Introduction
Acute ST-segment elevation myocardial infarction
(STEMI) is the most common type of coronary artery syndrome (ACS).
At present, the preferred option to treat STEMI patients in clinic
is the early implementation of myocardial reperfusion therapy, in
order to save the dying heart muscle. However, due to the
continuous occlusion of small blood vessels and difficulties in
reversing the prolonged lack of blood supply caused myocardial
necrosis, the occurrence of heart failure, cardiac rupture, and
other serious adverse events in patients after reperfusion
treatment cannot be ignored. At present, TIMI, GRACE, CCP and other
scoring systems have been used for STEMI risk assessment in clinic,
and a number of studies have also shown that several risk scores
can clearly indicate the prognosis of STEMI patients (1–3).
However, this existing system needs to integrate the patient's body
mass index, pathological condition, electrocardiogram analysis,
cardiac function classification and other indicators, in order to
prevent poor performance. Therefore, there is an important need to
establish a STEMI reperfusion risk score system that has a high
degree of accuracy and is easy to implement, in order to guide
clinical treatment and prevent poor prognosis after reperfusion.
Four-dimensional speckle tracking imaging (4D-STI) is the result of
the latest development in the field of ultrasound medicine, in
which four-dimensional trajectories of echo spots in the myocardium
are employed to calculate the myocardial relaxation function. Due
to its measurement accuracy, ease of use and high repeatability,
its great potential for the clinical diagnosis and treatment of
cardiovascular disease, it has become the focus of cardiovascular
imaging research. To date, the application of 4D-STI for analyzing
the prognosis of STEMI patients after reperfusion treatment remains
unreported. In the present study, STEMI was determined by 4D-STI
within 72 h after reperfusion treatment through the
four-dimensional strain of the patient's heart. Data were collected
after STEMI reperfusion treatment to establish a new risk
stratification classification, and this was compared with the
traditional TIMI risk score system to determine its predictive
value, aiming to improve postoperative patient management and
effectively prevent poor prognosis.
Materials and methods
General information
From March 2013 to November 2015, patients who
attended the Department of Cardiology of Shanghai Jiading Center
Hospital (Shanghai, China) due to the onset of acute myocardial
infarction, and were diagnosed according to the 2010 edition of the
acute STEMI diagnostic and treatment guidelines for STEMI in
parallel with emergency percutaneous coronary intervention (PCI),
were studied (4). Inclusion criteria
were: i) Patients who were 20–75 years, with first occurrence of
STEMI; ii) patients who were admitted (<12 h from onset),
received reperfusion treatment, and underwent direct line PCI
without thrombolysis. Exclusion criteria were: i) Patients with
serious arrhythmias such as frequent premature beats, atrial
fibrillation, acute heart failure, or cardiogenic shock detected by
electrocardiogram and echocardiography; ii) patients suffering from
severe emphysema, pulmonary fibrosis, or other ventilated
dysfunction; iii) patients with obvious acidosis or uremia, or
previously in a coma; iv) patients with a tendency to severe
bleeding; and v) patients with poor acoustic conditions.
According to these criteria, a total of 120 patients
were included in the present study. Among these patients, 81 were
male and 39 patients were female; and the average age was
50.21±11.66 years. This study was approved by the Ethics Committee
of Shanghai Jiading Center Hospital. The patients and their
families were informed of the details and possible risks of the
study, and a signed consent form was obtained from the patients or
guardians prior to enrollment into the study.
Instruments and ultrasound detection
indicators
A Vivid E9 color ultrasound diagnostic apparatus (GE
Healthcare, Milwaukee, WI, USA) with a 4D real-time
three-dimensional phased array probe was used within 12 h after all
patients underwent PCI. Then, four-dimensional echocardiography was
performed on the 2nd and 3rd day after the operation. The subjects
were asked to take the supine position and breathe normally during
the probe scan: i) Conventional series of standard sections; ii)
the three short axis views of the sternal left ventricular mitral
valve level, papillary muscle level and apical level; iii) the
three long axis sections of the apical four-chamber, two-chamber
and long axis; and iv) the four-dimensional surface of the apical
four-chamber view. The ECHO-PAC left ventricular quantitative
software (GE Healthcare) was used to automatically analyze the
segments of the myocardium (17 segment standard) in the
three-dimensional longitudinal strain (LS), circumferential strain
(CS), radial strain (RS) and area strain (AS).
Method
After the enrollment of each patient, their contact
numbers and home address were kept to facilitate the follow-up. Age
at admission, body weight, history of diabetes/hypertension/angina,
clinical symptoms, records of the time of reperfusion therapy and
surgery, detection of the three observation points within 72 h
after the operation (12 h after PCI, 2nd and 3rd day after
operation) in the myocardial four-dimensional strain, as well as
the evaluation of systolic blood pressure at 3rd day after
operation, and the heart rate and cardiac function Killip
classification of patients, were collected. For the 1-year
postoperative follow-up, the follow-up was first conducted one
month after the end of treatment, and every three months
thereafter. Follow-up was conducted on an outpatient basis, by
telephone, or once through home visit, in order to collect patient
outcomes. Patients were grouped according to the outcome of the
follow-up period: Cured cases were assigned in the good prognosis
group, while patients at postoperative one year after the
occurrence of adverse cardiac events (myocardial infarction, heart
failure or malignant arrhythmia) and mortality cases were assigned
in the poor prognosis group.
