Introduction
Osteoporosis affects the spine most frequently and
it is the most common in thoracolumbar spine, which often occurs in
the elderly female patients. Once the osteoporosis occurs, it will
seriously affect the bearing capacity and stability of spine, thus
leading to spontaneous fractures (1). In the treatment of such patients with
internal screw fixation, the strength of internal fixator and
postoperative recovery will be negatively affected, which is the
relevant risk factor to the postoperative complications and even
surgical failure (2). Studies have
shown that the proportion of postoperative screw loosening in
patients complicated with osteoporosis is ~15% (3). In the past, the internal fixation
strength in osteoporosis patients with lumbar fracture was often
enhanced through increasing the screw length and diameter, or
combined application with bone cement (4), which, however, increased the risk of
nerve and vascular injury, and even pedicle fracture (5). Expansive pedicle screw has higher
internal fixation stability, especially anti-prolapse capacity,
compared with the ordinary screw, so it has been paid increasingly
more attention in clinical practice (6). In this study, the internal fixation
treatment of lumbar short-segment compression fracture in
osteoporosis patients with expansive pedicle screw was studied.
Patients and methods
General patient data
A total of 80 patients with lumbar compression
fracture treated in the First People's Hospital of Wujiang District
(Suzhou, China) from November 2015 to January 2017 were selected.
All patients signed the informed consent before enrollment. This
study was approved by the Ethics Committee of the First People's
Hospital of Wujiang District.
Inclusion criteria: patients aged 45–70 years were
definitely diagnosed with lumbar compression fracture and
osteoporosis via clinical manifestations, computed tomography (CT),
magnetic resonance imaging (MRI) examination and bone mineral
density (BMD).
Exclusion criteria: patients with obvious nerve
compression, coagulation dysfunction, mental illness, systemic
infection, severe cardiopulmonary insufficiency or hepatorenal
insufficiency, malignant tumor, fracture of lower limb, or low back
pain caused by other reasons were excluded.
All patients enrolled were divided into the
observation group (n=40) and the control group (n=40) using a
random number table. In the observation group, there were 12 males
and 28 females aged 45–70 years (65.5±2.0 years on average) with
the course of disease of 1–5 months (3.0±0.3 months on average).
The nerve injury was classified according to the Frankel score:
there were 11 cases of grade C, 23 cases of grade D and 6 cases of
grade E. In terms of the pathogenic site, there were 30 cases in
L1, 5 cases in L2 and 5 cases in
L3 and below. The anterior height ratio of injured
vertebra was 25.0–75.0% (45.0±2.0% on average). The Cobb's angle
was 15.0–40.5° (29.3±1.1° on average). In the control group, there
were 11 males and 29 females aged 45–70 years (65.6±2.0 years on
average) with the course of disease of 1–5 months (3.1±0.3 months
on average). The nerve injury was classified according to the
Frankel score: there were 12 cases of grade C, 23 cases of grade D
and 5 cases of grade E. In terms of the pathogenic site, there were
31 cases in L1, 4 cases in L2 and 5 cases in
L3 and below. The anterior height ratio of injured
vertebra was 25.0–75.0% (45.3±2.0% on average). The Cobb's angle
was 15.0–40.5° (29.5±1.0° on average). The sex, age, course of
disease, Frankel score of nerve injury, pathogenic site, anterior
height ratio of injured vertebra and Cobb's angle had no
statistically significant differences between the two groups
(p>0.05).
Methods
All patients received the operative treatment via
trachea cannula under general anesthesia. Under the prone position,
patients with compression fracture underwent the manual reduction
after successful anesthesia from posterior approach. Whether the
total laminectomy and bone graft fusion were performed was
determined based on the injury severity. The internal fixator used
in the observation group was the expansive pedicle screw. The
vertebral pedicle was drilled and the expansive pedicle screw was
placed in it under the C-arm guidance. A fine needle with 3 mm in
diameter penetrated into the vertebral body for positioning and
guidance, and then ~2 ml bone cement prepared in advance was
injected using the injector into the hole on each vertebral
pedicle. But the amount of bone cement was reduced appropriately
for patients complicated with severe vertebral compression
fracture, so as to reduce the bone cement leakage. After injection
of bone cement, the syringe needle was immediately drawn out and
the expansive pedicle screw was screwed into the vertebral pedicle
along the hole approach. Then the expansive inner core was placed
into the pedicle screw to fully expand the screw precursor,
followed by fixation using screw rod. The tail cap was screwed and
the autogenous bone cage was implanted. The control group was
treated with conventional pedicle screw and bone graft fusion via
the same surgical approach, as well as the screw placement and bone
graft fusion under the C-arm guidance.
