Introduction
Gestational hypertension is an obstetrical and
gynecological disease with a high morbidity rate, and its onset
often brings serious consequences to patients, such as eclampsia,
dyspnea and abortion. If timely diagnosis and treatment are not
received, it can even be life-threatening (1,2). As the
mechanism has been far from explicated, there are still many
difficulties in treatment (3,4). It is
found clinically that the onset of gestational hypertension has a
good correlation with vascular endothelial injury, the latter of
which is also closely related to hyperlipidemia, suggesting that
there is a correlation between abnormal lipid metabolism and
gestational hypertension (5–7).
Metabolic diseases are usually manifested as
abnormal insulin resistance, and gestational hypertension is also a
kind of metabolic disease, thus there are possibly a number of
changes in its insulin resistance (8). Blood coagulation and fibrinolysis are
common manifestations in patients with gestational hypertension and
such physical changes have a great relation with D-dimer, which can
be used to deduce the function of D-dimer in gestational
hypertension. Therefore, the treatment and prevention of
gestational hypertension can be achieved by controlling the D-dimer
(9). A total of 73 patients with
gestational hypertension and 70 healthy subjects were selected into
the study, and the abnormal lipid metabolism, insulin resistance
and D-dimer in the two groups were compared. The correlations of
gestational hypertension with the above-mentioned indexes were
analyzed in order to provide more therapeutic targets for
gestational hypertension.
Patients and methods
General data
A total of 73 patients with gestational hypertension
in Jinhua People's Hospital (Jinhua, China) from December 2016 to
December 2017 were selected and divided into the observation and
control groups. Patients in the observation group (aged 27.3±2.6
years, gestational weeks 35.3±3.4 weeks, pre-pregnant body mass
index BMI 22.34±2.8 kg/m2) and the subjects in the
control group (aged 28.9±2.8 years, gestational weeks 34.5±3.3
weeks, pre-pregnant BMI 23.09±2.4 kg/m2) were
primiparae. Inclusion criteria: patients with gestational
hypertension conforming to the diagnostic criteria of gestational
hypertension specified in the 8th edition of Obstetrics and
Gynaecology and patients without serious injury in the heart, liver
and kidney. Exclusion criteria: patients with poor compliance and
unable to cooperate with the diagnosis of doctors, patients with
other metabolic diseases affecting insulin resistance, or patients
with lipid metabolic disease.
The study was approved by the Ethics Committee of
Jinhua People's Hospital and informed consents were signed by the
patients or guardians.
Classification of gestational
hypertension
Based on the classification methods in the 8th
edition of Obstetrics and Gynaecology, gestational hypertension was
divided into three grades (mild, moderate and severe). Mild:
patients have no obvious physical discomfort and slight discomfort
will disappear naturally after several days. Moderate: patients
suffer from hypertension and edema. Severe: patients have various
adverse reactions, such as nausea, tachypnea, chest stuffiness,
diastolic blood pressure >14.7 kPa and systolic blood pressure
>21.3 kPa.
Indexes of lipid metabolism
The levels of triglyceride (TG), total cholesterol
(TC), high-density lipoprotein cholesterol (HDL-C) and low-density
lipoprotein cholesterol (LDL-C) were detected with a full-automatic
biochemical analyzer. HDL-C was detected via shielded method and
other indexes were detected via enzyme assay.
Insulin resistance index
The level of fasting insulin (FINS) was detected
with a FINS kit, the level of fasting blood glucose (FBG) was
detected via glucose oxidase method. Then HOMA index was calculated
using the levels of FINS and FBG.
Detection of D-dimer
The fasting venous blood was extracted from the
pregnant woman and then the upper-layer serum was taken for
centrifugation at 3,000 × g for 5 min. The level of D-dimer in
plasma was detected within 2 h via immunoturbidimetry.
