Introduction
Valvular heart disease is one of the most common
types of heart disease in the clinic, of which mitral valve disease
appears most frequently. Due to the long-term abnormality of blood
flow, low body immunity and malnutrition easily occurs making
corporeity of patients susceptible (1,2). Heart
valve replacement is the main surgical mode in the treatment of
valvular heart disease at present with a significant effect, which
saves lives and improves the quality of life (2,3).
However, valve replacement must be performed under specific
hypothermic cardiopulmonary bypass conditions, which are severe and
time-consuming, involving operations of invasive and allogeneic
implantation; it severely impairs the patient's immune system, and
incurs various infections after operation, of which pulmonary
infection is particularly significant, thus aggravating
cardiopulmonary circulating load, and leading to prolonged
hospitalization, increased hospital costs, and even danger to the
lives of patients, seriously affecting the patient's surgical
outcome and prognosis (4).
Metabolic syndrome (MS) is a multiple metabolic
disorder mainly involving obesity, hyperinsulinemia, hyperglycemia,
dyslipidemia and hypertension, and it is a disease closely related
to cardiovascular diseases. The risk of coronary heart disease in
patients with MS is increased 3-fold, cardiovascular mortality
increased 2-fold, and the risk of total mortality increased
1.5-fold (5). The characteristics of
pulmonary infection after mitral valve repair in patients with MS
are rarely reported.
The aim of the current study was to investigate the
characteristics of pulmonary infection after mitral valve repair in
patients with MS and its relationship with blood pressure, blood
glucose, blood lipid and other factors, and to take targeted
measures to provide reference for reducing the incidence of
pulmonary infection.
Materials and methods
Clinical data
The complete clinical data of 126 patients
undergoing mitral valve replacement from March 2013 to February
2015 in Luoyang Center Hospital Affiliated to Zhengzhou University
(Luoyang, China) were retrospectively analyzed, including 45 males
and 81 females, with an average age of (47.12±6.98) years. Valve
replacement was performed among patients under intravenous combined
anesthesia and hypothermic cardiopulmonary bypass. The clinical
data of all the patients are shown in Table I. Diagnostic criteria for pulmonary
infection (6) were in accordance
with the standards formulated by the Centers for Disease Control
and Prevention (Atlanta, GA, USA). The patients were divided into
the infection group (n=19) and non-infection group (n=107)
according to whether pulmonary infection occurred. The diagnosis of
MS is based on the recommendations of the Diabetes Branch of
Chinese Medical Association (Beijing, China) on MS (7).
 | Table I.Clinical data of 126 patients
undergoing mitral valve replacement. |
Table I.
Clinical data of 126 patients
undergoing mitral valve replacement.
| Item | Case (n) | Constituent ratio
(%) |
|---|
| Type of heart
disease |
|
|
| Rheumatic
heart disease | 112 | 88.89 |
|
Congenital heart disease | 9 | 7.14 |
| Valvular
degeneration | 5 | 3.97 |
| Cardiac function
(grade) |
|
|
| I | 5 | 3.97 |
| II | 25 | 19.84 |
| III | 83 | 65.87 |
| IV | 13 | 10.32 |
The present study was approved by the Ethics
Committee of the Affiliated Hospital of Hebei University (Baoding,
China), and the Ethics Committee of Luoyang Center Hospital
Affiliated to Zhengzhou University (Luoyang, China). Written
informed consents were signed by the patients or guardians.
Methods
Measurement of physiological
indexes
The clinical data of all the patients were recorded,
including age, sex, type of heart disease and cardiac function
classification. Patients were weighed at fasting and with unlined
clothes, and the height was measured. Each index was measured two
times and averaged. Body mass index (BMI) = body
weight/height2. Blood pressure of brachial artery in the
right upper extremity was measured (using mercury sphygmomanometer)
after patients rested quietly for 15 min, and the average was taken
from the values of three times of blood pressure.
