Introduction
Rheumatoid arthritis (RA) is a common chronic
autoimmune inflammatory disease of unknown etiology that affects 1%
of the global population (1–3). In China, the prevalence of RA is
0.24–0.50%, and RA is more common among women compared with men
(4). The primary features of
rheumatoid arthritis are joint swelling, joint stiffness and
deformity, and cartilage destruction (5,6). At
present, the pathogenesis of RA has not been fully elucidated, but
it is generally accepted that RA is caused by the interaction of
genetic, immune and environmental factors (7). The current treatment of RA is primarily
invasive anti-rheumatic therapy in the early stages of the disease.
In order to avoid potential adverse reactions caused by second-line
drugs, non-invasive and highly specific diagnostic and therapeutic
methods are necessary.
Synovial fibroblasts (SFs), also known as
fibroblast-like synoviocytes, have been demonstrated to serve an
important role in the pathogenesis of RA, and their tumor-like
proliferation leads to the development of synovial hyperplasia
(8,9). During RA, activated SFs accumulate in
the hyperplastic synovium of patients with RA. Increased levels of
inflammatory cytokines, chemokines and matrix metalloproteinases
(MMPs) mediate inflammation and cartilage degradation, eventually
leading to joint destruction (9). At
present, basic in vitro experiments using RA SFs have been
performed to examine the pathogenesis of RA, in order to provide a
theoretical basis for the exploration of RA ideal treatment methods
(10–12). At present, although great progress
has been made in the therapeutic strategy of RA, the efficacy
remains unsatisfactory. Therefore, novel treatment therapies for RA
are urgently required.
Avicularin, quercetin-3-α-L-arabinofuranoside, is a
bio-active flavonol that may be isolated from a number of plants.
Flavonoids have been previously suggested to exhibit various
biological properties, including hepatoprotective, anti-oxidative,
anti-allergic, anti-tumor and anti-inflammatory activities
(13–18). Quercetin (19,20) and
other flavonoids (21) have also
been demonstrated to serve a role in RA. Avicularin is a glycoside
of quercetin, and quercetin is lipophilic while avicularin is
hydrophilic, and they may differ in absorption rates (22). Although the biological activities of
quercetin, an aglycone of avicularin, have been extensively
examined, the biological properties of avicularin itself have not
been fully studied. A recent study revealed that avicularin may
reverse multidrug resistance in human gastric cancer by increasing
the expression levels of B-cell lymphoma 2 (Bcl-2)-associated X
protein (Bax) and BOK (16). Vo
et al (17) suggested that
avicularin serves an anti-inflammatory role by inhibiting the
extracellular signal-related kinase signaling pathway in
lipopolysaccharide-stimulated RAW 264.7 macrophages. Fujimori and
Shibano (18) indicated that
avicularin may suppresses lipid accumulation in mouse adipocytic
3T3-L1 cells. These data indicated that avicularin has a specific
regulatory effect in cell growth and the inflammatory response,
suggesting that it may have a certain effect on RA development by
regulating the growth and inflammatory response of RA SFs. However,
to the best of our knowledge, no study has been conducted
investigating the effects of avicularin in RA.
The aim of the present study was to investigate the
effect and the underlying molecular mechanisms of avicularin in RA
treatment in vitro. The in vitro model of RA was
established by treatment of the human rheumatoid arthritis
fibroblast-like synoviocytes MH7A cell line with tumor necrosis
factor-α (TNF-α), a well-recognized cell model that is widely used
in in vitro studies of RA (23–25). The
current study demonstrated that avicularin inhibited the
inflammatory response and cell viability, and induced apoptosis in
TNF-α-treated human RA synovial cells through preventing the
activation of the mitogen-activated protein kinase kinase/nuclear
factor kappa light-chain-enhancer of activated B-cells pathway.
Materials and methods
Cell culture
The human RA synovial MH7A cell line was obtained
from Shanghai Guandao Biological Engineering Co., Ltd. (Shanghai,
China; cat no. C0878). Cells were grown in RPMI-1640 medium
(Hyclone; GE Healthcare Life Sciences, Logan, UT, USA) containing
10% fetal bovine serum (Gibco; Thermo Fisher Scientific, Inc.,
Waltham, MA, USA) and 1% penicillin-streptomycin solution
(Sigma-Aldrich; Merck KGaA, Darmstadt, Germany), and incubated at
37°C with 5% CO2.
Cell treatment
MH7A cells were pre-treated with various
concentrations of avicularin (10, 30, 100 and 300 µM) for 2 h, then
the cells were subjected to treatment with TNF-α (10 ng/ml;
Sigma-Aldrich; Merck KGaA) at room temperature for 24 h to
establish the in vitro model of RA. Cells in the control
group were treated with normal RPMI-1640 medium.
MTT assay
An MTT assay was used to detect cell viability. The
MH7A cells were seeded into each well (5×105 cells per
well) and incubated with various concentrations of avicularin (10,
30, 100 and 300 µM) for 24 h at 37°C. Then, 0.5 mg/ml MTT (in PBS)
was added to every well, and the cells were incubated for an
additional 3 h at 37°C with 5% CO2. Dimethyl sulfoxide
was used to dissolve the formazan crystals. Finally, absorbance was
detected at 590 nm using a microplate reader (Bio-Rad Laboratories,
Inc., Hercules, CA, USA).