Statistical analysis
Statistical Product and Service Solutions (SPSS)
17.0 software (SPSS, Inc., Chicago, IL, USA) was used for data
statistics and analysis. t-test was used for the difference
comparison between the two groups (measurement data). Chi-square
test was used for the difference comparison of enumeration data.
Pearson's method was used for correlation analysis. P<0.05 was
considered to indicate a statistically significant difference.
Results
Comparison of general data between two
groups
Patients in the observation group (aged 27.3±2.6
years, gestational weeks 35.3±3.4 weeks, pre-pregnant BM 22.34±2.8
kg/m2) and the subjects in the control group (aged
28.9±2.8 years, gestational weeks 34.5±3.3 weeks, pre-pregnant BMI
23.09±2.4 kg/m2) were primiparae. There were no
significant differences in any of these indexes (Table I).
 | Table I.Comparison of general data between two
groups (mean ± SD). |
Table I.
Comparison of general data between two
groups (mean ± SD).
| Groups | n | Age (years) | Gestational weeks
(weeks) | Pre-pregnant BMI
(kg/m2) | History of
gestation |
|---|
| Observation
group | 73 | 27.3±2.6 | 35.3±3.4 | 22.34±2.8 | Primiparae |
| Control group | 70 | 28.9±2.8a | 34.5±3.3a |