Detection of serological indexes
Fasting anterior cubital vein blood (5 ml) was
extracted from patients the next day in the morning, followed by
anticoagulation, centrifugation at 3,000 × g at 4°C for 15 min and
refrigeration at 4°C, in preparation for the testing. The fasting
blood glucose (FBG), triglyceride (TG), total cholesterol (TC),
high-density lipoprotein cholesterol (HDL-C) and low-density
lipoprotein cholesterol (LDL-C) were detected by enzyme method.
Blood (2 ml) was collected from patients under the strict aseptic
operation, and sent to the clinical laboratory of the hospital,
followed by culture and identification of bacteria by specialized
staff.
Statistical analysis
Data were analyzed by Statistical Product and
Service Solutions 18.0 software (SPSS, Inc., Chicago, IL, USA). The
measurement data conforming to normal distribution were expressed
as (mean ± SD), and statistically analyzed by t-test and chi-square
test. Univariate and multivariate logistic regression analyses were
used to analyze the risk factors and independent risk factors of
pulmonary infection after mitral valve repair in patients with MS.
P<0.05 was considered to indicate a statistically significant
difference.
Results
Pulmonary infection and comparison of
metabolic indexes in patients between the two groups
There were 19 cases with pulmonary infection, and
the infection rate was 15.08% (19/126). The remaining 107 patients
were in the non-infection group. The BMI, blood pressure, FBG, TG,
TC, LDL-C in the infection group were higher than those in the
non-infection group, and HDL-C was lower in the infection group
than that in the non-infection group. The differences were
statistically significant (p<0.05) (Table II).
 | Table II.Comparison of metabolic indexes in
patients between the two groups. |
Table II.
Comparison of metabolic indexes in
patients between the two groups.
| Index | Non-infection group
(n=107) | Infection group
(n=19) | t-value | P-value |
|---|
| Age (years) | 47.31±6.87 | 47.02±7.14 | 0.14 | 0.09 |
| BMI
(kg/m2) | 22.12±2.98 | 24.90±4.86 | 4.16 | 0.01 |
| Systolic pressure
(mmHg) | 110.23±21.14 | 119.47±12.63 | 2.25 | 0.04 |
| Diastolic pressure
(mmHg) | 65.57±13.70 | 75.58±11.27 | 2.98 | 0.03 |
| FBG (mmol/l) | 4.96±1.32 | 6.19±2.36 | 2.36 | 0.04 |
| TG (mmol/l) | 1.08±1.01 | 1.86±1.34 | 4.10 | 0.01 |
| TC (mmol/l) | 4.19±0.13 | 5.24±0.70 | 2.32 | 0.04 |
| LDL-C (mmol/l) | 3.40±0.56 | 3.93±1.42 | 3.45 | 0.02 |
| HDL-C (mmol/l) | 1.02±0.35 | 1.35±0.41 | 3.09 | 0.03 |
Relationship between MS and pulmonary
infection
Of the 126 patients studied, 24 were complicated
with MS, 10 of whom had pulmonary infection, with an infection rate
of 41.67%. Of the 102 cases without MS, 9 cases had pulmonary
infection, and the infection rate was 8.82%. The difference was
statistically significant (p<0.05) (Table III).
 | Table III.Relationship between MS and pulmonary
infection. |
Table III.
Relationship between MS and pulmonary
infection.