In analyzing the LS, CS, RS and AS data of the two
groups at PCI 12 h, 2nd and 3rd day after operation, the STEMI
reperfusion criteria for risk assessment (4D-STI system) was
established based on the myocardial dimensional strain from which
the relevant parameters were screened out. Patient risk factors
were summarized according to the respective statistical scores in
the 4D-STI and TIMI risk score systems, and patients were
classified according to their scores: Low-, middle- and high-risk
groups. The TIMI system risk score criteria are presented in
Table I.
 | Table I.The TIMI system risk score
criteria. |
Table I.
The TIMI system risk score
criteria.
| Risk factors | Score | Grade |
|---|
| 65–74 years | 2 points |
|
| ≥75 years | 3 points |
|
| Systolic blood
pressure <100 mmHg | 3 points |
|
| Heart rate >100
beats/min | 2 points |
|
| Heart function
(Killip classification) class II–IV | 3 points | 7–14 points high risk
4–6 points middle risk |
| Anterior wall ST
segment elevation | 1 points | 0–3 points low
risk |
| History of
diabetes/hypertension/angina anterior wall ST-segment
elevation | 1 points |
|
| Female | 1 points |
|
| Onset to reperfusion
time >4 h | 1 points |
|
Statistical analysis
SPSS 19.0 statistical software (SPSS, Inc., Chicago,
IL, USA) was used for statistical analysis. Myocardial
four-dimensional strain indicators (LS, CS, RS and AS) were
expressed as (x ± SD), and compared between the two groups by using
t-test. The ROC curve analysis was drawn, and patient prognosis
related to the myocardial four-dimensional strain for STEMI after
reperfusion treatment was evaluated to determine the effects of
poor prognosis and the cutoff points. In the 4D-STI and TIMI risk
score system, the multiple group comparisons of the adverse cardiac
events and incidence of death in the low-, middle- and high-risk