23.09±2.4a | Primiparae |
Comparison of lipid metabolism indexes
between two groups
The level of HDL-C in control group was significant
higher than that in the observation group, while the levels of
other indexes were all lower than those in the observation group
(P<0.05), and the differences were statistically significant
(Table II).
 | Table II.Comparison of lipid metabolism indexes
between two groups (mean ± SD). |
Table II.
Comparison of lipid metabolism indexes
between two groups (mean ± SD).
| Indexes | Observation
group | Control group |
|---|
| TG (mmol/l) | 3.23±0.32 |
2.43±0.21a |
| TC (mmol/l) | 5.85±0.52 |
5.33±0.55a |
| HDL-C (mmol/l) | 1.80±0.12 |
2.09±0.21a |
| LDL-C (mmol/l) | 3.21±0.31 |
2.32±0.21a |
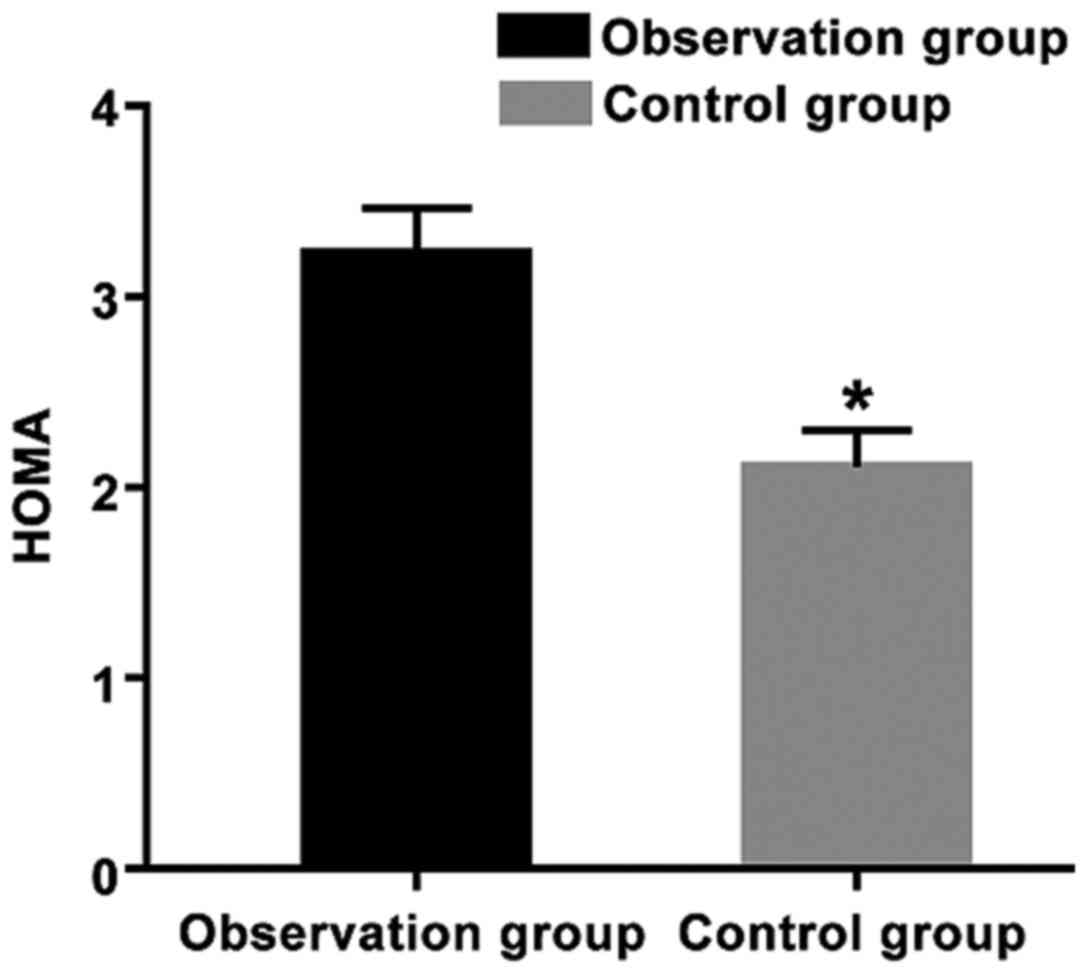
Comparison of insulin resistance
between two groups
HOMA index in the observation group was
significantly higher than that in the control group (P<0.05),
and the difference was statistically significant (Fig. 1).
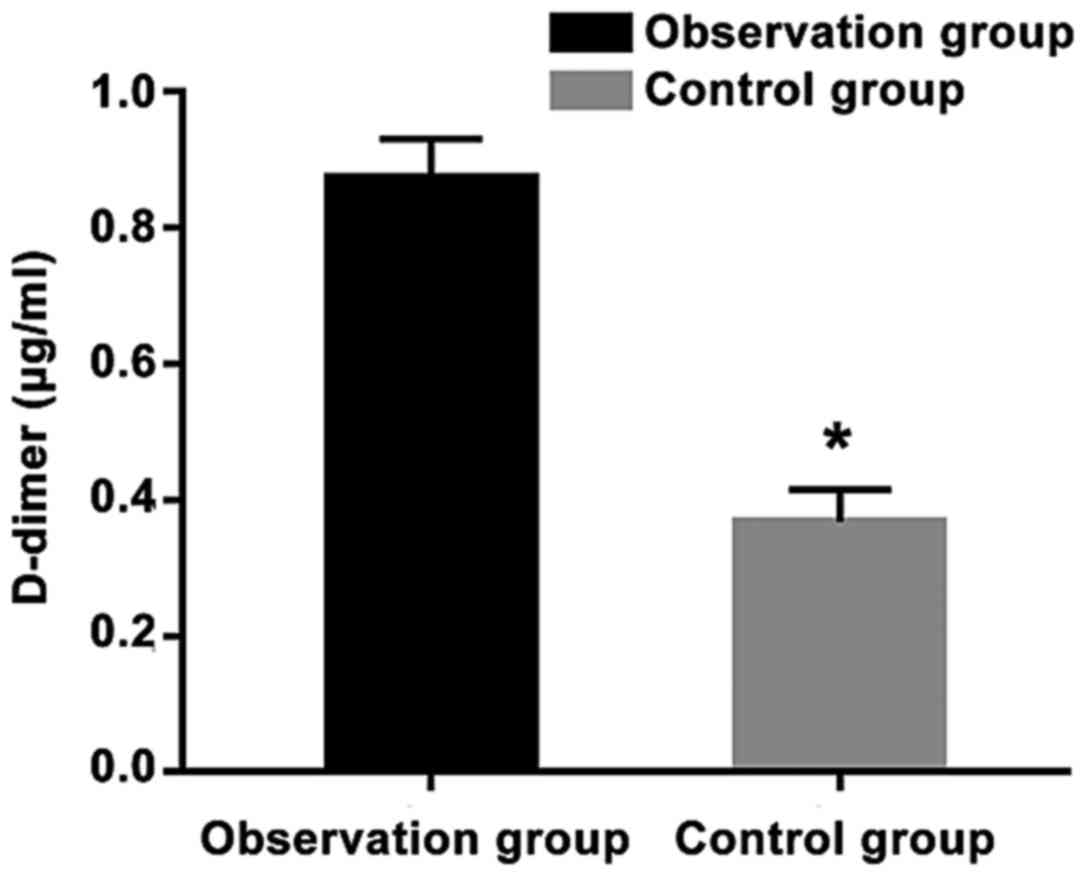
Comparison of D-dimer between two
groups
The level of D-dimer in the observation group was
significantly higher than that in the control group (P<0.05)
(Fig. 2).
