Introduction
With the progress of socialization in China, the
aging of population has been increasingly prominent. The elderly
population is often accompanied with various medical diseases,
especially in middle-aged women who are often accompanied with
osteoporosis, so the slight trauma can lead to femoral
intertrochanteric fracture easily (1). Intertrochanteric fractures in senile
patients are mostly unstable fractures accompanied with
osteoporosis, while the fractures are often comminuted, involving
the large and small intertrochanteric fractures. Mostly the femoral
distance was destroyed, resulting in the loss of its mechanical
support, and even involving the proximal femoral medullary cavity.
At present, surgery is the preferred treatment means for the
disease to avoid venous thrombosis, malnutrition, bed sores and
joint stiffness, caused by long-term immobilization (2). Although there are many surgical methods
for the disease, such as internal fixation with multi-Kirschner
wires, with Richard nail and Gamma nail and with dynamic hip screw
(DHS) locking screw (3), they will
cause larger trauma, it is hard for patients, especially the senile
patients, to get out of bed early after operation, and
postoperative complications, such as severe pain, occur, affecting
the prognosis of patients (4).
Proximal femur locking plate (PFLP) is widely used
for the treatment of proximal femoral fractures in recent years,
which belongs to the extramedullary fixation system (5). The PFLP is reasonably designed and
anatomically matches with the proximal epiphysis of the femur. It
is able to fix the coronal plane fracture of the large as well as
small intertrochanteric fracture, meeting the demands of
intertrochanteric comminuted fracture fixation internally.
Artificial femoral head replacement is a relative
simple operation with modeled procedures, which causes less trauma,
and patients can get out of bed early after operation thus reducing
the complications caused by long-term immobilization. Besides,
patients could begin early hip exercise and walk with weight to
quickly restore hip function to the preoperative state. Moreover,
this operation could help to avoid many complications caused by
internal fixation (6). Therefore, it
is recommended as one of the preferred methods in the treatment of
senile femoral intertrochanteric fracture (7). In this study, the experience of
performing PFLP fixation as well as artificial femoral head
replacement for the senile femoral intertrochanteric fracture in
recent years was summarized and its clinical application effect is
reported.
Patients and methods
General data
Eighty patients with femoral intertrochanteric
fractures who received artificial femoral head replacement under
intraspinal anesthesia in Zhangjiagang Hospital from May 2014 to
December 2016 were selected. They were aged 60–85 years, and signed
the informed consent for enrollment, operation and anesthesia. At
the same time, this study was discussed and approved by the Medical
Ethics Committee of Zhangjiagang Hospital of Traditional Chinese
Medicine Affiliated to Nanjing University of Chinese Medicine
(Zhangjiagang, China). Patients complicated with severe
cardiopulmonary insufficiency, severe liver and kidney function
deficiency, coagulation disorders, spinal deformity, malignant
tumors, fractures in other parts of lower limbs or mental illness,
or who used analgesia device after operation or refused to be
enrolled were excluded. Patients enrolled were divided into two
groups, the observation group (n=40) and the control group (n=40),
using the random number method. In the observation group, there
were 20 males and 20 females aged 60–85 years with an average of
73.5±1.3 years; in terms of injured part, there were 16 cases on
the left and 24 cases on the right. Based on Evans-Jensen
classification (8), 2 were in type
I, 6 in type II, 15 in type III, 16 in type IV and 1 in type V. In
the control group, there were 21 males and 19 females aged 60–85
years with an average of 73.6±1.3 years; in terms of injured part,
there were 15 cases on the left and 25 cases on the right. Based on
Evans-Jensen classification, 3 were in type I, 3 in type II, 16 in
type III and 18 in type IV. The differences in sex, age and injured
part and Evans-Jensen classification between the two groups were
not statistically significant (P>0.05).
Methods
The observation group was treated with artificial
femoral head replacement. The incision was entered using the
Smith-Petersen method. All patients received the combined
spinal-epidural anesthesia in a lateral position. A 8 cm-long
incision was made in the greater trochanter of femur till 5 cm
below the greater trochanter of femur, followed by blunt separation
to fully expose the fracture site in greater trochanter of femur.