groups were compared by using the χ2 test or Fishers
exact test. The post hoc test was performed using χ2
test or Fishers exact test as well. The area under the ROC curve
was used to evaluate the 4D-STI and TIMI system, and determine its
effectiveness in predicting poor prognosis and mortality. P<0.05
was considered to indicate a statistically significant
difference.
Results
Comparison of myocardial
four-dimensional strain indicators at 12 h, 2nd and 3rd day after
operation between the good prognosis and poor prognosis groups
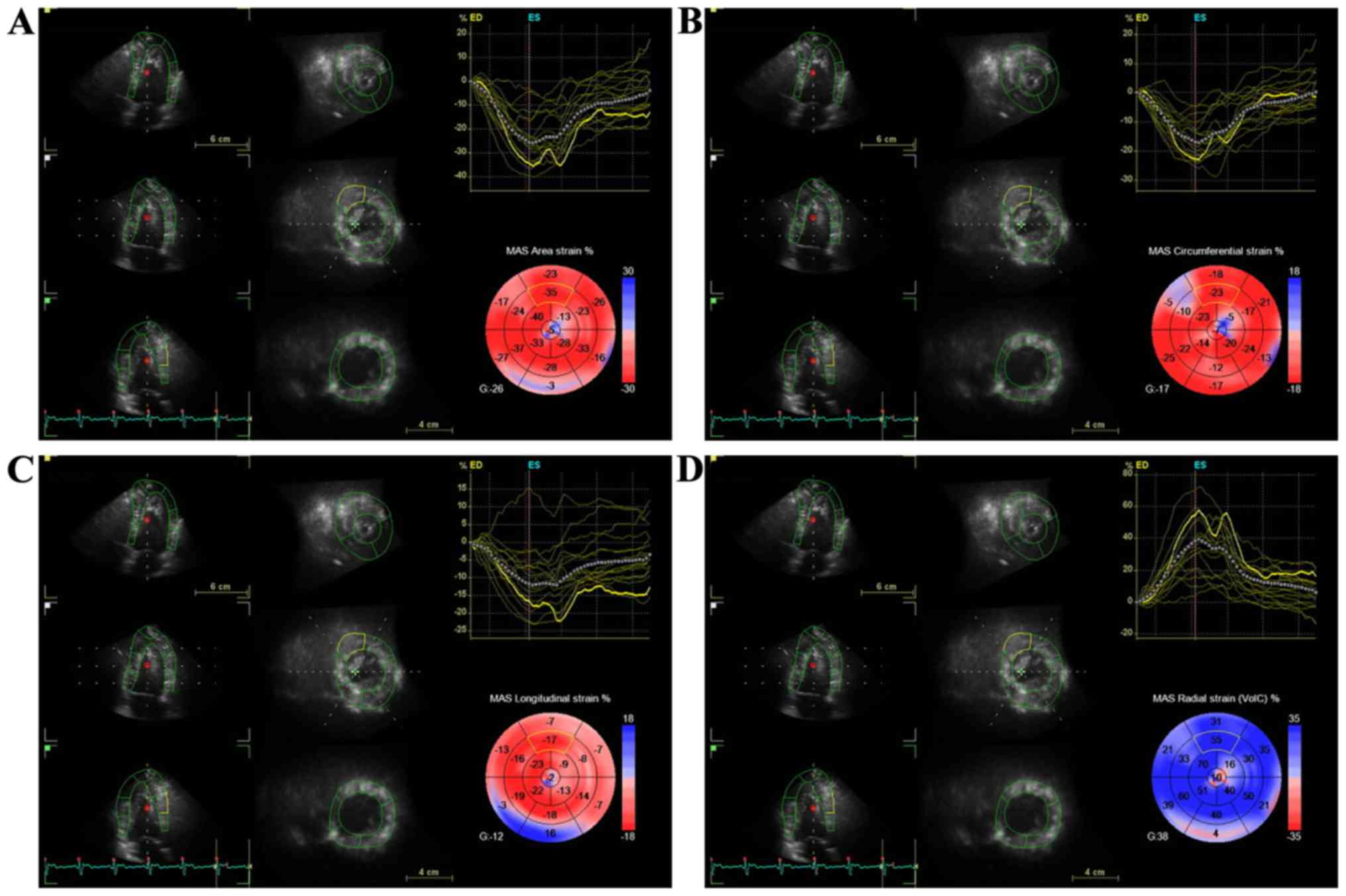
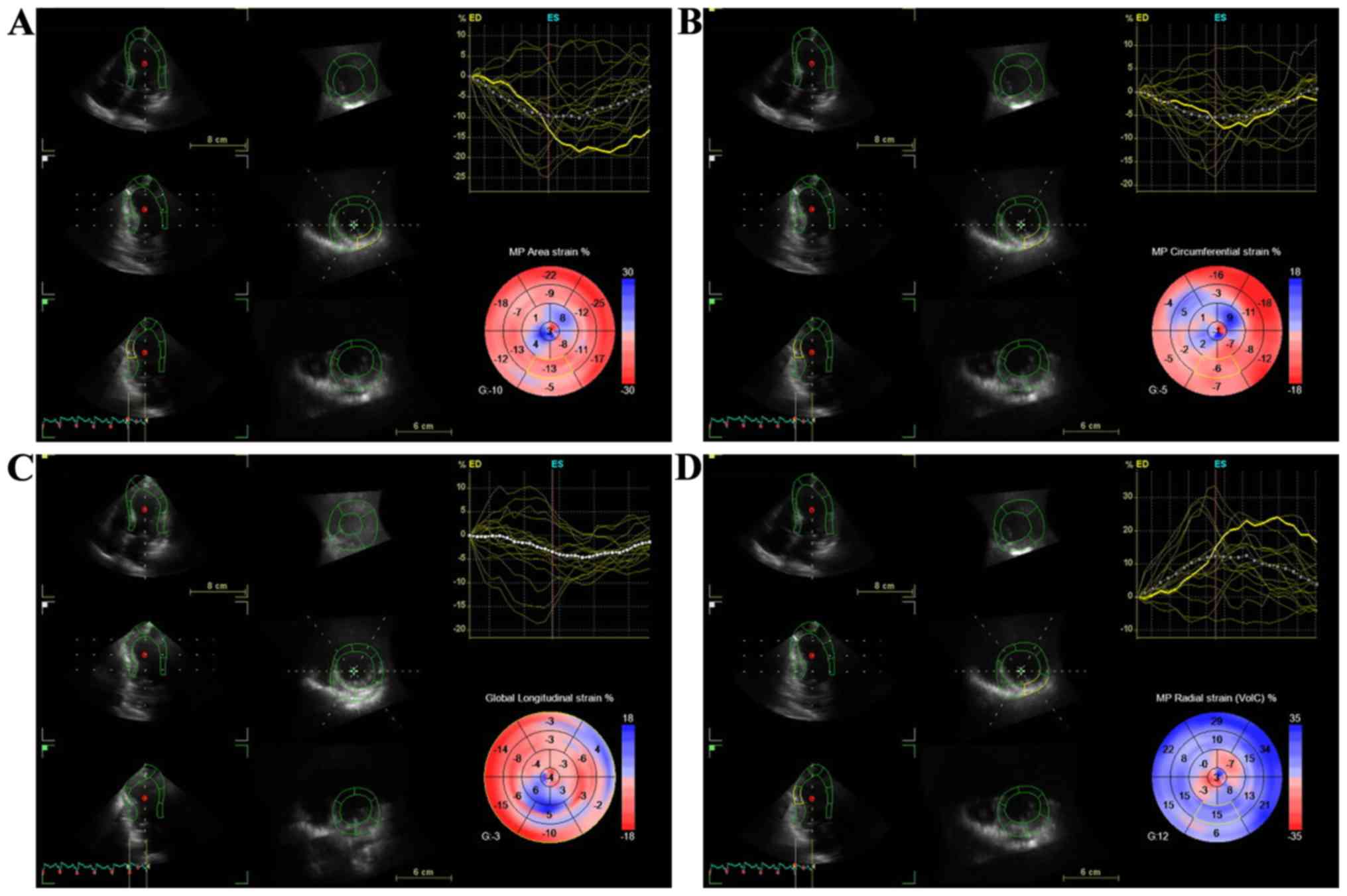
In the present study, the four-dimensional
myocardial strain indicators (AS, LS, CS and RS) of the three
observation points were detected in 120 patients with STEMI within
72 h after reperfusion through the successful application of 4D-STI
(Figs. 1 and 2). The AS, LS, CS and RS absolute values in
the poor prognosis group were significantly lower than those in the
good prognosis group at 12 h, 2nd and 3rd day after reperfusion
treatment, and the difference was statistically significant
(P<0.05; Tables II–IV).
 | Table II.Comparison of the four-dimensional
myocardial strain indicators between the two groups at
postoperative 12 h. |
Table II.
Comparison of the four-dimensional
myocardial strain indicators between the two groups at
postoperative 12 h.
| Groups | AS | LS | CS | RS |
|---|
| Good prognosis
(n=50) | −22.451±5.443 | −12.557±3.228 | −13.009±4.072 | 33.806±7.001 |
| Poor prognosis
(n=70) | −17.677±5.372 | −9.761±3.290 | −11.498±4.036 | 26.525±7.619 |
| P-value | <0.001 | <0.001 | 0.046 | <0.001 |
| t-test | −4.773 | −4.626 | −2.014 | 5.336 |
 | Table IV.Comparison of the four-dimensional
myocardial strain indicators between the two groups at 3rd day. |
Table IV.