Observational indexes
The operation time, intraoperative bleeding and
postoperative indwelling drainage were compared between the two
groups. After operation, the straight leg raising test (SLRT)
score, visual analogue scale (VAS) score of lumbocrural pain and
lower limb sensory score were evaluated in the postoperative
follow-up. Moreover, the operation-related complications, the bone
graft fusion rates at 3 and 6 months after operation, the spinal
stenosis rates after operation, the vertebral height ratios and
Cobb's angles of the two groups were recorded. Finally, the
correlation between BMD and hospitalization time after operation in
the observation group was analyzed.
Evaluation criteria
Sensory score: the puncture sensation and light
touching of 17 dermatomes in bilateral lower limbs were scored. The
total score is 112 point, and the higher the score is, the more
perfect the function will be; the VAS score was used for
lumbocrural pain: 10 points indicate unbearable pain, while 0 point
indicates no pain. SLRT score: under the supine position on hard
bed, the patients raised the leg on the affected side. Raising
angle ≥70° indicates normal, 0 point; 50–60° for 1 point; 40–50°
for 2 points; 20–40° for 3 points; <20° for 4 points; the higher
the score is, the more obvious the clinical symptoms will be.
Bridwell bone healing standard was used for bone graft fusion:
level I: complete fusion and remodeling after intervention with
newly-formed trabeculae; level II: complete bone block after
intervention, but incomplete remodeling without lucent area; level
III: complete bone block after intervention, but incomplete
remodeling with a few lucent areas; level IV: significant collapse
and absorption of bone block after intervention, no bone healing or
remodeling. In this study, level I and II was included into the