The fracture re-displacement was avoided. The femoral head and
labrum acetabulare were exposed, the lateral iliac artery was
ligated and then the joint capsule was cut. The femoral neck was
broken from 1.5 cm in the femoral lesser trochanter. The femoral
head was removed, and the bone marrow was enlarged. The femoral
prosthesis was placed into the fracture site of femur, and bound
with wire after determining the location and stability. Then the
prosthesis handle was removed, and the medullary cavity was filled
with the bone cement. Then the prosthesis handle was placed once
again at 15° forward; the excess bone cement was cleaned up. The
control group was treated with PFLP fixation. First, a 20 cm-long
longitudinal incision was made on the greater trochanter of femur,
followed by blunt separation to expose the femoral membrane. Under
the C-arm, the Kirschner wire was placed at approximately 5 cm
under the greater trochanter. The Kirschner wire at an appropriate
position under the femoral neck was used as the guide pin, and the
cancellous bone screw was placed and the locking screws were
screwed on.
Observational indexes
The elderly patients were all followed up for 12
months, and the relevant data were obtained through calling them or
their guardians combined with outpatient follow-up. The relevant
situations of operation, 10 m walking speed and 5-time sit-stand
time at 3, 6 and 12 months after operation, Harris hip score before
and after operation, pain at different time-points before and after
operation, total hospitalization time, time of walking on crutches
and walking without crutches, complications and 36-item short-form
health survey questionnaire (SF-12) scores before and after
intervention were compared between the two groups.
Evaluation criteria
The length of lower limbs was measured using the
tape from iliac spine to inferior margin of medial malleolus. Those
with difference in length of the lower limbs greater than 1.5 cm
were diagnosed as length discrepancy of both lower limbs; the 10 m
walking speed was based on the measurement of 10 m plane linear
distance using the stopwatch, and the 5-time sit-stand time was
based on the measurement using the knee-high back bench and
stopwatch. The pain score was measured using the visual analogue
scale (VAS); the highest score (10 points) indicated severe pain,
while the lowest score (0 point) indicated no pain; the higher the
score was, the more severe the pain was. Harris hip function score
(0–100 points): >90 points indicated excellent and good, while
>70 points indicated the hip joint dysfunction. SF-12 score
(0–50 points): the patient's physical function and psychological
function were scored at the same time; the higher the score was,
the better the life quality was.
Statistical analysis
Statistical Product and Service Solutions (SPSS)
21.0 (IBM Corp., Armonk, NY, USA) was used for the statistical
analysis. All measurement data in this study are presented as mean
± standard deviation, and all enumeration data are presented as
percentage. t-test was used for the comparison of measurement data,
while the Chi-square test was used for the comparison of
enumeration data. One-way ANOVA test followed by post hoc test
(Least Significant Difference) was performed for multiple
comparisons between the groups. P<0.05 was considered to
indicate a statistically significant difference.
Results
Comparison of relevant situations of
operation between the two groups
In the observation group, the operation time was
significantly shorter than that in the control group, the
intraoperative bleeding was less than that in the control group
(P<0.05), and the postoperative indwelling drainage time was
significantly shorter than that in the control group (P<0.05)
(Table I).
 | Table I.Comparison of relevant situations of
operation between the two groups (mean ± standard deviation). |
Table I.
Comparison of relevant situations of
operation between the two groups (mean ± standard deviation).
|
| Operation time
(min) | Intraoperative
bleeding (ml) | Postoperative
drainage time (days) |
|---|
| Observation
group | 45.6±2.8 | 103.5±10.5 | 2.1±0.2 |
| Control group | 63.2±3.9 | 256.8±23.9 | 3.3±0.3 |
| t value | 23.185 | 37.141 | 21.049 |
| P-value | <0.001 | <0.001 | <0.001 |
Comparison of 10 m walking speed and
5-time sit-stand time at 3, 6 and 12 months after operation between
the two groups
At 3 months after operation, the 10 m walking speed
in the observation group was significantly higher than that in the
control group (P<0.05), and the 5-time sit-stand time was
shorter than that in the control group (P<0.05) (Table II).
 | Table II.Comparison of 10 m walking speed and
5-time sit-stand time at 3, 6 and 12 months after operation between
the two groups (mean ± standard deviation). |
Table II.