Cell apoptosis assay
MH7A cells were treated with 10, 30, 100 or 300 µM
avicularin and 10 ng/ml TNF-α. Then, MH7A cell apoptosis was
analyzed using an Annexin V-fluorescein isothiocyanate (FITC)
apoptosis detection kit [cat no. 70-AP101-100; Hangzhou
MultiSciences (Lianke) Biotech, Co., Ltd., Hangzhou, China].
Briefly, MH7A cells (5×105 cells per well) were dyed
with Annexin V-FITC and propidium iodide according to the
manufacturer's protocol. Flow cytometry (BD Biosciences, Franklin
Lakes, NJ, USA) was performed to analyze cell apoptosis, and data
were analyzed using Version 2.5 WinMDI (Purdue University Cytometry
Laboratories; http://www.cyto.purdue.edu/flowcyt/software/Catalog.html)
software.
ELISA
To detect the production of interleukin (IL)-1β
(cat. no. Ab100562), IL-6 (cat no. Ab46027), IL-8 (cat. no.
Ab46032), MMP-1 (cat no. Ab100603) and MMP-13 (cat. no. Ab100605),
the MH7A cell culture medium was collected by centrifugation at 4°C
and 1,048 × g for 10 min. ELISAs were performed according to the
manufacturer's protocol of each ELISA kit (all Abcam, Cambridge,
UK).
Reverse transcription quantitative
polymerase chain reaction (RT-qPCR)
Total RNA from MH7A cells was isolated using
TRIzol® reagent (Thermo Fisher Scientific, Inc.)
according to the manufacturer's protocol. cDNA was generated using
the PrimeScript™ RT reagent kit (Takara Bio, Inc., Otsu, Japan)
following the manufacturer's protocol. qPCR was performed by using
the SYBR® Premix Ex Taq™ II (Takara Bio Inc.).
Amplification conditions were as following: 95°C for 10 min,
followed by 37 cycles at 95°C for 15 sec and 72°C for 30 sec and
78°C for 1.5 min, following which samples were stored at 4°C. GAPDH
was used as an internal control. Primers are stated in Table I. Relative gene expression was
analyzed by performing the 2−ΔΔCq method (26).
 | Table I.Primer sequences of reverse
transcription quantitative polymerase chain reaction. |
Table I.
Primer sequences of reverse
transcription quantitative polymerase chain reaction.
|
| Primer (5′-3′) |
|---|
|
|
|
|---|
| Gene | Forward | Reverse |
|---|
| Inducible nitric
oxide synthase |
GAGAAGTCCAGCCGCACCAC |
GAACAATCCACAACTCGCCCAAG |
| Cyclooxygenase 2 |
TCCATTGACCAGAGCAGAGA |
TCTGGACGAGGTTTTTCCAC |
| B-cell lymphoma
2 |
TTGGATCAGGGAGTTGGAAG |
TGTCCCTACCAACCAGAAGG |
| Bcl-2-associated X
protein |
CGTCCACCAAGAAGCTGAGCG |
TGTCCCTACCAACCAGAAGG |
| GAPDH |
CTTTGGTATCGTGGAAGGACTC |
GTAGAGGCAGGGATGATGTTCT |
Western blot analysis
MH7A cells were treated with 10, 30, 100 or 300 µM
avicularin and 10 ng/ml TNF-α. Then, total proteins from MH7A cells
were isolated using radioimmunoprecipitation assay lysis buffer
(Beijing Solarbio Science and Technology Co., Ltd., Beijing,
China). The quantification of the proteins was measured by BCA
assay (Thermo Fisher Scientific, Inc.) following the manufacturer's
protocol. Equal amounts of protein samples (25 µg/lane) were
separated on 12% SDS-PAGE and then transferred to polyvinylidene
fluoride membranes. The membranes were firstly blocked with 5%
non-fat milk in PBS with 0.1% Tween-20 for 2 h at room temperature,
and then incubated with primary antibodies (all Cell Signaling
Technology, Inc., Danvers, MA, USA) against phosphorylated
mitogen-activated protein kinase kinase 1/2 (p-Mek1/2; cat. no.
2338), p-transcription factor p65 (p-p65; cat. no. 3033), inducible
nitric oxide synthase (iNOS; cat. no. 13120), cyclooxygenase 2
(COX-2; cat. no. 12282), Bcl-2 (cat. no. 4223), Bax (cat. no. 5023;
all dilution, 1:1,000) or β-actin (cat. no. 4970; dilution,
1:2,000) at 4°C overnight. Subsequently, the membranes were
incubated with the horseradish peroxidase-conjugated anti-rabbit
IgG secondary antibody (cat. no. 7074; dilution, 1:5,000; Cell
Signaling Technology, Inc.) for 2 h at room temperature. Finally, a
chemiluminescence detection kit (Cell Signaling Technology, Inc.)
was used to visualize the blots according to the manufacturer's
protocol. Gel-Pro Analyzer densitometry software (version 6.3;
Media Cybernetics, Inc., Rockville, MD, USA) was used for band
density quantification.
