Introduction
Allergic rhinitis (AR) is a common chronic
inflammatory condition of the upper airways that affects 10–40% of
the global population (1,2). In China, it has been reported that
8.7–24.1% of the population suffers from AR (3). The differences in incidence may be due
to region-specific environmental conditions. As a major public
health problem, AR affects the quality of life, and imposes a
financial and social burden (4). The
current therapeutic strategies for AR include allergen avoidance,
symptomatic pharmacotherapy and allergen-specific immunotherapy
(5). While these strategies are
effective, the majority of them require lifelong use and have a
number of side effects (4). These
medications, such as nasal decongestants, H1-antihistamines, and
nasal corticosteroids can relieve nasal symptoms, although not
completely, in a considerable number of patients (4).
An increasing number of studies have indicated that
molecular hydrogen (H2) induces beneficial effects in
numerous oxidative stress-associated diseases (6–17). It
has been demonstrated that oxidative stress contributes to allergic
inflammation, including asthma and AR (6–8). As an
antioxidative agent, H2 mediates therapeutic benefits in
different systems by selectively scavenging free hydroxyl radicals
and reactive oxygen species (ROS) (8–10).
Inhaled H2 can prevent or reduce pathological or
biochemical alterations in cerebral infarction (10), lung graft injury (11), hepatic injury (12), intestinal ischemic injury (13), cisplatin-induced nephrotoxicity
(14), cutaneous anaphylaxis
(15), general inflammation
(16), and asthma (17). Recently, it has been demonstrated
that H2-rich saline attenuates allergic inflammation and
suppresses the release and activation of eosinophils in AR
(8,18). Mast cells are the key effector cells
in the immunoglobulin E (IgE)-mediated allergic reactions, and
H2 can attenuate the high-affinity IgE receptor-mediated
signal transduction (15). However,
to the best of our knowledge, it remains unclear whether
H2 induces therapeutic effects in nasal inflammation and
whether high concentrations of H2 could be applicable to
the treatment of AR.
AR is a chronic inflammatory condition associated
with T-helper cell (Th)1/Th2 imbalance. In the present study, the
beneficial effects of small molecule gases, H2 and
helium (He), were compared in a murine model of AR. The expression
levels of Th1/Th2 cytokines in the serum were also studied using a
multiplex cytokine assay. The current study demonstrated that
inhalation of H2 alleviated nasal allergic inflammation
and reversed the weight loss caused by AR in mice.
Materials and methods
Animals
A total of 106 female BALB/c mice (age, 6–8 weeks;
weight, 19–22 g) were purchased from Shanghai Laboratory Animals
Center (Shanghai, China) and housed in a temperature-controlled
room (23±2°C) with 55±10% humidity under a 12-h light/dark cycle.
The mice had ad libitum access to standard rodent chow and
tap water. All of the experimental procedures performed on mice
were in accordance with the Guide for the Care and Use of
Laboratory Animals of Tongji University and approved by the Ethics
Committee of Laboratory Animal Center of Tongji Universtiy
(Shanghai, China).
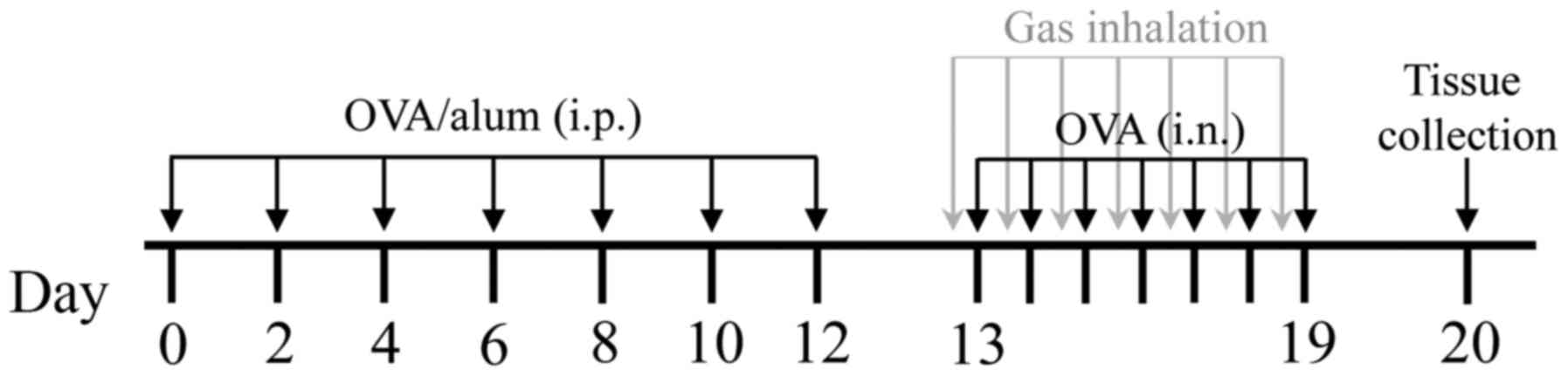
AR model
The murine model of AR was established as described
previously with minor modifications (19). Briefly, the mice were sensitized by
intraperitoneal injection of 40 µg ovalbumin (OVA; grade V;
Sigma-Aldrich; Merck KGaA, Darmstadt, Germany) used in conjunction
with 2 mg aluminum hydroxide adjuvant diluted in normal saline (NS)
on days 0, 2, 4, 6, 8, 10 and 12. Starting on day 13, the mice were
intranasally challenged with 10% OVA (10 µl/nostril) once a day for
7 consecutive days. The control mice were sensitized with aluminum
hydroxide diluted in NS alone and challenged with NS.
Gas inhalation and study groups
Hydrogen gas was produced using the AMS-H-01
hydrogen oxygen nebulizer (Asclepius Meditec Co., Ltd., Shanghai,
China), which simultaneously produced oxygen by electrolyzing water
(vol/vol: 66.7% H2 and 33.3% O2). Mice were
housed in a standard cage with food and water available ad
libitum and the cage was placed in a semi-closed metal box. The
cage was supplied with H2 mixture, in which the volume
of oxygen was automatically adjusted to 21% by controlling nitrogen
(N2) input. The final volume fraction of H2
mixture in the cage was ~40% H2, 21% O2, and
39% N2. In the inert gas experiments, the mice were
subject to He inhalation. These mice were kept in a cage supplied
with a He mixture (He/O2/N2: 40/21/39%).