Comparison of 10 m walking speed and
5-time sit-stand time at 3, 6 and 12 months after operation between
the two groups (mean ± standard deviation).
|
| 3 months | 6 months | 12 months |
|---|
|
|
|
|
|
|---|
|
| 10 m walking speed
(m/sec) | 5-time sit-stand time
(sec) | 10 m walking speed
(m/sec) | 5-time sit-stand time
(sec) | 10 m walking speed
(m/sec) | 5-time sit-stand time
(sec) |
|---|
| Observation
group | 1.6±0.2 | 56.6±11.0 | 2.1±0.3 | 45.2±5.7 | 2.7±0.5 | 40.5±5.3 |
| Control group | 0.7±0.1 | 73.0±13.1 | 1.6±0.2 | 53.1±4.5 | 2.3±0.3 | 48.6±3.1 |
| t value | 25.456 | 6.064 | 20.126 | 7.82 | 23.32 | 5.69 |
| P-value | <0.001 | <0.001 | 0.0023 | 0.0016 | 0.015 | 0.025 |
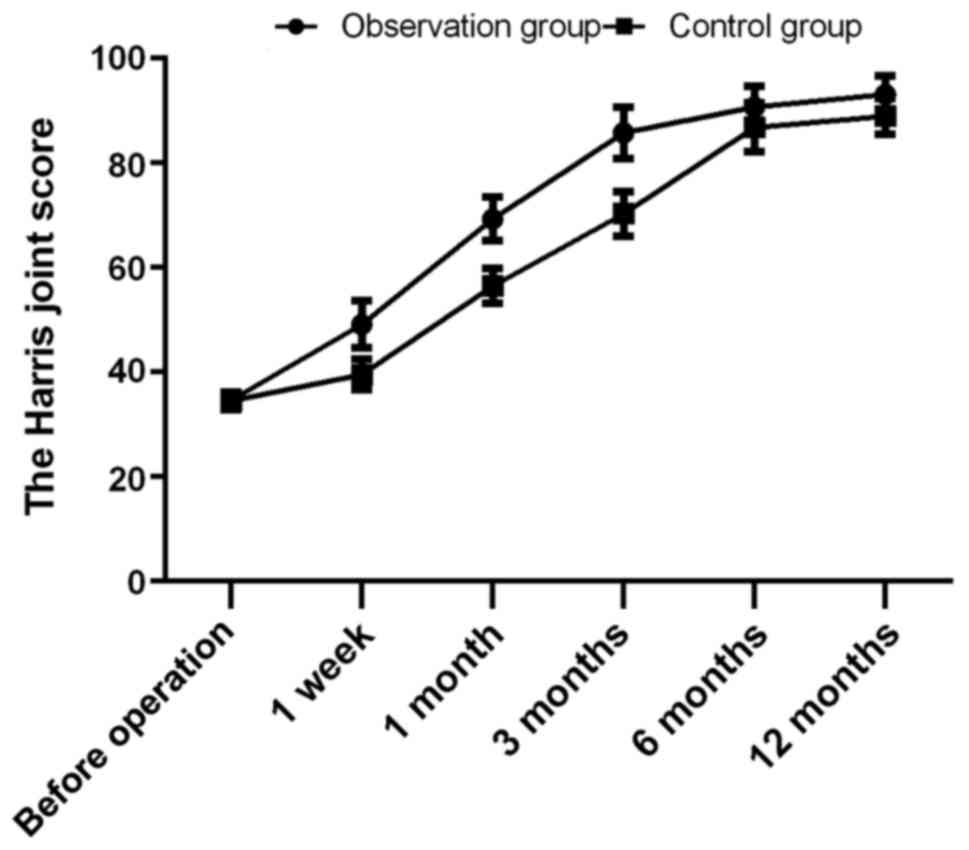
Comparison of Harris hip scores before
and after operation between the two groups
The Harris hip scores of the two groups before
operation were 35.6±2.1 and 35.5±2.1 points, and there was no
statistically significant difference (t=0.000; P>0.05). At 1
week, 1 month, 3, 6 and 12 months after operation, the Harris hip
scores of the observation group were 49.6±3.1, 68.9±6.5, 85.6±7.2,
90.7±5.3 and 93.1±2.3 points, respectively, which were superior to
those of the control group in the same period (40.3±2.6, 56.1±4.0,
70.3±5.0, 86.8±3.5 and 88.9±2.6 points) (t=14.537, 10.607, 11.039,
9.835, 12.117; P<0.05) (Fig.
1).