statistics of bone graft fusion. Diagnostic criteria of
osteoporosis: it was mainly based on BMD, combined with the
characteristics of Chinese population; generally, L3 BMD
lower than the average BMD for two standard deviations indicates
osteoporosis; reference value of L3 BMD SD=1.228
g/cm3; spinal stenosis rate = [normal sagittal diameter
(A) - sagittal diameter in the narrowest part (B)]/A ×100%;
vertebral height ratio (%) is the geometric mean of adjacent
vertebral height; Cobb's angle: it is measured in the adem position
using the Cobb's angle protractor under the X-ray guidance.
Statistical analysis
Statistical Product and Service Solutions (SPSS)
13.0 (SPSS, Inc., Chicago, IL, USA) was used for statistical
treatment. Measurement data were presented as mean ± standard
deviation (SD), t-test was used for the comparison of means between
the two groups, and the Chi-square test was used for the comparison
of ratio between the two groups. P<0.05 suggested that the
difference was statistically significant.
Results
Comparison of the SLRT score, VAS
score of lumbocrural pain, lower limb sensory score before
operation between the two groups
The SLRT score, VAS score of lumbocrural pain and
lower limb sensory score had no statistically significant
differences before operation between the two groups, respectively
(p>0.05).
Comparison of operation time,
intraoperative bleeding and hospitalization time after operation
between the two groups
In the observation group, the operation time was
shorter than that in the control group (p<0.05), the
intraoperative bleeding was less than that in the control group
(p<0.05), and the hospitalization time after operation was also
shorter than that in the control group (p<0.05) (Table I).
 | Table I.Comparison of operation time,
intraoperative bleeding and hospitalization time after operation
between the two groups (mean ± standard deviation). |