| Group | Pulmonary infection
(n) | Constituent ratio
(%) | χ2 | P-value |
|---|
| MS (n=24) | 10 | 41.67 | 9.54 | <0.001 |
| Non-MS (n=102) | 9 | 8.82 |
|
|
Characteristics of pathogenic bacteria
in pulmonary infection
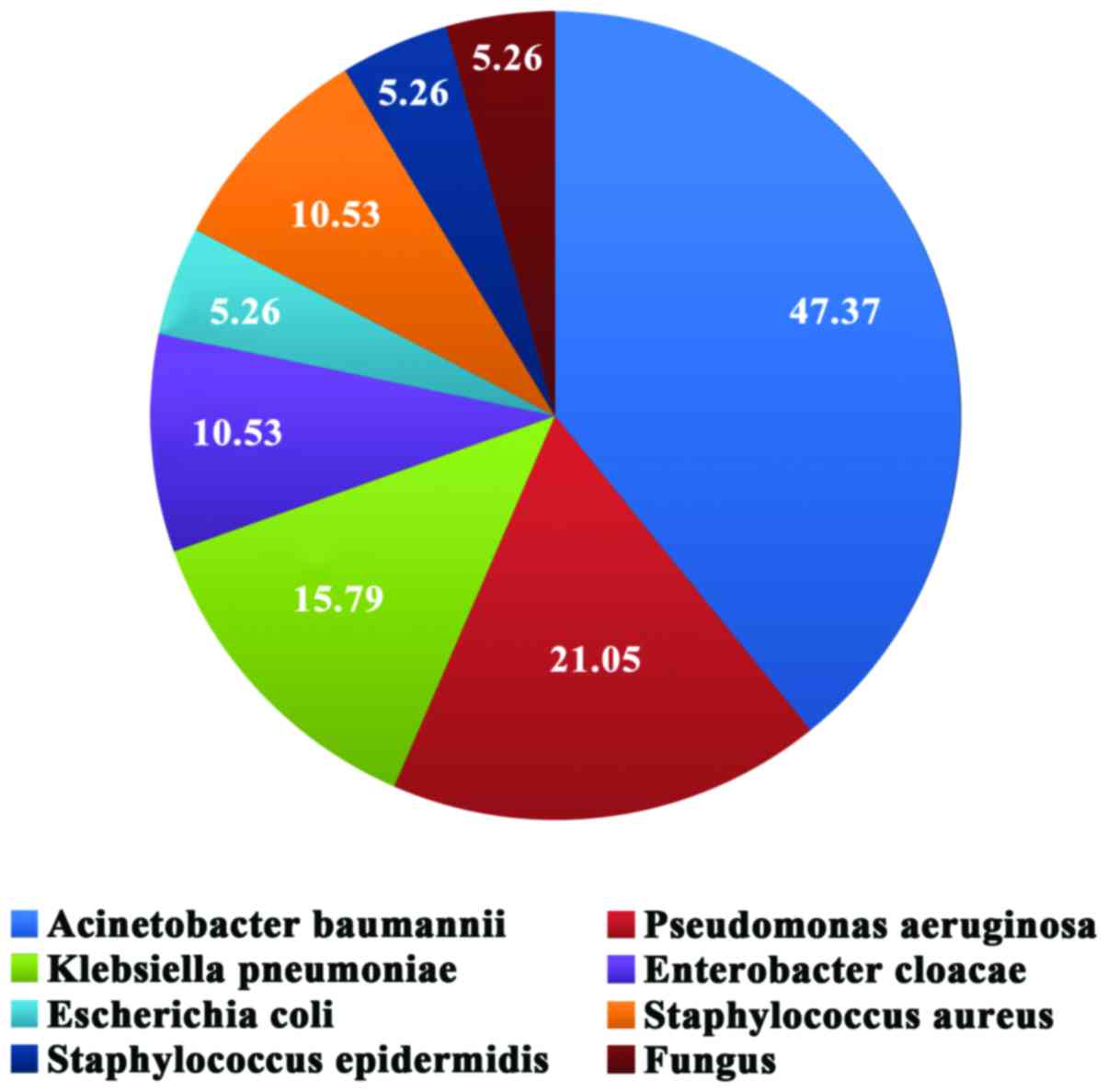
By analyzing the blood samples of 19 mitral valve
replacement patients with pulmonary infection and positive
bacteriology, it was found that each specimen was detected with a
single strain. Among them, 14 strains were gram-negative bacteria,
accounting for 73.68%, including 9 strains of Acinetobacter
baumannii (47.37%), 4 strains of Pseudomonas aeruginosa
(21.05%), 3 strains of Klebsiella pneumoniae (15.79%), 2
strains of Enterobacter cloacae (10.53%) and 1 strain of
Escherichia coli (5.26%); there were 3 strains of
gram-positive bacteria, including 2 strains of Staphylococcus
aureus (10.53%), 1 strain of Staphylococcus epidermidis
(5.26%) and 1 strain of fungus (5.26%) (Fig. 1).