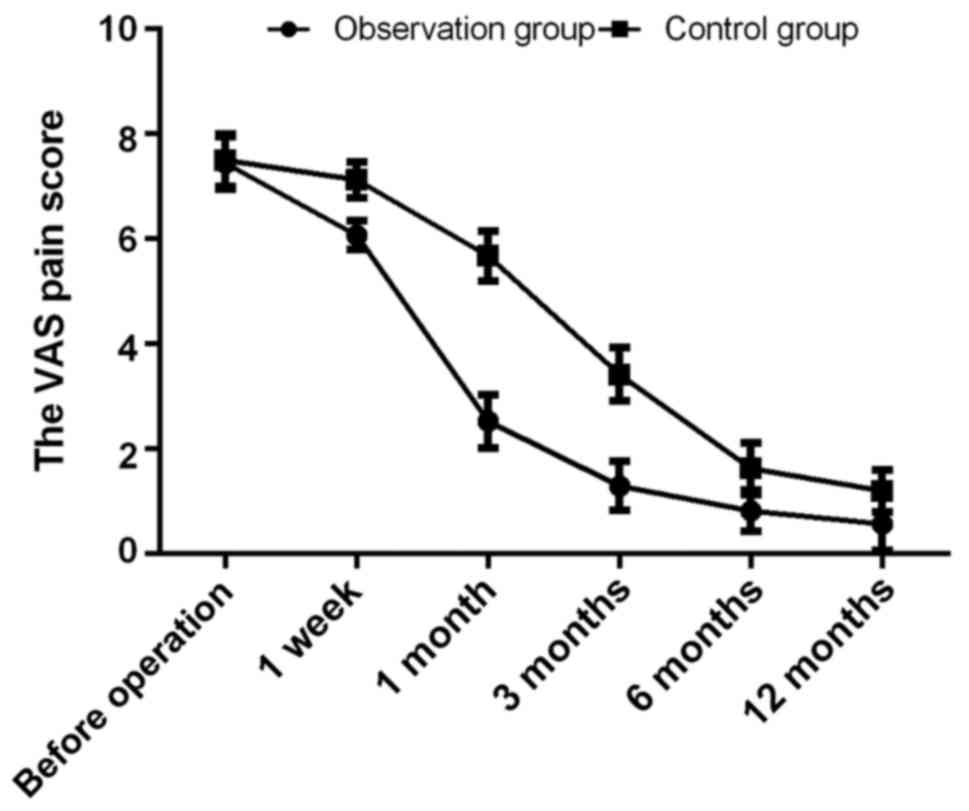
Comparison of VAS pain scores at
different time-points before and after operation
The VAS pain scores of the two groups before
operation were 7.5±0.3 and 7.5±0.4 points, and there was no
statistically significant difference (t=0.213; P>0.05). At 1
week, 1 month, 3, 6 and 12 months after operation, the VAS pain
scores of the observation group were 6.1±0.2, 2.5±0.2, 1.3±0.1,
0.8±0.4 and 0.5±0.2 points, respectively, which were superior to
those of the control group in the same period (7.0±0.2, 5.6±0.3,
3.5±0.2, 1.6±0.3 and 1.2±0.2 points) (t=20.125, 54.378, 44.000,
32.236, 25.560; P<0.05) (Fig.
2).
Comparison of total hospitalization
time and time of walking on crutches and walking without crutches
between the two groups
The total hospitalization time in the observation
group was shorter than that in the control group, and the time of
walking on crutches and walking without crutches was earlier than
that in the control group (P<0.05) (Table III).
 | Table III.Comparison of total hospitalization
time and time of walking on crutches and walking without crutches
between the two groups (days, mean ± standard deviation). |
Table III.
Comparison of total hospitalization
time and time of walking on crutches and walking without crutches
between the two groups (days, mean ± standard deviation).
|
| Total hospitalization
time | Time of walking on
crutches | Time of walking
without crutches |
|---|
| Observation
group | 14.6±0.8 | 10.2±0.3 | 96.3±8.5 |
| Control group | 16.5±1.1 | 15.6±0.9 | 158.6±11.4 |
| t value | 14.572 | 36.000 | 27.709 |
| P-value | <0.001 | <0.001 | <0.001 |
Comparison of complications between
the two groups
The proportions of postoperative chronic pain,
failed operation (including prosthesis or internal fixation loose
and nonunion) in the observation group were significantly lower
than those in the control group (P<0.05) (Table IV).
 | Table IV.Comparison of complications between
the two groups (n, %). |
Table IV.