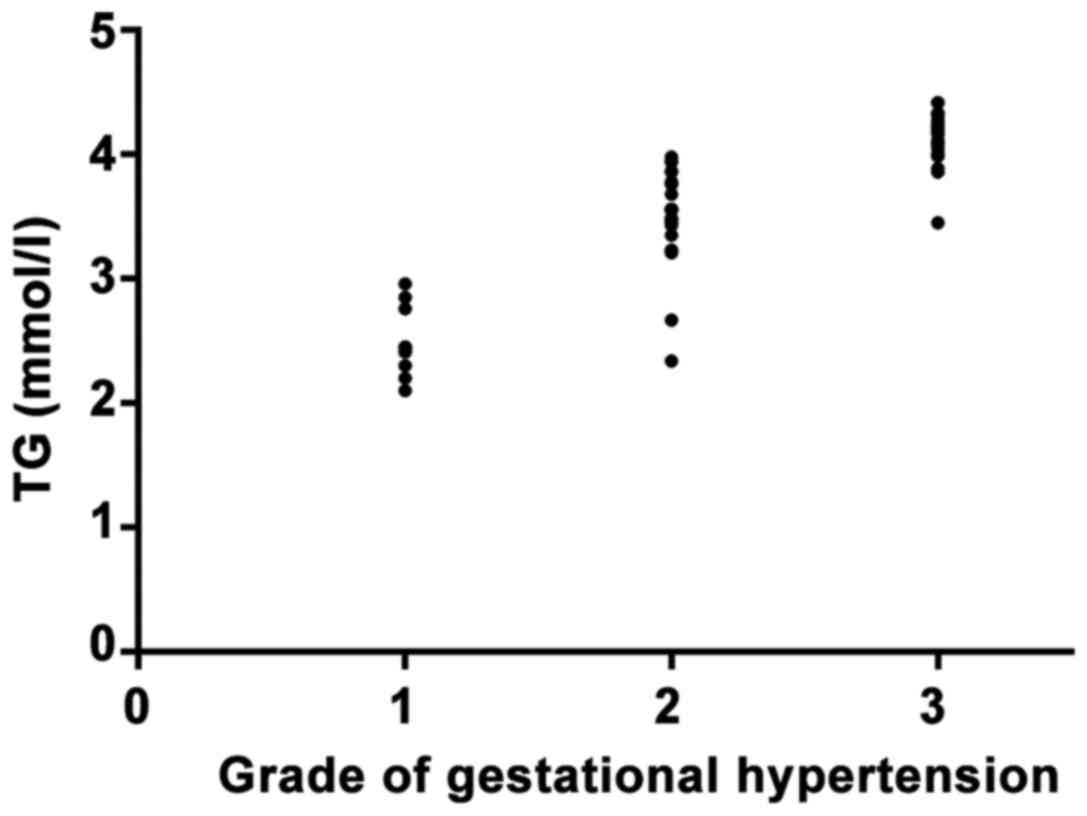
Correlation analysis of TG and the
grade of gestational hypertension
In the correlation analysis of TG and the grade of
gestational hypertension, it was found that TG was positively
correlated with gestational hypertension (r=0.8767, P<0.01)
(Fig. 3).