Statistical analysis
Data are presented as the mean ± standard deviation.
SPSS 16.0 statistical software (SPSS, Inc., Chicago, IL, USA) was
used for all statistical analyses. The associations between two
groups were analyzed by a paired Student's t-test, and the
comparisons among more than two groups were performed using a
one-way analysis of variance followed by a Student-Newman-Keuls
post-hoc test. P<0.05 was considered to indicate a statistically
significant difference.
Results
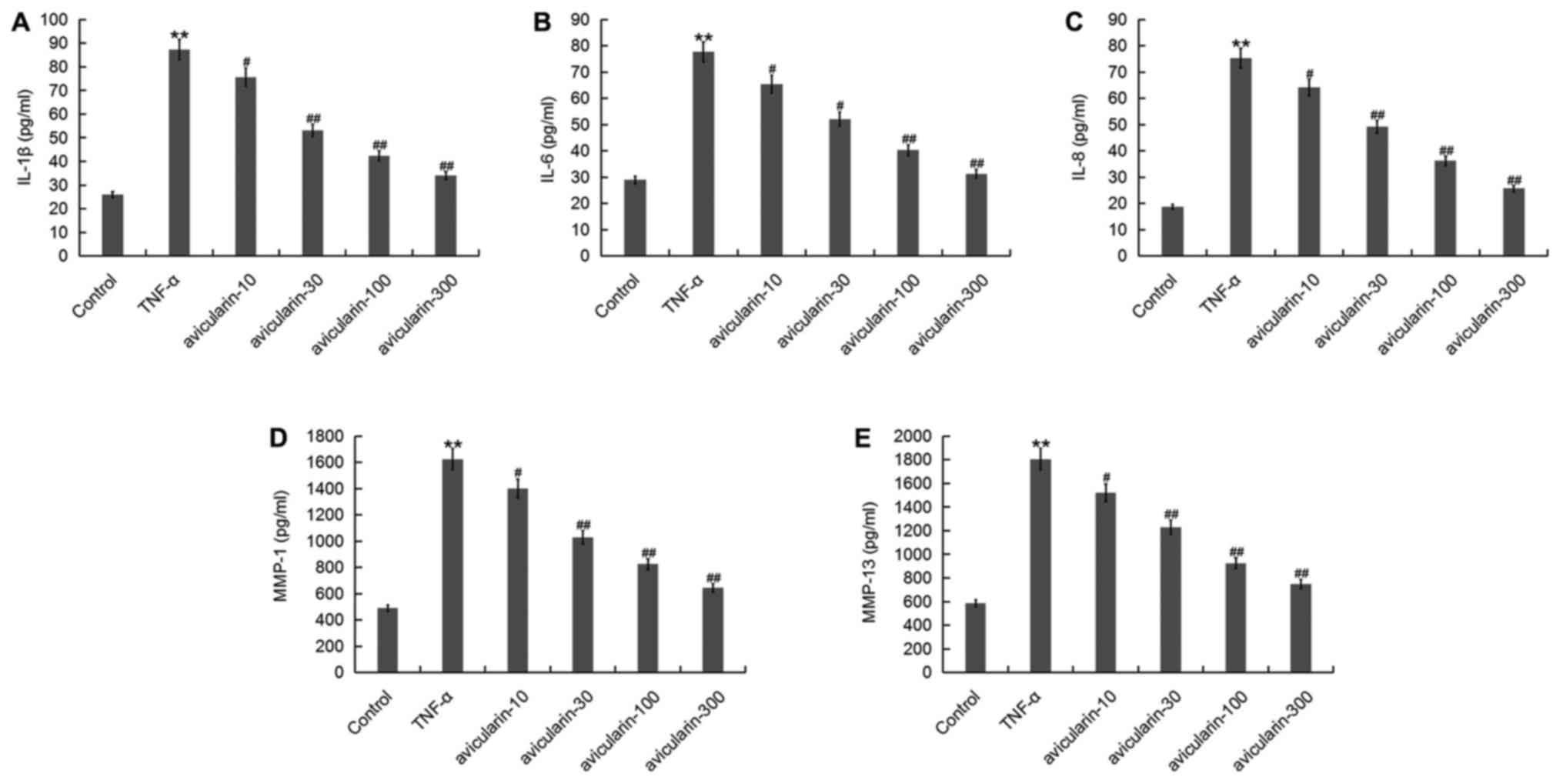
Avicularin inhibits the production of
inflammatory factors increased by TNF-α
The effect of avicularin on the inflammatory
response in the human RA synovial MH7A cell line was first
investigated. As demonstrated in Fig.
1, the expression of inflammatory factors, including IL-1β,
IL-6, IL-8, MMP-1 and MMP-13 were significantly increased by TNF-α
treatment. However, compared with the TNF-α-alone treatment group,
avicularin significantly decreased the level of IL-1β, IL-6, IL-8,
MMP-1 and MMP-13 in MH7A cells in a dose-dependent manner.