Comparison of complications between
the two groups (n, %).
|
| Postoperative chronic
pain | Failure of
operation | Total incidence
rate |
|---|
| Observation
group | 1 | 2 | 3 (7.5%) |
| Control group | 3 | 8 | 11 (27.5%) |
| χ2 |
|
| 4.242 |
| P-value |
|
| 0.039 |
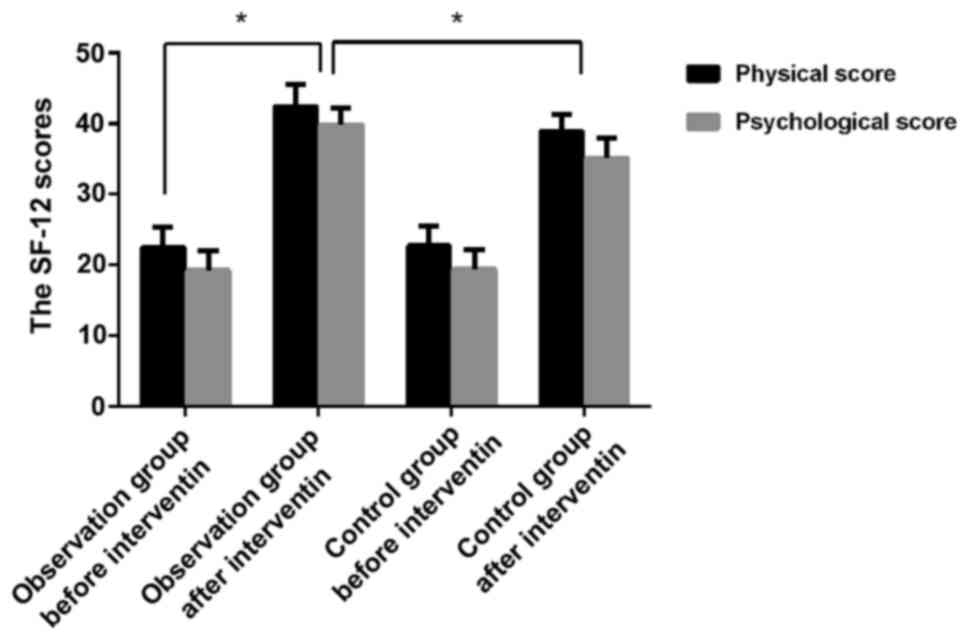
Comparison of SF-12 scores between the
two groups before and after intervention
In SF-12 scores, the physical score and
psychological score in the two groups before intervention were
23.1±1.7, 18.9±1.5 and 23.2±1.7, 18.8±1.5 points, respectively, and
there were no statistically significant differences (t=0.263 and
0.298; P>0.05). After intervention, the physical score and
psychological score in the observation group were 43.5±2.3 and
40.8±2.0 points, respectively, which were obviously higher than
those in the observation group before intervention (t=45.111 and
55.403; P<0.05) and the control group after intervention
(38.6±2.1 and 35.6±1.9 points) (t=9.950 and 11.923; P<0.05)
(Fig. 3).
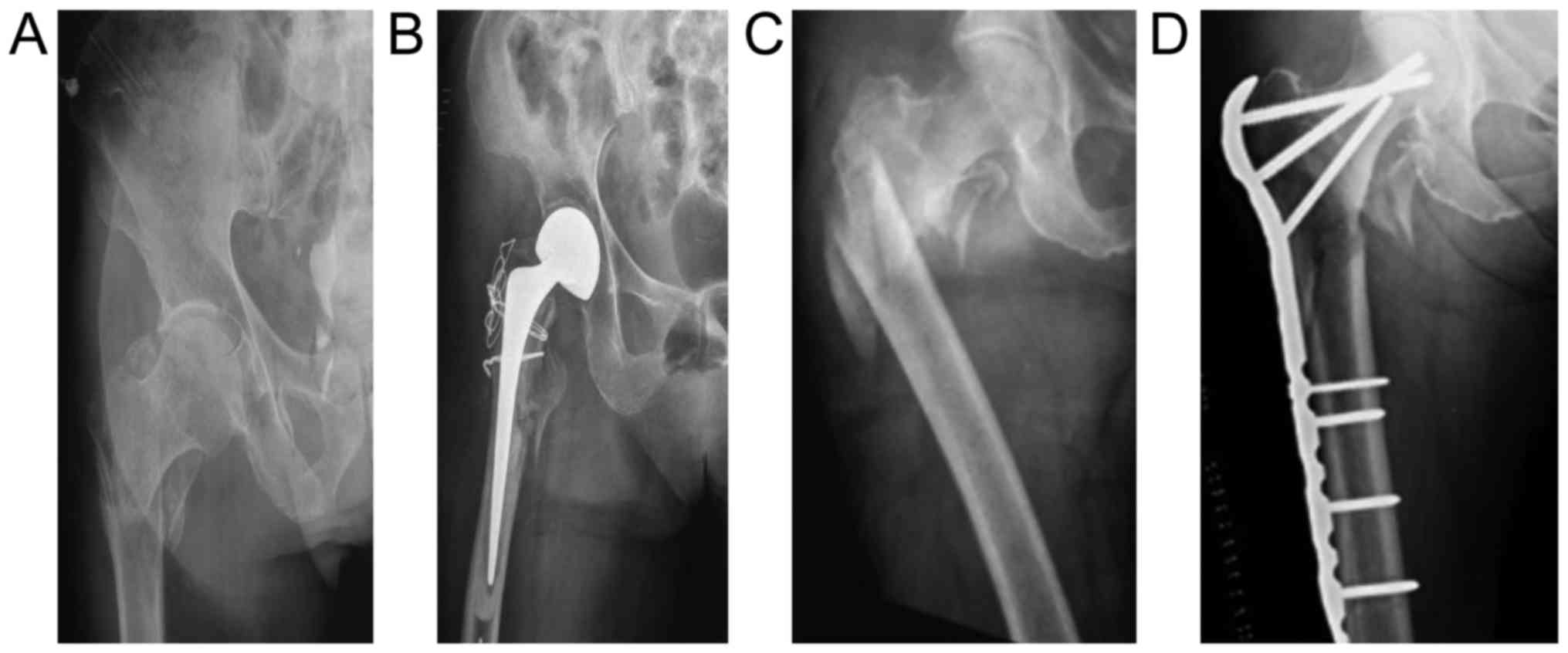
Comparison of X-ray between the two
groups before and after intervention
Preoperative and postoperative X-ray comparison of
two groups of patients are shown in Fig.
4 (A and B represent the preoperative and postoperative X-ray
of the observation group; C and D represent the preoperative and
postoperative X-ray of the control group).
Discussion
Femoral intertrochanteric fracture is a kind of
common fracture in skeletal system in the elderly, which is mainly
based on osteoporosis. The pathological fracture will be caused
under the action of external forces, or even slight forces. If
there is no timely and effective treatment, the mortality rate will
be significantly increased (9). The
key in the successful treatment of this disease is the choice of
surgical method and surgical techniques (10). The surgical treatment of senile
femoral intertrochanteric fracture mainly aims to promote the