Table I.
Comparison of operation time,
intraoperative bleeding and hospitalization time after operation
between the two groups (mean ± standard deviation).
| Groups | Operation time
(min) | Intraoperative
bleeding (ml) | Hospitalization time
after operation (days) |
|---|
| Observation
group | 149.7±8.7 | 500.0±60.0 | 12.6±2.3 |
| Control group | 178.1±10.8 | 1,000.0±100.0 | 20.6±3.5 |
| t | 12.952 | 27.116 | 12.081 |
| P-value | <0.001 | <0.001 | <0.001 |
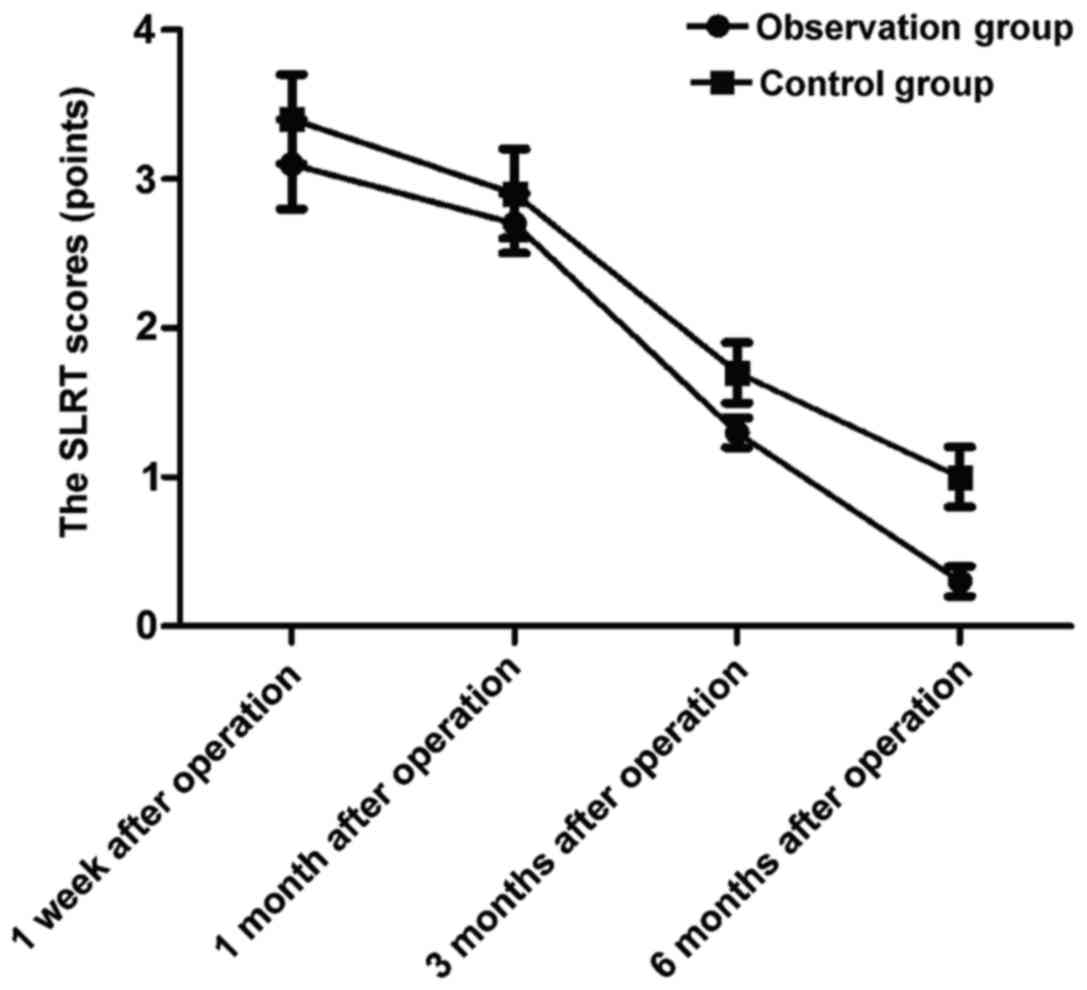
Comparison of SLRT scores in
postoperative follow-up between the two groups
At 1 week, 1, 3 and 6 months after operation, the
SLRT scores of the observation group were 3.4±0.3, 2.7±0.2, 1.3±0.1
and 0.3±0.1 points, respectively, which were significantly superior
to those of the control group (3.4±0.3, 2.9±0.3, 1.7±0.2 and
1.0±0.2 points) (t=4.472, 3.508, 11.314 and 19.799; p<0.05)
(Fig. 1).
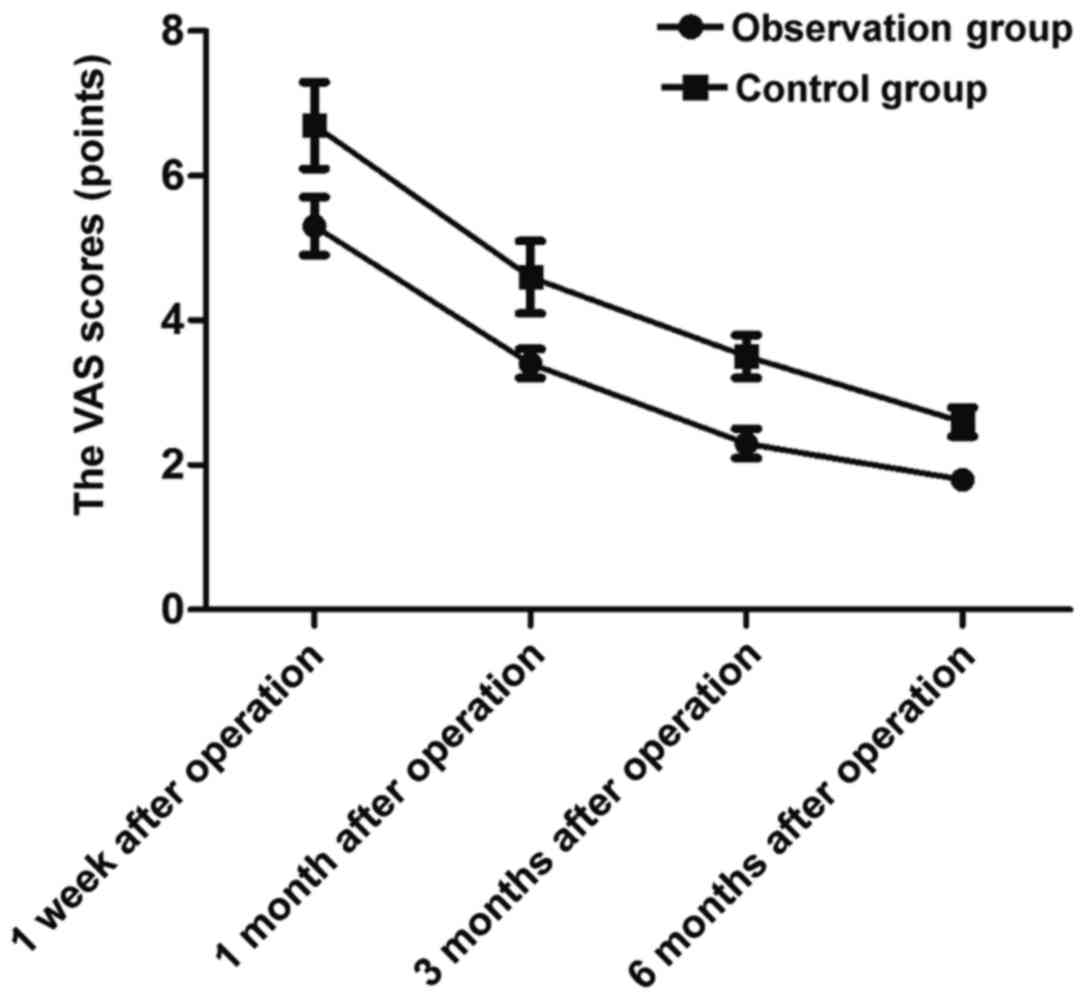
Comparison of VAS scores of
lumbocrural pain in postoperative follow-up between the two
groups
At 1 week, 1, 3 and 6 months after operation, the
VAS scores of lumbocrural pain of the observation group were
5.3±0.4, 3.4±0.2, 2.3±0.2 and 1.8±0.1 points, respectively, which
were significantly lower than those of the control group (6.7±0.6,
4.6±0.5, 3.5±0.3 and 2.6±0.2 points) (t=12.279, 14.093, 21.049 and
22.627; p<0.05) (Fig. 2).
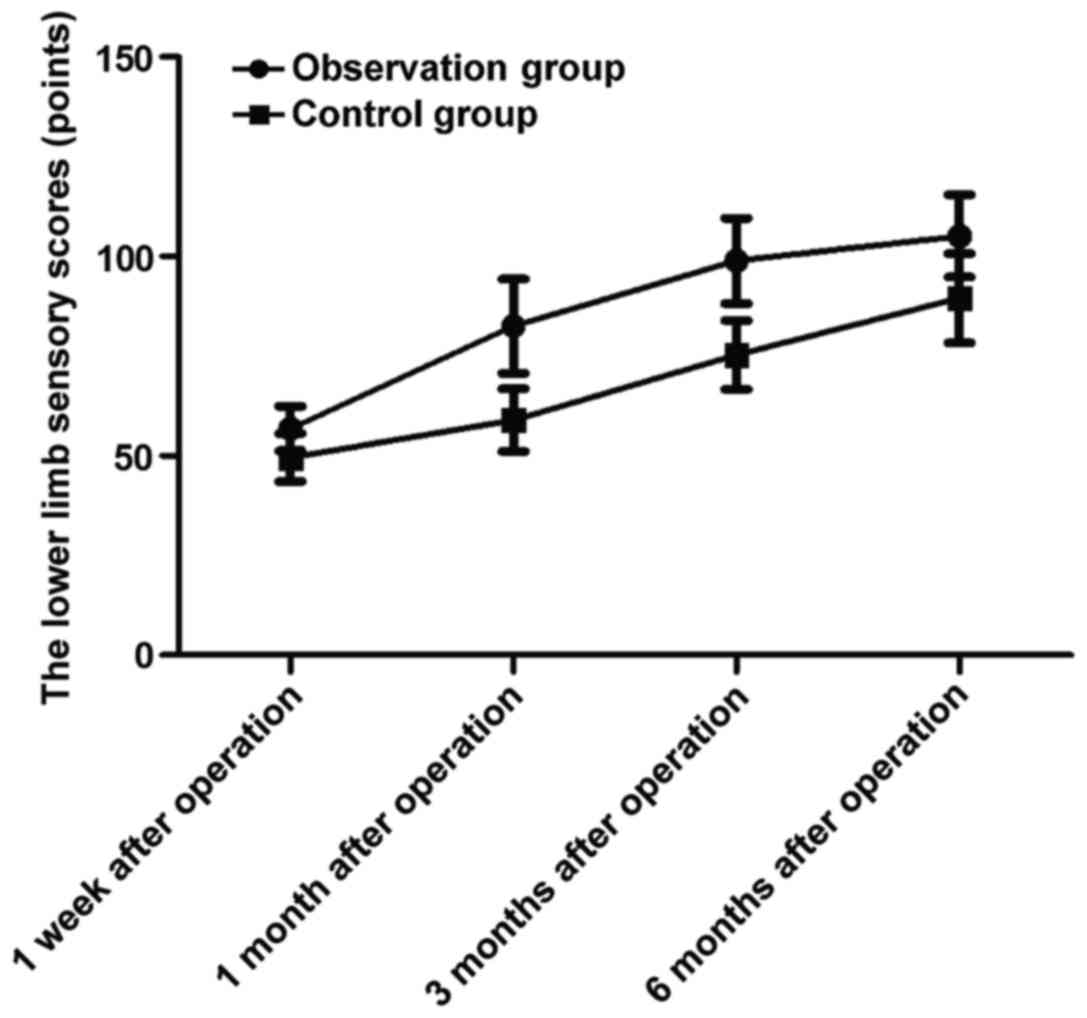
Comparison of lower limb sensory
scores in postoperative follow-up between the two groups
At 1 week, 1, 3 and 6 months after operation, the
lower limb sensory scores of the observation group were 56.8±5.6,
82.5±11.8, 98.9±10.7 and 105.1±10.3 points, respectively, which
were significantly higher than those of the control group
(49.6±6.0, 58.9±7.9, 75.3±8.6 and 89.5±11.2 points) (t=5.548,
10.511, 10.873 and 6.484; p<0.05) (Fig. 3).
