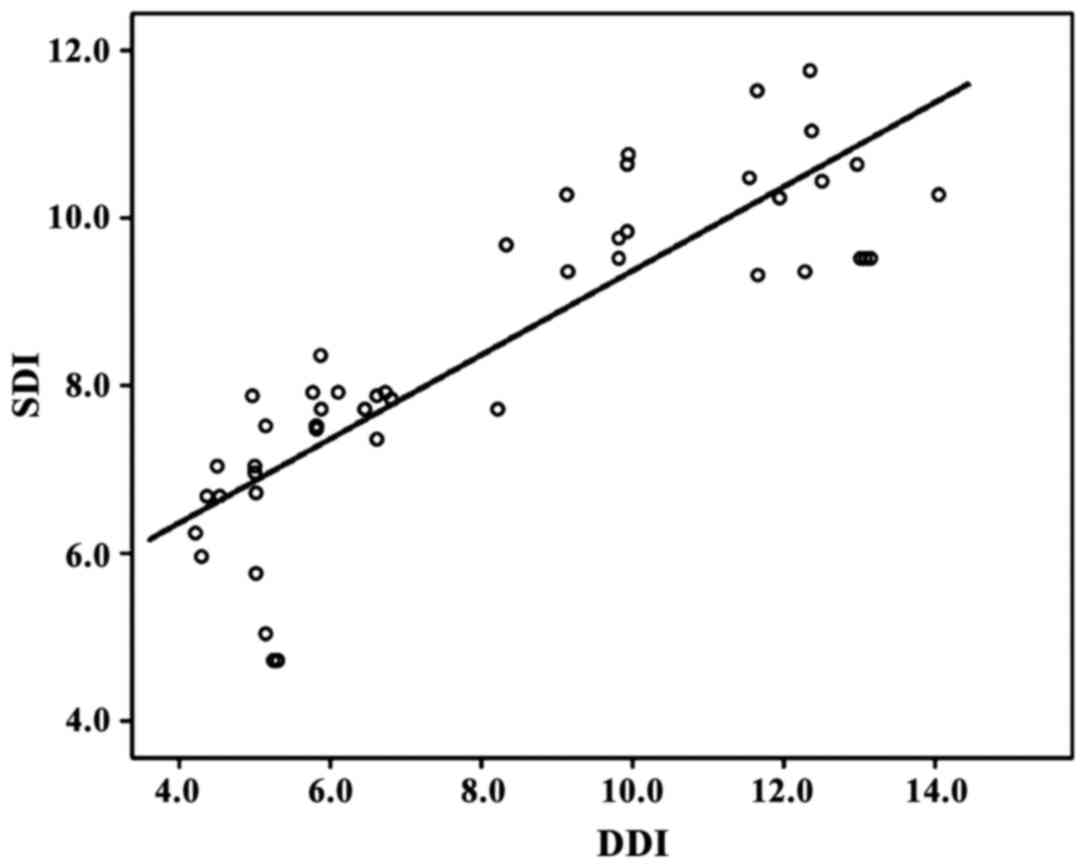
Pearson's correlation coefficient analysis showed
that SDI and DDI were positively correlated (r=0.413, P<0.05)
(Fig. 3).
Discussion
HCM is a hereditary cardiomyopathy, which is caused
by mutations in the gene encoding the sarcoma structural protein
gene. HCM is mainly expressed as the left ventricular wall
asymmetric thickening, and the prevalence rate is approximately
0.2% (8). The most important
pathophysiological change of HCM is the left ventricular diastolic
dysfunction, resulting in increased left ventricular filling
pressure, then blood will be transferred through the left atrial to
pulmonary vein to cause high pulmonary blood flow. Patients usually
show symptoms such as shortness of breath and chest tightness and
severe symptoms can cause sudden death. Cardiac death and malignant
arrhythmia and other events are also common, seriously affecting
the quality of life of patients (9,10). HCM
is mainly affected by genetic factors, and a variety of internal
and external environmental factors can also contribute to the
phenotypes (11). The pathogenesis
of diastolic dysfunction of HCM patients is complex with the
involvement of myocardial fibrosis, ventricular wall diastolic
dyssynchrony, energy metabolism, decreased ventricular wall
compliance and ventricular wall hypertrophy and other factors
(12).
In the 1970s, three-dimensional imaging of the heart
was first applied, and three-dimensional ultrasound imaging was
developed from static to dynamic, and even in real time, and was
widely used clinically (13). The
results of the present study showed that LVEF in observation was
significantly lower than that in control group, while LVEDV, LVESV,
E/A and E/Ea were significantly higher in observation than those in
the control group (P<0.05). This is because the cardiac
hypertrophy, myocardial fiber abnormalities and low ventricular
compliance occured in HCM patients, in addition, ventricular wall
of HCM patients is harder than that of normal people, and wall
tension is also higer, leading to the increased left ventricular
load, resulting in left ventricular enlargement. Thus, LVEDV and
LVESV of HCM patients are significantly higher than those of normal
people (14). Myocardial compliance
and relaxation ability of HCM patients were reduced, leading to the
limited early ventricular diastolic filling and increased left
atrial pressure, and thus E/A and E/Ea ratio were increased
(15).