recovery of autonomic activities of patients to throw away the
crutches as soon as possible (11)
and reduce the complications caused by long-term immobilization
(12). Therefore, the treatment of
this disease should be targeted: i) strong internal fixation; ii)
early and safe activities; iii) less surgical trauma and short
operative time; iv) better functional recovery after surgery, so
the surgical treatment within 48 h is recommended if medical
conditions permit.
Proximal femoral locking plate is designed based on
the anatomy of the proximal femur (5). Due to the locking function of its screw
thread in distance and depth as well as the locking function of
screw tail, the screw could lock the plate hole to fix the
fracture. At the same time, the plate and screw can be fixed
through the thread, making the locking plate a whole part, so that
the fracture could be fixed on the ‘surface’, which could avoid
stress concentration and enhance the capacity of anti-rotation and
internal fixation. It is applied to the senile intertrochanteric
fracture combined with osteoporosis (13). The PFLP surgery does not require
shaping to make the large intertrochanteric fractures and the small
intertrochanteric fractures to be well fixed. The upper end of the
plate consists of 3 cancellous bone locking screws, which can
effectively prevent the occurrence of hip varus and maintain the
stability of the broken end. The PFLP is easy to operate and has a
good short-term efficacy, allowing early activity. The 40 cases of
the control group in our study had good effect overall, while the
follow-up Harris hip function score, VAS score and SF-12 were
improved compared with those of preoperative conditions. However,
there were 8 cases (20%) of internal fixation loosening and
nonunion in the treatment of PFLP, which might be related to the
blood supply and the seriousness of osteoporosis in elderly
patients.