A total of 60 female BALB/c mice were randomly
divided into six groups of 10 mice each, as follows: i) Control
group, mice were exposed to ambient atmosphere; ii) control +
H2 group, mice inhaled the H2 mixture for 4 h
daily for 7 consecutive days before each intranasal NS challenge;
iii) control + He group, mice inhaled the He mixture for 4 h daily
for 7 consecutive days before each intranasal NS challenge; iv) AR
group, AR mice were exposed to ambient atmosphere; v) AR +
H2 group, AR mice inhaled the H2 mixture for
4 h daily for 7 consecutive days before each intranasal OVA
challenge; and vi) AR + He group, AR mice inhaled the He mixture
for 4 h daily for 7 consecutive days before each intranasal OVA
challenge (Fig. 1). The body weight
of the mice was measured on days 0, 12 and 20.
In dose-effect experiments, 4 control mice were
exposed to air and 42 AR mice (7 groups; 6 AR mice in each group)
were exposed to the H2 mixture for 0, 0.5, 1 or 2 h each
time, once or twice a day, for 7 consecutive days.
Assessment of nasal symptoms
The severity of nasal allergic symptoms was
determined by measuring the frequencies of sneezing and
nose-scratching for 10 min after the last intranasal OVA/NS
challenge. In order to eliminate bias, mice were subjected to an
observation in a single-blinded manner by examiners.
Serum multiple cytokine assay
Mice were euthanized with an intraperitoneal
overdose of sodium pentobarbital (100 mg/kg bodyweight) 24 h after
the last intranasal challenge. Blood was collected from the
retro-orbital sinus and centrifuged at 1,000 × g for 10 min at 4°C.
Serum was collected and stored at −80°C for cytokine assays.
Quantitative assays for multiple cytokines were performed using the
commercially available Mouse Cytokine 23-Plex Immunoassay (Bio-Rad
Laboratories, Inc., Hercules, CA, USA) according to the
manufacturer's protocol. The 23-Plex Immunoassay mainly detects Th1
and Th2 cytokines.
Tissue preparation
Decapitated mouse heads were fixed in 4%
paraformaldehyde for 48 h at room temperature, decalcified in 10%
EDTA for 4–5 weeks, and embedded in paraffin. The embedded nasal
cavities were cut into 4-µm-thin sections in the coronal direction.
The sections were stained in hematoxylin solution for 5 min and
stained in eosin-phloxine solution for 1 min at room temperature.
Images were captured under optical microscopy at ×400
magnification.
Statistical analysis
Statistical analyses were performed using SPSS
software (version 19.0; IBM Corp., Armonk, NY, USA). All data are