Analysis of pulmonary infection
factors
Among patients between the non-infection group and
the infection group, left ventricular ejection fraction (LVEF)
(56.23±13.10) vs. (44.14±12.16%), extubation time of trachea
cannula: (23.98±6.37) vs. (29.60±6.85) h, ventilator use time:
(11.21±4.35) vs. (17.01±5.52) h, suggesting that the LVEF value was
distinctly lower in patients of infection group than that of
non-infection group, extubation time of trachea cannula in
infection group was markedly longer than that in non-infection
group, and the differences were statistically significant
(p<0.05) (Table IV). Among
patients between non-infection group and infection group: Sternal
dehiscence rate: 5.61 vs. 21.05%, rethoracotomy hemostasis rate:
1.87 vs. 10.53%, incidence of low-cardiac-output syndrome: 2.80 vs.
10.53%, indicating that the incidence rates of sternal dehiscence,
rethoracotomy hemostasis and low-cardiac-output syndrome were
obviously higher in infection group than those in non-infection
group, and the differences were statistically significant
(p<0.05) (Table V). Univariate
analysis of risk factors for pulmonary infection was performed. The
univariate analysis revealed that cardiac function, BMI, FBG, TG,
LDL-C, HDL-C, LVEF value, extubation time of trachea cannula,
ventilator use time, sternal dehiscence, rethoracotomy hemostasis
and low-cardiac-output syndrome were risk factors for pulmonary
infection after mitral valve repair in patients with MS (Table VI).
 | Table IV.Analysis of pulmonary infection
factors. |
Table IV.
Analysis of pulmonary infection
factors.
| Factor | Non-infection group
(n=107) | Infection group
(n=19) | t-value | P-value |
|---|
| LVEF (%) | 56.23±13.10 | 44.14±12.16 | 6.45 | <0.001 |
| Extubation time of
trachea cannula (h) | 23.98±6.37 | 29.60±6.85 | 8.17 | <0.001 |
| Ventilator use time
(h) | 11.21±4.35 | 17.01±5.52 | 5.83 | <0.001 |
 | Table V.Analysis of pulmonary infection
factors. |
Table V.
Analysis of pulmonary infection
factors.
|
| Non-infection group
(n=107) | Infection group
(n=19) |
|
|
|---|
|
|
|
|
|
|
|---|
| Factor | Case | Incidence rate | Case | Incidence rate | χ2 | P-value |
|---|
| Sternal
dehiscence | 6 | 5.61 | 4 | 21.05 | 5.75 | 0.01 |
| Rethoracotomy
hemostasis | 2 | 1.87 | 2 | 10.53 | 6.53 | <0.001 |
| Low-cardiac-output
syndrome | 3 | 2.80 | 2 | 10.53 | 4.84 | 0.02 |
 | Table VI.Univariate analysis of risk factors
for pulmonary infection. |
Table VI.
Univariate analysis of risk factors
for pulmonary infection.