Compared with two-dimensional, real-time
three-dimensional ultrasound can more precisely and accurately
reflect the local changes in the heart, it can also solve the
over-reliance of two-dimensional ultrasound on geometric model
assumptions (16). Single-cardiac
real-time three-dimensional ultrasonography can be a perfect
solution for the problem of splicing in multi-cardiac cycles
three-dimensional ultrasound, it also offers the time needed for
image acquisition and data analysis, and the left ventricular
volume can also be directly evaluated (17). Results of this study showed that
EDSI, DDI-late and DISPED-late were significantly higher in
observation than in control group, and ESSI, SDI and DISPES in
observation were also significantly higher than those in control
group (P<0.05). Cardiac activity of the normal is expressed by
the orderly systolic and diastolic activities of atria and
ventricles. Real-time three-dimensional echocardiography showed
that the left ventricular 16 segments of the control reached the
minimum systolic volume at the same time point of the cardiac
cycle, and the volume-time curve showed a smooth trend and the
synchronization was good, while mechanical delay was observed in
observation group with the most important manifestation of
ventricular systolic and diastolic dyssynchrony, therefore, the
time points of the 16 segments reached the minimum systolic volume
will be different, so the volume-time curve showed irregularity and
loss of synchronization. DDI was obtained from the analysis using
real-time three-dimensional ultrasonic software to effectively
evaluate left ventricular diastolic function. Increased DDI
indicate the diastolic dysfunction in HCM patients, while increased
SDI is associated with varying degrees of systolic dysfunction
(18).
Pearson's correlation coefficient analysis showed
that SDI was positively correlated with DDI (r=0.413, P<0.05).
This is because HCM patients usually had coexistence of left
ventricular diastolic and systolic dysfunction. With the progress
of HCM disease, myocardial fibrosis will gradually occur, thus
affecting the normal metabolism of myocardial energy, increased
diastolic dysfunction and DDI, so left ventricular diastolic
dyssynchrony will happen, which in turn leads to increased SDI
(19,20). SDI will increase with the increase in
DDI, and the two are positive correlated, indicating the coexisting
of left ventricular diastolic and systolic dyssynchrony in HCM
patients.
Collectively, the use of single-cardiac real-time
three-dimensional ultrasound examination of HCM patients can
effectively shorten the image acquisition and analysis time. This
technique can be used to intuitively and accurately reflect the
left ventricular diastolic and systolic dyssynchrony in HCM
patients to assist clinical diagnosis and treatment. This study is
limited by the small sample size, future studies with larger sample
size are needed to confirm the conclusions in the present
study.
Acknowledgements
Not applicable.
Funding
No funding was received.
Available of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
BX drafted this manuscript. BX and AC were mainly
devoted on collecting and interpreting the data. XH revised it
critically for important intellectual content. WS and XH were
responsible for the conception and design of the study. All authors
read and approved the final manuscript.
Consent for publication
Τhis study was reviewed and approved by the Ethics
Committee of Jining No. 1 People's Hospital (Jining, China).
Patients provided written informed consent.
Competing interests
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Semsarian C, Ingles J, Maron MS and Maron
BJ: New perspectives on the prevalence of hypertrophic
cardiomyopathy. J Am Coll Cardiol. 65:1249–1254. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Maron BJ, Rowin EJ, Casey SA, Link MS,
Lesser JR, Chan RH, Garberich RF, Udelson JE and Maron MS:
Hypertrophic cardiomyopathy in adulthood associated with low
cardiovascular mortality with contemporary management strategies. J
Am Coll Cardiol. 65:1915–1928. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Elliott PM, Anastasakis A, Borger MA,
Borggrefe M, Cecchi F, Charron P, Hagege AA, Lafont A, Limongelli
G, Mahrholdt H, et al: Authors/Task Force members: 2014 ESC
Guidelines on diagnosis and management of hypertrophic
cardiomyopathy: The Task Force for the diagnosis and management of
hypertrophic cardiomyopathy of the European Society of Cardiology
(ESC). Eur Heart J. 35:2733–2779. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Wasilewska M, Gardziejczyk W and
Gierasimiuk P: Evaluation of skid resistance using CTM, DFT and
SRT-3 devices. Transportat Res Proced. 14:3050–3059. 2016.
View Article : Google Scholar
|
|
5
|
Cai Q and Ahmad M: Left ventricular
dyssynchrony by three-dimensional echocardiography: Current
understanding and potential future clinical applications.