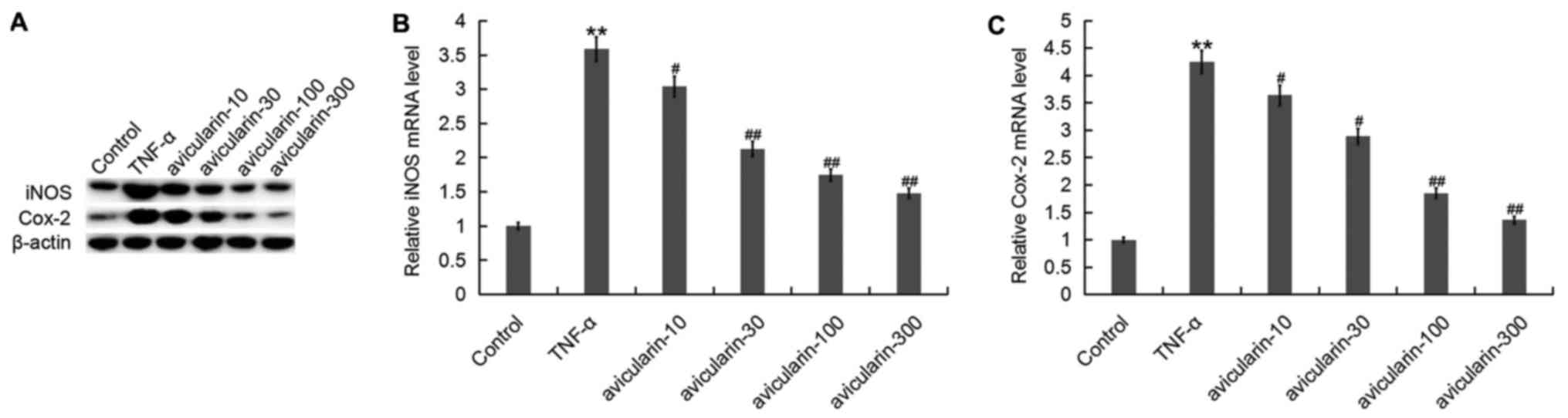
Avicularin inhibits the expression of
iNOS and COX-2 increased by TNF-α
Then, the effect of avicularin treatment on iNOS and
COX-2 expression was examined using RT-qPCR and western blot
analysis. The results indicated that avicularin administration
dose-dependently inhibited the protein (Fig. 2A) and mRNA (Fig. 2B and C) expression of iNOS and COX-2,
which were increased by TNF-α treatment in MH7A cells (Fig. 2).
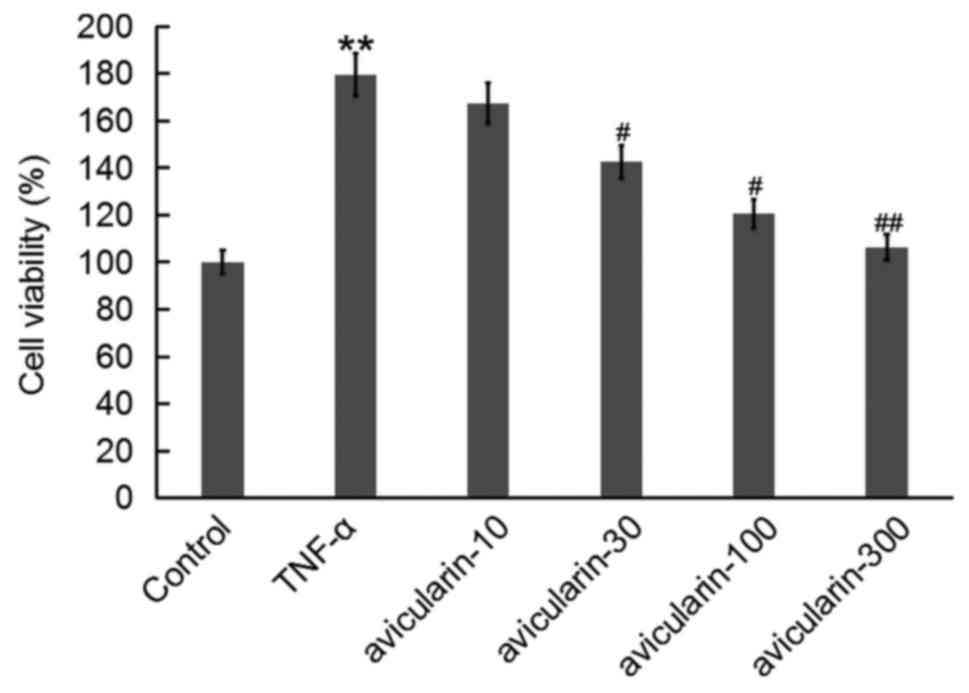
Avicularin inhibits the
TNF-α-dependent increase in MH7A cell viability
To examine whether avicularin affected the cell
viability of MH7A cells, an MTT assay was performed. It was
identified that TNF-α treatment significantly increased the cell
viability of MH7A cells, while avicularin dose-dependently
prevented the cell viability of MH7A cells (Fig. 3).