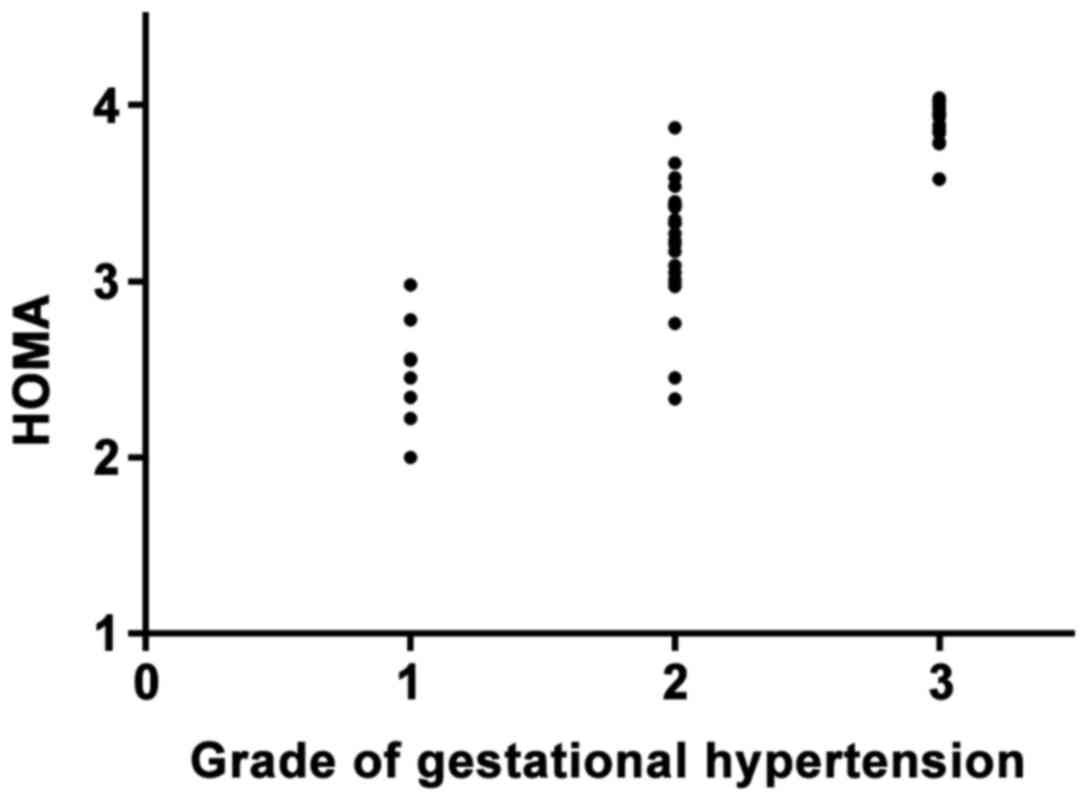
Correlation analysis of HOMA and the
grade of gestational hypertension
The correlation analysis of HOMA and the grade of
gestational hypertension demonstrated that HOMA was positively
correlated with gestational hypertension (r=0.8819, P<0.01)
(Fig. 4).