Echocardiography. 32:1299–1306. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kalsi KK, Smolenski RT, Pritchard RD,
Khaghani A, Seymour AM and Yacoub MH: Energetics and function of
the failing human heart with dilated or hypertrophic
cardiomyopathy. Eur J Clin Invest. 29:469–477. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Dubourg O, Mansencal N and Charron P:
Recommendations for the diagnosis and management of hypertrophic
cardiomyopathy in 2014. Arch Cardiovasc Dis. 108:151–155. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Alfares AA, Kelly MA, McDermott G, Funke
BH, Lebo MS, Baxter SB, Shen J, McLaughlin HM, Clark EH, Babb LJ,
et al: CORRIGENDUM: Results of clinical genetic testing of 2,912
probands with hypertrophic cardiomyopathy: Expanded panels offer
limited additional sensitivity. Genet Med. 17:3192015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Cardim N, Galderisi M, Edvardsen T, Plein
S, Popescu BA, D'Andrea A, Bruder O, Cosyns B, Davin L, Donal E, et
al: Role of multimodality cardiac imaging in the management of
patients with hypertrophic cardiomyopathy: An expert consensus of
the European Association of Cardiovascular Imaging endorsed by the
Saudi Heart Association. Eur Heart J Cardiovasc Imaging.
16:2802015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Hensley N, Dietrich J, Nyhan D, Mitter N,
Yee MS and Brady M: Hypertrophic cardiomyopathy: A review. Anesth
Analg. 120:554–569. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Nomura A, Konno T, Fujita T, Tanaka Y,
Nagata Y, Tsuda T, Hodatsu A, Sakata K, Nakamura H, Kawashiri MA,
et al: Fragmented QRS predicts heart failure progression in
patients with hypertrophic cardiomyopathy. Circ J. 79:136–143.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ho CY, Lakdawala NK, Cirino AL, Lipshultz
SE, Sparks E, Abbasi SA, Kwong RY, Antman EM, Semsarian C, González
A, et al: Diltiazem treatment for pre-clinical hypertrophic
cardiomyopathy sarcomere mutation carriers: A pilot randomized
trial to modify disease expression. JACC Heart Fail. 3:180–188.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Zhu M, Ashraf M, Zhang Z, Streiff C,
Shimada E, Kimura S, Schaller T, Song X and Sahn DJ: Real time
three-dimensional echocardiographic evaluations of fetal left
ventricular stroke volume, mass, and myocardial strain: In vitro
and in vivo experimental study. Echocardiography. 32:1697–1706.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Maron BJ, Casey SA, Chan RH, Garberich RF,
Rowin EJ and Maron MS: Independent assessment of the European
Society of Cardiology sudden death risk model for hypertrophic
cardiomyopathy. Am J Cardiol. 116:757–764. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Patel P, Dhillon A, Popovic ZB, Smedira
NG, Rizzo J, Thamilarasan M, Agler D, Lytle BW, Lever HM and Desai
MY: Left ventricular outflow tract obstruction in hypertrophic
cardiomyopathy patients without severe septal hypertrophy:
Implications of mitral valve and papillary muscle abnormalities
assessed using cardiac magnetic resonance and echocardiography.
Circ Cardiovasc Imaging. 8:e0031322015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Lu KJ, Chen JX, Profitis K, Kearney LG,
DeSilva D, Smith G, Ord M, Harberts S, Calafiore P, Jones E, et al:
Right ventricular global longitudinal strain is an independent
predictor of right ventricular function: A multimodality study of
cardiac magnetic resonance imaging, real time three-dimensional
echocardiography and speckle tracking echocardiography.
Echocardiography. 32:966–974. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Elsayed M, Hsiung MC, Meggo-Quiroz LD,
Elguindy M, Uygur B, Tandon R, Guvenc T, Keser N, Vural MG, Bulur
S, et al: Incremental value of live/real time three-dimensional
over two-dimensional transesophageal echocardiography in the
assessment of atrial septal pouch. Echocardiography. 32:1858–1867.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Wada Y, Aiba T, Matsuyama TA, Nakajima I,
Ishibashi K, Miyamoto K, Yamada Y, Okamura H, Noda T, Satomi K, et
al: Clinical and pathological impact of tissue fibrosis on lethal
arrhythmic events in hypertrophic cardiomyopathy patients with
impaired systolic function. Circ J. 79:1733–1741. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Zhao B, Wang S, Chen J, Ji Y, Wang J, Tian
X and Zhi G: Echocardiographic characterization of hypertrophic
cardiomyopathy in Chinese patients with myosin-binding protein C3
mutations. Exp Ther Med. 13:995–1002. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Parthiban A, Li L, Kindel SJ, Shirali G,
Roessner B, Marshall J, Schuster A, Klas B, Danford DA and Kutty S:
Mechanical dyssynchrony and abnormal regional strain promote
erroneous measurement of systolic function in pediatric heart
transplantation. J Am Soc Echocardiogr. 28:1161–1170. 2015.
View Article : Google Scholar : PubMed/NCBI
|