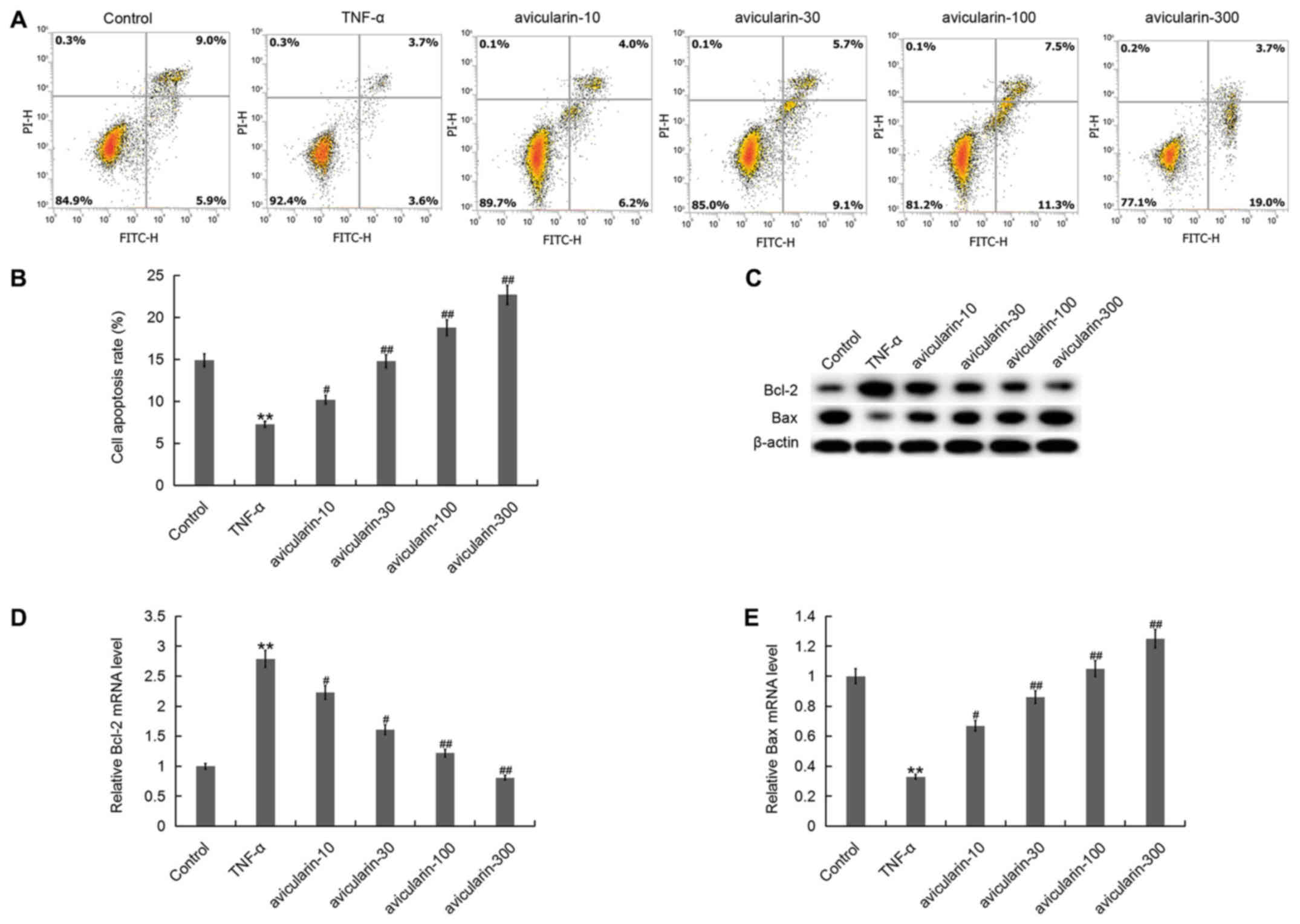
Avicularin induces MH7A cell apoptosis
inhibited by TNF-α
To investigate the effect of avicularin on MH7A cell
apoptosis, flow cytometry was performed. As indicated in Fig. 4A and B, compared with the control
group, the number of apoptotic cells in the TNF-α treatment group
was significantly decreased, and avicularin dose-dependently
induced MH7A cell apoptosis. Concomitantly, the expression levels
of apoptosis-associated proteins Bcl-2 and Bax were measured. The
results suggested that TNF-α treatment significantly increased
Bcl-2 expression and inhibited Bax expression in MH7A cells.
Compared with the TNF-α-alone treatment group, the level of Bcl-2
was notably decreased and Bax was increased by avicularin treatment
in a dose-dependent manner (Fig.
4C-E).