Comparison of the four-dimensional
myocardial strain indicators between the two groups at 3rd day.
| Groups | AS | LS | CS | RS |
|---|
| Good prognosis
(n=50) | −23.593±5.756 | −11.372±3.705 | −12.963±3.642 | 36.379±9.901 |
| Poor prognosis
(n=70) | −18.479±5.719 | −9.622±3.296 | −11.134±3.617 | 27.475±9.511 |
| P-value | <0.001 | 0.007 | 0.007 | <0.001 |
| t-test | −4.798 | −2.722 | −2.723 | 4.970 |
Comparison of the ability of the
myocardial four-dimensional strain to evaluate the prognosis of
patients at 12 h, 2nd and 3rd day after operation
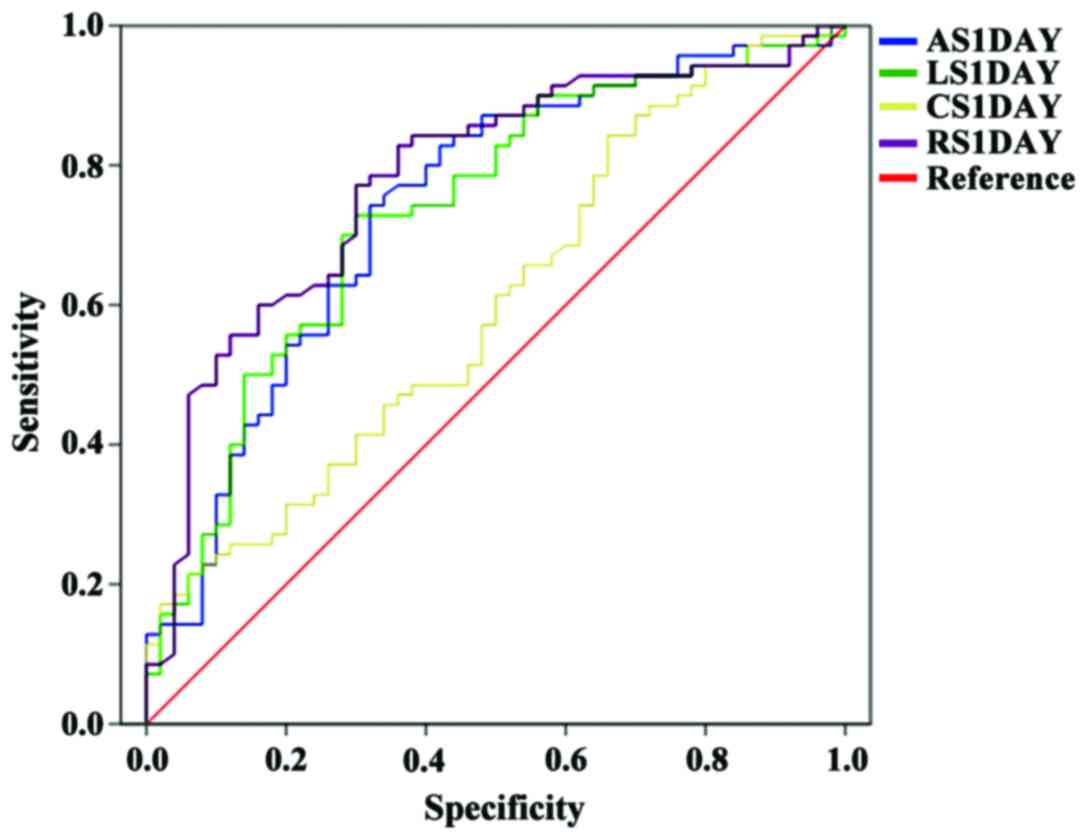
The area under the ROC curve of AS, LS and RS within
12 h after reperfusion was 0.740, 0.735 and 0.781, respectively;
the cutoff points were ≥-20.716, ≥11.285 and ≤30.902, respectively;
the sensitivity to predict poor prognosis was 74.3, 72.9 and 77.1%,
respectively; the specificity to predict poor prognosis was 68.0,
70.0 and 70.0%, respectively. The area under the ROC curve of AS
and RS on 2nd day was 0.785 and 0.765, respectively; the cutoff
points were ≥18.060 and ≤28.420, respectively; the sensitivity to
predict poor prognosis was 68.6 and 71.4%, respectively; the
specificity to predict poor prognosis was 80.0 and 80.0%,
respectively. The area under the ROC curve of AS and RS on 3rd day
was 0.742 and 0.743, respectively; the cutoff points were ≥-21.298
and ≤32.236, respectively; the sensitivity to predict poor
prognosis was 68.6 and 72.9%, respectively; the specificity to
predict poor prognosis was 76.0 and 66.0%, respectively (Figs. 3–5).
In the ROC analysis, the area under the ROC curve
was between 0.735 and 0.785 for AS, LS and RS at postoperative 12
h, AS and RS at 2nd day, and AS and RS at 3rd day. The assessments
of the prognosis of patients were similar. Hence, the set impact
factor score was equal. With reference to the TIMI risk score,
according to the cutoff points of these seven indicators and based
on the myocardial four-dimensional strain, the risk scoring system
for STEMI after reperfusion treatment was established (4D-STI
system; Table V).
 | Table V.4D-STI system risk score criteria. |
Table V.