presented as the mean ± standard error of the mean. Statistical
analyses of data were performed using one-way analysis of variance
followed by Least Significant Difference post hoc test for
comparisons among groups. P<0.05 was considered to indicate a
statistically significant difference.
Results
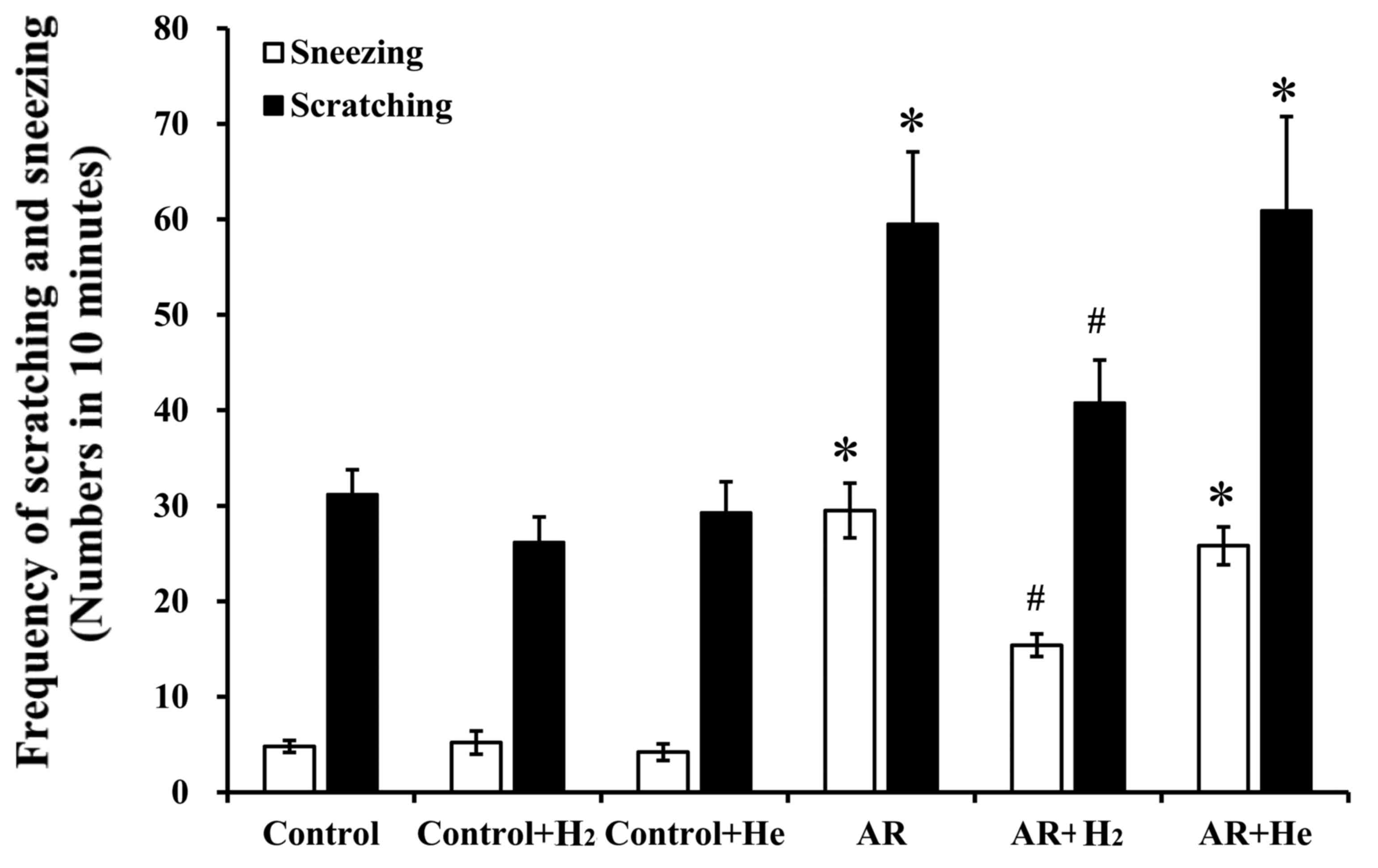
Hydrogen inhalation alleviates nasal
allergic symptoms
The murine model of AR established via sensitization
and challenge with OVA in the present study, has been previously
used to investigate the pathological and physiological mechanisms
of AR (19). Allergic symptoms,
including sneezing and nasal itching, were assessed based on
behavioral observations in mice. The current study examined the
effects of H2 or He inhalation on allergic symptoms. As
shown in Fig. 2, the numbers of
sneezing and nose scratching events within 10 min following the
last OVA challenge in the AR group (29.5±2.9 and 59.5±7.6,
respectively) significantly increased compared with the control
group (4.8±0.6 and 31.2±2.6, respectively, P<0.001), the control
+ H2 group (5.2±1.2 and 26.2±2.6, respectively,
P<0.001), and the control + He group (4.2±0.9 and 29.3±3.2,
respectively, P<0.001). In the AR + H2 group, the
frequencies of sneezing and scratching (15.4±1.2 and 40.8±4.5/10
min, respectively) decreased significantly compared with the AR
group (P<0.001 and P=0.025, respectively). He inhalation did not
markedly alter the frequencies of sneezing and nasal itching in the
AR+He group compared with the AR group (25.8±1.9 and 60.9±9.8/10
min; P=0.117 and P=0.864, respectively). Additionally,
H2 and He inhalation pretreatment in the control mice
exhibited no significant effects on nasal symptoms compared with
the control group. These results indicate that H2
inhalation, rather than He, could alleviate nasal allergic symptoms
in OVA-challenged mice.
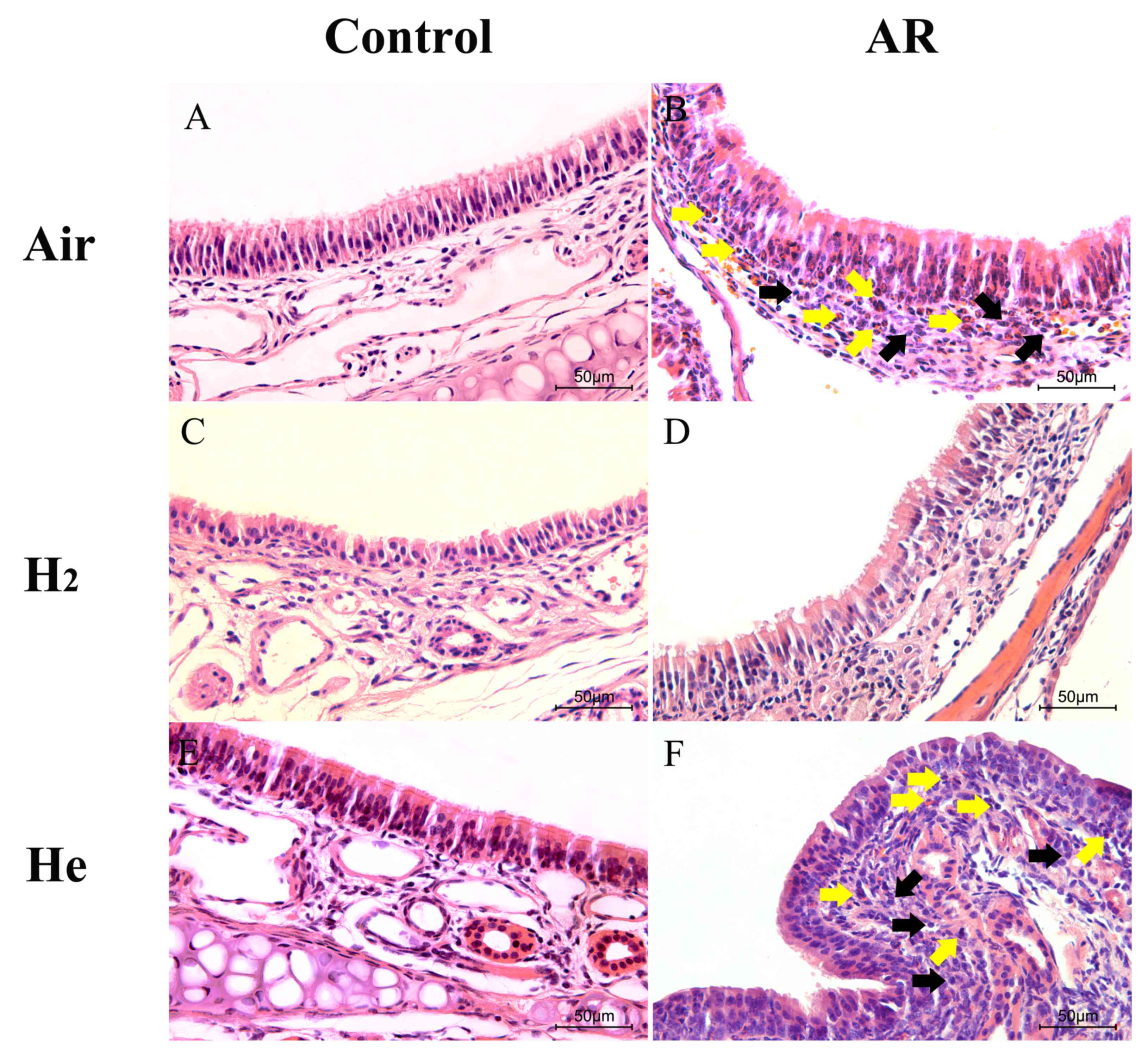
H2 inhalation inhibits
allergic inflammation of nasal mucosa
Sensitization and challenge with OVA can induce
significant allergic inflammation in mouse nasal mucosa (Fig. 3A). The ciliated epithelium was
damaged and discontinuous in the AR group (Fig. 3B). Numerous inflammatory cells,
including lymphocytes and eosinophils, were observed in the
submucosa. In the AR + H2 group, the elevated
infiltration of inflammatory cells into the mucosa and submucosa
was inhibited compared with the AR group (Fig. 3D), and the integrity of the mucosa
was protected. No apparent difference was observed between the AR
and AR + He groups (Fig. 3B and F).