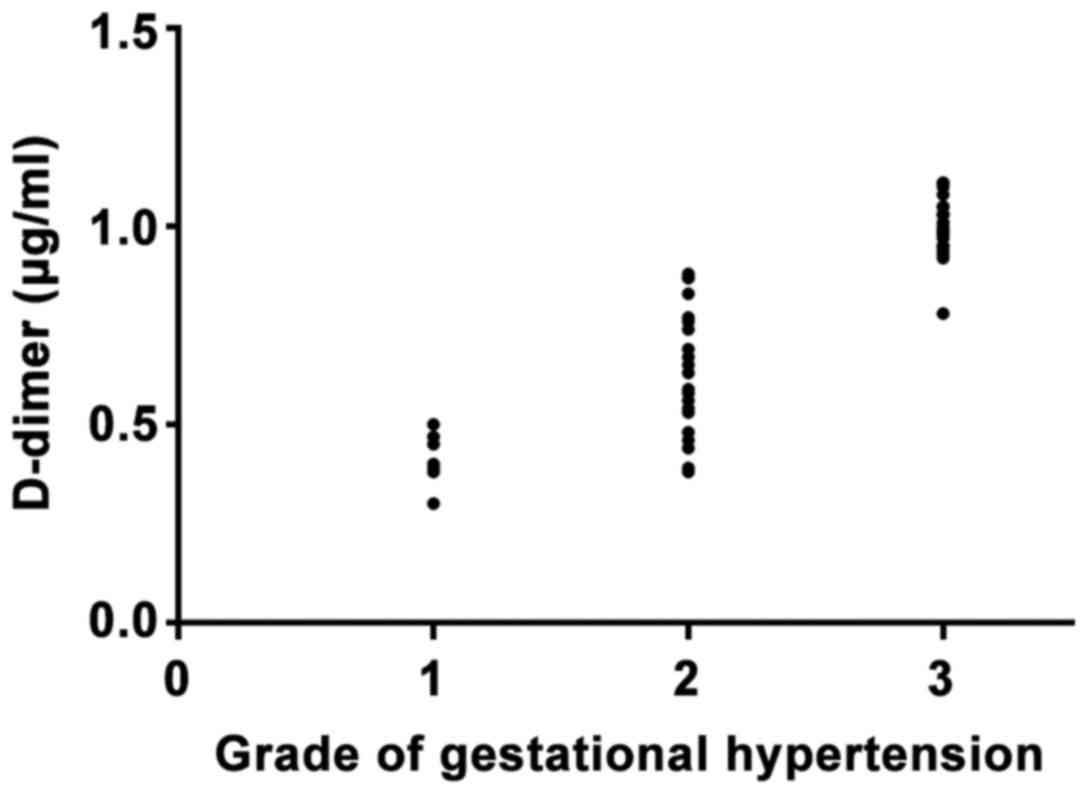
Correlation analysis of D-dimer and
the grade of gestational hypertension
In the correlation analysis of D-dimer and the
grades of gestational hypertension, it was revealed that D-dimer
was positively correlated with gestational hypertension (r=0.8933,
P<0.01) (Fig. 5).
Discussion
The morbidity rate of gestational hypertension is
higher among women during pregnancy, and if timely treatment is not
received, severe consequences will be caused, such as placental
abruption, shock and even death (10). Though great attention has been put on
gestational hypertension in clinic, its mechanism has not been
fully investigated. Therefore, there are considerable difficulties
in treatment (3,11).
Clinically, gestational hypertension is considered
to be correlated with endothelial injury. The more severe the
injury is, the higher the morbidity rate of gestational
hypertension will be. As abnormal lipid metabolism often leads to
vascular endothelial cell damage, it can be considered that there
is a correlation between abnormal lipid metabolism and gestational
hypertension (12,13).
In this study, it was found that the level of HDL-C
in the observation group was significantly lower than that in the
control group (P<0.05), while the levels of other indexes were
all significantly higher than those in the control group. Moreover,
gestational hypertension was found to be positively correlated with
TG, suggesting that the morbidity rate of gestational hypertension
will increase with the increased level of TG. Intestinal absorption
capacity of pregnant women will increase during pregnancy,
especially the absorption of fat, which may lead to the increased
levels of TG and TC in pregnant women.
In case of excessive increase, severe endothelial
cell damage will be caused, leading to gestational hypertension.