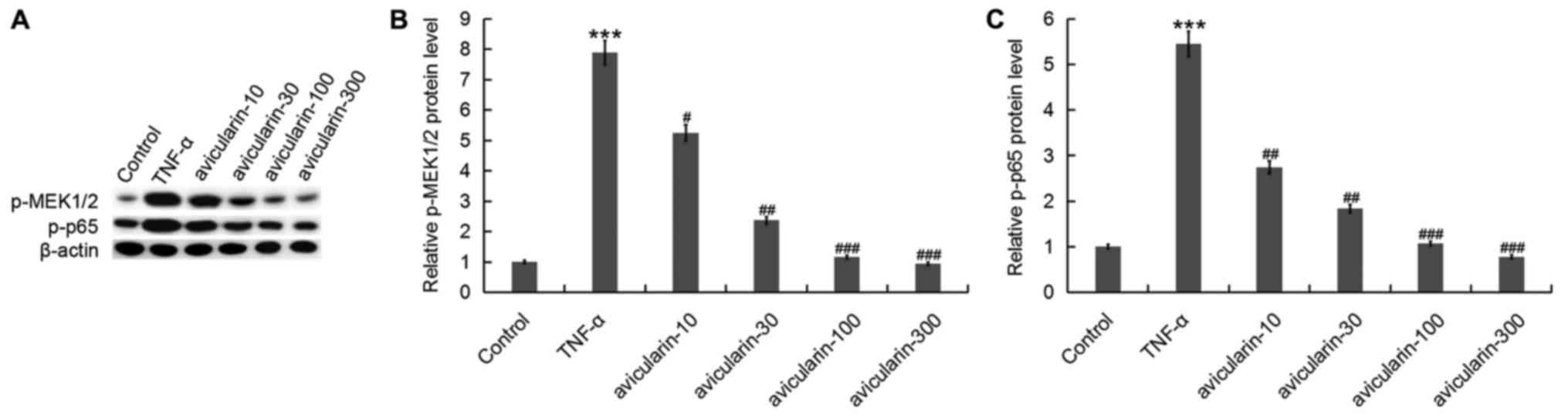
Avicularin prevents the activation of
the MEK/nuclear factor kappa light-chain-enhancer of activated
B-cells (NF-κB) pathway activated by TNF-α
Finally, to explore the molecular mechanism of the
effect of avicularin treatment on MH7A cells, the MEK/NF-κB pathway
was analyzed. As hypothesized, it was identified that TNF-α
significantly increased the protein levels of p-MEK/1/2 and p-p65,
and avicularin treatment dose-dependently decreased the protein
expression levels of p-MEK/1/2 and p-p65 (Fig. 5).
Discussion
In the present study, it was demonstrated that
avicularin inhibited the production of inflammatory factors
enhanced by TNF-α treatment. The results also indicated that TNF-α
administration significantly promoted MH7A cell viability and
inhibited cell apoptosis, and avicularin treatment dose-dependently
inhibited MH7A cell viability and induced cell apoptosis through
repressing the MEK/NF-κB pathway. It was revealed that avicularin
may be a promising therapeutic agent for the treatment of RA.
RA is a systemic autoimmune disease characterized by
chronic inflammation, synovial hyperplasia, and bone and cartilage
destruction as the primary pathological symptoms (27,28). At
present, there is no drug that may completely controls the
condition of RA, and prevents bone destruction and erosion; a
method of specifically and successfully treating RA has not yet
been identified. The treatment and successful cure of RA remains a
challenge to the global medical community, and requires additional
study.
Avicularin, a bioactive flavonol isolated from a
large number of plants, has been identified to exhibit a variety of
pharmacological properties, including anti-inflammatory effects
(16,17). Avicularin serves an important role in
regulating the inflammatory response and cell growth. Avicularin is
a glycoside of quercetin, and quercetin has been suggested to serve
a protective role in RA (19,20);
however, the effect of avicularin on RA remains unknown. A large
number of studies have indicated that SFs are the primary cells of
synovial hyperplasia and that they serve a key role in the
pathogenesis of RA synovium (9–12). SFs
participate in the entire process of inflammation and angiogenesis,
eventually causing invasive destruction of bone joints (29,30). At
present, to the best of our knowledge, the specific effect and
mechanism of avicularin on SFs in RA remains unclear. Therefore,
the present study was conducted to explore whether avicularin
exerted an effect on RA through regulating SFs.
Firstly, an in vitro model of RA was
established by treating the human RA synovial MH7A cell line with
10 ng/ml TNF-α for 24 h. It was identified that TNF-α treatment
significantly increased the inflammatory response in MH7A cells,
evidenced by increased expression levels of inflammatory factors
including IL-1β, IL-6, IL-8, MMP-1 and MMP-13. It was also
identified that TNF-α treatment significantly promoted cell
viability and inhibited cell apoptosis in MH7A cells. As
hypothesized, additional analysis indicated that avicularin
administration dose-dependently decreased the levels of IL-1β,
IL-6, IL-8, MMP-1 and MMP-13, inhibited MH7A cell viability and
induced cell apoptosis.
iNOS is a major producer of NO and serves an
important role in the progression of inflammatory diseases,
including RA (31). COX-2, which is
involved in the inflammatory response and is increased in
inflammation-associated cells following cytokine stimulation during
the immune reaction, was revealed to be upregulated during RA
development (31,32). Consistent with previous studies
(31,33), the present study identified that
TNF-α treatment significantly increased the expression levels of
iNOS and COX-2 in MH7A cells, and the increased levels of iNOS and
COX-2 caused by TNF-α treatment were dose-dependently decreased by
avicularin administration. To additionally explore the underlying
mechanism of the effect of avicularin on MH7A cells, the MEK-NF-κB
pathway, which has been identified to be repressed by avicularin in
RAW 264.7 macrophages (17), was
investigated. The results suggested that the activation of
MEK-NF-κB pathway caused by TNF-α treatment was prevented by
avicularin treatment in a dose-dependent manner.