| Risk factor | OR (95% CI) | P-value |
|---|
| Age (years) | 1.104
(1.007–1.068) | >0.05 |
| Type of heart
disease | 1.001
(0.958–0.997) | >0.05 |
| Cardiac
function | 8.214
(0.812–8.738) | <0.05 |
| BMI | 20.137
(11.879–25.145) | <0.05 |
| Blood pressure | 0.962
(0.661–1.374) | >0.05 |
| FBG | 20.121
(11.476–26.769) | <0.05 |
| TG | 3.712
(2.196–6.321) | <0.05 |
| TC | 1.121
(0.715–1.474) | >0.05 |
| LDL-C | 12.741
(6.243–25.681) | <0.05 |
| HDL-C | 9.514
(5.576–15.901) | <0.05 |
| LVEF value | 14.016
(6.438–24.013) | <0.05 |
| Extubation time of
trachea cannula | 4.681
(3.359–6.124) | <0.05 |
| Ventilator use
time | 10.827
(7.109–16.032) | <0.05 |
| Sternal
dehiscence | 28.142
(12.365–33.248) | <0.05 |
| Rethoracotomy
hemostasis | 5.919
(2.586–13.215) | <0.05 |
| Low-cardiac-output
syndrome | 4.231
(2.057–8.243) | <0.05 |
Multivariate analysis of independent
risk factors for pulmonary infection
Multivariate logistic regression analysis on the
above risk factors revealed that 10 independent predictive risk
factors for pulmonary infection were cardiac function, BMI, FBG,
HDL-C, LVEF value, extubation time of trachea cannula, ventilator
use time, sternal dehiscence, rethoracotomy hemostasis and
low-cardiac-output syndrome (Table
VII).
 | Table VII.Multivariate analysis of independent
risk factors for pulmonary infection. |
Table VII.
Multivariate analysis of independent
risk factors for pulmonary infection.
| Risk factor | OR (95% CI) | P-value |
|---|
| Cardiac
function | 10.8
(4.9–13.6) | <0.05 |
| BMI | 3.9 (1.2–9.1) | <0.05 |
| FBG | 11.4
(6.1–16.3) | <0.05 |
| HDL-C | 4.6 (1.5–6.4) | <0.05 |
| LVEF | 25.1
(12.7–38.3) | <0.05 |
| Extubation time of
trachea cannula | 9.2 (4.2–14.1) | <0.05 |
| Ventilator use
time | 21.6
(10.2–28.2) | <0.05 |
| Sternal
dehiscence | 15.3
(7.2–20.4) | <0.05 |
| Rethoracotomy
hemostasis | 19.2
(9.7–24.5) | <0.05 |
| Low-cardiac-output
syndrome | 12.9
(6.1–15.9) | <0.05 |
Discussion
According to literature, the prevalence of pulmonary
infection after cardiac surgery is 2.80–15.30% (8), which is consistent with that of
pulmonary infection after mitral valve replacement reported in this
study (15.08%). Moreover, the incidence of pulmonary infection in
patients with MS is higher than that in patients without MS
(p<0.05). MS is a morbid state with multiple metabolic disorders
mainly involving obesity, hyperinsulinemia, hyperglycemia,
dyslipidemia and hypertension, and it is closely related to
cardiovascular disease (9).
Multivariate logistic regression analysis in this study revealed
that BMI, FBG and HDL-C are independent risk factors for pulmonary
infection after mitral valve repair in patients with MS. The study
indicated that obesity increases the alveolar arterial oxygen
difference in thoracic surgery, which leads to imbalance of
ventilation and blood flow, easily resulting in hyoxemia (10). In addition, given that it causes
difficulty in anesthesia intubation and large dosage of anesthetic
drug and easily complicated reflux esophagitis, it is regarded as a
risk factor of postoperative aspiration pulmonary infection. This
study demonstrated that BMI in the group of pulmonary infection
after mitral valve replacement was significantly higher than that
in the group without pulmonary infection (p<0.05). Another
important risk factor for postoperative infection of heart is
diabetes mellitus (11,12). If the patient has diabetes or liver
disease before operation, it is more likely to have limited glucose
utilization in the body and aggravate blood glucose; furthermore,
the increase of blood glucose also increases the incidence of
postoperative infection (13). This
study showed that FBG in the group of pulmonary infection after
mitral valve replacement was significantly higher than that in the
group without pulmonary infection (p<0.05). In plasma, the
binding of HDL-C with endotoxin has anti-endotoxemia effect
(14). This study also found that
HDL-C in the group with pulmonary infection after mitral valve
replacement was lower than that in the group without pulmonary
infection (p<0.05). Thus, with the decrease of HDL-C, the
anti-endotoxemia effect is weakened, and the infection easily
occurs. This study indicated that pulmonary infection easily occurs
in patients with MS after mitral valve replacement, so attention
should be paid to the risk of MS in clinical practice, and
emphasize the early prevention and treatment of MS.