Besides, the level of HDL-C in the observation group was found to
be significantly lower than that in the control group during the
investigation, suggesting that the level of TG is very high in body
and its synthetic process is highly active, thus inhibiting the
histolysis function of surrounding tissues. In addition, the level
of LDL-C in the observation group was significantly higher than
that in the control group. When there is excessive LDL-C, part of
LDL-C is converted to oxidized LDL-C, which brings a series of
consequences, such as serious injury to endothelial cells, higher
cell permeability, more release of endothelin, higher blood
pressure and even intravascular coagulation (14,15).
In this study, the HOMA index in the observation
group was significant higher than that in the control group
(P<0.05) and HOMA was positively correlated with gestational
hypertension. Insulin resistance refers to the decrease in the
sensibility of tissues and muscles in body to insulin, which
results in such symptoms as lower sugar tolerance and abnormal
lipid metabolism. In this case, the conversion of glucose to TG is
promoted and the level of free fatty acid is increased, thus,
causing abnormal lipid metabolism (16,17).
Patients with gestational hypertension usually have
symptoms of spasm, blood coagulation and fibrinolysis, which result
in thrombus, seriously threatening the health of patients and
fetuses. Therefore, the occurrence of blood coagulation should be
reduced in treatment. D-dimer is the representative factor of
hyperfibrinolysis and its increase indicates that fibrinolysis
system activity is abnormal and the fibrinolysis function is
reduced (18,19). Moreover, the level of D-dimer in the
observation group was found to be significantly lower than that in
the control group in the study, and it was increased with the
exacerbation of the disease.
In conclusion, patients with gestational
hypertension are found to have abnormal lipid metabolism, higher
insulin resistance (HOMA) and significant higher D-dimer.
Gestational hypertension is positively correlated with TG, HOMA and
D-dimer. It is suggested that more attention should be paid to the
detection of the above-mentioned indexes in the treatment and
prevention of gestational hypertension, and preventive measures
should be enhanced once these indexes are found to be abnormal.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and material
All data generated or analyzed during this study are
included in this published manuscript. The datasets used and/or
analyzed during the current study are available from the
corresponding author on reasonable request.
Authors' contributions
YJ wrote the manuscript. YJ and MW recorded and
analyzed indexes of lipid metabolism. HX and BY interpreted indexes
of lipid metabolism. MZ and YZ helped with insulin resistance
index. JW detected D-dimer. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Jinhua People's Hospital (Jinhua, China) and informed consents were
signed by the patients or guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Sibai BM: Diagnosis and management of
gestational hypertension and preeclampsia. Obstet Gynecol.
102:181–192. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Wang YA, Chughtai AA, Farquhar CM, Pollock
W, Lui K and Sullivan EA: Increased incidence of gestational
hypertension and preeclampsia after assisted reproductive
technology treatment. Fertil Steril. 105:920–926.e2. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Zeng L, Yang K and Ge J: Uncovering the
pharmacological mechanism of astragalus salvia compound on
pregnancy-induced hypertension syndrome by a network pharmacology
approach. Sci Rep. 7:168492017. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Liang C, Wang J, Xia X, Wang Q, Li Z, Tao
R, Tao Y, Xiang H, Tong S and Tao F: Serum cobalt status during
pregnancy and the risks of pregnancy-induced hypertension syndrome:
A prospective birth cohort study. J Trace Elem Med Biol. 46:39–45.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Long ML, Xia AB, Cheng CX and Li RZ:
Therapeutic effect of hemin on gestational hypertension in rats and
the mechanism. Nan Fang Yi Ke Da Xue Xue Bao. 35:583–586. 2015.(In
Chinese). PubMed/NCBI
|
|
6
|
Wang JX, Knottnerus AM, Schuit G, Norman
RJ, Chan A and Dekker GA: Surgically obtained sperm, and risk of
gestational hypertension and pre-eclampsia. Lancet. 359:673–674.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Roberts JM, Bodnar LM, Lain KY, Hubel CA,
Markovic N, Ness RB and Powers RW: Uric acid is as important as
proteinuria in identifying fetal risk in women with gestational
hypertension. Hypertension. 46:1263–1269. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Guo J, Liu G and Guo G: Association of
insulin resistance and autonomic tone in patients with
pregnancy-induced hypertension. Clin Exp Hypertens. Nov
27–2017.(Epub ahead of print).