Jin et al have shown that the failure rate of
internal fixation of 8–16% in the unstable intertrochanteric
fracture (14). Therefore, it is
suggested by some researchers that treatment of artificial joint
replacement should be adopted for femoral intertrochanteric
fractures in special populations (15). This method allows immediate and
effective recovery of the function of the hip joint while the
patients could resume the weight-bearing function as soon as
possible, making them leave the bed early and shortening the bed
rest time. The patients get good recovery of their limb function
and quality of life is improved as well. Furthermore, the
artificial joint replacement could avoid hip varus deformity,
failure of internal fixation and complications caused by long-term
immobilization (16). Babst et
al demonstrated that we should not simply rely on some strong
internal fixtures, but also should pay attention to the reset. The
ideal reset could stabilize the fracture, however, on this basis
the internal fixation will increase its own strength (17). Compared with the artificial femoral
head replacement, the proximal femoral locking plate fixation would
cause larger surgical trauma, more surgical field exposure and more
surgical bleeding to achieve a better reset, which exerts greater
impact on the organ function of patients. In contrast, the
observation group in our study experienced short surgery time, less
bleeding and fast postoperative recovery. Moreover, the total
hospitalization time of the observation group was shorter than that
of the control group; the walking time with the crutches and the
time taken for walking without crutches were both earlier in the
observational group than in the control group, which were conducive
for early functional activities in patients and reduced
complications caused by long-term immobilization.
Postoperative follow-up showed that the Harris hip
score of the observation group was better than the control group,
while the pain VAS score was lower than the control group. In
addition, the comparisons of SF-12 scores between the two groups
before and after intervention revealed that in SF-12 scores, the
physical score and psychological score in the observation group
after intervention were obviously superior to those in the
observation group before intervention and the control group after
intervention, which further indicated that artificial femoral head
replacement in the treatment of senile femoral intertrochanteric
fracture has a positive significance in improving the overall life
quality of patients after operation. Moreover, the stable
artificial femoral head replacement can make patients get out of
bed and bear load earlier after operation (18). At the same time, it avoids the pain
caused by secondary internal fixation, and improves patients'
confidence and compliance (19). It
is particularly suitable for the senile (18) and unstable fractures (20,21), and
those with obvious osteoporosis and old fractures receiving failed
conventional internal fixation (22).
In conclusion, artificial femoral head replacement
is characterized by the short operation time, less intraoperative
bleeding, fast postoperative recovery of joint function, low degree
of pain and fewer complications caused by long-term immobilization,
which can improve the postoperative life quality of patients. It
has a good clinical efficacy in the treatment of senile femoral
intertrochanteric fractures. At the same time, the orthopedic
surgeon should take full account of the patient's age, type of
fracture, bone quality, with or without other medical diseases and
economic conditions in the face of elderly patients with
intertrochanteric fractures, select the appropriate treatment to
minimize patients pain and to achieve rapid recovery.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
HS designed the study. LX and ZW were responsible
for data collection and analysis. ZW performed the operations. HS
prepared the manuscript. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
This study was approved by the Ethics Committee of
Zhangjiagang Hospital of Traditional Chinese Medicine Affiliated to
Nanjing University of Chinese Medicine (Zhangjiagang, China).
Signed informed consents were obtained from the patients or
guardians.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Peng MJ, Chen HY, Hu Y, Ju X and Bai B:
Finite element analysis of porously punched prosthetic short stem
virtually designed for simulative uncemented hip arthroplasty. BMC
Musculoskelet Disord. 18:2952017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Khanna R, Kokubo T, Matsushita T and
Takadama H: Fabrication of dense α-alumina layer on Ti-6Al-4V alloy
hybrid for bearing surfaces of artificial hip joint. Mater Sci Eng
C. 69:1229–1239. 2016. View Article : Google Scholar
|
|
3
|
Zhang BL, Wang F, Tian MB, Yin WL, You XY,
Li D, Ma LG and Xing LQ: Articular capsule repair in initial
artificial hip replacement via anterolateral approach to the hip
joint. J Biol Regul Homeost Agents. 30:441–447. 2016.PubMed/NCBI
|
|
4
|
Lin YT, Wu JS and Chen JH: The study of
wear behaviors on abducted hip joint prostheses by an alternate
finite element approach. Comput Methods Programs Biomed.
131:143–155. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Fankhauser F, Boldin C, Schippinger G,
Haunschmid C and Szyszkowitz R: A new locking plate for unstable
fractures of the proximal humerus. Clin Orthop Relat Res.
430:176–181. 2005. View Article : Google Scholar
|
|
6
|
Hsu CJ, Chou WY, Chiou CP, Chang WN and
Wong CY: Hemi-arthroplasty with supplemental fixation of greater
trochanter to treat failed hip screws of femoral intertrochanteric
fracture. Arch Orthop Trauma Surg. 128:841–845. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Li N, Liu HN, Gong XF, Zhu SW, Wu XB and
He L: Epidemiological analysis of hospitalized patients with
femoral neck fracture in a first-class hospital of Beijing. Beijing
Da Xue Xue Bao Yi Xue Ban. 48:292–296. 2016.(In Chinese).