With the development of modern medicine, the
curative effect of mitral valve replacement is beyond doubt.
However, the incidence of postoperative pulmonary infection is
still as high as 15.08% (19/126). Due to the different regions,
times and ages, and with the advent of new antibacterial drugs, a
large number of antibiotics are clinically abused, resulting in the
constant change in the species of pathogenic bacteria, which brings
difficulties to diagnosis and treatment. The majority of pathogenic
bacteria causing pulmonary infection are gram-negative bacteria
(73.68%) (14/19), the top three are 9 strains of Acinetobacter
baumannii (47.37%), 4 strains of Pseudomonas aeruginosa
(21.05%) and 3 strains of Klebsiella pneumoniae (15.79%).
This study showed that the extubation time of trachea cannula,
ventilator use time, rethoracotomy hemostasis rate, sternal
dehiscence rate and incidence of low-cardiac-output syndrome in
patients of pulmonary infection group were significantly higher
than those of non-infection group, but LVEF value was lower in the
infection group than that in the non-infection group, and the
differences were statistically significant (p<0.05).
Multivariate logistic regression analysis in this study revealed
that cardiac function, LVEF value, extubation time of trachea
cannula, ventilator use time, sternal dehiscence, rethoracotomy
hemostasis and low-cardiac-output syndrome were independent risk
factors for pulmonary infection after mitral valve repair in
patients with MS. Rethoracotomy hemostasis mostly belongs to
emergency surgery, of which the disinfection effect is poorer and
incomplete, which will cause more massive intrathoracic bleeding
and larger trauma, further reducing the immune function of
patients. In addition, allogeneic blood transfusion is needed for
severely ill patients, which increases the risk of infection
(15,16). On the one hand, sternal dehiscence
destroys the integrity of bony thorax; on the other hand, it
increases the pain time of patients, seriously affects the cough
and breathing of patients, causes weak cough and shallow and rapid
breathing, and hinders secretion discharge from the respiratory
tract (17). LVEF is an important
index to evaluate cardiac function, and cardiac function reduces
with the decrease of LVEF value (18). Once the left ventricular function is
abnormal, pulmonary edema or congestion can be induced, affecting
cardiac and pulmonary function. Therefore, the effective management
of LVEF before surgery will contribute to the prognosis and
rehabilitation of patients. Ventilator is necessary for assisted
breathing of patients after heart valve replacement; the
ventilator-associated complications, including respiratory tract
infection and pulmonary infection, can occur if the ventilator is
used improperly or over time (19).
On the one hand, the airway, which is open to the outside world,
loses its function of defense barrier; on the other hand, the
connecting pipes of ventilator are easily polluted, and the
purification degree of aspiration gas is low, leading to the
invasion and colonization of pathogenic bacteria into lung
incurring infection (20). The
airway mucosa of patients with long-term intubation is easily
damaged, plus the increase of secretions caused by foreign body
stimulation, can induce infection (21). During the operation, the use of acid
suppression agents reduces the secretion of gastric acid, and the
intestinal flora moves into the respiratory tract, which will cause
gram-negative bacilli to induce endogenous infection (22). After oral and tracheal intubation,
the oral self purification capacity under the semi-open state
decreases, leading to the excessive increase in oropharyngeal
bacteria, and it will enter the lower respiratory tract with the
invasive operation, thus incurring pulmonary infection (23). In order to obtain better surgical
effect, shorten the operation and hospitalization time (24–26), we
should pay attention to preoperative health education: i) To guide
the cough method and expectoration manipulation before operation is
conducive to the adequate and effective expectoration of patients
after operation; ii) to guide the standard use of ventilator is
helpful to prevent the occurrence of pulmonary infection; iii) to
emphasize the oral cleaning care, strengthen the basic nutritional
support and improve the patient's own state, are beneficial to
ameliorate the treatment and prognosis, thus promoting the
harmonious development of doctor-patient relationship.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets analyzed during the present study are
not publicly available due to the protection of patient privacy but
are available from the corresponding author on reasonable
request.