These results indicate that H2 inhalation pretreatment
could reduce the inflammatory injury of nasal mucosa.
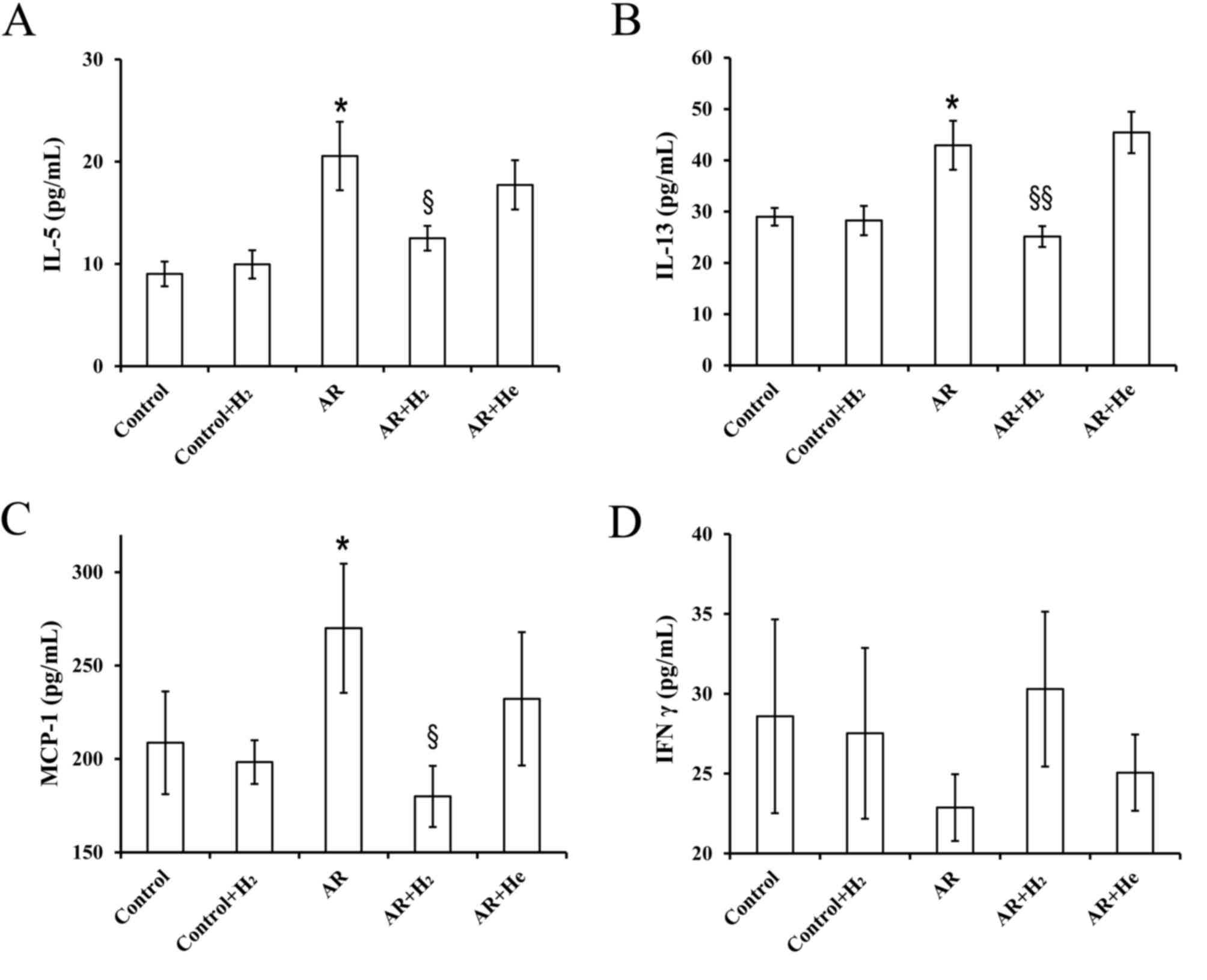
Hydrogen inhalation decreases cytokine
and chemokine levels in serum
Th2 cytokines, interleukin (IL)-4, −5 and −13, serve
roles in airway allergic inflammation, including AR and asthma
(18). The present study
investigated the effects of H2 inhalation on the
expression of several cytokines and chemokines in serum using the
Cytokine 23-Plex Immunoassay. Expression levels of IL-5, IL-13 and
monocyte chemoattractant protein-1 (MCP-1) were significantly
increased in the AR group compared with the control. H2
inhalation significantly decreased the expression levels of these
cytokines and chemokines (Fig.
4A-C). Th1/Th2 immunological imbalance is involved in the
pathophysiological process of allergic inflammation (18). The expression level of interferon-γ
(IFN-γ), a Th1 cytokine, decreased in the AR group compared with
the control, and H2 inhalation increased the level of
IFN-γ; however, these differences were not statistically
significant. Furthermore, no significant difference was found
between the AR and AR + H2 groups (Fig. 4D).