In summary, to the best of our knowledge, the
present study identified for the first time that avicularin
inhibited the inflammatory response, prevented cell viability and
induced apoptosis in TNF-α-treated human RA synovial cells through
preventing the activation of the MEK/NF-κB pathway. Therefore,
avicularin may serve as a promising therapeutic agent for the
treatment of RA. However, this is a preliminary study examining the
effect of avicularin on RA; the protective effect of avicularin on
RA requires additional study. Compared with other flavonoids, the
advantage of using avicularin for RA is largely unclear; future
studies are required to compare the effects of avicularin and other
flavonoids on RA. In addition, the in vitro model of RA is
significantly different from in vivo RA in humans;
therefore, additional in vivo experiments and clinical
studies are also required to demonstrate the protective effect of
avicularin on RA. Future studies conducted by this group will
examine these issues in-depth.
Acknowledgements
Not applicable.
Funding
The present study was supported by Hangzhou
Municipal Science and Technology Commission (grant no.
20150733Q43).
Availability of data and materials
The analyzed data sets generated during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
WW designed the study. HZ, MZ and XL accessed and
analyzed the data. JY collaborated to analysis the data and write
the paper. All authors collaborated to interpret results and
develop the manuscript.
Ethics and consent to participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Smolen JS, Aletaha D and McInnes IB:
Rheumatoid arthritis. Lancet. 388:2023–2038. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Challal S, Minichiello E, Boissier MC and
Semerano L: Cachexia and adiposity in rheumatoid arthritis.
Relevance for disease management and clinical outcomes. Joint Bone
Spine. 83:127–133. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ji L, Geng Y, Zhou W and Zhang Z: A study
on relationship among apoptosis rates, number of peripheral T cell
subtypes and disease activity in rheumatoid arthritis. Int J Rheum
Dis. 19:167–171. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Symmons DP: Epidemiology of rheumatoid
arthritis: Determinants of onset, persistence and outcome. Best
Pract Res Clin Rheumatol. 16:707–722. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Sun J, Yan P, Chen Y, Chen Y, Yang J, Xu
G, Mao H and Qiu Y: MicroRNA-26b inhibits cell proliferation and
cytokine secretion in human RASF cells via the Wnt/GSK-3β/β-catenin
pathway. Diagn Pathol. 10:722015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
van der Geest KS, Smigielska-Czepiel K,
Park JA, Abdulahad WH, Kim HW, Kroesen BJ, van den Berg A, Boots
AM, Lee EB and Brouwer E: SF Treg cells transcribing high levels of
Bcl-2 and microRNA-21 demonstrate limited apoptosis in RA.
Rheumatology (Oxford). 54:950–958. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Xu WD, Zhang M, Zhang YJ and Ye DQ: IL-33
in rheumatoid arthritis: Potential role in pathogenesis and
therapy. Hum Immunol. 74:1057–1060. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Song YJ, Li G, He JH, Guo Y and Yang L:
Bioinformatics-based identification of microRNA-regulated and
rheumatoid arthritis-associated genes. PLoS One. 10:e01375512015.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Huber LC, Distler O, Tarner I, Gay RE, Gay
S and Pap T: Synovial fbroblasts: Key players in rheumatoid
arthritis. Rheumatology (Oxford). 45:669–675. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Lowin T and Straub RH: Synovial fbroblasts
integrate inflammatory and neuroendocrine stimuli to drive
rheumatoid arthritis. Expert Rev Clin Immunol. 11:1069–1071. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
McInnes IB and Schett G: Pathogenetic
insights from the treatment of rheumatoid arthritis. Lancet.
389:2328–2337. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Edhayan G, Ohara RA, Stinson WA, Amin MA,
Isozaki T, Ha CM, Haines GK III, Morgan R, Campbell PL, Arbab AS,
et al: Inflammatory properties of inhibitor of DNA binding 1
secreted by synovial fibroblasts in rheumatoid arthritis. Arthritis
Res Ther. 18:872016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Williams RJ, Spencer JP and Rice-Evans C:
Flavonoids: Antioxidants or signalling molecules? Free Radic Biol
Med. 36:838–849. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kim JA, Jung YS, Kim MY, Yang SY, Lee S
and Kim YH: Protective effect of components isolated from
Linderaerythrocarpa against oxidative stress-induced apoptosis of
H9c2 cardiomyocytes. Phytother Res. 25:1612–1617. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kim SM, Kang K, Jho EH, Jung YJ, Nho CW,
Um BH and Pan CH: Hepatoprotective effect of flavonoid glycosides
from lespedeza cuneata against oxidative stress induced by
tertbutyl hyperoxide. Phytother Res. 25:1011–1017. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Guo XF, Liu JP, Ma SQ, Zhang P and Sun WD:
Avicularin reversed multidrug-resistance in human gastric cancer
through enhancing Bax and BOK expressions. Biomed Pharmacother.