Comparison of operation-related
complications between the two groups
The proportions of postoperative infection, dural
mater tear, nerve root injury and spinal cord injury during
operation in the observation group were lower than those in the
control group (p<0.05) (Table
II).
 | Table II.Comparison of operation-related
complications between the two groups [n (%)]. |
Table II.
Comparison of operation-related
complications between the two groups [n (%)].
| Groups | Spinal cord
injury | Dural mater tear | Nerve root
injury | Wound infection | Total incidence rate
(%) |
|---|
| Observation
group | 0 | 1 | 0 | 2 | 3 (7.5%) |
| Control group | 1 | 6 | 2 | 3 | 12 (30.0%) |
| χ2 |
|
|
|
| 5.251 |
| P-value |
|
|
|
| 0.022 |
Comparison of bone graft fusion rates
at 3 and 6 months after operation between the two groups
The bone graft fusion rates at 3 and 6 months after
operation were obviously superior to those in the control group
(p<0.05) (Table III).
 | Table III.Comparison of bone graft fusion rates
at 3 and 6 months after operation between the two groups [n
(%)]. |
Table III.
Comparison of bone graft fusion rates
at 3 and 6 months after operation between the two groups [n
(%)].
| Groups | 3 months after
operation | 6 months after
operation |
|---|
| Observation
group | 23 (57.5%) | 36 (90.0%) |
| Control group | 11 (27.5%) | 20 (50.0%) |
| χ2 | 7.366 | 15.238 |
| P-value | 0.007 | <0.001 |
Comparison of spinal stenosis rate,
vertebral height ratio and Cobb's angle between the two groups
After operation, the spinal stenosis rate in the
observation group was lower than that in the control group
(p<0.05), the vertebral height ratio was larger than that in the
control group (p<0.05), and the Cobb's angle was smaller than
that in the control group (p<0.05) (Table IV).
 | Table IV.Comparison of spinal stenosis rate,
vertebral height ratio and Cobb's angle between the two groups
(mean ± standard deviation). |
Table IV.
Comparison of spinal stenosis rate,
vertebral height ratio and Cobb's angle between the two groups
(mean ± standard deviation).