|
|
9
|
Ai L, Lan X, Wang L, Xu Y and Zhang B:
Clinical study on the influence of phloroglucinol on plasma
angiotensin II and D-Dimer index in patients with severe
pregnancy-induced hypertension. Pak J Pharm Sci. 29 Suppl
4:1375–1378. 2016.PubMed/NCBI
|
|
10
|
Saraswat L and Bhattacharya S, Maheshwari
A and Bhattacharya S: Maternal and perinatal outcome in women with
threatened miscarriage in the first trimester: A systematic review.
BJOG. 117:245–257. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Zhang W, Yuan W, Xu N, Li J and Chang W:
Icariin improves acute kidney injury and proteinuria in a rat model
of pregnancy-induced hypertension. Mol Med Rep. 16:7398–7404. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Yang LG, Song ZX, Yin H, Wang YY, Shu GF,
Lu HX, Wang SK and Sun GJ: Low n-6/n-3 PUFA ratio improves lipid
metabolism, inflammation, oxidative stress and endothelial function
in rats using plant oils as n-3 fatty acid source. Lipids.
51:49–59. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Yu JE, Han SY, Wolfson B and Zhou Q: The
role of endothelial lipase in lipid metabolism, inflammation, and
cancer. Histol Histopathol. 33:1–10. 2018.PubMed/NCBI
|
|
14
|
Kawai T, Ng MC, Hayes MG, Yoshiuchi I,
Tsuchiya T, Robertson H, Cox NJ, Polonsky KS, Bell GI and Ehrmann
DA: Variation in the perilipin gene (PLIN) affects glucose and
lipid metabolism in non-Hispanic white women with and without
polycystic ovary syndrome. Diabetes Res Clin Pract. 86:186–192.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Christoffersen C, Jauhiainen M, Moser M,
Porse B, Ehnholm C, Boesl M, Dahlbäck B and Nielsen LB: Effect of
apolipoprotein M on high density lipoprotein metabolism and
atherosclerosis in low density lipoprotein receptor knock-out mice.
J Biol Chem. 283:1839–1847. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Sun X, Zhang R, Jiang F, Tang S, Chen M,
Peng D, Yan J, Wang T, Wang S, Bao Y, et al: Common variants
related to serum uric acid concentrations are associated with
glucose metabolism and insulin secretion in a Chinese population.
PLoS One. 10:e01167142015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Medina-Urrutia A, Posadas-Romero C,
Posadas-Sánchez R, Jorge-Galarza E, Villarreal-Molina T,
González-Salazar MC, Cardoso-Saldaña G, Vargas-Alarcón G,
Torres-Tamayo M and Juárez-Rojas JG: Role of adiponectin and free
fatty acids on the association between abdominal visceral fat and
insulin resistance. Cardiovasc Diabetol. 14:202015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Wada T, Gando S, Maekaw K, Katabami K,
Sageshima H, Hayakawa M and Sawamura A: Disseminated intravascular
coagulation with increased fibrinolysis during the early phase of
isolated traumatic brain injury. Crit Care. 21:2192017. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Tanaka K, Kobayashi Y, Dozono K, Shibuya
H, Nishigaya Y, Momomura M, Matsumoto H and Iwashita M: Elevation
of plasma D-dimer levels associated with rupture of ovarian
endometriotic cysts. Taiwan J Obstet Gynecol. 54:294–296. 2015.
View Article : Google Scholar : PubMed/NCBI
|