103:67–74. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Vo VA, Lee JW, Chang JE, Kim JY, Kim NH,
Lee HJ, Kim SS, Chun W and Kwon YS: Avicularin inhibits
lipopolysaccharide-induced inflammatory response by suppressing ERK
phosphorylation in RAW 264.7 macrophages. Biomol Ther (Seoul).
20:532–537. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Fujimori K and Shibano M: Avicularin, a
plant flavonoid, suppresses lipid accumulation through repression
of C/EBPα-activated GLUT4-mediated glucose uptake in 3T3-L1 cells.
J Agric Food Chem. 61:5139–5147. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Pan F, Zhu L, Lv H and Pei C: Quercetin
promotes the apoptosis of fibroblast-like synoviocytes in
rheumatoid arthritis by upregulating lncRNA MALAT1. Int J Mol Med.
38:1507–1514. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Javadi F, Ahmadzadeh A, Eghtesadi S,
Aryaeian N, Zabihiyeganeh M, Rahimi Foroushani A and Jazayeri S:
The effect of quercetin on inflammatory factors and clinical
symptoms in women with rheumatoid arthritis: A double-blind,
randomized controlled trial. J Am Coll Nutr. 36:9–15. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Hong Z, Li J, Biswas S, Jiang CS, Huang Y,
Sun T, Niu Y, Yu JQ, Li WQ and Yao Y: Ramosissimin, a new flavonol
from tararix ramosissima, induces apoptosis in rheumatoid arthritis
fibroblast-like synoviocytes. Pharmazie. 73:169–173.
2018.PubMed/NCBI
|
|
22
|
Hollman PC, de Vries JH, van Leeuwen SD,
Mengelers MJ and Katan MB: Absorption of dietary quercetin
glycosides and quercetin in healthy ileostomy volunteers. Am J Clin
Nutr. 62:1276–1282. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Mo X, Chen J, Wang X, Pan Z, Ke Y, Zhou Z,
Xie J, Lv G and Luo X: Krüppel-like factor 4 regulates the
expression of inducible nitric oxide synthase induced by TNF-α in
human fibroblast-like synoviocyte MH7A cells. Mol Cell Biochem.
438:77–84. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Lee GH, Lee J, Lee JW, Choi WS and Moon
EY: B cell activating factor-dependent expression of vascular
endothelial growth factor in MH7A human synoviocytes stimulated
with tumor necrosis factor-α. Int Immunopharmacol. 17:142–147.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Jia Q, Cheng W, Yue Y, Hu Y, Zhang J, Pan
X, Xu Z and Zhang P: Cucurbitacin E inhibits TNF-α-induced
inflammatory cytokine production in human synoviocyte MH7A cells
via suppression of PI3K/Akt/NF-κB pathways. Int Immunopharmacol.
29:884–890. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta-Delta C(T)) method. Methods. 25:402–408. 2011.
View Article : Google Scholar
|
|
27
|
Pope RM: Apoptosis as a therapeutic tool
in rheumatoid arthritis. Nat Rev Immunol. 2:527–535. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Huang H, Xiao Y, Lin H, Fu D, Zhan Z,
Liang L, Yang X, Fan J, Ye Y, Sun L and Xu H: Increased
phosphorylation of ezrin/radixin/moesin proteins contributes to
proliferation of rheumatoid fibroblast-like synoviocytes.
Rheumatology (Oxford). 50:1045–1053. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Gerlag DM and Tak PP: Novel approaches for
the treatment of rheumatoid arthritis: Lessons from the evaluation
of synovial biomarkers in clinical trials. Best Pract Res Clin
Rheumatol. 22:311–323. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Szekanecz Z and Koch AE: Angiogenesis and
its targeting in rheumatoid arthritis. Vascul Pharmacol. 51:1–7.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Sultana F and Rasool M: A novel
therapeutic approach targeting rheumatoid arthritis by combined
administration of morin, a dietary flavanol and non-steroidal
anti-inflammatory drug indomethacin with reference to
pro-inflammatory cytokines, inflammatory enzymes, RANKL and
transcription factors. Chem Biol Interact. 230:58–70. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Orita K, Hiramoto K, Kobayashi H, Ishii M,
Sekiyama A and Inoue M: Inducible nitric oxide synthase (inos) and
α-melanocyte-stimulating hormones of inos origin play important
roles in the allergic reactions of atopic dermatitis in mice. Exp
Dermatol. 20:911–914. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Yao RB, Zhao ZM, Zhao LJ and Cai H:
Sinomenine inhibits the inflammatory responses of human
fibroblast-like synoviocytes via the TLR4/MyD88/NF-κB signaling
pathway in rheumatoid arthritis. Pharmazie. 72:355–360.
2017.PubMed/NCBI
|