| Groups | Spinal stenosis rate
(%) | Vertebral height
ratio (%) | Cobb's angle (°) |
|---|
| Observation
group |
3.6±0.2 | 96.5±2.1 | 3.0±0.2 |
| Control group | 10.9±1.1 | 86.5±3.3 | 8.2±1.1 |
| t | 41.295 | 16.169 | 29.416 |
| P-value | <0.001 | <0.001 | <0.001 |
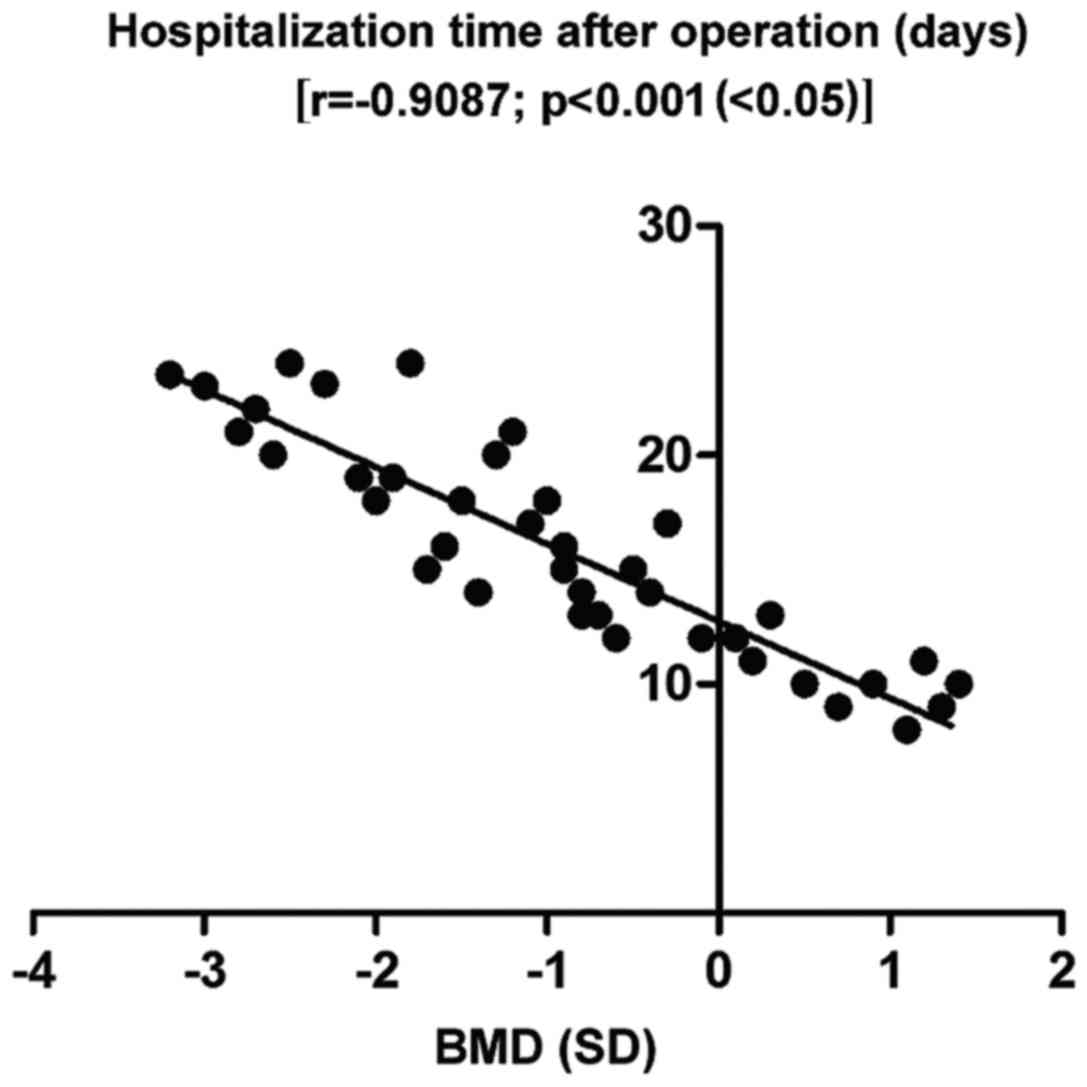
Correlation analysis of BMD with
hospitalization time after operation in the observation group
Pearsons correlation analysis showed that there was
a negative correlation between BMD and hospitalization time after
operation in the observation group [r=−0.9087; p<0.001
(<0.05)] (Fig. 4).
Discussion
The pedicle screw fixation treatment is one of the
good methods for the clinical treatment of lumbar compression
fractures (7). However, the
stability of conventional pedicle screw fixation for patients with
osteoporosis is significantly reduced due to lumbar osteoporosis,
and it is difficult to achieve a solid internal fixation effect
(8). Expansive pedicle screw can fix
the vertical axial section through the front expansive effect
(9), thus forming the triangular
support (10), and significantly
increasing the screw bonding (11);
at the same time, the surrounding bone trabecula is appropriately
compressed, thereby further improving the bone density and the
stability of internal fixation (12). In addition, the front end of internal
fixation screw after expansion can expand to both sides, thus
effectively embedding into the bone and better improving the
anti-rotation capacity of the screw (13). Therefore, expansive pedicle screw has
been widely used in the treatment of lumbar compression fractures
in patients with osteoporosis (14).