Dose-effect of H2
inhalation on AR
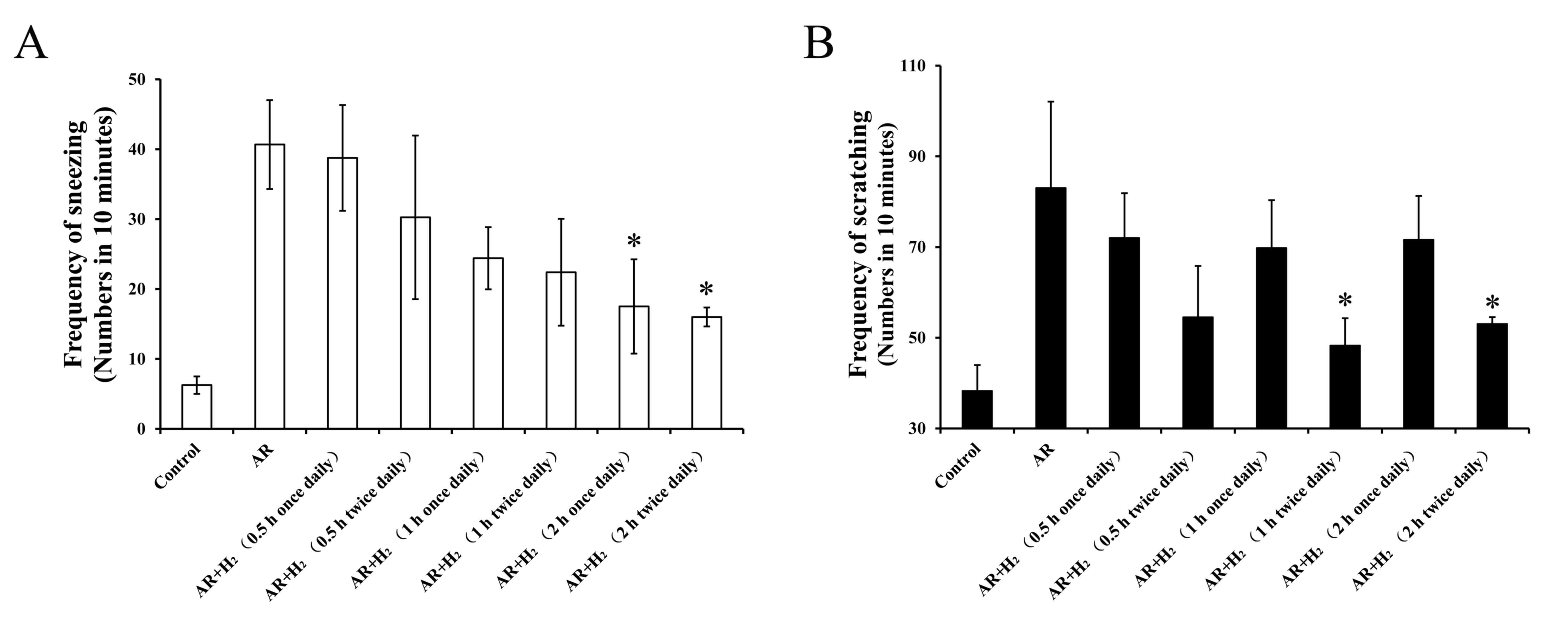
To investigate the dose-effect association between
H2 inhalation and allergic symptoms, different
inhalation frequencies and durations were used in the murine models
of AR. The frequency of sneezing decreased following administration
of H2 in a dose-dependent manner (Fig. 5A). The frequencies of sneezing
following 2-h exposure once a day (17.5±6.7/10 min) and 2-h
exposure twice a day (16±1.4/10 min) significantly decreased
compared with the AR group (40.7±6.4/10 min; P=0.037 and P=0.027,
respectively). Frequencies of scratching were lower in the twice
daily H2 administration groups compared with once daily
H2 administration groups, regardless of the duration of
inhalation (Fig. 5B). While, only
the frequencies of scratching following a 1 and 2-h exposure twice
a day (48.3±6.0 and 53.0±1.5/10 min, respectively) were
significantly decreased compared with the AR group (83.0±19.1/10
min; P=0.028 and P=0.045, respectively). These results indicated
that H2 inhalation for 2 h twice a day exhibited a
significant therapeutic effect on AR in the mouse models used in
the present study.
H2 inhalation regulates
mice weight
Our earlier work indicated that AR could limit the
increase in mice body weight (data not published). In the present
study, the baseline weight in all groups was comparable. During the
modeling phase, there was no significant difference in weight gain
between mice after OVA-sensation or OVA-challenge alone, compared
with the control (Tables I and
II, respectively). After the model
had been successfully established, the weight gain in the AR group
was 0.95±0.20 g, which was lower than in the control group
(1.57±0.41 g; P=0.081; Table III).
Furthermore, reduced food intake behavior was observed in AR mice
(data not shown). The hair of mice in the AR group were disordered
with a lack of luster. Similarly, no significant differences were
observed for weight gain in the control + H2 group
compared with the AR + H2 group, and the control + He
group compared with the AR + He group (Table III). Hydrogen inhalation increased
the bodyweight in AR mice by 0.36±0.12 g (Table III). Although no statistically
significant difference in weight gain was identified compared with
the control + H2 group (−0.10±0.30 g; P=0.293), AR mice
with H2 exposure appeared more active. He inhalation did
not improve the weight loss in AR mice (−0.38±0.14 g) compared with
the control group (0.57±0.17 g; Table
III).
 | Table I.Effect of ovalbumin-sensitization on
the bodyweight of mice. |
Table I.
Effect of ovalbumin-sensitization on
the bodyweight of mice.
| Group | Weight gain
(g) | P-value |
|---|
| Non-sensitized | 0.58±0.12 | 0.078 |
| Sensitized | 0.93±0.15 |
|
 | Table II.Effect of ovalbumin-challenge on the
bodyweight of mice. |
Table II.
Effect of ovalbumin-challenge on the
bodyweight of mice.
| Group | Weight gain
(g) | P-value |
|---|
| Control | 0.57±0.17 | 0.264 |
| AR | 0.23±0.24 |
|
| Control + H2 | −0.46±0.15 | 0.644 |
| AR + H2 | 0.60±0.21 |
|
| Control + He | 0.18±0.14 | 0.102 |
| AR + He | −0.73±0.32 |
|
 | Table III.Effect of AR on the bodyweight of
mice. |
Table III.