4D-STI system risk score criteria.
| Risk factors | Score | Grade |
|---|
| AS (1 day)
≥-20.716 | 2 points |
|
| AS (1 day)
<-20.716 | 0 point |
|
| LS (1 day)
≥-11.285 | 2 points |
|
| LS (1 day)
<-11.285 | 0 point |
|
| RS (1 day)
≤30.902 | 2 points |
|
| RS (1 day)
>30.902 | 0 point | 0–4 points
low-risk |
| AS (2 days)
≥-18.060 | 2 points | 6–8 points
medium-risk |
| AS (2 days)
<-18.060 | 0 point | 10–14 points
high-risk |
| RS (2 days)
≤28.420 | 2 points |
|
| RS (2 days)
>28.420 | 0 point |
|
| AS (3 days)
≥-21.298 | 2 points |
|
| AS (3 days)
<-21.298 | 0 point |
|
| RS (3 days)
≤32.236 | 2 points |
|
| RS (3 days)
>32.236 | 0 point |
|
Comparison of patient groups under the
4D-STI and TIMI risk score system
All patients were divided into three groups
according to 4D-STI and TIMI risk score system: Low-, medium- and
high-risk groups. Under the 4D-STI risk score system and TIMI risk
score system, the differences of the poor prognosis and mortality
rates in the three groups were statisticaly significant
(P<0.01). Under these two scoring systems, poor prognosis and
mortality were significantly higher in the high- and medium-risk
groups compared with the low-risk group. Compared to the
medium-risk group, poor prognosis and mortality in the high-risk
group also exhibited a significant increase. The differences were