In this study, the observation group was treated
with expansive pedicle screw, while the control group was treated
with conventional internal screw fixation. In the observation
group, the operation time was shorter than that in the control
group, the intraoperative bleeding was less than that in the
control group and the postoperative hospitalization time was
shorter than that in the control group, suggesting that the
expansive pedicle screw treatment of osteoporosis patients with
lumbar compression fractures can significantly shorten the
operation time, reduce the intraoperative bleeding and promote the
postoperative recovery of patients. In addition, the SLRT score,
VAS score of lumbocrural pain and lower limb sensory score were
compared between the two groups in the postoperative follow-up and
it was found that at 1 week, 1, 3 and 6 months after operation, the
SLRT scores of the observation group were significantly superior to
those of the control group, the VAS scores of lumbocrural pain were
significantly lower than those of the control group, but the lower
limb sensory scores were significantly higher than those of the
control group, indicating that after the expansive pedicle screw
treatment of osteoporosis patients with lumbar compression
fractures, the lower limb motor and sensory functions of patients
after operation are improved significantly, and the pain degree is
reduced. At the same time, the study on the operation-related
complications in the two groups showed that the proportions of
postoperative infection, dural mater tear, nerve root injury and
spinal cord injury during operation in the observation group were
lower than those in the control group, and there were no spinal
cord injury, nerve root injury or other severe peripheral nerve
injury in the observation group, suggesting that the expansive
pedicle screw treatment of osteoporosis patients with lumbar
compression fractures has fewer postoperative complications than
conventional internal screw fixation; in particular, it avoids the
impact on the spinal cord, nerve root and other important tissues,
so its safety is better. The bone graft fusion rates at 3 and 6
months after operation were obviously superior to those in the
control group. Moreover, after operation, the spinal stenosis rate
in the observation group was lower than that in the control group,
the vertebral height ratio was larger than that in the control
group, and the Cobb's angle was smaller than that in the control
group, further suggesting that the expansive pedicle screw
treatment of osteoporosis patients with lumbar compression
fractures has a higher bone graft fusion rate, effectively improves
the acute compression fractures, thus improving the surgical
effects. Finally, the correlation analysis of BMD and
hospitalization time after operation in the observation group
showed that there was a negative correlation between BMD and
hospitalization time after operation, indicating that osteoporosis
has a negative effect not only on the conventional screw internal
fixation treatment, but also on the expansive pedicle screw
internal fixation treatment. Therefore, the expansive pedicle screw
treatment of osteoporosis patients with lumbar compression
fractures is not a universal method, and the strict control over
indications and the active treatment of osteoporosis are of great
significance in improving the prognosis of patients. These results
are in accordance with previous studies (15,16).
Expansive pedicle screw, compared with the
conventional pedicle screw, mainly consists of two major
components, hollow outer tube screws and built-in cylinder screw
expander (17). During operation,
the cylindrical tube screw is compressed to expand the hollow outer
tube, making the diameter of nail tip reach ~2.5 cm (18), thereby strengthening the compression
against the osteoporotic vertebral bone around the nail and
improving the screw bonding (19).
One third of the end of expansive pedicle screw has no expansion
effect (20), so the pedicle
fracture is effectively avoided and the surgical results are
improved; at the same time, the vertical tail of pedicle screw can
realize the universal fixation (21), effectively avoiding the compression
and enhancement during the conventional screw implantation, thereby
shortening the operation time. In addition, after the screw
implantation, the vertebral trabeculae around the implantation has
a certain expansion and compression with the extension of
implantation time (22), inducing
longitudinal endogenous fusion and realizing the bone-nail fusion
(23), which further increases the
stability of screw fixation and reduces the risk of postoperative
screw shedding and loosening. It must be mentioned, however, that a
limitation of this study was the small sample size. Further studies
with a larger number of samples will be needed in the future.
In conclusion, the internal fixation with expansive
pedicle screw for osteoporosis patients with lumbar compression
fracture is characterized by short operation time, less
intraoperative bleeding, few complications, quick recovery of
postoperative neurological function and satisfactory surgical
effect. However, reasonable intervention in osteoporosis is also
necessary.
Acknowledgements
Not applicable.
Funding
We received no funding support for this study.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
FW and ZT designed the study. JW, LY and JZ
collected the data. FW and YC performed the data analysis and
statistics. JW and LY conducted the data interpretation. FW
prepared the manuscript. FW, JW and ZT performed the operations.
All authors read and approved the final manuscript.
Ethics approval and consent to
participate
This study was approved by the Ethics Committee of
the First People's Hospital of Wujiang District (Suzhou, China).
Signed informed consents were obtained from the patients or the
guardians.
Patient consent for publication
Patients or their guardians provided written
informed consents for publication.
Competing interests
The authors declare no competing interests.
References
|
1
|
Aycan MF, Tolunay T, Demir T, Yaman ME and
Usta Y: Pullout performance comparison of novel expandable pedicle
screw with expandable poly-ether-ether-ketone shells and
cement-augmented pedicle screws. Proc Inst Mech Eng H. 231:169–175.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kehayov II, Zhelyazkov CB, Kalnev BM,
Davarski AN, Kitov BD and Raykov SD: Initial experience with O-arm
navigated spinal surgery - report on two cases. Folia Med
(Plovdiv). 58:293–298. 2016.PubMed/NCBI
|
|
3
|
Wang MY, Chang PY and Grossman J:
Development of an Enhanced Recovery After Surgery (ERAS) approach
for lumbar spinal fusion. J Neurosurg Spine. 26:411–418. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Fischer CR, Hanson G, Eller M and Lehman
RA: A systematic review of treatment strategies for degenerative
lumbar spine fusion surgery in patients with osteoporosis. Geriatr
Orthop Surg Rehabil. 7:188–196. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Gazzeri R, Roperto R and Fiore C: Surgical
treatment of degenerative and traumatic spinal diseases with
expandable screws in patients with osteoporosis: 2-year follow-up
clinical study. J Neurosurg Spine. 25:610–619. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Mueller JU, Baldauf J, Marx S, Kirsch M,
Schroeder HW and Pillich DT: Cement leakage in pedicle screw
augmentation: A prospective analysis of 98 patients and 474
augmented pedicle screws. J Neurosurg Spine. 25:103–109. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Pakzaban P: Modified mini-open
transforaminal lumbar interbody fusion: Description of surgical
technique and assessment of free-hand pedicle screw insertion.