Authors' contributions
PX and WS collected the patient clinical information
and analyzed the data. PX wrote the manuscript and ZH helped with
detection of serological indexes. All authors read and approved the
final study.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of the Affiliated Hospital of Hebei University (Baoding,
China), and the Ethics Committee of Luoyang Center Hospital
Affiliated to Zhengzhou University (Luoyang, China). All the
patients provided written informed consent for publication.
Patient consent for publication
Not applicable.
Competing of interests
The authors declare that they have no competing
interests.
References
|
1
|
Blasi A, Muñoz G, de Soto I, Mellado R,
Taura P, Rios J, Balust J and Beltran J: Reliability of
thromboelastometry for detecting the safe coagulation threshold in
patients taking acenocoumarol after elective heart valve
replacement. Thromb Res. 136:669–672. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Weber B and Hoerstrup SP: The future of
heart valve replacement. Eur Heart J. 36:326–328. 2015.PubMed/NCBI
|
|
3
|
Zhang XW, Song ZG, Wang L, Lu FL, Zou LJ,
Xu JB and Xu ZY: The use of intra-aortic balloon pump in patients
undergoing heart valve replacement: Outcome and risk analysis. J
Heart Valve Dis. 23:458–462. 2014.PubMed/NCBI
|
|
4
|
Weimar T, Roser D, Liebrich M, Horke A,
Doll N and Hemmer WB: Strategies for biological heart valve
replacement: Stentless xenografts fail to evolve into an
alternative pulmonary valve substitute in a Ross procedure.
Biotechnol J. 8:345–351. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Eckle RH, Grundy SM and Zimmet PZ: The
metabolism syndrome. Lancet. 365:1415–1428. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Li DL, Dong PS, Du LJ, Li ZZ, Sh XY and
Fan XM: Analysis of related risk factors of pulmonary infection
after heart valve replacement. J Hosp Infect. 23:3908–3910.
2013.
|
|
7
|
Metabolic syndrome study group of Chinese
Diabetes Association. Recommendations of the Chinese Medical
Association Diabetes Branch on metabolic syndrome. Chin J Diabetes
Mellitus. 12:156–161. 2004.(In Chinese).
|
|
8
|
Riera M, Ibáñez J, Herrero J, Ignacio Sáez
De Ibarra J, Enríquez F, Campillo C and Bonnín O: Respiratory tract
infections after cardiac surgery: Impact on hospital morbidity and
mortality. J Cardiovasc Surg (Torino). 51:907–914. 2010.PubMed/NCBI
|
|
9
|
Salazar MR, Carbajal HA, Espeche WG,
Dulbecco CA, Aizpurúa M, Marillet AG, Echeverría RF and Reaven GM:
Relationships among insulin resistance, obesity, diagnosis of the
metabolic syndrome and cardio-metabolic risk. Diab Vasc Dis Res.