statistically significant (P<0.01) (Table VI).
 | Table VI.Comparison of poor prognosis and
mortality among groups using the 4D-STI and TIMI risk score
system. |
Table VI.
Comparison of poor prognosis and
mortality among groups using the 4D-STI and TIMI risk score
system.
|
| 4D-STI risk score
system | TIMI risk score
system |
|---|
|
|
|
|
|---|
| Groups | Nο. of cases | Mortality (n/%) | Poor prognosis
(n/%) | Nο. of cases | Mortality (n/%) | Poor prognosis
(n/%) |
|---|
| Low risk | 41 | 0 | 8/19.51 | 37 | 0 | 11/29.73 |
| Medium risk | 54 | 1/1.85 |
37/68.52a | 60 | 2/3.33 |
40/66.67a |
| High risk | 25 |
6/24.00a,b | 25/100a,b | 23 |
5/21.74a,b |
19/82.61a,b |
Comparison of the efficacy of the
4D-STI and TIMI risk score system for predicting the poor prognosis
and mortality of patients
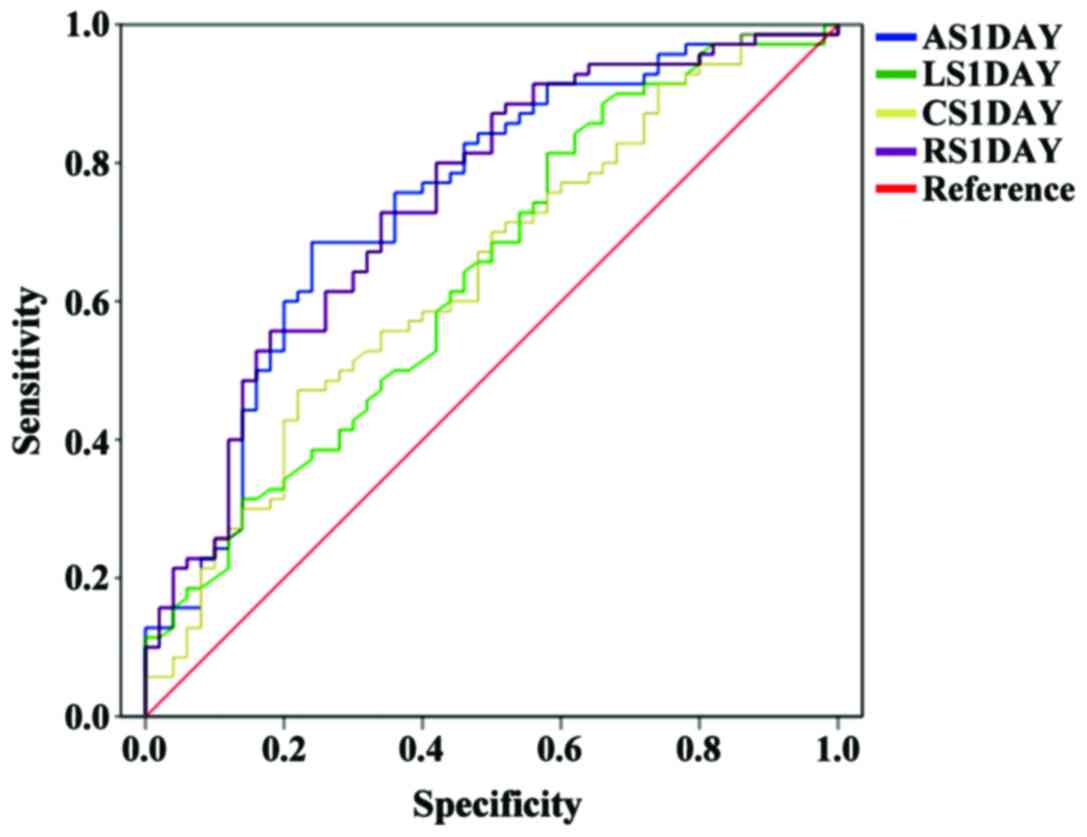
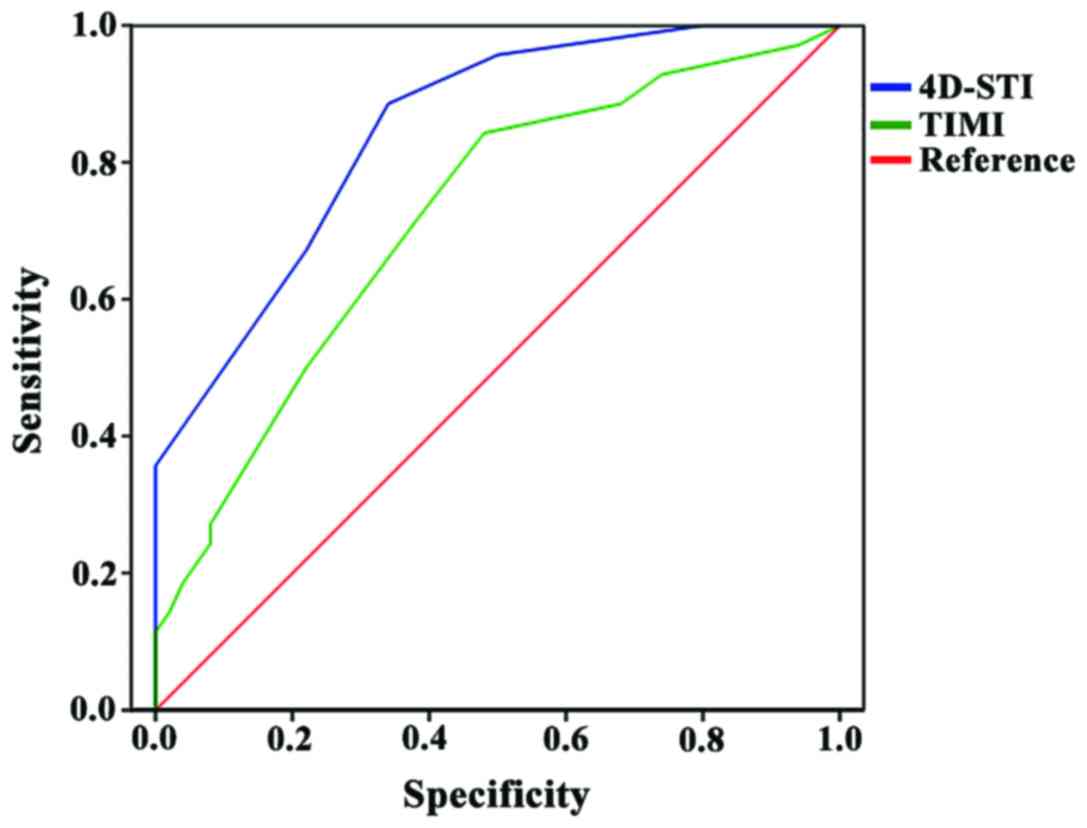
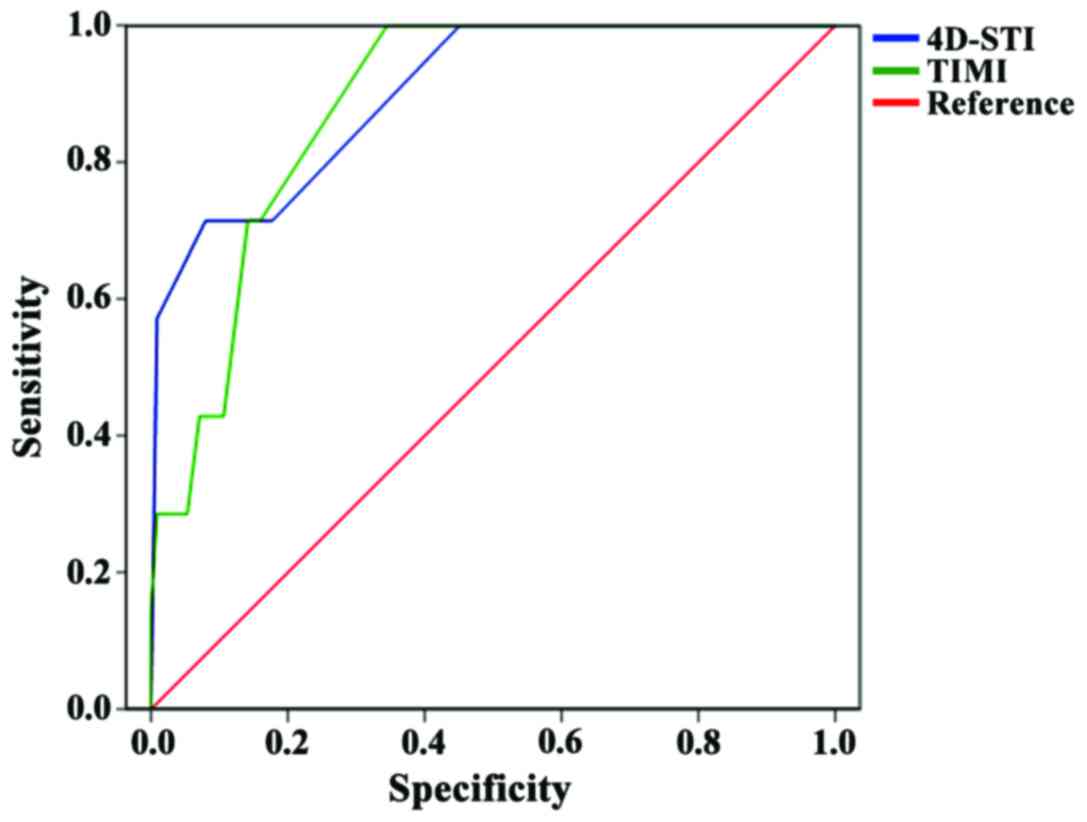
The corresponding ROC curve for the poor prognosis
and mortality of patients within one year after reperfusion
treatment based on the 4D-STI and TIMI risk score system is shown
in Figs. 6 and 7. Compared with the TIMI risk score system,
the corresponding area under the ROC curve based on the 4D-STI risk
score system was larger (0.848 vs. 0.720 and 0.901 vs. 0.883,
respectively).