Spine (Phila Pa 1976). 41:E1124–E1130. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Cannestra AF, Peterson MD, Parker SR,
Roush TF, Bundy JV and Turner AW: MIS expandable interbody spacers:
A literature review and biomechanical comparison of an expandable
MIS TLIF with conventional TLIF and ALIF. Spine. 41(Suppl 8):
S44–S49. 2016.PubMed/NCBI
|
|
9
|
Weiss HR and Moramarco M: Congenital
scoliosis (mini-review). Curr Pediatr Rev. 12:43–47. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Mundis GM, Eastlack RK, Moazzaz P, Turner
AW and Cornwall GB: Contribution of round vs. rectangular
expandable cage endcaps to spinal stability in a cadaveric
corpectomy model. Int J Spine Surg. 9:532015.
|
|
11
|
Chen YL, Chen WC, Chou CW, Chen JW, Chang
CM, Lai YS, Cheng CK and Wang ST: Biomechanical study of expandable
pedicle screw fixation in severe osteoporotic bone comparing with
conventional and cement-augmented pedicle screws. Med Eng Phys.
36:1416–1420. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Gonzalez-Blohm SA, Doulgeris JJ, Aghayev
K, Lee WE III, Laun J and Vrionis FD: In vitro evaluation of a
lateral expandable cage and its comparison with a static device for
lumbar interbody fusion: A biomechanical investigation. J Neurosurg
Spine. 20:387–395. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Bartanusz V, Harris J, Moldavsky M, Cai Y
and Bucklen B: Short segment spinal instrumentation with index
vertebra pedicle screw placement for pathologies involving the
anterior and middle vertebral column is as effective as long
segment stabilization with cage reconstruction: A biomechanical
study. Spine. 40:1729–1736. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Mantell M, Cyriac M, Haines CM, Gudipally
M and O'Brien JR: Biomechanical analysis of an expandable lateral
cage and a static transforaminal lumbar interbody fusion cage with
posterior instrumentation in an in vitro spondylolisthesis model. J
Neurosurg Spine. 24:32–38. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Xie W, Gao P and Ji L: Three-dimensional
spiral CT measurement of atlantal pedicle and its clinical
application. Exp Ther Med. 14:1467–1474. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Zhou W, Kong W, Zhao B, Fu Y, Zhang T and
Xu J: Posterior internal fixation plus vertebral bone implantation
under navigational aid for thoracolumbar fracture treatment. Exp
Ther Med. 6:152–158. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Donnelly DJ, Abd-El-Barr MM and Lu Y:
Minimally invasive muscle sparing posterior-only approach for
lumbar circumferential decompression and stabilization to treat
spine metastasis - technical report. World Neurosurg. 84:1484–1490.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Demir T: A new alternative to expandable
pedicle screws: Expandable poly-ether-ether-ketone shell. Proc Inst
Mech Eng H. 229:386–394. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kang SH, Cho YJ, Kim YB and Park SW:
Pullout strength after expandable polymethylmethacrylate
transpedicular screw augmentation for pedicle screw loosening. J
Korean Neurosurg Soc. 57:229–234. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Lehman RA Jr, Kang DG and Wagner SC:
Management of osteoporosis in spine surgery. J Am Acad Orthop Surg.
23:253–263. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Eschler A, Ender SA, Schiml K, Mittlmeier
T and Gradl G: Bony healing of unstable thoracolumbar burst
fractures in the elderly using percutaneously applied titanium mesh
cages and a transpedicular fixation system with expandable screws.
PLoS One. 10:e01171222015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Galbusera F, Volkheimer D, Reitmaier S,
Berger-Roscher N, Kienle A and Wilke HJ: Pedicle screw loosening: A
clinically relevant complication? Eur Spine J. 24:1005–1016. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Jandial R, Kelly B and Chen MY:
Posterior-only approach for lumbar vertebral column resection and
expandable cage reconstruction for spinal metastases. J Neurosurg
Spine. 19:27–33. 2013. View Article : Google Scholar : PubMed/NCBI
|