PubMed/NCBI
|
|
8
|
Jensen JS and Michaelsen M: Trochanteric
femoral fractures treated with McLaughlin osteosynthesis. Acta
Orthop Scand. 46:795–803. 1975. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Richmond J, Aharonoff GB, Zuckerman JD and
Koval KJ: Mortality risk after hip fracture. J Orthop Tauma.
17:2–5. 2003. View Article : Google Scholar
|
|
10
|
van Embden D, Rhemrev SJ, Meylaerts SA and
Roukema GR: The comparison of two classifications for trochanteric
femur fractures: the AO/ASIF classification and the Jensen
classification. Injury. 41:377–381. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Khanna R, Kokubo T, Matsushita T, Nomura
Y, Nose N, Oomori Y, Yoshida T, Wakita K and Takadama H: Novel
artificial hip joint: A layer of alumina on Ti-6Al-4V alloy formed
by micro-arc oxidation. Mater Sci Eng C. 55:393–400. 2015.
View Article : Google Scholar
|
|
12
|
Clarke A, Pulikottil-Jacob R, Grove A,
Freeman K, Mistry H, Tsertsvadze A, Connock M, Court R, Kandala NB,
Costa M, et al: Total hip replacement and surface replacement for
the treatment of pain and disability resulting from end-stage
arthritis of the hip (review of technology appraisal guidance 2 and
44): Systematic review and economic evaluation. Health Technol
Assess. 19:1–668. 2015. View
Article : Google Scholar
|
|
13
|
Konstantinidis L, Papaioannou C, Mehlhorn
A, Hirschmüller A, Südkamp NP and Helwig P: Salvage procedures for
trochanteric femoral fractures after internal fixation failure:
biomechanical comparison of a plate fixator and the dynamic
condylar screw. Proc lnst Mech Eng H. 225:710–717. 2011. View Article : Google Scholar
|
|
14
|
Jin WJ, Dai LY, Cui YM, Zhou Q, Jiang LS
and Lu H: Reliability of classification systems for
intertrochanteric fractures of the proximal femur in experienced
orthopaedic surgeons. Injury. 36:858–861. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Hwang DS, Kwak SK and Woo SM: Results of
cementless hemiarthroplasty for elderly patients with unstable
intertrochanteric fractrres. J Korean Hip Soc. 16:386–391.
2004.
|
|
16
|
Chan KC and Gill GS: Cemented
hemiarthroplasties for elderly patients with intertrochanteric
fractures. Clin Orthop Relat Res. 371:206–215. 2000. View Article : Google Scholar
|
|
17
|
Babst R, Renner N, Biedermann M, Rosso R,
Heberer M, Harder F and Regazzoni P: Clinical results using the
trochanter stabilizing plate (TSP): the modular extension of the
dynamic hip screw (DHS) for internal fixation of selected unstable
intertrochanteric fractures. J Orthop Trauma. 12:392–399. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Feng W, Hao T, Liu WL, Jia YF, Hao ZT and
Bai SB: Clinical outcome of endoprosthetic replacement for failed
treatment of intertrochanteric fractures: A retrospective case
series. Pak J Med Sci. 29:633–637. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Lizhang J, Taylor SD, Jin Z, Fisher J and
Williams S: Effect of clearance on cartilage tribology in hip
hemi-arthroplasty. Proc Inst Mech Eng H. 227:1284–1291. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Suzuki A, Koshida K and Matsubara K:
Adjustment of overestimated CT-based attenuation correction on bone
SPECT/CT after hip-resurfacing arthroplasty. J Nucl Med Technol.
41:203–207. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Figved W, Dahl J, Snorrason F, Frihagen F,
Röhrl S, Madsen JE and Nordsletten L: Radiostereometric analysis of
hemiarthroplasties of the hip - a highly precise method for
measurements of cartilage wear. Osteoarthritis Cartilage. 20:36–42.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Yu X, Jiang W, Pan Q, Wu T, Zhang Y, Zhou
Z and Du D: Umbrella-shaped, memory alloy femoral head support
device for treatment of avascular osteonecrosis of the femoral
head. Int Orthop. 37:1225–1232. 2013. View Article : Google Scholar : PubMed/NCBI
|