Discussion
According to survey statistics, new cases of acute
ACS in China have reached nearly one million cases annually.
Furthermore, morbidity and mortality have increased year by year,
and long-term prognosis after treatment remains poor (5). Data indicate that mortality for ACS
patients at one year after onset is 15%, and increases to 25% at
three years after onset. At the same time, complications due to
disability have caused the quality of life of some patients to
rapidly decline (6). Although
reperfusion therapy has been widely implemented in hospitals to
significantly reduce patient mortality, the incidence of STEMI has
rapidly increased due to profound changes in diet and lifestyle.
However, clinical studies have shown that the possibility of
incomplete myocardial reperfusion after coronary recanalization can
reach as high as 37 to 43%. If not found in time, disease
progression would lead to complete myocardial necrosis, expanded
infarct size and ventricular remodeling, leading to heart failure,
increased risk of arrhythmia, and a 5–10 times increase in patient
mortality (7,8). In order to improve the prognosis of
patients, researchers have continuously worked to establish a score
system that can objectively reflect the risk factors of malignant
heart events after reperfusion treatment, which could assist
physicians in determining a timely and accurate case-based
reasonable and effective treatment program, and reduce the
occurrence of poor prognosis.
Establishment of the myocardial four-dimensional
strain 4D-STI risk score system using 4D-STI. The study conducted
by Szymczyk et al (9)
suggests that two-dimensional ultrasound speckle tracking imaging
can effectively evaluate the degree of structural and functional
repair of the damaged myocardium in STEMI cases. In addition,
4D-STI has become an emerging assessment method for wall motion
abnormalities in recent years, and is the extended application of
two-dimensional echocardiography. It overcomes the shortcoming of
not being able to fully detect changes in myocardial motion in a
single section, allows the overall analysis of the local myocardial
strain and strain rate to be achieved, and provides a more
objective and accurate evaluation of the myocardial systolic and
diastolic function (10,11). In the present study, 4D-STI was
applied to determine the four-dimensional myocardial strain
indicators of the three observation points of STEMI patients within
72 h after reperfusion treatment, and it was found that the AS, CS,
LS and RS absolute values of patients with poor prognosis were
lower than those in patients with good prognosis. This is because
STEMI causes the patient's heart blood supply to throttle, impairs
heart muscle elasticity and reduces compliance, causing
difficulties in cardiac wall motion performance, and resulting in
decreased myocardial response (12,13). The
difference in the four-dimensional echocardiographic data between
the two groups can be presumed or applied to the relevant
four-dimensional myocardial strain indicators to predict the
prognosis of STEMI patients after reperfusion treatment. Further
research revealed that AS, LS and RS within 12 h after reperfusion
therapy, AS and RS at 2nd and 3rd day had a certain degree of
prediction accuracy for STEMI patients with poor prognosis after
surgery. Furthermore, the area under the ROC curve was between
0.735 and 0.785, suggesting that the seven indicators for
evaluating the prognosis of patients were similar. Thus, the 4D-STI
risk score system was established based on the myocardial
four-dimensional strain to predict the prognosis of STEMI after
reperfusion treatment.
Comparison of the prognostic values of the 4D-STI
and TIMI risk score system. At present, the TIMI risk score is the
most commonly used means to assess acute ACS prognosis in clinic,
which is a summary of 15,000 cases of STEMI patients who underwent
thrombolytic therapy, including historical data, hemodynamic
parameters, electrocardiogram indicators, and clinical treatment
and development. A number of studies have confirmed that TIMI
scores are closely correlated with acute ACS cases, and have a good
correlation with the long-term prognosis of the incidence of
adverse events (14,15). In the present study, in the 4D-STI
and TIMI risk score system, as the risk assessment score increased,
the probability of occurrence of deaths and poor prognosis were
substantially increased in the high- and low-risk groups. In the
medium- and high-risk groups, mortality and poor prognosis were
significantly different, clearly demonstrating that the indicative
prognostic value of the 4D-STI and TIMI risk score system for STEMI
patients was the same. Moreover, compared to the TIMI risk score,
the 4D-STI system for patients with poor prognosis and mortality
under the ROC curve area was greater, showing the application of
the 4D-STI score and its stratification allows the determination of
the prognosis of the outcome to have higher accuracy. Presumably,
the reason may be as follows: i) The four-dimensional myocardial
strain indicators can be measured by 17 segments of the myocardial
dysplasia distribution, and the proportion of unfavorable areas of
the microcirculation to the total myocardium is the most intuitive
reflection of myocardial segment activity; and ii) the TIMI system
provides a comprehensive reference for the clinical risk factors of
patients. However, in the score of evaluation factors such as
history of chronic diseases and other health concerns by patient
awareness, the medical level of residence has a huge impact, and
errors may exist in the information.
In the present study, the predictive effect of the
four-dimensional myocardial strain indicators was only able to
determine the one year prognosis of patients within 72 h after
reperfusion treatment, and the number of research samples was
small. On this basis, it is expected to further expand the number
of samples, increase the frequency of myocardial four-dimensional
strain measurements, and conduct in-depth study on the prognostic
significance of the various stages of AS, CS, LS and RS, while
extending follow-up time, in order to further study the predictive
value of four-dimensional echocardiography long-term prognosis.
In conclusion, four-dimensional echocardiography can
better evaluate the prognosis of STEMI patients after reperfusion.
AS, LS and RS at postoperative 12 h, AS and RS at 2nd and 3rd day
has a certain predictive value for poor prognosis after reperfusion
therapy. The predictive efficacy of the risk stratification of
STEMI after reperfusion treatment based on the established
myocardial four-dimensional strain on poor prognosis and mortality
was superior to the TIMI risk score. The 4D-STI score is expected
to be the most sensitive and easy to operate prognostic indicator
to improve the prognosis of patients in clinical management.