Effect of AR on the bodyweight of
mice.
| Group | Weight gain
(g) | P-value |
|---|
| Control | 1.57±0.41 | 0.081 |
| AR | 0.95±0.20 |
|
| Control + H2 | −0.10±0.30 | 0.293 |
| AR + H2 | 0.36±0.12 |
|
| Control + He | 0.57±0.17 | 0.560 |
| AR + He | −0.38±0.14 |
|
The weight gain in the control + H2 group
(−0.46±0.15 g) was significantly lower compared with the control
group (0.57±0.17 g; P=0.001). Mice in the control + He group
exhibited a 0.18±0.14 g weight gain which was not significantly
different compared with the weight gain in the control group
(P=0.161; Table IV). Mice in the AR
+ H2 group exhibited a 0.60±0.21 g weight gain, which
was significantly higher compared with the weight gain in the AR
group (0.23±0.24 g; P=0.008). He inhalation did not improve the
weight gain in mouse models of AR. These results indicated that
H2 inhalation can restrain weight increase in healthy
mice and reverse weight loss induced by AR.
 | Table IV.Effect of H2 inhalation on the
bodyweight of mice. |
Table IV.
Effect of H2 inhalation on the
bodyweight of mice.
| Group | Weight gain
(g) | P-value |
|---|
| Control | 0.57±0.17 |
|
| Control + H2 | −0.46±0.15 | 0.001a |
| Control + He | 0.18±0.14 | 0.161a |
| AR | 0.23±0.24 |
|
| AR + H2 | 0.60±0.21 | 0.008b |
| AR + He | −0.73±0.32 | 0.002b |
Discussion
H2 is a medical gas with antioxidative,
anti-inflammatory and antiapoptotic properties (6,8,16,20).
Previous studies have indicated that a low concentration of
H2 can be used in a number of diseases (9,11–14,20).
Both inhalation of low-concentration H2 (1–4%) and
administration of H2-rich saline are effective treatment
methods (18,21,22).
Water electrolysis is a feasible and convenient H2
source for large-scale clinical use. In the current study, the
concentration of H2 produced by electrolyzing water was
markedly higher compared with the concentration used in previous
studies (11–17). No mice succumbed during the
observation period, thus the present study demonstrated that a high
concentration of H2 can safely and efficiently
ameliorate OVA-induced nasal allergy symptoms in a mouse model of
AR.
Oxidant/antioxidant imbalance serves an important
role in airway inflammation (23,24).
Oxidative stress and ROS contribute to allergic inflammation
(6–8). Inflammatory cells, including
eosinophils, neutrophils and lymphocytes from the airway/blood,
have been demonstrated to produce oxidants in response to various
stimuli (23,25). Oxidative stress and ROS can disrupt
the integrity and function of epithelial cilia and alter the
expression of adhesion molecules, resulting in an osmotic increase
in mucosa and mucus production (8).
Eosinophils and mast cells are the main effector cell populations
of allergic airway inflammation. Antigen challenge improves the
release of ROS from eosinophils in the airway and blood of patients
with asthma (26,27). H2-rich saline can suppress
active eosinophils by decreasing serum levels of eosinophil
cationic protein in AR (8). In the
current study, inhalation of high concentrations of H2
(40%) decreased the infiltration of the mucosa and submucosa by
inflammatory cells including eosinophils and lymphocytes, and the
damaged and discontinuous ciliated epithelium was effectively
protected by treatment with H2. Zhang et al
(17) demonstrated that inhalation
of 67% H2 markedly improved the lung function and
protected the airway inflammation in an asthmatic murine model. In
their experimental settings, the concentrations of inhaled
O2 was 33% (17). In the
present study, the concentration of oxygen inhaled by mice was 21%,
the same as that in the ambient atmosphere. This method excluded
the effect of high concentration oxygen on mice. The current data
revealed that a high concentration of H2 from water
electrolysis may exhibit a therapeutic effect on AR.
The immune dysfunction resulting from the Th1/Th2
response imbalance is a major cause of chronic allergic
inflammation, including AR (18,19). Th2
cells and Th2 cytokines serve an important role in the
pathophysiology of AR (28,29), and the allergic symptoms can be
controlled by inhibiting Th2 responses. Th2 cytokines, including
IL-5 and IL-13, are involved in multiple steps in the lifecycle of
eosinophils (18). IL-5 promotes the
differentiation and maturation of eosinophil progenitors,
stimulates cell migration, induces cytokine synthesis and
degranulation, enhances production of oxygen radicals and
leukotrienes, and promotes and prolongs the survival of eosinophils
(30). IL-13 serves a role in airway
hypersensitivity and mucus hypersecretion (18). It acts on B cells to produce IgE by
activating eosinophils and basophils (18). The current study indicated that the
levels of IL-5 and −13 were significantly decreased in the serum of
the AR + H2 group compared with the AR group. These
results are consistent with previous research (17,18) and
reveal that high concentrations of inhaled H2 could
markedly decrease the levels of Th2 cytokines and inhibit Th2
responses in allergic diseases. IFN-γ is one of the major Th1
cytokines, which promotes the differentiation of Th0 cells to Th1
and inhibits the generation of Th2 cells by inducing T-bet
expression (31). In our previous
study, a decreased level of IFN-γ was observed in the nasal cavity
lavage fluid from AR mice (31). In
the present study, the level of IFN-γ in serum was slightly
decreased in the AR group mice compared with the control group.
However, H2 inhalation reversed the decreased level of
IFN-γ in the AR + H2 group. Although H2
inhalation had no statistically significant influence on IFN-γ
expression, the significantly decreased levels of IL-5 and −13 and
slightly increased IFN-γ levels indicated that H2 may
serve a role in the regulation of the Th1/Th2 immune responses.
MCP-1 is a small cytokine primarily secreted by monocytes,
macrophages and dendritic cells. MCP-1 recruits monocytes, T cells
and dendritic cells to the sites of inflammation resulting from
tissue injury, antigens or infection. H2 inhalation was
demonstrated to significantly reverse the increased MCP-1
expression level in AR mice, reducing the inflammation in the later
stage of AR.