8:109–116. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Suemitsu R, Sakoguchi T, Morikawa K,
Yamaguchi M, Tanaka H and Takeo S: Effect of body mass index on
perioperative complications in thoracic surgery. Asian Cardiovasc
Thorac Ann. 16:463–467. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Lola I, Levidiotou S, Petrou A,
Arnaoutoglou H, Apostolakis E and Papadopoulos GS: Are there
independent predisposing factors for postoperative infections
following open heart surgery? J Cardiothorac Surg. 6:1512011.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Sato H, Carvalho G, Sato T, Lattermann R,
Matsukawa T and Schricker T: The association of preoperative
glycemic control, intraoperative insulin sensitivity, and outcomes
after cardiac surgery. J Clin Endocrinol Metab. 95:4338–4344. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Hu QG and Zheng QC: The influence of
enteral nutrition in postoperative patients with poor liver
function. World J Gastroenterol. 9:843–846. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Murphy AJ, Chin-Dusting JP, Sviridov D and
Woollard KJ: The anti inflammatory effects of high density
lipoproteins. Curr Med Chem. 16:667–675. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Habal P, Simek J and Stĕtina M: Improving
of treatment safety in emergency thoracic surgery. Rozhl Chir.
89:261–264. 2010.(In Czech). PubMed/NCBI
|
|
16
|
Zhang C, Gao J and He B: Analysis of
related factors of patientos undergoing cardiac valve replacement
complicated with pulmonary infection and nursing strategies of it.
Chin Nurs Res. 90:64–66. 2008.
|
|
17
|
Weimar T, Roser D, Liebrich M, Horke A,
Doll N and Hemmer WB: Strategies for biological heart valve
replacement: Stentless xenografts fail to evolve into an
alternative pulmonary valve substitute in a Ross procedure.
Biotechnol J. 8:345–351. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Bax JJ, Visser FC, Poldermans D, Elhendy
A, Cornel JH, Boersma E, Valkema R, Van Lingen A, Fioretti PM and
Visser CA: Relationship between preoperative viability and
postoperative improvement in LVEF and heart failure symptoms. J
Nucl Med. 42:79–86. 2001.PubMed/NCBI
|
|
19
|
Yang TH, Webb JG, Blanke P, Dvir D,
Hansson NC, Nørgaard BL, Thompson CR, Thomas M, Wendler O, Vahanian
A, et al: Incidence and severity of paravalvular aortic
regurgitation with multidetector computed tomography nominal area
oversizing or undersizing after transcatheter heart valve
replacement with the Sapien 3: A comparison with the Sapien XT.
JACC Cardiovasc Interv. 8:462–471. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Phan K, Tsai YC, Niranjan N, Bouchard D,
Carrel TP, Dapunt OE, Eichstaedt HC, Fischlein T, Gersak B, Glauber
M, et al: Sutureless aortic valve replacement: A systematic review
and meta-analysis. Ann Cardiothorac Surg. 4:100–111.
2015.PubMed/NCBI
|
|
21
|
Cai XH: Risk factors for nosocomial
pulmonary infection after tracheal intubation under general
anesthesia. Chin J Nosocomiology. 9:1780–1782. 2011.(In
Chinese).
|
|
22
|
Flynn DM, Weinstein RA and Kabins SA:
Infections with gram-negative bacilli in a cardiac surgery
intensive care unit: the relative role of enterobacter. J Hosp
Infect. 11 Suppl A:367–373. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Farran L, Llop J, Sans M, Kreisler E, Miró
M, Galan M and Rafecas A: Efficacy of enteral decontamination in
the prevention of anastomotic dehiscence and pulmonary infection in
esophagogastric surgery. Dis Esophagus. 21:159–164. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Miljeteig I, Skrede S, Langørgen J,
Haaverstad R, Jøsendal O, Sjursen H and Norheim OF: Should patients
who use illicit drugs be offered a second heart-valve replacement?
Tidsskr Nor Laegeforen. 133:977–980. 2013.(In Norwegian).
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Berg SK, Zwisler AD, Pedersen BD, Haase K
and Sibilitz KL: Patient experiences of recovery after heart valve
replacement: Suffering weakness, struggling to resume normality.
BMC Nurs. 12:232013. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Nietlispach F and Maisano F: Balloon
post-dilation after transcatheter aortic valve replacement: A
solution worth trying in patients with residual aortic
insufficiency. JACC Cardiovasc Interv. 7:790–791. 2014. View Article : Google Scholar : PubMed/NCBI
|