Acknowledgements
Not applicable.
Funding
The study was financed by Medical Guidance Project
of Shanghai Municipal Science and Technology Commission
(134119b2300); and Research Project of Shanghai Municipal Health
and Family Planning Commission (21440589).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
YW and JZ conceived and designed the study, and
finally approved the manuscript. RX and XY collected the patient
data. JW and LF were responsible for the analysis and
interpretation of the data. YW drafted and revised the manuscript
critically for important intellectual content. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
This study was approved by the Ethics Committee of
Shanghai Jiading Center Hospital (Shanghai, China). Signed informed
consents were obtained from the patients or guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Abbasnezhad M, Soleimanpour H, Sasaie M,
Golzari SE, Safari S, Soleimanpour M and Esfanjani Mehdizadeh R:
Comparison of prediction between TIMI (thrombolysis in myocardial
infarction) risk score and modified TIMI risk score in discharged
patients from Emergency Department with atypical chest pain. Iran
Red Crescent Med J. 16:e139382014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Correia LCL, Garcia G, Kalil F, Ferreira
F, Carvalhal M, Oliveira R, Silva A, Vasconcelos I, Henri C and
Noya-Rabelo M: Prognostic value of TIMI score versus GRACE score in
ST-segment elevation myocardial infarction. Arq Bras Cardiol.
103:98–106. 2014.PubMed/NCBI
|
|
3
|
Yeh YT, Liu CW, Li AH, Ke SR, Liu YH, Chen
KC, Liao PC and Wu YW: Rapid early triage by Leukocytosis and the
thrombolysis in myocardial infarction (TIMI) risk score for
ST-elevation myocardial infarction undergoing primary percutaneous
coronary intervention: An observational study. Medicine
(Baltimore). 95:e28572016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Worner F, Cequier A, Bardají A, Bodí V,
Bover R, Martínez-Sellés M, Sabaté M, Sionis A, de Prada Vázquez
JA, Arós F, et al: Spanish Society of Cardiology Working Group on
the Clinical Practice Guidelines for ST-Elevation Acute Coronary
Syndrome; Group of Expert Reviewers for the Clinical Practice
Guidelines for ST-Elevation Acute Coronary Syndrome; Spanish
Society of Cardiology Clinical Practice Guidelines Committee:
Comments on the ESC guidelines for the management of acute
myocardial infarction in patients presenting with ST-segment
elevation. Rev Esp Cardiol (Engl Ed). 66:5–11. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Cheng TO and Zhao D: Current practice on
the management of acute coronary syndrome in China. Int J Cardiol.
169:1–6. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Karabinos I, Grassos C, Kostaki P and
Kranidis A: Echocardiography in the evaluation of a hypertensive
patient: An invaluable tool or simply following the routine?
Hellenic J Cardiol. 54:47–57. 2013.PubMed/NCBI
|
|
7
|
Na JP, Shin KC, Kim S, Park YS, Chung SP,
Park IC, Park JM and Kim MJ: Performance of reperfusion therapy and
hospital mortality in ST-elevation myocardial infarction patients
with non-chest pain complaints. Yonsei Med J. 55:617–624. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Singh V and Cohen MG: Therapy in
ST-elevation myocardial infarction: Reperfusion strategies,
pharmacology and stent selection. Curr Treat Options Cardiovasc
Med. 16:3022014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Szymczyk E, Lipiec P, Michalski B,
Szymczyk K, Shim A, Woźniakowski B, Rotkiewicz A, Stefańczyk L and
Kasprzak JD: 2D speckle tracking echocardiography for the
assessment of regional contractile reserve after myocardial
infarction. J Cardiovasc Med (Hagerstown). 17:374–381. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Abduch MC, Alencar AM, Mathias W Jr and
Vieira ML: Cardiac mechanics evaluated by speckle tracking
echocardiography. Arq Bras Cardiol. 102:403–412. 2014.PubMed/NCBI
|
|
11
|
Reant P, Barbot L, Touche C, Dijos M,
Arsac F, Pillois X, Landelle M, Roudaut R and Lafitte S: Evaluation
of global left ventricular systolic function using
three-dimensional echocardiography speckle-tracking strain
parameters. J Am Soc Echocardiogr. 25:68–79. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kilickesmez Orta K, Baydar O, Bostan C,
Coskun U and Kucukoglu S: Four-dimensional speckle tracking
echocardiography in patients with hypertrophic cardiomyopathy.
Echocardiography. 32:1547–1553. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Smith BC, Dobson G, Dawson D,
Charalampopoulos A, Grapsa J and Nihoyannopoulos P:
Three-dimensional speckle tracking of the right ventricle: Toward
optimal quantification of right ventricular dysfunction in
pulmonary hypertension. J Am Coll Cardiol. 64:41–51. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Popovic B, Girerd N, Rossignol P, Agrinier
N, Camenzind E, Fay R, Pitt B and Zannad F: Prognostic value of the
thrombolysis in myocardial infarction risk score in ST-elevation
myocardial infarction patients with left ventricular dysfunction
(from the EPHESUS Trial). Am J Cardiol. 118:1442–1447. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Feder SL, Schulman-Green D, Geda M,
Williams K, Dodson JA, Nanna MG, Allore HG, Murphy TE, Tinetti ME,
Gill TM, et al: Physicians' perceptions of the thrombolysis in
myocardial infarction (TIMI) risk score in older adults with acute
myocardial infarction. Heart Lung. 44:376–381. 2015. View Article : Google Scholar : PubMed/NCBI
|