Previous results concerning the effects of allergic
inflammation on body weight are inconsistent. Loerbroks et
al (32) reported that the
prevalence of asthma among obese women was almost twice as high as
among normal weight women, and a causal relationship between asthma
and incident weight gain cannot be excluded. In an animal model
study, Hong et al (33)
observed that normal group mice exhibited increased weight compared
with AR mice. The current study indicated that food intake was
decreased and that weight increase was lower in AR group mice.
However, H2 inhalation differentially regulated the body
weight in different groups of mice. For normal mice, H2
inhalation inhibited the weight gain. In AR mice, H2
inhalation promoted weight increase.
There are certain limitations in the current study.
The study only presented results for certain cytokines which
expression levels between groups were statistically significantly
different. Oxidative stress serves an important role in the
pathogenesis of allergic diseases and H2 can selectively
reduce the levels of ROS (9,12,13,17).
H2 can significantly increase the expression of nuclear
factor erythroid 2-related factor 2 (Nrf2) in epithelial cells and
Nrf2 is the key molecule of antioxidative stress of hydrogen
(34,35). Therefore, future studies are required
to determine the effects of H2 on the Nrf2 signaling
pathway in the nasal epithelial cells of AR.
In conclusion, H2 inhalation at a high
concentration may improve nasal allergic symptoms, reduce
inflammatory cell infiltration in nasal mucosa, and regulate
Th1/Th2 responses. The inhibitory effect of H2
inhalation on nasal allergic symptoms over a long period is more
effective than that over a short period. At an equal inspiratory
volume, multiple inhalation events result in greater improvements
compared with single inhalation events. In addition, treatment with
H2 exhibited a beneficial effect on mouse health through
selective weight control. The present study indicated that
H2 may have a therapeutic value for allergic
diseases.
Acknowledgements
Not applicable.
Funding
The present study was supported by National Natural
Science Foundation of China (cat. no. 81300809) and Shanghai Pudong
New Area Science & Technology Development Fund (cat. nos.
PKJ2016-Y02 and PW2016D-11).
Availability of data and materials
The datasets of the present study are available from
the corresponding authors.
Authors' contributions
SF, XL, XW, YZ, and ZM were responsible for
performance of experiment, and data analysis. YW and WW were
responsible for manuscript writing and revision, and experimental
design.
Ethics approval and consent to
participate
The experiment protocols were approved by the Ethics
Committee of Laboratory Animal Center of Tongji Universtiy
(Shanghai, China; approval no: TJLAC-017-028).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
AR
|
allergic rhinitis
|
|
IgE
|
immunoglobulin E
|
|
IL-5
|
interleukin-5
|
|
IL-13
|
interleukin-13
|
|
IFN-γ
|
interferon-γ
|
|
MCP-1
|
monocyte chemoattractant protein-1
|
|
NS
|
normal saline
|
|
OVA
|
ovalbumin
|
|
ROS
|
reactive oxygen species
|
References
|
1
|
Bousquet J, Jacot W, Vignola AM, Bachert C
and Van Cauwenberge P: Allergic rhinitis: A disease remodeling the
upper airways? J Allergy Clin Immunol. 113:43–49. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Warner JO: Allergic rhinitis is an
extremely common problem, but prevalence rates widely vary between
countries. Pediatr Allergy Immunol. 21:e105–e106. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Zhang L, Han D, Huang D, Wu Y, Dong Z, Xu
G, Kong W and Bachert C: Prevalence of self-reported allergic
rhinitis in eleven major cities in China. Int Arch Allergy Immunol.
149:47–57. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Zhang Y and Zhang L: Prevalence of
allergic rhinitis in china. Allergy Asthma Immunol Res. 6:105–113.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Cheng L, Chen J, Fu Q, He S, Li H, Liu Z,
Tan G, Tao Z, Wang D, Wen W, et al: Chinese society of allergy
guidelines for diagnosis and treatment of allergic rhinitis.
Allergy Asthma Immunol Res. 10:300–353. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Sim CS, Lee JH, Kim SH, Han MW, Kim Y, Oh
I, Yun SC and Lee JC: Oxidative stress in schoolchildren with
allergic rhinitis: Propensity score matching case-control study.
Ann Allergy Asthma Immunol. 115:391–395. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sagdic A, Sener O, Bulucu F, Karadurmus N,
Özel HE, Yamanel L, Tasci C, Naharci I, Ocal R and Aydin A:
Oxidative stress status and plasma trace elements in patients with
asthma or allergic rhinitis. Allergol Immunopathol (Madr).
39:200–205. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Yu S, Zhao C, Che N, Jing L and Ge R:
Hydrogen-rich saline attenuates eosinophil activation in a guinea
pig model of allergic rhinitis via reducing oxidative stress. J
Inflamm (Lond). 14:12017. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ohsawa I, Ishikawa M, Takahashi K,
Watanabe M, Nishimaki K, Yamagata K, Katsura K, Katayama Y, Asoh S
and Ohta S: Hydrogen acts as a therapeutic antioxidant by
selectively reducing cytotoxic oxygen radicals. Nat Med.
13:688–694. 2007. View
Article : Google Scholar : PubMed/NCBI
|
|
10
|
Sato Y, Kajiyama S, Amano A, Kondo Y,
Sasaki T, Handa S, Takahashi R, Fukui M, Hasegawa G, Nakamura N, et
al: Hydrogen-rich pure water prevents superoxide formation in brain
slices of vitamin C-depleted SMP30/GNL knockout mice. Biochem
Biophys Res Commun. 375:346–350. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Zhou H, Fu Z, Wei Y, Liu J, Cui X, Yang W,
Ding W, Pan P and Li W: Hydrogen inhalation decreases lung graft
injury in brain-dead donor rats. J Heart Lung Transplant.
32:251–258. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Fukuda K, Asoh S, Ishikawa M, Yamamoto Y,
Ohsawa I and Ohta S: Inhalation of hydrogen gas suppresses hepatic
injury caused by ischemia/reperfusion through reducing oxidative
stress. Biochem Biophys Res Commun. 361:670–674. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Buchholz BM, Kaczorowski DJ, Sugimoto R,
Yang R, Wang Y, Billiar TR, McCurry KR, Bauer AJ and Nakao A:
Hydrogen inhalation ameliorates oxidative stress in transplantation
induced intestinal graft injury. Am J Transplant. 8:2015–2024.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Nakashima-Kamimura N, Mori T, Ohsawa I,
Asoh S and Ohta S: Molecular hydrogen alleviates nephrotoxicity
induced by an anti-cancer drug cisplatin without compromising
anti-tumor activity in mice. Cancer Chemother Pharmacol.
64:753–761. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Itoh T, Fujita Y and Ito M, Masuda A, Ohno
K, Ichihara M, Kojima T, Nozawa Y and Ito M: Molecular hydrogen
suppresses FcepsilonRI-mediated signal transduction and prevents
degranulation of mast cells. Biochem Biophys Res Commun.
389:651–656. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Xie K, Yu Y, Zhang Z, Liu W, Pei Y, Xiong
L, Hou L and Wang G: Hydrogen gas improves survival rate and organ
damage in zymosan-induced generalized inflammation model. Shock.
34:495–501. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Zhang N, Deng C, Zhang X, Zhang J and Bai
C: Inhalation of hydrogen gas attenuates airway inflammation and
oxidative stress in allergic asthmatic mice. Asthma Res Pract.
4:32018. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Zhao C, Yu S, Li J, Xu W and Ge R: Changes
in IL-4 and IL-13 expression in allergic-rhinitis treated with
hydrogen-rich saline in guinea-pig model. Allergol Immunopathol
(Madr). 45:350–355. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Wang W, Jiang T, Zhu Z, Cui J, Zhu L and
Ma Z: Dexamethasone suppresses allergic rhinitis and amplifies
CD4(+) Foxp3(+) regulatory T cells in vitro. Int Forum Allergy
Rhinol. 5:900–906. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Diao M, Zhang S, Wu L, Huan L, Huang F,
Cui Y and Lin Z: Hydrogen gas inhalation attenuates seawater
instillation-induced acute lung injury via the Nrf2 pathway in
rabbits. Inflammation. 39:2029–2039. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Cui J, Chen X, Zhai X, Shi D, Zhang R, Zhi
X, Li X, Gu Z, Cao L, Weng W, et al: Inhalation of water
electrolysis-derived hydrogen ameliorates cerebral
ischemia-reperfusion injury in rats-a possible new hydrogen
resource for clinical use. Neuroscience. 335:232–241. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Xin Y, Liu H, Zhang P, Chang L and Xie K:
Molecular hydrogen inhalation attenuates postoperative cognitive
impairment in rats. Neuroreport. 28:694–700. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Al-Harbi NO, Nadeem A, Al-Harbi MM, Imam
F, Al-Shabanah OA, Ahmad SF, Sayed-Ahmed MM and Bahashwan SA:
Oxidative airway inflammation leads to systemic and vascular
oxidative stress in a murine model of allergic asthma. Int
Immunopharmacol. 26:237–245. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Campos D, Ravagnani FG, Gurgueira SA,
Vercesi AE, Teixeira SA, Costa SKP, Muscará MN and Ferreira HHA:
Increased glutathione levels contribute to the beneficial effects
of hydrogen sulfide and inducible nitric oxide inhibition in
allergic lung inflammation. Int Immunopharmacol. 39:57–62. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Sutcliffe A, Hollins F, Gomez E, Saunders
R, Doe C, Cooke M, Challiss RA and Brightling CE: Increased
nicotinamide adenine dinucleotide phosphate oxidase 4 expression
mediates intrinsic airway smooth muscle hypercontractility in
asthma. Am J Respir Crit Care Med. 185:267–274. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Calhoun WJ, Reed HE, Moest DR and Stevens
CA: Enhanced superoxide production by alveolar macrophages and
air-space cells, airway inflammation, and alveolar macrophage
density changes after segmental antigen bronchoprovocation in
allergic subjects. Am Rev Respir Dis. 145:317–325. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Vachier I, Chanez P, Le Doucen C, Damon M,
Descomps B and Godard P: Enhancement of reactive oxygen species
formation in stable and unstable asthmatic patients. Eur Respir J.
7:1585–1592. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Ryan MW: Asthma and rhinitis:
Comorbidities. Otolaryngol Clin North Am. 41283–295. (vi)2008.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Broide DH: Immunomodulation of allergic
disease. Annu Rev Med. 60:279–291. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Hamelmann E and Gelfand EW: IL-5-induced
airway eosinophilia-the key to asthma? Immunol Rev. 179:182–191.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Wang W, Zhu Z, Zhu B and Ma Z: Peroxisome
proliferator-activated receptor-gamma agonist induces regulatory T
cells in a murine model of allergic rhinitis. Otolaryngol Head Neck
Surg. 144:506–513. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Loerbroks A, Apfelbacher CJ, Amelang M and
Stürmer T: Obesity and adult asthma: Potential effect modification
by gender, but not by hay fever. Ann Epidemiol. 18:283–289. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Hong SH, Kim SR, Choi HS, Ku JM, Seo HS,
Shin YC and Ko SG: Effects of Hyeonggaeyeongyo-tang in
ovalbumin-induced allergic rhinitis model. Mediators Inflamm.
2014:4187052014. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Rangasamy T, Cho CY, Thimmulappa RK, Zhen
L, Srisuma SS, Kensler TW, Yamamoto M, Petrache I, Tuder RM and
Biswal S: Genetic ablation of Nrf2 enhances susceptibility to
cigarette smoke-induced emphysema in mice. J Clin Invest.
114:1248–1259. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Liu L, Xie K, Chen H, Dong X, Li Y and Yu
Y, Wang G and Yu Y: Inhalation of hydrogen gas attenuates brain
injury in mice with cecal ligation and puncture via inhibiting
neuroinflammation, oxidative stress and neuronal apoptosis. Brain
Res. 1589:78–92. 2014. View Article : Google Scholar : PubMed/NCBI
|